Abstract
The Patient Care Connect Program (PCCP) is a lay patient navigation program, implemented by the University of Alabama at Birmingham Health System Cancer Community Network. The PCCP’s goal is to provide better health and health care, as well as to lower overall expenditures. The program focuses on enhancing the health of patients, with emphasis on patient empowerment and promoting proactive participation in health care. Navigator training emphasizes palliative care principles and includes development of skills to facilitate advance care planning conversations. Lay navigators are integrated into the health care team, with the support of a nurse supervisor, physician medical director, and administrative champion. The intervention focuses on patients with high needs to reach those with the greatest potential for benefit from supportive services. Navigator activities are guided by frequent distress assessments, which help to identify patient concerns across multiple domains, triage patients to appropriate resources, and ultimately overcome barriers to health care. In this article, we describe the PCCP’s development, infrastructure, selection and training of lay navigators, and program operations.
GERIATRIC ONCOLOGY WITHIN A STRAINED HEALTH CARE SYSTEM
The number of geriatric patients with cancer is anticipated to rise to unprecedented levels in the next 20 years; the current medical system is ill prepared for the influx of patients as a result of work force shortages and fragmentation in the health care system.1 In addition, the cost of cancer care has continued to increase at an unsustainable rate and is expected to reach $173 billion annually by 2020.2 Health system reforms are needed to better manage geriatric oncology patients, with the goal of reaching the triple aim of providing better health and health care while lowering overall costs.3
PATIENT NAVIGATION: A POTENTIAL SOLUTION
Patient navigation emerged in the 1990s as a potential strategy to expand the work force, improve coordination within the fragmented health care system, and eliminate barriers to timely diagnosis and treatment of cancer for vulnerable populations. Patient navigation is a patient-centered delivery model that aims to ensure timely access to health care services, guide patients through the increasingly complex health care system, and overcome barriers to health care.4 Many early patient navigators were nurses, but over the past decade a growing number of lay navigation programs have used non-nurse community members to provide these services to patients, particularly in underserved communities.5 The use of lay, or nonclinical, personnel allows for a low-cost expansion of the work force available to support patients with cancer.
Navigation programs have demonstrated reductions in cancer screening disparities, increased appointment adherence, improved clinical trial retention, and have resulted in improved patient satisfaction.6-15 These trials focused primarily on younger, vulnerable populations during the diagnostic and early treatment period. To our knowledge, there have been no navigation programs focused specifically on the geriatric oncology population. In addition, few navigation programs have supported patients across the cancer trajectory, from diagnosis through survivorship and until the end of life. We anticipate that navigating geriatric patients during all phases of cancer care may reduce costs through reductions in avoidable emergency room (ER) visits and hospitalizations. In addition, supporting patients across the cancer continuum may allow for earlier recognition of the need for palliative and supportive care services aimed at maintaining function and quality of life, and obviate overly aggressive treatment and hospitalization at the end of life.16 Therefore, we developed the Patient Care Connect Program (PCCP), a lay navigation program across the cancer trajectory for geriatric patients with cancer. The goal of this article is to describe the development, infrastructure, lay navigator selection and training, and program operations of the PCCP.
SETTING THE STAGE
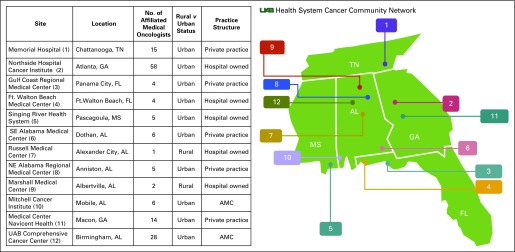
The University of Alabama at Birmingham Health System Cancer Community Network
The PCCP was implemented in the University of Alabama at Birmingham (UAB) Health System Cancer Community Network (CCN), which includes 12 cancer centers located in five states in the Deep South (Alabama, Georgia, Florida, Mississippi, and Tennessee; Appendix Fig A1, online only). It comprises academic medical centers and community cancer centers located in geographically distinct regions, both rural and urban. The practice structures vary among sites and include hospital-based practices and affiliated traditional private practices. The number of medical oncologists at each site ranges from a single medical oncologist at Russell Medical Center in Alexander City, Alabama to a 58-oncologist multisite practice at Northside Hospital Cancer Institute in Atlanta, Georgia. The network represents a microcosm of the United States, with the variety of practices engaged and patient populations served.
