Highlights
-
•
Adrenal gland hemangioma is an extremely rare benign vascular tumor.
-
•
It is frequently discovered as incidental radiological findings in abdominal imaging performed for various reasons.
-
•
The preoperative diagnosis is very difficult, generally CT and MR imaging are useful for the diagnosis of hemangioma.
-
•
In front of an adrenal mass discovered incidentally there are several factors to consider: the tumor size, its secreting character or not, imaging data suggestive of malignancy and complications.
-
•
These factors help in determining which incidental adrenal masses should be excised.
Keywords: Adrenal gland, Heamangioma, Incidentaloma
Abstract
Bakground
Adrenal glands hemangiomas are rare, benign and non-functional tumors. They are often discovered as incidentalomas either during imaging or autopsies. Nearly 70 cases were reported in the literature.
Case report
We report a case of a non-functional adrenal hemangioma (AH) that was incidentally found on abdominal ultra sonography (US) during the routine control of diabetes of a 58 year-old man. Imaging with US and Computed tomography (CT) showed an heterogeneous and partially calcified 6 cm tumor of the right adrenal gland. The mass was surgically excised and the histological examination concluded to an adrenal haemangioma.
Conclusion
Although rare, AH should be included in the differential diagnosis of the adrenal neoplasmas.
1. Introduction
Adrenal hemangioma (AH) is an extremely rare benign vascular tumor occurring in adrenal glands. Its clinical presentation is usually vague and it is frequently discovered as incidentaloma during imaging by ultrasonography, computed tomography or magnetic resonance imaging (MRI) [1]. It represents 0.01% of adrenal tumors and nearly 70 surgical cases have been reported in different database since 1955 [2].
