Abstract
In recurrent breast cancer, the tumor phenotype, as assessed by estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor 2 (HER2) status, occasionally changes. This change, in addition to the Ki67 index were evaluated at sites of recurrence and the correlation between changes in tumor phenotype and survival were assessed in breast cancer patients. Comparisons in pathological parameters between primary and metastatic lesions were drawn between ER, PR, HER2, and the Ki67 index in 70 patients with recurrent breast cancer. The association between changes in tumor phenotype and patient survival was assessed. The hormone receptor status changed from positive, in the primary lesions, to negative, in the metastatic lesions in 19.8% (ER) and 39.5% (PR) of patients, respectively. Conversion from negative to positive status was confirmed in 27.2% (ER) and 31.2% (PR) of patients, respectively. A change in HER2 status from negative (primary lesion) to positive (metastatic lesion) occurred in seven patients (10%). The mean Ki67 index of primary lesions with positive hormone receptor status was significantly lower than at sites of recurrence with any hormone receptor status, from 10.9±9.8 standard deviation (SD) to 22.9±18.6 (P=0.031) and 12.2±10.5 SD to 27.4±20.9 (P=0.023), for ER and PR, respectively. The mean overall survival of patients with ER status conversion from positive to negative was 7.4±1.2 standard error (SE) years, and 14.8±1.4 SE years for patients who retained positive ER status (P=0.005, log-rank), with a hazard ratio of 3.44 (95% confidence interval, 1.36–8.33). This difference in survival based upon change in ER status was similarly observed in patients with PR status conversion in the same direction. Thus, ER and PR status conversion at the time of recurrence strongly impact survival, particularly if the change is from positive (primary lesion) to negative (metastatic lesion). Monitoring the biological behavior of breast cancer may benefit a patient by allowing for a novel personalized treatment strategy.
Keywords: estrogen receptor, progesterone receptor, human epidermal growth factor 2, Ki67 index, receptor conversion and metastatic breast cancer
Introduction
Approximately one-third of breast cancer patients develop recurrent tumors and subsequently succumb to the disease. The treatment strategy for recurrent breast cancer is generally determined based on information from the pathological diagnosis of the primary lesion. However, tumor phenotype, as represented by estrogen receptor (ER), progesterone receptor (PR) and human epidermal growth factor 2 (HER2) status occasionally changes at recurrence (1–4). Therefore, pathological assessment of recurrent tumors may provide important information to guide the therapeutic strategy.
In the present study, the status of hormonal receptors, ER, PR and HER2, and the Ki67 index were compared in primary and recurrent tumors, as well as those of metastatic lymph nodes that were dissected at the time of primary tumor evaluation. In addition, correlations between alterations in tumor status and patient survival were examined. To the best of our knowledge, this is the first study to report survival risk upon recognition of alterations in hormonal receptors.
Patients and methods
Patients
A total of 70 breast cancer patients with a date of original diagnosis between August 1990 and January 2012 were enrolled in the present study. The initial surgical procedures for the primary lesions were performed at Aichi Medical University Hospital (Nagakute, Japan) for 54 patients, at Marumo Hospital (Nagoya, Japan) for 13, at Kato Clinic (Nagoya, Japan) for 2, and at Nagoya City University Hospital (Nagoya, Japan) for 1 patient. All the patients were subsequently continuously followed-up at Aichi Medical University Hospital. During the follow-up period, the attending physician of the outpatient clinic planned for annual mammography. Computed tomography of the total body and/or blood tests were performed if indicated by the patient's clinical condition or at the discretion of the attending physician. When recurrence was diagnosed, the lesion was biopsied or excised for pathological confirmation. For 15 patients, fine needle aspiration cytology was used to diagnose metastatic lesions. For immunohistochemical examination of cytology specimens, cell blocks were prepared using cyto-puncture materials as described by Kumar et al (5). Clinical data of the study patients were obtained from their medical records.
Tumor pathology
Pathological assessment of recurrent lesions in all patients was performed by the Department of Pathology at the Aichi Medical University Hospital. Diagnosis of the primary lesion was made at Aichi Medical University Hospital for 59 patients. For the remaining 11 patients, pathological examination of the primary lesion was performed at the institution where surgery was performed. The histologic type was determined according to the World Health Organization criteria (6). Histopathological grading was as described by TNM classification of the 6th edition (7). Primary and metastatic lesions were compared based on the ER, PR and HER2 status, as well as the Ki67 index, a marker of proliferation. ER or PR positivity was defined as an Allred score of ≥3 and moderate-to-intense nuclear staining of ≥10%, respectively, while for cell block specimens, moderate to intense staining of ≥10% of all countable tumor cells was considered to indicate ER or PR positivity (8,9). Immunohistochemical assessment of HER2 expression levels was conducted using an anti-HER2 monoclonal antibody (A0485; Agilent Technologies, Inc., Santa Clara, CA, USA). HER2 overexpression was scored as 0 (negative), 1+ (incomplete membrane staining in any proportion of tumor cells), 2+ (complete membrane staining that was either nonuniform or weak in intensity but with obvious circumferential distribution in ≥10% tumor cells, or invasive tumors with intense, complete membrane staining of ≤30% tumor cells) and 3+ (uniform, intense membrane staining of >30% invasive tumor cells), in accordance with the guidelines of the American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) (10). Scores of 0 and 1+ were considered negative while 3+ was considered positive (10). When the immunohistochemical score was 2+, fluorescence in situ hybridization (FISH) was performed using the PathVysion HER-2 DNA Probe kit (Abbott Pharmaceutical Co. Ltd., Lake Bluff, IL, USA) and the results were assessed according to the manufacturer's instructions. A FISH score >2 was defined as positive. The same procedure was used for the evaluation of HER2 in cell block specimens. The Ki67 index was expressed as the proportion of positive cells within at least 500 tumor cells. Interpretation of Ki67 staining and scoring was based upon the recommendations described by Dowsett et al (11). Similarly, the proportion of cells with moderate to intense staining, using the anti-Ki67 antibody (M7240; Agilent Technologies, Inc.), within all countable tumor cells in the cell block specimen was interpreted as the Ki67 index. Lymph node metastases were observed in 39 patients at the time of initial surgery. The same pathological assessments were performed for metastatic lymph nodes for 30 patients for whom paraffin blocks could be made.
