Abstract
[Purpose] To verify the effects of individual and group exercise programs on pain, balance, mobility and perceived benefits of rheumatoid arthritis patients (RA) with pain and foot deformities. [Subjects and Methods] Thirty patients with RA pain and foot deformity were allocated into two groups: G1: individual exercise program and G2: group exercise program. The variables analyzed were Numerical Rating Scale (NRS) for pain, Berg Balance Scale (BBS) for balance, Timed Up & Go Test (TUG) and Functional Reach (FR) for mobility, and Foot Health Status Questionnaire (FHSQ-Br) for perceived benefits. Both exercise programs consisted of functional rehabilitation exercises and self-care guidance aimed at reducing pain and improving balance and mobility. Intragroup comparisons of variables between A1 (pre-intervention) and A2 (post-intervention) were performed. [Results] Patients in both groups were similar in A1 (pre-intervention) in all the variables analyzed. Comparison between A1 and A2 for each variable showed improvement for G1 in the NRS, BBS, FR, TUG and in four out of ten domains of FHSQ-Br. G2 showed improvement in the NRS, BBS and eight out of ten domains of FHSQ-Br. [Conclusion] Both individual and group programs revealed benefits for patients with RA, however, group exercise programs showed better perception of benefits.
Keywords: Exercise therapy, Mobility limitation, Rheumatoid arthritis
INTRODUCTION
Rheumatoid arthritis (RA) is a common systemic disease in which foot involvement has been largely damaged. Synovial hypertrophy and capsular tension generated by hyperplasia, ligamentous laxity, muscular imbalance and ultimately joint subluxation and dislocation all play a role in the development of foot deformities in RA. Furthermore, inflammation causes destruction in the cartilage and pericapsular structures. Due to these changes, the loading on joints causes different deformities and constitutes a severe disability in the patient’s mobility and functional independence.
A functional foot must reveal musculoskeletal integrity such as joint alignment and range of motion, mobility and muscular strength1). Healthy feet are also essential for posture and balance control, as well as effective propulsion during gait and mobility2, 3). Many reports state that impairment of foot somatosensory information leads to balance instability and produces a severe negative impact on mobility and in activities of daily living4, 5). Plantar sensitivity is decreased in patients with RA, reinforcing that RA patients show deficits in balance and functional activities as a result of alterations of foot functioning2, 3, 6).
Despite the significant importance of pharmaceutical intervention, physiotherapy and training exercises are also meaningful to patients with RA7,8,9,10). However, RA patients tend to avoid physical activity due to their fear of overloading or pain exacerbations10, 11). There is a need for interventions that support RA patients in overcoming barriers of pain and foot deformities.
In our study, we elaborated two programs: one for individual exercise and one for group exercise. The programs take into consideration that participants are chronic patients with mobility limitations and foot pain, who rely on public healthcare and who would benefit from fast and effective programs. Both programs will provide similar exercises and guidelines for self-care.
Our objective is to verify the effects of individual and group exercise programs on pain, balance, mobility and perceived benefits of rheumatoid arthritis patients with pain and foot deformities.
SUBJECTS AND METHODS
The study was conducted in the Divisão de Fisioterapia do Hospital das Cínicas da Faculdade de Medicina da Universidade de São Paulo. Approval was obtained from Local Ethics Committees (CAPPESq Nº 276/06). Patients were informed about the study, and their written informed consent was obtained.
Participants who were admitted in this study were diagnosed with RA, complaining of pain and foot deformity, with more than five years of disease and classification I–III of global functional status in RA (American Rheumatism Association 1991 revised criteria for RA). Subjects were excluded if they had a neurological or respiratory pathology, sensorial systems diseases, previous surgery in lower limbs or trunk, dizziness, cognitive impairments or other musculoskeletal disorder associated with RA. During the period of the study, prescription medication could not be changed. If changes in medication were needed, the participant continued the treatment, however, the patient would be excluded from the study.
