Abstract
Fears of food are common in individuals with eating disorders and contribute to the high relapse rates. However, it is unknown how fears of food contribute to eating disorder symptoms across time, potentially contributing to an increased likelihood of relapse. Participants diagnosed with an eating disorder (N = 168) who had recently completed intensive treatment were assessed after discharge and one month later regarding fear of food, eating disorder symptoms, anxiety sensitivity, and negative affect. Cross lagged path analysis was utilized to determine if fear of food predicted subsequent eating disorder symptoms one month later. Fear of food—specifically, anxiety about eating and feared concerns about eating—predicted drive for thinness, a core symptom domain of eating disorders. These relationships held while accounting for anxiety sensitivity and negative affect. There is a specific, direct relationship between anxiety about eating and feared concerns about eating and drive for thinness. Future research should test if interventions designed to target fear of food can decrease drive for thinness and thereby prevent relapse.
Keywords: eating disorders, anorexia nervosa, fear of food, anxiety
Eating disorders (EDs) are serious mental illnesses that cause extreme suffering and carry an increased risk of mortality (Klump, Bulik, Kaye, Treasure, & Tyson, 2009). Individuals diagnosed with EDs have high rates of comorbid anxiety disorders, with rates estimated up to 80% (Pallister & Waller, 2008). Even without a comorbid anxiety disorder, individuals with EDs are highly anxious, with much of their anxiety centered around food, eating, and appearance-related concerns (Halmi, 2007).
Recent research has begun to explore food-related anxieties and fears that are common in EDs in more depth. Specifically, researchers have identified fear of food as a particular type of anxiety that is common in the eating disorders (Levinson & Byrne, 2015). It was found that three cognitive-behavioral aspects of fear of food (i.e., anxiety about eating, food avoidance behaviors, and feared concerns related to eating) were significantly higher in individuals diagnosed with an ED versus healthy controls. Further, each of these three cognitive-behavioral aspects of fear of food decreased across a four-session exposure intervention, suggesting that exposure therapy may be an efficacious approach to treat these fears. Anxiety occurring within the context of eating disorders is a focus of recent treatment advances, with researchers finding that exposure and response prevention therapy for anorexia nervosa is successful at increasing food intake and weight gain (Levinson et al., 2015; Steinglass et al., 2012). However, it is still unknown how fears that may be addressed in exposure therapy impact eating disorder symptoms, though it seems clear that such fears are an important treatment target.
The period immediately after discharge from intensive treatment centers may be a critical time to address these fears. Individuals with eating disorders continue to struggle with fears of food after discharge from intensive treatment, with research finding that individuals with anorexia nervosa (AN) continue to exhibit difficulty eating, consuming fewer calories than healthy controls (Mayer, Schebendach, Bodell, Shingleton, & Walsh, 2012). Given that difficulty adhering to a meal plan is associated with poor treatment outcomes (McFarlane, Olmsted, & Trottier, 2008), it seems likely that the high rates of relapse in the eating disorders are influenced by a failure to maintain or gain weight in outpatient settings (Kaplan et al., 2009), which may be influenced by fears of food. This research highlights the importance of understanding how fears of food impact eating disorder symptoms, especially after discharge from intensive treatment.
In particular, it seems worthwhile to examine eating disorder symptoms related to a consistent desire to maintain a low weight, such as drive for thinness. Drive for thinness is characteristic of individuals who have a high fear of weight gain and consequently diet to prevent it, such as those with AN and BN (Chernyak & Lowe, 2010; Penas-Lledo, Bulik, Lichtenstein, Larsson, & Baker, 2015). Ramacciotti and colleagues (2002) found that individuals with AN or BN with a low drive for thinness reported less severe eating disorder-related psychopathology than those with a high drive for thinness, highlighting how drive for thinness may be an indicator of future relapses. Further, drive for thinness is associated with intentional weight loss and disordered eating patterns (e.g., restrictive eating; Keski-Rahkonen et al., 2005). It seems likely that fear of food may be specifically associated with drive for thinness (versus other symptoms such as bulimia and body dissatisfaction), as individuals may feel anxious about eating to avoid their fear of gaining weight, and that this fear may be heightened in the period after discharge from treatment. However, to the best of our knowledge, the relationship between fear of food and drive for thinness has not been examined in prospective data. Furthermore, it is unclear if there is a specific relationship between fear related to food and drive for thinness, or if general anxiety not focused on food might account for such a relationship. If we identify that fear of food specifically impacts the desire to lose weight over time, we may be able to develop treatments targeted to this specific type of anxiety (e.g., fear of food) with the ultimate goals of reducing anxiety, increasing caloric intake to stabilize a healthy weight, and preventing relapse.
In the current study, we surveyed a sample of individuals diagnosed with an eating disorder and recently discharged from a residential or partial hospital program. We assessed fears of food after discharge and then one month later. We hypothesized that the three cognitive-behavioral components of fear of food (i.e., anxiety about eating [emotions], feared concerns related to eating [thoughts], and food avoidance behaviors [behaviors]) would predict later eating disorder symptoms, specifically symptoms related to the desire to be thin (but not to bulimia symptoms and body dissatisfaction), given that is the eating disorder symptom directly related to fears of gaining weight. We also hypothesized that these relationships would not be accounted for by general anxiety, negative affect, and eating- or weight-related concerns, but rather, fear specific to food would be a primary driver behind eating disorder symptoms.
Methods
Procedure
All procedures were approved by the Washington University Institutional Review Board. Participants were recruited from a research database from an eating disorder clinic in the Midwest. All participants had recently discharged from either a partial hospital or residential program for eating disorders. Participants completed online measures of eating disorder symptoms, anxiety, and fear of food at two time points, each one month apart (i.e., Time 1 and Time 2).