Preparing Sites for Navigation
The successful introduction and effectiveness of the lay navigators within the health care team requires engagement with key stakeholders and assessment of organizational readiness. Given that the PCCP aims to reduce health care utilization, and potentially hospital revenue, hospital leadership and clinical staff must share an understanding of program goals. Therefore, before implementation, UAB administrators met with site administrators to discuss potential implications for the health system. The UAB administrators emphasized the likelihood of a transition from fee-for-service payment to value-based health care17,18 and argued that the PCCP could prepare sites for this transition. In addition, sites could become preferred providers in their regions, thus achieving the CCN’s mission of delivering local, high-quality care.
Developing the PCCP Infrastructure
The program is composed of the PCCP coordinating center at UAB and PCCP teams at the participating sites. The coordinating center includes a PCCP leadership team consisting of the medical director, administrative director, director of nursing, and other support staff. The coordinating center provides infrastructure and support that could not be achieved locally, including navigator training, program implementation, quality control audits, monitoring and sharing of results, and communication of best practices across the CCN.
The PCCP site teams include trained lay navigators, a registered nurse site manager, a physician medical director, and an administrative champion. The nurse site manager supervises the team of lay navigators and addresses clinical concerns. The administrator and medical director provide support to the nurse site manager and navigators to ensure program success. The multilevel, interprofessional nature of the team facilitates the integration of lay navigators into the care team and promotes the link among patients, oncologists and their staff, community-based referring physicians and staff, hospitals in the CCN, and community resources that can assist patients.
Physician Engagement
Sites identify medical directors who have influence within the community and the ability to garner support for the program. The medical directors for the PCCP include medical, radiation, and surgical oncologists. Medical director responsibilities include: encouraging all physicians and staff to integrate lay navigators into the care team; participating in the navigation teams through regular contact with the site manager and as-needed contact with lay navigators for difficult cases; acting as a liaison between the PCCP leadership team and the community physicians at their locations; providing information about the PCCP at local events (eg, cancer committee meetings); and participating in quality improvement to address quality-of-care gaps identified during program implementation.
Communication Strategy
The communication strategy between the UAB and the sites is built upon both interdisciplinary and peer-to-peer communications to maximize efficiency and uptake of the program. We use regular in-person, telephone, and online communications to maintain frequent contact between the PCCP leadership team and PCCP sites. We also conduct annual meetings to bring team members together from all sites for education and to share program successes, challenges, and best practices.
Navigator selection
To align the lay navigators with the unique local CCN communities, each network site selects and hires lay navigators independently, with minimal restrictions from the UAB. Because of the advanced nature of services provided, lay navigators are required to have a bachelor’s degree, yet are not licensed clinical providers, such as nurses or social workers. The recommended characteristics of an effective lay navigator include being empathetic, respectful, warm, genuine, trustworthy, empowering, communicative, and professional.
Navigation framework
The PCCP is grounded in the frameworks of empowerment and health promotion. Lay navigators concentrate on helping patients achieve health, rather than emphasizing disease. Lay navigators promote personal empowerment for the patient and his/her caregiver(s) and proactive participation in health care. The lay navigator partners with the patient, providing psychosocial support, information, opportunities for problem solving, and logistical assistance to mitigate or overcome obstacles to health.13,19,20
Navigator training
The curriculum was developed and delivered by a multidisciplinary team that comprises clinical and research faculty from medicine, psychology, allied health, nursing, social work, and chaplain services. We use multiple training modalities including Web-based self-paced modules, in-person skills workshops, and telephone-based booster sessions. Core training components include the following:
Navigation basics: Training modules focus on basic concepts of health promotion, empowerment, the history of navigation, and navigation principles. This training also highlights practical skills, such as effective communication, distress screening, critical thinking, problem solving to overcome barriers to health care, experiences of cancer patients (eg, navigating the cancer journey), time management, managing compassion fatigue and setting boundaries, data collection using navigation software, and use of care maps.
