Significance
Immunosuppression by regulatory T cells (Tregs) is essential for the maintenance of self-tolerance, but it is detrimental in cancer because Tregs inhibit antitumor immunity. Development of therapeutic tools to block Tregs in patients with cancer requires a precise understanding of how human Tregs suppress immune responses. We recently identified an important mechanism implicating release of the active form of TGF-β1, a potently immunosuppressive cytokine, from GARP/latent TGF-β1 complexes on the surface of human Tregs. Here we unravel the molecular process leading to this release. We identify integrin αVβ8 as indispensable for TGF-β1 activation from GARP/latent TGF-β1 complexes. We show that anti-β8 monoclonals block immunosuppression by human Tregs in vivo and could thus serve in cancer immunotherapy.
Keywords: GARP (LRRC32), integrin αVβ8, human regulatory T cells, TGF-β, cancer immunotherapy
Abstract
Human regulatory T cells (Tregs) suppress other T cells by converting the latent, inactive form of TGF-β1 into active TGF-β1. In Tregs, TGF-β1 activation requires GARP, a transmembrane protein that binds and presents latent TGF-β1 on the surface of Tregs stimulated through their T cell receptor. However, GARP is not sufficient because transduction of GARP in non-Treg T cells does not induce active TGF-β1 production. RGD-binding integrins were shown to activate TGF-β1 in several non-T cell types. Here we show that αVβ8 dimers are present on stimulated human Tregs but not in other T cells, and that antibodies against αV or β8 subunits block TGF-β1 activation in vitro. We also show that αV and β8 interact with GARP/latent TGF-β1 complexes in human Tregs. Finally, a blocking antibody against β8 inhibited immunosuppression by human Tregs in a model of xenogeneic graft-vs.-host disease induced by the transfer of human T cells in immunodeficient mice. These results show that TGF-β1 activation on the surface of human Tregs implies an interaction between the integrin αVβ8 and GARP/latent TGF-β1 complexes. Immunosuppression by human Tregs can be inhibited by antibodies against GARP or against the integrin β8 subunit. Such antibodies may prove beneficial against cancer or chronic infections.
Regulatory T cells (Tregs) are a subset of CD4+ T lymphocytes that are specialized in the suppression of immune responses. They are essential for the maintenance of peripheral immunological tolerance, but detrimental in cancer or chronic infections (1). Manipulation of Treg numbers or function is a therapeutic approach explored for several diseases. It has faced limited success thus far, notably because the mechanisms by which human Tregs suppress immune responses are still largely unknown (2).
A variety of Treg suppressive mechanisms have been identified in murine models and include production of soluble immunosuppressive cytokines, reduction of the T cell-stimulatory capacity of antigen presenting cells, transfer of cAMP to effector T cells through GAP junctions, or increased production of adenosine (1). The importance of any one mechanism may depend on the type or class of immune response to suppress and may vary according to environmental cues (1, 3). Which of these mechanisms, if any, plays a major role in humans is not known.
We recently proposed that the production of active TGF-β1 is a dominant mechanism of immunosuppression by human Tregs in vivo. This hypothesis is based on observations in a humanized mouse model in which the xenogeneic graft-vs.-host disease (GVHD; xGVHD) induced by the transfer of human peripheral blood mononuclear cells (PBMCs) into immunodeficient mice can be suppressed by cotransfer of autologous Tregs. In this model, monoclonal antibodies that block active TGF-β1 production by Tregs, but not by other cells, inhibited immunosuppression by human Tregs (4).
TGF-β1 is a potent immunosuppressive cytokine that also exerts many actions outside the immune system. Most cells produce inactive forms of TGF-β1, but a few are known to activate the cytokine via tightly regulated mechanisms that are cell type-specific. In all cells, homodimerization of the TGFB1 gene product yields pro–TGF-β1, further cleaved to produce latent TGF-β1. In latent TGF-β1, the C-terminal fragment, or mature TGF-β1, remains noncovalently bound to the N-terminal fragment known as the latency associated peptide or LAP. All immune cells secrete latent TGF-β1, which is inactive because LAP prevents mature TGF-β1 from binding to its receptor (5). Further processing, referred to as TGF-β1 activation, is required to release mature TGF-β1 from LAP, allow binding of the cytokine to its receptor, and initiate a signaling cascade via phosphorylation of the SMAD2 and SMAD3 transcription factors. It should be noted that two other TGF-β isoforms (TGF-β2 and TGF-β3) can be produced by human cells via a similar mechanism. However, human Tregs express the TGFB1 gene but do not express TGFB2 or TGFB3 (Fig. S1). Thus, all references to TGF-β production by Tregs in the present study deal only with products of the TGFB1 gene and the TGF-β1 isoform (i.e., pro-TGF-β1, latent TGF-β1, mature TGF-β1, and LAP, which is sometimes referred to as β1-LAP).
How human Tregs activate TGF-β1 is not completely understood. We and others showed that Tregs display latent TGF-β1 on their surface via disulfide linkage of LAP to a transmembrane protein called GARP (6–9). We obtained antibodies against GARP/latent TGF-β1 complexes that block TGF-β1 activation and immunosuppression by human Tregs in vitro and in vivo (4). GARP is therefore required for TGF-β1 activation by human Tregs. However, it is not sufficient: transduction of GARP in non-Treg T cells leads to presentation of latent TGF-β1 on the cell surface, but not to its activation (7). This suggests that at least one additional, as yet unidentified Treg protein is required for TGF-β1 activation by human Tregs.
Several proteins were shown to mediate TGF-β1 activation in non-Treg cell types, and include surface integrins that bind RGD motifs in their ligands or extracellular proteins such as Thrombospondin or proteases of the matrix metalloproteinase (MMP) family (10). RGD-binding integrins represent the most evolutionary conserved TGF-β1 activators with the best-established roles in vivo (10). Integrins are surface heterodimeric proteins composed of noncovalently associated α and β membrane–spanning subunits. They mediate cell adhesion and cell-to-cell communications by binding ligands on other cells or in the ECM (11). There are 24 known human integrin heterodimers, eight of which bind RGD motifs in their ligands. Of these so-called RGD-binding integrins, αVβ1, αVβ6, and αVβ8 bind an RGD motif in LAP, activate latent TGF-β1 in vitro, and appear to play roles related to their TGF-β1–activating capacity in pathological conditions in vivo. Integrins αVβ1 and αVβ6 are expressed on fibroblasts and epithelial cells, respectively, and were mostly implicated in lung, pulmonary, and renal fibrosis (12–18). Expression of integrin αVβ8 was observed in epithelial cells, fibroblasts, neurons, and glial cells, as well as in dendritic cells (DCs) and CD4+ T cells. Conditional deletions of the Itgb8 gene in DCs, in glial cells, or in fibroblasts suggest that TGF-β1 activation mediated by integrin αVβ8 contributes to autoimmune colitis and encephalomyelitis, vascular development in the central nervous system, or pulmonary fibrosis and asthma, respectively (19–28). More recently, it was shown that murine Tregs express Itgb8, and that Itgb8−/− murine Tregs failed to activate TGF-β1 in vitro and to suppress ongoing autoimmune colitis in vivo (29, 30).
Here we set out to determine whether an RGD-binding integrin contributes to the GARP-mediated activation of TGF-β1 by human Tregs.
Results
An RGD-Binding Integrin Activates TGF-β1 on Human Tregs.