Participants
Participants were 168 individuals recently discharged from intensive eating disorder treatment. Participants had all recently been discharged from a residential or partial hospitalization eating disorder treatment center (Median days since discharge at start of study = 140 days, Range = 1 day to 868 days; SD = 40.12). 125 participants (74.4%) reported that they were currently in some type of treatment for their eating disorder. Specifically, 96 participants (n = 57.1%) were in outpatient treatment, sixteen participants (9.5%) were in intensive outpatient, five participants were in partial hospitalization (3.03%), and eight participants (4.7%) were in inpatient or residential treatment. Participants median time in treatment is 2.00 hours (SD = 42.26) a week.
The majority of participants were female (n = 159; 94.6%) and European American (n = 156; 92.9%). Other ethnicities reported include multiracial or biracial (n = 3; 1.8%), Hispanic (n = 3; 1.8%), Black (n = 1; 0.6%), and Japanese American (n = 1; 0.6%). Four participants did not report their ethnicity. Participants ranged in age from 14 to 59 years old, with an average age of 26.27 (SD = 9.44).
Measures
Eating Disorder Diagnostic Scale (EDDS; Stice, Telch, & Rizvi, 2000)
The EDDS is a brief self-report measure used to diagnose eating disorders, such as anorexia, bulimia, and binge eating disorder. The EDDS has demonstrated adequate internal consistency as well as criterion and convergent validity (Stice, Fisher, & Martinez, 2004). Internal consistency in this sample was adequate (α = .78).
Fear of Food Measure (FOFM; Levinson & Byrne, 2015)
The FOFM is a 25-item self-report questionnaire measuring fear of food through a cognitive-behavioral approach (i.e., thoughts, feelings, and behaviors). The measure includes three subscales addressing each aspect of the cognitive-behavioral model of fear of food: trait anxiety about eating (i.e., feelings), feared concerns related to eating (i.e., thoughts), and food avoidance behaviors (i.e., behaviors). Example items from the anxiety about eating subscale include: I feel tense when I am around food and I worry about eating. Example items from the feared concerns about eating subscale include: Eating makes me feel anxious because I am afraid I might get fat and I don’t like to eat around other people because they might judge me. Example items from the food avoidance behaviors subscale include: There are certain foods I avoid because they make me anxious and I have to eat my food in a certain order. The FOFM has been shown to have good convergent and divergent validity as well as excellent test-retest reliability (Levinson & Byrne, 2015). In the current sample, anxiety about eating (α = .96) and feared concerns about eating (α = .92) exhibited excellent internal consistency and food avoidance behaviors (α = .89) exhibited good internal consistency.
Eating Disorder Inventory-2 (EDI-2; Garner, Olmstead, & Polivy, 1983)
The EDI-2 is a 91-item self-report questionnaire designed to measure psychological features commonly associated with anorexia nervosa and bulimia nervosa. It has been shown to have good internal consistency and good convergent and discriminant validity (Garner et al., 1983), and is frequently used by clinicians for the assessment of eating disorder symptoms (Brookings & Wilson, 1994). Three of the eleven subscales were used for this study: the Drive for Thinness (DT), Body Dissatisfaction (BD), and Bulimia symptoms (BN) subscales. In the current sample, body dissatisfaction (α = .92) and bulimic symptoms (α = .91) exhibited excellent internal consistency and drive for thinness (α = .76) exhibited adequate internal consistency.
Eating Disorder Examination-Questionnaire (EDE-Q; Fairburn & Beglin, 1994)
The EDE-Q is a 38-item self-report measure of eating disorder-related attitudes and behaviors in the past 28 days based on the Eating Disorder Examination (EDE) interview (Fairburn & Cooper, 1993). The current study used the weight concerns and eating concerns subscales, which assess disordered eating concerns around weight and eating respectively. Example items are: Have you had a strong desire to lose weight and Have you had a definite fear of losing control over eating. The EDE-Q has evidenced good internal consistency (Peterson et al., 2007). In this sample, internal consistency for the weight concerns subscale (α = .88) was good and internal consistency for the eating concerns subscale (α = .70) was adequate.
Positive and Negative Affect Schedule (PANAS; Watson, Clark, & Tellegen, 1988)
The PANAS is a 20-item self-report measure of positive and negative affect that asks participants to describe the extent to which they generally feel different emotions. The current study utilized the ten-item negative affect subscale. Example items include: upset, guilty, and irritable. The PANAS has exhibited good internal consistency as well as good convergent and divergent validity. Internal consistency of the negative affect subscale in this sample was excellent (α = .90).
Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007)
The ASI-3 is an 18-item multidimensional measure of physical, social, and cognitive concerns related to anxiety sensitivity. Example items include: It scares me when I blush in front of people and When my thoughts speed up, I worry that I might be going crazy. The ASI-3 has been shown to have good internal consistency, criterion-related validity, and convergent validity. Internal consistency in this sample was excellent (α = .91).
Data Analytic Strategy
Mplus Version 7.1 (Muthen & Muthen, 1998) was used for all analyses. The MLR estimator, an Mplus option for maximum likelihood estimation with robust standard error, was used to report standardized path estimates. MLR was used because it is robust to potential non-normal data and is able to estimate missing data efficiently (Muthen & Muthen, 1998). Model fit was evaluated using the comparative fit index (CFI; Bentler, 1990), the Tucker-Lewis incremental fit index (TLI; Tucker & Lewis, 1973), the root mean square error of approximation (RMSEA; Steiger & Lind, 1980), and the standardized root mean square residual (SRMR; Jöreskog & Sörbom, 1981). For the RMSEA and SRMR, values below or equal to .08 were considered adequate and below or equal to .05 were considered very good (Hu & Bentler, 1999). For the CFI and TLI, values above or equal to .90 were considered adequate and above or equal to .95 were considered very good (Hu & Bentler, 1999). All missing data for Time 2 were efficiently estimated because the MLR estimator was used.