Advanced navigation: After lay navigators complete the above training, we provide advanced training specific to the needs of the PCCP. Topics include reasons for ER visits within the geriatric oncology population, palliative care principles, caregiver interactions, motivational interviewing skills, and identification of personal and community resources to address barriers to patient care.
Addressing pain, fatigue, and functional mobility: We include educational modules on the top three patient-reported distress items identified by PCCP self-monitoring: pain, fatigue, and mobility problems. During the training module, a personal trainer demonstrates exercises that are appropriate for geriatric oncology patients. Training also includes identification of reliable resources for patient education, such as the American Cancer Society and the National Institutes of Health materials on pain and fatigue21-26 and geriatric oncology–specific exercise materials from the National Institute on Aging (Exercise & Physical Activity-Go4Life).27 Together, these resources are aimed at improving the navigator’s ability to empower patients to maintain a healthy lifestyle.
Advance care planning education: We train the lay navigators and site managers to facilitate advance care planning conversations using the Respecting Choices curriculum.28 They complete six online modules with content regarding advance care planning, choosing a decision maker, and documentation of preferences. The training is solidified with an in-person 1-day practicum led by a UAB training team. Upon completion of the training, the lay navigators engage patients and decision makers in advance care planning.
Target population and triage mechanisms
All Medicare primary fee-for-service beneficiaries ≥ 65 years old, with a cancer diagnosis after 2008, are eligible for receipt of navigation services as a part of standard of care. Incarcerated patients and nursing home residents are excluded. To target patients who are at high risk, special emphasis is placed on individuals with metastatic disease, cancers with high morbidity and mortality (eg, lung, pancreatic), high distress, psychosocial needs, or patients have barriers to receiving appropriate cancer care (Table 1). To target these high-acuity, high-risk patients, lay navigators and/or site managers review ER and hospital census reports to identify eligible patients to enroll in the program. Navigation teams also encourage providers to refer patients with high levels of psychosocial distress, multiple concerns, or provider-identified barriers to care. These strategies result in a high proportion of navigated patients with high-risk cancers of advanced stage. Thus, the PCCP actively targets this high-need population with the greatest capacity for change with the addition of supportive services.29
Table 1.
Characteristics of Patients Navigated in the Patient Care Connect Program Between January 1, 2014, and June 30, 2015
| Characteristic | No. | % |
|---|---|---|
| Age, years | ||
| 65-74 | 4,412 | 50.2 |
| 75-84 | 3,370 | 38.4 |
| ≥ 85 | 1,005 | 11.4 |
| Sex | ||
| Female | 4,688 | 53.4 |
| Male | 4,039 | 46 |
| Missing | 60 | 0.7 |
| Race/ethnicity | ||
| White | 7,368 | 83.9 |
| Black | 1,171 | 13.3 |
| Asian | 46 | 0.5 |
| Hispanic | 28 | 0.3 |
| Other/missing | 174 | 2 |
| Cancer type (top five) | ||
| Breast | 1,748 | 18.1 |
| Lung | 1,665 | 17.3 |
| Prostate | 791 | 8.2 |
| Colon | 725 | 7.5 |
| Skin | 574 | 6 |
| Navigated patients by site, range | ||
| Program size | ||
| Large (≥ 500 beds; three sites) | 967-1,113 | 24 |
| Medium (250-499 beds; four sites) | 320-1,094 | 63 |
| Small (< 250 beds; four sites) | 200-938 | 13 |
Navigation tools
The PCCP uses three critical strategies to streamline and standardize navigation services: (1) care maps for interventions; (2) comprehensive distress assessment; and (3) a navigation software platform.
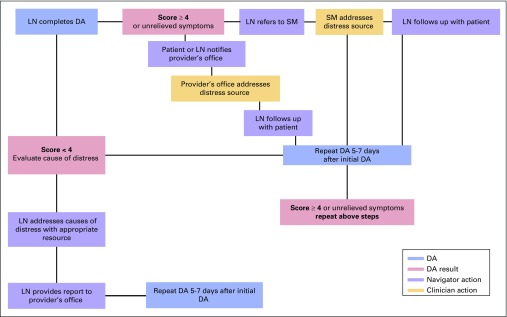
Care maps: The care maps are interventional process guides that provide a workflow sequence and timing for the lay navigator to interact with the patient, the site manager, and the physician on the basis of the patient’s self-reported issue or their specific time point in care. The care maps are intended to provide consistency in navigator interventions and interprofessional communication. Specific care maps address the process for managing patients receiving radiation/chemotherapy and those reporting specific concerns such as high distress, significant symptoms, or knowledge deficits. A care map for navigator distress assessment is shown in Fig 1.
