Abstract
This study assessed key test parameters and pass/fail criteria options for developing a respirator fit capability (RFC) test for half-mask air-purifying particulate respirators. Using a 25-subject test panel, benchmark RFC data were collected for 101 National Institute for Occupational Safety and Health-certified respirator models. These models were further grouped into 61 one-, two-, or three-size families. Fit testing was done using a PortaCount® Plus with N95-Companion accessory and an Occupational Safety and Health Administration-accepted quantitative fit test protocol. Three repeated tests (donnings) per subject/respirator model combination were performed. The panel passing rate (PPR) (number or percentage of the 25-subject panel achieving acceptable fit) was determined for each model using five different alternative criteria for determining acceptable fit.
When the 101 models are evaluated individually (i.e., not grouped by families), the percentages of models capable of fitting >75% (19/25 subjects) of the panel were 29% and 32% for subjects achieving a fit factor ≥100 for at least one of the first two donnings and at least one of three donnings, respectively. When the models are evaluated grouped into families and using >75% of panel subjects achieving a fit factor ≥100 for at least one of two donnings as the PPR pass/fail criterion, 48% of all models can pass. When >50% (13/25 subjects) of panel subjects was the PPR criterion, the percentage of passing models increased to 70%.
Testing respirators grouped into families and evaluating the first two donnings for each of two respirator sizes provided the best balance between meeting end user expectations and creating a performance bar for manufacturers. Specifying the test criterion for a subject obtaining acceptable fit as achieving a fit factor ≥100 on at least one out of the two donnings is reasonable because a majority of existing respirator families can achieve an PPR of >50% using this criterion. The different test criteria can be considered by standards development organizations when developing standards.
Keywords: Fit test, N95 respirator, NIOSH-certified respirator, respirator fit capability
Introduction
This article explores the development of new fit test criteria for air-purifying respirators (APR) which could be considered for adoption by Standards Development Organizations (SDO) or governmental respirator certification agencies where updated test requirements are needed. Air-purifying respirators are used by a wide variety of workers, from healthcare workers, who typically wear filtering facepiece respirators (FFR), to factory workers, who may use elastomeric half-mask (EHR) APRs. When respiratory protection is required in U.S. workplaces, the Occupational Safety and Health Administration (OSHA) requires the use of respirators certified by the National Institute for Occupational Safety and Health (NIOSH). Tight-fitting APRs must fit properly to provide their expected level of protection. Face seal leakage has been observed to be the dominant source of inward leakage for these types of devices.[1]
A fit test requirement for non-powered air-purifying particulate filtering respirators was not included in the 1995 update to the NIOSH certification regulation 42 Code of Federal Regulations (CFR) Part 84.[2] A fit test requirement for non-powered air-purifying particulate filtering respirators was included in the previous version of the certification regulation; however, NIOSH acknowledged in the preamble of the 1995 update that there was insufficient evidence to demonstrate that an isoamly acetate fit test or other fit tests accepted by the American National Standards Institute (ANSI) or OSHA could predict actual workplace protection provided to workers.[2] Since the 1995 regulation revision, a number of studies have been conducted to compare different fit test methods and assess characteristics associated with fit.[3–7] Numerous researchers and external organizations such as the National Academy of Medicine (formerly the Institute of Medicine) have urged NIOSH to resolve the remaining technical issues and move forward with a process to ensure that NIOSH-certified respirators are capable of fitting a specified percentage of intended user populations and users with a wide range of facial sizes.[8–11]
Since 2004, NIOSH has proposed new fit test standards utilizing human test subjects for evaluating the performance of half-mask particulate APRs. These proposed standards have utilized new fit test equipment and a more in-depth understanding of the factors affecting respirator fit, including new anthropometric surveys of face shapes and sizes.[12–14] More recently, an SDO, the American Society of Safety Engineers (ASSE), established a new subcommittee (ANSI Z88.15) to develop a national consensus standard for assessing respirator fit capability (RFC) of half-mask air-purifying particulate respirators. The scope of this effort is to define performance requirements that could be used as part of a conformity assessment program to ensure certified respirator models (or families of models in different sizes) are capable of fitting a specified percentage of the intended user population. The approach of developing respirator test requirements with the intent of using an SDO to finalize the standard was similarly used in Project BREATHE, led by the Veterans’ Health Administration and NIOSH, to develop a B95 respirator class to specifically address the needs of healthcare workers.[15,16]
This study was conducted to evaluate test method options (test parameters) and propose possible pass/fail criteria for a RFC test of half-mask air-purifying particulate respirators (filtering facepiece and half-mask). Panel passing rate (PPR) is defined as the percentage (or number) of subjects in a 25-subject panel that a respirator model or family of respirator models are capable of providing acceptable fit as defined by specific pass/fail criteria. The RFC test concept developed in this paper utilizes test panels of 25 subjects who performed multiple tests to evaluate respirator fit.
