ABSTRACT
Purpose: Gaps remain in the public's knowledge of the human papillomavirus (HPV). We assessed racial/ethnic and gender disparities in knowledge and awareness of HPV and the HPV vaccine among US adults.
Methods: Data from the Health Information National Trends Survey 4 Cycle 3 (September – December 2013) and Cycle 4 (August – November 2014) were analyzed for 6,862 respondents aged 18 years and older. Weighted multivariable logistic regression models were used to estimate racial/ethnic and gender disparities in HPV knowledge and HPV vaccination awareness.
Results: Sixty-six percent of respondents had heard of HPV and the HPV vaccine (57% of men vs. 75% of women). In multivariable analyses, compared with men, women were 225% (95% CI: 2.60 – 4.07) more likely to have heard of HPV, and 281% (95% CI: 3.06 – 4.74) more likely to have heard of the HPV vaccine. Non-Hispanic Blacks were 33% (95% CI: 0.47 – 0.96) and 44% (95% CI: 0.39 – 0.81) less likely than non-Hispanic Whites to have heard of HPV and the HPV vaccine, respectively. Hispanics were 27% (95% CI: 0.52 – 1.02) and 53% (95% CI: 0.34 – 0.64) less likely than non-Hispanic Whites to have heard of HPV and the HPV vaccine, respectively.
Conclusions: There was evidence of disparities in HPV and HPV vaccine awareness among men compared with women and non-Hispanic Blacks and Hispanics compared with non-Hispanic Whites. To foster improvements in HPV vaccine uptake and reduce disparities in HPV associated cancers, future interventions must target men and minority populations, for whom knowledge gaps exist.
KEYWORDS: gender, HPV, HPV vaccine, knowledge and awareness, race
Introduction
Human papillomavirus (HPV) is the most common sexually transmitted infection in the United States (US), with nearly 80 million people currently infected.1 Although most subtypes are cleared by the body without any harm,2 there are a few oncogenic types associated with virtually all cases of cervical, 95% of anal, 73% of oropharyngeal, 65% of vaginal, 50% of vulvar, and 35% of penile cancers.3,4 Additionally, HPV-associated oropharyngeal cancer, a distinct subset of head and neck cancer, has grown more than 225% in incidence in the last 3 decades,4 and it is the most common HPV-associated cancer in men. The burden of cervical cancer remains substantial, especially among non-Hispanic Black and Hispanic women compared with non-Hispanic White women.5 For example, compared with non-Hispanic White women, incidence and mortality from cervical cancer are 25% and 95% greater, respectively, for non-Hispanic Blacks, and 53% and 41% greater, respectively, for Hispanics.6
The Advisory Committee on Immunization Practices (ACIP) first recommended a quadrivalent HPV vaccine in 2006, and a bivalent vaccine in 2009.7 In 2015, a nonavalent HPV vaccine was approved,8 and has become the mainstay HPV vaccine used in the United States since the end of 2016.9 These HPV vaccines protect against 70–90% of cervical cancer causing HPV types as well as other male related HPV-associated cancers such as penile, anal, and potentially oropharyngeal cancers.7,8,10,11 Although the HPV vaccine was first recommended in 2006 for girls and 2011 for boys, disparities in knowledge and awareness about HPV and the HPV vaccine persist, and vaccination rates remain suboptimal. While the current vaccine completion rates among girls aged 13–17 years is 42%, among boys it is 28%.12 If current trends in HPV vaccination uptake continue, the Healthy People 2020 goal of 80% HPV vaccine completion rates among eligible girls and boys will not be met.13
While not universally accepted, one of the suggested interventions to improve HPV vaccine uptake is increasing HPV and HPV vaccine knowledge.14-16 Previous studies have demonstrated that HPV knowledge and awareness is associated with interest in receiving the HPV vaccine,17 acceptance of the HPV vaccine,18 intent to receive the HPV vaccine,19 and actual uptake of the HPV vaccine.20 Similarly, HPV awareness among parents of adolescent children is associated with a greater interest in having one's child vaccinated.17 Yet, HPV knowledge and awareness remains relatively low, especially among minorities,17,21,22 and conversations around HPV and HPV vaccine are often female-centered.23 Given the importance of HPV knowledge and awareness in vaccine uptake, current and reliable estimates of HPV knowledge and awareness among racial minorities, who have significantly greater incidence of and mortality from cervical cancer, and men are needed.
