Abstract
We present two cases of daptomycin-induced eosinophilic pneumonia with characteristic chest x ray, CT scan and bronchoalveolar lavage (BAL) findings. It is not a commonly seen complication of Daptomycin but when it happens, it could cause a diagnostic and treatment dilemma. Patients could present acutely with hypoxic respiratory failure or a less dramatic chronic presentation is also possible. Our two patients presented with acute hypoxic respiratory failure and presentation resembles that of an infectious etiology. Diagnosis is confirmed by bronchoscopy with BAL in one of them and the other was treated empirically as the clinical and radiologic presentation was typical. Treatment includes removal of the offending agent, daptomycin. Corticosteroids are used if symptoms are severe and can result in rapid clinical improvement. There is no agreed upon dose and duration of steroids and we suggest a long taper of steroids for patients who present with severe symptoms and a short course steroid for patients with milder symptoms.
Eosinophilic pneumonia (EP) represents a spectrum of disease from a mild transient process to severe interstitial fibrosis. It is characterized by pulmonary infiltrates and increased numbers of eosinophils in Broncho-alveolar lavage (BAL) fluid, with or without increased levels of eosinophils in the peripheral blood [1], [2]. Several medications have been reported to cause eosinophilic pulmonary opacities and acute eosinophilic pneumonia. Nonsteroidal anti-inflammatory drugs and antibiotics are mainly implicated [3]. The pathophysiology of EP is not clearly known but it is hypothesized that it is related to T helper 2 lymphocytes recruitment by alveolar macrophages and release of interleukin 5 which promotes eosinophil production and migration to the lung. Production of a potent eosinophil chemoattractant by macrophages also is considered to have an effect on the pathophysiology [2], [4]. Daptomycin is an intravenous cyclic lipopeptide antibiotic with a spectrum of activity similar to vancomycin. It is FDA-approved for complicated skin, skin structure and blood stream infections caused by gram-positive organisms, including both methicillin-susceptible and resistant strains of Staphylococcus aureus, including patients with right-sided infective endocarditis [3], [5]. It was initially approved for skin and soft tissue infections and it is now being used to treat more serious infections involving the blood stream and the endocardium and is expected to be used more frequently. Eosinophilic pneumonia has been reported with daptomycin in post marketing in 2007 [6]. Daptomycin is distributed into lung tissue; however, it is inhibited by pulmonary surfactant and this daptomycin-surfactant interaction was also hypothesized to change the lipid integrity and induces an inflammatory response seen in daptomycin induced eosinophilic pneumonitis [4]. A case of eosinophilic pneumonia most likely associated with daptomycin was defined as meeting all of the following criteria, Concurrent exposure to daptomycin, Fever, Dyspnea with increased oxygen requirement or requiring mechanical ventilation, New infiltrates on chest x-ray or computed tomography scan, Bronchoalveolar lavage with >25% eosinophils, and Clinical improvement following daptomycin withdrawal [6].
It is not a common complication, but it requires prompt recognition since it can be associated with respiratory failure and potentially fatal outcome. As health professionals use this medication more frequently, daptomycin induced eosinophilic pneumonia is expected to increase in prevalence and physicians should have a high index of suspicion of the condition and treat it accordingly. We present two cases of daptomycin induced eosinophilic Pneumonitis.
1. Case 1
The first case is a 68-year-old white male, a retired welder, who was seen at infectious disease clinic when he was remaining with 2 more weeks of a 6 week course of Daptomycin/Rifampin. He had staphylococcus epidermidis septic arthritis and was placed on Vancomycin but developed significant renal toxicity and was placed on Daptomycin and Rifampin. The patient reported dry cough with occasional production of clear sputum, low grade fever but denied skin rash or joint swelling.
On examination vital signs were stable except for a low-grade fever of 100.3 and SPO2 of 89% that dropped down further to 84% upon ambulation. Fine basilar crackles were auscultated bilaterally but no murmurs, JVD or leg edema were observed.
