INTRODUCTION
The cost-benefit ratio of routine pre-operative investigations is not favourable, and the traditional practice of ordering routine pre-operative tests before elective surgery is not recommended.[1,2] Evidence suggests that pre-operative tests are not associated with decreased mortality or better outcomes.[3] However, the practice of routine pre-operative tests before elective surgery has remained widely prevalent.[4,5] Health-care practices not only depend on practitioners' knowledge but also on the local laws, protocols, administrative policies, etc. The present study was aimed to assess the reasons behind this continued practice.
METHODS
A cross-sectional survey was conducted using free online survey software and questionnaire tool service from SurveyMonkey® (SurveyMonkey Inc., US, https://www.surveymonkey.com). The study sample was calculated with a hypothesised frequency of outcome ‘practice of routine pre-operative testing’ (65 + 10%) with a design effect of 1.4 which gave a sample size of 123 for 95% confidence level. To cope up with the non–responder, 100% add-on was done making the sample size 246. Totally 255 qualified anaesthesiologists and surgeons of different surgical disciplines from both public and corporate sectors, practising in more than 70 set-ups across India, were approached through e-mail during December 25, 2016–January 30, 2017. A questionnaire containing 5 simple questions with multiple choices.was prepared. The reasons given as options were however mostly taken from a previously conducted study with similar objectives.[6] The questions with binominal data (options) were based on current recommendations and guidelines.[1,2] This was however not validated beforehand. The responses of the entire cohort were expressed in absolute number and percentage scale. The responses of anaesthesiologists and surgeons were screened and compared by Fisher's exact test using INSTAT software (GraphPad software Inc., La Jolla, CA, USA). P <0.05 was considered statistically significant.
RESULTS
Twenty-one (8.24%) of the e-mails bounced and two (0.78%) recipients opted out from the survey. Seventy-one (30.6%) recipients responded to the e-mail invitation; 43 (60.56%) were anaesthesiologists. Fifty-eight respondents (34 [58.62%] anaesthesiologists and 24 [41.38%] surgeons) associated with 36 hospitals across India completed the questionnaire. The incomplete responses were excluded from the analysis as they responded only about their speciality.
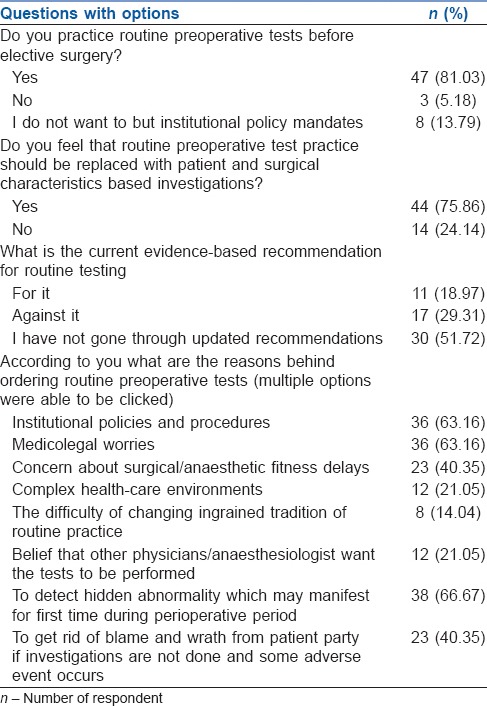
Fifty-five (94.82%) respondents were practising routine pre-operative tests while only 29.31% knew that the current recommendations were against routine pre-operative laboratory tests [Table 1]. Among the reasons cited for ordering routine pre-operative laboratory tests, detection of hidden abnormality which may manifest for the first time during perioperative period was the most common reason (66.67%) [Table 1].
Table 1.
Responses of the entire cohort expressed in absolute number and percentage scale (n=58)
The routine practices were higher among surgeons than anaesthesiologists (95.83% vs. 70.59%; P = 0.018). Anaesthesiologists were more updated with the current evidence and recommendations as compared to surgeons {47.06% versus 8.33%, relative risk (95% confidence of 1.97 (1.35–2.88); P = 0.001)}.
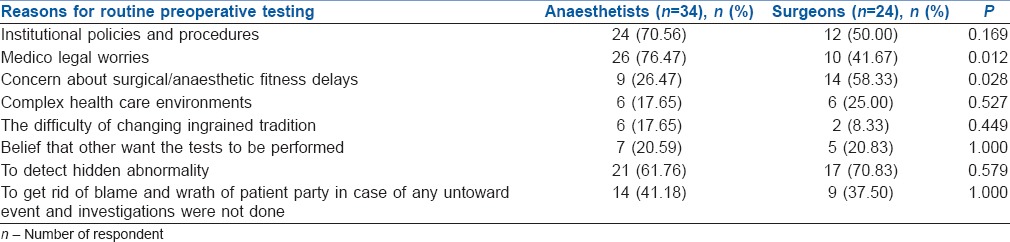
Although there was a good agreement between anaesthesiologists and surgeons for the different reasons cited for continued routine practice, the most common reasons for practising routine pre-operative testing were different among anaesthesiologists and surgeons [Table 2].
Table 2.
Reasons cited for continued routine preoperative testing and comparison using Fisher's exact test (total number)
DISCUSSION
Our study found that only 5.18% of the participants did not prescribe routine pre-operative tests, despite the existence of recommendations to the contrary being available for nearly 15 years.[7] This indicates that the guidelines have failed to convince the practitioners. One of the reasons may be the practitioner's apprehensions and practice environment.