Our objective was to assess racial/ethnic and gender disparities in knowledge and awareness of HPV and the HPV vaccine among US adults. Examining the role of inequalities in HPV awareness and knowledge may help target interventions to achieve greater levels of vaccine uptake and reduce HPV associated cancer disparities.
Results
Table 1 summarizes weighted characteristics of the 6,862 survey respondents. The average age among the overall sample of adults was 54 years (standard deviation [SD] = 16 years), among the subgroup of adults who had children aged between 9 and 27 years in the household was 42 years (SD = 11 years), and among the subgroup of adults less than 55 years old was 41 years (SD = 9 years). Most of the sample were non-Hispanic White (66.8%), married or living as married (57.6%), attained some college education or graduated from college (68.1%), had health insurance (85.2%) and a regular healthcare provider (63.8%), and reported good or excellent health (48.1%). In addition, the majority did not have any children younger than 18 years in their household (63.0%) and reported using the Internet (80.9%).
Table 1.
Weighted, respondent characteristics, HINTS 4, Cycle 3 and 4, 2013–2014 (N = 6,862).
| n | w% | |
|---|---|---|
| Race/Ethnicity | ||
| Non-Hispanic White | 3,544 | 66.8 |
| Non-Hispanic Black | 955 | 10.9 |
| Hispanic | 1,051 | 15.3 |
| Other | 448 | 7.1 |
| Gender | ||
| Male | 2621 | 48.3 |
| Female | 4090 | 51.7 |
| Age | ||
| 18–34 | 893 | 29.0 |
| 35–49 | 1,455 | 28.6 |
| 50–64 | 2,290 | 25.1 |
| 65+ | 1,939 | 17.3 |
| Marital Status | ||
| Married/Living as Married | 3,412 | 57.6 |
| Divorced/Widowed/Separated | 2,051 | 15.8 |
| Never Married | 1,127 | 26.6 |
| Education | ||
| College Graduate | 2,625 | 36.7 |
| Some College | 2,023 | 31.4 |
| High School Graduate | 1,369 | 21.3 |
| Less than High School | 605 | 10.6 |
| Income Level | ||
| $100,000 or more | 1,075 | 20.6 |
| $75,000 to $99,999 | 705 | 13.8 |
| $50,000 to $74,999 | 996 | 17.5 |
| $35,000 to $49,999 | 876 | 14.7 |
| $20,000 to $34,999 | 907 | 13.6 |
| $0 to $19,999 | 1,454 | 19.8 |
| Health Insurance | ||
| Yes | 5,965 | 85.2 |
| No | 786 | 14.8 |
| Regular Healthcare Provider | ||
| Yes | 4,615 | 63.8 |
| No | 2,074 | 36.2 |
| General Health | ||
| Excellent/Very good | 3,007 | 48.1 |
| Good | 2,480 | 38.4 |
| Fair/Poor | 1,158 | 13.5 |
| Number of Children under 18yrs old in Household | ||
| 0 | 4,236 | 63.0 |
| ≥ 1 | 1,734 | 37.0 |
| Use Internet | ||
| Yes | 5,086 | 80.9 |
| No | 1,707 | 19.1 |
w% – weighted percentages; HINTS = Health Information National Trends Survey
Awareness of HPV
Sixty-six percent of respondents had heard of HPV (Figure 1) – 57.1% of men and 74.5% of women (Table 2). Our sensitivity analysis showed a change from 66.0% in the overall proportion of those who had heard of HPV to 71.3% among respondents who were less than 55 years old and 71.4% among those who had children between 9 and 27 years old. Women were 3 times more likely than men to have heard of HPV (aOR = 3.25; 95% CI: 2.60 – 4.07). Non-Hispanic Blacks (aOR = 0.68; 95% CI: 0.47 – 0.98) and those in the “Other race” category (aOR = 0.29; 95% CI: 0.19 – 0.46) were significantly less likely to have heard of HPV compared with non-Hispanic Whites. In the sensitivity analysis including respondents who were less than 55 years old (n = 3,543), the gender and racial/ethnic differences remained. We found that women (aOR = 3.51; 95% CI: 2.60 – 4.75 were more likely to have heard about HPV whereas Hispanics (aOR = 0.63; 95% CI: 0.43 – 0.94) vs. non-Hispanic Whites were less likely to know about HPV. Similarly, when we only included respondents who had children between 9 and 27 years of age (n = 1,734), we again found that women (aOR = 3.07; 95% CI: 2.06 – 4.59) were more likely to have heard about HPV whereas Hispanics (aOR = 0.42; 95% CI: 0.26 – 0.69) vs. non-Hispanic Whites were less likely to know about HPV.