Cross-lagged path analysis was used for all analyses, which allows us to test which correlated variables are the most salient predictors of eating disorder symptoms. This type of model allows tests of causal precedence by statistically controlling for the value of the outcome variable at a previous iteration (time point), while testing the independent variables impact on the outcome (for more information on this type of model please see Newson, 2015). We first tested nine individual models with each of the three subscales of the FOFM (anxiety about eating, feared concerns, and food avoidance behaviors) at both Time 1 and Time 2 paired with the three eating disorder symptoms tested (drive for thinness, body dissatisfaction, and bulimic symptoms). This analysis is analogous to conducting multiple regression for each outcome, except that cross-lagged path analysis allows for tests in both directions (e.g., simultaneously testing if anxiety about eating predicts drive for thinness and drive for thinness predicts anxiety about eating). If there was a significant relationship between fear of food and an eating disorder symptom, we then added additional predictors that are hypothesized to relate to the outcome (eating and weight concern, negative affect, and anxiety sensitivity) to the model to test if the relationship held when accounting for these additional variables. These analyses would only be necessary if there was a significant relationship between fear of food and the eating disorder outcomes and show that the relationship between fear of food and an eating disorder outcome is not because of a general relationship between anxiety, negative affect, and weight and eating concerns, but rather because of a specific relationship between fear of food and eating disorder symptoms.
Results
Diagnoses and Clinical Characteristics
The following diagnoses were made based on the Eating Disorder Diagnostic Scale (Stice et al., 2000): anorexia nervosa (n = 34; 14.7%) or atypical anorexia nervosa (all but below 18.5 BMI) (n = 104; 61.9%); purging disorder (n = 16; 9.5%); bulimia nervosa or subthreshold bulimia nervosa (n = 13; 7.7%); and binge eating disorder (n = 1; 0.6%). Mean body mass index (BMI) was 21.41 (range = 14.92–44.91; SD = 4.44). Other self-reported diagnoses were anxiety disorder (n = 101; 60.1%), depressive disorder (n = 100; 59.5%), obsessive-compulsive disorder (n = 23; 13.7%), attention deficient disorder or attention deficit hyperactivity disorder (n = 12; 7.1%), borderline personality disorder (n = 7; 4.2%), and bipolar disorder (n = 13; 7.7%).
Zero-order Correlations and Descriptive Statistics
Please see Table 1 for descriptive statistics for each study variable. Please see Table 2 for zero-order correlations from Time 1 and Time 2 among fear of food, eating disorder symptoms, eating concern, weight concern, negative affect, and anxiety sensitivity. As expected, most all variables were significantly correlated.
Table 1.
Descriptive statistics for all Time 1 and Time 2 variables.
| Mean | SD | Range | Minimum | Maximum | |
|---|---|---|---|---|---|
| T1Bulimia | 15.17 | 8.14 | 32.00 | 7.00 | 39.00 |
| T2Bulimia | 15.07 | 7.45 | 26.00 | 7.00 | 33.00 |
| T1DT | 23.12 | 6.85 | 27.00 | 5.00 | 32.00 |
| T2DT | 23.31 | 5.84 | 26.00 | 9.00 | 35.00 |
| T1BD | 7.68 | 10.39 | 44.00 | −25.00 | 19.00 |
| T2BD | 8.28 | 9.16 | 32.00 | −13.00 | 19.00 |
| T1ASI | 24.38 | 14.85 | 64.00 | 0.00 | 64.00 |
| T2ASI | 23.00 | 14.26 | 59.00 | 0.00 | 59.00 |
| T1NA | 30.24 | 8.68 | 35.00 | 13.00 | 48.00 |
| T2NA | 30.65 | 7.97 | 33.00 | 13.00 | 46.00 |
| T1AE | 34.96 | 13.74 | 48.00 | 8.00 | 56.00 |
| T2AE | 35.44 | 12.89 | 46.00 | 10.00 | 56.00 |
| T1FAB | 34.38 | 12.74 | 48.00 | 8.00 | 56.00 |
| T2FAB | 35.78 | 11.57 | 44.00 | 12.00 | 56.00 |
| T1FC | 39.37 | 14.90 | 54.00 | 9.00 | 63.00 |
| T2FC | 40.53 | 13.39 | 51.00 | 11.00 | 62.00 |
| T1WC | 17.34 | 8.80 | 30.00 | 0.00 | 30.00 |
| T2WC | 17.68 | 8.35 | 30.00 | 0.00 | 30.00 |
| * T1EC | 7.81 | 5.57 | 24.00 | 0.00 | 24.00 |
| * T2EC | 6.94 | 4.52 | 19.00 | 0.00 | 19.00 |
Note. T1 = Time 1; T2 = Time 2; Bulimia = bulimic symptoms; DT = Drive for Thinness; BD = Body Dissatisfaction; ASI = Anxiety Sensitivity Index; NA = Negative Affect; AE = Anxiety about Eating; FAB = Food Avoidance Behaviors; FC = Feared Concerns; WC = Weight Concern; and EC = Eating Concern.
The only significant difference across time points is eating concern from Time 1 to Time 2.
Table 2.
Zero-order correlations among all Time 1 and Time 2 variables.
