Highlights
-
•
Giant juvenile fibroadenomas are very rare and they have very low prevalence in prepubertal period. Although they should not be ruled out in differential diagnosis in premenarchal period.
-
•
Breast examination in premenarchal girls and adolescents plays a pivotal role in order to prevent these peculiar giant lesions.
-
•
Another remarkable point is the rapid growth of these breast lesions that should not be ruled out in the diagnostic process of the continuously growth of the adolescent breast.
Keywords: Fibroadenoma, Giant juvenile fibroadenoma, Adolescence, Breast, Prepuberty
Abstract
Introduction
Giant juvenile fibroadenomas represent only the 0.5% of all fibroadenomas, constituting a rare condition in adolescence. In prepuberty, the presence of this condition is extremely rare.
Presentation of case
We describe a rare case of a 12- year-old Caucasian girl who presented to our Hospital complaining of a palpable mass with rapid enlargement in her right breast that she had first noticed 3 months ago. Her menarche hadn’t occurred yet.
Discussion
Physical examination showed a giant mass of 15 × 13 cm in the right breast. The patient was further evaluated via ultrasonography showing a sole large lesion of 13 × 12 cm in the right breast. A surgical procedure under general anesthesia was performed. Histopathological findings after the surgical excision were suggestive of giant juvenile fibroadenoma. The patient has a normal breast development over a period of 9 month follow up.
Conclusion
Giant juvenile fibroadenomas should be included in differential diagnosis of a breast mass in prepubertal girls despite the fact that they are very rare in prepuberty, tend to appear later during adolescence and their prevalence is lower in Caucasians. The remarkable size and the rapid growth of the lesion should not be ruled out in the diagnostic process of an adolescent breast.
1. Introduction
Fibroadenoma is the most common type of benign lesions diagnosed in young women. Juvenile fibroadenoma is the term used for fibroadenomas with first appearance in childhood or adolescence. A juvenile fibroadenoma is further called ‘giant’ when it is greater than 5 cm, more than 500 g or replaces more than 80% of the breast. Giant juvenile fibroadenomas represent 1–8% of breast disorders in adolescents [1]. In pre-pubertal girls, the presence of this condition is extremely rare [2]. Phyllodes tumor and virginal breast hypertrophy (juvenile macromastia) should be included in the differential diagnosis [3]. Based on the literature, we report an extremely rare case of a giant 14 cm juvenile fibroadenoma, in a pre-pubertal Caucasian girl. This work has been reported according to the SCARE criteria [4].
2. Case summary
A 12-year-old Caucasian child presented to the Emergency Unit of our Hospital in July 2016 complaining of a palpable mass with rapid enlargement in her right breast that she first noticed 3 months ago. She had no gynecologic complaints or contralateral breast pain and her menarche hadn’t occurred yet. Her personal medical history was unremarkable with no drug using. Her family history for cancer was negative. Her psychosocial and family medical history was uneventful. She was non smoker. Fever, burning sensation, redness, trauma, pyorrhea, lactorrhea, weight loss or fatigue were not mentioned.
Upon arrival, physical examination revealed a giant 15 × 13 cm mass in the right breast, while the contralateral breast was normal. The mass was located in the upper outer quadrant. The contralateral breast was found to be Tanner 2 stage of maturity. The lesion was firm, non tender and mobile. There was no associated lymphadenopathy in the axilliary and supraclavicular regions. The overlying skin was tense, while subcutaneous enlarged veins were present. The pain was managed with paracetamol per os.
Her BMI was 14.4 kg/m2. She had a temperature of 36.3 °C, her blood pressure was 123/72 mmHg and her pulse rate was 75 beats/min. All laboratory examinations were within normal range.
The patient was further evaluated with breast ultrasonography via 4–9 MHz linear transducer; a sole, quiet large (13 × 12) iso-to hypoechoic lesion with normal walls and small cystic spaces was revealed in the right breast. Increased internal vascularization was found through color Doppler ultrasound (Fig. 1).
Fig. 1.
Breast ultrasonography; a–c. B-Mode – well defined, encapsulated, lobulated, iso- to hypoechoic mass with small cystic spaces; d–f. Color Doppler – Increased internal vascularity.
A trucut biopsy (core needle biopsy) of the breast mass was the next step of the lesion’s investigation and was suggestive of fibroadenoma.