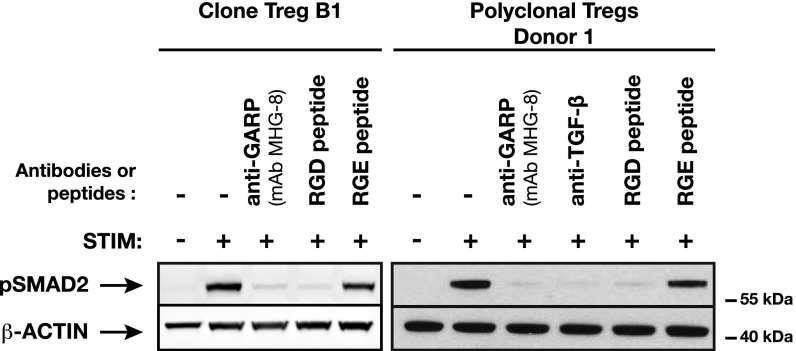
We examined whether the RGD-containing decapeptide GRRGDLATIH, derived from LAP and known to compete with LAP for binding to RGD-binding integrins (31), could inhibit TGF-β1 activation by human Tregs. As a source of human Tregs, we used Treg clones, i.e., pure populations of cells bearing a demethylated FOXP3i1 allele (32), or polyclonal blood CD4+CD25hiCD127lo cells that were shortly amplified in vitro and contained 46–98% of cells with a demethylated FOXP3i1 allele (Table S1). We assessed SMAD2 phosphorylation by Western blot to detect the autocrine activity of TGF-β1 produced by Tregs after T cell receptor (TCR) stimulation (Fig. 1). As expected, phosphorylated SMAD2 (pSMAD2) was detected in stimulated Tregs, but not in nonstimulated Tregs or in Tregs stimulated in the presence of blocking anti–TGF-β or anti-GARP antibodies (4). pSMAD2 was not detected in stimulated Tregs incubated with the RGD peptide, whereas it was readily detected in Tregs incubated with the control RGE-containing decapeptide (GRRGELATIH). These results indicate that an RGD-binding integrin is involved in the production of active TGF-β1 by human Tregs.
Fig. 1.
An RGD-containing peptide inhibits the production of active TGF-β1 by human Tregs. The indicated Treg cells were stimulated (STIM) or not with anti-CD3/CD28 antibodies in the presence of blocking antibodies (20 µg/mL) or peptides (230 µM), collected after 24 h, and analyzed by Western blot with antibodies against pSMAD2 or β-actin. Figure is representative of experiments performed with three different Treg clones and with polyclonal Tregs from three different donors.
Stimulated Human Tregs, but Not T Helper Cells, Express Integrin αVβ8.
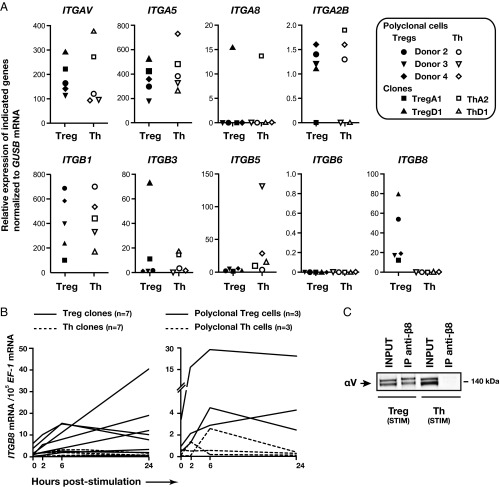
We next sought to determine which RGD-binding integrin contributes to latent TGF-β1 activation in human Tregs. Non-Treg CD4+ T cells [i.e., T helper (Th) cells] do not produce active TGF-β1, even when forced to express GARP by viral transduction (7). We therefore postulated that the RGD-binding integrin that activates TGF-β1 on human Tregs is not expressed or is expressed at very low levels in Th cells. RGD-binding integrins comprise integrins αVβ1, αVβ3, αVβ5, αVβ6, αVβ8, α5β1, α8β1, and αIIbβ3. We used a quantitative RT-PCR (RT-qPCR) array to measure levels of the mRNAs encoding the four α- and five β-subunits of these integrins in stimulated Treg and Th cells. As shown in Fig. 2A, genes encoding the α-subunits were not differentially expressed in Tregs compared with Th cells: mRNAs ITGA5 and ITGAV (encoding the α5 and αV subunits, respectively) were present at high levels in Tregs and Th cells, whereas mRNAs ITGA8 and ITGA2B (encoding the α8 and αIIb subunits) were absent or present at very low levels in both cell types. Similar to genes encoding the α-subunits, most genes encoding the β-subunits were not differentially expressed in Tregs compared with Th cells. More particularly, mRNA ITGB1 (encoding the β-subunit of integrin αVβ1, known to activate TGF-β in fibroblasts) was found at high levels in Tregs and Th cells, whereas mRNA ITGB6 (encoding the β-subunit of αVβ6, known to activate TGF-β in epithelial cells) was absent in both cell types. We confirmed the absence of ITGB6 expression with a different set of ITGB6-specific primers on an independently derived set of human Treg and Th cell samples collected at different time points after TCR stimulation (Table S2). However, the expression levels of gene ITGB8, encoding the β8 subunit, were at least 10–80 fold higher in stimulated Tregs than in stimulated Th cells. We confirmed these results with a different set of ITGB8-specific primers on an independently derived set of human Treg and Th cell samples (Fig. 2B). ITGB8 expression was up-regulated 24 h after TCR stimulation in 8 of 10 Treg cell clones or polyclonal populations, whereas it remained low at all time points in all 10 Th cell populations.
Fig. 2.
ITGB8 is expressed at higher levels in human Tregs compared with Th cells. (A) The indicated Treg and Th cells were stimulated with anti-CD3/CD28 antibodies during 24 h. Expression of the indicated genes and of housekeeping gene GUSB was analyzed by RT-qPCR. Values correspond to 1,000 × 2∆Ct, where ∆Ct = Ct [GUSB] − Ct [integrin subunit], and therefore represent copies of the indicated mRNA per 1,000 copies of the GUSB mRNA. (B) The indicated Treg and Th cells were stimulated with anti-CD3/CD28 antibodies and collected at various time points. Expression of ITGB8 and housekeeping gene EF-1 were analyzed by RT-qPCR. Values correspond to mRNA copy number as determined by using a standard curve. (C) Polyclonal Treg and Th cells from donor 6 were stimulated with anti-CD3/CD28 antibodies for 24 h. Cell lysates were immunoprecipitated with anti-integrin β8 mAb (mAb 37E1-B5). Total lysates (4% of input in IP) and IP products were analyzed by Western blot with an antibody against integrin αV subunit. Results are representative of three independent experiments.
The β8 subunit is only known to pair with the αV subunit, encoded by an mRNA also expressed in Tregs (Fig. 2A). Thus, we expected integrin αVβ8 dimers to be present on stimulated Tregs but not on Th cells. The αV subunit was readily detected on the surface of Th and Treg cells by flow cytometry (Fig. S2). However, we could not detect β8 on the surface of any type of T cells with the use of various anti-β8 antibodies. Detection of endogenous β8 levels by flow cytometry is notoriously difficult. As none of the available anti-β8 antibodies works in Western blot studies, we used anti-β8 antibodies to immunoprecipitate β8 from T cell lysates and then checked for the presence of αV in the IP products by Western blot. As shown in Fig. 2C, αV was coimmunoprecipitated with β8 in stimulated Tregs but not Th cells.
Altogether, these results show that αVβ8 is the only RGD-binding integrin expressed at higher levels in stimulated human Tregs compared with Th cells. Thus, αVβ8 could be the RGD-binding integrin that activates latent TGF-β1 in human Tregs.
Antibodies Against Integrin αVβ8 Block TGF-β1 Activation by Human Tregs in Vitro.
