Highlights
-
•
Skeletal deformity surgery is a difficult procedure which requires meticulous planning.
-
•
Good results demand precise application of the surgical plan during the surgery.
-
•
3D software helps to make precise surgical plans and design case specific surgical tools.
-
•
3D printing of case specific tools renders surgery easy and precise.
Keywords: Skeletal deformity, Malunion, Patient specific planning, Patient specific surgery, 3D print, 3D plan
Abstract
Introduction
Skeletal deformity correction is a procedure of high aesthetic and functional demand. Therefore, meticulous surgical planning has always been mandatory. However, it is known that during the surgery things may often get slippery, leaving the surgeon no chance but improvisation. Because of this shortcoming it is not a rare occasion to find unhappy patients that have undergone deformity correction surgery.
Presentation of case
Our patient was an eighteen-year-old male who had 40° cubitus varus deformity (with 20° flexion and extension deficits) due to a right humerus supracondylar fracture, obtained eight years ago. He had two prior surgeries at the year of injury. Considering the severity of the deformity we decided to plan the surgery with 3D software, obtain 3D printed models (to further help with surgical fixation options) and finally, use a custom 3D printed resection guide to apply the plan during the surgery.
Discussion
Traditional methods of skeletal deformity correction lack the preoperative precision and tools to perform the plan during the surgery. Deformity correction with 3D images and 3D printed patient specific instruments do help the surgeon to accomplish correct deformities with results identical to surgical plan.
Conclusion
Superior precision of the 3D planning and very easy utilization of the patient specific 3D printed instruments during the skeletal deformity surgery provides unparalleled and foreseeable results. This methodology is prone to be gold standard for deformity surgery in the near future.
1. Introduction
Fractures of the elbow supracondylar region has been defined as one of the most frequent fractures of the childhood with cubitus varus deformity as a complication [1]. Cubitus varus deformity consists of varus angulation in all patients and various amounts of internal rotation and extension deformity [2]. The comorbidities which acompany the afore mentioned bony deformties are; cosmetic problems, loss of range of motion, pain, posterolateral rotatory instability, tardy ulnar nerve palsy, and internal rotational malalignment [3]. The surgical indications of deformity correction is not very well established making this a question of debate between orthopaedic surgeons [4]. Nevertheless, when an indication is made per patient basis, the cosmetic results after the surgical correction is generally on the very top of expectations list.
The defined methods of correctional osteotomy methods have their pros and cons [4], [5]. Lateral closing wedge osteotomy as being the simplest of all methods generally results in prominent lateral condyle which in return affects patient expectaions negatively [4], [5]. Lately computer model planing and patient specific instrumentation have been advocated to over come this problem [5], [6]. The previously proposed computerized osteotomy patterns and patient specific surgery tecniques still need to be investigated further to decide if they match the needs of the surgeon and the patient.
Here we describe a totally new method which we believe overcomes most of the problems of cubitus varus correctional surgery. Apart from utilizing 3D computer model planing and custom osteotomy guides overall it is very simple in phylosophy and it seems to eliminate cosmetic problem due to lateral condyle prominence. Furthermore, it provides the surgeon with 3D printed bone models which are very useful for determining bone fixation options to assure secure fixation which in return helps to start vigorious range of motion exercises as soon as surgical inflamation diminishes.
