Abstract
[Purpose] This case series presents the unique application of the non-commutative property of finite rotation angles under addition to the CBP® mirror image® treatment protocol for adult lumbar and thoraco-lumbar scoliosis. [Subjects and Methods] Five adult patients having lumbar/thoraco-lumbar scoliosis and back pain, and having at least two prominent thoracic postural abnormalities according to Harrison’s rotations and translations of thoracic postures were included. After initial assessment, mirror-image stress x-rays were taken. For each patient, one stress film was taken using the order of mirror image movements with the largest displacement followed by the second largest (primary + secondary) and one stress film was taken in the opposite order (secondary + primary). The consecutive ordered movements that resulted in the largest reduction of curvature were chosen as the order-specific series of movements all exercises and postural traction were to be performed for each patient. Spinal manipulation was also performed. [Results] All patients had a reduction of curvature concomitant with a reduction in pain levels. [Conclusion] This unique treatment approach offers a patient-specific, targeted structural rehabilitative procedure to stress the spine towards a more straightened configuration. Adult lumbar and thoraco-lumbar curves can be reduced and improved by these non-invasive CBP methods.
Keywords: Scoliosis, Mirror Image, CBP
INTRODUCTION
Scoliosis is defined as a lateral spinal curvature of at least a 10° Cobb angle as measured on an AP spinal radiograph with vertebral rotation1). Its pathogenesis is thought to be genetic2), however, the true etiology remains unknown3), and is probably multifactorial3, 4). Stehbens5) suggests idiopathic scoliosis is arguably postural in nature.
The factors considered significant in predicting the progression of scoliotic deformities include the magnitude of curve, age at presentation, the Risser sign, and menarchal status6). However, curves even as small as ten degrees at post-puberty may not rule out later progression7). In fact, because the possible pathogenesis of later progression results from “the unavoidable repetitive biomechanical stresses of daily living applied unremittingly and asymmetrically to the spinal deformity7),” any conservative approach to successfully better balance the scoliotic spine would be beneficial regardless of age, at least biomechanically7, 8).
It has been determined that most chiropractors would treat patients with scoliosis; in fact, most clinicians would provide six months of therapy including manipulation, exercise, and muscle stimulation, and follow the patient to skeletal maturity9). Despite the high treatment rate chiropractors would potentially give to scoliotic patients, the effectiveness for spinal manipulative therapy (SMT) in reducing deformity has not been established8), and quite frankly has been proven ineffective10).
Alternatively, there has been a substantial amount of evidence accumulating in support of corrective exercise programs through different schools of techniques. Berdishevsky et al.11) presented a comprehensive review of seven major schools of physiotherapy scoliosis specific exercise programs (PSSE) and concluded that “the evidence supporting the effectiveness of PSSE is growing, with more high quality research studies being published in recent years.”
Although many non-surgical PSSE methods are now used to treat scoliosis, many have been criticized for lacking patient-specificity, and not being truly three-dimensional12,13,14). For instance, yoga and Dobomed approaches are general exercises and lack a defined correction procedure15). These types of treatments are more ‘cookie cutter’ in approach and do not address the particular nuances of the patient’s spinal deformity14). This major criticism has been supported by the recent studies that have directly compared ‘conventional’ exercise programs for AIS versus methods employing ‘patient-specific’ customized exercise programs that have demonstrated better patient outcomes12, 16).
The purpose of this study is to describe the reduction of deformity in five patients with lumbar or thoraco-lumbar scoliosis by application of the engineering concept of non-commutative property of finite rotation angles under addition. This is a special case of incorporating Chiropractic BioPhysics® (CBP) mirror image® concepts to treat scoliosis17). This concept has been shown to apply to the human spine17,18,19), and illustrates the remarkable phenomenon of how an object (spine/posture) can end up in a totally different three-dimensional orientation based on reversing the order of two or more sequential movements (Fig. 1)17).