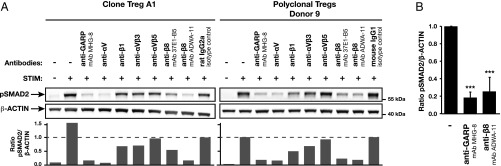
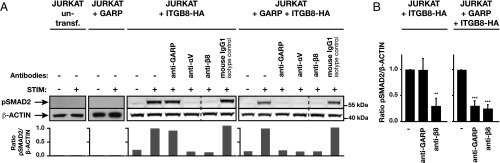
To test this hypothesis, we stimulated human Tregs in the presence or absence of blocking antibodies against RGD-binding integrin dimers or subunits and measured pSMAD2 by Western blot as a readout for active TGF-β1 production. Antibodies against the β1 subunit or the αVβ3 or αVβ5 dimers did not block active TGF-β1 production by human Tregs. In contrast, an antibody against the αV subunit, as well as one of two antibodies against the β8 subunit, blocked active TGF-β1 production as efficiently as a blocking anti-GARP antibody, taken here as a positive control (Fig. 3A). Blocking anti-β8 and anti-GARP mAbs inhibited active TGF-β1 production by 74 ± 16% and 81 ± 6%, respectively (Fig. 3B). TGF-β activation by integrin αVβ8 was shown in some cell types to depend on the recruitment of MMP-14 and the subsequent proteolytic degradation of LAP (31). However, neither the broad-spectrum MMP inhibitor GM6001 nor inhibitors of serine, aspartyl, and cysteine proteases blocked active TGF-β1 production by human Tregs (Fig. S3).
Fig. 3.
Active TGF-β1 production by human Tregs requires integrin αVβ8, but not αVβ1, αVβ3, or αVβ5 integrins. (A) The indicated Treg cells were stimulated (STIM) or not with anti-CD3/CD28 antibodies in the presence or absence of the indicated blocking antibodies. Cell lysates were collected after 24 h and analyzed by Western blot with antibodies against pSMAD2 or β-actin. mAbs used were as follows: anti-GARP, MHG-8 (mIgG1); anti-αV, 272–17E6 (mIgG1); anti-β1, mab13 (rIgG2a); anti-αVβ3, LM609 (mIgG1); anti-αVβ5, P1F6 (mIgG1); and anti-β8, 37E1-B5 (mIgG1) or ADWA-11 (mIgG1). Images were captured with the Fusion Solo 4S station and quantified with Bio-1D software. (B) Quantification of pSMAD2:β-actin ratios measured by Western blot in six independent experiments performed as in A with two Treg clones and polyclonal Tregs from four different donors. Values represent mean ratios ± SD (***P < 0.001 vs. no antibody treatment by ANOVA followed by Tukey post hoc test).
We concluded that TGF-β1 activation on the surface of human Tregs is mediated by GARP and integrin αVβ8 and does not require protease activity. Whether GARP and integrin αVβ8 collaborate to activate the same pool of latent TGF-β1 on the surface of Tregs or act independently from one another on distinct pools of surface latent TGF-β1 cannot be inferred from these experiments.
Integrin αVβ8 Interacts with GARP/Latent TGF-β1 Complexes.
GARP forms disulfide-linked complexes with latent TGF-β1 in human Tregs (6, 9), and integrin αVβ8 forms noncovalently linked complexes with exogenous, recombinant latent TGF-β1 in transfected cells (31). Thus, if integrin αVβ8 and GARP collaborate to activate the same pool of latent TGF-β1, one expects to find complexes of the three proteins on cells expressing all partners.
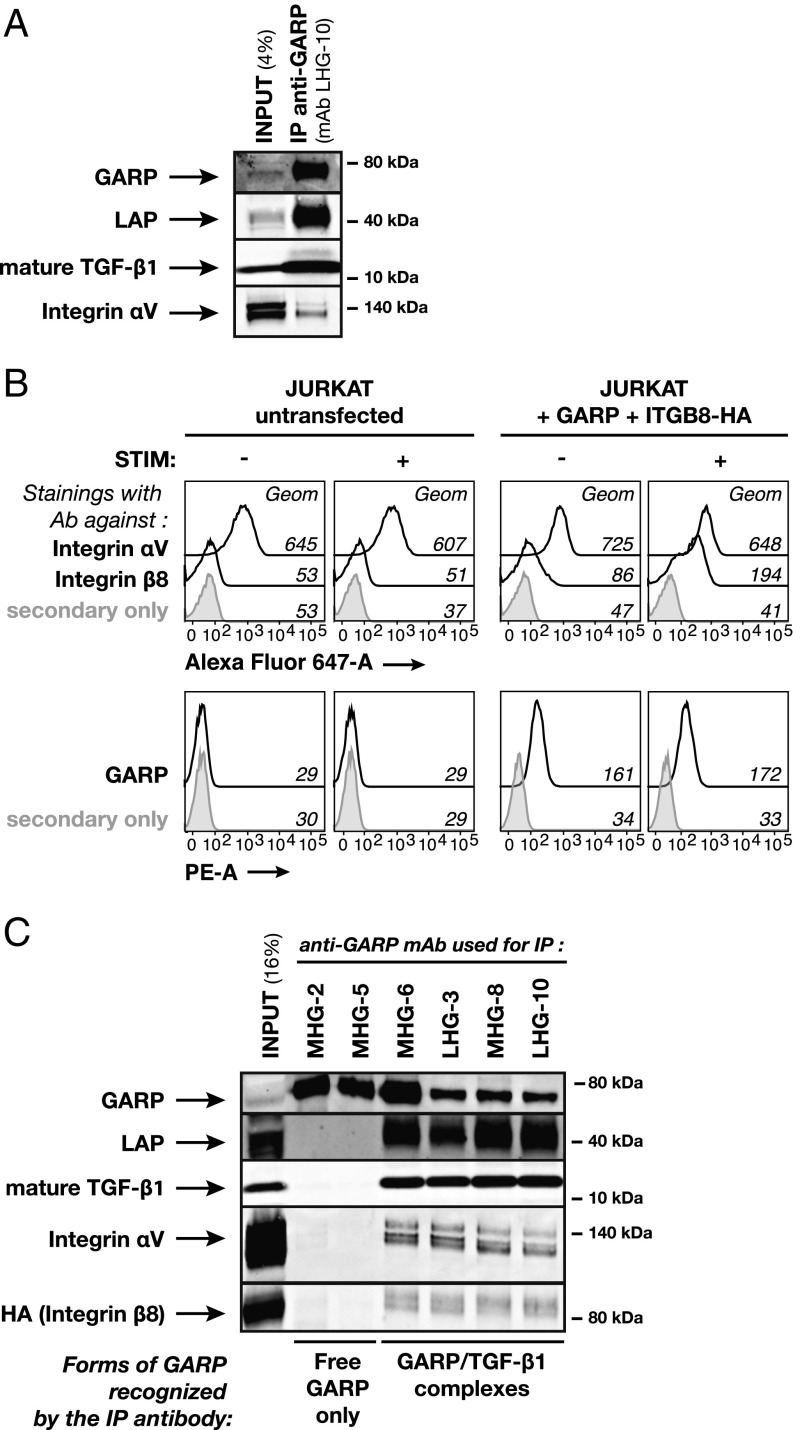
We first used stimulated human Tregs, which express endogenous GARP, latent TGF-β1, and integrin αVβ8. As shown in Fig. 4A, an antibody directed against GARP (mAb LHG-10) immunoprecipitated GARP and coimmunoprecipitated LAP, mature TGF-β1, and the αV integrin subunit. These results indicate that GARP/latent TGF-β1 complexes interact with an αV-containing integrin in human Tregs. We could not examine whether it also coimmunoprecipitated the β8 subunit because of the lack of an antibody that detects β8 by Western blot.
Fig. 4.