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. T1AE | - | |||||||||||||||||||
| 2. T1FAB | .78** | - | ||||||||||||||||||
| 3. T1FC | .89** | .79** | - | |||||||||||||||||
| 4. T1DT | .71** | .57** | .78** | - | ||||||||||||||||
| 5. T1Bulimia | .29** | .11 | .31** | .40** | - | |||||||||||||||
| 6. T1BD | .61** | .49** | .62** | .66** | .31** | - | ||||||||||||||
| 7. T1WC | .71** | .56** | .70** | .77** | .40** | .78** | - | |||||||||||||
| 8. T1EC | .66** | .49** | .63** | .62** | .64** | .48** | .70** | - | ||||||||||||
| 9. T1NA | .65** | .51** | .65** | .56** | .38** | .55** | .64** | .63** | - | |||||||||||
| 10. T1ASI | .38** | .31** | .49** | .33** | .27** | .34** | .33** | .33** | .47** | - | ||||||||||
| 11. T2AE | .82** | .66** | .76** | .50** | .29* | .41** | .50** | .58** | .57** | .31** | - | |||||||||
| 12. T2FAB | .67** | .76** | .65** | .41** | .20 | .37** | .43** | .52** | .55** | .27* | .80** | - | ||||||||
| 13. T2FC | .76** | .59** | .81** | .55** | .31** | .47** | .50** | .55** | .57** | .41** | .90** | .81** | - | |||||||
| 14. T2DT | .66** | .51** | .69** | .74** | .31** | .56** | .56** | .49** | .50** | .22 | .64** | .56** | .69** | - | ||||||
| 15. T2Bulimia | .31* | .07 | .31* | .35** | .93** | .20 | .31* | .55** | .29* | .08 | .29* | .16 | .27* | .34** | - | |||||
| 16. T2BD | .48** | .39** | .48** | .41** | .23 | .86** | .69** | .42** | .56** | .29* | .51** | .43** | .54** | .55** | .22 | - | ||||
| 17. T2WC | .62** | .49** | .60** | .64** | .48** | .71** | .82** | .68** | .53** | .11 | .65** | .55** | .63** | .71** | .45** | .71** | - | |||
| 18. T2EC | .51** | .32** | .47** | .45** | .57** | .30** | .39** | .69** | .41** | .09 | .62** | .44** | .54** | .53** | .65** | .32** | .66** | - | ||
| 19. T2NA | .51** | .41** | .49** | .37** | .25* | .51** | .57** | .49** | .80** | .39** | .60** | .58** | .60** | .55** | .30* | .64** | .63** | .44** | - | |
| 20. T2ASI | .26* | .20 | .36** | .08 | .16 | .19 | .14 | .19 | .36** | .85** | .37** | .32** | .43** | .17 | .12 | .24* | .17 | .21 | .39** | - |
Note. T1 = Time 1; T2 = Time 2; AE = Anxiety about Eating; FAB = Food Avoidance Behaviors; FC = Feared Concerns; DT = Drive for Thinness; Bulimia = bulimic symptoms; BD = Body Dissatisfaction; WC = Weight Concern; EC = Eating Concern; NA = Negative Affect; ASI = Anxiety Sensitivity Index;
p < .05,
p < .01.
Does Fear of Food Prospectively Predict Drive for Thinness?
We first examined whether there was appreciable variance to be explained in Time 2 scores given Time 1 drive for thinness scores. Time 1 drive for thinness predicted 58.0% of the variance in Time 2 drive for thinness, indicating that there was 42.0% of the variance left to explain.
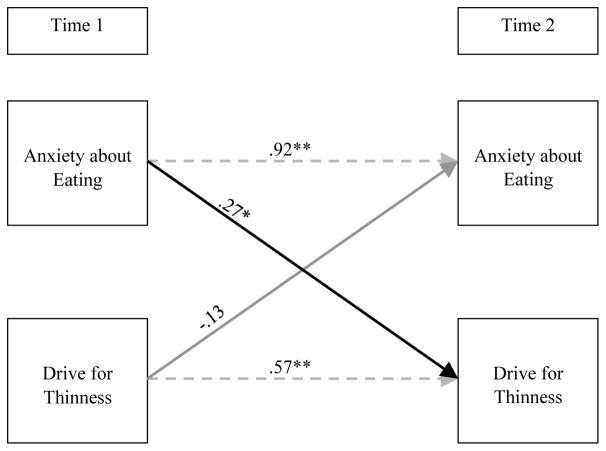
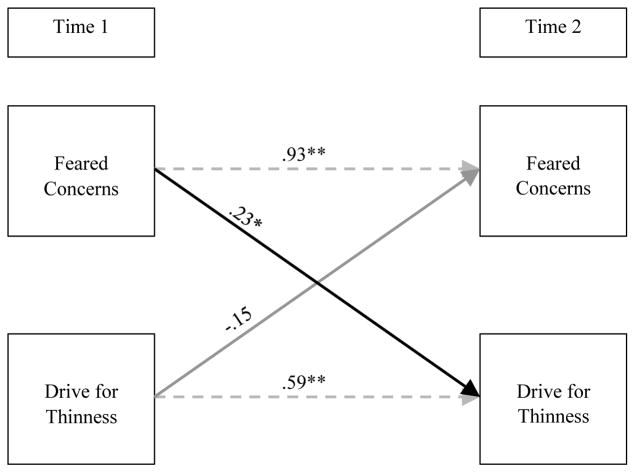
As can be seen in Figure 1, anxiety about eating at Time 1 significantly predicted drive for thinness at Time 2 (while accounting for Time 1 drive for thinness), whereas drive for thinness at Time 1 did not predict anxiety about eating at Time 2. Fit for this model was excellent (CFI = 1.00, TLI = 1.00, RMSEA = < .001, SRMR = < .001). As can be seen in Figure 2, Time 1 feared concerns about food significantly predicted Time 2 drive for thinness (while accounting for Time 1 drive for thinness), but Time 1 drive for thinness did not predict Time 2 feared concerns about food. Fit for this model was excellent (CFI = 1.00, TLI = 1.00, RMSEA = < .001, SRMR = < .001). Time 1 food avoidance did not predict Time 2 drive for thinness (b = .11, p = .31), nor did Time 1 drive for thinness predict Time 2 food avoidance (b = .01, p = .87).