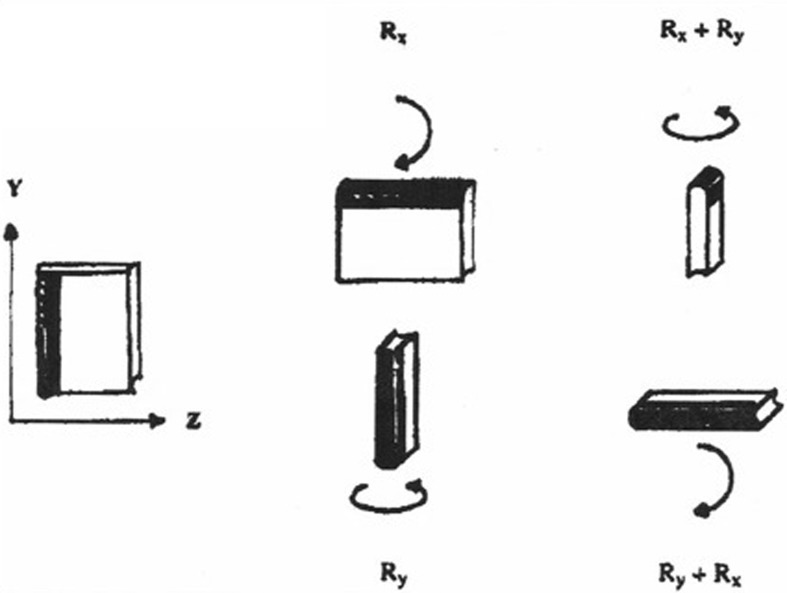
Fig. 1.
Non-commutative property of finite rotation angles under addition. On the left, a book is placed in the Y-Z plane with the spine of the book facing to the left as its starting position. On the top middle column, the book is then rotated +90° around the x-axis (Rx), followed by a +90° rotation around the vertical y-axis (Ry). Top right: 90° + Rx + 90° + Ry=Book perpendicular to original start position with its spine facing up. Alternatively, upon reversing the order (bottom middle and right): 90° +Ry + 90°+ Rx=Book perpendicular to original start position with its spine horizontal.
SUBJECTS AND METHODS
This is a retrospective case series, where the patients included for analysis had to meet the following inclusion criteria: 1) lumbar or thoraco-lumbar scoliosis only, 2) female gender, 3) age past the female growth spurt (10–14 years), 4) anatomical leg length inequality less than 12 mm, 5) no fractures or lumbar spine instability, 6) chronic low back pain (LBP) with a minimum duration of 6 months, and 7) two moderate to large thoracic region postural displacements relative to the pelvis in any combination of lateral thoracic translation (x-axis translation), rotation about gravity (y-axis rotation), and lateral flexion (z-axis rotation) (Fig. 2)17, 20).
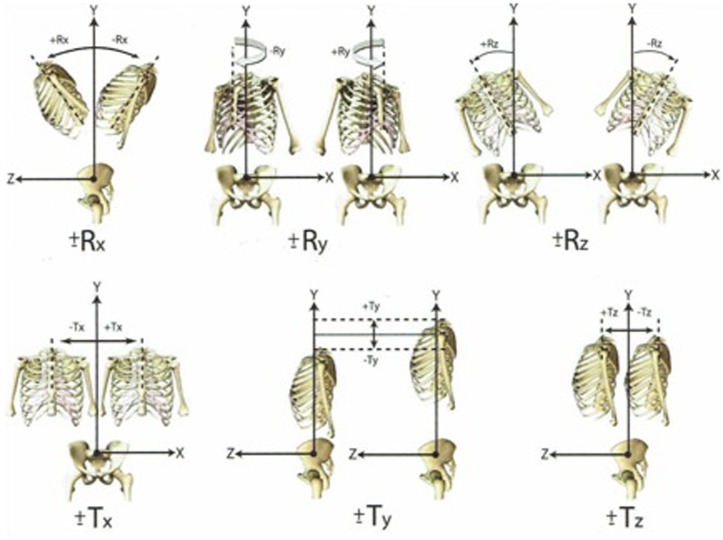
Fig. 2.
Harrison’s categorization of the thoracic cage relative to the pelvis. There are 12 simple movements in 6 degrees of freedom in three-dimensions. These 12 postures can be decomposed into 6 translations (±Tx, ±Ty, ±Tz) and 6 rotations (±Rx, ±Ry, ±Rz).
Radiographic measurements used to quantify lateral spinal curve as well as lateral thoracic translation from the vertical, was the modified Risser-Ferguson method (Fig. 3)17, 21, 22). This method approximates the centroid of each vertebra and then uses a best fit line to measure the spinal curve (lumbo-dorsal angle), and an angle that deviates from a 90° comparing the lower best fit line along the lower lumbar and the line approximating the top of the sacrum (lumbosacral angle). This measurement method has good to very good intra and inter-reliability21, 22). Although most consider the ‘Cobb angle’ as the standard for scoliosis measurement, there are many disadvantages to this angle23), so we chose the modified Risser-Ferguson as it more closely resembles the actual spinal configuration. One can convert the modified Risser-Ferguson angle to a Cobb angle by multiplying it by a factor of 1.624).
