Abstract
[Purpose] To present a case demonstrating the reduction of progressive thoracolumbar scoliosis by incorporating Chiropractic BioPhysics® (CBP®) technique’s mirror image® exercises, traction and blocking procedures based on the ‘non-commutative properties of finite rotation angles under addition’ engineering law. [Subject and Methods] A 15-year-old female presented with a right thoracolumbar scoliosis having a Cobb angle from T5–L3 of 27° and suffering from headaches and lower back pains. Her curve had progressed over the last two years despite being under traditional chiropractic care. [Results] The patient was treated using CBP structural rehabilitation protocols incorporating mirror image traction, home blocking, corrective exercises and spinal manipulation. The patient was treated 24 times (including 45 home self-treatment blocking sessions) over the course of 15-weeks. Her thoracolumbar curve reduced from 27° to 8° and her headache and low back pain disability improved significantly. [Conclusion] CBP mirror image exercises and traction are consistent with other successful non-surgical approaches and show promise in treating adolescent idiopathic scoliosis.
Keywords: CBP, Scoliosis, Mirror image
INTRODUCTION
Adolescent idiopathic scoliosis (AIS) is the most common spinal disorder in children and adolescents affecting up to 5.2% of the population1). It is characterized by curvature of the spine over 10 degrees with concomitant vertebral rotation2).
Although the specific cause of AIS remains unknown3); so-called ‘idiopathic,’ the optimal non-surgical conservative treatment approach remains controversial. There have been many different approaches to treating AIS with the goals of slowing progression, stabilization, and reducing curve magnitude, by physiotherapy, exercises, surgery, traction, bracing, casting, biofeedback, and observation4,5,6,7).
Regardless of chosen treatment, the primary goal for scoliosis management is always to stop curve progression and to avoid surgery. According to SOSORT guidelines, children presenting with Risser 4 as well as having a Cobb angle greater than 25° are recommended for physical therapy and scoliosis intensive rehabilitation (SIR)5).
There has been much progress in the non-surgical treatment of AIS by ‘corrective’ exercise/stretching type programs8). These conservative non-surgical intervention techniques have also been shown to increase the quality of life in AIS patients by increasing pulmonary function, spinal strength, mobility, decreasing pain, and improving body image9,10,11,12,13,14).