Figure 1. Anxiety about eating and drive for thinness across time.
Autoregressive relationships are light gray and dashed for clarity; Estimates on arrows represent standardized beta values. **p < .01, *p < .05. Time 1 = after discharge, Time 2 = one-month follow-up. Solid black arrows indicate significant relationships. Solid gray lines represent non-significant relationships.
Figure 2. Feared concerns and drive for thinness across time.
Autoregressive relationships are light gray and dashed for clarity; Estimates on arrows represent standardized beta values. **p < .01, *p < .05. Time 1 = after discharge, Time 2 = one-month follow-up. Solid black arrows indicate significant relationships. Solid gray lines represent non-significant relationships.
Does Fear of Food Prospectively Predict Bulimic Symptoms?
We first examined whether there was appreciable variance to be explained in Time 2 scores given Time 1 bulimic symptoms scores. Time 1 bulimic symptoms predicted 87.8% of the variance in Time 2 bulimic scores, indicating that there was 12.2% of the variance left to explain. There were no significant relationships between Time 1 fears of food and Time 2 bulimic symptoms (all ps> .23), nor were there any significant relationships between Time 1 bulimic symptoms and Time 2 fears of food (all ps > .11).
Does Fear of Food Prospectively Predict Body Dissatisfaction?
We first examined whether there was appreciable variance to be explained in Time 2 scores given Time 1 body dissatisfaction scores. Time 1 body dissatisfaction symptoms predicted 76.2% of the variance in Time 2 body dissatisfaction scores, indicating that there was 23.8% of the variance left to explain. There were no significant relationships between Time 1 fears of food and Time 2 body dissatisfaction (all ps> .51), nor were there any significant relationships between Time 1 body dissatisfaction and Time 2 fears of food (all ps > .57).
Does Anxiety About Eating and Feared Concerns About Eating Predict Drive for Thinness Over and Above Other Related Concerns and Anxieties?
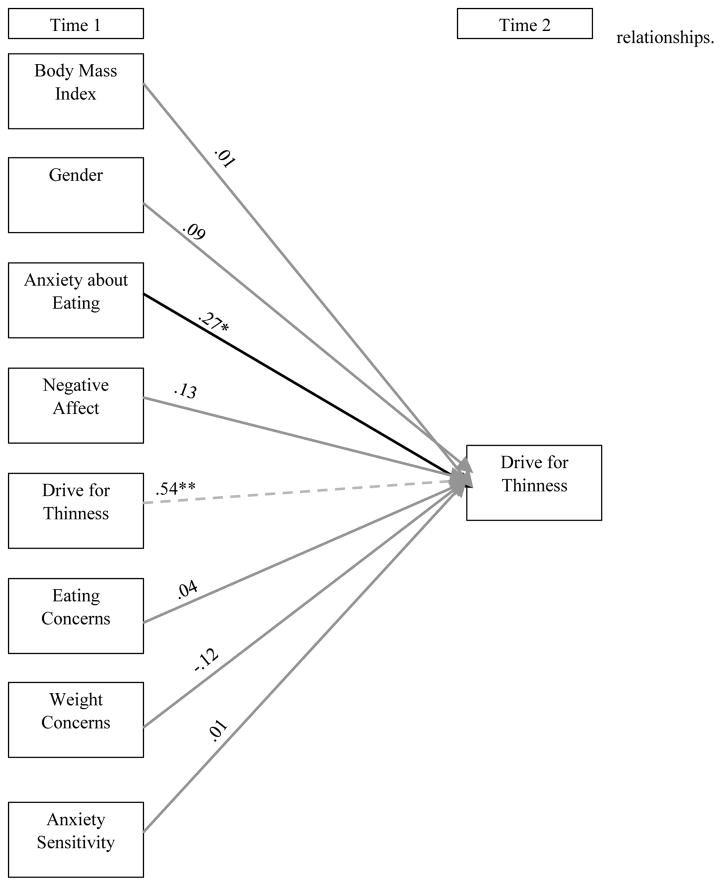
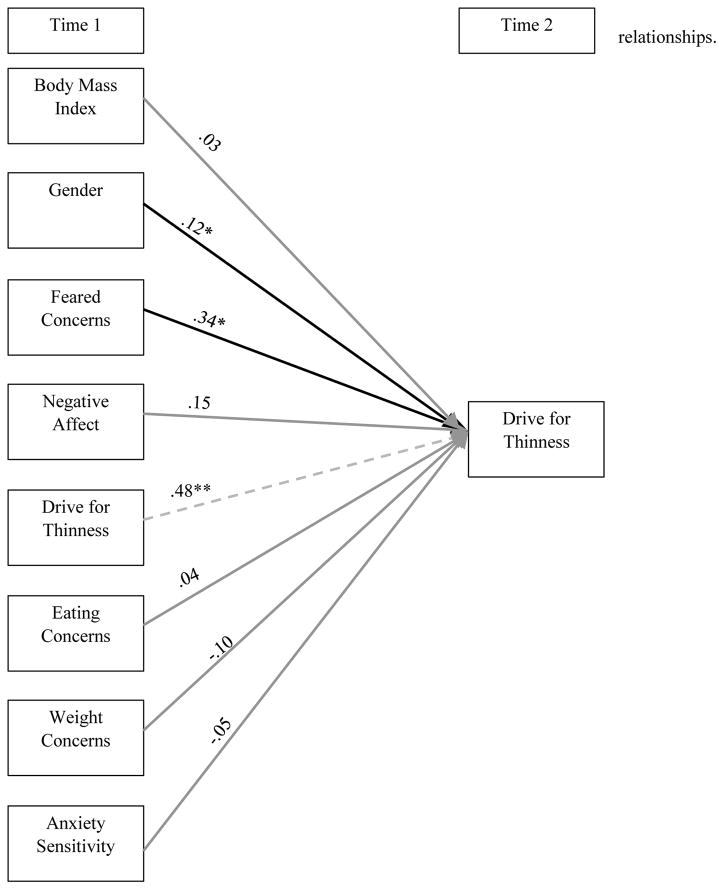
As can be seen in Figure 3, Time 1 anxiety about eating continued to predict Time 2 drive for thinness over and above Time 1 drive for thinness, eating concerns, weight concerns, anxiety sensitivity, body mass index, gender, and negative affect, suggesting that there is a specific relationship between anxiety about eating and drive for thinness which is not accounted for by general anxiety and negative affect. Fit for this model was excellent (CFI = 1.00, TLI = 1.00, RMSEA = < .001, SRMR = .01). As can be seen in Figure 4, Time 1 feared concerns about eating continued to predict Time 2 drive for thinness over and above Time 1 drive for thinness, eating concerns, weight concerns, anxiety sensitivity, body mass index, gender, and negative affect, again suggesting that there is a specific relationship between feared concerns about eating and drive for thinness that is not accounted for by general eating and weight concerns. Fit for this model was excellent (CFI = .99, TLI = .99, RMSEA = .02, SRMR = .02).