Distress assessment: The PCCP comprehensive, interactive distress assessment tool was modeled after the distress thermometer used by the National Cancer Comprehensive Network.30 The tool includes a thermometer image, which quantifies the level of distress from zero (no distress) to ten (extreme distress). Distress scores equal to or greater than four signify elevated levels of anxiety and distress,31 and prompt navigator intervention. The tool also contains a problem list to delineate the sources of distress within the last week.32,33 To provide a comprehensive view of a patient’s distress, lay navigators identify distress related to the following domains: Practical, Family, Emotional, Spiritual, Financial, and Physical. We expand the problem list under each domain to include additional barriers identified from lay navigator encounters with patients or through literature review.34-36
Navigation software: The 12 participating sites used different electronic medical records (EMR); thus there was a need to develop a network-wide electronic solution for documentation. To track the lay navigator work process and to capture consistent data across sites, we worked collaboratively with a navigation software vendor, Medical Concierge, to further develop a publicly available, Web-based navigation software that enables lay navigators to track encounters with patients, providers, and community resources and help guide patient engagement. This system labels patients as high risk on the basis of specific cancer type, comorbidities, and medications. This allows the lay navigator to tailor interactions according to these risk factors. This software also incorporates the previously described distress assessment tool that helps lay navigators to document patient distress, prompts the lay navigator to assess specific barriers, and explores potential resolutions in an objective, consistent manner. The platform is designed to include select data elements and drop-down boxes with minimal free-text fields to simplify reporting and increase capacity. Reports are run in real time at both the site and lay navigator levels to monitor progress, trends, and compliance with PCCP protocols. Although the reports did not integrate with the EMRs, physicians at each site developed a preferred reporting style of navigator–physician communication. For example, several sites provided paper summary reports of patient interactions on a weekly basis, others requested that reports be faxed into the EMR, and some preferred direct communication between the navigator and physician or nurse.
FIG 1.
Distress assessment (DA) care map. LN, lay navigator; SM, nurse site manager.
Navigator contacts
The PCCP navigators engage with providers and patients beyond traditional, in-person clinic and hospital settings. Navigators contact patients via telephone, mail, and face-to-face encounters during clinical care visits. The frequency of contact varies based on patient-reported distress. Active patients, defined by patient-reported distress scores ≥ four or those with requests for assistance, are contacted at least monthly, and high-acuity patients are contacted more frequently. Patients who report low distress and no significant concerns are contacted at least once every 3 months.
Case Example.
Day 1: Ms Jones is a 70-year-old woman with lung cancer who is seen in the emergency room (ER) for nausea and vomiting while on chemotherapy.
Day 2: The nurse site manager identifies her as an eligible patient for PCCP through an ER census report and assigns a navigator to her case.
Day 3: The navigator meets Ms Jones at her follow-up clinic appointment and completes a distress assessment. Ms Jones reports a distress level of 5. She expresses concerns about her pain, feeling depressed, and lack of transportation to her clinic appointments. The navigator communicates the patient’s reports of pain and depression to the clinic nurse and oncologist, who make a referral to the palliative and supportive care clinic. The navigator connects the patient with a resource that provides gas cards, which her niece is able to use to drive her to the clinic for appointments.
Day 10: The navigator follows up with the patient 1 week later at 9 AM. The patient reports that she called the clinic due to nausea and vomiting, but gave up because the phone triage took “too long.” She is thinking of going to the ER again. The navigator calls the clinic nurse, who contacts the patient and establishes an urgent care appointment and intravenous hydration in the infusion center.
Navigator operations are shown in Table 2. Over the period from January 1, 2014 to June 30, 2015, on average, each navigator was assigned 152 patients per quarter, of whom 91 were high-acuity patients (Table 2). Navigators completed an average of 275 contacts per quarter, for a mean of 2.9 contacts per patient per quarter. The maximum number of contacts for an individual patient was 73 contacts in one quarter.