One key parameter for a successful RFC method involves the selection and use of a respirator fit test panel. Much research has been done in this area since 1995. Zhuang et al. developed two new respirator fit test panels based on a large scale NIOSH anthropometric survey of U.S. workers.[17] The NIOSH bivariate respirator fit test panel with 10 cells was defined based on face length and face width. A panel convened by the National Academy of Medicine concluded that the new panel was an improvement over the existing panels. The new panel has since been used in product investigation studies and was recommended as part of the proposed NIOSH B95 test requirements.[16,18,19]
A number of approaches have been taken to determine the subject sample size for a fit test panel, for example, BerryAnn used a 40-person panel in an N95 FFR product investigation, while the proposed B95 standard chose a 35-person panel.[16,19] Generally, increasing sample size will improve the accuracy of a fit test panel, but at the expense of increased costs. Achieving the appropriate balance is challenging. In one study, a binomial approach was used achieve this balance by estimating Type I and Type II error rates.[20] Type I error was defined as falsely passing a respirator which in truth achieved adequate fit for 100 × θ0% of the population. Type II error was defined as falsely failing a respirator model which achieved adequate fit for 100 × θ1% of the population. Studying three 35 person respirator fit test panels, Zhuang et al. found that inter-panel variability exists, but it is small relative to the other sources of variation in fit testing data.[21] Thus, a 25-person panel should provide sufficient inter-panel consistency, while being less burdensome to a test laboratory.
Another area where significant advances have been made since 1995 is in the area of fit test instrumentation. The TSI PortaCount (model 8020A) with N95-Companion accessory, as well as more recent PortaCount models, are now widely used for quantitative fit testing. For fit testing N95, N99, or P100 class filters, the N95-Companion accessory was designed to measure only negatively charged 40–60 nm size particles to effectively negate the influence of filter penetration.[22] Rengasamy et al. evaluated the performance of the PortaCount with N95-Companion and concluded that utilizing the N95-Companion accessory measured predominantly face seal leakage.[23] A study from Cho et al.[24] found that subjects obtaining fit factors (FF) ≥100 utilizing the N95-Companion accessory were able to achieve geometric mean workplace protection factors ranging from 18–154 for various biological contaminants, confirming the validity of using the TSI PortaCount with N95-Companion for respirator fit testing. Not surprisingly, many studies assessing fit performance as well as the proposed B95 test requirement used the TSI PortaCount with N95-Companion and chose a pass/fail criterion of FF ≥100 for individual fit tests.[8,16,19,25,26]
While the ability to define some RFC test parameters has been made easier based on the previously mentioned studies, some test parameters are harder to define based on being highly dependent upon the parameters discussed above (e.g., fit test panel type and size) or have rarely been studied. The number of donnings and how the individual FF results are used is important. Most studies incorporate multiple donnings to account for the donning-to-donning variation that occurs with human subject testing of respirator fit. While different options exist in the literature for deciding the pass/fail outcome for an individual fit test (e.g., requiring one of two fit tests to have a FF ≥100, or one of three fit tests to have a FF ≥100),[8,16,19,21] no studies have been done to assess the relative advantages of the various options or the impacts those advantages have on PPR. While the effect of changing the percentage of subjects passing the individual fit tests has been studied and an initial proposal was made by NIOSH during the Total Inward Leakage process (pass/fail criterion of ≥75%) and in the B95 proposed requirements (pass/fail criterion of ≥75%), this parameter is highly dependent upon other RFC parameters and needs to be studied after other test parameters are fixed.[16,20,21]
Finally, one issue that has not been studied previously, but will likely impact the PPR is the decision to test individual respirator models or respirator families of models that come in multiple sizes. In the respirator family approach, as long as one member (e.g., size) of the family results in a successful fit test outcome for an individual subject, it would be considered as passing for that individual; for example, if a subject passed an individual fit test in a medium size then testing on the small or large size (if available) would not be done. This approach was used in the proposed B95 test requirements and in at least one other research study.[8,16]
One challenge faced by SDOs in the development of an RFC test is the large number of inter-dependent test parameters (e.g., number of test subjects, number of donnings, etc.) and possible pass/fail criteria used to determine PPR (e.g., percent of subjects in the panel passing individual fit tests). Studies performed in the last decade have provided scientific justification for the number of test subjects in the fit test panel and instrumentation needed to perform RFC testing. However, other parameters still require additional studies in order to provide SDOs enough information to make informed decisions. Furthermore, the interactions between the test parameters can make decisions complicated. For example, minor changes in how the tests are conducted (e.g., number of donnings allowed or minimum FF to pass) can have a large impact on how many tests are needed to be performed to meet the PPR requirement. Test conditions and pass/fail criteria should be selected so that the conditions and criteria result in rejection of a high percentage of poor fitting respirators, while passing a high percentage of highly effective respirators. Implementing a standard of this kind will provide many advantages. For example, with higher fitting capability respirators, it should be easier for a potential wearer to obtain the OSHA required FF of 100 during a workplace fit test (for air-purifying FFRs and EHRs), which will save workers time and help employers be in compliance with OSHA regulations. Respirators with good fitting characteristics will also reduce assignment error and improve worker protection.