Figure 3. Anxiety about eating, negative affect, eating concerns, weight concerns, and anxiety sensitivity predicting drive for thinness over time.
Autoregressive relationships are light gray and dashed for clarity; Estimates on arrows represent standardized beta values. **p < .01, *p < .10. Time 1 = after discharge, Time 2 = one-month follow-up. Solid black arrows indicate significant relationships. Solid gray lines represent non-significant relationships.
Figure 4. Feared concerns, negative affect, eating concerns, weight concerns, and anxiety sensitivity predicting drive for thinness over time.
Autoregressive relationships are light gray and dashed for clarity; Estimates on arrows represent standardized beta values. **p < .01, *p < .05. Time 1 = after discharge Time 2 = one-month follow-up. Solid black arrows indicate significant relationships. Solid gray lines represent non-significant relationships.
Conclusions
In patients recently discharged from intensive eating disorder treatment, we found that there was a specific prospective relationship between anxiety about eating and feared concerns about eating after discharge and drive for thinness one month later, while accounting for drive for thinness after discharge. These relationships held over and above general eating and weight concerns, as well as general anxiety (negative affect and anxiety sensitivity). Thus, there is a direct connection between anxiety about eating and drive for thinness that is not related to general anxiety sensitivity and negative affect. Similarly, there is a specific relationship between feared concerns about eating and drive for thinness that is not related to general eating and weight concerns. These findings suggest that interventions focused on decreasing anxiety about eating and feared concerns about eating may prevent later drive for thinness. This finding is particularly important given that elevated drive for thinness might represent an indicator of potential future relapses (Keski-Rahkonene et al., 2005; Ramacciotti et al., 2002), is associated with more severe psychopathology in patients with AN (Vervaet, van Heeringen, & Audenaert, 2004), and is related to persistent symptoms of bulimia nervosa in the community (Keski-Rahkonen et al., 2013). Future research should continue to test the link between drive for thinness, fear of food, and relapse.
Though both anxiety about eating and feared concerns about eating predicted drive for thinness, they did not predict other aspects of eating disorder symptoms, namely bulimic symptoms or body dissatisfaction. Again, these findings suggest that anxiety about eating and feared concerns of eating are a specific predictor of later drive for thinness. It seems likely that individuals who are very anxious about eating and fearful of what may happen to them if they eat, will be motivated to strive explicitly for thinness and low weight, rather than engaging in binge eating and purging, per se. Alternatively, these food-related fears may not impact body dissatisfaction or bulimic symptoms because body dissatisfaction and bulimic symptoms may be influenced more by other types of affect, rather than fear (Crosby et al., 2009; Lavender et al., 2014; Lavender et al., 2015; Smyth et al., 2007).
These findings have implications for treatment, as well as for relapse prevention. Addressing anxiety about eating, as well as feared concerns of eating, may help prevent drive for thinness and could prevent the high rates of relapse after patients discharge from intensive treatments (Herzog et al., 1999). Treatments could focus on reducing anxiety about eating by using exposures to feared foods (Levinson & Byrne, 2015). Relatedly, feared concerns of eating, such as fearing that eating will make one gain weight or not eating because of fear of judgment, could be focused on using imaginal or in-vivo exposures, in which the patient imagines they are gaining weight or are being judged because of weight gain. Our findings fit with other research suggesting that fears of weight gain (and therefore related fears of food) may be a primary driver behind eating disorder symptomatology (Levinson et al., 2017; Murray, Loeb, & Le Grange, 2016) and suggest fear of food may be an avenue to target drive for thinness.