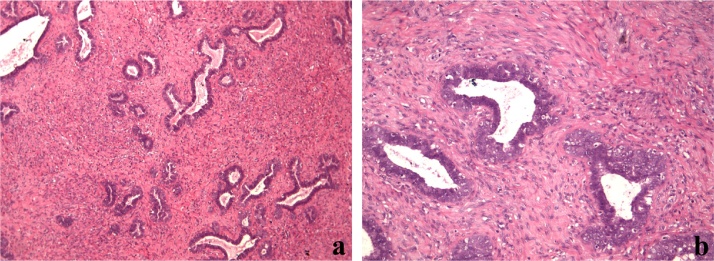
A surgical procedure by a gynecologist specialized in breast surgery with 5 years experience in breast surgical procedures was performed under general anesthesia; a total excision of the lesion was performed conserving the normal tissue of the breast, the nipple and the areola. The excised mass was 14 × 12 cm and weighed 800 g. The risk of hematoma was minimized through the use of monopolar electrocautery pressure dressings. Also, a simple silicone drainage was inserted in the wound and was removed the second postoperative day to avoid the potential post-operative seroma or hematoma. There were no peri-operative complications and the breast healed well (Fig. 2). Post-operatively the patient was followed up in a regular ward. She was administered antibiotics, fluids and painkillers intravenously. Histopathology was suggestive of giant juvenile fibroadenoma with pericanalicular growth pattern. Epithelial hyperplasia was present; mild to moderate stromal cellularity was observed without nuclear atypia or multiformity; mitotic count was 0–3 mitoses/10-HPFs (Fig. 3). The patient was compliant with the therapeutic program which was well tolerated, with no significant side-effects or further hospitalization. The girl has a normal breast development over a period of 9 month follow up with clinical evaluation and ultrasound examination.
Fig. 2.
a. Preoperative image of the breast; b–e. Intraoperative images of the mass; f, g. postoperative images of the breasts.
Fig. 3.
Histopathological images after haematoxylin- eosin stain; a, b. Juvenile fibroadenoma is characterized by stromal cellularity, epithelial hyperplasia and more often by pericanalicular architecture.
3. Discussion
The presence of breast lesions in children and adolescent females is a rare event including benign and malignant tumors such as fibroadenomas, phyllode tumors and secretory carcinoma [5].
When fibroadenomas occur in children and adolescent females, they are categorized as ‘juvenile fibroadenomas’ [1]; they usually present between 10 and 18 years and they tend to appear more commonly in African-American females [3]. The presence in Caucasian females, like it is in our case, is not common. They constitute an unusual type of tumor, representing 1–2% of breast lesions in young females [6]. Possible pathogenetic mechanisms include increased stimulation of estrogens and/or mammary receptor sensitivity or decreased estrogen antagonists’ levels, such as progesterone, during puberty [3].
In women between the second and third decade of life, fibroadenomas have a prevalence of 2,2% whereas the prevalence seems to be even higher (7–13%) among patients presenting to specialized clinics [7].
Fibroadenomas are benign neoplasms with epithelial (glandular) and stromal (fibrous) components [8]. The presence of epithelial polyclonal tissue increases the risk of malignancy with the relative risk ranging from 2.1 to 3.1. Lobular malignant tumor is the most common related malignancy [9]. The incidence of malignancy arising from a fibroadenoma specimen is rare, and ranges from 0.002% to 0.125% [10].
Recently, Dara Ross et al. showed that fibro epithelial lesions (FELs) were the most common type of lesion characterized by a pericanalicular growth pattern, collagenous stroma and floridly glandular lobular architecture [5].
Clinical examination and medical history can provide pivotal details and clues for the underlying cause of the lesion. Clinically, fibroadenomas are usually asymptomatic and painless. Additionally, they are smooth, firm, non-tender and mobile lesions not damaging the overlying skin and the nipple areola complex area [6].
The term ‘Giant fibroadenoma’ is used when the lesion reaches a size larger than 5 cm, exceeds 500 g in weight or occupy the four-fifths of the breast; it also may lead to skin stretching and ulceration due to pressure, nipple and areolar enlargement and distended veins [11]. In our case, the excised mass was much larger than 5 cm (14 cm) and its weight was much larger than 500 g (800 g).
Giant juvenile fibroadenomas represent only 0,5% of all fibroadenomas. Michael Sosin et al., in a systematic literature review based on 153 patients, showed that mean age of giant juvenile fibroadenomas was 16.7 years old, with a mean lesion size of 11.2 cm [1]. In prepuberty, the presence of this condition is extremely rare [2]. Here is another crucial point showing the rarity of our presented case; the young female was just 12 years old and her menarche hadn’t occurred yet.
Evaluation includes history, physical examination, and radiographic evaluation, usually ultrasound [12]. Clinically, the presence of giant fibroadenomas typically is associated with pain and breast enlargement. They are usually smooth, firm, non tender and mobile to palpation; most commonly they occur in the upper outer quadrant of the breast [13].