Methods
Subjects
This study was approved by the NIOSH Institutional Review Board. Subjects, both men and women, were recruited from the pool of subjects who periodically participate in NIOSH respirator certification fit testing; thus, subjects were experienced in wearing respirators. NIOSH employees were not used. Subjects were medically cleared as per the requirements of the approved protocol. All subjects in the pool were given an annual physical examination (which includes completing the OSHA Respirator Medical Evaluation Questionnaire and Clinical History and Exam Form) by a licensed physician. Exclusion criteria for the study included a history of uncontrolled chronic asthma, pneumonia, and high blood pressure. Individuals who chose to participate signed a consent form. Subjects were monetarily reimbursed on a per visit basis.
For each respirator model, a 25-subject fit test panel was randomly selected. An individual subject could be picked to test multiple models. The 25-subject fit test panel was based on the NIOSH bivariate respirator fit test panel that is divided into 10 cell categories.[17] In the current study, subject facial characteristics, including face length and face width, were measured to assign test subjects to the 10 cells. Each subject could be a member of only one panel cell, and at least two subjects for each cell are specified. The number of subjects sampled from each cell was then determined by matching the percentage of subjects in each cell to the distribution of the U.S. workforce as close as possible, as shown in Figure 1 and Table 1.
Figure 1.
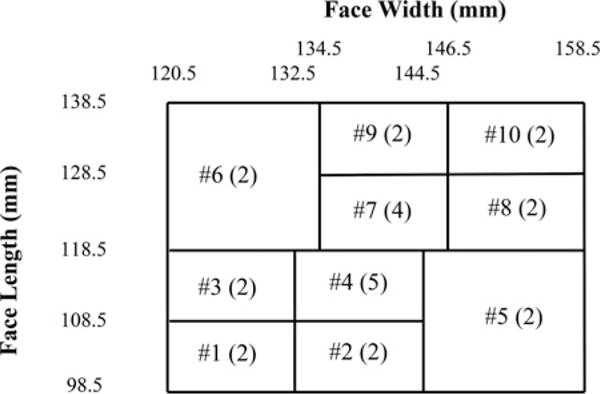
NIOSH panel based on face length and face width is shown. The cells are numbered 1–10 and the numbers in parentheses indicate the number of subjects sampled from each cell. When the subject’s face length or face width fall on the boundaries, the subject is classified into the higher number cell with greater face dimensions.
Table 1.
Calculated number of test subjects by test cell for a 25 subject test panel for a respirator designed to fit the entire population.a
| Cell Number | Percentage of Population (%) | Number of Subjects in Each Cell |
|---|---|---|
| 1 | 5.5 | 2 |
| 2 | 5.3 | 2 |
| 3 | 10.5 | 2 |
| 4 | 25.0 | 5 |
| 5 | 7.1 | 2 |
| 6 | 5.7 | 2 |
| 7 | 21.3 | 4 |
| 8 | 8.7 | 2 |
| 9 | 5.2 | 2 |
| 10 | 3.5 | 2 |
| Total | 97.7 | 25 |
Independent of the number of respirator sizes.
Respirators
The 101 models tested were 57 N95 FFRs, 43 EHRs, and one quarter-mask elastomeric respirator. These models were randomly selected from the list of NIOSH-certified models at the time of the study. Elastomeric respirators were equipped with N95, N99, or P100 filters, depending on what class of filter was available for each respirator approval. The respirators models (grouped as families) were available in three classifications: one-size-only, two sizes, or three sizes. There were a total of 61 families: 32 families of one-size-only FFRs, 3 families of one-size-only elastomeric respirators (2 half-mask and 1 quarter-mask), 11 families of 2- or 3-size FFR models, and 15 families of 2 or 3-size EHR.
Fit test methodology
The PortaCount (model: 8020A; TSI, Inc.; Shoreview, MN) and N-95 Companion Accessory (model: 8095; TSI, Inc.) were used for all fit tests. Each respirator was probed for measuring the concentration of aerosol particles inside the facepiece; a separate tube sampled the ambient air. For FFRs, a flush probe (having its sample inlet flush with the interior surface of the respirator facepiece) was inserted into the facepiece at the point of quadrilateral symmetry of the mouth and nose, i.e., midway between the nose and upper lip. For EHRs, the manufacturer’s specified test adapter was fitted between the facepiece and filter. Outside the facepiece, the PortaCount sampling tube was attached to the fitting from the exterior. Inside the facepiece, there was a sampling tube with one end attached to the fitting’s interior and the other end extended into the facepiece. A test adapter was also used to measure particle concertation inside the quarter-mask respirator.
The study used the OSHA ambient aerosol condensation nuclei counter (CNC) quantitative fit test protocol (described in Appendix A of 29 CFR 1910.134).[27] Each test subject was given training on the manufacturer’s donning and fitting procedures for each respirator model. Subjects were then asked to don the respirator, perform a user seal check in accordance with the manufacturer’s user instructions, wait 5 min to acclimate to wearing the respirator, and then perform a fit test. During an individual fit test, subjects conducted eight fit test exercises: normal breathing, deep breathing, turning head side to side, moving head up and down, talking (reciting the “rainbow passage”), grimacing, bending over (bending at the waist as if to touch the toes), and normal breathing. The overall FF (the harmonic average of the individual exercise FFs, excluding the grimace exercise) was calculated by the PortaCount.
