ABSTRACT
Background: The aim of this systematic review was to examine the etiology of community-acquired pneumonia (CAP) among Chinese children younger than 5 y and provide evidence for further cost-effectiveness analyses for vaccine development, diagnostic strategies and empirical treatments.
Methods: The literature review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement. Data were obtained by searching PubMed, Embase, Web-of Science, and the Chinese databases Wanfang Data and China National Knowledge Infrastructure. All CAP etiological studies on children under 5 y of age from China published in Chinese and English between the years of 2001 and 2015 were included. A total of 48 studies were included in the final review, comprising 100 151 hospitalized children with CAP episodes. Heterogeneity and the percentage of variation between studies was analyzed based on Q statistic and I2 indices, respectively. Random effect models were used to calculate the weighted average rate in all analyses.
Results: The most frequently detected bacterial agents were Klebsiella pneumoniae (5.4%), Streptococcus pneumoniae (5.2%), Escherichia coli (5.2%), Staphylococcus aureus (3.9%), Haemophilus influenza (3.6%) and Haemophilus parainfluenzae (3.3%). The most frequently detected viruses were human rhinovirus (20.3%, in just 2 studies), respiratory syncytial virus (RSV, 17.3%), human bocavirus (9.9%), parainfluenza virus (5.8%), human metapneumovirus (3.9%) and influenza (3.5%). Mycoplasma pneumoniae and Chlamydophila pneumoniae were identified in 9.5% and 2.9%, respectively, of children under 5 y of age with CAP.
Conclusion: This article provides the most comprehensive analysis to date of the factors contributing to CAP in children under 5 y of age. S. pneumoniae, H. influenzae and influenza were the most common vaccine-preventable diseases in children. Corresponding, vaccines should be introduced into Chinese immunization programs, and further economic evaluations should be conducted. RSV is common in Chinese children and preventative measures could have a substantial impact on public health. These data also have major implications for diagnostic strategies and empirical treatments.
KEYWORDS: children, China, etiology, pneumonia, systematic review
Introduction
Community-acquired pneumonia (CAP) is a significant cause of morbidity and mortality worldwide and a major public health threat to children in China.1,2 The incidence density of pneumonia for children under 5 y of age was 0.06–0.27 per person-year in China.3 The mortality of children under 5 y of age was 153.2 per 100,000 live births according to the China Mortality Surveillance System.4 CAP can be caused by many different microorganisms, most prominently by viruses and bacteria. There are many difficulties in studying the etiology of CAP in children, such as the low yield of blood cultures, lack of satisfactory sputum specimens and hesitancy to perform pulmonary aspiration and bronchoalveolar lavage.5 In addition, it may be difficult to determine the cause of an individual case of CAP.6
Immunization against Haemophilus influenzae type b (Hib), pneumococcus, measles and influenza is the most effective way to prevent pneumonia. In developed countries, at least a third of severe episodes and two-thirds of deaths due to pneumonia can be prevented through vaccination.7 By 2015, the pneumococcal conjugate vaccine (PCV), Hib vaccine and influenza vaccine had been introduced into national immunization programs in 129, 192 and 102 member states, respectively.8 Due to the lack of a disease surveillance system for pneumonia, meningitis and otitis media in China, the true disease burden and proportion of diseases prevented by vaccines are unknown. In many previous cost-effectiveness analyses of pneumococcal vaccination for Chinese infants,9-11 all causes of pneumonia were incorporated into models, due to a lack data on the proportion of pneumonia cases caused by pneumococcus. Due to the lack of clear data on this issue, the introduction of the PCV, Hib and influenza vaccines into the Chinese immunization program has been delayed.
Due to the limitations of microbiological testing, children with CAP were poorly studied in China before the year 2000, and the usual initial treatments of many childhood pneumonias were empiric. The selection and administration of appropriate empiric medication and therapy is dependent on the experience of the doctor and the common pathogens identified in previous studies. The routine use of antibiotics and antiviral drugs in China has led to lower mortality rates, but both under use and over use of broad-spectrum antibiotics to treat CAP could be harmful due to the increasing development of antimicrobial resistance.12 Recently, there have been many comprehensive studies in children of the etiology of CAP cases serious enough to require hospitalization. However, many studies were limited to one hospital, and a systematic review of the etiology of CAP in children in China has not been performed.
The aim of this systematic review was to examine the etiology of CAP among Chinese children younger than 5 y and provide evidence for further cost-effectiveness analyses for vaccine development, diagnostic strategies and empirical treatments.
Results
Study selection
After screening titles and abstracts, 33 115 citations were retrieved and 2735 relevant articles were identified. We reviewed the full text of 2735 articles and identified 3 articles through a search of references. Of the subsequently identified 180 articles, 48 were included in the quantitative review and 132 were excluded because they contained no data, duplicate data or did not meet the selection criteria (Fig. 1).
Figure 1.
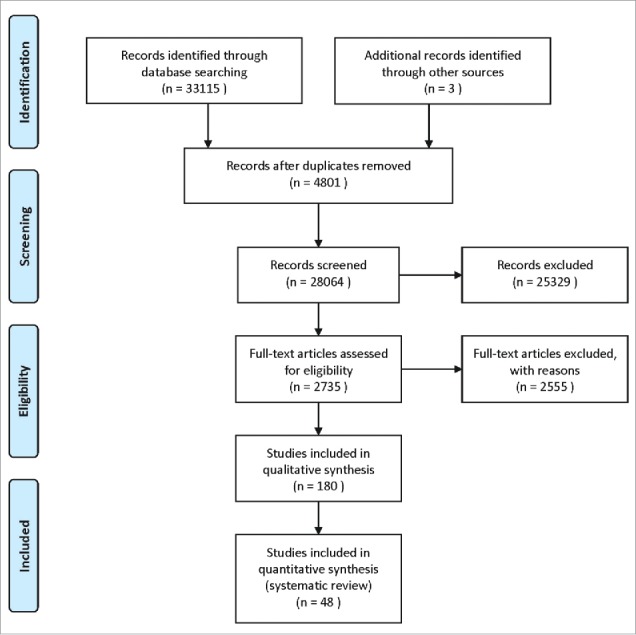
Flow diagram of the literature search and article selection.