Immunohistochemistry
Primary tumors, metastatic lymph nodes and histologically proven metastases were subjected to immunohistochemical analysis with anti-ER (1:1; 107925) and anti-PR (1:1; 102333) (both from Roche Diagnostics, Basel, Switzerland), anti-HER2 (1:100; A0485) and anti-Ki67 (1:100; M7240) (both from Agilent Technologies, Inc.) antibodies according to routine protocols. Briefly, 4-µm sections of paraffin-embedded tissue and cell block specimens were deparaffinized 3 times in xylene, rehydrated in graded alcohol, and rinsed in Tris-buffered saline (TBS). To improve antigen retrieval, dewaxed sections were immersed in 0.1 M Tris-buffer, pH 9.5 (for ER and PR) or citrate buffer, pH 6.0 (for HER2 and Ki67), heated for 7 min in a pressure cooker, cooled at room temperature for 5 min, and washed 3 times in TBS. All subsequent steps were performed at room temperature. Endogenous peroxidase activity was blocked by incubation for 15 min in methanol containing 0.3% hydrogen peroxidase, followed by 3 washes in TBS. Non-specific binding was blocked by incubating the sections for 10 min in phosphate-buffered saline containing 5% skim milk. After removing excess blocking agents, the primary antibodies were applied and the sections were incubated in a moist chamber (20CG; Cosmo Bio Co., Ltd., Tokyo, Japan) for 1 h at room temperature to enable primary antibody binding. Following several rinses, labeling was detected by administering dextran coupled with peroxidase molecules and goat secondary antibody molecules against rabbit and mouse immunoglobulin (1:1) of a Dako EnVision peroxidase kit (K1491; Agilent Technologies, Inc.) for 1 h. Subsequently, the sections were rinsed and a chromogenic substrate, prepared by mixing 20 µl 3,3′-diaminobenzidine tetrahydrochloride and 1 ml imidazole-buffered solution containing hydrogen peroxide (Dako Liquid DAB Substrate Chromogen System; K3465; Agilent Technologies, Inc.), was applied for 1.5 min for ER, 2 min for PR, 3 min for HER2 and 2 min for Ki67 staining. The slides were lightly counterstained with hematoxylin to provide cellular details. Positive expression of the hormonal receptors (ER and PR) was defined as nuclear staining of cancer cells at any intensity. Ki67 staining was recognized in nucleus of the cancer cell at all cell cycle phases other than G0 phase according to a previous method described by Gerdes et al (12). For HER2, membrane staining was evaluated in accordance with the guidelines of ASCO/CAP. The evaluation of immunostained slides was performed in random order by a single pathologist blinded to the other data of the paired samples. The assessment of slides was performed by optical microscopy.
Statistical analysis
The association between changes in hormone receptor status and other characteristics was evaluated using the c2 test. Student's t-test and the Mann-Whitney U test were performed to assess the Ki67 index. Student's t-test was applied when the Ki67 index exhibited a normal distribution and the Mann-Whitney U test was used to evaluate the remaining data. Disease-free survival was defined as the time from initial surgery to pathological confirmation of recurrence. Overall survival was defined as the time from initial surgery to mortality. Overall survival was analyzed using the Kaplan-Meier function, the log-rank test and Cox regression. P<0.05 was considered to indicate a statistically significant difference. All statistical analyses were performed using IBM SPSS Statistics, version 20 (IBM Corporation, Armonk, NY, USA).
Results
ER and PR status
The clinicopathological characteristics of the patients are presented in Table I. The data in Table I are divided into four groups according to primary tumor hormonal receptor status. No significant difference was present in the distribution among the four groups (c2 test). Of the 70 patients, 48 (68.5%) were positive for ER and 38 (54.2%) were positive for PR at the primary site. The conversion rate for ER, from positive in the primary lesion to negative in the metastatic lesion (denoted as ER+/−), was 19.8%. The PR+/− conversion rate was 39.5%. Positive conversions, i.e., ER−/+ and PR−/+, occurred in 27.2 and 31.2% of all patients enrolled, respectively. One of the 32 patients, who was negative for PR at the primary site, was excluded from the assessment due to paraffin block deterioration. Among the 30 patients with lymph node metastasis, for whom pathological re-examination could be performed, hormone receptor status conversion in a metastatic lymph node occurred in only one patient with an ER-positive primary lesion (4.0%), in 18.8% of 16 patients with a PR-positive primary lesion and in 35.7% of 14 patients with a PR-negative primary lesion (Table II). ER status conversion in metastatic lymph nodes was rarely observed, whereas the PR status frequently differed at a metastatic site. For PR, conversion occurs relatively easily at recurrent sites, as well as in metastatic lymph nodes. No statistically significant associations were observed between changes in hormone receptor status and adjuvant treatment (Table II). In addition, metastatic locations were divided into two groups (lymph nodes, local metastases and bone metastases versus other sites, such as the lung, liver, brain and gastrointestinal tract, indicating visceral crisis). Patients exhibiting positive receptor status at metastatic sites were predominantly in the former group, with 61.8% for ER and 69.2% for PR. By contrast, approximately half of patients with negative receptor status at metastatic sites had visceral crisis (48.0% for ER and 44.3% for PR). These findings imply that tumors with negative hormone receptor status at metastatic sites demonstrate aggressive progression.