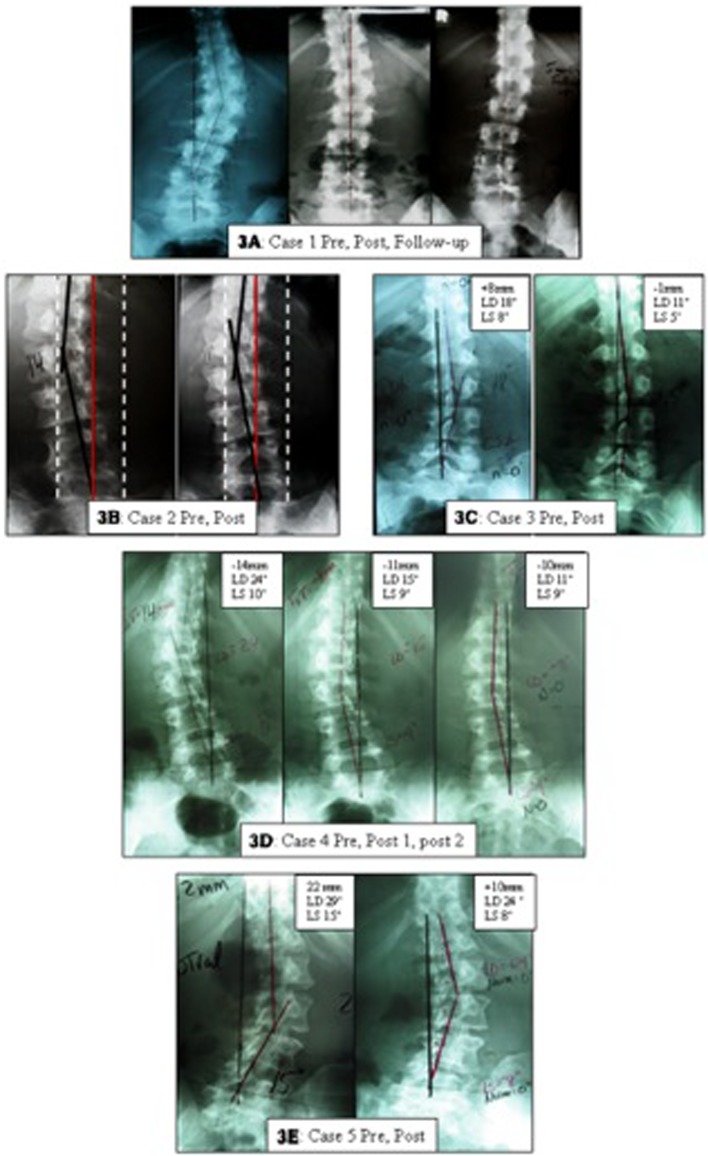
Fig. 3.
Initial and follow-up lumbo-pelvic radiographs of the five cases with scoliosis. In A, a 17 year old female’s initial, 72 visit post analysis, and 5-month follow-up AP lumbo-pelvic x-rays are shown. In B, a 35 year old female’s initial and 72 visit post analysis AP lumbo-pelvic x-rays are shown. In C, a 19 year old female’s initial and 18 visit post AP lumbo-pelvic x-rays are shown. In D, a 41 year old female’s initial, 36 visit, and 84 visit post analysis AP lumbo-pelvic x-rays are shown. In E, a 45 year old female’s initial and 36 visit post analysis AP lumbo-pelvic x-rays are shown.
For each subject, the two main thoracic-to-pelvis postures were identified from the combination of the initial neutral posture AP lumbo-pelvic radiographs and posture analysis17, 20). Two further AP lumbar stress radiographic views were taken on each subject following application of a small (less than 12 mm) heel lift if indicated (only 2 out of 5 cases; cases #1; 4). The stress films were taken in the opposite direction, i.e. mirror image, of the abnormal postural positions found in the neutral position. For each patient, 1 stress film was taken using the order of mirror image movements with the largest displacement followed by the second largest (primary + secondary) and 1 stress film was taken in the opposite order (secondary + primary). In other words, the stress films were taken in a combination movement displacement with order of movements altered.
The stress film resulting in greatest reduction of the scoliosis deformity was determined to be the posture-specific order that the CBP mirror image adjusting, exercises, and traction procedures would be performed in. All patient measures are shown in Table 1, and all patient before, after and follow-up x-rays are shown in Fig. 3. This study received IRB approved waiver of informed consent through IntegReview IRB (www.integreview.com) on March 27, 2017 (protocol No. CBP2017-001).