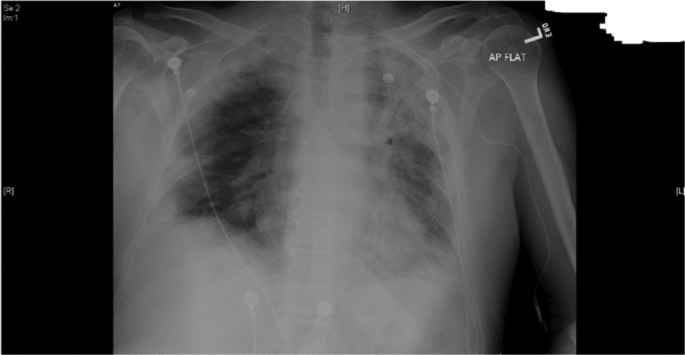
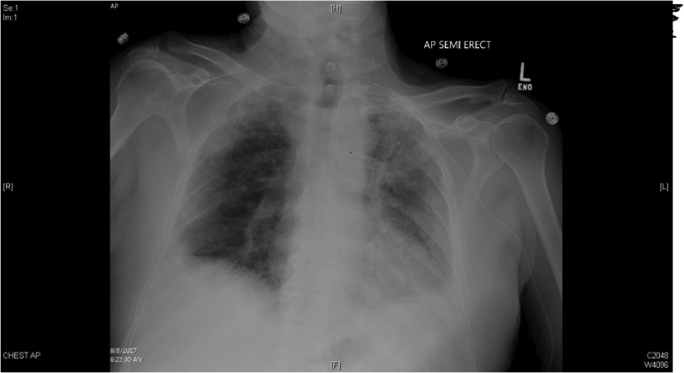
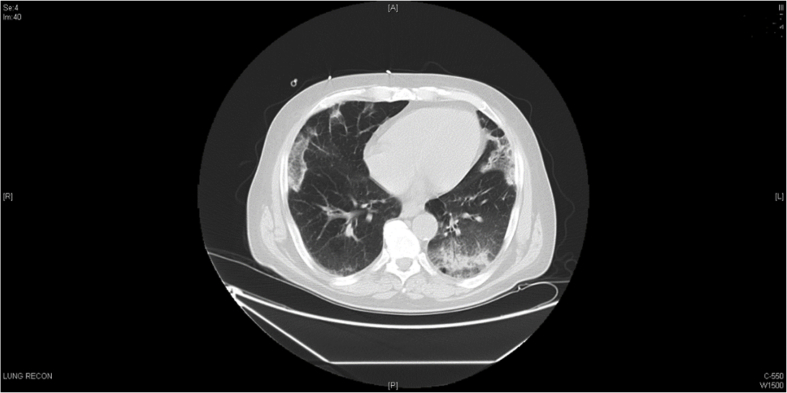
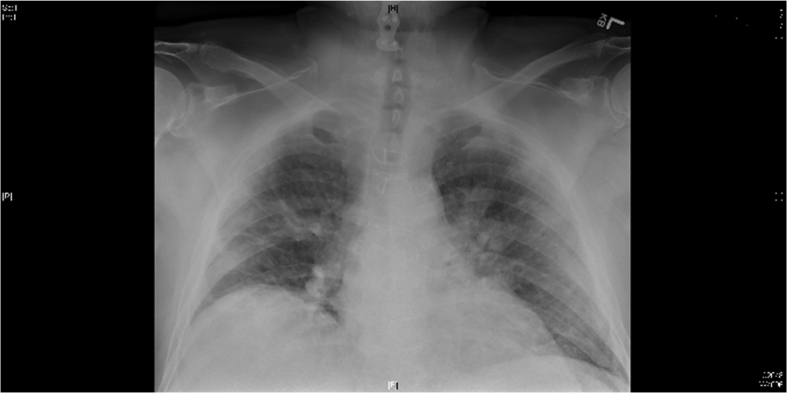
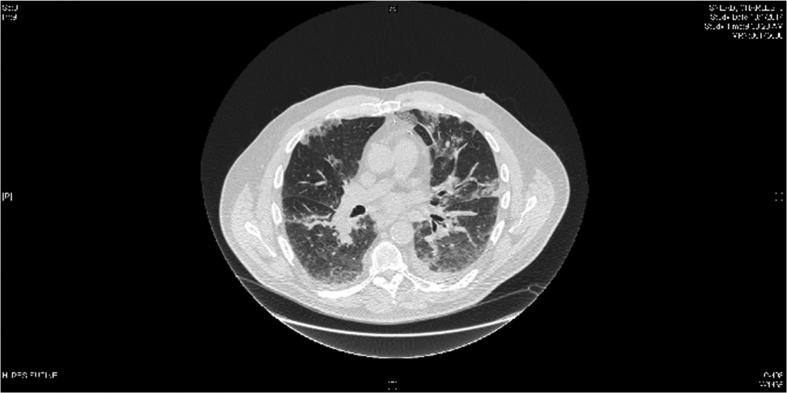
CXR showed bilateral ill-defined opacities more on the left side as shown in the x ray picture. High resolution CT scan showed interstitial and ground glass opacities.