Only one sample (i.e., a physical respirator) of each model was tested by each subject; the model was tested three times (i.e., one fit test for each of three sequential donnings). Following each donning, the subject rested for 2 min before the subsequent donning. The subjects were not told if they passed or failed the test nor were they shown the FF values. After each donning an FFR model, the subject removed the respirator and returned it to the test operator who then returned the head straps and/or noseband (if equipped) to their original positions as though the respirator where in its “as received” (new) condition from the manufacturer. For EHRs and the quarter-mask, the same readjustment procedures were performed by the test operator (as applicable to each model); however, because these were elastomeric models capable of being cleaned and reused, the facepieces were disinfected per the manufacturers’ instructions and the filters were replaced before being worn by other subjects.
All subjects (regardless of panel cell size) tested respirators manufactured with a one-size-only facepiece. For respirators manufactured in two unique sizes, subjects in panel cell sizes 1–5 (where 13 subjects are needed for panel cell requirements) tested the small/medium facepiece (or the smaller of the two facepieces) and subjects in panel cells 5–10 (12 subjects needed) tested the medium/large facepiece (or the larger of the two facepieces). If the subject achieved two failing FFs (i.e., FF <100) on the first two donnings of the assigned size, then the subject was allowed to test the alternative size facepiece in that respirator family.
For respirators manufactured in three unique sizes, subjects in panel cell sizes 1–3 (6 subjects needed) tested the small size facepiece, subjects in panel cells 4–7 tested the medium size facepiece (13 subjects need), and subjects in panel cell sizes 8–10 tested the large size (6 subjects needed). If the subject achieved two failing FFs (i.e., FF <100) on the first two donnings of the assigned size, then the subject was allowed to test the alternative size facepiece in that respirator family. Subjects in cells 1–3 who failed the small size were only allowed to test the medium size. Subjects in cells 4–5 who failed the medium size were only allowed to test the small size. Subjects in cells 6–7 who failed the medium size were only allowed to test the large size. Subjects in cells 8–10 who failed the large size were only allowed to test the medium size.
For two and three size families, some subjects may not have tested both applicable respirator sizes; thus, in the case of a subject not being able to pass a fit test on the first two donnings of the originally assigned respirator size and if the same subject did not test the alternative size, then data from another subject of the same cell size who tested the alternative respirator size were used as replacement for the original subject’s missing data for that size. Using this replacement method, some two and three size families have more than 25 subjects who actually performed testing; however, using this data replacement method, all data analyzed for these families have only 25 sets of the maximum possible test trials (i.e., 25 sets of the allowable test trials for a 25-subject panel for a family).
Data analysis
Respirator testing resulted in a total of 7,575 FF values for analysis (101 models × 25 subjects per model × 3 donnings per subject/model combination). For the current study, 5 different criteria for determining acceptable respirator fit were used to determine the percentages of the 101 models which could meet the specified test criterion for a designated PPR of the 25-subject panel (for example, PPR >75% or PPR >50%).
Criterion 1
Achieve a harmonic mean FF of ≥ 100 using three donnings. The harmonic mean fit factor is the reciprocal of the arithmetic mean of the reciprocals of the three fit factors. (Equation (1)):
| (1) |
where FFHM = harmonic mean fit factor.
FF1 …3 = individual fit factors achieved on each of three donnings.
Criterion 2
Achieve a FF ≥100 for both of the first two donnings. In this method, only the first two donnings were evaluated. For acceptable fit, the subject needed to achieve a FF ≥100 on both donnings.
Criterion 3
Achieve FF ≥100 on the first donning only; the second and third donnings are not considered in this method.
Criterion 4
Achieve FF ≥100 on at least one of the first two donnings. In this method, only the first two donnings were evaluated. For acceptable fit, the subject needed to achieve a FF ≥100 on at least one of the first two donnings.
Criterion 5
Achieve a FF ≥100 on at least one of three donnings. In this method, all three donnings were evaluated. For acceptable fit, the subject needed to achieve a FF ≥100 on at least one of the three donnings.
Criterion 1 was originally proposed as a method for determining pass/fail status for a test subject in the 2009 Federal Register Proposed Rule on TIL.[13] Because each subject performed three donnings in our current study, we had to opportunity to evaluate the data using one, two, or three donnings and thus developed Criteria 2–5. It was necessary to develop several methods in order to assess their relative strengths and weaknesses in terms of the percentages of models which could meet each of them.