Table 1. Patient age, gender, number of treatments, pre- and post-pain and radiographic details.
| Subject | Age | Gender | # Visits | NRS pre | NRS post | Oswestry pre | Oswestry post | Tx (T12–S1) pre | Tx (T12–S1) post | LD pre | LD post | LS pre | LS post |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Case 1* | 17 | F | 72 | 3 | 0 | NR | NR | +15 mm | –6 mm | 47° | 23° | NR | NR |
| Case 2** | 35 | F | 84 | 6 | 1 | 24% | 16% | –20 mm | +8 mm | 14° | 11° | 10° | 2° |
| Case 3 | 19 | F | 18 | 6 | 0 | 32% | 8% | +9 mm | –1 mm | 18° | 11° | 8° | 5° |
| +Case 4** | 41 | F | 84 | 3 | 0 | 18% | 8% | –14 mm | –10 mm | 24° | 11° | 10° | 9° |
| +Case 5 | 45 | F | 36 | 4 | 1 | 22% | 14% | +22 mm | +10 mm | 29° | 24° | 15° | 8° |
NRS: Numerical rating scale (0=no pain; 10=bed ridden with pain). * This case received two programs each of 3 months. A re-examination at 36 visits was also performed but omitted for brevity. ** These cases received 2–3 programs of care totaling 84 treatments. Three other re-exams were performed but omitted for brevity. + These cases completed the SF-36 questionnaire at all re-exams. Progressive improvement was noted at each re-examination but this information was omitted for brevity.
RESULTS
Case 1
On Feb 21, 2000, a 17-year-old female with mid/LBP presented to our spine clinic. She claimed that her pain had been present for the past few years and was not due to any recent or past accidents or injuries. On a pain diagram, the patient indicated her pain was bilateral extending from T8–L5. A numerical rating scale (NRS) assessment indicated her pain as a 3/10 (0=no pain; 10=severe pain with the patient bed ridden). Her pain was described as intermittent in nature, being present 25% of the time; when present it caused mild impairment to her activities of daily living. Pain was described as a dull ache. The patient denied the presence of bowel, bladder, muscle weakness, and numbness or tingling in any bodily area. No relieving or aggravating factors for her pain were described.
Posture analysis revealed a left lateral thoracic translation (+TxT) and a right thoracic lateral flexion (+RzT). An AP lumbar radiograph revealed a +47° left convex mid-lumbar angle (LD angle) and a +15 mm left lateral translation of T12–S1.
Two mirror image postural stress x-rays were taken by altering the orders for the combination of +TxT and +RzT, with the order of first −TxT followed by −RzT showing the best reduction in scoliosis. The patient was treated for 6-months using mirror image adjustments, exercise, and traction in the pre-determined order of movements.
At final re-examination, the AP thoraco-lumbar scoliosis measured a right thoracic translation of −6 mm (a 21 mm change) and a LD angle of 23° (24° improvement). The patient reported complete amelioration of her pain NRS=0. After 5-months of no treatment, the patient returned for a follow-up evaluation. She reported mild, occasional low back pain and a slight regression of the scoliosis was found (LD angle 30° and lateral translation of +8mm) (Table 1 and Fig. 3A).
Case 2
A 35-year-old female presented with a primary complaint of right-sided mid and low back pain following a motor vehicle accident 8 months previously. The Oswestry low back questionnaire indicated a 24% impairment. The pain was rated as a 6/10 on the NRS. Two main thoracic-to-pelvis postures were identified: a right thoracic translation (−TxT) and a right thoracic rotation (−RyT). The initial AP lumbar radiograph revealed a right convex scoliosis with a LD angle of −14°, a LS angle of +10° right thoracic, and a right translation of T12–S1 of −20 mm.
Two mirror image stress views were obtained with the order of left thoracic translation followed by left thoracic rotation (+TxT, +RyT) showing the greatest reduction of scoliotic deformity. The patient was treated 3 times per week for 7 months with order specific mirror image methods; periodic re-evaluations were obtained. At final re-examination, the AP thoraco-lumbar scoliosis measured a right thoracic translation of 7 mm (a 13 mm improvement), a LD angle of 11° (3° improvement), a LS angle of 2° (8° improvement) (Table 1 and Fig. 3B).
Case 3
A 19-year-old-female presented for treatment of chronic lower back pain in the summer of 2004. On a numerical rating scale (NRS) she rated the intensity of her pain as a 6/10 and on a revised Oswestry low back pain questionnaire she scored a 32% disability. Postural analysis using computerized digital photographs revealed a left lateral thoracic translation (+TxT) and a left thoracic rotation about gravity (+RyT). An AP lumbar radiograph, using the modified Riser-Fergusson method, revealed a +18° left convex mid-lumbar angle (LD angle), a −8° lumbo-sacral angle, and a +9 mm left lateral translation of T12–S1.