Study characteristics
100 151 patients were included in the 48 articles. The sizes of enrolled patients populations in the studies ranged from 193 to 29 183, with a median of 713. Eleven studies (52 687 patients) analyzed prospective inpatient cohorts, 32 (45 394 patients) analyzed retrospective inpatient cohorts and 5 (2070 patients) analyzed unknown cohorts. One large inpatient study was multiprovincial, with 17 127 patients. Thirty-eight studies (31 096 patients) were of CAP, 7 (22 111 patients) were of clinical pneumonias meeting the WHO definition and 3 (46 944 patients) investigated forms of acute lower respiratory tract infections (ALRIs). A total of 44 studies were published in the core journals, and 4 were published in English. Two provinces, Xizang and Jilin, had no eligible studies (Supplementary file 1).
Quality assessment and study heterogeneity
Quality scores were used to assess the risk of bias in individual studies. Thirty-five studies had a quality score between 23 and 24, 10 had a quality score between 21 and 22, 3 had a quality score between 16 and 18. In general, the qualities of the included studies were high.
Results of the meta-analysis are detailed in supplementary file 2. Because of the high degree of variability in the source of samples and detection methods, all the weighted average detection rates were estimated using a random effects model.
Spectrum of bacterial agents
In the 35 reviewed studies on bacteria (44 147 patients, Table S3), 31 (23 882 patients) relied on nasal aspirate (NA) cultures, 2 (2378 patients) relied on sputum and NA cultures, 1 (1147 patients) relied on NAs and lung aspirate (LA) cultures, and the specimens used in 1 study (16 740 patients) were of unknown origin. Most studies that used cultures also reported some quality criteria to improve reliability, although these criteria varied.
The most commonly identified pathogen was S. pneumoniae (5.2%, Fig. 2). The % of pneumonias positive for S. pneumoniae varied between age groups, with weighted average rates of 6.1% in children under 1 y of age, 9.6% in children 1–3 y of age, and 11.0% in children 3–5 y of age.
Figure 2.
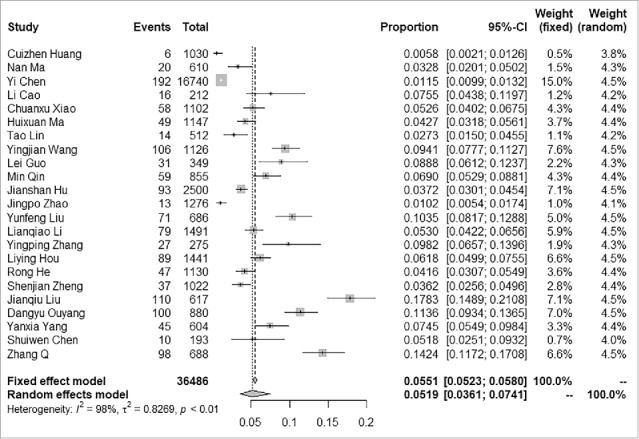
Forest plot of S. pneumoniae detected in children under 5 y of age with community-acquired pneumonia in mainland China, 2001–2015.
The overall rate of H. influenza in children under 5 y of age was 3.6% (Fig. 3). The highest rates were in children 1–3 y old (6.0%), followed by children under 1 y old (5.7%) and 3–5 y old (5.3%).
Figure 3.
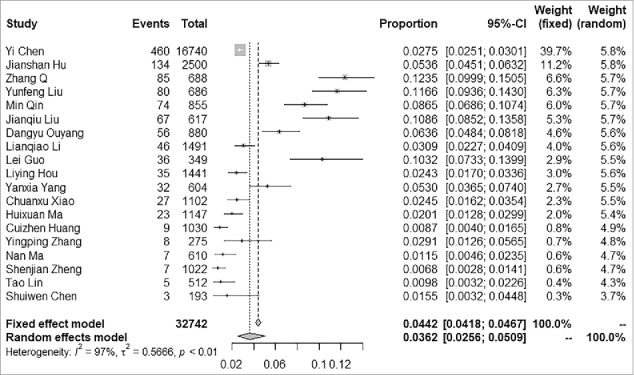
Forest plot of H. influenza detected in children under 5 y of age with community-acquired pneumonia in mainland China, 2001–2015.
The proportion of patients diagnosed with Haemophilus parainfluenzae was 3.5% for children under the age of 1 year, 6.3% in children 1–3 y of age, 4.7% in children 3–5 y old and 3.3% in children under 5 y of age.
Klebsiella Pneumoniae, Escherichia coli and Staphylococcus aureus were identified in 5.4%, 5.1% and 3.9%, respectively, of hospitalized patients under 5 y of age.
Spectrum of viral agents
In the 32 reviewed virus studies (67 744 patients, Table S4), serum samples were tested in 11 (5510 patients) and NA were tested in 15 (41 479 patients). Sputum samples (1465 patients) and unknown specimens (18 143 patients) were tested in 2 of the studies, respectively. NAs and LA were tested in 1 (1147 patients). Immunofluorescence assays were performed in 16 studies (13 949 patients), ELISAs were performed in 8 (4239 patients), PCRs were performed in 6 (48 978 patients) and the alkaline phosphatase-anti-alkaline phosphatase technique was used in 1 (578 patients).
All of the viral agents were detected in each age group. Aside from human rhinovirus (20.3%, detected in only 2 studies), respiratory syncytial virus (RSV, 17.3%, Fig. 4) was consistently the most frequently detected, representing up to 40% of identified viral pathogens in children with CAP under 5 y of age. Human bocavirus, parainfluenza virus, human metapneumovirus and influenza were identified in 9.9%, 5.8%, 3.9%, 3.5%, respectively, of hospitalized patients under 5 y of age. Adenovirus (ADV) and human coronaviruses were less frequently detected.
Figure 4.
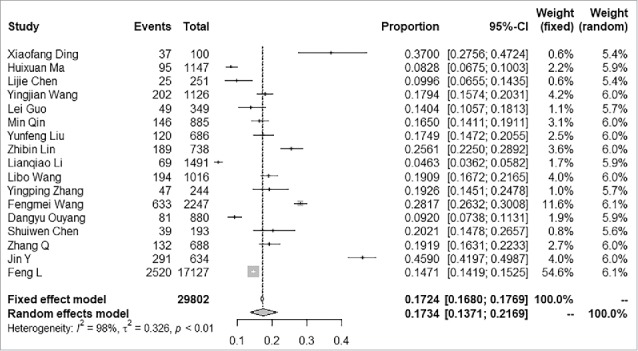
Forest plot of RSV detected in children under 5 y of age with community-acquired pneumonia in mainland China, 2001–2015.
A study by Feng et al.55 was conducted in 108 sentinel hospitals in 24 provinces in China. RSV was the most dominant pathogen, accounting for 9.9% of cases (2795/28 369), followed by influenza at 6.6% (1869/28 369), human parainfluenza virus at 4.8% (1366/28 369) and adenoviruses at 3.4% (957/28 369). More than 1 type of virus were identified in 7.2% (2032/28 369) of patients, and RSV was the most frequent etiology in cases with co-detection.