In a recent trial, Noh et al.15) determined that although two groups of AIS patients receiving exercise protocols had improved postural parameters as measured on x-ray, the treatment group, receiving a more customized, three- dimensional ‘corrective spinal technique,’ had better outcomes to that of the control group who performed a ‘conventional’ protocol. The authors note that most ‘corrective’ exercise protocols predominantly focus on one or two-dimensional spinal deformity, but rarely address full three-dimensions as their treatment group, experiencing better outcomes, received.
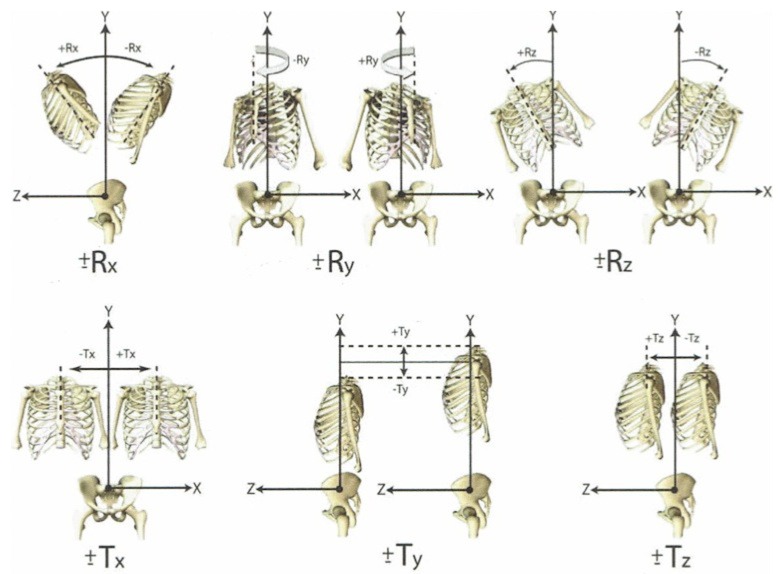
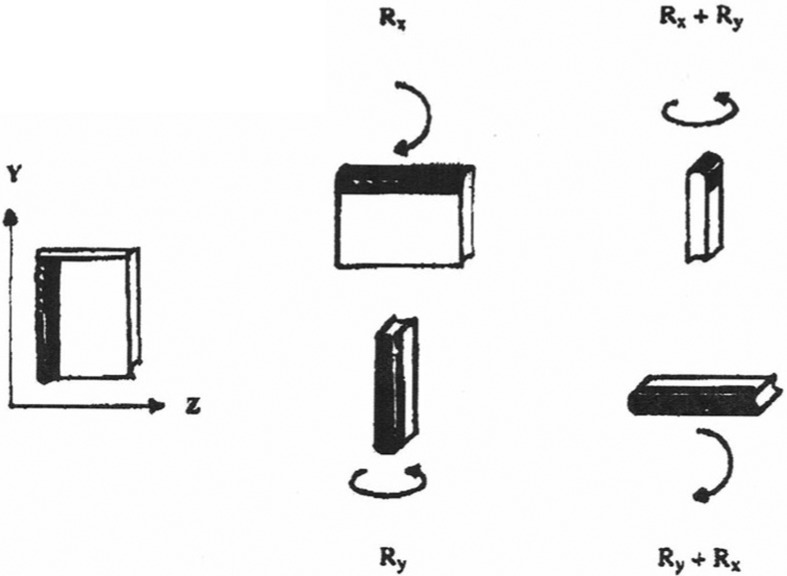
Another neglected approach incorporated into the care of scoliosis patients is a concept that is essential for determining patient specificity in regards to the ordering of postural/spinal movements in the prescription of exercises and/or traction. Based on the fundamental initial presentation of a patients thoracic posture; that is, Harrison’s rotations and translations of the thorax in relation to the pelvis (Fig. 1)16,17,18,19), the ‘non-commutative properties of finite rotation angles under addition’ is an engineering law describing the phenomenon of an object ending up in totally different three-dimensional positions based on reversing the order of two or more movements (Fig. 2). It is important to note that in the application to patients with AIS, these movements, in turn, force simultaneous spinal coupling patterns to affect the scoliotic curve; thereby reducing it.
Fig. 1.
Harrison’s categorization of the thoracic cage relative to the pelvis. There are 12 simple movements in 6 degrees of freedom in three-dimensions. These 12 postures can be decomposed into 6 translations (±Tx, ±Ty, ±Tz) and 6 rotations (±Rx, ±Ry, ±Rz). (Image compliments of CBP Seminars, Inc).
Fig. 2.
Non-commutative property of finite rotation angles under addition
On the left, a book is placed in the Y-Z plane with the spine of the book facing to the left as its starting position. On the top middle column, the book is then rotated +90° around the x-axis (Rx), followed by a +90° rotation around the vertical y-axis (Ry). Top right: 90° + Rx + 90° + Ry=Book perpendicular to original start position with its spine facing up. Alternatively, upon reversing the order (bottom middle and right): 90° + Ry + 90° + Rx=Book perpendicular to original start position with its spine horizontal. (Image compliments of CBP Seminars, Inc.)
Although initially abstract, the non-commutative properties of finite rotation angles under addition law applies to human spines and remains only briefly documented in a few cases19,20,21,22). We present the successful reduction of a progressive thoracolumbar scoliosis in a 15-year-old female treated with Chiropractic BioPhysics® (CBP®) mirror image® structural rehabilitation protocols based on this principle19, 22).