Table 3.
Weighted, adjusted logistic regression models estimating HPV and HPV vaccine awareness, HINTS 4, Cycle 3 and 4, 2013—2014.
| Heard of HPV aOR (95%CI) |
Heard of HPV Vaccine aOR (95%CI) |
|||||
|---|---|---|---|---|---|---|
| Full Sample$ (n = 6,742) | Sensitivity‡ Aged < 55 yrs (n = 3,543) | Sensitivity‡ Child between 9 and 27 (n = 1,458) | Full Sample$ (n = 6,660) | Sensitivity‡ Aged < 55 yrs (n = 3,543) | Sensitivity‡ Child between 9 and 27 (n = 1,452) | |
| Race/Ethnicity | ||||||
| Non-Hispanic White | Ref | Ref | Ref | Ref | Ref | Ref |
| Non-Hispanic Black | 0.68 (0.47 – 0.98)∼ | 0.70 (0.43 – 1.13) | 0.53 (0.28 –0.99)∼ | 0.57 (0.40 – 0.84)# | 0.57 (0.34 – 0.93)∼ | 0.44 (0.23 – 0.84)∼ |
| Hispanic | 0.73 (0.52 – 1.02) | 0.63 (0.43 – 0.94)∼ | 0.42 (0.26 – 0.69)# | 0.49 (0.35 – 0.67)* | 0.41 (0.28 – 0.60)* | 0.41 (0.25 – 0.69)# |
| Other | 0.29 (0.19 – 0.46)* | 0.25 (0.15 – 0.44)* | 0.30 (0.15 – 0.60)# | 0.42 (0.27 – 0.66)# | 0.38 (0.22 – 0.66)# | 0.41 (0.21 – 0.80)# |
| Gender | ||||||
| Male | Ref | Ref | Ref | Ref | Ref | Ref |
| Female | 3.25 (2.60 – 4.07)* | 3.51 (2.60 – 4.75)* | 3.07 (2.06 – 4.59)* | 3.81 (3.06 – 4.74)* | 4.27 (3.17 – 5.74)* | 3.07 (2.08 – 4.55)* |
| Age | ||||||
| 18–34 | Ref | Ref | ||||
| 35–49 | 0.74 (0.52 – 1.05) | 0.69 (0.49 – 0.99)∼ | ||||
| 50–64 | 0.61 (0.43 – 0.87)# | 0.62 (0.44 – 0.89)∼ | ||||
| 65+ | 0.27 (0.18 – 0.40)* | 0.35 (0.23 – 0.52)* | ||||
| Marital Status | ||||||
| Married/Living as Married | Ref | Ref | ||||
| Divorced/Widowed/Separated | 1.20 (0.90 – 1.60) | 0.85 (0.64 – 1.13) | ||||
| Never Married | 1.33 (0.95 – 1.87) | 1.24 (0.87 – 1.76) | ||||
| Education | ||||||
| College Graduate | Ref | Ref | ||||
| Some College | 0.95 (0.71 – 1.27) | 0.95 (0.72 – 1.27) | ||||
| High School Graduate | 0.56 (0.41 – 0.78)# | 0.60 (0.43 – 0.84)# | ||||
| Less than High School | 0.60 (0.37 – 0.97)∼ | 0.93 (0.60 – 1.45) | ||||
| Income level | ||||||
| $100,000 or more | Ref | Ref | ||||
| $75,000 to $99,999 | 0.88 (0.60 – 1.31) | 0.80 (0.54 – 1.19) | ||||
| $50,000 to $74,999 | 0.67 (0.46 – 0.96)∼ | 0.62 (0.43 – 0.88)# | ||||
| $35,000 to $49,999 | 0.80 (0.54 – 1.19) | 0.51 (0.34 – 0.76)# | ||||
| $20,000 to $34,999 | 0.60 (0.39 – 0.92)∼ | 0.44 (0.28 – 0.70)# | ||||
| $0 to $19,999 | 0.51 (0.32 – 0.83)∼ | 0.42 (0.26 – 0.68)# | ||||
| Health Insurance | ||||||
| Yes | Ref | Ref | ||||
| No | 0.75 (0.53 – 1.06) | 1.01 (0.72 – 1.41) | ||||
| Regular Healthcare Provider | ||||||
| Yes | Ref | Ref | ||||
| No | 0.82 (0.63 – 1.07) | 0.69 (0.53 – 0.89)# | ||||
| General Health | ||||||
| Excellent/ Very good | Ref | Ref | ||||
| Good | 0.79 (0.62 – 1.02) | 0.99 (0.78 – 1.26) | ||||
| Fair/Poor | 0.75 (0.53 – 1.05) | 0.87 (0.62 – 1.24) | ||||
| Number of Children under 18yrs old in Household | ||||||
| 0 | Ref | Ref | ||||
| ≥ 1 | 1.15 (0.86 – 1.53) | 1.19 (0.89 – 1.57) | ||||
| Use Internet | ||||||
| Yes | Ref | Ref | ||||
| No | 0.54 (0.4 – 0.74)* | 0.66 (0.49 – 0.90)# | ||||
p-value:
<0.0001
<0.01
<0.05
aOR = Adjusted Odds Ratios; CI = Confidence Interval; HPV = Human papillomavirus; HINTS = Health Information National Trends Survey
Full sample models adjusted for age, gender, race, marital status, education, income level, health insurance, regular healthcare provider, general health, number of children under 18yrs old in household, internet use
Sensitivity models adjusted for age, gender, race, marital status, education, income level, health insurance, regular healthcare provider, general health, number of children under 18yrs old in household, internet use
Figure 1.