Mycoplasma pneumoniae and Chlamydia pneumoniae
Twenty-four studies (17 005 patients) included diagnostic tests for these organisms (Table S5). PCRs were used in 13 studies (10 698 patients), ELISAs was used in 5 (1829 patients), immunofluorescence assays were used in 3 (2523 patients), latex agglutination test was used in 1 (251 patients), and the diagnostic methods used were unknown in 2 (1704 patients). Mycoplasma pneumoniae and Chlamydia pneumoniae were common atypical CAP pathogens and were identified in 9.5% and 2.9% of all hospitalized children under 5 y of age, respectively.
Discussion
This article is the first to describe the etiologies in children with CAP under 5 y of age from 29 Chinese provinces, and it reveals several important patterns.
S. pneumoniae is the most frequent cause of bacterial pneumonia in young children but is infrequently found in blood cultures.5,57 The serotype distribution of pneumococcal infections in Chinese children under 5 y of age from 1996 to 2004 was 19A (33.3%), 19F (16.7%), 14 (12.9%), 23F (8.3%), NT (6.5%), 5 (5.6%) and 9V (2.8%); serotypes included in PCV7 and PCV13 covered 60.2% and 87.7% of cases respectively.58 PCV7 was approved for the Chinese market between 2008 and 2014, and the low coverage of PCV7 (9.9% in 201359) is not sufficient to significantly reduce pneumococcal pneumonia rates. The proportions of S. pneumoniae were relatively lower than in most European studies,60,61 and the true pneumococcal pneumonia burden may be underestimated due to the overuse of antibiotics and the limited ability to perform bacteriological tests in most hospitals.
More than 90% of cases of invasive Hib infection occur in children under 5 y of age, and Hib is responsible for more than 90% of systemic H. influenza infections.62 The coverage for a 3rd dose of the Hib vaccine for children was 45.3% in 2013.59 H. influenza infections in children have been dramatically decreased, and the detection rate of H. influenza in children with CAP (3.6%) was lower than in adults with CAP (9.2%) in China.63
A lack of rigorous microbiological standards, such as collecting specimens after using antibiotics, specimen transport delays, or specimen cultures without adequate microscopic white blood cell screening, may result in reduced isolation of more fastidious bacteria (such as S. pneumoniae and H. influenza) and increased isolation of E. coli and S. aureus. With the widespread use of broad-spectrum antibiotics, 30.1% of E. coli strains were found to be extended-spectrum β-lactamase producing strains. E. coli is the common bacterial pathogen in the etiology of pneumonia, as reported in another study.64 K. Pneumoniae was the most common gram-negative bacilli isolated from sputum in most studies; however, the high rate of isolation of K. Pneumoniae could also relate to the above-mentioned causes. S. aureus was identified in a small proportion of children with CAP in China, but S. aureus is an uncommon cause of CAP and is usually found in hospital-acquired pneumonia in the West. Bordetella pertussis can cause severe pneumonia, particularly in the first 6 months of life.7 However, because of the lack of high-quality specialized pertussis surveillance and of available data obtained through research in China, the true level of the pneumonia disease burden caused by pertussis is largely unknown. In contrast to adult pneumonia, Legionella sp. is rarely identified in children, which is consistent with published studies from other countries.65,66
RSV is the major cause of viral CAP, especially in the first year of life, and the substantial CAP-related morbidity and mortality of children could be associated with RSV in China, as reported in studies from other countries.67,68 Since the influenza positivity rate was high in children, a substantial burden on the health care system could be attributed to influenza viruses, especially in a large country such as China. This is consistent with the reported estimates of influenza disease burden based on studies in China and throughout the world.67,69 Parainfluenza virus and adenovirus were the most common pathogens identified in children under 5 y of age. These data are important for informing public health policy officials, and could be helpful in estimating disease burdens associated with these pathogens, guiding priorities for future research and the allocation of resources to control infectious diseases.
The proportions of M. pneumoniae varied greatly, though less than in recent European studies (27–36%).70,71 C. pneumoniae appears to be responsible for 3% of cases when it was specifically looked for. M. pneumoniae was mostly identified in older children, whereas C. pneumoniae was often identified in infants.
It is crucial to select appropriate diagnostic tests and empirical treatments of CAP, which depends on knowledge of the commonly identified pathogens and the results of therapeutic trials. Although the available etiological data from China are limited, studies suggest that the use of empirical guidelines based on other countries may be inappropriate. When treating gram-negative pneumonia, insufficiently broad antibiotic coverage may result in avoidable morbidity and mortality. However, the excessive use of broad-spectrum antibiotics increases healthcare costs and financial burdens and contributes to the recent problem of antibiotic resistance in China.
Biases in these reports that require consideration include geographical or incidental variation in different study periods. Furthermore, significant variations in diagnostic techniques and diagnostic criteria occurred in many study. Due to the heterogeneity between studies, all the weighted average detection rates were estimated using a random effects model. It has been reported that heterogeneity cannot be avoided in a meta-analysis, particularly in one based on etiological detection.
Limitations of this review include the following: 1) A variety of laboratory tests were used to establish etiological diagnoses of CAP. It is therefore difficult to compare etiologies of CAP between published studies. In many children with CAP, more than 2 pathogens may be identified in diagnostic testing, including viral and bacterial combinations, which makes it difficult to determine the significance of any single pathogen.55,72 2) There were constraints in determining etiologies based on available methods. Most bacterial pathogens were isolated from NA and sputum cultures; this could represent colonization rather than infection. However, NA and sputum culturing are still recommended by many hospitals and experts in China for the diagnosis and control of bacterial pathogens, such as S. pneumoniae.73 Most blood cultures obtained from children undergoing antimicrobial therapy before hospitalization are free of bacteria, and the likelihood of a positive blood culture in children with CAP was less than 3% in American studies.74,75 Blood cultures are not recommended in the guidelines for the management of CAP in children released by the Chinese Pediatric Society76 and were not routinely performed in all children hospitalized with CAP. 3) Etiology (sub)-typing or serotyping were not performed systematically and were not reviewed. 4) Due to the development of the immune system and age-related exposure, infections caused by bacteria and viruses are different, and the proportion of CAP caused by several pathogens showed significant variability among age groups.6 However, most studies lacked data on specific age groups and could not be reviewed. 5) There are less routine etiological detection methods for the outpatient cases of CAP in China; therefore, the data in articles reviewed were obtained only from the inpatients cases.