For further analysis, FF data from all 101 models were grouped into individual families, resulting in 61 families total (35 one-size-only families and 26 two- or three-size families). For each family, data from 25 subjects were pooled for all respirator sizes within that family. For 1-size families, there was only one model for each family. Criterion 4 was used to determine the percentages of family groupings which could achieve acceptable fit at different PPR levels. In the case of evaluating all 61 families combined (which includes all 101 models), if a multiple size family met the pass/fail requirement of Criterion 4, then all of the models in that family were considered to have achieved acceptable fit, even if one or more sizes of that family did not met the criteria when evaluated on an individual model basis; thus, using this method to evaluate all 61 families combined has the effect of passing a greater number of models compared to evaluating the 101 models individually. The rationale for evaluating all 61 families combined in this way is that it does not penalize individual model sizes for failing when tested individually. Its implication is that users in the workplace can select a different model size of a particular family if one model size does not fit them.
Results
Comparing Criterion 1 and 2, 13% and 10% of the 101 individual respirator models were capable of a PPR >75% of the 25 member fit test panel (19/25 subjects), respectively. Alternatively, 35% and 31% of the 101 individual respirator models, respectively for Criterion 1 and 2, were capable of aPPR >50% of the 25 member fit test panel (13/25 subjects) (Figure 2). The percentages of the 101 models capable of a PPR >75% of the panel (19/25 subjects) were 19%, 29%, and 32% for Criterion 3, 4, and 5, respectively. When easing the passing level to a PPR of >50% of the panel (13/25 subjects), 40%, 55%, and 58% of the 101 models could exceed the PPR for Criterion 3, 4, and 5, respectively (Figure 2). The results of Criteria 1– 5 for the 101 models meeting PPR >75% and >50% of panel subjects are summarized in Table 2. Criteria 1, 2, and 3 may be too challenging for many manufacturers to meet and therefore less attractive candidates as methods. For the fourth and fifth options (Criterion 4, achieving at least one out of two donnings with FF ≥100; and Criterion 5, achieving at least one out of three donnings with FF ≥100), 55% and 58% of the 101 individual respirator models were capable of a PPR >50% of the 25-subject panel, respectively. Either of these two criteria can be considered to determine if the PPR required by the RFC test is achieved; however, because the method of passing at least one of two repeated donnings is more economical (i.e., takes less time) than performing three repeated donnings, the method of passing at least one of two tests, Criterion 4, is preferred.
Figure 2.
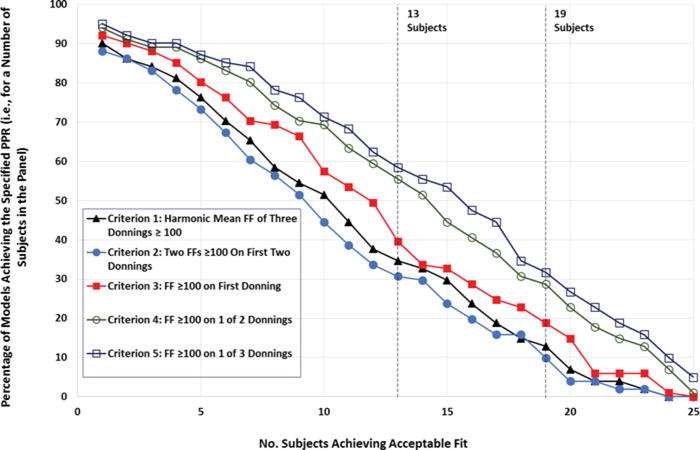
Percentages of 101 respirator models achieving acceptable fit for a given number of test subjects for Criteria 1–5. Note: Analysis performed as individual models (i.e., models were not grouped as families for this analysis).
Table 2.
Percentage of 101 respirator models meeting the specified RFC criteria using five different evaluation methods for acceptable fit.a
| Percentage of 101 Models Meeting the Specified PPR (%)
|
||
|---|---|---|
| Criteria for Determining Acceptable Fit | 19 of 25 Subjects Passing (PPR >75%) | 13 of 25 Subjects Passing (PPR >50%) |
| Criterion 1: Achieve Harmonic Mean FF ≥100 for Three Donnings |
13 | 35 |
| Criterion 2: Achieve Two FFs ≥100 On First Two Donnings |
10 | 31 |
| Criterion 3: Achieve FF ≥100 On First Donning |
19 | 40 |
| Criterion 4: Achieve FF ≥100 On At Least One of First Two Donnings |
29 | 55 |
| Criterion 5: Achieve FF ≥100 On At Least One of Three Donnings |
32 | 58 |
Analysis performed as individual models (i.e., models were not grouped as families for this analysis).
The families grouping approach was used with Criterion 4 (Figure 3). When >75% of panel subjects (19/25 subjects) was used as the PPR, 48% of all 61 families (including 6% of one-size-only FFR families, 36% of two or three size FFR families, and 87% of two or three size EHR families) could pass (Table 3). When a PPR >50% (13/25 subjects) of panel subjects was evaluated, the number of passing respirator families increased to 70% (including 34% of one-size-only FFR families, 73% of two or three size FFR families, and 100% of two or three size EHR families). It should be noted that PPRs were higher for 2- and 3-size families than for the 1-size family. The relationship between passing rates of one-size family respirators by groups of cells (i.e., passing rate of subjects in cells 1–3 vs. cells 4–7) was not examined because PPR is specifically defined as the overall percentage of passing subjects in the panel. The data series “All 61 Families” represents all 101 respirator models. For 2- or 3-size families, when an individual family met the pass/fail criterion, then all model sizes of that family were considered to meet that criterion; the data series “All 61 Families” is plotted to reflect the passing percentages of the 101 models calculated this way.