SUBJECT AND METHODS
On January 21, 2015, a 15-year-old female presented with a previous diagnosis of AIS (Table 1). She suffered from headaches and chronic low back pain (LBP), as well as left sided body pain in general, especially after sitting for longer than 45 minutes. Her LBP was reported to be constant, and described as a dull ache with slight changes in intensity throughout the day.
Table 1. Chronological scoliosis Cobb angles and treatment details.
| Date | 3/15/13 | 3/13/14 | 1/21/15 | 2/3/15 | 2/23/15 | 3/9/15 | 5/12/15 |
|---|---|---|---|---|---|---|---|
| Cobb | 16° | 24° | 27.3° | n/a | n/a | n/a | 8.2° |
| Txt info | SMT | SMT | CBP care | New ex: Seated rows | New txn: Standing | New ex: Underhand rows | 24 office txts; 45 home txts |
| PM | PM | MI ex, Planks, Cross-crawl | |||||
| MI txn | Shoulder | ||||||
| SMT | Shrugs | ||||||
CBP: Chiropractic BioPhysics®; MI: mirror image®; txn: traction; txt(s): treatment(s); SMT: spinal manipulable therapy; PM: passive mobilization. All exercise done while holding sequence-specific corrective position (+TxT then +RzT). At all dates after 1/21/15, all treatments were in addition to initial except for the new traction on 2/23/15 that replaced the former in-office traction.
On a numeric rating scale (NRS: 0=no pain; 10=worst pain ever) the patient rated her headaches at a 6/10 when present, and her low back pain a 4/10 at worst. She scored 28 (18 functional and 10 emotional) on the Headache Disability Inventory Questionnaire (HDI) and a 24% on the revised Oswestry Chronic Low Back Pain Disability Questionnaire (ODI).
Palpation revealed tenderness on the right paraspinal musculature within the lower thoracic and lumbar areas. Posture assessment16,17,18) revealed a right lateral thoracic translation (−TxT)23), a left lateral thoracic flexion (i.e. high right shoulder: −RzT), and a posterior thoracic translation posture relative to the pelvis (−TzT)24). She also had forward head posture (+TzH) and a right lateral head translation (−TxT)25).
She had been under previous monthly chiropractic care consisting of manipulation and passive mobilization via a roller table. Despite this, her curve had progressed (as defined as ≥6° increase26)) since first being diagnosed two years previous, on March 15, 2013 with a 16° curve. On a subsequent x-ray dated March 13, 2014, her thoracolumbar curve had progressed to 24° Cobb angle (Table 1). In December 2014 she was evaluated for a brace and was referred to our clinic for rehabilitation.
Radiographs were digitized and analyzed using the PostureRay® digital measurement program (Trinity, FL, USA) that uses the Harrison posterior tangent method for lateral spine images27,28,29), and both the modified Risser-Ferguson30) and Cobb31) methods for AP spine images. These measurement methods are proven to be repeatable and reliable27,28,29,30,31,32). The AP thoracolumbar image revealed a 27.3° (Cobb angle) right thoracolumbar scoliosis measured from T5 to L3, having an apex at T12 (Fig. 3A).
Fig. 3.