Two mirror image postural stress x-rays were taken by altering the orders of mirror image movements, with the combination of −TxT and −RyT showing the best reduction in scoliosis. The patient was then treated with 18 treatments of mirror image adjustments, exercise, and traction using the pre-determined order of movements.
At final re-examination, it was found that the LD angle reduced to 11° (7° improvement), the LS angle to 5° (3° improvement), and the TxT to −1 mm (10 mm improvement). The patient reported a 0/10 on the NRS and scored an 8% on the Oswestry questionnaire (Table 1 and Fig. 3C).
Case 4
A 41-year-old-female presented for treatment of chronic lower back pain. She claimed that her pain had been present for many years and was not due to any recent or past injury. She rated the intensity of her pain a 3/10 on the NRS and scored an 18% on the Oswestry low back pain disability questionnaire. SF-36 questionnaire revealed significantly decreased scores in physical and emotional scales. Computerized postural analysis revealed a right lateral thoracic translation (−TxT) and a left thoracic lateral flexion (−RzT). An AP lumbar radiograph revealed a mild right anatomical short leg, a −24° right convex mid-lumbar angle (LD angle), a +10° left convex lumbo-sacral angle (LS) and a −14 mm right lateral translation of T12–S1.
Two mirror image postural stress x-rays were taken by altering the orders for the combination of −TxT and −RzT, with the order of first +RzT followed by +TxT showing the best reduction in scoliosis. The patient was treated for 6-months, including periodic re-examinations, using mirror image adjustments, exercise, and traction in the pre-determined order of movements.
At final re-examination, the AP thoraco-lumbar scoliosis measured a right thoracic translation of −10 mm (a 4 mm improvement), a LD angle of −11° (13° improvement), a LS angle of +9° (1° improvement). Pain and disability measures showed steady improvement and were significantly improved at final follow-up (Table 1 and Fig. 3D).
Case 5
A 45-year-old-female presented for treatment of chronic lower back pain. She claimed that her pain had been present for several years and was not due to any recent or past injury. She rated the intensity of her pain a 4/10 on the NRS and scored a 22% on the Oswestry low back disability questionnaire. SF-36 questionnaire revealed significantly decreased scores in physical and emotional scales. Computerized postural analysis revealed a left lateral thoracic translation (+TxT) and a left thoracic long-axis rotation (+RyT). An AP lumbar radiograph revealed a +29° left convex mid-lumbar angle (LD angle), a −15° lumbo-sacral angle, and a +22 mm left lateral translation of T12–S1.
Two mirror image postural stress x-rays were taken by altering the orders for the combination of +TxT and +RyT, with the order of first −TxT followed by −RyT showing the best reduction in scoliosis. The patient was treated for 3-months (including periodic re-examinations) using mirror image adjustments, exercise, and traction in the pre-determined order of movements.
At final re-examination, the AP thoraco-lumbar scoliosis measured a left thoracic translation of +10 mm (a 12 mm improvement), a LD angle of +24° (5° improvement), a LS angle of −8° (7° improvement). Pain and disability measures showed steady improvement and were significantly improved at final follow-up (Table 1 and Fig. 3E).
DISCUSSION
This report presented the application of the engineering concept non-commutative property of finite rotation angles under addition to the spine in the treatment of scoliosis as a special form of CBP mirror image methods. The demonstration of reduction in scoliotic curvature in these five cases verifies that this concept is indeed applicable to the spine in patients with scoliotic deformities.
As with brace treatment, where the in-brace correction is crucial to the outcome25), so too seems the prescription of exercises and traction. Stress views of asymmetric over-correcting movements/exercises give the practitioner more incite into actual spinal coupling response to particular prescribed movements. Further, we have demonstrated, that the order of two consecutive movement patterns have a different effect on the final spinal over-corrected position. The most over-corrective position/movement sequence is always the better option by being the most effective exercise/traction prescription.
As mentioned, many scoliosis rehabilitation programs are criticized for not being patient-specific, or customized to the patient’s deformity12,13,14). This has been supported by recent studies showing that patient-specific exercise protocols are superior to generalized exercise programs. We ask how often is the sequence of multiple movements/positions in prescribing scoliosis-specific treatments overlooked and not ascertained? We propose this to be true in the majority of cases and/or approaches.