Figure 3.
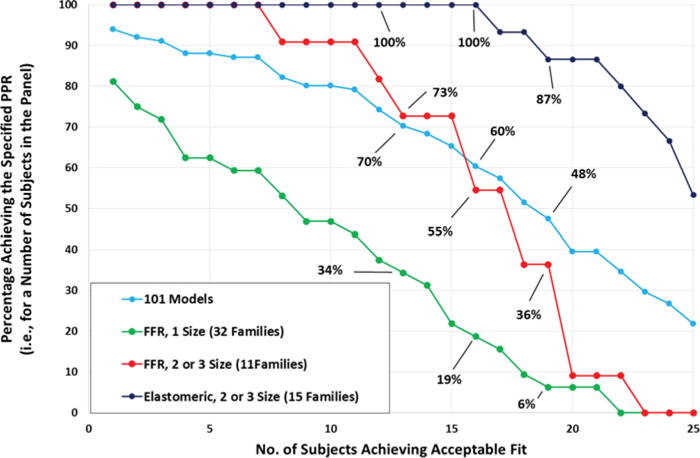
Percentages of respirator families achieving the specified PPR (i.e., for a number of subjects in the panel) using Criterion 4 (achieving FF ≥100 on at least one of two donnings). Note: The “All 61 Families” data series represents the 101 models. For this data series only, if at least one model size of a multiple size family met Criterion 4, then all model sizes in that family were considered to have passed.
Table 3.
Percentage of respirator families meeting the specified PPR.
| PPR (%)a | Percentage of Families that Meet the Specified PPR (%)
|
|||
|---|---|---|---|---|
| All 61 Families (101 models)b | 1-size FFR (32 families) | 2 or 3-size FFR (11 families) | 2 or 3-size EHR (15 families) | |
| > 75% | 48 | 6 | 36 | 87 |
| > 64% | 60 | 19 | 55 | 100 |
| > 50% | 70 | 34 | 73 | 100 |
Percentage of a subjects in a 25-subject panel meeting Criterion 4 (obtaining FF ≥100 on at least one on the first two donnings).
The “All 61 Families” data represents the 101 models. For this data column only, if at least one model size of a multiple size family met Criterion 4, then all model sizes in that family were considered to have passed.
Discussion
Five different criteria were applied to determine the number of donnings and how to use the individual FF data in determining an appropriate PPR to define a RFC test requirement. For the Criterion 4 analysis (evaluating the PPR percentages for obtaining FF ≥100 on at least one of two donnings), when >75% and >50% of panel subjects (19 and 13 subjects) were chosen as the required PPR, 29% and 55% of the 101 models (evaluated on an individual model basis) and 48% and 70% of the models (evaluated by grouping into families) met the requirement. These results suggest that setting the PPR requirement initially at >50% (13 subjects) is attainable and that using the families grouping approach can allow for a higher percentage of models meeting the requirement as opposed to using the individual models approach. The use of a respirator family mirrors a recommended approach for employers when implementing a respiratory protection program.[8] In that procedure, subjects (or workers) are initially tested with a medium/regular size respirator and then, if there is a failure, tested with a different size of the same brand (or model).
Pass/fail criteria used to determine PPRs for RFC tests of half-mask respirators should be set stringent enough to meet end user expectations, but not so challenging that the criteria create too great of a barrier for manufacturers to produce qualified respirators.[16] An SDO using the RFC concept in its standard could choose to initially use >50% as the acceptable PPR threshold for passing and then increase the criterion gradually over time as technology improves. Using either a >50% or >75% PPR requirement still falls short of the “ideal” respirator to fit ∼90% of U.S. healthcare workers as reported by the Project BREATHE working group,[15] but would greatly benefit employers who must find respirators that fit all employees in a respiratory protection program.
One concern raised by manufacturers with the use of respirator fit test panels has been the variability between different anthropometric panels. Two recent NIOSH papers addressed this concern.[21,28] The geometric mean (GM) inward leakage (IL) (combined leakage through the filter element and leaks across the face sealing area) values for all 10 studied respirators were not significantly different among the three randomly selected 35 subject panels. Passing rate was not significantly different among the three panels for all respirators combined or by each model. This was true for all IL pass/fail levels of 1%, 2%, and 5%. Using 26 or more subjects to pass the IL test, all three panels had consistent passing/failing results for pass/fail levels of 1% and 5%. Some disagreement was observed for the 2% pass/fail level. Inter-panel variability exists, but it is small relative to the other sources of variation in fit testing data. The percentage of the subjects meeting the pass/fail criteria of an RFC test (i.e., the PPR) is expected to be similar to the percentage of workers passing OSHA fit test in the workplaces because of the small inter-panel variability and the same test protocol used in the RFC test and OSHA fit test.