From the waiting list of RA patients referred to the Physiotherapy Service of the hospital, the secretary of the service allocated patients into groups G1 and G2 sequentially.
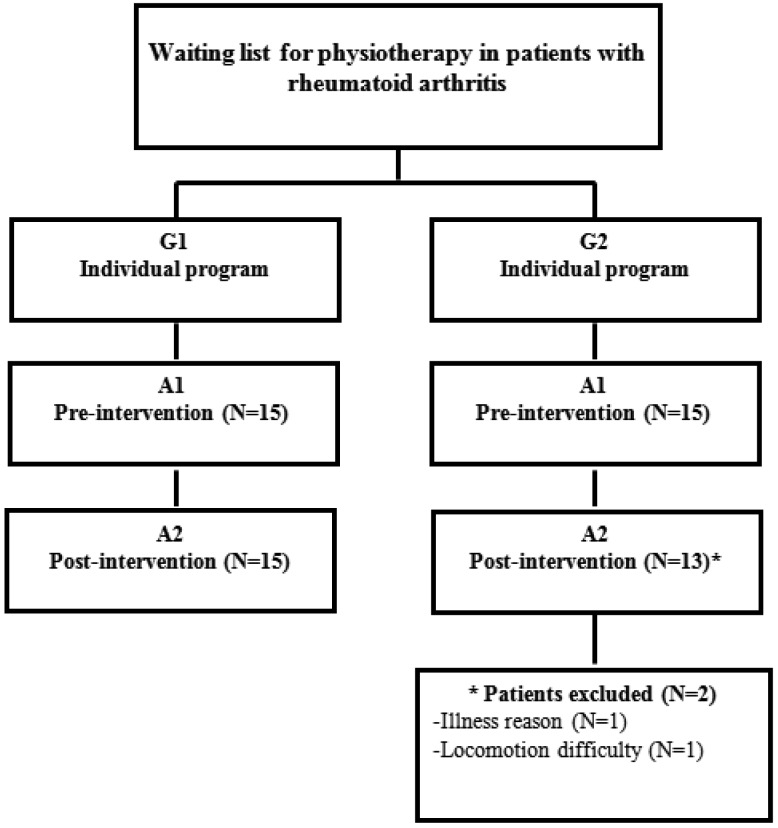
The study was outlined as shown in Fig. 1.
Fig. 1.
Study outline diagram
Group 1: Individual exercise program. Group 2: Group exercise program. A1: Pre-intervention, A2: Post-intervention, 30 days after A1.
All measurements were carried out by trained examiners. Measurements of all the variables were performed for both groups in the pre-intervention period (A1) and post-intervention period (A2) so that the effect of the treatment could be verified.
The Numerical Rating Scale (NRS) was applied to pain. Patients were asked about the intensity of foot pain in the last 24 hours on a scale of 0 (no pain) to 10 (worst pain).
The Berg Balance Scale (BBS)12) was used for balance. BBS was developed to measure balance among older people with impairment in balance function, and it was translated and validated for our language and country. It uses 14 items (graded 0–4), and the maximum score is 56 points, where the higher scores denote better balance performance.
Mobility was measured with two tests: (i) Functional Reach (FR)13). FR has been proposed as a clinical measure of dynamic mobility; it is the measurement of the maximum distance of the outstretched arm at shoulder height that one can reach without moving his/her feet. (ii) Timed Up & Go Test (TUG)14). The test begins with the patient sitting in a chair, then standing up, walking three meters, turning around, walking back, and ending when the patient sits down again. The test is timed in seconds, while the patient performs the test from the beginning to the end. The time taken to complete the task is strongly correlated to level of mobility.
For self-perception of benefits, the questionnaire Foot Health Status Questionnaire (FHSQ-Br) was applied15). The FHSQ-Br is a validated tool that measures the level of foot health status in relation to factors regarding the quality of life and lifestyle. It has been used to investigate the outcome of foot surgery and foot interventions. After patients completed the questionnaire, the scores were obtained on a scale from 0 (poorest health) to 100 (best possible health).