2. Presentation of case
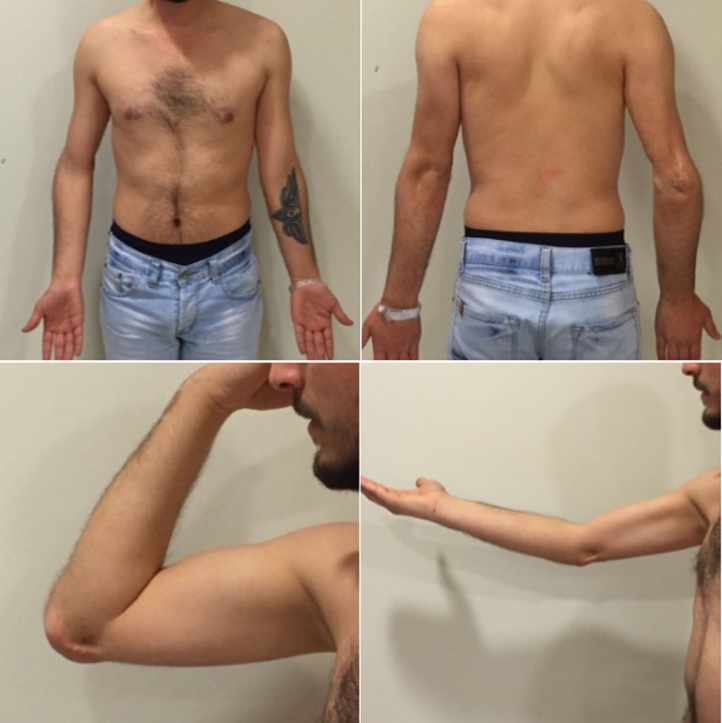
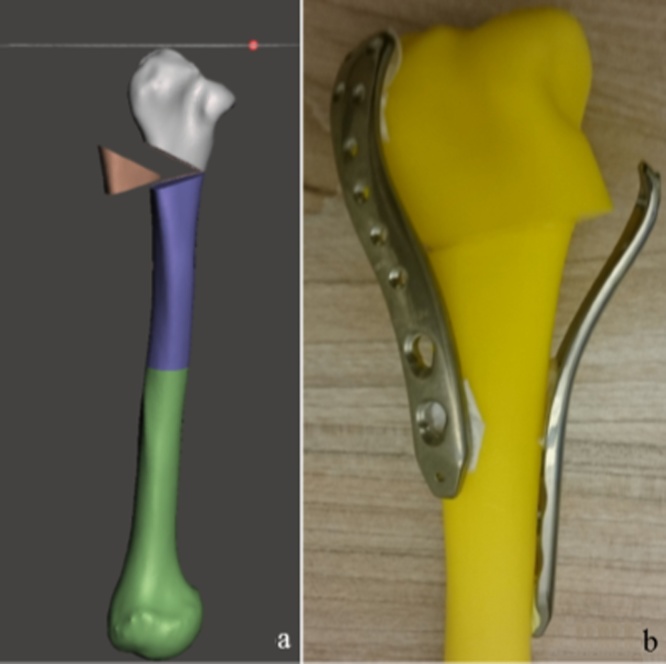
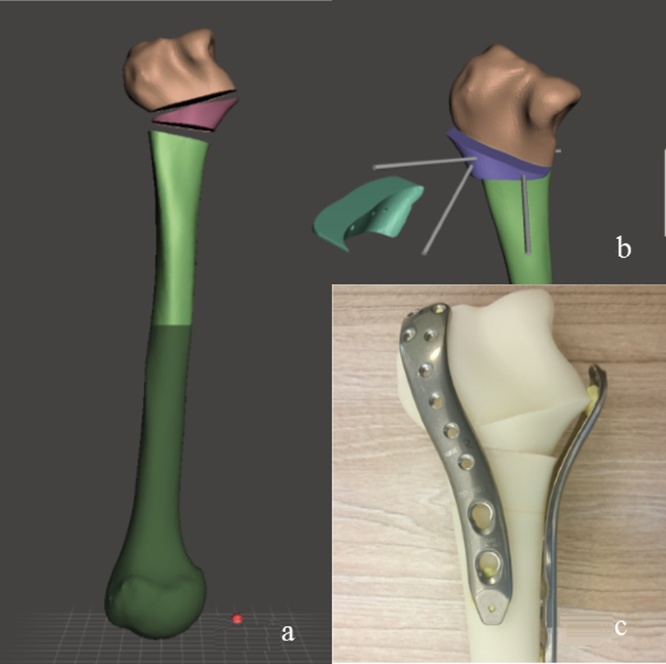
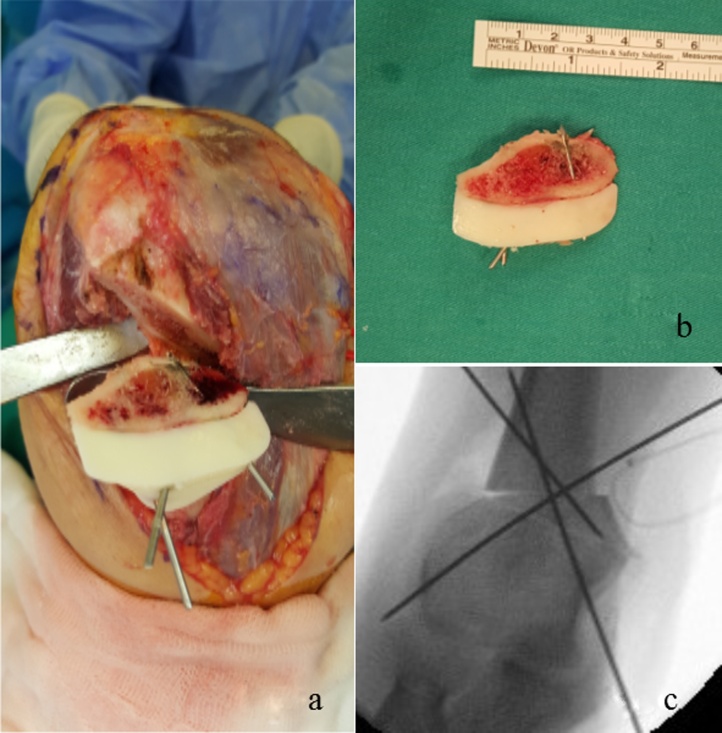
This case report has been written in line with the SCARE statements [7]. Our patient was an eighteen-year-old male who had 40° cubitus varus deformity with 20° flexion and extension deficits due to a right humerus supracondylar fracture, obtained eight years ago (Fig. 1). The patient’s written informed consent was obtained prior to the study. He had two prior surgeries at the year of injury. His medial epicondyle was not apparent in his radiological workout probably due to avascular necrosis of the medial epicondylar fragment. Although he had reasonable range of motion he was also complaining of mild to moderate pain during and after heavy duty activities. He was also very upset with the appearance of his arm. We worked with a web based orthopedic consultancy firm specialized in 3D orthopedics and patient specific instrumentation called Metaklinik (Metaklinik.com) to create the surgical plan and obtain patient specific osteotomy guide for our case. First, 3D computer models of the patient’s both humeri were obtained. Later, the uninjured side’s model was mirrored to represent original anatomy for the injured side. Later, both models were visually aligned over each other in the 3D working environment to better visualize and comprehend the deformity (Fig. 2). The graphics software was used to simulate possible osteotomy options and results. Analyzing osteotomy options in the 3D environment we found out that resecting a 40° wedge, all at once to correct the deformity would either result in joint translation in