Of course, there are several limitations we should discuss. First, our sample was derived from participants recently discharged from an intensive treatment center. Therefore, we do not know if these findings would apply to community samples of individuals with eating disorders or non-treatment seeking individuals. However, given that the relapse rates in such intensive treatment centers are high, it seems desirable to identify factors that might prevent relapse and repeated admissions to intensive treatment in high-risk eating disorder patients. Additionally, we did not use a semi-structured interview to determine diagnoses, but rather relied on a self-reported diagnostic measure. This limits the validity of our diagnostic information. However, given that these individuals were recently treated in an intensive eating disorder facility, we know that they suffered from a clinically significant eating disorder. Of course, future research should strive for better diagnostic information, a larger sample size to determine if there are differences between diagnostic categories, and tests to determine if this finding generalizes in other contexts. Furthermore, we do not have detailed information on discharge weight and post-discharge weight, which would be an informative variable to test if fear of food impacts change in body mass index. Despite these limitations, this study is the first to prospectively test relationships between fear of food and eating disorder outcomes, which can help inform targeted treatments aimed at reducing the anxiety that is common in the eating disorders.
Overall, we found that anxiety about eating and feared concerns of eating predicted later drive for thinness, whereas drive for thinness did not predict later anxiety about eating or feared concerns of eating. These findings were also specific to drive for thinness and not bulimic symptoms or body dissatisfaction. We hope that future research will clarify if interventions targeting anxiety about eating and feared concerns about eating can decrease a desire to maintain thinness, thus possibly reducing the suffering associated with eating disorders.
Highlights.
Fear of food predicted drive for thinness across one month
This relationship was not accounted for by anxiety sensitivity or negative affect
There is a specific, direct prospective relationship between fear of food and drive for thinness
Intervening on fear of food may prevent drive for thinness
Acknowledgments
This research was supported by T32 DA007261-25 to Washington University in St. Louis. We have no conflicts of interest to report.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. https://doi.org/10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brookings JB, Wilson JF. Personality and family-environment predictors of self-reported eating attitudes and behaviors. Journal of Personality Assessment. 1994;63(2):313–326. doi: 10.1207/s15327752jpa6302_10. https://doi.org/10.1207/s15327752jpa6302_10. [DOI] [PubMed] [Google Scholar]
- Crosby RD, Wonderlich SA, Engel SG, Simonich H, Smyth J, Mitchell JE. Daily mood patterns and bulimic behaviors in the natural environment. Behaviour Research and Therapy. 2009;47(3):181–188. doi: 10.1016/j.brat.2008.11.006. https://doi.org/10.1016/j.brat.2008.11.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairburn CG, Cooper Z. The Eating Disorder Examination. In: Fairburn CG, Wilson GT, editors. Binge eating: Nature, assessment, and treatment. 12. New York, NY: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- Fairburn CG, Beglin SJ. Assessment of eating disorders: Interview or self-report questionnaire? International Journal of Eating Disorders. 1994;16(4):363–370. [PubMed] [Google Scholar]
- Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. International Journal of Eating Disorders. 1983;2(2):15–34. https://doi.org/10.1002/1098-108x(198321)2:2<15::aid-eat2260020203>3.0.co;2-6. [Google Scholar]
- Halmi KA. Anorexia nervosa and bulimia nervosa. In: Martin IA, Volkmar F, editors. Lewis’s child and adolescent psychiatry: A comprehensive textbook. 4. New York, NY: Lippincott, Williams and Wilkins; 2007. pp. 592–602. [Google Scholar]
- Herzog DB, Dorer DJ, Keel PK, Selwyn SE, Ekeblad ER, Flores AT, … Keller MB. Recovery and relapse in anorexia and bulimia nervosa: A 7.5-year follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38(7):829–837. doi: 10.1097/00004583-199907000-00012. https://doi.org/10.1097/00004583-199907000-00012. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. https://doi.org/10.1080/10705519909540118. [Google Scholar]
- Jöreskog K, Sörbom D. LISREL: Analysis of linear structural relationships by the method of maximum likelihood (versión V) Chicago, IL: National Education Resources, Inc; 1981. [Google Scholar]
- Kaplan AS, Walsh BT, Olmsted M, Attia E, Carter JC, Devlin MJ, … Parides M. The slippery slope: Prediction of successful weight maintenance in anorexia nervosa. Psychological Medicine. 2009;39(6):1037–1045. doi: 10.1017/S003329170800442X. https://doi.org/10.1017/S003329170800442X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keski-Rahkonen A, Raevuori A, Bulik CM, Hoek HW, Sihvola E, Kaprio J, Rissanen A. Depression and drive for thinness are associated with persistent bulimia nervosa in the community. European Eating Disorders Review. 2013;21(2):121–129. doi: 10.1002/erv.2182. https://doi.org/10.1002/erv.2182. [DOI] [PubMed] [Google Scholar]
- Keski-Rahkonen A, Bulik CM, Neale BM, Rose RJ, Rissanen A, Kaprio J. Body dissatisfaction and drive for thinness in young adult twins. International Journal of Eating Disorders. 2005;37(3):188–199. doi: 10.1002/eat.20138. [DOI] [PubMed] [Google Scholar]