We report a rare case of a non- functioning AH that was incidentally found during ultrasonography.
2. Case report
A 58 year-old male, with a history of diabetes for 4 years and surgery for an umbilical hernia 16 years ago, was referred to our institution for an adrenal mass found on an abdominal ultrasound performed during the supervision of his diabetes.
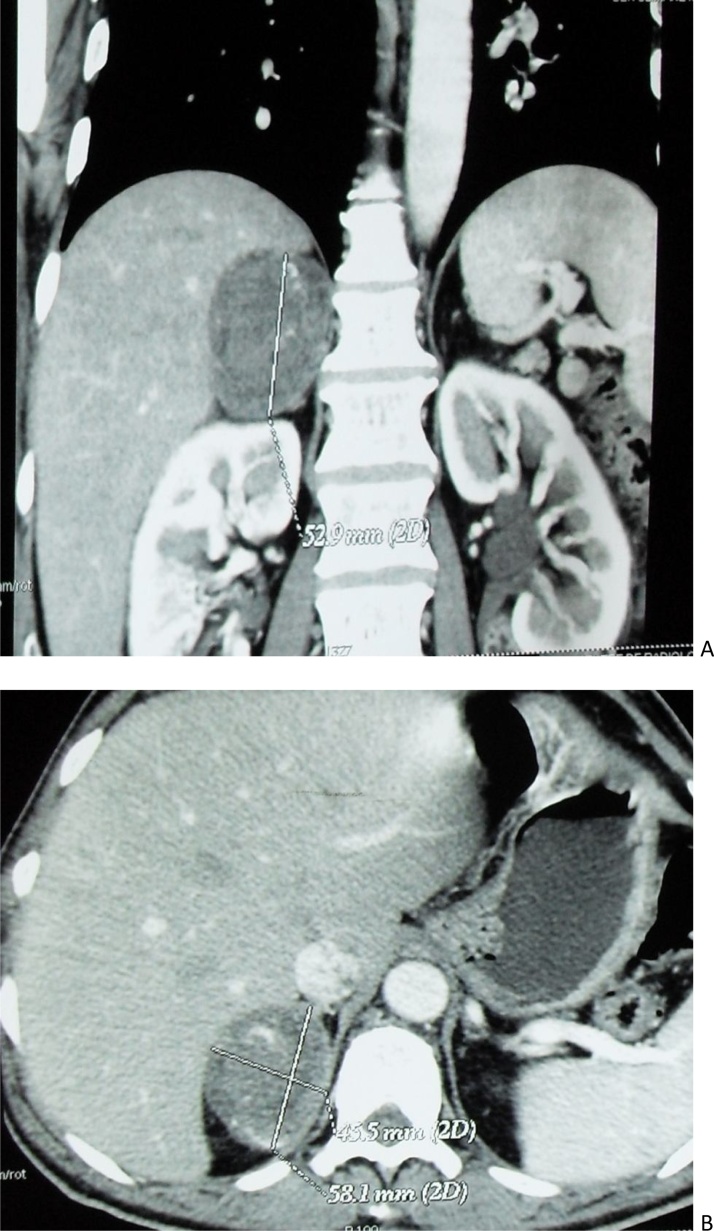
Clinical examination was normal; the patient had no clinical manifestations of adrenal medullary or cortical hyperfunction. Laboratory tests including Adrenal levels (plasma renine 3,3 ng/l, plasma aldosterone 27 ng/l, 24 h normetadrenalin excretion 263 ug/l, 24 h noradrenalin excretion 118 ug/l) were normal except 24 h 3 orthomethyldopamin that was slightly elevated (393 ug/l). Ultrasonography showed a well-defined 6 cm mass in the upper pole of the right kidney. Abdominal CT showed a well circumscribed, heterogeneous, partially calcified, retroperitoneal mass of the right adrenal gland (Fig. 1, Fig. 2).
Fig. 1.
Contrast-enhanced l abdominal CT image (A: axial cut, B: coronal reconstruction) showing an heterogeneous 6 cm right adrenal mass.
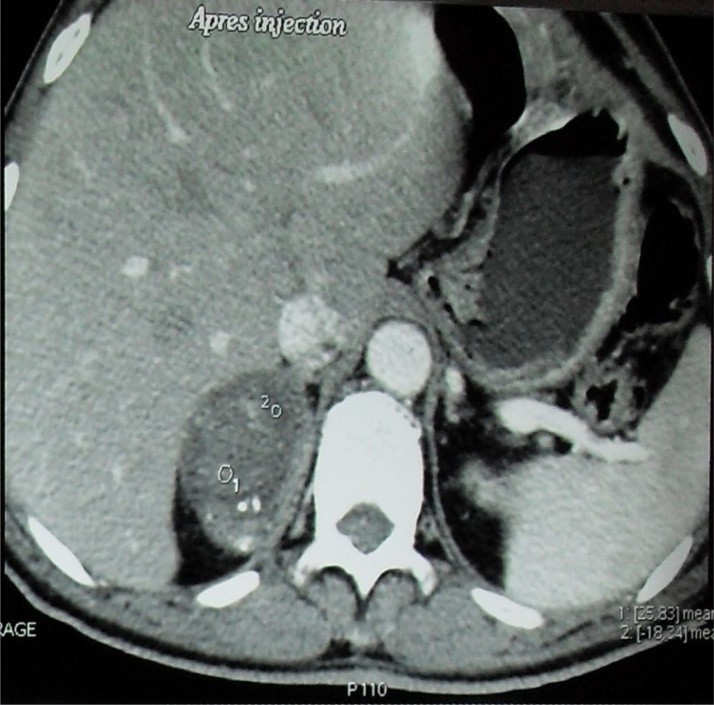
Fig. 2.
Contrast-enhanced l axial abdominal CT image showing an heterogeneous right adrenal mass containing microcalcification.
The size of the adrenal gland lesion, which indicated a possibility of malignant tumors, and the non-specific radiological features led to a mandatory surgical resection.
At laparotomy, through midline incision, we did not find any ascites or peritoneal carcinomatosis.
After a detachment of the right colon and detachment of Kocher we found that the adrenal mass was encapsulated. Excision proved to be relatively simple because the mass was separated easily from the surrounding tissues. Right adrenalectomy was performed without incidents.