Integrin αVβ8 interacts with GARP/TGF-β1 complexes. (A) Polyclonal Tregs from donors 8 and 10 were stimulated with anti-CD3/CD28 antibodies for 24 h. Cell lysates were pooled and immunoprecipitated with anti-GARP mAb LHG-10. Total lysate (4% of input in IP) and IP product were analyzed by Western blot with antibodies against GARP, LAP, mature TGF-β1, or integrin αV subunit. Results are representative of three independent experiments. (B) Flow cytometry analyses of untransfected Jurkat cells (Left) or Jurkat cells transfected with GARP and HA-ITGB8 (Right), resting or 24 h after stimulation (STIM) with anti-CD3 antibody, and labeled with mAbs to integrin αV subunit or integrin β8 subunit followed by anti-mIgG1 antibodies coupled to Alexa Fluor 647 (Top) or with biotinylated anti-GARP mAb MHG-6 followed by streptavidin coupled to phycoerythrin (Bottom). (C) Jurkat cells transfected with GARP and HA-ITGB8 were stimulated with anti-CD3/CD28 antibodies for 24 h. Cell lysate was immunoprecipitated with the indicated anti-GARP mAbs. Total lysate (16% of input in IP) and IP products were analyzed by Western blot with antibodies against GARP, LAP, mature TGF-β1, integrin αV subunit, or HA (as a readout of integrin β8 subunit expression).
We resorted to Jurkat T cells, which express high levels of αV but neither GARP nor β8 (Fig. 4B, Left), and transfected them with constructs encoding GARP and an HA-tagged form of β8 (Fig. 4B, Right). The cells were stimulated with anti-CD3/CD28 antibodies to further increase expression of the HA-tagged β8 subunit (Fig. 4B). We then used previously characterized anti-GARP mAbs (4) to immunoprecipitate GARP. GARP was immunoprecipitated with all anti-GARP antibodies tested (Fig. 4C). As expected, mAbs MHG-2 and MHG-5, which bind free GARP (i.e., not bound to latent TGF-β1) but do not bind GARP/latent TGF-β1 complexes, did not coimmunoprecipitate LAP and mature TGF-β1. MHG-2 and MHG-5 did not coimmunoprecipitate αV or β8 either, suggesting that integrin αVβ8 does not interact with free GARP (Fig. 4C). In contrast, mAbs MHG-6, LHG-3, MHG-8, and LHG-10 bind GARP/latent TGF-β1 complexes, and, as expected, coimmunoprecipitated LAP and mature TGF-β1. They also coimmunoprecipitated αV and β8 integrin subunits, indicating that integrin αVβ8 interacts with GARP/latent TGF-β1 complexes (Fig. 4C). It is noteworthy that MHG-8 and LHG-10 not only bind GARP/latent TGF-β1 complexes, but also block TGF-β1 activation by human Tregs (4). As these blocking anti-GARP mAbs coimmunoprecipitate integrin αVβ8, it appears that their mode of action does not imply disruption of the interaction between GARP/latent TGF-β1 complexes and integrin αVβ8.
To determine if this interaction is direct, we incubated recombinant GARP/latent TGF-β1 complexes with recombinant integrin αVβ8, loaded the mixture on a gel filtration column, and monitored protein content in the eluate by UV spectrophotometry (Fig. S4A). We identified three major peaks containing protein complexes of decreasing molecular sizes. Western blot analysis of the corresponding fractions indicated that they contained GARP/latent TGF-β1/integrin αVβ8 complexes, integrin αVβ8 dimers, and GARP/latent TGF-β1 complexes, respectively (Fig. S4B).
These results show that, on human Tregs, integrin αVβ8 forms complexes with GARP/latent TGF-β1 but not with free GARP, and that the formation of these complexes does not require an additional partner.
Integrin αVβ8 Activates TGF-β1 from GARP/Latent TGF-β1 Complexes.
If, on human Tregs, integrin αVβ8 and GARP collaborate to activate the same pool of latent TGF-β1, this activation by integrin αVβ8 should be inhibited by blocking anti-GARP. This appears to be the case in human Tregs, as anti-GARP antibodies abolish TGF-β1 activation almost completely, and as efficiently as anti-αV or anti-β8 antibodies (Fig. 3). To confirm this, we compared the activity of blocking anti-GARP antibodies on Jurkat cells transfected with GARP and/or integrin β8-encoding constructs or not transfected. Untransfected Jurkat cells secrete latent TGF-β1 but do not activate the cytokine, as shown by Western blot analysis of pSMAD2 (Fig. 5A). A Jurkat clone stably transfected with GARP alone did not activate TGF-β1, confirming that GARP is not sufficient to induce TGF-β1 activation in human T cells. In contrast, a Jurkat clone stably transfected with integrin β8 (therefore expressing integrin αVβ8 but not GARP) activated latent TGF-β1 upon TCR stimulation. Activation was inhibited by anti-αV and anti-β8 mAbs, but not by a blocking anti-GARP mAb. Thus, integrin αVβ8 can activate latent TGF-β1 in the absence of GARP. A Jurkat clone coexpressing integrin αVβ8 and GARP also activated latent TGF-β1 upon TCR stimulation. Interestingly, activation was inhibited by anti-αV or anti-β8 mAbs, and also by a blocking anti-GARP mAb (Fig. 5). Altogether, theses results supports the notion that, when GARP is present, the activation of latent TGF-β1 by integrin αVβ8 depends on GARP, probably because most of the latent TGF-β1 pool that is available for activation is present within GARP/latent TGF-β1 complexes.
Fig. 5.
Blocking anti-GARP mAb inhibits the integrin αVβ8-mediated TGF-β1 activation from GARP/TGF-β1 complexes. (A) The indicated Jurkat clones were stimulated (STIM) with anti-CD3/CD28 antibodies or not stimulated in the presence or absence of the indicated blocking antibodies. Cell lysates were collected after 24 h and analyzed by Western blot with antibodies against pSMAD2 or β-actin. mAbs used were as follows: anti-GARP, MHG-8 (mIgG1); anti-αV, 272–17E6 (mIgG1); and anti-β8, ADWA-11 (mIgG1). Images were captured with the Fusion Solo 4S station and quantified with Bio-1D software. (B) Quantification of pSMAD2:β-actin ratios measured by Western blot in three independent experiments performed as in A. Values represent mean ratios ± SD (**P < 0.01 and ***P < 0.001 vs. no antibody treatment by ANOVA followed by Tukey post hoc test).
Antibodies Against β8 Block Immunosuppression by Human Tregs in Vivo.