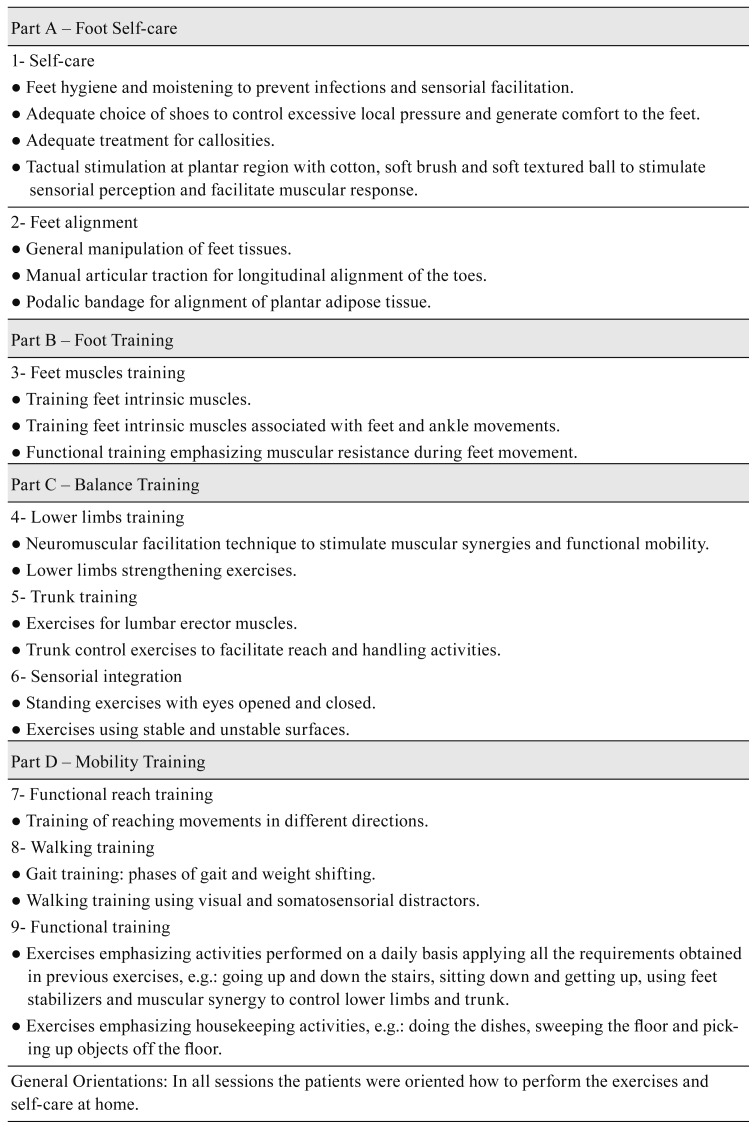
For the applied interventions, exercise programs addressing G1 and G2 were composed of functional rehabilitation exercises and self-care information. Foot exercises emphasized alignment, joint mobility and muscular synergy. Balance training was carried out with trunk control, and mobility in activities of daily living was included. Both programs were applied in two weekly sessions of 60 minutes each, over four weeks. The programs were composed of Part A: foot self-care, Part B: foot training, Part C: balance training and Part D: mobility training. The program was delivered on an individualized basis for G1 and in groups for G2. For both groups, the sessions comprised exercises of Part A to Part D with progressive difficulty throughout the treatment.
In G1, the emphasis and progression of the exercises were applied according to the patient’s performance. The patient was assisted individually under direct supervision of the physiotherapist.
In G2, patients received practical training for exercises and orientation on how to perform them correctly. During the treatment, patients received a handout listing the exercises and orientations, developed especially to be performed in a home setting. The exercises took into consideration an easy way of learning and accomplishing the tasks, in addition to safety during execution so as not to put the patient at excessive risk of pain, falls or articular overload.
The programs are shown in Fig. 2.