The recent evidence showing the most effectiveness for non-surgical scoliosis reduction comes from Germany; an intensive scoliosis in-patient rehabilitation (SIR) program has been used for decades for reduction and prevention of deformity progression12, 16, 26,27,28,29,30,31,32,33). This treatment is based on an intensive multi- modality ‘Schroth method’ program consisting of exercises, bracing, passive transverse forces (PTF), massage therapy, breathing exercises, psychological counseling, as well as optional psychotherapy, relaxation therapies, manipulation, and acupuncture. The successful result of curvature reduction12, 16, 28, 29, 33), increased vital capacity and rib mobility27) have been documented, where it has even been stated that the positive outcomes of this practice validate a policy of offering conservative scoliosis treatment as an alternative to patients, including those for whom surgery is indicated30). Recent trials have demonstrated this approach superior to the prescription of general, non-specific exercise/stretching programs in treating scoliosis12, 16).
Several techniques used within the Schroth method are likened to the CBP mirror image techniques employed on these five cases. The use of ‘asymmetric standing exercises designed to employ targeted traction to restore torso balance28),’ and the use of passive transverse forces in a ‘vertical frame with adjustable belts28)’ may be similar, albeit not precisely, to the patient’s opposite posture as determined by using the concept of rotations and translations as put forth by Harrison20). Perhaps the application of the current engineering concept as applied in these five cases affords a more specific means to develop subject-specific, targeted adjusting, exercise, and traction procedures to stress the spine towards a more straightened/reversed, over-corrected configuration.
Scoliotic curves are those lateral curvatures of at least ten degrees1). As mentioned earlier, small curves such as those of ten degrees are not immune to progression even in patients past adolescence7). Stokes34) suggested that if scoliotic curves progress from asymmetric loading, the shearing force component would be the culprit. Thus, any correction by conservative means would be beneficial, as a straighter spine would be subject to less shearing force and would therefore be less vulnerable to progression.
The evidence put forth does demonstrate that this new, CBP order specific treatment technique, is feasible in the treatment of those with lumbar scoliosis. It should be noted that surveys monitoring the natural history suggest that curvatures may remain stable or spontaneously reduce with no treatment35,36,37), however, this applies mainly to growing children38), of which there were none in the present study.
The fact that 2–4 weeks of manipulation was initially given for pain relief may theoretically have contributed to the correction seen in these patients. It has been determined, however, that manipulation is not effective at correcting scoliosis curvatures10), or even at changing the alignment of the spine in general39,40,41,42).
Further, the application of a heel lift has been shown to correct postural imbalances, reduce lumbar curvature43, 44), and reduce pain45). Only two of the five patients in this series required a heel lift; it was determined by radiograph, that the deformity was not significantly reduced by application of the lift.
Finally, because standard CBP protocol involves the use of mirror image adjusting, exercise, and traction procedures, it is not known which contributed to the correction of deformity. Regardless, it was the application of the patient-specific ordering of mirror image postural correction methods that led to observable success pre-treatment (stress films), following treatment and at follow-up. Since traditional manipulation has proven ineffective in reducing scoliosis curvature10), further study in these methods is recommended to evaluate different postural combinations and results obtained within a larger population of scoliosis patients.
Acknowledgments
We thank Dr. Donald D. Harrison (deceased) for his insights into developing the unique approach to treating scoliosis as presented in these cases.
REFERENCES
- 1.Berven S, Bradford DS: Neuromuscular scoliosis: causes of deformity and principles for evaluation and management. Semin Neurol, 2002, 22: 167–178. [DOI] [PubMed] [Google Scholar]