coronal plane or poor bone contact with possible fixation difficulties (Fig. 3a,b). Afterwards, we simulated for an intercalary osteotomy by resecting a 20° (half the amount of varus deformity) wedge. After obtaining the wedge it was flipped 180° in coronal plane and was relocated in the osteotomy site as an intercalary graft to obtain a total of 40° correction. The proposed osteotomy was further simulated by means of obtaining 3D print outs and making rehearsals with available plate options. As a result, the intercalary osteotomy proved to have much better bone contact with stronger fixation and elimination of the cosmetic problem of prominent lateral condyle (Fig. 4a–c). To facilitate the resection of the desired wedge from desired location a patient specific 3D resection guide was designed and 3D printed. A tourniquet inflated to 280 mm/Hg pressure was used. The surgery started with a posterior longitudinal incision through which firstly ulnar nerve was explored and was found to be already anteriorly transposed. We strongly suggest the release and anterior transposition of the ulnar nerve in our intercalary technique since it would further stretch the ulnar nerve. After determining the status of the ulnar nerve the procedure carried on with a triceps sparing technique to expose osteotomy site. The sterilized patient specific osteotomy guide was used to make the osteotomies flawlessly and (Fig. 5a,b). The resulting wedge was flipped 180° degrees in coronal plane and used as an intercalary graft to obtain a total correction of 40°. After obtaining the one and only C-arm verification to prove everything was as planned, plate and screw fixation was performed to finish the procedure (Fig. 5c).