Table 2.
Navigator Activities Between January 1, 2014, and June 30, 2015
| Navigator Activities Per Quarter | Average | Range |
|---|---|---|
| Average number of navigators | 37 | 31-40 |
| Average number of patients per navigator | 152 | 105-213 |
| High-acuity patients* | 91 | 64-126 |
| New patients | 31 | 23-40 |
| Average number of contacts per quarter | 275 | 246-312 |
| Mode of patient contact | ||
| Face-to-face | 117 | 109-127 |
| Telephone | 158 | 136-185 |
| Provider/resource | 40 | 33-46 |
| Percentage of patients with a face-to-face contact | 62.2 |
NOTE. Average includes all quarters, and ranges are reported per navigator.
High acuity is defined as the presence of stage IV cancer, a high-morbidity cancer, high-risk comorbidities or medication, or with distress scores ≥ 4.
During these contacts, the navigator screens for distress and causes of distress, as demonstrated in the case example of Ms Jones. They identify and collaborate with the patient to address concerns early to minimize the likelihood of adverse outcomes, such as patients missing follow-up appointments or experiencing symptoms that might lead to a hospitalization if not promptly addressed. In addition, navigators encourage the patient to call either the navigator or the health care team rather than presenting directly to the ER for non–life-threatening concerns. Navigators also promote shared decision making by empowering patients to participate in health care decisions. For example, they conduct advance care planning conversations and encourage patients to ask questions of their medical team to better understand their disease.
Resolution or Requests for Assistance
Navigator interventions are based on patient-reported distress items. In 34% of cases, patients request help from the navigator for their specific cause of distress. Navigators use several strategies to address concerns and 92% are resolved, often directly, by the navigator. For example, lay navigators often address transportation needs by helping patients identify family members or friends who can assist them. When this is not possible, lay navigators can connect patients with community resources such as “Angel Wheels to Healing,”37 or other charitable organizations that provide gas cards or transportation. For information needs, lay navigators provide written or electronic information, using material from the National Cancer Institute, American Cancer Society, and other trusted resources. For clinical concerns, navigators encourage patients to write down questions or call clinical staff directly, thus empowering the patient to communicate concerns. Navigators then follow up with the patients to close the communication loop and resolve the patient’s concern. This approach encourages the patient to be proactive in managing their health care. Another strategy, typically used for more serious concerns, is to escalate the issue directly to the patient’s health care provider or the nurse site manager (Fig 1).
Patient Satisfaction
Patient satisfaction with the navigation program is high: 83% (n = 336) are satisfied or very satisfied, 14% are neutral or uncertain, and 3% are unsatisfied or very unsatisfied. Perhaps more importantly, when asked if they would recommend the program to another cancer survivor, 89.5% of navigated patients surveyed reported yes, 7.8% were uncertain, and 2.7% would not recommend the program.
The PCCP is evaluated using data from the navigation software system, patient surveys, and Medicare administrative claims. Data from the navigation software are used to monitor navigation workload and process measures, such as the number and type of patients enrolled, the number and length of navigator contacts, the distress items selected, the assistance provided, and the time from the assistance request to resolution. The patient surveys measure quality of life, symptom burden, and satisfaction with their health care and the PCCP. The claims data are used to monitor the utilization of health care services (eg, ER visits, hospitalizations, admissions to the intensive care unit, hospice use, and chemotherapy at the end of life) and the cost to Medicare. This continuous data monitoring and feedback is critical for making adjustments to the program, demonstrating program value, and fostering a culture of quality improvement and opportunities for future research.