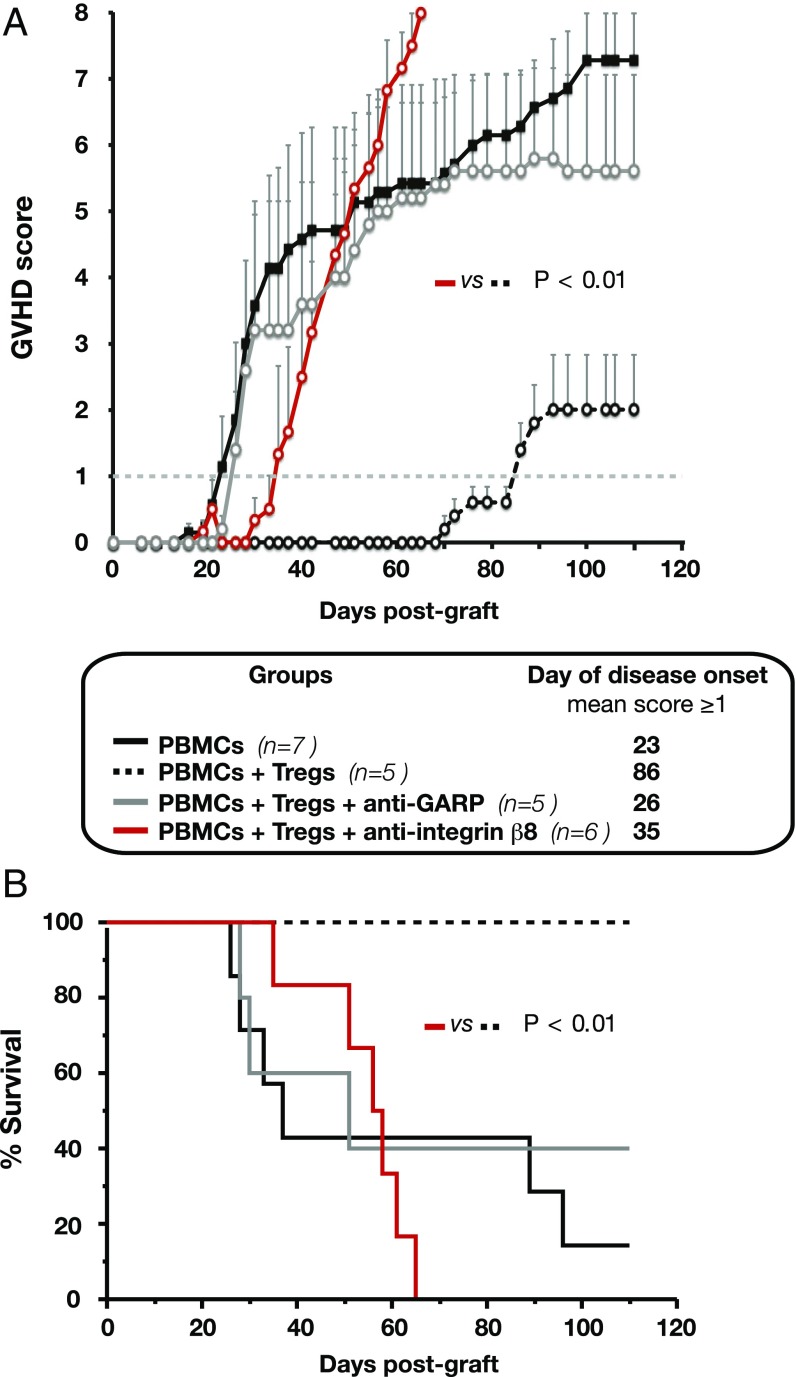
NOD.Cg-Prkdcscid Il2rgtm1Wjl/SzJ (NSG) mice have defective cytokine signaling and lack functional T, B, and natural killer cells, allowing very efficient engraftment of human T cells. Shortly after PBMC transfer, the mice develop GVHD as a result of the activity of human T cells against murine tissues (33). In this model, the cotransfer of human Tregs attenuates GVHD (34). We previously showed that anti-GARP antibodies that block TGF-β1 activation inhibited immunosuppression by human Tregs in this model (4). We used the same model with anti-β8 antibodies.
We transferred into NSG mice human PBMCs with or without autologous Tregs, namely blood CD4+CD25hiCD127lo cells shortly amplified in vitro as described here earlier. One day before the graft and weekly thereafter, mice were injected with blocking antibodies against human β8 (mAb ADWA-11) or human GARP (mAb LHG-10.6) or not injected. Objective signs of GVHD were monitored biweekly to establish a disease score. As expected, cotransfer of Tregs delayed GVHD onset from 23 d to 86 d (Fig. 6A). It also augmented survival, as the proportion of mice alive at the end of the observation period (110 d) increased from 14% to 100% (Fig. 6B). Treg immunosuppression was abrogated by the administration of anti-human GARP (disease onset, day 26; long-term survival, 40%). The administration of the blocking anti-β8 did also reduce the immunosuppression by Tregs: disease started on day 35, and no mice survived longer than 65 d (Fig. 6A). Similar results were obtained in a repeat experiment with cells from a second donor (Fig. S5). In this experiment, we verified that anti-β8 did not aggravate GVHD in the absence of Tregs (i.e., in mice receiving PBMCs but no Tregs). As the blocking anti-human β8 is cross-reactive against mouse β8, we also verified that it did not induce disease in mice not grafted with human cells (Fig. S5).
Fig. 6.
Anti-integrin β8 mAb that blocks TGF-β1 activation inhibits suppression by human Tregs in vivo. On day 0, PBMCs and autologous Tregs from donor 6 were injected i.v. in preconditioned NSG mice (1.5 Gy on day −1). Mice received weekly i.p. injections of 400 µg of anti-GARP (mAb LHG-10.6), anti-integrin β8 (mAb ADWA-11), or PBS solution as indicated. (A) Clinical GVHD was monitored at least biweekly to establish a score based on weight loss, reduced mobility, anemia or icterus, and hair loss. Graph shows progression of disease score (means per group ± SEM). The day of disease onset is when the mean disease score becomes ≥1. n, number of mice per group. P value was calculated by Mann–Whitney U test. (B) Survival analysis by Kaplan–Meier curve. Statistical significance of differences in survival was calculated by log-rank (Mantel–Cox) test.
Altogether, these results show that immunosuppression by human Tregs can be inhibited in vivo with anti-β8 antibodies that block the production of active TGF-β from GARP/latent TGF-β1 complexes.
Discussion
Understanding how human Tregs suppress other immune cells may help in the design of novel approaches for the immunotherapy of various diseases associated with dysfunctional immune responses. Accumulating evidence indicates that, in response to TCR activation, human Tregs exert immunosuppression at least by producing active TGF-β1 close to their cell surface. We have previously shown that TGF-β1 activation by human Tregs requires GARP, which covalently binds and presents latent TGF-β1 on the Treg surface. We now show that integrin αVβ8 binds and activates the latent TGF-β1 pool tethered by GARP on the surface of human Tregs. Like GARP, integrin αVβ8 dimers are present on TCR-stimulated Tregs but not other CD4+ T cells (i.e., Th cells), reinforcing the notion that this immunosuppressive mechanism is restricted to Tregs in the human T cell lineage. Importantly, anti-β8 antibodies blocked immunosuppression by human Tregs in vivo as potently as anti-GARP antibodies. This suggests that both types of antibodies could increase immune responses in patients with cancer or chronic infections by targeting the same Treg immunosuppressive mechanism.
This mechanism may also operate in the mouse. Itgb8 mRNA was found at higher levels in murine Tregs by comparison with Th cells, and Itgb8−/− Tregs failed to produce active TGF-β1 (29, 30). Although none of these studies demonstrated the existence of GARP/latent TGF-β1/integrin αVβ8 supramolecular complexes in mouse Tregs, one did show reduced immunosuppression by Itgb8−/− Tregs in mice with colitis induced by naïve T cell transfer or by dextran sulfate sodium (29).
In transfected 293T cells, GARP/latent TGF-β1 complexes were shown to form supramolecular complexes with αVβ6, another RGD-binding integrin (9). This interaction is not relevant to the biology of Tregs, which do not express integrin β6. Incidentally, to our awareness, no cell type that coexpresses GARP and αVβ6 has been identified thus far. Nevertheless, the ability of GARP/latent TGF-β1 complexes to interact with αVβ8 as well as with αVβ6 suggests that the molecular mechanism of TGF-β1 activation by αVβ8 in Tregs is similar to that by αVβ6 in non-Treg cells. In line with this, crystal structure analyses by Springer and coworkers (35) reveal that the β6 residues that are crucial for binding to TGF-β1 are conserved in β8 and different in all other β-subunits. Activation by αVβ6-expressing cells requires, on one side, the attachment of the integrin to the cytoskeleton, and, on the other side, the disulfide bonding of LAP Cys33 to Latent TGF-β Binding Protein (LTBP) anchored in the ECM (13, 36). This allows pulling forces exerted by integrin αVβ6 on LAP to release active TGF-β1 (36–38). On human Tregs, TGF-β1 activation from GARP/latent TGF-β1 complexes requires disulfide bonding of LAP Cys33 to GARP and anchoring of GARP to the cell membrane (6, 9), supporting a TGF-β1 activation mechanism with pulling forces by αVβ8 on LAP tethered to the Treg membrane via GARP. This contrasts with the mechanism usually proposed for activation by αVβ8 on epithelial cells, thought to occur via recruitment of MMP-14 and subsequent proteolytic degradation of LAP to release active TGF-β (31). Proteases clearly do not play a role in mouse and human Tregs, as protease inhibitors do not reduce their production of active TGF-β1 (ref. 30 and the present study).