Fig. 1.
Preoperative photographs of the patient depicting his range of motion and deformity.
Fig. 2.
Preoperative AP x-ray of the case and superimposed images of injured and uninjured (mirrored) humerus to depict deformity.
Fig. 3.
(a and b) Graphics simulation and 3D print-out rehearsals for surgery if done with traditional method.
Fig. 4.
(a, b and c) Graphics simulation and 3D print-out rehearsals for surgery when done with our intercalary method.
Fig. 5.
(a and b) Photographs showing the osteotomy and resulting intercalary graft. (c) C-arm output showing temporary fixation of flipped intercalary grafting.
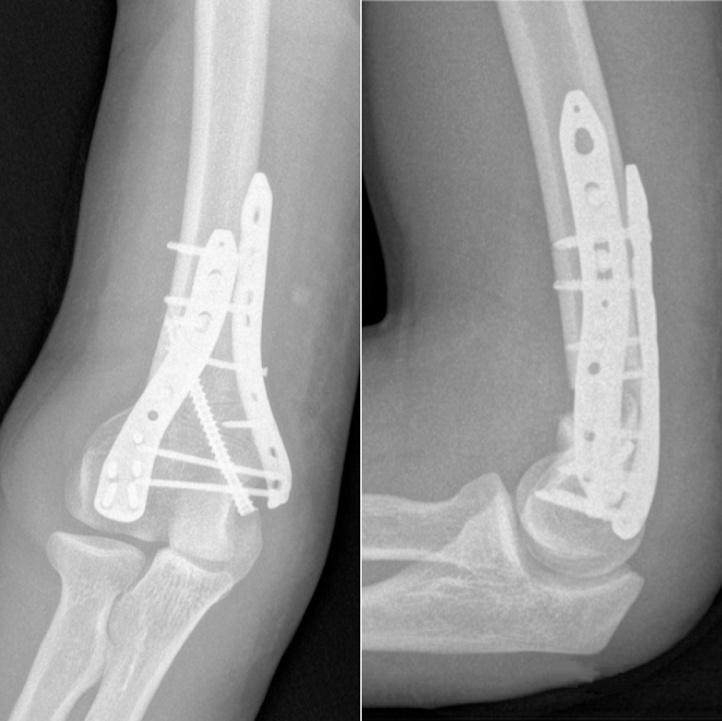
The postoperative x-ray of the patient showed perfect conformity of the plate and screw fixation with a very hard to see, faint osteotomy line perfectly matching the preoperative plans (Fig. 6). Knowing that the osteotomy had best possible bone contact and fixation the patient was encouraged to start joint mobilization and stretching exercises 1 week after the surgery with permission to use the arm for mild daily use. At 4th week he had no pain around the joint with only 5–10° of extension and flexion deficit and no lateral condylar prominence. His third month follow up revealed full range of motion with no pain and confirmation of osteotomy site union (Fig. 7).
Fig. 6.
Early postoperative x-rays showing the alignment, final fixation and barely visible osteotomy lines.
Fig. 7.
Postoperative photographs of the patient at 3 months after surgery showing restored range of motion and cosmetic results.