The major findings of this review include the following: 1) Although this review has some limitations, the studies reviewed represent most areas of China and therefore, the results reflect the etiologies of pneumonia to a certain extent in Chinese children under 5 y of age and provide important background information concerning the etiology of CAP in China. 2) The data on the spectrum of etiologies can be used to estimate disease burdens associated with these pathogens, helping to guide priorities of future research and to allocate resources to reduce the incidence of pneumonia. 3) The weighted average detection rates of S. pneumoniae, Hib and influenza by age were estimated in the studies reviewed here, which could provide reference data for further cost-effectiveness analyses of new vaccine development and implementation. 4) The available etiological data from this review has major implications for determining diagnostic strategies and empirical treatments.
Conclusion
To date, this article provides the most comprehensive analysis of the contributing causes of CAP in children under 5 y of age. S. pneumoniae, Hib and Influenza were the most common vaccine preventable disease in children, and corresponding vaccines should be introduced into Chinese immunization programs, and further economic evaluations should be conducted. RSV is common in children, and preventative measures could have a substantial impact on public health. These data also have major implications for diagnostic strategies and empirical treatment.
Method
Search strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement.77 The PubMed (www.ncbi.nlm.nih.gov/pubmed, United States), Embase (www.embase.com, Netherlands), Web-of Science (www.webofknowledge.com, Canada), Wanfang Data (www.wanfangdata.com, China) and CNKI (National Knowledge Infrastructure, www.cnki.net, China) databases were searched for all studies on CAP in children under 5 y of age published in Chinese and English between the years 2001 and 2015. The medical subject heading (MeSH) terms were as follows: “pneumonia,” “respiratory tract infections,” and “China.” Before the literature search, a pilot study was performed to revise the MeSH terms and combinations, especially when the terms were translated to Chinese, before searching Wanfang Data and CNKI.
The articles cited in the identified manuscripts were also searched and added to the review. The reference lists of the retrieved papers were downloaded and searched for additional relevant studies.
Definitions
The following definitions for pneumonia were used in the studies: (1) the pneumonia definition as defined by the WHO,78 (2) guidelines for the management of CAP in children released by the Chinese Pediatric Society of the Chinese Medical Association,76 and (3) physician assessments with or without chest X-ray findings. Additional signs and symptoms for these case definitions are detailed in supplementary file 6.
Suspected CAP was defined as children < 5 y of age with any one of the first 4 signs, symptoms, or laboratory tests results described below, accompanied by the conditions described in the criteria 5 and 6: (1) Recent cough or sticky sputum, with or without pleural pain; (2) fever; (3) consolidation from physical examination and/or moist rales; (4) WBC > 10 × 109/L or WBC < 4 × 109/L, with or without a left nucleus shift; (5) flaky, patchy infiltrative shadows or lung mesenchymal changes in a chest radiograph, with or without pleural effusion; (6) no diagnoses of tuberculosis, pulmonary tumor, noninfectious interstitial pulmonary disease, pulmonary edema, pulmonary embolism, atelectasis, embolism, pulmonary infiltrate with eosinophilia syndrome or pulmonary vasculitis.
Review strategy and data extraction
MedRef® (V4.7, King YEE, Inc., Beijing, China) bibliographic software was used to compile an electronic library of references identified through the database searches. PubMed, Embase and Web-of Science searches were made in MedRef®, and duplicate records were deleted. If the same data were published in Chinese and English, the article in English was used. Every study was assigned a unique ID to enable tracking of reviews and analyses before title/abstract screening.
Data were independently extracted into standardized forms (Microsoft Excel; Microsoft, Redmond, Washington, USA) by 3 reviewers, which included the first author, title, year of publication, setting, journal information, study design, specimen type, diagnostic testing, age group, results, evaluate ratings, and other relevant data.
Inclusion and exclusion criteria
All studies published in the Chinese and English identified from the databases defined above were assessed.
The inclusion criteria for studies were as follows: (1) study of CAP or ALRI, (2) enrollment of children under 5 y of age, (3) published between January 2001 and December 2015, (4) data collection beginning in the year 2001 and later, (5) conducted in mainland China, (6) consistent testing for at least 2 specific etiologies in enrolled patients, (7) ≥ 100 inpatient cases, and (8) ≥ 12 calendar months of surveillance.
The exclusion criteria were as follows: (1) studies of case reports (single case), therapies, case-control populations, pure basic research, clinical diagnostic methods, policy analysis, health education or hospital-acquired pneumonia (pneumonia that occurs 48 hours or more after admission and did not appear to be incubating at the time of admission); (2) studies not published in a core journal (as evaluated by the Institute of Scientific and Technical Information of China); (3) age groups or total number of cases not specified.
Quality assessment
Three trained reviewers performed the title/abstract screenings, and full text screenings were then assigned to 2 groups. Quality assessment was performed by 2 reviewers independently Discrepancies were resolved through discussion.
A 3-point quality scoring system (2 = well, 1 = poorly, 0 = not) was used to rate the following 8 requirements from the Strengthening the Reporting of Observational Studies in Epidemiology statement79: (1) study participants, (2) study setting, (3) definitions for pneumonia, (4) specimen sources, (5) detection methods and quality control, (6) sample size, (7) results, and (8) discussion and interpretation.
Statistical analysis
R (V3.3.2, Vienna, Austria) statistical software and the “meta” package80 were used to estimate the weighted average detection rate and 95% CI of each pathogen. The Q statistic was used to evaluate heterogeneity between studies and the percentage of variation across studies due to heterogeneity was estimated using the I2 index.81 Random effect models were used to calculate the weighted average rate in all analyses.
Ethics
No ethical review was required because all results were from published literature.
Supplementary Material
Abbreviations
- ADV
adenovirus
- APAAP
alkaline phosphatase-anti-alkaline phosphatase technique
- CAP
community-acquired pneumonia
- DFA
direct fluorescent assay
- E. aerogenes
Enterobacter aerogenes
- E. cloacae
Enterobacter cloacae
- E. coli
Escherichia coli
- H. influenza
Haemophilus influenza
- HBoV
human bocavirus
- HCoV
human coronaviruses
- Hib
Haemophilus influenzae type b
- hMPV
human metapneumovirus
- HRV
human rhinovirus
- IFA
indirect fluorescent assay
- K. Pneumoniae
Klebsiella Pneumoniae
- LA
lung aspirates
- LAT
latex agglutination test
- MC
Moraxella catarrhalis
- NA
nasal aspirate
- P. aeruginosa
Pseudomonas aeruginosa
- PCV
pneumococcal conjugate vaccine
- PIV
parainfluenza virus
- RSV
respiratory syncytial virus
- S. marcescens
Serratia marcescens
- S. pneumonia
Streptococcus pneumoniae
- S.aureus
Staphylococcus aureus
Disclosure of potential conflicts of interest
No potential conflicts of interest were disclosed.