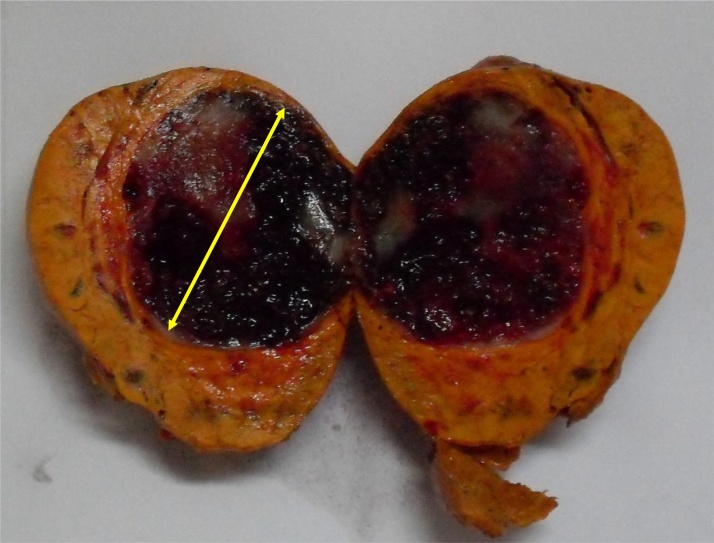
Pathological examination revealed a 6 cm mass, weighing 100 g. At section, it contained a 3.7 cm, well circumscribed, brownish nodule focally calcified with cystic areas (Fig. 3).
Fig. 3.
Gross section of adrenal hemangioma showing a well circumscribed, brownish nodule focally calcified with cystic areas.
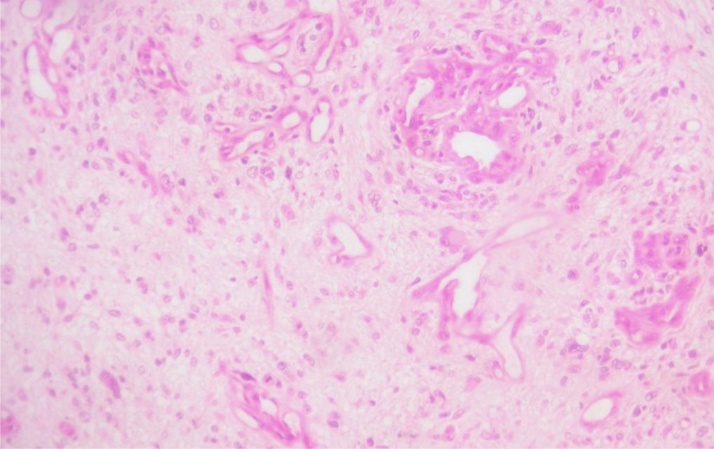
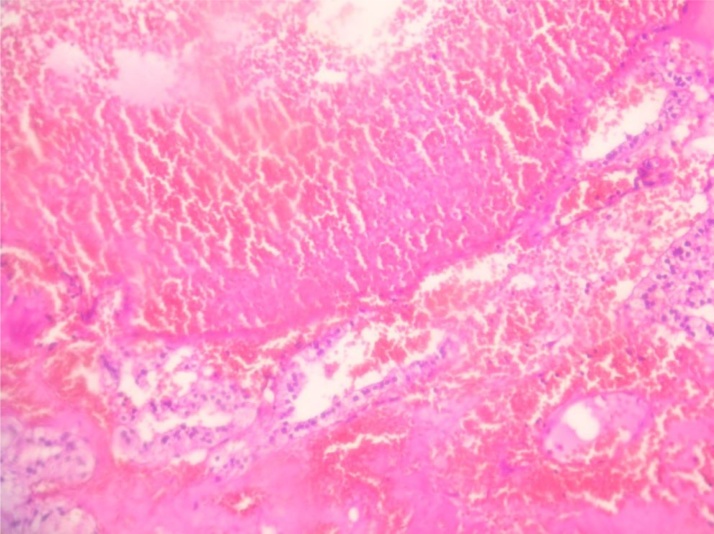
Microscopic evaluation showed multiple capillary vascular structures of variable sizes and shapes with a wall of variable thickness. These vascular structures showed a regular endothelial border. It contained diffuse calcifications and thrombi. The adrenal parenchyma surrounding the mass was hyperplasic (Fig. 4, Fig. 5).
Fig. 4.
Histopathological appearance of the adrenal hemangioma (hematoxylin-eosin staining ×40).
Fig. 5.
Histopathological findings of resected specimen with microscopic image showing multiple capillary vascular structures with a regular endothelial border. (hematoxylin-eosin staining ×100).