Majority (51.7%) of respondents were not updated with the current recommendations, and nearly one-fifth were not even aware of these recommendations. This indicates that lack of updated information is a contributor to the continued practice. However, the finding that 47.06% practitioners, despite being aware were not willing to follow the recommendations due to the institutes' protocol, indicates that practitioners are not solely responsible. This is reinforced by another finding of the present survey where 75.86% of the practitioners think that the routine testing should be replaced with patient characteristic-based investigations. Selective testing has shown to reduce consultations, delays and cancellations.[8] American Society of Anesthesiologists also supported testing based on risk assessment and opposed to the routine approach.[9]
The most common reason stated by the participants was to detect a hidden abnormality. A study reviewing data of 46,977 patients from a national database who underwent routine pre-operative testing found that neither laboratory testing nor abnormal results were associated with post-operative complications.[10] Even abnormal test values found in routine testing among elderly patients failed to predict post-operative complications.[3] Analysing data from Mayo clinic, it was found that even though routine testing found hidden abnormalities yet, it was possible to eliminate these tests without changing outcomes.[11]
Two of top three reasons were associated with the administration and law which indicates that even if all the practitioners are updated with knowledge and willing to abandon routine testing, it may still not be be possible to eliminate this practice. The current wide prevalence of violence and wrath of patients and their families may also a major contributor. Institutional norms, law and government have their role to play. A previous study conducted with nearly same aims in 2011 had findings similar to our study.[6]
Anaesthesiologists were more informed and updated with the current recommendations.
Although the study was designed to get adequate power, the non-responders were much more than assumed (70%) leading to relatively underpowered study. The average response rate for online survey is nearly 33%; in the present study, the response rate was 30%.[12]
Representatives were also from a relatively smaller number of institutes. However, although these issues are limitations of our study, the present survey can serve as a pilot to prepare our further action plan. A nationwide survey can give more accurate values.
CONCLUSION
Knowledge of the current recommendations is greater among anaesthesiologists than surgeons. Routine pre-operative testing practice is very much prevalent both among anaesthesiologists and surgeons. The most common reason for routine testing is to detect a hidden abnormality. Medicolegal worries, institutional policy and worsening patient–doctor relationship are also important reasons for the routine preoperative tests.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
I would like to thank all the respondents who spared their valuable time to take this survey.
REFERENCES
- 1.National Guideline Centre (UK) Preoperative Tests (Update): Routine Preoperative Tests for Elective Surgery. London: National Institute for Health and Care Excellence (UK); 2016. [Last accessed on 2016 Jul 22]. Available from: https://www.nice.org.uk/guidance/ng45/chapter/recommendations . [PubMed] [Google Scholar]
- 2.Committee on Standards and Practice Parameters; American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Apfelbaum JL, Connis RT, Nickinovich DG, Pasternak LR, et al. Practice advisory for preanesthesia evaluation: An updated report by the American society of anesthesiologists task force on preanesthesia evaluation. Anesthesiology. 2012;116:522–38. doi: 10.1097/ALN.0b013e31823c1067. [DOI] [PubMed] [Google Scholar]
- 3.Dzankic S, Pastor D, Gonzalez C, Leung JM. The prevalence and predictive value of abnormal preoperative laboratory tests in elderly surgical patients. Anesth Analg. 2001;93:301–8. doi: 10.1097/00000539-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Karim HM, Yunus M, Bhattacharyya P. An observational cohort study on pre-operative investigations and referrals: How far are we following recommendations>. Indian J Anaesth. 2016;60:552–9. doi: 10.4103/0019-5049.187783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Keshavan VH, Swamy CM. Pre-operative laboratory testing: A prospective study on comparison and cost analysis. Indian J Anaesth. 2016;60:838–42. doi: 10.4103/0019-5049.193678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown SR, Brown J. Why do physicians order unnecessary preoperative tests? A qualitative study. Fam Med. 2011;43:338–43. [PubMed] [Google Scholar]
- 7.National Collaborating Centre for Acute Care (UK) Preoperative Tests: The Use of Routine Preoperative Tests for Elective Surgery – Evidence, Methods and Guidance. London: National Institute of Clinical Excellence; 2003. [Last accessed on 2016 Jul 22]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK48489/ [PubMed] [Google Scholar]
- 8.Fischer SP. Development and effectiveness of an anesthesia preoperative evaluation clinic in a teaching hospital. Anesthesiology. 1996;85:196–206. doi: 10.1097/00000542-199607000-00025. [DOI] [PubMed] [Google Scholar]
- 9.Pasternak LR, Arens JF, Caplan RA, Connis RT, Fleisher LA, Flowerdew R, et al. Practice advisory for preanesthesia evaluation: A report by the American Society of Anesthesiologists Task Force on preanesthesia evaluation. Anesthesiology. 2002;96:485–96. [Google Scholar]
- 10.Benarroch-Gampel J, Sheffield KM, Duncan CB, Brown KM, Han Y, Townsend CM, Jr, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518–28. doi: 10.1097/SLA.0b013e318265bcdb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Narr BJ, Hansen TR, Warner MA. Preoperative laboratory screening in healthy mayo patients: Cost-effective elimination of tests and unchanged outcomes. Mayo Clin Proc. 1991;66:155–9. doi: 10.1016/s0025-6196(12)60487-x. [DOI] [PubMed] [Google Scholar]
- 12.Nulty DD. The adequacy of response rates to online and paper surveys: What can be done? Assess Eval High Educ. 2008;33:301–14. [Google Scholar]