Fig. 2.
Individual and group exercise program of functional rehabilitation exercises and self-care information
The Wilcoxon signed-rank test was applied to verify the effect of programs comparing the results between A1 and A2 in both groups. A p-value<0.05 was considered statistically significant.
RESULTS
Socio-demographic and clinical characteristics are shown in Table 1. Considering the characteristics, groups were homogeneous, except for G2 which revealed to be older (p=0.016) and with lower body weight (p=0.011) when compared to G1.
Table 1. Socio-demographic and clinic characteristics of RA patients (n=28).
| Variables | Group 1 | Group 2 | |
|---|---|---|---|
| N | 15 | 13 | |
| Age (years) | Mean ± dp | 54.3 ± 9.28 | 62.5 ± 4.35 |
| Gender | Female, N (%) | 11 (73.3%) | 13 (100.0%) |
| Male, N (%) | 4 (26.7 %) | 0 (0%) | |
| Weight (kg) | Mean ± dp | 70.9 ± 12.7 | 60.7 ± 10.01 |
| Schooling | Illiterate, N (%) | 1 (6.7%) | 0 (0.0%) |
| 1º degree, N (%) | 9 (60.0%) | 6 (46.2%) | |
| 2º degree, N (%) | 3 (20.0%) | 4 (30.8%) | |
| 3º degree, N (%) | 2 (13.3%) | 3 (23.1%) | |
| Marital status | Single, N (%) | 2 (13.3%) | 4 (30.8%) |
| Married, N (%) | 10 (66.7%) | 4 (30.8%) | |
| Divorced, N (%) | 3 (20.0%) | 1 (7.7%) | |
| Widowed, N (%) | 0 (0.0%) | 4 (30.8%) | |
| Work situation | Active, N (%) | 2 (13.3%) | 0 (0.0%) |
| Inactive, N (%) | 4 (26.7%) | 5 (38.5%) | |
| Retired, N (%) | 9 (60.0%) | 8 (61.5%) | |
| Duration of disease (years) | Mean ± dp | 13.3 ± 4.98 | 22.9 ± 15.05 |
| Functional classification | I, N (%) | 1 (6.7%) | 2 (15.4%) |
| II, N (%) | 6 (40.0%) | 4 (30.8%) | |
| III, N (%) | 8 (53.3%) | 7 (53.8%) | |
| Deformities | N (%) | ||
| Hallux valgus | 5 (33.3%) | 8 (61.5%) | |
| Claw/hammer toe | 7 (46.7%) | 7 (53.8%) | |
| Flat foot | 8 (53.3%) | 5 (38.5%) | |
| Cavus foot | 3 (20.0%) | 0 (0.0%) | |
| Collapse of the transverse arch | 8 (53.3%) | 10 (76.9%) | |
| Drift of plantar pad | 9 (60.0%) | 9 (69.2%) | |
| Overlapping fingers | 6 (40.0%) | 3 (23.1%) | |
| Forefoot abduction | 0 (0.0%) | 0 (0.0%) | |
All participants used their medications for controlling the disease, prescribed by their rheumatologists. During the period of this study, none of the patients showed modifications in response to this conduct.
There were no differences between the two groups in all the variables analyzed in A1.
Table 2 shows median and interquartile ranges for both groups in pre- and post-intervention assessment for all the variables.
Table 2. The median and interquartile range for A1 and A2 in G1 and G2 showed by the Wilcoxon test for Numerical Rating Scale, Berg Balance Scale, Functional Reach and Timed Up & Go.