Author contributions
GN and WY conceived the systematic review and designed the protocol. XW DW and YL performed the review and extracted the data. GN and ZY analyzed the data. HW and WY provided senior supervision for the systematic review. GN and WY drafted and revised the article.
References
- [1].Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, Abraham J, Adair T, Aggarwal R, Ahn SY, et al.. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380(9859):2095-128. doi: 10.1016/S0140-6736(12)61728-0. PMID:23245604 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Zhou M, Wang H, Zhu J, Chen W, Wang L, Liu S, Li Y, Wang L, Liu Y, Yin P, et al.. Cause-specific mortality for 240 causes in China during 1990–2013: a systematic subnational analysis for the Global Burden of Disease Study 2013. Lancet. 2016;387(10015):251-72. doi: 10.1016/S0140-6736(15)00551-6. PMID:26510778 [DOI] [PubMed] [Google Scholar]
- [3].Guan X, Silk BJ, Li W, Fleischauer AT, Xing X, Jiang X, Yu H, Olsen SJ, Cohen AL. Pneumonia incidence and mortality in Mainland China: systematic review of Chinese and English literature, 1985–2008. PLoS One. 2010;5(7):e11721. doi: 10.1371/journal.pone.0011721 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].He C, Kang L, Miao L, Li Q, Liang J, Li X, Wang Y, Zhu J. Pneumonia mortality among children under 5 in China from 1996 to 2013: An analysis from National Surveillance System. PLoS One. 2015;10(7):e0133620. doi: 10.1371/journal.pone.0133620. PMID:26186717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Harris M, Clark J, Coote N, Fletcher P, Harnden A, McKean M, Thomson A, British Thoracic Society Standards of Care C. British Thoracic Society guidelines for the management of community acquired pneumonia in children: update 2011. Thorax. 2011;66 Suppl 2:ii1-23. doi: 10.1136/thoraxjnl-2011-200598. PMID:21903691 [DOI] [PubMed] [Google Scholar]
- [6].McIntosh K. Community-acquired pneumonia in children. N Engl J Med. 2002;346(6):429-37. doi: 10.1056/NEJMra011994. PMID:11832532 [DOI] [PubMed] [Google Scholar]
- [7].Walker CL, Rudan I, Liu L, Nair H, Theodoratou E, Bhutta ZA, O'Brien KL, Campbell H, Black RE. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381(9875):1405-16. doi: 10.1016/S0140-6736(13)60222-6. PMID:23582727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].WHO Immunization schedule by vaccine in the Immunization, Vaccines and Biologicals. 2015 revision. Available from: http://www.who.int/entity/immunization/monitoring_surveillance/data/schedule_data.xls?ua=1. Accessed 01 December 2016.
- [9].Maurer KA, Chen HF, Wagner AL, Hegde ST, Patel T, Boulton ML, Hutton DW. Cost-effectiveness analysis of pneumococcal vaccination for infants in China. Vaccine. 2016;34(50):6343-49. doi: 10.1016/j.vaccine.2016.10.051. PMID:27810315 [DOI] [PubMed] [Google Scholar]
- [10].Mo X, Gai Tobe R, Liu X, Mori R. Cost-effectiveness and Health Benefits of Pediatric 23-valent Pneumococcal Polysaccharide Vaccine, 7-valent Pneumococcal Conjugate Vaccine and Forecasting 13-valent Pneumococcal Conjugate Vaccine in China. Pediatr Infect Dis J. 2016;35(11):e353-61. doi: 10.1097/INF.0000000000001288. PMID:27753771 [DOI] [PubMed] [Google Scholar]
- [11].Caldwell R, Roberts CS, An Z, Chen CI, Wang B. The health and economic impact of vaccination with 7-valent pneumococcal vaccine (PCV7) during an annual influenza epidemic and influenza pandemic in China. BMC Infect Dis. 2015;15(1):284. doi: 10.1186/s12879-015-1021-x. PMID:26206275 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Hvistendahl M. Public health. China takes aim at rampant antibiotic resistance. Science. 2012;336(6083):795. doi: 10.1126/science.336.6083.795. PMID:22605727 [DOI] [PubMed] [Google Scholar]
- [13].Yiwen G, Yuhua Z, Yuanping M, Ming Z, Jingheng L. Etiology analysis of infant community-acquired pneumonia in Meizhou area. China Modern Doctor. 2015;53(1):52-4. [Google Scholar]
- [14].Huixuan M, Lin S, Xirong W, Yingjia L, Yan G, Qinjing L, Hao W, Weiwei J, Lanqin C, Qingqin Y, et al.. The etiology of community-acquired pneumonia in hospitalized children of single center in Beijing. Chinese Journal of Evidence Based Pediatrics. 2015;10(5):361-5. doi: 10.3969/j.issn.1673-5501.2015.05.008 [DOI] [Google Scholar]
- [15].Peng Y, Shu C, Fu Z, Li QB, Liu Z, Yan L. Pathogen detection of 1613 cases of hospitalized children with community acquired pneumonia. Chin J Contemp Pediatr. 2015;17(11):1193-9. [PubMed] [Google Scholar]
- [16].Lihong P, Yunqi G, Yunlan G. Microbiological etiology of community acquired pneumonia in children J Appl Clin Pediatr. 2011;26(22):1740-1. doi: 10.3969/j.issn.1003-515X.2011.22.018 [DOI] [Google Scholar]
- [17].Liu XT, Wang GL, Luo XF, Chen YL, Ou JB, Huang J, Rong JY. Spectrum of pathogens for community-acquired pneumonia in children. Chin J Contemp Pediatr. 2013;15(1):42-5. [PubMed] [Google Scholar]
- [18].Wang YJ, Liu J, Fang F, He LY, Li JM, Zhang Q, Fu Y, Xiao YQ. Microbiological etiology in children with community acquired pneumonia. Chin J Contemp Pediatr. 2010;12(3):184-7. [PubMed] [Google Scholar]
- [19].Lei G, Xiaoguo D. Pathogens and antibiotic resistance in children with community-acquired pneumonia in our hospital. Journal of Pediatric Pharmacy. 2014;20(7):42-5. [Google Scholar]
- [20].Ming Q, Man T, Wen X, Hui-yun W, Sheng-yun S, Qian C. Etiology of community-acquired pneumonia in children. Journal of Clinic Pediatrics. 2008;26(4):312-5. doi: 10.3969/j.issn.1000-3606.2008.04.013 [DOI] [Google Scholar]