Table I.
Patient characteristics.
| Primary tumor status | |||||||
|---|---|---|---|---|---|---|---|
| Estrogen receptor | Progesterone receptor | ||||||
| Variable | All patients | Positive | Negative | P-value | Positive | Negative | P-value |
| Patients (n) | 70 | 48 | 22 | 38 | 32 | ||
| Age (mean ± SD) | 54.5±15.5 | 55.8±15.5 | 51.8±15.6 | 0.320 | 53.6±17.3 | 55.6±13.3 | 0.603 |
| Menopausal status (at original diagnosis) | |||||||
| Premenopausal | 32 | 23 | 9 | 0.585 | 21 | 11 | 0.081 |
| Postmenopausal | 38 | 25 | 13 | 17 | 21 | ||
| Pathological type | |||||||
| Invasive ductal carcinoma | 61 | 41 | 20 | 0.213 | 32 | 29 | 0.398 |
| Invasive lobular carcinoma | 2 | 2 | 0 | 2 | 0 | ||
| Invasive micropapillary carcinoma | 3 | 3 | 0 | 2 | 1 | ||
| Medullary carcinoma | 2 | 0 | 1 | 0 | 1 | ||
| Spindle cell carcinoma | 1 | 0 | 1 | 0 | 1 | ||
| Ductal carcinoma in situ | 1 | 1 | 0 | 1 | 0 | ||
| Surgical procedure | |||||||
| Mastectomy | 54 | 39 | 15 | 0.227 | 30 | 24 | 0.695 |
| Partial resection | 16 | 9 | 7 | 8 | 8 | ||
| Histological grade | |||||||
| 1 | 8 | 6 | 2 | 0.001 | 5 | 3 | 0.314 |
| 2 | 35 | 30 | 5 | 22 | 13 | ||
| 3 | 18 | 10 | 8 | 8 | 10 | ||
| Unknown | 9 | 2 | 7 | 3 | 6 | ||
| TNM stage | |||||||
| Tis | 1 | 1 | 0 | 0.801 | 1 | 0 | 0.568 |
| T1 | 21 | 12 | 9 | 10 | 11 | ||
| T2 | 33 | 24 | 9 | 20 | 13 | ||
| T3 | 7 | 5 | 2 | 2 | 5 | ||
| T4 | 5 | 4 | 1 | 3 | 2 | ||
| Unknown | 3 | 2 | 1 | 2 | 1 | ||
| N0 | 29 | 16 | 13 | 0.198 | 15 | 14 | 0.673 |
| N1 | 34 | 25 | 9 | 19 | 15 | ||
| N2 | 3 | 3 | 0 | 1 | 2 | ||
| N3 | 2 | 2 | 0 | 1 | 1 | ||
| Unknown | 2 | 2 | 0 | 2 | 0 | ||
| Stage | |||||||
| 0 | 1 | 1 | 0 | 0.803 | 1 | 0 | 0.818 |
| I | 14 | 17 | 7 | 7 | 7 | ||
| II | 39 | 27 | 12 | 22 | 17 | ||
| III | 13 | 11 | 2 | 6 | 7 | ||
| Unknown | 3 | 2 | 1 | 2 | 1 | ||
SD, standard deviation.
Table II.
Distribution of changes in hormone receptor status at metastatic sites.