| Variables | G1 (Individual exercise program) | G2 (Group exercise program) | ||||
|---|---|---|---|---|---|---|
| A1 | A2 | p | A1 | A2 | p | |
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |||
| NRS (score) | 5 (4) | 3 (3) | 0.002 | 6 (3.5) | 5.5 (4) | 0.012 |
| BBS (score) | 51 (5) | 55 (3) | 0.002 | 48 (10) | 53 (3) | 0.002 |
| FR (centimeter) | 26.7 (9.5) | 28.7 (10.4) | 0.008 | 14.87 (6.0) | 17.5 (8.0) | 0.390 |
| TUG (seconds) | 11.0 (3.4) | 8.6 (2.9) | 0.001 | 12 (2.4) | 11.8 (2.6) | 0.377 |
G1: Group 1; G2: Group 2; NRS: Numerical Rating Scale; BBS: Berg Balance Scale; FR: Functional Reach; TUG: Timed Up & Go Test; IQR: interquartile range; A1: pre-intervention; A2: post intervention, 30 days after A1
Table 3 shows median and interquartile range for both groups in pre- and post-intervention assessment for each domain in the FHSQ-Br.
Table 3. The median and interquartile range for A1 and A2 in G1 and G2 showed by the Wilcoxon test for perceived benefits.
| FHSQ-Br (score) | G1 (Individual exercise program) | G2 (Group exercise program) | ||||
|---|---|---|---|---|---|---|
| A1 | A2 | p | A1 | A2 | p | |
| Median (IQR) | Median (IQR) | Median (IQR) | Median (IQR) | |||
| FP | 43.8 (36.9) | 60.6 (30.0) | 0.015 | 41.9 (35.6) | 54.4 (36.6) | 0.013 |
| FF | 50.0 (31.3) | 62.5 (56.3) | 0.230 | 50.0 (31.3) | 75.0 (37.5) | 0.005 |
| S | 8.3 (33.3) | 25.0 (41.7) | 0.012 | 8.3 (25.0) | 0.0 (33.3) | 0.467 |
| FGH | 25.0 (25.0) | 25.0 (17.5) | 0.062 | 12.5 (25.0) | 25.0 (35.0) | 0.001 |
| FGHI | 34.3 (30.8) | 43.3 (20.0) | 0.039 | 30.8 (14.4) | 46.3 (31.7) | 0.004 |
| GH | 40.0 (30.0) | 30.0 (40.0) | 0.300 | 60.0 (50.0) | 50.0 (45.0) | 0.377 |
| PA | 33.3 (27.8) | 50.0 (27.8) | 0.092 | 38.9 (22.2) | 50.0 (44.4) | 0.014 |
| SC | 62.5 (25.0) | 75.0 (50.0) | 0.123 | 62.5 (37.5) | 75.0 (25.0) | 0.001 |
| V | 43.8 (25.0) | 50.0 (12.5) | 0.054 | 50.0 (28.1) | 62.5 (46.9) | 0.125 |
| HI | 44.6 (15.4) | 48.8 (22.8) | 0.111 | 51.2 (24.3) | 62.9 (29.4) | 0.015 |
G1: Group 1; G2: Group 2; FHSQ-Br: Feet Health Status Questionnaire; FP: feet pain; FF: feet function; S: shoes; FGH: feet general health; FGHI: feet general health index; GH: general health; PA: physical activity; SC: social capacity; V: vigor; HI: health index; IQR: interquartile range; A1: pre-intervetion; A2: post-intervention, 30 days after A1
DISCUSSION
The majority of the studies on RA, address muscular strength, joint mobility or orthotics as rehabilitation models. Our study addressed exercise programs and orientation of foot self care and progressive exercise to improve balance and mobility, which was delivered in group or individualized; exercises programs was planned to be also executed during usual daily movements for example, going up and down the stairs, sitting down and getting up and housekeeping activities. Considering physical limitations of this chronic condition the possibility to practice the exercises in daily movements may be strongly beneficial to RA patients.
This study showed improvements in both groups in regards to pain, balance, mobility and perceived benefits in patients with RA. Individual exercise programs applied to G1 patients led to significant improvement in the variables related to pain (NRS), balance (BBS), functional mobility (TUG) and in four out of ten FHSQ-Br domains. Group exercise programs applied to G2 patients led to significant improvement in the variables related to pain (NRS), balance (BBS) and in eight out ten FHSQ-Br domains.