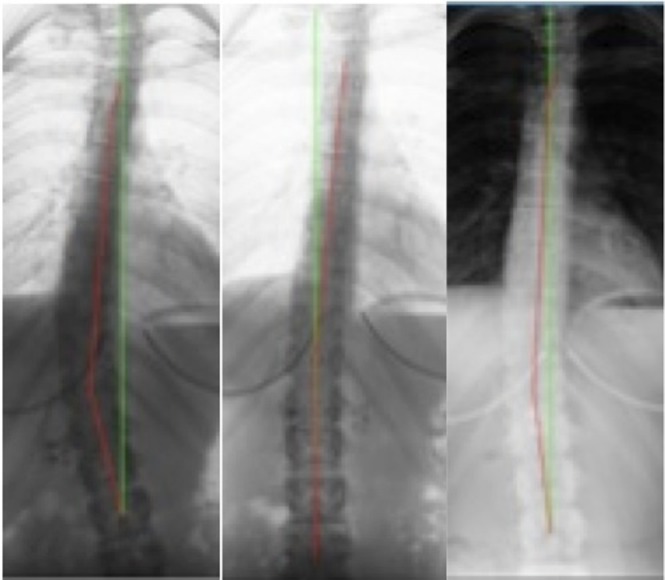
AP thoracolumbar x-rays
Green line is vertical; Red line is modified Risser-Ferguson angle; all angles reported as Cobb angles. Left: Initial view (Jan 21, 2015) revealing a 27.3° (T5–L3); Middle: ‘Stress view’ (Jan 21, 2015) with patient performing first a left thoracic translation (+TxT), then a right thoracic lateral flexion (+RzT) which showed a ‘reduction potential’ of 9.3°; Right: Post-treatment follow-up neutral standing view (May 12, 2015) showing a dramatically improved curve of 8.2°; an overall reduction/correction of 19.2° (27.3° vs. 8.2°).
Unique to CBP technique, ‘stress film’ x-rays were performed to determine the best combination of postural movements required to demonstrate the most reduction to the primary curve, and therefore the corrective movements as well as the sequence of these mirror image movements to be prescribed as the corrective exercises (Fig. 2). In the typical CBP treatment approach, any presenting postural rotation or translation, as in Fig. 2, would be treated by its ‘mirror image®, or reverse position in terms of adjustments, exercise, and traction set-ups17,18,19). After a series of treatments, typically three times a week for 12 weeks, a re-assessment is performed including a radiograph of the targeted spinal area being ‘corrected.’ In this case, the largest two thoracic postures were identified (Fig. 2) and the mirror image of these two postures were simultaneously performed.
The patient was instructed to translate the torso (T12) to the left (+TxT) and laterally flex the torso above T12 to the right (+RzT). The stress film revealed a reduction of scoliosis to 9.3 degrees (Fig. 3B). Since the first sequence- specific series of postural movements (+TxT; +RzT) showed a dramatic ‘reduction-potential,’ a second radiograph, reversing the order of these movements was forgone.
Treatment began on the day of her initial presentation and assessment. She was given specific mirror image exercises in the order that reduced her scoliosis during the stress radiograph; that is, a left thoracic translation (+TxT) followed by a right lateral flexion of the thorax (+RzT). She was instructed to perform these exercises 100 times a day holding each repetition for 5 seconds. She was also given 3 cross crawl exercises to perform for 20 seconds each (1 minute total) per day. She was also instructed to perform 3 minutes of planks every other day.
Initially, when receiving in office treatment she performed these specific exercises on the PowerPlate® (Northbrook, IL, USA). On her 7th treatment session (Feb. 3, 2015) she was prescribed another exercise, seated rows on the PowerPlate. She was instructed to maintain her mirror image corrective posture while performing 20 overhand rows with a bar held in front of her. On her 15th treatment session (Mar. 9, 2015) she was instructed to add underhand rows to her rowing exercise regimen. She was also given a new Fit Stik Pro Bar® (Clearfield, UT, USA) exercise. Standing on the PowerPlate, she was instructed to hold her mirror image position while performing 20 repetitions of shoulder shrugs. These exercises would all be performed in addition to the initially prescribed exercises for the remaining in-office treatments.
Her treatment plan also included traction at home as well as in the office (Fig. 4). She used a thoracic ScoliRoll® which was located at the level of T10 (T12 was too painful due to the floating ribs) for three minutes the first day, building up to 15–20 minutes per day over a couple of weeks (Fig. 4A). Twenty minutes was the maximum traction time since this would achieve a maximum visco-elastic creep of the ligamentous tissues33). She would lay on her right side, positioning the roll under her, and keeping the legs bent to secure her in a side laying position. She also would support her head in a neutral position by use of a pillow. This is the traction she initially performed at home and in office. In the office, two straps were placed cephalad and caudad to the ScoliRoll to accentuate the stretch over the fulcrum. The patient tolerated traction well and reported mostly a pressure feeling as opposed to a pain feeling.