The patient did well post operatively and was discharged six days later. The patient was checked in 1 month of the surgery he had a solid median scar with no recurrence. And after we have not indicated any clinical or radiological monitoring because it is a benign pathology
3. Discussion
While adrenal tumors are relatively common, adrenal hemangiomas are extremely rare and pose problems in the differential diagnosis, because preoperatively they can be confused with adenoma or malignant tumors of the adrenal gland [3], [4]. Cavernous hemangiomas are rare benign tumors usually localized in the liver and the skin. The pathogenesis of AH is unclear. In the skin, the brain or the liver, they are usually congenital and hereditary factors may play a role in their pathogenesis.
AH may be associated with malignant extra-adrenal lesions such as small-cell carcinoma of the lung, gynecologic cancers and recently with familial adenomatous polyposis [5]. AH are mostly cavernous, unilateral and appear in the sixth or seventh decade of life with a 2:1 female to male ratio. Their sizes range from 2 cm to 25 cm in diameter [6].
These benign tumors are usually discovered as incidental radiological findings in abdominal imaging performed for various reasons. Generally CT and MR imaging are useful for the diagnosis of hemangioma. Contrast enhanced CT displays a characteristic peripheral patchy enhancement and highly dense peripheral rim. This pattern of peripheral spotty contrast enhancement is crucial for diagnosing adrenal hemangioma. When the hemangioma is seen as only a thin-rim enhancement, the preoperative diagnosis is very difficult because this pattern is seen in other adrenal tumors. Marked hyperintensity on T2- weighted images and focal hyperintensity on T1 weighted images that showed focal hemorrhage and calcification may be seen [6], [7], [8]. These findings can also be seen in other adrenal tumors (pheochromocytoma, carcinoma and adenoma) and are not pathognomonic of adrenal haemangioma [6], [7].
In up to two thirds of cases, radiographs show speckled calcification throughout the entire neoplasm. However, observing the combination of these findings can lead to the correct diagnosis. Angiography usually reveals peripheral pooling of the contrast, persisting well during the venous phase [8].
AH are most commonly non-functional tumors with rare cases of hormone-secreting adrenal hemangiomas described in literature [9]. In our case, tumor was presented with a slightly increased rate of 3 orthomethyldopamine. This slight elevation is isolated and remains insignificant, especially since the patient did not have clinical features overtly suggestive of a functioning adrenal tumor.
In most cases the final diagnosis is made by histopathology after surgical resection.
In front of an adrenal mass discovered incidentally there are several factors to consider that are the tumor size, its secreting character or not and imaging data Suggestive of malignancy
For this reason guidelines have been developed to help clinicians and patient in determining which incidental adrenal masses should be excised.
Resection is generally advocated for all functioning lesions, as well as those with features suggestive of malignancy.
Adrenal incidentalomas larger than 5 cm in diameter must be excised since the risk of adrenal cancer ranges from 35% to 98%. For lesions measuring 4 cm–5 cm, other imaging features, history of extra adrenal malignancy, patient’s preference, age and comorbidities should be taken into consideration [10]. Adrenalectomy and follow-up with imaging are both acceptable in such cases.
Other indications for surgery include mass-effect type symptoms from neighboring organs and complications such as hemorrhage [11], [12].
Adrenalectomy can be performed laparoscopically for lesion measuring less than 5 cm [13]. Larger tumors with suspected malignancy are treated preferably with open technique through an anterior (subcostal or midline incision), posterior or thoracoabdominal approach [14].
In our case, the patient underwent laparotomy with midline incision because of the tumor size, malignancy suspicion and in order to cure an umbilical eventration.
4. Conclusion
Although rare, adrenal hemangioma should be included in differential diagnosis of adrenal neoplasms. The treatment of choice is surgical excision due the difficulty of excluding malignancy.
This work have been made following the SCARE Guidelines [15].
Data and supporting materials section
Pubmed have been used searching for the articles cited in the reference list.
Conflicts of interest
I declare no competing interests.
No financial and personal relationships with other people or organisations that could inappropriately influence (bias) their work.
Funding
No source of funding.
Ethical approval
No ethics committee approval is required at our institution for a case report involving a single patient. Military hospital ethic committee.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal. Written informed consent was obtained from the patient for publication of this case report and accompanying images.