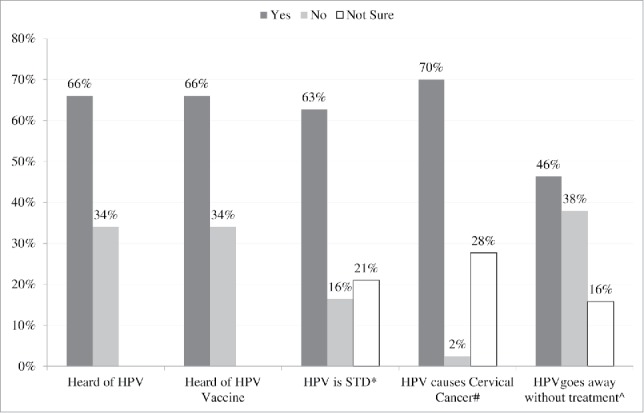
Weighted, unadjusted estimates for HPV awareness and knowledge, HINTS 4 Cycle 3 and 4, 2013—2014 *Correct response is: Yes #Correct response is: Yes ^Correct response is: Yes HPV = Human papillomavirus; STD = Sexually Transmitted Disease; HINTS = Health Information National Trends Survey.
Table 2.
Weighted, unadjusted estimates for HPV knowledge, and awareness stratified by gender and race*gender, HINTS 4, Cycle 3 and 4, 2013–2014, (N = 6,862).
| Gender (w%) |
Race/Ethnicity *Gender (w%) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Male | Female | White Female | Black Female | Hispanic Female | White Male | Black Male | Hispanic Male | |
| Heard of HPV | ||||||||
| Yes | 57.1 | 74.5 | 80.8 | 68.8 | 72.6 | 63.8 | 52.6 | 54.5 |
| No | 42.9 | 25.5 | 19.2 | 31.2 | 27.4 | 36.2 | 47.4 | 45.5 |
| Heard of HPV vaccine | ||||||||
| Yes | 55.2 | 76.4 | 82.8 | 68.0 | 66.8 | 62.8 | 49.8 | 43.9 |
| No | 44.8 | 23.6 | 17.2 | 32.0 | 33.2 | 37.2 | 50.2 | 56.1 |
| HPV is an STD | ||||||||
| Yes | 64.0 | 61.8 | 63.5 | 47.2 | 68.7 | 65.1 | 46.6 | 66.3 |
| No | 14.1 | 18.0 | 17.5 | 31.5 | 13.7 | 14.8 | 20.3 | 10.0 |
| Not Sure | 21.9 | 20.2 | 19.0 | 21.3 | 17.6 | 20.2 | 33.0 | 23.7 |
| HPV causes cervical cancer | ||||||||
| Yes | 66.7 | 72.4 | 73.9 | 66.8 | 72.5 | 69.2 | 52.9 | 62.9 |
| No | 2.1 | 2.6 | 2.2 | 3.2 | 4.1 | 1.5 | 2.7 | 2.1 |
| Not Sure | 31.3 | 25.0 | 23.9 | 30.0 | 23.4 | 29.3 | 44.4 | 35.0 |
| HPV goes away without treatment | ||||||||
| Yes | 45.8 | 46.4 | 45.9 | 46.3 | 51.7 | 45.4 | 51.6 | 44.8 |
| No | 34.6 | 40.5 | 41.7 | 43.1 | 32.3 | 36.3 | 20.3 | 34.2 |
| Not Sure | 19.7 | 13.1 | 12.4 | 10.6 | 16.0 | 18.3 | 28.1 | 21.0 |
w% – weighted percentages; HINTS = Health Information National Trends Survey; HPV = Human papillomavirus
Knowledge of HPV-associated STD and cancers
Seventy percent of respondents who had heard of HPV knew that HPV causes cervical cancer, 27.0% were unsure, and 2.0% inaccurately thought that HPV does not cause cervical cancer (Figure 1). Women (aOR = 1.47; 95% CI: 1.12 – 1.94) were significantly more likely than men to know that HPV causes cervical cancer, but non-Hispanic Blacks (aOR = 0.52; 95% CI: 0.35 – 0.76) compared with non-Hispanic Whites were significantly less likely to know that HPV causes cervical cancer (Table 4). Approximately 63.0% of respondents who had heard of HPV knew that HPV is a STD, 