- [21].Lianqiao L, Qionghua C, Yilin Y, Weilin P, Zhibin L. Drug resistance situation and etiology characteristics analysis of children with community-acquired pneumonia in Quanzhou area. Chinese Community Doctors. 2015;31(4):106-10. doi: 10.3969/j.issn.1007-614x.2015.4.65 [DOI] [Google Scholar]
- [22].Guochang Z, Xiaohong W, Qirong Z. Etiology and clinical epidemiology of children with acute pneumonia in Shanghai area. Chinese Journal of Infection and Chemotherapy. 2003;3(3):134-7. doi: 10.3321/j.issn:1009-7708.2003.03.002 [DOI] [Google Scholar]
- [23].Libo W, Mingzhi Z, Haiyan F, Xiaobo Z, Cifang R. Distribution of nasopharyngeal pathogen by age group in children with community acquired pneumonia. Chinese Journal of Infection and Chemotherapy. 2005;5(4):218-21. doi: 10.3321/j.issn:1009-7708.2005.04.007 [DOI] [Google Scholar]
- [24].Yongping Z, Deshui N, Jinhua X, Yonghong Z, Yonghua Z, Jing Z. Pathogenic analysis of community acquired pneumonia in 309 hospitalized children. Journal of Ningxia Medical University. 2015;37(8):931-3. doi: 10.16050/j.cnki.issn1674-6309.2015.08.017 [DOI] [Google Scholar]
- [25].Liying H, Yuejie Z, Jikui D, Ruizhen Z. Bacterial etiology and antimicrobial resistance patterns of community-acquired pneumonia in hospitalized children in Shenzhen. Chinese Journal of Microecology. 2008;20(6):586-8. doi: 10.3969/j.issn.1005-376X.2008.06.025 [DOI] [Google Scholar]
- [26].Yuqing W, Wei J, Zhengrong C, Aili Z. Study on etiology of acute pneumonia in children in Suzhou area. Journal of Applied Clinical Pediatrics. 2007;22(10):743-4,50. doi: 10.3969/j.issn.1003-515X.2007.10.009 [DOI] [Google Scholar]
- [27].Wu JG, Zhang Y, Gong HJ. Drug resistance of pathogens in infants with community acquired pneumonia from the south suburb of Xi'an. Chin J Contemp Pediatr. 2008;10(6):749-751. [PubMed] [Google Scholar]
- [28].Jianqiu L, Kunxia L, Qing C, AImin L. Etiology and antimicrobial resistance of community-acquired pneumonia in Yantai area. Chinese Pediatric Emergency Medicine. 2007;14(6):533-5. doi: 10.3760/cma.j.issn.1673-4912.2007.06.024 [DOI] [Google Scholar]
- [29].Dangyu O. Etiological analysis on community-acquired pneumonia of children hospitalized in Yueyang. Clinical Focus. 2013;28(11):1267-69. doi: 10.3969/j.issn.1004-583X.2013.11.023 [DOI] [Google Scholar]
- [30].Zheng-xiu L, En-mei L, Zhou F, Kun-hua C. Etiology and antimicrobial resistance of children with community-acquired pneumonia in Chongqing area. Journal of Pediatric Pharmacy. 2005;11(1):4-6. doi: 10.3969/j.issn.1672-108X.2005.01.002 [DOI] [Google Scholar]
- [31].Ying F, Zhengxiu L, Zhou F, Jian L, Enmei L. Etiology of children with community acquired pneumonia in Chongqing area. Journal of Pediatric Pharmacy. 2011;17(5):39-42. [Google Scholar]
- [32].Jieming O, Jinghong L, Haibin Y. Etiology research of children with community-acquired pneumonia in Zhuhai. Modern Medicine Journal of China. 2014;16(1):54-7. [Google Scholar]
- [33].Zhang Q, Guo Z, MacDonald NE. Vaccine preventable community-acquired pneumonia in hospitalized children in Northwest China. Pediatr Infect Dis J. 2011;30(1):7-10. doi: 10.1097/INF.0b013e3181ec6245. PMID:20625346 [DOI] [PubMed] [Google Scholar]
- [34].Cuizhen H, Guifeng C, Guangling P. Resistance analysis on 1030 isolates form children with pneumonia. Hainan Medical Journal. 2005;16(7):143-44. doi: 10.3969/j.issn.1003-6350.2005.06.096 [DOI] [Google Scholar]
- [35].Nan M, Aihua W, Baoquan Z. Pathogens and antibiotic resistance of community-acquired pneumonia in Children aged under 5 years old in Lanzhou. Chinese Journal of Obstetrics & Gynecology and Pediatrics(Electronic Edition). 2012;8(1):28-31. doi: 10.3877/cma.j.issn.1673-5250.2012.01.007 [DOI] [Google Scholar]
- [36].Yi C, Guozhang X, Rui M, Bo Y, Ting F, Qunying C, Yiping W, Aihuan S. A study on the epidemic of pneumonia among children in Ningbo city, Zhejiang province, 2009–2012. Chinese Journal of Preventive Medicine. 2014;48(12):1053-56. doi: 10.3760/cma.j.issn.0253-9624.2014.12.007 [DOI] [PubMed] [Google Scholar]
- [37].Li C, Dong W. Pathogens distribution and drug sensitivity on deep sputum culture from 212 cases of pneumonia. Journal of Pediatric Pharmacy. 2011;17(6):57-8. [Google Scholar]
- [38].Chuanxu X, Dongliang C, Yan C. Analysis on pathogens and drug susceptibility testing of community-acquired pneumonia in 428 children. Guide of China Medicine. 2013;11(1):541-3. [Google Scholar]
- [39].Tao L, Shi C, Ling W. Distribution and drug resistance of pathogens causing community-acquired pneumonia in children. Chinese Journal of Nosocomiology. 2014;24(2):483-5. [Google Scholar]
- [40].Jianshan H, Lixin H, Haixia M, Zengrong Y, Jinping S. A survey on bacterial etiology and drug resistance from community-acquired pneumonia of Children under 5 years in Fangshan. Maternal & Child Health Care of China. 2014;29(3):427-9. doi: 10.7620/zgfybj.j.issn.1001-4411.2014.03.36 [DOI] [Google Scholar]
- [41].Jingpo Z, Yanyang Z, Jianwei K, Zhongying S. Analysis on pathogen detected from community acquired pneumonia of children under 5 years in Nanyang. Chinese Journal of Practical Pediatrics. 2006;21(8):613-5. doi: 10.3969/j.issn.1005-2224.2006.08.021 [DOI] [Google Scholar]
- [42].Yunfeng L. Analysis on pathogen detected from community acquired pneumonia in Ninghai county. Journal of Hebei Medical University. 2012;33(2):211-3. doi: 10.3969/j.issn.1007-3205.2012.02.038 [DOI] [Google Scholar]