The tensile forces required for the αVβ6-mediated opening of the LAP are thought to result from the attachment of β6 to the cytoskeleton. The origin of the force at play when αVβ8 is involved is less clear because the cytoplasmic tail of β8 does not couple with the actin cytoskeleton and is not required for TGF-β activation in transfected cells (31). However, several studies in cell lines of various origins have now reported interaction between the short β8 tail and cytoplasmic signaling or adaptor molecules, which could in turn directly or indirectly interact with the cytoskeleton (39–43). In TCR-stimulated human Tregs, β8 may interact with similar proteins, which would provide the traction forces required for the mechanical opening of the LAP.
Anti-β8 antibodies could represent an alternative to anti-GARP mAbs for cancer immunotherapy because they inhibit the same Treg immunosuppressive mechanism. GARP is present on the surface of TCR-stimulated Tregs, but was also found on platelets, mesenchymal stromal cells, endothelial cells, hepatic stellate cells, fibroblasts, and, more recently, activated B cells (4,8,44–48). Expression of the gene ITGB8 was found in yet a broader range of cell types, most of which do not express GARP. Noteworthy, defining the αVβ8-expressing cells has remained difficult because of the lack of appropriate reagents. Expression of αV is yet broader than that of β8, and the TGFB1 gene is expressed ubiquitously. Thus, defining which cells produce active TGF-β1 from GARP/latent TGF-β1 complexes in an αVβ8-dependent manner will be required to try to predict differences in efficacy or toxicity of anti-GARP or anti-β8 antibodies in patients.
Materials and Methods
Cells and Lentiviral Transductions.
Human Treg and Th clones were derived and cultured as previously described (32). Human polyclonal Tregs were obtained by sorting CD4+CD25hiCD127lo cells by FACS from total PBMCs, followed by in vitro stimulation with anti-CD3/CD28–coated beads in the presence of IL-2 for 12–14 d as previously described (6). Experiments with human cells were approved by our Institution's ethics committee (Commission d'Ethique Biomédicale Hospitalo-Facultaire de l'Université catholique de Louvain), under registration number B403201110966. Written informed consent for the use of blood samples was not always obtained, in accordance with the Belgian law of 19 December 2008 which states that, in the absence of written opposition by the patient, consent is considered given for residual body material. This applies to blood samples from hemochromatosis patients. No patient opposed the use of blood samples. Data obtained from blood samples were analyzed anonymously. Jurkat cells (clone E6-1) were obtained from the American Type Culture Collection. We generated cells overexpressing an HA-tagged form of integrin β8 by electroporation of clone E6-1 and selection in neomycin under limiting dilution conditions (clone Jurkat + ITGB8-HA). Clone E6-1 or clone Jurkat + ITGB8-HA was transduced with a lentivirus encoding GARP as previously described (7) to generate Jurkat + GARP or Jurkat + GARP + ITGB8-HA cells, respectively.
Evaluation of Proportion of Cells with a Demethylated FOXP3i1 Allele in Human Polyclonal Treg Populations.
A methyl-specific quantitative PCR (qPCR) assay was used to quantify demethylated and total (demethylated + methylated) FOXP3i1 sequences in bisulfite-treated genomic DNA prepared from polyclonal Tregs as previously described (4). Proportions of cells with demethylated FOXP3i1 were calculated as the number of demethylated FOXP3i1 sequences divided by the number of total FOXPi1 sequences multiplied by the number of X chromosomes per cell.
Short-Term Stimulations of T Cells.
T cell clones and Jurkat cells (106 cells per milliliter) were stimulated in X-VIVO 10 serum-free medium (Lonza) with coated anti-CD3 (orthoclone OKT3; 1 μg/mL; Janssen–Cilag) and soluble anti-CD28 (1 μg/mL; BD Biosciences). Polyclonal T cells were incubated with Dynabeads Human T-activator CD3/CD28 (Gibco) at a 1:1 cell:bead ratio. Stimulations were made in the presence or absence of 20 μg/mL of the following inhibitory antibodies: anti-hGARP [mAb MHG-8 (4)], anti-TGF-β1,2,3 (mAb 1D11; R&D Systems), anti-αV integrin (mAb 272–17E6; Millipore), anti-β1 integrin (mab13; BD Pharmingen), anti-αVβ3 integrin (mAb LM609; Millipore), anti-αVβ5 integrin (mAb P1F6; Abcam), anti-β8 integrin [mAb ADWA-11 or mAb 37E1-B5 (28)]. GRRGDLATIH and GRRGELATIH peptides were synthesized in-house and used at 230 μM. GM6001 (Calbiochem), PMSF (Sigma), pepstatin (Sigma), and leupeptin (Sigma) were used at concentrations indicated in the Fig. S3 legend.
Western Blotting.
Cells were lysed in Laemmli buffer supplemented with 5% β-mercaptoethanol as previously described (32) and submitted to SDS/PAGE and Western blot with the following primary antibodies,: anti-pSMAD2 (no. 3108; Cell Signaling Technologies), anti–β-actin (Sigma), anti-αV integrin (ab179475; Abcam), anti-GARP (ALX-804-867; Enzo Life Sciences), anti-TGF-β1 (no. 555052; BD Pharmingen), biotinylated anti-LAP (BAF246; R&D Systems), anti-HA (MMS-101R; Eurogentec), and anti-β8 integrin (no. 10817; Santa Cruz). The anti-β8 antibody detects purified, recombinant αVβ8 integrin by Western blot, but, as a result of the very high background on cell lysates, it does not detect β8 expressed by untransfected or transfected cells.
IP.
IP analyses were performed using the Dynabeads co-IP kit (Novex) with slight modifications. Briefly, antibodies were immobilized on M-270 epoxy Dynabeads at a concentration of 5 μg/mg of beads according to the manufacturer’s instructions. The following antibodies were used for IP: anti-β8 integrin [mAb 37E1-B5 (28)] and anti-hGARP [mAbs tested, MHG-2, 5, 6, 8; LHG-3, 10 (4)]. Cells were lysed in 1× IP buffer containing 100 mM NaCl and protease inhibitors (CPI mini, EDTA-free; Roche). Cleared lysates were then incubated with 1.5 mg antibody-coated Dynabeads. After washing the beads, immunoprecipitates were directly eluted from the beads with Laemmli buffer supplemented with 5% β-mercaptoethanol.
RT-qPCR.
Total RNA was extracted and reverse-transcribed as previously described (32). qPCR amplifications were done in a final volume of 20 μL by using the Takyon Master Mix (Eurogentec) in a StepOnePlus Real-Time PCR System (Applied Biosystems) under standard conditions: 95 °C for 3 min, 45 cycles of 95 °C for 10 s, and 60 °C for 1 min. Primer sequences are listed in Table S3.
For the custom TaqMan array (Applied Biosystems), 1 μg RNA was reverse-transcribed by using SuperScript III Vilo RT Master Mix (Invitrogen), and qPCR amplifications were done in a final volume of 10 μL by using the TaqMan Fast Advanced Master Mix (Applied Biosystems) in a StepOnePlus Real-Time PCR System (Applied Biosystems) under fast conditions: 95 °C for 20 s, 45 cycles of 95 °C for 3 s, and 60 °C for 30 s. The array was designed on the Thermo Fisher Scientific Web site by using individual TaqMan Gene Expression Assays (Applied Biosystems), the list of which is available upon request.
Flow Cytometry.
Cells were labeled according to standard protocols by using combinations of the following primary and/or secondary reagents. Primary antibodies included biotinylated anti-hGARP [mAb MHG-6 (4)], anti-αV integrin (mAb L230; Enzo Life Sciences), and anti-β8 integrin [mAb 14E5 (31)]. Secondary antibodies or reagents included anti-mIgG1-AF647 (Life Technologies) and Streptavidin/PE (BD Biosciences). Labeled cells were analyzed on an LSR Fortessa cytometer (BD Biosciences), and results were computed with FlowJo software.
xGVHD in NSG Mice.