Patients from G1 received similar treatment to those in G2, however, the progression was applied according to the patient’s performance, always under direct and individual supervision of the physiotherapist. Many researchers believe that a program of balance and mobility needs to be individually tailored because older people vary considerably in their physical capacity and health in response to exercise. These authors suggest a list of strategies to improve balance that can be integrated into the participant’s everyday activities16).
In G2, some factors can improve perceived benefits, better perception and acknowledged improvement. Activities carried out in groups allow higher socialization, entertainment and contact with people who suffer from the same limitations caused by RA, thus improving motivation towards exercise practices16).
The effectiveness of individual and group exercise therapy for patients with knee or hip osteoarthritis were shown to be beneficial17), corroborating with our findings that there is no evidence of the superiority of one modality (individual or group) over the other. Our study also revealed that both programs are beneficial to RA patients.
Another important aspect to consider is that our RA patients, who rely on public healthcare, often report pain, physical limitation, and financial and transportation burdens to reach rehabilitation centers. With regard to that, illustrative handouts, including orientations and a few sessions of physiotherapy, play an important role and can potentially help to decrease trips to the hospital, to remember medical recommendations and to improve functional activities9, 18, 19).
About the exercise programs applied in G1 and G2, we believe that interventions for mobilizing toes and feet articulations were crucial for treating issues of balance, especially functional mobility. The movements of segments were transferred to functional movements, such as sitting and getting up, and going up and down the stairs, observed and oriented to be performed with body alignment and in the correct movement plane and axis.
In order to maintain feet articulation intact and performing its functions, daily prevention and feet care are necessary2). This information has been confirmed through the improvements reported in our study. A manual therapy is a technique that helps to restore proper functions and movements20).
This study has some limitations. Considering the chronic conditions and functional limitations of the patients, these programs can assist the physiotherapist in treatment of RA patients, however, it is difficult to define the moment in which new motor acquisitions were already assimilated and learned by patients. Follow-up of this study is necessary in order to assess the effectiveness of the programs following the end of the intervention. Finally, our sample was not large enough and it is possible that some differences are beneath the analysis performed.
Considering the chronic conditions and functional limitations of the patients, these programs can assist the physiotherapist in treatment of RA patients, however, it is difficult to define the moment in which new motor acquisitions were already assimilated and learned by patients. Follow-up of this study is necessary in order to assess the effectiveness of the programs following the end of the intervention.
Exercise programs delivered on an individual basis or in groups are beneficial and can be used in rehabilitation of patients with RA. Although both groups presented objective improvements, patients treated in groups showed better perception of the benefits.
Acknowledgments
We gratefully acknowledge the FAPESP: Fundação de Amparo a Pesquisa do Estado de São Paulo.