Fig. 4.
Spinal traction set-ups
Left: Traction performed over a Scoliroll; Right: Standing traction.
On the 13th treatment session (Feb. 23, 2015), she was graduated to a standing traction set-up (Fig. 4B). Here her right hip was positioned against a vertical support and held there by a strap, a horizontal oriented strap was positioned at the level of T10 and would be used to translate her thorax to the left (+TxT), the first of the double sequence of movements. A strap would be positioned under her left armpit angled approximately 30 degrees, pulling her upper body to the right, forcing a rotation of her thorax over the second translation band achieving the second movement (+RzT). She began this new traction with 5 minutes and built up to 20 minutes per session over the next several sessions.
She was also given spinal manipulative therapy (SMT) throughout the cervical, thoracic, and lumbar areas bilaterally. Her right ribs were also adjusted. She would lay on an intersegmental roller table as well as on ice for 10 minutes each at the end of her treatment session. The patient gave verbal consent and the parents provided written consent on behalf of their daughter for the publication of the treatment results, pictures and radiographs herein.
RESULTS
Between Jan. 21, 2015 and May 12, 2015 the patient had 24 in-office treatments over 15 weeks. She also performed 45 home blocking sessions over this time period. Upon re-assessment on May 12, 2015, her thoracolumbar scoliosis curve was reduced from 27° to 8° (Fig. 2C). This is a 19° improvement, much greater than the suggested 6° of minimal threshold for consideration for improvement according to the SOSORT/SRS criteria26). The patient reported her symptoms to be improved, and at the time of the exam, rated her LBP and headaches a 0/10 NRS. Her HDI score improved 64% and her ODI score improved 83%.
DISCUSSION
This case describes the successful reduction in curve magnitude and decrease in pain and disability scores in a 15-year-old female with AIS. Since curve progression is inevitable for most pediatrics with AIS without treatment34), all patients deserve an evidence-based, conservative, non-surgical treatment in attempt to stabilize/decrease their deformity. We believe the application of the engineering concept of the non-commutative properties of finite rotation angles under addition as a special form of CBP mirror image structural rehabilitation is a valid and under-utilized treatment.
The only other official documentation this unique CBP approach to scoliosis was reported in this journal by Harrison and Oakley22), who reported an average decrease of 10.4° curve reduction in five adult patients with lumbar or thoraco-lumbar scoliosis; the youngest of the five had a 24° improvement. The current case had a 19° improvement in an adolescent. It may be that greater changes may be achieved in those who are younger, having more pliable spines and less osteoarthritic changes and stiffness, however, future research should clarify this observation.
Most non-surgical AIS treatments have been criticized for lacking patient-specificity, and not being truly three- dimensional15, 35, 36). Specifically, many exercise programs seem ‘cookie cutter’ in approach and do not address the particular nuances of the patient’s spinal deformity35). This major criticism has been supported by the few studies that have directly compared ‘conventional’ exercise programs for AIS against methods employing ‘patient-specific’ customized exercise programs that have led to superior patient outcomes15, 37).
Noh et al.15) demonstrated that a group of AIS patients receiving a three-dimensional ‘corrective spinal technique’ (CST) showed greater improvements in Cobb angle, vertebral rotation, and quality of life measures, as measured on the scoliosis research society health related quality of life questionnaire (SRS-22), as compared to a ‘conventional’ exercise (CE) program. The CST treatment group underwent a program based on the concepts of ‘Schroth’11) as well as core stabilization, while the CE control group received a regimen focusing on core stabilization, including stretching exercises, lower-extremity and back muscle strengthening, as well as sensory motor training to restore back and posture alignment.
In another trial, Monticone et al.37) demonstrated that in AIS patients with curves less than 25° performing an exercise program consisting of ‘active self-correction and task-oriented spinal exercises’ had a reduction of their curve magnitude (>5°) and improvement in their quality of life scores (SRS-22) as compared to a group receiving ‘traditional’ spinal exercises. The control group’s spinal curve and quality of life measures remained stable, and these differences were also maintained for at least one year after the end of treatment.