NSG mice were purchased from The Jackson Laboratory and were bred at the animal facility of Université catholique de Louvain, Belgium. xGVHD was induced and monitored as previously described (4). One day before the graft and weekly thereafter, mice received i.p. injections of PBS solution or 400 μg of anti-β8 integrin (mAb ADWA-11, mIgG1), and anti-hGARP (mAb LHG-10.6, hIgG1). Isotype control mIgG1 anti-TNP clone B8401H5.M was used in Fig. S5.
Gel Filtration of Recombinant Complexes.
Recombinant integrin αVβ8 (containing a C-terminal clasp with a 10-aa flexible linker HPGGGSGGGS between αV-V992 and β8-R684) was purchased from R&D Systems. To prepare integrin αVβ8–GARP/latent TGF-β1 complexes, 10 μg of recombinant GARP/latent TGF-β1 complexes was incubated with a fourfold molar excess of recombinant αVβ8 overnight at 4 °C. Size-exclusion chromatography was performed by injecting samples into a Superdex 200 Increase (10/300) column connected to an AKTA FPLC system. Elution was done at a flow rate of 0.75 mL/min with a buffer containing 20 mM Tris⋅HCl, pH 7.5, 150 mM NaCl, 1 mM CaCl2, and 1 mM MgCl2.
Production of Anti-Integrin β8 mAb ADWA-11.
Mice lacking the integrin β8 gene crossed to the outbred CD1 background (which permits postnatal survival) were immunized at >6 wk of age with purified ectodomains of human integrin αVβ8 (R&D Systems) at 2-wk intervals. Serum was screened by solid-phase binding assay for reaction with purified integrin αVβ8, and effectively immunized mice were killed, spleens collected, and splenocytes fused with SP 2/0 fusion partners to generate hybridomas. Clone specificity for human integrin β8 was screened by flow cytometry by using untransfected SW480 colon carcinoma cells (that do not express integrin αVβ8, to exclude antibodies that bound to integrin αV or other surface proteins), SW480 cells transfected to express integrin αVβ3 or αVβ6 (as a further negative control), and cells transfected with integrin β8 cDNA. The ability of ADWA-11 to block ligand binding and function of integrin αVβ8 was demonstrated by inhibition of adhesion of the human glioblastoma integrin αVβ8-expressing cell line U251 to plates coated with 1 μg/mL of recombinant LAP and inhibition of TGF-β activation by U251 cells, measured by an active TGF-β reporter cell assay, as described for mAb ADWA-16 (49). mAb ADWA-11 was recently used by Reboldi et al. (50).
Statistics.
Statistical analyses were performed with Prism 6.0 (GraphPad) or SPSS Statistics version 24 (IBM). Groups were compared with ANOVA with Tukey’s post hoc test. P < 0.05 was considered statistically significant. Curves of disease-score progression were compared by using a Mann–Whitney U test. Survival curves were generated by Kaplan–Meier method and compared by using a log-rank test (Mantel–Cox).
Supplementary Material
Acknowledgments
The authors thank Nicolas Dauguet for FACS sorting, Vincent Stroobant for peptide synthesis, Maria Panagiotakopoulos for culture of T cell clones, and Suzanne Depelchin for expert editorial help. This work was supported by the Belgian Programme on Interuniversity Poles of Attraction initiated by the Belgian State, Prime Minister’s Office, Science Policy Programming; the Actions de Recherche Concertées of the Communauté Française de Belgique; grants from the European Union’s Horizon 2020 research and innovation programme under Grant Agreement 682818; Fonds National de la Recherche Scientifique (Belgium); and Walloon Excellence in Life Sciences and Biotechnology under Bridge Fund WELBIO-BF-2016-01 (Belgium).
Footnotes
Conflict of interest statement: S. Lucas and P.G.C. are co-owners of a patent for use of anti-GARP antibodies. D.S. is co-owner of a patent for use of anti-αVβ8 antibodies for immunotherapy of cancer and is funded by a grant from the joint University of California, San Francisco/Pfizer Center for Translational Innovation.
This article is a PNAS Direct Submission.
This article contains supporting information online at www.pnas.org/lookup/suppl/doi:10.1073/pnas.1710680114/-/DCSupplemental.
References
- 1.Josefowicz SZ, Lu LF, Rudensky AY. Regulatory T cells: Mechanisms of differentiation and function. Annu Rev Immunol. 2012;30:531–564. doi: 10.1146/annurev.immunol.25.022106.141623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sakaguchi S, Miyara M, Costantino CM, Hafler DA. FOXP3+ regulatory T cells in the human immune system. Nat Rev Immunol. 2010;10:490–500. doi: 10.1038/nri2785. [DOI] [PubMed] [Google Scholar]
- 3.Chaudhry A, Rudensky AY. Control of inflammation by integration of environmental cues by regulatory T cells. J Clin Invest. 2013;123:939–944. doi: 10.1172/JCI57175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cuende J, et al. Monoclonal antibodies against GARP/TGF-β1 complexes inhibit the immunosuppressive activity of human regulatory T cells in vivo. Sci Transl Med. 2015;7:284ra56. doi: 10.1126/scitranslmed.aaa1983. [DOI] [PubMed] [Google Scholar]
- 5.Massagué J. TGFβ signalling in context. Nat Rev Mol Cell Biol. 2012;13:616–630. doi: 10.1038/nrm3434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gauthy E, et al. GARP is regulated by miRNAs and controls latent TGF-β1 production by human regulatory T cells. PLoS One. 2013;8:e76186. doi: 10.1371/journal.pone.0076186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Stockis J, Colau D, Coulie PG, Lucas S. Membrane protein GARP is a receptor for latent TGF-β on the surface of activated human Treg. Eur J Immunol. 2009;39:3315–3322. doi: 10.1002/eji.200939684. [DOI] [PubMed] [Google Scholar]
- 8.Tran DQ, et al. GARP (LRRC32) is essential for the surface expression of latent TGF-β on platelets and activated FOXP3+ regulatory T cells. Proc Natl Acad Sci USA. 2009;106:13445–13450. doi: 10.1073/pnas.0901944106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang R, et al. GARP regulates the bioavailability and activation of TGFβ. Mol Biol Cell. 2012;23:1129–1139. doi: 10.1091/mbc.E11-12-1018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robertson IB, Rifkin DB. Unchaining the beast; insights from structural and evolutionary studies on TGFβ secretion, sequestration, and activation. Cytokine Growth Factor Rev. 2013;24:355–372. doi: 10.1016/j.cytogfr.2013.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell ID, Humphries MJ. Integrin structure, activation, and interactions. Cold Spring Harb Perspect Biol. 2011;3:a004994. doi: 10.1101/cshperspect.a004994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reed NI, et al. The αvβ1 integrin plays a critical in vivo role in tissue fibrosis. Sci Transl Med. 2015;7:288ra79. doi: 10.1126/scitranslmed.aaa5094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Munger JS, et al. The integrin α v β 6 binds and activates latent TGF β 1: A mechanism for regulating pulmonary inflammation and fibrosis. Cell. 1999;96:319–328. doi: 10.1016/s0092-8674(00)80545-0. [DOI] [PubMed] [Google Scholar]
- 14.Morris DG, et al. Loss of integrin α(v)β6-mediated TGF-β activation causes Mmp12-dependent emphysema. Nature. 2003;422:169–173. doi: 10.1038/nature01413. [DOI] [PubMed] [Google Scholar]