The data analyzed in this manuscript were initially collected in the 2004–2005 timeframe and the respirator models on the market today may have better or decreased fit performance. However, the focus of this article is on the evaluation of test method parameters and different pass/fail criteria which does not require current respirator models to assess. While only 101 models out of the many respirator models approved by NIOSH in the United States were included, the data do provide a representative subset for analysis. In addition, our analysis of the fit capability of one-size respirator families only examined PPR of subjects across all cells. Fit capability of a one-size respirator for someone in cells 4–7 may differ from someone in cells 1–3 or 8–10 if analyzed by grouping cells. For example, if the acceptable PPR is 50% when evaluated by a given criterion, a 1-size respirator may have >50% of subjects in cells 1–3 and 4–7 pass but <50% pass in cells 8–10. Overall the passing rate may be greater than 50% and therefore exceed the PPR requirements of the RFC test. However, it would fail a RFC test that requires >50% of subjects in each of the three groups of cells to pass. It may be restricting to manufacturers to require a new one-size respirator to exceed the 50% passing level in every group of cells. It may be possible for a manufacturer to design a one-size respirator to fit smaller face sizes better or to fit larger faces better and obtain an acceptable PPR for the entire subject panel. Therefore, respirator performance was only evaluated by the overall PPR. Similar to many workplaces, the fit testing was done in an open setting using the PortaCount model 8020A with N95-Companion. However, similar results would have been obtained had the testing been done inside a test chamber, using another validated method for quantitative fit testing using a generated aerosol, or with a newer PortaCount model.
Conclusions
For the RFC concept described here, the data suggest that respirators should be tested as a family using two donnings, allowing for testing two respirator sizes for two-size and three-size families, and using a panel of 25 subjects per the bivariate panel. Specifying a PPR pass/fail criterion that a subject achieve a FF ≥100 for at least one of two donnings is reasonable because nearly half (48%) of existing respirator models can meet this pass/fail criterion for >75% (19/25) of subjects using a 25-subject test panel. A majority (70%) of models can meet the pass/fail criterion when the criterion is reduced to >50% (13/25) of subjects. The methods presented here can be considered by SDOs when developing RFC test requirements.
Acknowledgments
The authors would like to thank NIOSH colleagues who reviewed draft versions of this manuscript and Bill Newcomb who served as the project officer during the time this data was collected.
Footnotes
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the National Institute for Occupational Safety and Health. Mention of commercial product or trade name does not constitute endorsement by the National Institute for Occupational Safety and Health.
References
- 1.Grinshpun SA, Haruta H, Eninger RM, Reponen T, McKay RT, Lee SA. Performance of an N95 filtering facepiece particulate respirator and a surgical mask during human breathing: two pathways for particle penetration. J Occup Environ Hyg. 2009;6(10):593–603. doi: 10.1080/15459620903120086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Respiratory Protective Devices. Code of Federal Regulations. 1995:30336–30404. Title 42, Part 84. [Google Scholar]
- 3.Coffey CC, Campbell DL, Myers WR, Zhuang Z, Das S. Comparison of six respirator fit test methods with an actual measurement of exposure in a simulated health care environment: Part I - Protocol development. Am Ind Hyg Assoc J. 1998;59(12):852–861. doi: 10.1080/15428119891011027. [DOI] [PubMed] [Google Scholar]
- 4.Coffey CC, Campbell DL, Myers WR, Zhuang Z. Comparison of six respirator fit test methods with an actual measurement of exposure in a simulated health care environment: Part II - Method comparison testing. Am Ind Hyg Assoc J. 1998;59(12):862–870. doi: 10.1080/15428119891011036. [DOI] [PubMed] [Google Scholar]
- 5.Zhuang Z, Coffey CC, Jensen PA, Campbell DL, Lawrence RB, Myers WR. Correlation between quantitative fit factors and workplace protection factors measured in actual workplace environments at a steel foundry. Am Ind Hyg Assoc J. 2003;64(6):730–738. doi: 10.1202/475.1. [DOI] [PubMed] [Google Scholar]
- 6.Zhuang Z, Coffey CC, BerryAnn R. The effect of subject characteristics and respirator features on respirator fit. J Occup Environ Hyg. 2005;2(12):641–649. doi: 10.1080/15459620500391668. [DOI] [PubMed] [Google Scholar]
- 7.Roberge RJ, Zhuang Z, Stein LM. Association of body mass index with facial dimensions for defining respirator fit test panels. J Int Soc Resp Protect. 2006;23:44–52. [Google Scholar]