| Primary tumor receptor status | ||||||||
|---|---|---|---|---|---|---|---|---|
| Estrogen receptor | Progesterone receptor | |||||||
| Variable | Positive | Negative | Positive | Negative | Positive | Negative | Positive | Negative |
| Patients (n) | 48 | – | – | 22 | 38 | – | – | 32 |
| Receptor status | ||||||||
| Metastatic lymph nodes from the primaries | ||||||||
| Number of patients (%) | 24 (96.0) | 1 (4.0) | 0 | 5 (100) | 13 (81.2) | 3 (18.8) | 5 (35.7) | 9 (64.3) |
| Metastatic site | ||||||||
| Number of patients (%) | 39 (81.2) | 9 (19.8) | 6 (27.2) | 16 (82.8) | 23 (60.5) | 15 (39.5) | 10 (31.2) | 21 (65.6) |
| Adjuvant treatment, n (%) | ||||||||
| Hormonal treatment only | 17 (43.6) | 4 (44.4) | 0 | 1 (6.2) | 10 (43.5) | 6 (40.0) | 2 (20.0) | 1 (4.8) |
| Hormonal treatment and/or chemotherapy | 19 (48.7) | 5 (55.6) | 6 (100) | 11 (68.8) | 12 (52.2) | 8 (53.3) | 7 (70.0) | 15 (71.4) |
| None | 1 (2.6) | 0 | 0 | 4 (25.0) | 1 (4.3) | 0 | 0 | 5 (23.8) |
| Unknown | 2 (5.1) | 0 | 0 | 0 | 0 | 1 (6.7) | 1 (10.0) | 0 |
| P-value | 0.858 | 0.297 | 0.529 | 0.106 | ||||
| Metastatic site, n (%) | ||||||||
| Lymph nodes | 19 (30.1) | 3 (15.8) | 1 (6.3) | 8 (24.3) | 10 (27.0) | 7 (38.9) | 4 (25.0) | 8 (17.4) |
| Local site | 15 (23.8) | 2 (10.5) | 1 (6.3) | 3 (9.1 | 10 (27.0) | 2 (11.1) | 3 (18.5) | 7 (15.2) |
| Bone | 8 (12.7) | 4 (21.0) | 3 (18.7) | 6 (18.2) | 7 (18.9) | 2 (11.1) | 2 (12.5) | 8 (17.4) |
| Lung and pleura | 7 (11.1) | 3 (15.8) | 4 (25.0) | 3 (9.1) | 3 (8.1) | 2 (11.1) | 3 (18.7) | 6 (13.0) |
| Liver | 7 (11.1) | 4 (21.0) | 3 (18.7) | 7 (21.2) | 3 (8.1) | 3 (16.7) | 4 (25.0) | 8 (17.4) |
| Brain | 3 (4.8) | 1 (5.3) | 2 (12.5) | 4 (12.1) | 2 (5.4) | 0 | 0 | 5 (10.9) |
| Gastrointestinal tract | 1 (1.6) | 1 (5.3) | 2 (12.5) | 1 (3.0) | 1 (2.7) | 1 (5.5) | 0 | 3 (6.5) |
| Other | 3 (4.8) | 1 (5.3) | 0 | 1 (3.0) | 1 (2.7) | 1 (5.5) | 0 | 1 (2.2) |
Ki67 index
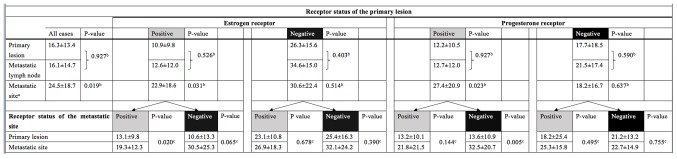
Overall, the mean Ki67 index of recurrent lesions was significantly greater than that of primary lesions (P=0.019). However, Ki67 index of synchronous metastatic lymph nodes exhibited almost the same value with that of primary lesions (P=0.927). This trend was only observed for patients with positive hormone receptor status in their primary lesion. By contrast, the Ki67 index of patients who had primary lesions that were hormone receptor negative did not change significantly with metastasis, which may indicate that hormone-negative tumors maintain high proliferative activity. Regarding changes in the Ki67 index with respect to changes in hormone receptor status, the Ki67 index of patients with primary lesions that were hormone receptor-positive exhibited increased proliferative activity with metastasis, but not in patients with primary lesions that were hormone receptor-negative (Fig. 1).
Figure 1.
Changes in the Ki67 index by hormone receptor status in primary and metastatic lesions. All values are presented as means ± standard deviation. aStatistical analyses between the primary lesion and the metastatic sites; bStudent's t-test; cMann-Whitney U test.
Overall survival
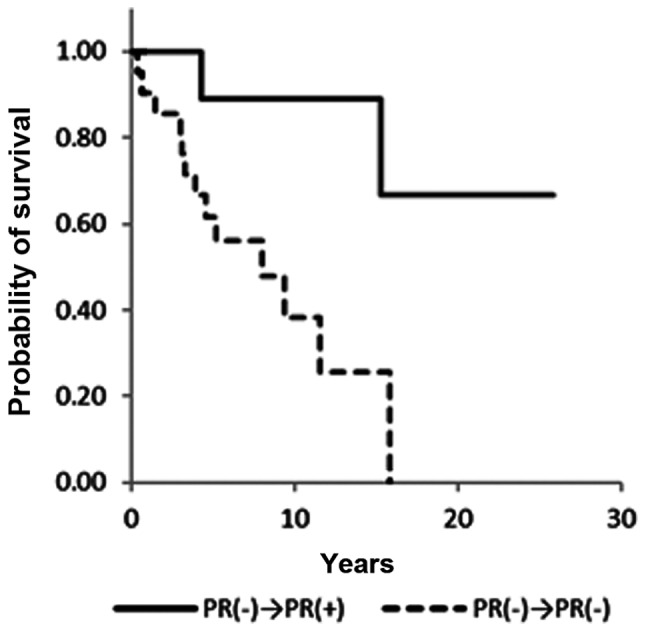
A significant difference in overall survival was observed between ER+/+ and ER+/− patients [hazard ratio (HR), 0.29; 95% confidence interval (CI), 0.12–0.73; P=0.008] and PR+/+ and PR+/− patients (HR, 0.12; 95% CI 0.03–0.43; P=0.001) (Figs. 2 and 3; Table III). ER−/+ and PR−/+ conversion was not associated with a significant difference in overall survival (Figs. 4 and 5). Notably, no statistical differences in overall survival were identified between the ER+/+ and ER−/+ groups (data not shown). Positive conversion from negative hormone receptor status in the primary lesion to positive status in the metastatic lesion improved overall survival (Table III).
Figure 2.