- [43].Rong H, Ruiyun C, Lili Z, Han H, Bing Z, Yun L. Etiology and drug sensitivity analysis on children with pneumonia. Journal of Chinese Physician. 2006;8(6):975-6. doi: 10.3760/cma.j.issn.1008-1372.2006.07.062 [DOI] [Google Scholar]
- [44].Shenjian Z. Analysis of bacterial distribution and drug resistance in community acquired pneumonia of children under 5 years old in Xiaogan area. Journal of Clinical Medicine in Practice. 2015;19(11):70-73+84. doi: 10.7619/jcmp.201511021 [DOI] [Google Scholar]
- [45].Yanxia Y, Chunyi L, Weidong H, Shuiwen C, Qiang L. Bacteriological pathogenic spectrum of children with severe pneumonia and its drug resistance. Practical Journal of Cardiac Cerebral Pneumal and Vascular Disease. 2015;23(11):90-2. doi: 10.3969/j.issn.1008-5971.2015.11.026 [DOI] [Google Scholar]
- [46].Shuiwen C, Chunyi L, Weidong H, Qixiu R, Ziqiang L, Hongbo X. Pathogenic spectrum and bacterial resistance of severe community-acquired pneumonia. Chinese Pediatric Emergency Medicine. 2013;20(3):273-6. doi: 10.3760/cma.j.issn.1673-4912.2013.03.011 [DOI] [Google Scholar]
- [47].Xiaofang D, Bing Z, Lili Z, Niguang X, Qionghua Z, ZhaoJun D, ZhiPing X, HanChun G. An analysis of viral etiology in 100 cases of severe community-acquired pneumonia in hospitalized children. Journal of Clinical Pediatrics. 2012;30(9):857-61. doi: 10.3969/j.issn.1000-3606.2012.09.014 [DOI] [Google Scholar]
- [48].Yi C, Guangwan L, Yingying Z, Tao L, Li D, Jiayu Z, Mingqi Z, Xiaomin L, Liang H, Bing Z. Etiology of community-acquired pneumonia among pediatric inpatients in Guangzhou during 2012 and 2013. Chinese Journal of Clinical Infectious Diseases. 2014;7(6):521-5. doi: 10.3760/cma.j.issn.1674-2397.2014.06.008 [DOI] [Google Scholar]
- [49].Lijie C, Tao M, Haiting L, Hongquan L. Investigation on non-bacterial etiology of community acquired pneumonia in children in Chengdu. Laboratory Medicine and Clinic. 2009;6(16):1368-9. doi: 10.3969/j.issn.1672-9455.2009.16.031 [DOI] [Google Scholar]
- [50].Quanxin Z, Bin Z, Aihong Y, Feng L. Virological research on community-acquired pneumonia in children. China Prcatical Medicine. 2007;2(21):103-4. doi: 10.3969/j.issn.1673-7555.2007.21.103 [DOI] [Google Scholar]
- [51].Zhibin L, Lianqiao L, Qionghua C, Jingyang Z, Qingliu F. Viral etiology investigation of children community acquired pneumonia in Quanzhou area. Chinese Community Doctors. 2015;31(4):102-5. doi: 10.3969/j.issn.1007-614x.2015.4.63 [DOI] [Google Scholar]
- [52].Fengmei W, Yunchun L, Yanyan Z, Lidan X. A study of viral etiology of inpatients below 5 years old with community acquired pneumonia in Wenzhou. Zhejiang Journal of Preventive Medicine. 2011;23(2):17-9. doi: 10.3969/j.issn.1007-0931.2011.02.006 [DOI] [Google Scholar]
- [53].Zhanghua Z, Wei T, Suoying W. Etiologic features of hospitalized children with pneumonia in Zhenjiang area. Modern Medical Journal. 2015;43(11):1396-9. [Google Scholar]
- [54].Jin Y, Zhang RF, Xie ZP, Yan KL, Gao HC, Song JR, Yuan XH, Cheng WX, Hou YD, Duan ZJ. Newly identified respiratory viruses associated with acute lower respiratory tract infections in children in Lanzou, China, from 2006 to 2009. Clin Microbiol Infect. 2012;18(1):74-80. doi: 10.1111/j.1469-0691.2011.03541.x. PMID:21767329 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Feng L, Li Z, Zhao S, Nair H, Lai S, Xu W, Li M, Wu J, Ren L, Liu W, et al.. Viral etiologies of hospitalized acute lower respiratory infection patients in China, 2009–2013. PLoS One. 2014;9(6):e99419. doi: 10.1371/journal.pone.0099419. PMID:24945280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Tang LF, Wang TL, Tang HF, Chen ZM. Viral pathogens of acute lower respiratory tract infection in China. Indian Pediatr. 2008;45(12):971-5. PMID:19129564 [PubMed] [Google Scholar]
- [57].Bradley JS, Byington CL, Shah SS, Alverson B, Carter ER, Harrison C, Kaplan SL, Mace SE, McCracken GH Jr., Moore MR, et al.. The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis. 2011;53(7):e25-76. doi: 10.1093/cid/cir531. PMID:21880587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].Ning W, Zhijie A, Huaqing W. A Systematic Review of the Serotype Distribution of Streptococcus Pneumoniae(pneumococcus)among all Cases under 18 Years Old of Pneumococcal Infection in China. Chinese Journal of Vaccines and Immunization. 2014; 20(6):547-54. [Google Scholar]
- [59].Ping Y, Jingshan Z, Lei C, Shicheng G, Jian C. Analysis of Category Ⅱ Vaccine Utilization using Data from the Immunization Monitoring System in China, 2013. Chinese Journal of Vaccines and Immunization. 2014;20(6):499-504. [Google Scholar]
- [60].Don M, Fasoli L, Paldanius M, Vainionpaa R, Kleemola M, Raty R, Leinonen M, Korppi M, Tenore A, Canciani M. Aetiology of community-acquired pneumonia: serological results of a paediatric survey. Scand J Infect Dis. 2005;37(11-12):806-12. doi: 10.1080/00365540500262435. PMID:16308213 [DOI] [PubMed] [Google Scholar]
- [61].Michelow IC, Olsen K, Lozano J, Rollins NK, Duffy LB, Ziegler T, Kauppila J, Leinonen M, McCracken GH Jr.. Epidemiology and clinical characteristics of community-acquired pneumonia in hospitalized children. Pediatrics. 2004;113(4):701-7.doi: 10.1542/peds.113.4.701. PMID:15060215 [DOI] [PubMed] [Google Scholar]