Laboratory studies revealed WBC of 5700/mcl, with 11% of eosinophils, hemoglobin level of 9.9 g/dl, platelet count of 364,000/mcl and creatinine level of 1.63mg/dl. His CRP level was 34.1, ESR of 25 with a total CK level of 92. ABGs showed a PH of 7.51, PCO2 of 30 and PO2 of 63. He was admitted and placed on a high flow oxygen. Daptomycin-induced pneumonitis was suspected. Bronchoscopy was done with BAL showing 28% eosinophils. He was continued on steroids with significant improvement. He was discharged home with a long taper and less oxygen requirements. Reevaluation after 4 weeks showed significant improvement of dyspnea and no more need for supplemental oxygen.
CXR Before the treatment
CXR after the treatment
HRCT at admission
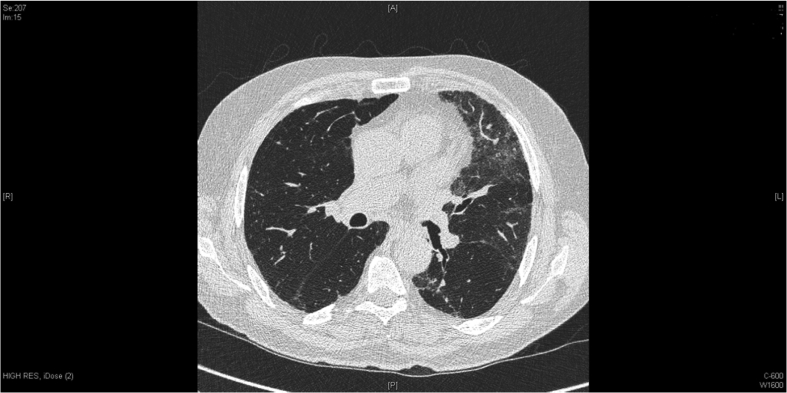
HRCT after 4 weeks on long prednisone taper.
2. Case 2
The second case is a 71-year-old male patient who was sent from another facility for evaluation of dyspnea, cough, fever and diaphoresis. He was discharged earlier on IV daptomycin to complete 6 weeks of treatment. Diagnosis of Health care associated pneumonia was entertained for which he was started on antibiotics along with Daptomycin. He required 2L of nasal cannula oxygen. Vital signs were stable except for a temperature 100 F. The SaO2 was 92% on 2L oxygen. He had decreased breath sounds in the lower lung field bilaterally with fine crackles. He had no raised JVP, murmurs, gallop or peripheral edema. Laboratory studies showed a WBC count of 6500/mcl with a 6.4% eosinophil, hemoglobin level of 9.6 g/dl, platelet count of 134,000/mcl and creatinine level of 1.28 mg/dl. Procalcitonin was 0.26 ng/ml and Chest HRCT revealed an upper lobe bilateral infiltrates. Daptomycin was stopped and patient was placed on steroids resulting in improvement of his symptoms and resolution of hypoxemia.