CONCLUSION
The PCCP is a lay patient navigation program that redesigns the way patient care is delivered. It is intended to improve health, enhance health care quality, and lower costs. The PCCP is hardwired for patient-centeredness by anchoring all navigator–patient interactions in patient distress assessment. The PCCP moves beyond traditional lay navigation programs, which focused on triaging patients to appropriate services, by training navigators in evidence-based strategies to activate and engage patients in health care. The emphasis on empowering patients is essential to the function of this navigation program, which maintains a high patient-to-navigator ratio, while leading the CCN toward delivery of high-quality care and improved patient outcomes. Effort should also be invested in training site health care systems to be proactive and engaged in the care of patients who are at high risk. Essential implementation strategies include the selection of influential site champions and ongoing efforts to guide and nurture their onsite PCCP leadership. The PCCP providers and administrators are critical in supporting lay navigator integration and promoting a culture of quality through sharing of data and best practices across the CCN. This program may be well positioned to support systems in the transition to high-quality, high-efficiency health care and to add to value-based payment models.
Acknowledgment
G.B.R. is supported by a Walter B. Frommeyer Jr. Fellowship in Investigative Medicine. This funding source had no role in the design and conduct of the study; collection, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript for publication. The project described was supported by Grant No.1C1CMS331023 from the Department of Health and Human Services, Centers for Medicare & Medicaid Services. The contents of this article are solely the responsibility of the authors and do not necessarily represent the official views of the US Department of Health and Human Services or any of its agencies. The research presented here was conducted by the awardee. Findings might or might not be consistent with or confirmed by the findings of the independent evaluation contractor. Patient Care Connect Group members and affiliations are listed in the Appendix (online only). We acknowledge John French III, the University of Alabama at Birmingham lead navigator, for his contribution to this article.
Appendix
FIG A1.
The University of Alabama at Birmingham (UAB) Health System Cancer Community Network (CCN): Locations and practice characteristics. AMC, academic medical center.
Patient Care Connect Group
Memorial Hospital, Chattanooga, TN: Lee Jackson, MD, Zoe Scott
Northside Hospital Cancer Institute, Atlanta, GA: Guilherme Cantuaria, MD, Debbie Bickes, Tina Berry
Gulf Coast Regional Medical Center, Panama City, FL: George Reiss, MD, Hang Mai
Ft Walton Beach Medical Center, Ft. Walton Beach, FL: Ming-Chen Chang, MD, Louiz Gomez, Rhonda Meeker
Singing River Health System, Pascagoula, MS: James Clarkson, MD, Maggie Clarkson
Southeast Alabama Medical Center, Dothan, AL: Steven Stokes, MD, Tina Newman
Russell Medical Center, Alexander City, AL: Mary Sheffield, DO
Northeast Alabama Regional Medical Center, Anniston, AL: Ellen Spremulli, MD, Wendy Watson
Marshall Medical Center, Albertville, AL: Tom Payne, MD, Hanna Bright, Stacey Holman
Mitchell Cancer Institute, Mobile, AL: Thomas Butler, MD, Cathy Tinnea
Medical Center Navicent Health, Macon, GA: Fred Schnell, MD, Cyndi Pyle
UAB Comprehensive Cancer Center, Birmingham, AL: Gabrielle B. Rocque, MD, Richard Taylor, DNP, CRNP, Aras Acemgil, MBA, Xuelin Li, PhD, Kelly M. Kenzik, PhD, Bradford E. Jackson, MD, Karina I. Halilova, MD, MPH, Maria Pisu, PhD, Wendy Demark-Wahnefried, PhD, RD, Karen Meneses, RN, PhD, Yufeng Li, PhD, Michelle Y. Martin, PhD, Carol Chambless, Nedra Lisovicz, PhD, MPH, Valeria Pacheco-Rubi, Terri L. Salter, Warren Smedley, Mona Fouad, MD, MPH, Elizabeth A. Kvale, MD, Edward E. Partridge, MD
AUTHOR CONTRIBUTIONS
Conception and design: Gabrielle B. Rocque, Edward E. Partridge, Maria Pisu, Michelle Y. Martin, Wendy Demark-Wahnefried, Aras Acemgil, Elizabeth A. Kvale, Karen. Meneses, Karina I. Halilova, Nedra Lisovicz, Mona Fouad, Richard A. Taylor
Collection and assembly of data: Gabrielle B. Rocque, Maria Pisu, Aras Acemgil, Xuelin Li, Yufeng Li, Carol Chambless
Data analysis and interpretation: Gabrielle B. Rocque, Edward E. Partridge, Maria Pisu, Wendy Demark-Wahnefried, Aras Acemgil, Kelly Kenzik, Elizabeth A. Kvale, Yufeng Li, Bradford E. Jackson, Richard A. Taylor
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
The Patient Care Connect Program: Transforming Health Care Through Lay Navigation