- [62].WHO WHO position paper on Haemophilus influenzae type b conjugate vaccines. (Replaces WHO position paper on Hib vaccines previously published in the Weekly Epidemiological Record. Wkly Epidemiol Rec. 2006;81(47):445-52. PMID:17124755 [PubMed] [Google Scholar]
- [63].Youning L, Minjun C, Tiemei Z, Hui W. A multicentre study on the pathogenic agents in 665 adult patients with community-acquired pneumonia in cities of China. Chinese Journal of Tuberculosis and Respiratory Diseases. 2006;29(1):3-8. PMID:16638292 [PubMed] [Google Scholar]
- [64].DeAntonio R, Yarzabal J. P, Cruz J. P, Schmidt J. E, Kleijnen J. Epidemiology of community-acquired pneumonia and implications for vaccination of children living in developing and newly industrialized countries: A systematic literature review. Hum Vaccin Immunother. 2016;12(9): 2422-40. doi: 10.1080/21645515.2016.1174356. PMID:27269963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Ng V, Tang P, Jamieson F, Guyard C, Low DE, Fisman DN. Laboratory-based evaluation of legionellosis epidemiology in Ontario, Canada, 1978 to 2006. BMC Infect Dis. 2009;9(1):68. doi: 10.1186/1471-2334-9-68 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Peto L, Nadjm B, Horby P, Ngan TT, van Doorn R, Van Kinh N, Wertheim HF. The bacterial aetiology of adult community-acquired pneumonia in Asia: a systematic review. Trans R Soc Trop Med Hyg. 2014;108(6):326-37. doi: 10.1093/trstmh/tru058. PMID:24781376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [67].Nair H, Nokes DJ, Gessner BD, Dherani M, Madhi SA, Singleton RJ, O'Brien KL, Roca A, Wright PF, Bruce N, et al.. Global burden of acute lower respiratory infections due to respiratory syncytial virus in young children: a systematic review and meta-analysis. Lancet. 2010;375(9725):1545-55. doi: 10.1016/S0140-6736(10)60206-1. PMID:20399493 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].Berkley JA, Munywoki P, Ngama M, Kazungu S, Abwao J, Bett A, Lassauniere R, Kresfelder T, Cane PA, Venter M, et al.. Viral etiology of severe pneumonia among Kenyan infants and children. JAMA. 2010;303(20):2051-57. doi: 10.1001/jama.2010.675. PMID:20501927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [69].Feng L, Shay DK, Jiang Y, Zhou H, Chen X, Zheng Y, Jiang L, Zhang Q, Lin H, Wang S, et al.. Influenza-associated mortality in temperate and subtropical Chinese cities, 2003–2008. Bull World Health Organ. 2012;90(4):279-88B. doi: 10.2471/BLT.11.096958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Korppi M, Heiskanen-Kosma T, Kleemola M. Incidence of community-acquired pneumonia in children caused by Mycoplasma pneumoniae: serological results of a prospective, population-based study in primary health care. Respirology. 2004;9(1):109-14. doi: 10.1111/j.1440-1843.2003.00522.x. PMID:14982611 [DOI] [PubMed] [Google Scholar]
- [71].Kurz H, Gopfrich H, Wabnegger L, Apfalter P. Role of Chlamydophila pneumoniae in children hospitalized for community-acquired pneumonia in Vienna, Austria. Pediatric pulmonology. 2009;44(9):873-6. doi: 10.1002/ppul.21059. PMID:19670403 [DOI] [PubMed] [Google Scholar]
- [72].Wang XF, Liu JP, Shen KL, Ma R, Cui ZZ, Deng L, Shang YX, Zhao DY, Wang LB, Wan LY, et al.. A cross-sectional study of the clinical characteristics of hospitalized children with community-acquired pneumonia in eight eastern cities in China. BMC Complement Altern Med. 2013;13(1):367. doi: 10.1186/1472-6882-13-367. PMID:24364897 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Sanjie Y, Hui W, Xuzhuang S, Yuxing N, Chuanqing W, Fan Y. Expert consensus document on clinical laboratory procedures of Streptococcus pneumoniae. CHin J Lab Med. 2012;35(12):6. doi: 10.3760/cma.j.issn.1009-9158.2012.12.003 [DOI] [Google Scholar]
- [74].Hickey RW, Bowman MJ, Smith GA. Utility of blood cultures in pediatric patients found to have pneumonia in the emergency department. Ann Emerg Med. 1996;27(6):721-5. doi: 10.1016/S0196-0644(96)70189-0. PMID:8644958 [DOI] [PubMed] [Google Scholar]
- [75].Shah SS, Dugan MH, Bell LM, Grundmeier RW, Florin TA, Hines EM, Metlay JP. Blood cultures in the emergency department evaluation of childhood pneumonia. Pediatr Infect Dis J. 2011;30(6):475-9. doi: 10.1097/INF.0b013e31820a5adb. PMID:21206393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [76].Subspecialty Group of Respiratory Diseases , The Society of Pediatrics Chinese Medical Association. Guidelines for management of community acquired pneumonia in children (the revised edition of 2013) Chin J Pediatr. 2013;51(10):745-52. [PubMed] [Google Scholar]
- [77].Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. PMID:19621072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].WHO Technical bases for the WHO recommendations on the management of pneumonia in children at first-level health facilities. Geneva: World Health Organization; 1991. [Google Scholar]
- [79].Gallo V, Egger M, McCormack V, Farmer PB, Ioannidis JP, Kirsch-Volders M, Matullo G, Phillips DH, Schoket B, Stromberg U, et al.. Strengthening the reporting of observational studies in epidemiology–molecular epidemiology (STROBE-ME): an extension of the STROBE statement. PLoS Med. 2011;8(10):e1001117. doi: 10.1371/journal.pmed.1001117. PMID:22039356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [80].Meta Schwarzer G.: An R package for meta-analysis. R News. 2007;7(3):40-5. [Google Scholar]
- [81].Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414): 557-60. doi: 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