3. Discussion
Regular methods of deformity surgery rely on 2D surgical planning, heavy use of C-arm and surgical mastery if not luck. Thus, complications, such as implant failure, non-union, malalignment and residual deformity are not rare [3], [5]. Considering the burden of a failed surgery to a patient and the surgeon, 3D planning (both in software environment and with 3D printed models) and 3D printed patient specific osteotomy guides are very promising, offering shortened surgical time, flawless osteotomy, ideal fixation and probably overall much lower rate of complications [3], [4], [6]. Although at first glance our method of intercalary grafting osteotomy may seem to have disadvantages, especially of stability issues; we believe that 3D planning and use of patient specific osteotomy guides successfully overcomes this retro problem as this truly is a precision problem. Thus, we believe our method of osteotomy may be beneficial over other osteotomies such as step-cut and dome osteotomy since the planning procedure and the application of the osteotomy is much simpler.
4. Conclusion
We strongly believe that, with the recent dissemination of additive 3D printing technology, the 3D surgical planning and use of patient specific guides may soon become gold standard for all deformity management.
Conflicts of interest
The Authors declare that there is no conflict of interest.
Funding source
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Ethical approval
Not applicable. No research study involved.
Consent
The patient received a thorough explanation of this report gave his oral and written informed consent to be included in this report as well as for publication of these case, anonymous data, and pictures. A copy of the written consent is available for review on request.
Author contribution
Halil Can Gemalmaz: Study concept and design, patient’s surgical treatment, drafting the paper.
Kerim Sariyilmaz: Patient’s surgical treatment.
Okan Ozkunt, Mustafa Sungur and Ibrahim Kaya: Data analysis and discussion of data.
Fatih Dikici: Final approval of the version to be published.
Guarantor
The corresponding author is the guarantor of submission.
Contributor Information
Halil Can Gemalmaz, Email: cgemalmaz@gmail.com, cangemalmaz@hotmail.com.
Kerim Sarıyılmaz, Email: ksariyilmaz@gmail.com.
Okan Ozkunt, Email: drdeto@gmail.com.
Mustafa Sungur, Email: drmsungur@gmail.com.
İbrahim Kaya, Email: drikaya27@hotmail.com.
Fatih Dikici, Email: fatihdikici71@hotmail.com.
References
- 1.Davids J.R., Lamoreaux D.C., Booker R.C., Tanner S.L., Westerberry D.E. Translation step-cut osteotomy for treatment of post traumatic cubitus varus. J. Pediatr. Orthop. 2011;31(4):353e365. doi: 10.1097/BPO.0b013e31821723a6. [DOI] [PubMed] [Google Scholar]
- 2.Bauer A.S., Pham B., Lattanza L.L. Surgical correction of cubitus varus. J. Hand Surg. Am. 2016;41(3):447–452. doi: 10.1016/j.jhsa.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 3.Raney E.M., Thielen Z., Gregory S., Sobralske M. Complications of supracondylar osteotomies for cubitus varus. J. Pediatr. Orthop. 2012;32(3):232e240. doi: 10.1097/BPO.0b013e3182471d3f. [DOI] [PubMed] [Google Scholar]
- 4.Solfelt D.A., Hill B.W., Anderson C.P., Cole P.A. Supracondylar osteotomy for the treatment of cubitus varus in children: a systematic review. Bone Joint J. 2014;96-B(May (5)):691–700. doi: 10.1302/0301-620X.96B5.32296. [DOI] [PubMed] [Google Scholar]
- 5.Pannu G.S., Eberson C.P., Abzug J., Horn B.D., Bae D.S., Herman M. Common errors in the management of pediatric supracondylar humerus fractures and lateral condyle fractures. Instr. Course Lect. 2016;65:385–397. [PubMed] [Google Scholar]
- 6.Zhang Y., Lu S., Chen B., Zhao J., Liu R., Pei G.X. Application of computer-aided design osteotomy template for treatment of cubitus varus deformity in teenagers: a pilot study. J. Shoulder Elbow Surg. 2011;20(1):51e56. doi: 10.1016/j.jse.2010.08.029. [DOI] [PubMed] [Google Scholar]
- 7.Agha R.A., Fowler A.J., Saetta A., Barai I., Rajmohan S., Orgill D.P., the SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34:180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]