We concur with Borysov et al.35) who argue that as with brace treatment, the in-brace correction is crucial to the final outcome in the patient38); therefore, so too should be the case when prescribing an exercise protocol. In this case, to ascertain the corrective effect on the patient, we performed a radiograph stress view to observe the reduction potential in a movement sequenced order of two mirror image positions/movements deduced from the initial static AP spinal radiograph. Although a second radiograph stress view was not obtained from the patient performing the series of movements in the opposite order, this would be the normal routine assessment for choosing the most appropriate sequence-specific order of mirror image movements to prescribe as an exercise and/or traction set-up19, 22).
This treatment approach is consistent with the trend with other successful non-surgical approaches by showing promise in treating AIS. This approach, however, is unique as it is a specific and fundamental application of an engineering law to treat human scoliosis posture and thus, demonstrates the pitfalls of other non-surgical approaches that have not considered the effect different sequences that two or more movements may have on the spinal configuration.
As described in chapter 11 of Harrison et al.19), the first application of the non-commutative properties of finite rotation angles under addition was performed by Dr. Don Harrison in the early 1980s. This concept was first presented to doctors through CBP seminars (www.idealspine.com) in 1997, first documented in conference proceedings in 200520) and 200621) and in this journal in 201722). The results of this case are limited by the fact that it is only a single case with no follow-up. Further, more than one treatment was used, traction, exercises, and blocking —therefore, it is not possible to conclude which had the greater effect on the spinal correction—all three have scientific evidence supporting their effectiveness, and because all were applied in this case, it may be why such a dramatic correction was achieved. The successful results of this case and others22), as well as the practical application of the concept, warrants further research, such as more case studies/series for different ages, curve types and magnitudes.
Acknowledgments
We thank Dr. Donald D. Harrison (deceased) for his insights into developing the unique approach to treating scoliosis as presented in this case.
REFERENCES
- 1.Konieczny MR, Senyurt H, Krauspe R: Epidemiology of adolescent idiopathic scoliosis. J Child Orthop, 2013, 7: 3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berven S, Bradford DS: Neuromuscular scoliosis: causes of deformity and principles for evaluation and management. Semin Neurol, 2002, 22: 167–178. [DOI] [PubMed] [Google Scholar]
- 3.Stokes IA, Burwell RG, Dangerfield PH, IBSE: Biomechanical spinal growth modulation and progressive adolescent scoliosis—a test of the ‘vicious cycle’ pathogenetic hypothesis: summary of an electronic focus group debate of the IBSE. Scoliosis, 2006, 1: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hawes MC, O’brien JP: The transformation of spinal curvature into spinal deformity: pathological processes and implications for treatment. Scoliosis, 2006, 1: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Negrini S, Aulisa AG, Aulisa L, et al. : 2011 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis, 2012, 7: 3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Weiss HR: Rehabilitation of adolescent patients with scoliosis--what do we know? A review of the literature. Pediatr Rehabil, 2003, 6: 183–194. [DOI] [PubMed] [Google Scholar]