- 15.Ma LJ, et al. Transforming growth factor-β-dependent and -independent pathways of induction of tubulointerstitial fibrosis in β6(-/-) mice. Am J Pathol. 2003;163:1261–1273. doi: 10.1016/s0002-9440(10)63486-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pittet JF, et al. TGF-β is a critical mediator of acute lung injury. J Clin Invest. 2001;107:1537–1544. doi: 10.1172/JCI11963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wang B, et al. Role of alphavbeta6 integrin in acute biliary fibrosis. Hepatology. 2007;46:1404–1412. doi: 10.1002/hep.21849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sugimoto K, et al. The αvβ6 integrin modulates airway hyperresponsiveness in mice by regulating intraepithelial mast cells. J Clin Invest. 2012;122:748–758. doi: 10.1172/JCI58815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Travis MA, et al. Loss of integrin α(v)β8 on dendritic cells causes autoimmunity and colitis in mice. Nature. 2007;449:361–365. doi: 10.1038/nature06110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lacy-Hulbert A, et al. Ulcerative colitis and autoimmunity induced by loss of myeloid alphav integrins. Proc Natl Acad Sci USA. 2007;104:15823–15828. doi: 10.1073/pnas.0707421104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Worthington JJ, Czajkowska BI, Melton AC, Travis MA. Intestinal dendritic cells specialize to activate transforming growth factor-β and induce Foxp3+ regulatory T cells via integrin αvβ8. Gastroenterology. 2011;141:1802–1812. doi: 10.1053/j.gastro.2011.06.057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Païdassi H, et al. Preferential expression of integrin αvβ8 promotes generation of regulatory T cells by mouse CD103+ dendritic cells. Gastroenterology. 2011;141:1813–1820. doi: 10.1053/j.gastro.2011.06.076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Melton AC, et al. Expression of αvβ8 integrin on dendritic cells regulates Th17 cell development and experimental autoimmune encephalomyelitis in mice. J Clin Invest. 2010;120:4436–4444. doi: 10.1172/JCI43786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Acharya M, et al. αv Integrin expression by DCs is required for Th17 cell differentiation and development of experimental autoimmune encephalomyelitis in mice. J Clin Invest. 2010;120:4445–4452. doi: 10.1172/JCI43796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hirota S, et al. The astrocyte-expressed integrin αvβ8 governs blood vessel sprouting in the developing retina. Development. 2011;138:5157–5166. doi: 10.1242/dev.069153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Arnold TD, et al. Defective retinal vascular endothelial cell development as a consequence of impaired integrin αVβ8-mediated activation of transforming growth factor-β. J Neurosci. 2012;32:1197–1206. doi: 10.1523/JNEUROSCI.5648-11.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kitamura H, et al. Mouse and human lung fibroblasts regulate dendritic cell trafficking, airway inflammation, and fibrosis through integrin αvβ8-mediated activation of TGF-β. J Clin Invest. 2011;121:2863–2875. doi: 10.1172/JCI45589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Minagawa S, et al. Selective targeting of TGF-β activation to treat fibroinflammatory airway disease. Sci Transl Med. 2014;6:241ra79. doi: 10.1126/scitranslmed.3008074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Worthington JJ, et al. Integrin αvβ8-mediated TGF-βactivation by effector regulatory T cells is essential for suppression of T-cell-mediated inflammation. Immunity. 2015;42:903–915. doi: 10.1016/j.immuni.2015.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Edwards JP, Thornton AM, Shevach EM. Release of active TGF-β1 from the latent TGF-β1/GARP complex on T regulatory cells is mediated by integrin β8. J Immunol. 2014;193:2843–2849. doi: 10.4049/jimmunol.1401102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Mu D, et al. The integrin α(v)β8 mediates epithelial homeostasis through MT1-MMP-dependent activation of TGF-β1. J Cell Biol. 2002;157:493–507. doi: 10.1083/jcb.200109100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stockis J, et al. Comparison of stable human Treg and Th clones by transcriptional profiling. Eur J Immunol. 2009;39:869–882. doi: 10.1002/eji.200838807. [DOI] [PubMed] [Google Scholar]
- 33.Shultz LD, Brehm MA, Garcia-Martinez JV, Greiner DL. Humanized mice for immune system investigation: Progress, promise and challenges. Nat Rev Immunol. 2012;12:786–798. doi: 10.1038/nri3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hannon M, et al. Infusion of clinical-grade enriched regulatory T cells delays experimental xenogeneic graft-versus-host disease. Transfusion. 2014;54:353–363. doi: 10.1111/trf.12279. [DOI] [PubMed] [Google Scholar]
- 35.Dong X, Hudson NE, Lu C, Springer TA. Structural determinants of integrin β-subunit specificity for latent TGF-β. Nat Struct Mol Biol. 2014;21:1091–1096. doi: 10.1038/nsmb.2905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Annes JP, Chen Y, Munger JS, Rifkin DB. Integrin alphaVbeta6-mediated activation of latent TGF-β requires the latent TGF-β binding protein-1. J Cell Biol. 2004;165:723–734. doi: 10.1083/jcb.200312172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Buscemi L, et al. The single-molecule mechanics of the latent TGF-β1 complex. Curr Biol. 2011;21:2046–2054. doi: 10.1016/j.cub.2011.11.037. [DOI] [PubMed] [Google Scholar]
- 38.Shi M, et al. Latent TGF-β structure and activation. Nature. 2011;474:343–349. doi: 10.1038/nature10152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lakhe-Reddy S, et al. β8 integrin binds Rho GDP dissociation inhibitor-1 and activates Rac1 to inhibit mesangial cell myofibroblast differentiation. J Biol Chem. 2006;281:19688–19699. doi: 10.1074/jbc.M601110200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Reyes SB, et al. αvβ8 integrin interacts with RhoGDI1 to regulate Rac1 and Cdc42 activation and drive glioblastoma cell invasion. Mol Biol Cel l. 2013;24:474–482. doi: 10.1091/mbc.E12-07-0521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cheerathodi M, et al. The cytoskeletal adapter protein spinophilin regulates invadopodia dynamics and tumor cell invasion in glioblastoma. Mol Cancer Res. 2016;14:1277–1287. doi: 10.1158/1541-7786.MCR-16-0251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McCarty JH, Cook AA, Hynes RO. An interaction between αvβ8 integrin and Band 4.1B via a highly conserved region of the Band 4.1 C-terminal domain. Proc Natl Acad Sci USA. 2005;102:13479–13483. doi: 10.1073/pnas.0506068102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lee HS, et al. Protein tyrosine phosphatase-PEST and β8 integrin regulate spatiotemporal patterns of RhoGDI1 activation in migrating cells. Mol Cell Biol. 2015;35:1401–1413. doi: 10.1128/MCB.00112-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Li Y, et al. Hepatic stellate cells inhibit T cells through active TGF-β1 from a cell surface-bound latent TGF-β1/GARP complex. J Immunol. 2015;195:2648–2656. doi: 10.4049/jimmunol.1500139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.O’Connor MN, et al. Bloodomics Consortium Functional genomics in zebrafish permits rapid characterization of novel platelet membrane proteins. Blood. 2009;113:4754–4762. doi: 10.1182/blood-2008-06-162693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Carrillo-Galvez AB, et al. Mesenchymal stromal cells express GARP/LRRC32 on their surface: Effects on their biology and immunomodulatory capacity. Stem Cells. 2015;33:183–195. doi: 10.1002/stem.1821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carambia A, et al. TGF-β-dependent induction of CD4+CD25+Foxp3+ Tregs by liver sinusoidal endothelial cells. J Hepatol. 2014;61:594–599. doi: 10.1016/j.jhep.2014.04.027. [DOI] [PubMed] [Google Scholar]
- 48.Dedobbeleer O, Stockis J, van der Woning B, Coulie PG, Lucas S. Cutting edge: Active TGF-β1 released from GARP/TGF-β1 complexes on the surface of stimulated human B lymphocytes increases class-switch recombination and production of IgA. J Immunol. 2017;199:391–396. doi: 10.4049/jimmunol.1601882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fenton TM, et al. Inflammatory cues enhance TGFβ activation by distinct subsets of human intestinal dendritic cells via integrin αVβ8. Mucosal Immunol. 2016;10:624–634. doi: 10.1038/mi.2016.94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Reboldi A, et al. IgA production requires B cell interaction with subepithelial dendritic cells in Peyer’s patches. Science. 2016;352:aaf4822. doi: 10.1126/science.aaf4822. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.