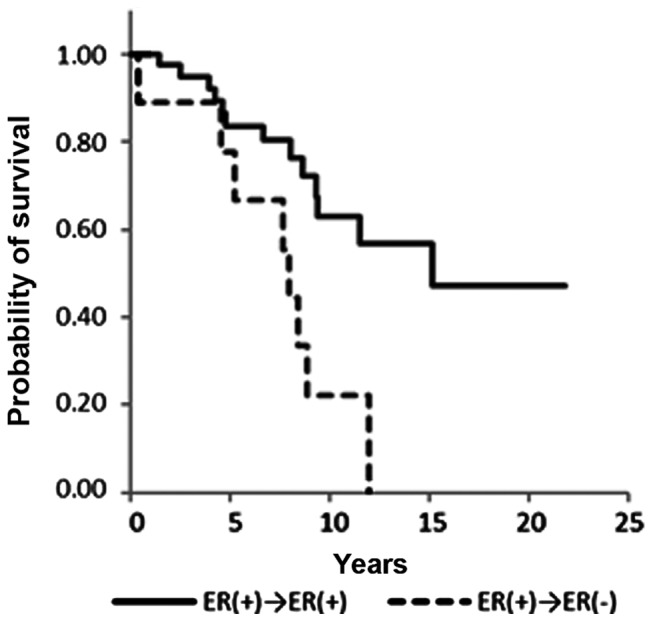
Survival curves of patients with recurrent breast cancer according to ER status. The figure represents patients in whom the primary tumor was positive for ER, according to the ER status of the metastatic site. ER, estrogen receptor.
Figure 3.
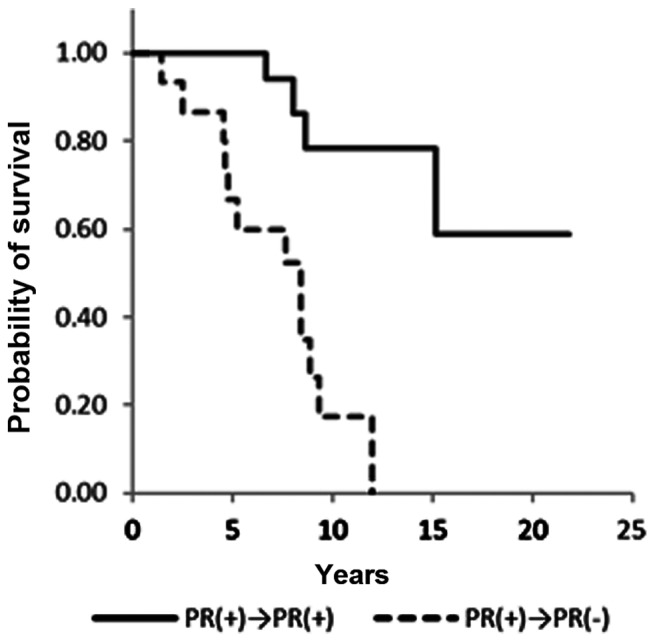
Survival curves of patients with recurrent breast cancer according to PR status. The figure represents patients in whom the primary tumor was positive for PR, according to the PR status of the metastatic site. PR, progesterone receptor.
Table III.
Log-rank test and Cox proportional HRs for overall survival.
| Receptor status | ||||||
|---|---|---|---|---|---|---|
| Primary tumor | Metastatic tumor | Disease-free interval Means ± SE (years) | Overall survival Means ± SE (years) | P-value | HR (95% CI) | P-value |
| Estrogen receptor | ||||||
| Positive | Positive | 5.4±0.8 | 14.8±1.4 | 0.005 | 1 | 0.008 |
| Negative | 4.1±1.2 | 7.4±1.2 | 3.44 (1.36–8.33) | |||
| Negative | Positive | 6.5±2.6 | 15.3±3.7 | 0.542 | 1 | 0.544 |
| Negative | 2.7±0.6 | 10.8±1.7 | 1.56 (0.38–6.66) | |||
| Progesterone receptor | ||||||
| Positive | Positive | 6.0±1.0 | 17.5±1.7 | 0.000 | 1 | 0.001 |
| Negative | 3.7±0.0 | 7.3±0.8 | 8.33 (2.32–33.3) | |||
| Negative | Positive | 7.7±2.1 | 19.3±3.6 | 0.116 | 1 | 0.018 |
| Negative | 2.7±0.0 | 9.6±1.4 | 6.66 (1.36–33.3) | |||
HR, hazard ratio; SE, standard error; CI, confidence interval.
Figure 4.
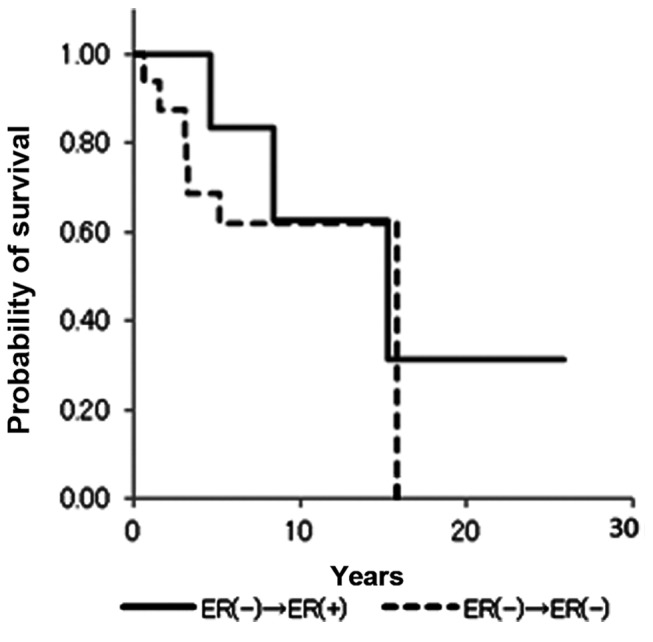
Survival curves of patients in whom the primary tumor was negative for ER. ER, estrogen receptor.