- 7.Weiss HR, Negrini S, Hawes MC, et al. Members of the SOSORT: Physical exercises in the treatment of idiopathic scoliosis at risk of brace treatment -- SOSORT consensus paper 2005. Scoliosis, 2006, 1: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Berdishevsky H, Lebel VA, Bettany-Saltikov J, et al. : Physiotherapy scoliosis-specific exercises—a comprehensive review of seven major schools. Scoliosis Spinal Disord, 2016, 11: 20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weiss HR, Weiss G, Petermann F: Incidence of curvature progression in idiopathic scoliosis patients treated with scoliosis in-patient rehabilitation (SIR): an age- and sex-matched controlled study. Pediatr Rehabil, 2003, 6: 23–30. [DOI] [PubMed] [Google Scholar]
- 10.Weiss HR, Klein R: Improving excellence in scoliosis rehabilitation: a controlled study of matched pairs. Pediatr Rehabil, 2006, 9: 190–200. [DOI] [PubMed] [Google Scholar]
- 11.Otman S, Kose N, Yakut Y: The efficacy of Schroth s 3-dimensional exercise therapy in the treatment of adolescent idiopathic scoliosis in Turkey. Saudi Med J, 2005, 26: 1429–1435. [PubMed] [Google Scholar]
- 12.Negrini S, Zaina F, Romano M, et al. : Specific exercises reduce brace prescription in adolescent idiopathic scoliosis: a prospective controlled cohort study with worst-case analysis. J Rehabil Med, 2008, 40: 451–455. [DOI] [PubMed] [Google Scholar]
- 13.Mooney V, Gulick J, Pozos R: A preliminary report on the effect of measured strength training in adolescent idiopathic scoliosis. J Spinal Disord, 2000, 13: 102–107. [DOI] [PubMed] [Google Scholar]
- 14.McIntire KL, Asher MA, Burton DC, et al. : Treatment of adolescent idiopathic scoliosis with quantified trunk rotational strength training: a pilot study. J Spinal Disord Tech, 2008, 21: 349–358. [DOI] [PubMed] [Google Scholar]
- 15.Noh DK, You JS, Koh JH, et al. : Effects of novel corrective spinal technique on adolescent idiopathic scoliosis as assessed by radiographic imaging. J Back Musculoskeletal Rehabil, 2014, 27: 331–338. [DOI] [PubMed] [Google Scholar]
- 16.Harrison DD: Abnormal postural permutations calculated as rotations and translations from an ideal normal upright static spine. In: Sweere JJ, ed. Chiropractic Family Practice. Gaithersburg: Aspen Publishers, 1992, pp 1–22. [Google Scholar]
- 17.Oakley PA, Harrison DD, Harrison DE, et al. : Evidence-based protocol for structural rehabilitation of the spine and posture: review of clinical biomechanics of posture (CBP) publications. J Can Chiropr Assoc, 2005, 49: 270–296. [PMC free article] [PubMed] [Google Scholar]
- 18.Harrison DD, Janik TJ, Harrison GR, et al. : Chiropractic biophysics technique: a linear algebra approach to posture in chiropractic. J Manipulative Physiol Ther, 1996, 19: 525–535. [PubMed] [Google Scholar]
- 19.Harrison DE, Betz JW, Harrison DD, et al. : CBP structural rehabilitation of the lumbar spine. Harrison Chiropractic Biophysics Seminars, Inc. 2007.
- 20.Harrison DE, Oakley PA, Harrison DD: Reduction of deformity after CBP mirror image care incorporating the non-commutative properties of finite rotation angles in three patients with thoraco-lumbar scoliosis.8th Biennial Congress of the World Federation of Chiropractic, International Conference on Chiropractic Research,Sydney, Australia, June 16–18, 2005. p 287.