Ultrasonography is the gold standard technique in the assessment of these masses. Smith et al. in a recent study showed that the most common benign lesion in females under 25 years was the fibroadenoma, while in 78,8% histopathology confirmed the ultrasonic examination [14]. Ultrasonographically, they appear as well circumscribed hypoisoechoic, homogeneous lesions tending to be oval, round or macrolobulated. Color Doppler reveals non-vascularization or minimal internal vascularity in 67% of patients in which 33% are central vessels.
Magnetic resonance imaging (MRI), even though it is not the first tool in the diagnosis of such cases, is very helpful in order to evaluate the exact size and location of the lesion, and to discriminate between vascular masses and normal breast tissue. Mammography isn’t used as a routine method of choice in order to evaluate these masses because the risk of breast malignancy is low, the adolescent breast tissue is not radiographically dense but it is more sensitive to ionizing radiation leading to an increased risk of malignancy [15].
In our case, the gold standard method of ultrasonography was used with excellent results, revealing the huge breast mass.
Trucut Needle Biopsy (TCB) or Core Needle Biopsy (CNB) which was used in our hospital, is a reliable, simple, reproducible, and inexpensive technique which can be adapted even for low-income group of patients and in developing countries [16].
The complete surgical excision of the mass is the most efficient therapeutic choice in the management of these lesions as their rapid growth may cause symptoms such as pain, as it was the case with our patient. Complete surgical excision is associated with minor post-operative complications and low rate of recurrence [1], [2]. However, recurrence may be occurring in about 33% at the 5-year follow up after excision [3]. Mastectomy is performed only in unusual cases or recurrent giant fibroadenomas [1]. Breast reconstruction should be performed after the mastectomy, especially in young patients, minimizing the psychological trauma; prosthesis or autologous tissue method may be used [12].
When the giant lesion is diagnosed, the surgical excision appears to be the treatment of choice in order to avoid complications including skin changes, ulceration and pain. Excision and reconstruction of the native breast are based on individual patient characteristics; sometimes they may require mastopexy, reduction mammoplasty, or augmentation as supplementary techniques [12].
In conclusion, we would like to clearly stress the three following points to learn from this case report: 1.The very low prevalence of the lesion. 2. The rapid growth of the tumor. 3. The remarkable large size of the mass which should not be excluded in the differential diagnosis of a breast lesion in adolescence.
Conflict of interest statement
NA.
Funding
NA.
Ethical approval
IRB/Ethics Committee ruled that approval was not required for this study.
Consent
Written parental or guardian consent is confirmed for the publication of this case report and accompanying images as the patient is only 12 years old. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Authors contribution
Conception and design the study: Aris Giannos, Sofoklis Stavrou.
Acquisition of data: Sofoklis Stavrou.
Analysis and/or interpretation of data: Aris Giannos, Sofoklis Stavrou.
Drafting the manuscript: Aris Giannos, Sofoklis Stavrou, Christina Gkali, Eleni Chra, Spyridon Marinopoulos, Athanasios Chalazonitis, Constantine Dimitrakakis, Peter Drakakis.
Revising the manuscript critically for important intellectual content: Constantine Dimitrakakis, Aris Giannos, Peter Drakakis.
Approval of the version of the manuscript to be published: Aris Giannos, Sofoklis Stavrou, Christina Gkali, Eleni Chra, Spyridon Marinopoulos, Athanasios Chalazonitis, Constantine Dimitrakakis, Peter Drakakis.
Guarantors
Aris Giannos.
Sofoklis Stavrou.
Christina Gkali.
Eleni Chra.
Spyridon Marinopoulos.
Athanasios Chalazonitis.
Constantine Dimitrakakis.
Peter Drakakis.
Acknowledgement
The authors are grateful to all who provided assistance during the preparation of this manuscript.
Contributor Information
Aris Giannos, Email: arisgiannos@yahoo.gr.
Sofoklis Stavrou, Email: sfstavrou@yahoo.com.
Christina Gkali, Email: chr.gkal@gmail.com.
Eleni Chra, Email: Eleni.chra@gmail.com.
Spyridon Marinopoulos, Email: smarinopoulos@outlook.com.
Athanasios Chalazonitis, Email: red-rad@ath.forthnet.gr.
Constantine Dimitrakakis, Email: dimitrac@ymail.com.
Peter Drakakis, Email: pdrakakis@hotmail.com.