Figure 5.
Survival curves of patients in whom the primary tumor was negative for PR. PR, progesterone receptor.
HER2 status
A total of 12 patients (17.1%) exhibited positivity for HER2 in the primary lesion. For the metastatic lesion, 19 patients (27.1%), including 7 patients whose HER2 expressions were negative in the primary lesions, exhibited overexpression of HER2 (data not shown). Therefore, a total of 7 patients (10.0%) exhibited increases in HER2 expression levels from 0, 1+ or 2+ in the primary lesion to 3+ or FISH score >2 in the metastatic lesion (Table IV). No downregulation of HER2 expression was observed in the present study, whereas Niikura et al (13) previously observed loss of HER2 in 24% of 182 metastatic breast cancer cases. The location of recurrence in these seven patients included loco-regional sites, bone, lung and liver. The mean Ki67 index of the primary lesion was 13.6±10.8 and that of the metastatic site was 15.1±15.9 (P=0.406, Mann-Whitney U test). The mean overall survival of these patients was 8.4±2.6 years, which is similar to the survival of patients with negative conversion, particularly ER+/− and PR+/−.
Table IV.
Changes in HER2 status.
| Primary tumor | Metastatic tumor | |||||
|---|---|---|---|---|---|---|
| Age at initial surgery (years) | Pathology | Hormone receptor status (ER, PR) | Hormonal status HER2 status | (ER, PR) | HER2 status | |
| 77 | Invasive ductal carcinoma | ER(+)/PR(+) | 1+ | ER(+)/PR(+) | 3+ | |
| 34 | Invasive ductal carcinoma | ER(+)/PR(+) | 1+ | ER(+)/PR(+) | 3+ | |
| 66 | Invasive ductal carcinoma | ER(+)/PR(+) | 0 | ER(+)/PR(−) | 3+ | |
| 52 | Invasive micropapillary carcinoma | ER(+)/PR(−) | 1+ | ER(−)/PR(−) | 3+ | |
| 31 | Invasive ductal carcinoma | ER(−)/PR(+) | 1+ | ER(+)/PR(−) | 3+ | |
| 40 | Invasive ductal carcinoma | ER(+)/PR(+) | 2+ (1.03)a | ER(+)/PR(+) | 3+ | |
| 50 | Invasive ductal carcinoma | ER(+)/PR(+) | 1+ | ER(−)/PR(−) | 2+ (2.23)a | |
Value in parentheses indicate the fluorescence in situ hybridization score; HER2, human epidermal growth factor 2; ER, estrogen receptor; PR, progesterone receptor.
Discussion
When considering the treatment strategy for patients with metastatic breast cancer, oncologists are eager to achieve an adequate antitumor effect while maintaining a high quality of life for the patient. Chemotherapy, hormonal therapy or radiotherapy may be the treatment of choice. Personalized treatment strategies are presently required, with clinicians making meticulous treatment plans that take into account the tumor phenotype. Various studies have reported that the receptor status of metastatic breast cancer may differ from that of the primary tumor (1–4). Aitken et al (14) reported that metastatic lymph node receptor status may be a more accurate parameter for guiding adjuvant therapy. Thus, it is necessary to understand the alterations in tumor phenotype for further therapeutic decision making.
In the present study, hormone receptor and HER2 status conversion were assessed at recurrence. In approximately 20–40% of cases, hormone receptor status conversion was observed. Conversion from positive to negative status was associated with a significantly worse overall survival (HR, 3.44; 95%CI, 1.36–8.33; P=0.008 for ER and HR, 8.33; 95% CI, 2.32–33.3; P=0.001 for PR). The difference in HR may be due to biological differences between ER and PR. Strong ER expression is associated with good response to hormonal treatment and strong PR expression favors survival, particularly in patients who are also ER positive (15,16). The Kaplan-Meier curves in the present study demonstrate that PR status is closely correlated with overall survival (Figs. 2 and 4). PR−/+ conversion appears to improve overall survival. Observing larger cohorts of metastatic or recurrent breast cancer patients with longer follow-up may demonstrate that the PR-/+ group significantly differs in survival when compared with the PR-/- group. Discordance of HER2 status was observed only in seven patients (10%) in the present study. The discordance rate ranges from 14 to 17% across studies (17,18). Six patients in the present study received intensive chemotherapy, including taxane and anthracycline, before changes in HER2 status were recognized. The etiology of hormone receptor and HER2 status discordance remains unknown. A variety of adjuvant treatments that were administered following initial surgery may have influenced the hormone receptor and HER2 status. The most plausible hypothesis is that the distribution of cancer cell types was altered, as chemo- and/or hormone-sensitive tumor cells were eliminated by certain types of treatment. Yang et al (19) demonstrated that chemo-sensitive tumor cells were targeted and killed in the setting of neoadjuvant chemotherapy; consequently, insensitive tumor cells with different biological properties survived in the residual lesion prior to surgery. Furthermore, Keen et al (20) revealed that tumor progression may induce genetic drift and also treatment-associated clone selection. For example, ER-negative cancer cells generally respond to chemotherapy better than ER-positive cancer cells. The chemotherapeutic agents preferentially eliminate chemo-sensitive cancer cells, such as ER-negative tumor cells and consequently the nest of breast cancer cells is rearranged into the new nest consisting of ER-positive dominant cancer cells (21). Niikura et al (13) reported that the discordance of HER2 status between primary and metastatic tumor sites increased following chemotherapy. However, hormonal treatment may induce receptor discordance at the metastatic sites. It remains controversial as to whether endocrine therapy with tamoxifen may influence the receptor discordance of the metastatic tumors. Johnston et al (22) demonstrated the ER expression levels in metastatic tumors were significantly reduced in the patients that had undergone tamoxifen treatment prior to cancer recurrence, whereas other studies identified that no significant correlation was observed between endocrine therapy and ER discordance rate (23,24). In the present study, only two cases received tamoxifen treatment alone as an adjuvant setting prior to recurrence. Almost all the patients experienced adjuvant chemotherapy postoperatively. Unfortunately, the effect of tamoxifen on the receptor discordance cannot be discussed using the present data due to the lack of applicable patients. In the present study, PR expression levels are reduced with the metastasis in 55% of ER+/− conversion and 5.1% of ER+/+. It is comprehensible that the downregulation of PR occurs concomitantly with the reduction of ER expression levels in the metastatic sites, as ER regulates PR expression levels. For the two cases (5.1%) that demonstrated reduced PR expression with ER+/+ conversion, the influence of growth factors may be considered. It has been reported that the phosphatidylinositol-3 kinase/Akt signaling pathway, which is occasionally activated in metastatic breast cancer cells, may deactivate PR expression, as the application of inhibitors for this signaling pathway may reverse PR downregulation (25).