- 21.Harrison DE, Oakley PA, Harrison DD: Reduction of deformity after chiropractic biophysics mirror image care incorporating the non-commutative properties of finite rotation angles in five patients with thoraco-lumbar scoliosis [Platform presentation; the Association of Chiropractic Colleges’ Thirteenth Annual Conference, 2006] J Chiropr Educ, 2006, 20: 19–20. [Google Scholar]
- 22.Harrison DE, Oakley PA: Scoliosis deformity reduction in adults: A CBP® mirror image® case series incorporating the ‘non-commutative property of finite rotation angles under addition’ in five patients with lumbar and thoraco-lumbar scoliosis. J Phys Ther Sci, 2017, 29: (In Press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Harrison DE, Cailliet R, Harrison DD, et al. : Lumbar coupling during lateral translations of the thoracic cage relative to a fixed pelvis. Clin Biomech (Bristol, Avon), 1999, 14: 704–709. [DOI] [PubMed] [Google Scholar]
- 24.Harrison DE, Cailliet R, Harrison DD, et al. : How do anterior/posterior translations of the thoracic cage affect the sagittal lumbar spine, pelvic tilt, and thoracic kyphosis? Eur Spine J, 2002, 11: 287–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Harrison DE, Harrison DD, Cailliet R, et al. : Cervical coupling during lateral head translations creates an S-configuration. Clin Biomech (Bristol, Avon), 2000, 15: 436–440. [DOI] [PubMed] [Google Scholar]
- 26.Negrini S, Hresko TM, O’Brien JP, et al. SOSORT BoardsSRS Non-Operative Committee: Recommendations for research studies on treatment of idiopathic scoliosis: Consensus 2014 between SOSORT and SRS non-operative management committee. Scoliosis, 2015, 10: 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Harrison DE, Harrison DD, Cailliet R, et al. : Cobb method or Harrison posterior tangent method: which to choose for lateral cervical radiographic analysis. Spine, 2000, 25: 2072–2078. [DOI] [PubMed] [Google Scholar]
- 28.Harrison DE, Cailliet R, Harrison DD, et al. : Reliability of centroid, Cobb, and Harrison posterior tangent methods: which to choose for analysis of thoracic kyphosis. Spine, 2001, 26: E227–E234. [DOI] [PubMed] [Google Scholar]
- 29.Harrison DE, Harrison DD, Cailliet R, et al. : Radiographic analysis of lumbar lordosis: centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine, 2001, 26: E235–E242. [DOI] [PubMed] [Google Scholar]
- 30.Harrison DE, Holland B, Harrison DD, et al. : Further reliability analysis of the Harrison radiographic line-drawing methods: crossed ICCs for lateral posterior tangents and modified Risser-Ferguson method on AP views. J Manipulative Physiol Ther, 2002, 25: 93–98. [DOI] [PubMed] [Google Scholar]
- 31.Lechner R, Putzer D, Dammerer D, et al. : Comparison of two- and three-dimensional measurement of the Cobb angle in scoliosis. Int Orthop, 2017, 41: 957–962. [DOI] [PubMed] [Google Scholar]
- 32.Harrison DE, Harrison DD, Colloca CJ, et al. : Repeatability over time of posture, radiograph positioning, and radiograph line drawing: an analysis of six control groups. J Manipulative Physiol Ther, 2003, 26: 87–98. [DOI] [PubMed] [Google Scholar]
- 33.Oliver MJ, Twomey LT: Extension creep in the lumbar spine. Clin Biomech (Bristol, Avon), 1995, 10: 363–368. [DOI] [PubMed] [Google Scholar]
- 34.Kuru T, Yeldan İ, Dereli EE, et al. : The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil, 2016, 30: 181–190. [DOI] [PubMed] [Google Scholar]
- 35.Borysov M, Moramarco M, Sy N, et al. : Postural re-education of scoliosis - state of the art (mini-review). Curr Pediatr Rev, 2016, 12: 12–16. [DOI] [PubMed] [Google Scholar]
- 36.Borysov M, Mogiliantseva T: Rehabilitation of adolescents with scoliosis during growth—preliminary results using a novel standardized approach in Russia (Methodology). Curr Pediatr Rev, 2016, 12: 31–35. [DOI] [PubMed] [Google Scholar]
- 37.Monticone M, Ambrosini E, Cazzaniga D, et al. : Active self-correction and task-oriented exercises reduce spinal deformity and improve quality of life in subjects with mild adolescent idiopathic scoliosis. Results of a randomised controlled trial. Eur Spine J, 2014, 23: 1204–1214. [DOI] [PubMed] [Google Scholar]
- 38.Landauer F, Wimmer C, Behensky H: Estimating the final outcome of brace treatment for idiopathic thoracic scoliosis at 6-month follow-up. Pediatr Rehabil, 2003, 6: 201–207. [DOI] [PubMed] [Google Scholar]