3. Discussion
In 2007, pulmonary eosinophilia was added to the Adverse Reactions, Post-Marketing Experience section of the Daptomycin product label. Since then, the Agency has reviewed published case reports of Daptomycin-associated eosinophilic pneumonia, and conducted a review of post-marketing adverse event reports from the FDA's Adverse Event Reporting System (AERS). FDA's review identified 7 definite, 13 probable and 38 possible cases of eosinophilic pneumonia between 2004 and 2010 that were most likely associated with Daptomycin as [3], [4] (see Table 1).
Table 1.
Criteria for inclusion as definite, probable, possible, and unlikely cases of daptomycin-induced eosinophilic pneumonia [6], [7].
| Definite | Probable | Possible | Unlikely |
|---|---|---|---|
| Concurrent exposure to daptomycin | Concurrent exposure to daptomycin | Concurrent exposure to daptomycin | All other cases that did not meet criteria |
| Dyspnea with increased oxygen requirement or requiring mechanical ventilation | Dyspnea with increased oxygen requirement or requiring mechanical ventilation | New infiltrates on CXR or CT | |
| New infiltrates on CXR or CT | New infiltrates on chest x-ray or CT | Clinical improvement following daptomycin withdrawal OR the patient died | |
| BAL with >25% eosinophils | BAL with ≤25% eosinophils OR peripheral eosinophilia | ||
| Clinical improvement following daptomycin withdrawal | Clinical improvement following daptomycin withdrawal | ||
| Fever |
Our first patient fits into class of a definite case of daptomycin induced EP and the second one into category of a probable case. In general, patients developed eosinophilic pneumonia 2 to 4 weeks after starting daptomycin. But it could come earlier than that [8], [9]. Our two patients presented to the hospital between the 3rd and 4th week after starting daptomycin and health care professionals should look for this complication any time after daptomycin is started.
According to literature, 87% of patients were Male and the mean age of patients is 65.4 a standard deviation of 15 years [2]. Old age and male sex are dominant risk factors for EP and that was observed in our 2 patients. It is shown in a review that the adverse effect does not appear to be dose dependent but time dependent exposure. Daptomycin dose and duration of administration were not significant risk factors for EP [2], [5]. The patients in our report are getting 6 and 8 mg/kg/dose every 24 hours and it is very difficult to reach to a conclusion on the relationship of dose, duration of antibiotics and side effect from the 2 patients in our review and this might need further study for better explanation.
Dyspnea was the most common documented symptom associated with eosinophilic pneumonia followed by the presence of either pulmonary infiltrates or opacities on chest x-ray or CT [2]. Both of our patients had dyspnea and pulmonary infiltrates on the CT, but EP patients might present with fever in the absence of respiratory symptoms [5], [10], [11]. EP may or may not be associated with peripheral blood eosinophilia, however pulmonary eosinophilic infiltrates or BAL eosinophilia are the corner stone for the diagnosis of EP. A lung biopsy can verify the diagnosis but is not always a requisite given a typical clinical appearance and consistent laboratory and radiographic findings [12], [13], [14].
Most patients with DIEP respond to discontinuation of the drug but some patients might have severe respiratory symptoms and might need treatment with steroids and respiratory assistance [2], [5]. In both of our patients we used steroids and the response is dramatic. Steroids act by programmed cell death and accelerating intracellular signaling resulting in death of eosinophils [2].
In the first patient we started him with methylprednisolone 60mg IV Q6H and that was changed to 40mg PO prednisolone daily and it was tapered in 4 weeks. In our second case, presentation was milder so we started the patient with 60mg IV methylprednisolone which was changed to 40mg PO prednisone to be continued for 5 days. Both patients were stable when they were seen after they finish their steroid treatment. Our 1st patient was needing up to 5 L of oxygen and was discharged with 3L but when he came back after a month, he was sent home without oxygen. Our second patient was needing 2L of oxygen and he was not needing any oxygen at discharge. Both clinical and radiologic improvement after the cessation of daptomycin administration and steroid treatment was dramatic.