The Ki67 index generally increases with metastasis or recurrence. In the present study, the Ki67 index of metastatic lesions was significantly upregulated when compared with that of the primary lesions. Notably, this trend was observed in patients with primary lesions that were hormone receptor-positive. The Ki67 index of patients who were hormone receptor-negative remained high during the life of the tumor, indicating high levels of proliferative activity.
There were certain limitations of the present study. A biopsy of recurrent tumors was performed at the discretion of the treating physicians. However, to assess recurrent tumors, a biopsy of the first recurrent site must be performed. Furthermore, the biopsy specimen of a recurrent tumor may not fully represent all of its biological features. As metastatic spread of breast cancer typically occurs systemically, a biopsy of all recurrent tumors is difficult due to limited accessibility.
In conclusion, the biological features of metastatic breast cancer may differ from those of primary breast cancer. When a recurrent tumor loses hormone receptor positivity, survival may be substantially worsened. To establish an appropriate treatment plan for a patient with recurrent disease, a biopsy of the recurrent tumor should be mandatory if access is feasible.
References
- 1.Holdaway IM, Bowditch JV. Variation in receptor status between primary and metastatic breast cancer. Cancer. 1983;52:479–485. doi: 10.1002/1097-0142(19830801)52:3<479::AID-CNCR2820520317>3.0.CO;2-O. [DOI] [PubMed] [Google Scholar]
- 2.Hull DF, III, Clark GM, Osborne CK, Chamness GC, Knight WA, III, McGuire WL. Multiple estrogen receptor assays in human breast cancer. Cancer Res. 1983;43:413–416. [PubMed] [Google Scholar]
- 3.Li BD, Byskosh A, Molteni A, Duda RB. Estrogen and progesterone receptor concordance between primary and recurrent breast cancer. J Surg Oncol. 1994;57:71–77. doi: 10.1002/jso.2930570202. [DOI] [PubMed] [Google Scholar]
- 4.Shimizu C, Fukutomi T, Tsuda H, Akashi-Tanaka S, Watanabe T, Nanasawa T, Sugihara K. c-erbB-2 protein overexpression and p53 immunoreaction in primary and recurrent breast cancer tissues. J Surg Oncol. 2000;73:17–20. doi: 10.1002/(SICI)1096-9098(200001)73:1<17::AID-JSO5>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 5.Kumar SK, Gupta N, Rajwanshi A, Joshi K, Singh G. Immunochemistry for oestrogen receptor, progesterone receptor and HER2 on cell blocks in primary breast carcinoma. Cytopathology. 2012;23:181–186. doi: 10.1111/j.1365-2303.2011.00853.x. [DOI] [PubMed] [Google Scholar]
- 6.The World Health Organization: Histological typing of breasr tumors. Neoplasma. 1983;30:113–123. [PubMed] [Google Scholar]
- 7.Sobin LH, Witterkind C, editors. TNM Classification of Malignant Tumours. 6th edition. Wiley; New York: 2002. pp. 131–141. [Google Scholar]
- 8.Allred DC, Harvey JM, Berardo M, Clark GM. Prognostic and predictive factors in breast cancer by immunohistochemical analysis. Mod Pathol. 1998;11:155–168. [PubMed] [Google Scholar]
- 9.Hammond ME, Hayes DF, Dowsett M, Allred DC, Hagerty KL, Badve S, Fitzgibbons PL, Francis G, Goldstein NS, Hayes M, et al. American Society of Clinical Oncology/College Of American Pathologists guideline recommendations for immunohistochemical testing of estrogen and progesterone receptors in breast cancer. J Clin Oncol. 2010;28:2784–2795. doi: 10.1200/JCO.2009.25.6529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wolff AC, Hammond ME, Schwartz JN, Hagerty KL, Allred DC, Cote RJ, Dowsett M, Fitzgibbons PL, Hanna WM, Langer A, et al. American Society of Clinical Oncology; College of American Pathologists: American Society of Clinical Oncology/College of American Pathologists guideline recommendations for human epidermal growth factor receptor 2 testing in breast cancer. J Clin Oncol. 2007;25:118–145. doi: 10.1200/JCO.2006.09.2775. [DOI] [PubMed] [Google Scholar]