References
- 1.Sosin M., Pulcrano M., Feldman E.D., Patel K.M., Nahabedian M.Y., Weissler J.M. Giant juvenile fibroadenoma: a systematic review with diagnosticand treatment recommendations. Gland Surg. 2015 Aug;4(4):312–321. doi: 10.3978/j.issn.2227-684X.2015.06.04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaurav K., Chandra G., Neelam K., Kumar S., Singla H., Yadav S.K. A pre-pubertalgirl with giant juvenile fibroadenoma: a rare case report. Int. J. Surg. Case Rep. 2015;16:87–89. doi: 10.1016/j.ijscr.2015.09.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Song B.S., Kim E.K., Seol H., Seo J.H., Lee J.A., Kim D.H. Giant juvenilefibroadenoma of the breast: a case report and brief literature review. Ann. Pediatr. Endocrinol. Metab. 2014;19(March (1)):45–48. doi: 10.6065/apem.2014.19.1.45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Ross D.S., Giri D.D., Akram M.M., Catalano J.P., Olcese C., Van Zee K.J. Fibroepithelial lesions in the breast of adolescent females: a clinicopathological study of 54 cases. Breast J. 2017 Mar;23(2):182–192. doi: 10.1111/tbj.12706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chang D.S., McGrath M.H. Management of benign tumors of the adolescent breast. Plast. Reconstr. Surg. 2007;120(July (1)):13e–19e. doi: 10.1097/01.prs.0000264396.03452.62. [DOI] [PubMed] [Google Scholar]
- 7.Santen R.J., Mansel R. Benign breast disorders. N. Engl. J. Med. 2005;353(July (3)):275–285. doi: 10.1056/NEJMra035692. [DOI] [PubMed] [Google Scholar]
- 8.Townsend C.M. Jr., Beauchamp R.D., Evers B.M., Mattox K.L., editors. Sabiston Textbook of Surgery. 16th ed. WB Saunders; Philadelphia: 2001. [Google Scholar]
- 9.Templeman C., Hertweck S.P. Breast disorders in the pediatric and adolescent patient. Obstet. Gynecol. Clin. N. Am. 2000;27:19–34. doi: 10.1016/s0889-8545(00)80004-2. [DOI] [PubMed] [Google Scholar]
- 10.Wu Y.T., Chen S.T., Chen C.J. Breast cancer arising within fibroadenoma: collective analysis of case reports in the literature and hints on treatment policy. World J. Surg. Oncol. 2014;12(1):335. doi: 10.1186/1477-7819-12-335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gatta G., Iaselli F., Parlato V., Di Grezia G., Grassi R., Rotondo A. Differential diagnosis between fibroadenoma, giant fibroadenoma and phyllodes tumour: sonographic features and core needle biopsy. Radiol. Med. 2011;116(September (6)):905–918. doi: 10.1007/s11547-011-0672-y. [DOI] [PubMed] [Google Scholar]
- 12.Kozomara D., Šutalo N., Galić G., Jurišić S., Trninć Z. Giant unilateral breast juvenile fibroadenoma – the aesthetic outcome of surgical treatment should be considered. Psychiatr. Danub. 2016;28(December (Suppl.-2)):256–259. [PubMed] [Google Scholar]
- 13.De Silva N.K., Brandt M.L. Disorders of the breast in children and adolescents, part 2: breast masses. J. Pediatr. Adolesc. Gynecol. 2006;19:415–418. doi: 10.1016/j.jpag.2006.09.002. [DOI] [PubMed] [Google Scholar]
- 14.Smith G.E., Burrows P. Ultrasound diagnosis of fibroadenoma – is biopsy alwaysnecessary? Clin. Radiol. 2008;63(May (5)):511–515. doi: 10.1016/j.crad.2007.10.015. discussion 516–7. [DOI] [PubMed] [Google Scholar]
- 15.Gobbi D., Dall'Igna P., Alaggio R., Nitti D., Cecchetto G. Giant fibroadenoma of the breast in adolescents: report of 2 cases. J. Pediatr. Surg. 2009;44(February (2)):e39–e41. doi: 10.1016/j.jpedsurg.2008.11.041. [DOI] [PubMed] [Google Scholar]
- 16.Samantaray Sagarika, Panda Niharika, Besra Kusumabati, Pattanayak Lucy, Samantara Subrat, Dash Sashibhusan. Utility of tru-cut biopsy of breast lesions – an experience in a regional cancer center of a developing country. J. Clin. Diagn. Res. 2017;11(March (3)):EC36–EC39. doi: 10.7860/JCDR/2017/23572.9548. [DOI] [PMC free article] [PubMed] [Google Scholar]