- 2.Hadley Miller N: Spine update: genetics of familial idiopathic scoliosis. Spine, 2000, 25: 2416–2418. [DOI] [PubMed] [Google Scholar]
- 3.Lowe TG, Edgar M, Margulies JY, et al. : Etiology of idiopathic scoliosis: current trends in research. J Bone Joint Surg Am, 2000, 82-A: 1157–1168. [DOI] [PubMed] [Google Scholar]
- 4.Ahn UM, Ahn NU, Nallamshetty L, et al. : The etiology of adolescent idiopathic scoliosis. Am J Orthop, 2002, 31: 387–395. [PubMed] [Google Scholar]
- 5.Stehbens WE: Pathogenesis of idiopathic scoliosis revisited. Exp Mol Pathol, 2003, 74: 49–60. [DOI] [PubMed] [Google Scholar]
- 6.Lonstein JE, Carlson JM: The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Joint Surg Am, 1984, 66: 1061–1071. [PubMed] [Google Scholar]
- 7.Stehbens WE, Cooper RL: Regression of juvenile idiopathic scoliosis. Exp Mol Pathol, 2003, 74: 326–335. [DOI] [PubMed] [Google Scholar]
- 8.Danbert RJ: Scoliosis: biomechanics and rationale for manipulative treatment. J Manipulative Physiol Ther, 1989, 12: 38–45. [PubMed] [Google Scholar]
- 9.Feise RJ: An inquiry into chiropractors’ intention to treat adolescent idiopathic scoliosis: a telephone survey. J Manipulative Physiol Ther, 2001, 24: 177–182. [PubMed] [Google Scholar]
- 10.Lantz CA, Chen J: Effect of chiropractic intervention on small scoliotic curves in younger subjects: a time-series cohort design. J Manipulative Physiol Ther, 2001, 24: 385–393. [DOI] [PubMed] [Google Scholar]
- 11.Berdishevsky H, Lebel VA, Bettany-Saltikov J, et al. : Physiotherapy scoliosis-specific exercises—a comprehensive review of seven major schools. Scoliosis Spinal Disord, 2016, 4: 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Noh DK, You JS, Koh JH, et al. : Effects of novel corrective spinal technique on adolescent idiopathic scoliosis as assessed by radiographic imaging. J Back Musculoskeletal Rehabil, 2014, 27: 331–338. [DOI] [PubMed] [Google Scholar]
- 13.Borysov M, Moramarco M, Sy N, et al. : Postural re-education of scoliosis—state of the art (mini-review). Curr Pediatr Rev, 2016, 12: 12–16. [DOI] [PubMed] [Google Scholar]
- 14.Borysov M, Mogiliantseva T: Rehabilitation of adolescents with scoliosis during growth—preliminary results using a novel standardized approach in Russia. (Methodology). Curr Pediatr Rev, 2016, 12: 31–35. [DOI] [PubMed] [Google Scholar]
- 15.Weiss HR, Lehnert-Schroth C, Moramarco M, et al. : Schroth therapy—Advancements in conservative scoliosis treatment. Lambert (LAP) Saarbrucken, Germany 2015. [Google Scholar]
- 16.Monticone M, Ambrosini E, Cazzaniga D, et al. : Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J, 2014, 23: 1204–1214. [DOI] [PubMed] [Google Scholar]
- 17.Harrison DE, Betz JW, Harrison DD, et al. 2007. CBP structural rehabilitation of the lumbar spine. Harrison Chiropractic Biophysics Seminars, Inc.
- 18.Harrison DE, Oakley PA, Harrison DD: Reduction of deformity after CBP mirror image care incorporating the non-commutative properties of finite rotation angles in three patients with thoraco-lumbar scoliosis. 8th Biennial Congress of the World Federation of Chiropractic, International Conference on Chiropractic Research, Sydney, Australia, June 16–18, 2005. p.287.
- 19.Harrison DE, Oakley PA, Harrison DD: Reduction of deformity after chiropractic biophysics mirror image care incorporating the non-commutative properties of finite rotation angles in five patients with thoraco-lumbar scoliosis [Platform presentation; the Association of Chiropractic Colleges’ Thirteenth Annual Conference, 2006]. J Chiropr Educ, 2006, (20:1): 19–20.
- 20.Harrison DD: Abnormal postural permutations calculated as rotations and translations from an ideal normal upright static spine. In: Sweere JJ, ed. Chiropractic Family Practice. Gaithersburg: Aspen Publishers, 1992, pp 1–22. [Google Scholar]
- 21.Harrison DE, Holland B, Harrison DD, et al. : Further reliability analysis of the Harrison radiographic line-drawing methods: crossed ICCs for lateral posterior tangents and modified Risser-Ferguson method on AP views. J Manipulative Physiol Ther, 2002, 25: 93–98. [DOI] [PubMed] [Google Scholar]
- 22.Troyanovich SJ, Harrison SO, Harrison DD, et al. : Chiropractic biophysics digitized radiographic mensuration analysis of the anteroposterior lumbopelvic view: a reliability study. J Manipulative Physiol Ther, 1999, 22: 309–315. [DOI] [PubMed] [Google Scholar]