- 11.Dowsett M, Nielsen TO, A'Hern R, Bartlett J, Coombes RC, Cuzick J, Ellis M, Henry NL, Hugh JC, Lively T, et al. International Ki-67 in breast cancer working group: Assessment of Ki67 in breast cancer: Recommendations from the International Ki67 in breast cancer working group. J Natl Cancer Inst. 2011;103:1656–1664. doi: 10.1093/jnci/djr393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gerdes J, Lemke H, Baisch H, Wacker HH, Schwab U, Stein H. Cell cycle analysis of a cell proliferation-associated human nuclear antigen defined by the monoclonal antibody Ki-67. J Immunol. 1984;133:1710–1715. [PubMed] [Google Scholar]
- 13.Niikura N, Liu J, Hayashi N, Mittendorf EA, Gong Y, Palla SL, Tokuda Y, Gonzalez-Angulo AM, Hortobagyi GN, Ueno NT. Loss of human epidermal growth factor receptor 2 (HER2) expression in metastatic sites of HER2-overexpressing primary breast tumors. J Clin Oncol. 2012;30:593–599. doi: 10.1200/JCO.2010.33.8889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Aitken SJ, Thomas JS, Langdon SP, Harrison DJ, Faratian D. Quantitative analysis of changes in ER, PR and HER2 expression in primary breast cancer and paired nodal metastases. Ann Oncol. 2010;21:1254–1261. doi: 10.1093/annonc/mdp427. [DOI] [PubMed] [Google Scholar]
- 15.Liu S, Chia SK, Mehl E, Leung S, Rajput A, Cheang MCU, Nielsen TO. Progesterone receptor is a significant factor associated with clinical outcomes and effect of adjuvant tamoxifen therapy in breast cancer patients. Breast Cancer Res Treat. 2010;119:53–61. doi: 10.1007/s10549-009-0318-0. [DOI] [PubMed] [Google Scholar]
- 16.Purdie CA, Quinlan P, Jordan LB, Ashfield A, Ogston S, Dewar JA, Thompson AM. Progesterone receptor expression is an independent prognostic variable in early breast cancer: A population-based study. Br J Cancer. 2014;110:565–572. doi: 10.1038/bjc.2013.756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nishimura R, Osako T, Okumura Y, Tashima R, Toyozumi Y, Arima N. Changes in the ER, PgR, HER2, p53 and Ki-67 biological markers between primary and recurrent breast cancer: Discordance rates and prognosis. World J Surg Oncol. 2011;9:131. doi: 10.1186/1477-7819-9-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ibrahim T, Farolfi A, Scarpi E, Mercatali L, Medri L, Ricci M, Nanni O, Serra L, Amadori D. Hormonal receptor, human epidermal growth factor receptor-2, and Ki67 discordance between primary breast cancer and paired metastases: Clinical impact. Oncology. 2013;84:150–157. doi: 10.1159/000345795. [DOI] [PubMed] [Google Scholar]
- 19.Yang YF, Liao YY, Li LQ, Xie SR, Xie YF, Peng NF. Changes in ER, PR and HER2 receptors status after neoadjuvant chemotherapy in breast cancer. Pathol Res Pract. 2013;209:797–802. doi: 10.1016/j.prp.2013.08.012. [DOI] [PubMed] [Google Scholar]
- 20.Keen JC, Davidson NE. The biology of breast carcinoma. Cancer. 2003;97(Suppl):825–833. doi: 10.1002/cncr.11126. [DOI] [PubMed] [Google Scholar]
- 21.Gong Y, Han EY, Guo M, Pusztai L, Sneige N. Stability of estrogen receptor status in breast carcinoma: A comparison between primary and metastatic tumors with regard to disease course and intervening systemic therapy. Cancer. 2011;117:705–713. doi: 10.1002/cncr.25506. [DOI] [PubMed] [Google Scholar]
- 22.Johnston SRD, Saccani-Jotti G, Smith IE, Salter J, Newby J, Coppen M, Ebbs SR, Dowsett M. Changes in estrogen receptor, progesterone receptor, and pS2 expression in tamoxifen-resistant human breast cancer. Cancer Res. 1995;55:3331–3338. [PubMed] [Google Scholar]
- 23.Broom RJ, Tang PA, Simmons C, Bordeleau L, Mulligan AM, O'Malley FP, Miller N, Andrulis IL, Brenner DM, Clemons MJ. Changes in estrogen receptor, progesterone receptor and Her-2/neu status with time: Discordance rates between primary and metastatic breast cancer. Anticancer Res. 2009;29:1557–1562. [PubMed] [Google Scholar]
- 24.Lower EE, Glass EL, Bradley DA, Blau R, Heffelfinger S. Impact of metastatic estrogen receptor and progesterone receptor status on survival. Breast Cancer Res Treat. 2005;90:65–70. doi: 10.1007/s10549-004-2756-z. [DOI] [PubMed] [Google Scholar]
- 25.Cui X, Schiff R, Arpino G, Osborne CK, Lee AV. Biology of progesterone receptor loss in breast cancer and its implications for endocrine therapy. J Clin Oncol. 2005;23:7721–7735. doi: 10.1200/JCO.2005.09.004. [DOI] [PubMed] [Google Scholar]