- Klump KL, Bulik CM, Kaye WH, Treasure J, Tyson E. Academy for Eating Disorders position paper: Eating disorders are serious mental illnesses. International Journal of Eating Disorders. 2009;42(2):97–103. doi: 10.1002/eat.20589. https://doi.org/10.1002/eat.20589. [DOI] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Peterson CB, Crosby RD, Engel SG, Mitchell JE, … Berg KC. Dimensions of emotion dysregulation in bulimia nervosa. European Eating Disorders Review. 2014;22(3):212–216. doi: 10.1002/erv.2288. https://doi.org/10.1002/erv.2288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavender JM, Wonderlich SA, Engel SG, Gordon KH, Kaye WH, Mitchell JE. Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: A conceptual review of the empirical literature. Clinical Psychology Review. 2015;40:111–122. doi: 10.1016/j.cpr.2015.05.010. https://doi.org/10.1016/j.cpr.2015.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Byrne M. The Fear of Food Measure: A novel measure for use in exposure therapy for eating disorders. International Journal of Eating Disorders. 2015;48(3):271–283. doi: 10.1002/eat.22344. https://doi.org/10.1002/eat.22344. [DOI] [PubMed] [Google Scholar]
- Levinson CA, Rodebaugh TL, Fewell L, Kass AE, Riley EN, Stark L, … Lenze EJ. D-cycloserine facilitation of exposure therapy improves weight regain in patients with anorexia nervosa: A pilot randomized controlled trial. Journal of Clinical Psychiatry. 2015;76(6):e787–e793. doi: 10.4088/JCP.14m09299. https://doi.org/10.4088/jcp.14m09299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levinson CA, Zerwas S, Calebs B, Forbush K, Kordy H, Watson H, … Bulik CM. The core symptoms of bulimia nervosa, anxiety, and depression: A network analysis. Journal of Abnormal Psychology. 2017;126(3):340–354. doi: 10.1037/abn0000254. https://doi.org/10.1037/abn0000254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mayer LES, Schebendach J, Bodell LP, Shingleton RM, Walsh BT. Eating behavior in anorexia nervosa: Before and after treatment. International Journal of Eating Disorders. 2012;45(2):290–293. doi: 10.1002/eat.20924. https://doi.org/10.1002/eat.20924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarlane T, Olmsted MP, Trottier K. Timing and prediction of relapse in a transdiagnostic eating disorder sample. International Journal of Eating Disorders. 2008;41(7):587–593. doi: 10.1002/eat.20550. https://doi.org/10.1002/eat.20550. [DOI] [PubMed] [Google Scholar]
- Murray SB, Loeb KL, Le Grange D. Dissecting the core fear in anorexia nervosa: Can we optimize treatment mechanisms? JAMA Psychiatry. 2016;73(9):891–892. doi: 10.1001/jamapsychiatry.2016.1623. https://doi.org/10.1001/jamapsychiatry.2016.1623. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 7. Los Angeles, CA: Muthén & Muthén; 1998. [Google Scholar]
- Newsom JT. The Encyclopedia of Adulthood and Aging. 2015. Cross-lagged Panel Analysis. [Google Scholar]
- Pallister E, Waller G. Anxiety in the eating disorders: Understanding the overlap. Clinical Psychology Review. 2008;28(3):366–386. doi: 10.1016/j.cpr.2007.07.001. https://doi.org/10.1016/j.cpr.2007.07.001. [DOI] [PubMed] [Google Scholar]
- Penas-Lledo E, Bulik CM, Lichtenstein P, Larsson H, Baker JH. Risk for self-reported anorexia or bulimia nervosa based on drive for thinness and negative affect clusters/dimensions during adolescence: A three-year prospective study of the TChAD cohort. International Journal of Eating Disorders. 2015;48(6):692–699. doi: 10.1002/eat.22431. https://doi.org/10.1002/eat.22431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson CB, Crosby RD, Wonderlich SA, Joiner T, Crow SJ, Mitchell JE, … le Grange D. Psychometric properties of the Eating Disorder Examination-Questionnaire: Factor structure and internal consistency. International Journal of Eating Disorders. 2007;40(4):386–389. doi: 10.1002/eat.20373. https://doi.org/10.1002/eat.20373. [DOI] [PubMed] [Google Scholar]
- Ramacciotti CE, Dell’Osso L, Paoli RA, Ciapparelli A, Coli E, Kaplan AS, Garfinkel PE. Characteristics of eating disorder patients without a drive for thinness. International Journal of Eating Disorders. 2002;32(2):206–212. doi: 10.1002/eat.10067. [DOI] [PubMed] [Google Scholar]
- Smyth JM, Wonderlich SA, Heron KE, Sliwinski MJ, Crosby RD, Mitchell JE, Engel SG. Daily and momentary mood and stress are associated with binge eating and vomiting in bulimia nervosa patients in the natural environment. Journal of Consulting and Clinical Psychology. 2007;75(4):629–638. doi: 10.1037/0022-006X.75.4.629. https://doi.org/10.1037/0022-006x.75.4.629. [DOI] [PubMed] [Google Scholar]
- Steiger JH, Lind JC. Statistically-based tests for the number of factors. Paper presented at the annual spring meeting of the Psychometric Society; Iowa City, IA. 1980. May, [Google Scholar]
- Steinglass J, Albano AM, Simpson HB, Carpenter K, Schebendach J, Attia E. Fear of food as a treatment target: Exposure and response prevention for anorexia nervosa in an open series. International Journal of Eating Disorders. 2012;45(4):615–621. doi: 10.1002/eat.20936. https://doi.org/10.1002/eat.20936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stice E, Telch CF, Rizvi SL. Development and validation of the Eating Disorder Diagnostic Scale: A brief self-report measure of anorexia, bulimia, and binge-eating disorder. Psychological Assessment. 2000;12(2):123–131. doi: 10.1037//1040-3590.12.2.123. https://doi.org/10.1037/1040-3590.12.2.123. [DOI] [PubMed] [Google Scholar]
- Stice E, Fisher M, Martinez E. Eating Disorder Diagnostic Scale: Additional evidence of reliability and validity. Psychological Assessment. 2004;16(1):60–71. doi: 10.1037/1040-3590.16.1.60. https://doi.org/10.1037/1040-3590.16.1.60. [DOI] [PubMed] [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, … Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. https://doi.org/10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38(1):1–10. https://doi.org/10.1007/bf02291170. [Google Scholar]
- Vervaet M, van Heeringen C, Audenaert K. Is drive for thinness in anorectic patients associated with personality characteristics? European Eating Disorders Review. 2004;12(6):375–379. https://doi.org/10.1002/erv.586. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54(6):1063–1070. doi: 10.1037//0022-3514.54.6.1063. https://doi.org/10.1037/0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]