REFERENCES
- 1.Veldhuijzen van Zanten JJ, Rouse PC, Hale ED, et al. : Perceived barriers, facilitators and benefits for regular physical activity and exercise in patients with rheumatoid arthritis: a review of the literature. Sports Med, 2015, 45: 1401–1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vaillant J, Vuillerme N, Janvey A, et al. : Effect of manipulation of the feet and ankles on postural control in elderly adults. Brain Res Bull, 2008, 75: 18–22. [DOI] [PubMed] [Google Scholar]
- 3.Bal A, Aydoğ E, Aydoğ ST, et al. : Foot deformities in rheumatoid arthritis and relevance of foot function index. Clin Rheumatol, 2006, 25: 671–675. [DOI] [PubMed] [Google Scholar]
- 4.Aydoğ E, Bal A, Aydoğ ST, et al. : Evaluation of dynamic postural balance using the Biodex Stability System in rheumatoid arthritis patients. Clin Rheumatol, 2006, 25: 462–467. [DOI] [PubMed] [Google Scholar]
- 5.Turner DE, Helliwell PS, Emery P, et al. : The impact of rheumatoid arthritis on foot function in the early stages of disease: a clinical case series. BMC Musculoskelet Disord, 2006, 7: 102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karaca Umay E, Gurcay E, Karsli PB, et al. : Sensory disturbance and polyneuropathy in rheumatoid arthritis patients with foot deformity. Rev Bras Reumatol Engl Ed, 2016, 56: 191–197. [DOI] [PubMed] [Google Scholar]
- 7.Baillet A, Vaillant M, Guinot M, et al. : Efficacy of resistance exercises in rheumatoid arthritis: meta-analysis of randomized controlled trials. Rheumatology (Oxford), 2012, 51: 519–527. [DOI] [PubMed] [Google Scholar]
- 8.Hurkmans EJ, Li L, Verhoef J, et al. : Physical therapists’ management of rheumatoid arthritis: results of a Dutch survey. Musculoskelet Care, 2012, 10: 142–148. [DOI] [PubMed] [Google Scholar]
- 9.Breedland I, van Scheppingen C, Leijsma M, et al. : Effects of a group-based exercise and educational program on physical performance and disease self-management in rheumatoid arthritis: a randomized controlled study. Phys Ther, 2011, 91: 879–893. [DOI] [PubMed] [Google Scholar]
- 10.Mayoux Benhamou MA: Reconditioning in patients with rheumatoid arthritis. Ann Readapt Med Phys, 2007, 50: 382–385, 377–381. [DOI] [PubMed] [Google Scholar]
- 11.Vliet Vlieland TP: Non-drug care for RA—is the era of evidence-based practice approaching? Rheumatology (Oxford), 2007, 46: 1397–1404. [DOI] [PubMed] [Google Scholar]
- 12.Miyamoto ST, Lombardi Junior I, Berg KO, et al. : Brazilian version of the Berg balance scale. Braz J Med Biol Res, 2004, 37: 1411–1421. [DOI] [PubMed] [Google Scholar]
- 13.Duncan PW, Weiner DK, Chandler J, et al. : Functional reach: a new clinical measure of balance. J Gerontol, 1990, 45: M192–M197. [DOI] [PubMed] [Google Scholar]
- 14.Podsiadlo D, Richardson S: The timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc, 1991, 39: 142–148. [DOI] [PubMed] [Google Scholar]
- 15.Ferreira AF, Laurindo IM, Rodrigues PT, et al. : Brazilian version of the foot health status questionnaire (FHSQ-BR): cross-cultural adaptation and evaluation of measurement properties. Clinics (Sao Paulo), 2008, 63: 595–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shier V, Trieu E, Ganz DA: Implementing exercise programs to prevent falls: systematic descriptive review. Inj Epidemiol, 2016, 3: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tiffreau V, Mulleman D, Coudeyre E, et al. : The value of individual or collective group exercise programs for knee or hip osteoarthritis. Clinical practice recommendations. Ann Readapt Med Phys, 2007, 50: 741–746, 734–740. [DOI] [PubMed] [Google Scholar]
- 18.Sierakowska M, Klepacka M, Sierakowski SJ, et al. : Assessment of education requirements for patients with rheumatoid arthritis, based on the Polish version of the Educational Needs Assessment Tool (Pol-ENAT), in the light of some health problems—a cross-sectional study. Ann Agric Environ Med, 2016, 23: 361–367. [DOI] [PubMed] [Google Scholar]
- 19.Vervloesem N, Van Gils N, Ovaere L, et al. : Are personal characteristics associated with exercise participation in patients with rheumatoid arthritis? A cross-sectional explorative survey. Musculoskelet Care, 2012, 10: 90–100. [DOI] [PubMed] [Google Scholar]
- 20.Lubbe D, Lakhani E, Brantingham JW, et al. : Manipulative therapy and rehabilitation for recurrent ankle sprain with functional instability: a short-term, assessor-blind, parallel-group randomized trial. J Manipulative Physiol Ther, 2015, 38: 22–34. [DOI] [PubMed] [Google Scholar]