Authors’ contribution
IZ performed the clinical evaluation of the patient. IZ and SH conceived of the report. IZ, AH and SH performed the literature search and drafted the report. MM and ME critically reviewed and edited the manuscript. All authors read and approved the final manuscript.
Guarantor
Zemni Ines.
Contributor Information
I. Zemni, Email: ines.zemni@yahoo.fr, ines.zemni81@gmail.com.
S. Haddad, Email: sabriinea@yahoo.com.
A. Hlali, Email: abj_hlali@yahoo.fr.
M.H. Manai, Email: manaihedi@planet.tn.
M. Essoussi, Email: mdessousii@yahoo.fr.
References
- 1.Arkadopoulos N., Kyriazi M., Yiallourou A.I., Stafyla V.K., Theodosopoulos T., Dafnios N., Smyrniotis V., Kondi-Pafiti A. World J. Surg. Oncol. 2009;5(February (7)):13. doi: 10.1186/1477-7819-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Johnson C.C., Jeppesen F.B. Haemangioma of the adrenal. J. Urol. 1955;74:573–577. doi: 10.1016/S0022-5347(17)67320-8. [DOI] [PubMed] [Google Scholar]
- 3.Wang Li, Dang Yiwu, He Rukun, Chen Gang. Rare cavernous hemangioma of adrenal gland: case report. Sao Paulo Med. J. 2014;132(4):249–252. doi: 10.1590/1516-3180.2014.1324715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Heis H.A., Bani-Hani K.E., Bani-Hani B.K. Singapore Med. J. 2008;49(September (9)):e236–e237. [PubMed] [Google Scholar]
- 5.Bacha D., Chaabane A., Khanchel F. Giant adrenal cavernous hemangioma in a patient withfamilial adenomatous polyposis. Clin. Pract. 2016;6:878. doi: 10.4081/cp.2016.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Xu H.X., Liu G.J. Huge cavernous hemangioma of the adrenal gland: sonographic, computed tomographic, and magnetic resonance imaging findings. J. Ultrasound Med. 2003;22:523–526. doi: 10.7863/jum.2003.22.5.523. [DOI] [PubMed] [Google Scholar]
- 7.Yamada T., Ishibashi T., Saito H. Two cases of adrenal hemangioma: CT and MRI findings with pathological correlations. Radiat. Med. 2002;20:51–56. [PubMed] [Google Scholar]
- 8.Abou El-Ghar M., Refaie H., El-Hefnawy A. Adrenal hemangioma: findings at multidetector CT with short review of the literature. Case Rep. Radiol. 2011;2011 doi: 10.1155/2011/601803. 3 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Thiele J.W., Bodie B. Adrenal hemangioma. Surgery. 2001;129:373–374. doi: 10.1067/msy.2001.105653. [DOI] [PubMed] [Google Scholar]
- 10.Oh B.R., Jeong Y.Y., Ryu S.B., Park Y.I., Kang H.K. A case of adrenal cavernoushaemangioma. Int. J. Urol. 1997;4:608–610. doi: 10.1111/j.1442-2042.1997.tb00318.x. [DOI] [PubMed] [Google Scholar]
- 11.Forbes T.L. Retroperitoneal haemorrhage secondary to rupturedcavernous hemangioma. Can. J. Surg. 2005;48:78–79. [PMC free article] [PubMed] [Google Scholar]
- 12.Johnson E., Sherif A., Bermudez F. Hemorrhage; unusual presentation of adrenal hemangioma. Am. J. Med. Case Rep. 2016;4(7):248–250. [Google Scholar]
- 13.Nigri G., Bellagamba R., Giaccaglia V., Felicioni F., Aurello P., D’Angelo F., Del Gaudio M., Ramacciato G. Minimally invasive adrenalectomyfor incidentally discovered cavernous haemangioma. Minim. Invasive Ther. Allied Technol. 2008;17(4):255–258. doi: 10.1080/13645700802274323. [DOI] [PubMed] [Google Scholar]
- 14.Trupka A., Hallfeldt K., Schmidbauer S. Laparoscopic adrenalectomy with lateral approach–a comparison with the conventional dorsal technique. Chirurg. 2001;72:1478–1484. doi: 10.1007/s001040170014. [DOI] [PubMed] [Google Scholar]
- 15.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., for the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]