- 8.Lee K, Slavcev A, Nicas M. Respiratory protection against Mycobacterium tuberculosis: Quantitative fit test outcomes for five Type N95 filtering facepiece respirators. J Occup Environ Hyg. 2004;1(1):22–28. doi: 10.1080/15459620490250026. [DOI] [PubMed] [Google Scholar]
- 9.Larson EL, Liverman CT, editors. Institute of Medicine. Preventing Transmission of Pandemic Influenza and Other Viral Respiratory Diseases: Personal Protective Equipment for Healthcare Workers: Update 2010. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 10.Lofgren D. A Must For NIOSH: Certify fit performance of the half-mask particulate respirator. J Occup Environ Hyg. 2012;9(12):D191–195. doi: 10.1080/15459624.2012.733578. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Certifying Personal Protective Technologies: Improving Worker Safety. Washington, DC: The National Academies Press; 2011. [PubMed] [Google Scholar]
- 12.NIOSH. Program Concept for Total Inward Leakage (TIL) Performance Requirements and Test Methods. Available at http://www.cdc.gov/niosh/npptl/standardsdev/til/ (accessed August 4, 2016)
- 13.National Institute for Occupational Safety and Health (NIOSH) Total Inward Leakage Requirements for Respirators. Available at: https://www.federalregister.gov/articles/2009/10/30/E9-26008/total-inward-leakage-requirements-for-respirators”(2009) (accessed August 4, 2016)
- 14.National Institute for Occupational Safety and Health (NIOSH) Development of Inward Leakage Standards for Half-Mask Air-Purifying Particulate Respirators. Available at: https://www.federalregister.gov/articles/20-13/11/19/2013-27445/development-of-inward-leakage-standards-for-half-mask-air-purifying-particulate-respirators(2013) (accessed August 4, 2016)
- 15.Gosch ME, Shaffer RE, Eagan AE, Roberge RJ, Davey VJ, Radonovich LJ., Jr B95: a new respirator for health care personnel. Am J Infect Contr. 2013;41(12):1224–1230. doi: 10.1016/j.ajic.2013.03.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shaffer R, Zhuang Z, Bergman M, et al. Recommended requirements, test methods, and pass/fail criteria for a “B95” respirator for healthcare workers. J Int Soc Resp Protect. 2014;13(1):23–42. [Google Scholar]
- 17.Zhuang Z, Bradtmiller B, Shaffer RE. New respirator fit test panels representing the current US civilian work force. J Occup Environ Hyg. 2007;4(9):647–659. doi: 10.1080/15459620701497538. [DOI] [PubMed] [Google Scholar]
- 18.Institute of Medicine. Assessment of the NIOSH Head-and-Face Anthropometric Survey of US Respirator Users. Washington, DC: The National Academies Press; 2007. [Google Scholar]
- 19.U.S Department of Health and Human Service. NIOSH Investigation of 3M Model 8000 Filtering Facepiece Respirators As Requested By The California Occupational Safety and Health Administration, Division of Occupational Safety and Health (Health Hazard Evaluation Report, HETA 2010-0044-3109) Oakland, CA: National Institute for Occupational Safety and Health and California Occupational Safety and Health Administration, Division of Occupational Safety and Health; 2010. [Google Scholar]
- 20.Landsittel D, Zhuang Z, Newcomb W, BerryAnn R. Determining sample size and a passing criterion for respirator fit test panels. J Occup Environ Hyg. 2014;11(2):77–84. doi: 10.1080/15459624.2013.843780. [DOI] [PubMed] [Google Scholar]
- 21.Zhuang Z, Liu Y, Coffey CC, Miller C, Szalajda J. Inward leakage variability between respirator fit test panels - Part I. Deterministic approach. J Occup Environ Hyg. 2015;12(11):753–760. doi: 10.1080/15459624.2015.1047025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Han HS, Holm R, Prell M, Remiarz R. Penetration of N95 filtering facepiece respirators by charged and charge-neutralized nanoparticles. J Int Soc Resp Protect. 2012;29(2):75–81. [Google Scholar]
- 23.Rengasamy S, Eimer BC, Shaffer RE. Evaluation of the performance of the N95-companion: effects of filter penetration and comparison with other aerosol instruments. J Occup Environ Hyg. 2012;9(7):417–426. doi: 10.1080/15459624.2012.685838. [DOI] [PubMed] [Google Scholar]
- 24.Cho KJ, Reponen T, McKay R, et al. Comparison of workplace protection factors for different biological contaminants. J Occup Environ Hyg. 2011;8(7):417–425. doi: 10.1080/15459624.2011.585094. [DOI] [PubMed] [Google Scholar]
- 25.Yu Y, Jiang L, Zhuang Z, et al. Fitting characteristics of N95 filtering facepiece respirators used widely in China. PLoS One. 2014;9(1):e85299. doi: 10.1371/journal.pone.0085299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Richardson A, Hofacre K, Weed J, Holm R, Remiarz R. Evaluation of a faster fit testing method for filtering facepiece respirators based on the TSI PortaCount. J Int Soc Resp Protect. 2014;31(1):43–56. [Google Scholar]
- 27.Respiratory Protection: Final Rule. Federal Register. 1998 Jan 8;63:1152–1300. [PubMed] [Google Scholar]
- 28.Liu J, Zhuang Z, Coffey C, Rengasamy S, Niezgoda G. Inward leakage variability between respirator fit test panels – Part II. Probabilistic approach. J Occup Environ Hyg. 2016;13(8):604–611. doi: 10.1080/15459624.2016.1161198. [DOI] [PubMed] [Google Scholar]