- 23.Harrison DE, Betz JW, Cailliet R, et al. : Radiographic pseudoscoliosis in healthy male subjects following voluntary lateral translation (side glide) of the thoracic spine. Arch Phys Med Rehabil, 2006, 87: 117–122. [DOI] [PubMed] [Google Scholar]
- 24.Morningstar M, Stitzel CJ.: Cobb’s angle in scoliosis −gold standard or golden calf? A commentary on scoliosis outcome assessments. J Pediatr Matern & Fam Health −Chiropr: Winter 2010 (2010:1): Online access only pp 6–10. [Google Scholar]
- 25.Landauer F, Wimmer C, Behensky H: Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr Rehabil, 2003, 6: 201–207. [DOI] [PubMed] [Google Scholar]
- 26.Lehnert-Schroth C: [The “four-curved” scoliosis. The effect on the additional lumbosacral spinal curve by the three dimensional Schroth’s scoliosis treatment]. ZFA (Stuttgart), 1981, 57: 2227–2231 (in German). [PubMed] [Google Scholar]
- 27.Weiss HR: The effect of an exercise program on vital capacity and rib mobility in patients with idiopathic scoliosis. Spine, 1991, 16: 88–93. [DOI] [PubMed] [Google Scholar]
- 28.Weiss HR, Weiss G, Petermann F: Incidence of curvature progression in idiopathic scoliosis patients treated with scoliosis in-patient rehabilitation (SIR): an age- and sex-matched controlled study. Pediatr Rehabil, 2003, 6: 23–30. [DOI] [PubMed] [Google Scholar]
- 29.Weiss HR: Influence of an in-patient exercise program on scoliotic curve. Ital J Orthop Traumatol, 1992, 18: 395–406. [PubMed] [Google Scholar]
- 30.Weiss HR: [Conservative treatment of idiopathic scoliosis with physical therapy and orthoses]. Orthopade, 2003, 32: 146–156 (in German). [DOI] [PubMed] [Google Scholar]
- 31.Hansen T: [Practical verification of Schroth’s method]. Z Orthop Ihre Grenzgeb, 1976, 114: 462–464 (in German). [PubMed] [Google Scholar]
- 32.Lehnert-Schroth C: [Schroth’s three dimensional treatment of scoliosis]. ZFA (Stuttgart), 1979, 55: 1969–1976 (in German). [PubMed] [Google Scholar]
- 33.Kuru T, Yeldan İ, Dereli EE, et al. : The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil, 2016, 30: 181–190. [DOI] [PubMed] [Google Scholar]
- 34.Stokes IA: Analysis of symmetry of vertebral body loading consequent to lateral spinal curvature. Spine, 1997, 22: 2495–2503. [DOI] [PubMed] [Google Scholar]
- 35.Weinstein SL: Natural history. Spine, 1999, 24: 2592–2600. [DOI] [PubMed] [Google Scholar]
- 36.Rowe DE, Bernstein SM, Riddick MF, et al. : A meta-analysis of the efficacy of non-operative treatments for idiopathic scoliosis. J Bone Joint Surg Am, 1997, 79: 664–674. [DOI] [PubMed] [Google Scholar]
- 37.Woolf S,US Preventive Services Task Force: Screening for adolescent idiopathic scoliosis. Review article. JAMA, 1993, 269: 2667–2672. [PubMed] [Google Scholar]
- 38.Mehta MH: Pain provoked scoliosis. Observations on the evolution of the deformity. Clin Orthop Relat Res, 1978, (135): 58–65. [PubMed] [Google Scholar]
- 39.Plaugher G, Cremata EE, Phillips RB: A retrospective consecutive case analysis of pretreatment and comparative static radiological parameters following chiropractic adjustments. J Manipulative Physiol Ther, 1990, 13: 498–506. [PubMed] [Google Scholar]
- 40.Harrison DD, Jackson BL, Troyanovich S, et al. : The efficacy of cervical extension-compression traction combined with diversified manipulation and drop table adjustments in the rehabilitation of cervical lordosis: a pilot study. J Manipulative Physiol Ther, 1994, 17: 454–464. [PubMed] [Google Scholar]
- 41.Harrison DE, Cailliet R, Harrison DD, et al. : A new 3-point bending traction method for restoring cervical lordosis and cervical manipulation: a nonrandomized clinical controlled trial. Arch Phys Med Rehabil, 2002, 83: 447–453. [DOI] [PubMed] [Google Scholar]
- 42.Hurwitz EL, Aker PD, Adams AH, et al. : Manipulation and mobilization of the cervical spine. A systematic review of the literature. Spine, 1996, 21: 1746–1759, discussion 1759–1760. [DOI] [PubMed] [Google Scholar]
- 43.Zabjek KF, Leroux MA, Coillard C, et al. : Acute postural adaptations induced by a shoe lift in idiopathic scoliosis patients. Eur Spine J, 2001, 10: 107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Irvin RE: Reduction of lumbar scoliosis by use of a heel lift to level the sacral base. J Am Osteopath Assoc, 1991, 91: 34–44, 37–44. [PubMed] [Google Scholar]
- 45.Giles LG, Taylor JR: Low-back pain associated with leg length inequality. Spine, 1981, 6: 510–521. [DOI] [PubMed] [Google Scholar]