4. Conclusion
Daptomycin is being used extensively by infectious disease specialists and ICU physicians. Its indications are being extended from time to time because of its excellent antimicrobial activity and coverage. Because of this, the relatively rare complication of DIEP is expected to rise significantly proportional to use of daptomycin. Life threatening respiratory failure can happen if the diagnosis is missed and appropriate treatment not instituted. Physicians should make themselves aware of this condition and properly treat these patients.
Contributor Information
Yonas Raru, Email: raru@marshall.edu.
Fuad Zeid, Email: zeid@marshall.edu.
Shannon Browning, Email: fudge1@marshall.edu.
Elizabeth Saunders, Email: saunde27@marshall.edu.
References
- 1.Kalogeropoulos A.S., Tsiodras S., Loverdos D. Eosinophilic pneumonia associated with daptomycin: a case report and a review of the literature. J. Med. Case Rep. 2011;5:13. doi: 10.1186/1752-1947-5-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Uppal Antimicrob. Resist. Infect. Control. 2016;5:55. doi: 10.1186/s13756-016-0158-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Murray and Nadel's Textbook of Respiratory Medicine, 68, 1221–1242.e13.
- 4.Silverman J.A., Mortin L.I., Vanpraagh A.D. Inhibition of daptomycin by pulmonary surfactant: in vitro modeling and clinical impact. J. Infect. Dis. 2005;191:2149–2152. doi: 10.1086/430352. [DOI] [PubMed] [Google Scholar]
- 5.Hirai J., Kinjo T., Hagihara M. Eosinophilic pneumonia caused by daptomycin: five case reports and review of the literature. Am. J. Respir. Crit. Care Med. 2016;193:A1586. American Thoracic Society 2016 International Conference, May 13–18, 2016; San Francisco,California. [Google Scholar]
- 6.6 US Food and Drug Administration. FDA drug safety communication: eosinophilic pneumonia associated with the use of Cubicin (daptomycin). http://www.fda.gov/Drugs/DrugSafety/ PostmarketDrugSafetyInformationforPatientsandProviders/ucm220273.htm. (Accessed 30 Nov 2016).
- 7.Kim P.W., Sorbello A.F., Wassel R.T. Eosinophilic pneumonia in patients treated with daptomycin: review of the literature and US FDA adverse event reporting system records. Drug Saf. 2012;35:447–457. doi: 10.2165/11597460-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Patel J.J., Atony A., Herrera M., Lipchik R.J. Daptomycin-induced acute eosinophilic pneumonia. WMJ. 2014;113:199–201. [PubMed] [Google Scholar]
- 9.Chiu S.Y., Faust A.C., Dand H.M. Daptomycin-induced eosinophilic pneumonia treated with intravenous corticosteroids. J. Pharm. Pract. 2015;28:275–279. doi: 10.1177/0897190014568678. [DOI] [PubMed] [Google Scholar]
- 10.Hagiya H., Hasegawa K., Asano K. Myopathy and eosinophilic pneumonia coincidentally induced by treatment with daptomycin. Intern Med. 2015;54:525–529. doi: 10.2169/internalmedicine.54.3397. [DOI] [PubMed] [Google Scholar]
- 11.Wojtaszczyk A., Jankowich M. Dyspnea on daptomycin: eosinophilic pneumonia. R. I. Med. J. 2015;98:41–43. [PubMed] [Google Scholar]
- 12.Yusuf E., Perrottet N., Orasch C. Daptomycin-associated eosinophilic pneumonia in Two patients with prosthetic joint infection. Surg. Infect. 2014;15:834–837. doi: 10.1089/sur.2013.200. [DOI] [PubMed] [Google Scholar]
- 13.Rajagopal A., Mintz E., Reese L. Daptomycin-induced eosinophilic pneumonia without Peripheral eosinophilia. Chest. 2014;145 (3_MeetingAbstracts):127A. CHEST World Congress 2014, March 21–24, 2014; Madrid, Spain. [Google Scholar]
- 14.Azam M., Asghar S., Aggen D. Acute eosinophilic pneumonia: a rare side effect of daptomycin. Chest. 2014;146 (4_Meeting Abstracts):179A. American College of Chest Physicians Annual Meeting October 25–30, 2014; Austin, Texas. [Google Scholar]