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Gabrielle B. Rocque
Honoraria: Medscape
Research Funding: PackHealth, Medscape, Carevive Systems
Travel, Accommodations, Expenses: Medscape
Edward E. Partridge
No relationship to disclose
Maria Pisu
No relationship to disclose
Michelle Y. Martin
No relationship to disclose
Wendy Demark-Wahnefried
No relationship to disclose
Aras Acemgil
No relationship to disclose
Kelly Kenzik
No relationship to disclose
Elizabeth A. Kvale
Employment: Aspire Health
Karen Meneses
Honoraria: QHealth
Xuelin Li
No relationship to disclose
Yufeng Li
No relationship to disclose
Karina I. Halilova
No relationship to disclose
Bradford E. Jackson
No relationship to disclose
Carol Chambless
No relationship to disclose
Nedra Lisovicz
No relationship to disclose
Mona Fouad
No relationship to disclose
Richard A. Taylor
No relationship to disclose
References
- 1. Levit L, Balogh E, Nass S, et al (eds): Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, DC, National Academies Press, 2013. [PubMed] [Google Scholar]
- 2.American Society of Clinical Oncology : The state of cancer care in America, 2014: A report by the American Society of Clinical Oncology J Oncol Pract 10:119–142,2014 [DOI] [PubMed] [Google Scholar]
- 3.Berwick DM, Nolan TW, Whittington J: The triple aim: Care, health, and cost Health Aff (Millwood) 27:759–769,2008 [DOI] [PubMed] [Google Scholar]
- 4. doi: 10.1016/j.soncn.2013.02.002. Freeman HP: The history, principles, and future of patient navigation: Commentary. Semin Oncol Nurs 29:72-75, 2013. [DOI] [PubMed] [Google Scholar]
- 5.Hedlund N Risendal BC Pauls H, etal: Dissemination of patient navigation programs across the United States J Public Health Manag Pract 20:E15–E24,2014 [DOI] [PubMed] [Google Scholar]
- 6.Fouad M Wynn T Martin M, etal: Patient navigation pilot project: Results from the Community Health Advisors in Action Program (CHAAP) Ethn Dis 20:155–161,2010 [PubMed] [Google Scholar]
- 7.Fouad MN Partridge E Dignan M, etal: Targeted intervention strategies to increase and maintain mammography utilization among African American women Am J Public Health 100:2526–2531,2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lisovicz N Johnson RE Higginbotham J, etal: The Deep South Network for cancer control. Building a community infrastructure to reduce cancer health disparities Cancer 107:1971–1979,2006 [DOI] [PubMed] [Google Scholar]
- 9.Partridge EE Fouad MN Hinton AW, etal: The Deep South network for cancer control: Eliminating cancer disparities through community-academic collaboration Fam Community Health 28:6–19,2005 [DOI] [PubMed] [Google Scholar]
- 10.Fouad MN Johnson RE Nagy MC, etal: Adherence and retention in clinical trials: A community-based approach Cancer 120:1106–1112,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Freund KM Battaglia TA Calhoun E, etal: Impact of patient navigation on timely cancer care: The Patient Navigation Research Program J Natl Cancer Inst 106:dju115,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Freund KM Battaglia TA Calhoun E, etal: National Cancer Institute Patient Navigation Research Program: Methods, protocol, and measures Cancer 113:3391–3399,2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Paskett ED, Harrop JP, Wells KJ: Patient navigation: An update on the state of the science CA Cancer J Clin 61:237–249,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wagner EH Ludman EJ Aiello Bowles EJ, etal: Nurse navigators in early cancer care: A randomized, controlled trial J Clin Oncol 32:12–18,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hryniuk W Simpson R McGowan A, etal: Patient perceptions of a comprehensive cancer navigation service Curr Oncol 21:69–76,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rocque GB, Cleary JF: Palliative care reduces morbidity and mortality in cancer Nat Rev Clin Oncol 10:80–89,2013 [DOI] [PubMed] [Google Scholar]
- 17.Clough JD, Kamal AH: Oncology care model: Short- and long-term considerations in the context of broader payment reform J Oncol Pract 11:319–321,2015 [DOI] [PubMed] [Google Scholar]
- 18. Stanek M: Quality Measurement to Support Value-Based Purchasing: Aligning Federal and State Efforts. Washington, DC, National Academy for State Health Policy, 2014. [Google Scholar]
- 19.Carroll JK Humiston SG Meldrum SC, etal: Patients’ experiences with navigation for cancer care Patient Educ Couns 80:241–247,2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Adler NE, Page AEK (eds): Cancer Care for the Whole Patient: Meeting Psychosocial Health Needs. Washington, DC, National Academies Press, 2008. [PubMed] [Google Scholar]
- 21. American Cancer Society: Daily Pain Diary. 2012 (004620). www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-033203.pdf.
- 22. American Cancer Society: Getting Help for Cancer Pain, 2009 (213300). 5/14 update. www.cancer.org/acs/groups/content/@editorial/documents/document/acspc-031603.pdf.
- 23. Pain Control: Support for People With Cancer. Bethesda, MD, National Cancer Institute, NIH publication No. 14-6287, 2014. 3/29/13 update.
- 24. American Cancer Society: Fatigue (Feeling Weak and Very Tired): Managing Chemotherapy Side Effects. National Cancer Institute, NIH, 2012. 2/12 update www.cancer.gov/publications/patient-education/fatigue.pdf.
- 25. American Cancer Society: Fatigue in People With Cancer, 2014. 10/22/14 update www.cancer.org/acs/groups/cid/documents/webcontent/002842-pdf.pdf.
- 26.2014. Talking With Your Doctor: A Guide for Older People. Bethesda, MD, National Institute on Aging, NIH publication No. 05-34521/22/15 update https://www.nia.nih.gov/health/publication/talking-your-doctor/opening-thoughts-why-does-it-matter.
- 27. Exercise & Physical Activity: Your Everyday Guide from the National Institute on Aging at NIH. National Institute on Aging, NIH publication No. 15-4258, 2015. 5/28/15 updated https://www.nia.nih.gov/health/publication/exercise-physical-activity/introduction.
- 28.Pecanac KE Repenshek MF Tennenbaum D, etal: Respecting Choices® and advance directives in a diverse community J Palliat Med 17:282–287,2014 [DOI] [PubMed] [Google Scholar]
- 29.Yabroff KR Lamont EB Mariotto A, etal: Cost of care for elderly cancer patients in the United States J Natl Cancer Inst 100:630–641,2008 [DOI] [PubMed] [Google Scholar]
- 30.Donovan KA, Jacobsen PB: Progress in the implementation of NCCN guidelines for distress management by member institutions J Natl Compr Canc Netw 11:223–226,2013 [DOI] [PubMed] [Google Scholar]
- 31.Baken DM, Woolley C: Validation of the Distress Thermometer, Impact Thermometer and combinations of these in screening for distress Psychooncology 20:609–614,2011 [DOI] [PubMed] [Google Scholar]
- 32. National Comprehensive Cancer Network: Development and Update of the NCCN Guidelines. https://www.nccn.org/professionals/physician_gls/guidelines-development.asp.
- 33.Vitek L, Rosenzweig MQ, Stollings S: Distress in patients with cancer: Definition, assessment, and suggested interventions Clin J Oncol Nurs 11:413–418,2007 [DOI] [PubMed] [Google Scholar]
- 34.Graves KD Arnold SM Love CL, etal: Distress screening in a multidisciplinary lung cancer clinic: Prevalence and predictors of clinically significant distress Lung Cancer 55:215–224,2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tuinman MA, Gazendam-Donofrio SM, Hoekstra-Weebers JE: Screening and referral for psychosocial distress in oncologic practice: Use of the Distress Thermometer Cancer 113:870–878,2008 [DOI] [PubMed] [Google Scholar]
- 36.Carlson LE, Waller A, Mitchell AJ: Screening for distress and unmet needs in patients with cancer: Review and recommendations J Clin Oncol 30:1160–1177,2012 [DOI] [PubMed] [Google Scholar]
- 37.Angel Wheels for Healing : http://angelwheels.org