21.0% were unsure, and 16.0% inaccurately believed that it is not a STD (Figure 1). Although not statistically significant, women were more likely than men to know that HPV is a STD. Non-Hispanic Blacks (aOR = 0.48; 95% CI: 0.33 – 0.70) were significantly less likely to know that HPV is a STD compared with non-Hispanic Whites (Table 4). Finally, approximately 46.0% of respondents who had heard of HPV were aware that HPV often clears on its own without treatment, 16.0% were unsure, and 38.0% answered incorrectly that HPV would not go away on its own (Figure 1). There were no significant differences by gender or by race/ethnicity regarding knowledge that HPV will often resolve without treatment (Table 4).
Table 4.
Weighted, adjusted logistic regression models estimating HPV knowledge, HINTS 4, Cycle 3 and 4, 2013—2014.
| HPV Cause Cervical Cancer (n = 4,165) aOR (95%CI) | HPV is an STD (n = 4,179) aOR (95%CI) | HPV goes away on its own (n = 4,133) aOR (95%CI) | |
|---|---|---|---|
| Race/Ethnicity | |||
| Non-Hispanic White | Ref | Ref | Ref |
| Non-Hispanic Black | 0.52 (0.35 – 0.76)# | 0.48 (0.33 – 0.70)* | 1.20 (0.84 – 1.72) |
| Hispanic | 0.83 (0.56 – 1.22) | 1.14 (0.78 – 1.66) | 1.13 (0.79 – 1.60) |
| Other | 0.91 (0.57 – 1.44) | 0.77 (0.50 – 1.18) | 0.82 (0.53 – 1.28) |
| Gender | |||
| Male | Ref | Ref | Ref |
| Female | 1.47 (1.12 – 1.94)# | 1.04 (0.80 – 1.34) | 1.07 (0.84 – 1.36) |
| Age | |||
| 18–34 | Ref | Ref | Ref |
| '35–49 | 0.76 (0.52 – 1.12) | 0.77 (0.55 – 1.09) | 0.93 (0.67 – 1.27) |
| 50—64 | 0.64 (0.43 – 0.96)∼ | 0.62 (0.44 – 0.89)∼ | 1.14 (0.82 – 1.57) |
| 65+ | 0.51 (0.32 – 0.80)# | 0.66 (0.43 – 1.01) | 1.17 (0.79 – 1.74) |
| Marital Status | |||
| Married/Living as Married | Ref | Ref | Ref |
| Divorced/Widowed/Separated | 1.01 (0.75 – 1.36) | 1.19 (0.88 – 1.62) | 1.02 (0.76 – 1.36) |
| Never Married | 1.12 (0.76 – 1.66) | 1.24 (0.87 – 1.79) | 1.03 (0.73 – 1.44) |
| Education | |||
| College Graduate | Ref | Ref | Ref |
| Some College | 0.60 (0.44 – 0.81)# | 0.69 (0.52 – 0.91)∼ | 0.81 (0.61 – 1.06) |
| High School Graduate | 0.36 (0.24 – 0.53)* | 0.50 (0.35 – 0.73)# | 0.75 (0.52 – 1.08) |
| Less than High School | 0.50 (0.28 – 0.90)∼ | 0.69 (0.39 – 1.22) | 0.89 (0.53 – 1.52) |
| Income Level | |||
| $100,000 or more | Ref | Ref | Ref |
| $75,000 to $99,999 | 0.68 (0.44 – 1.05) | 0.72 (0.49 – 1.04) | 1.11 (0.77 – 1.59) |
| $50,000 to $74,999 | 0.73 (0.48 – 1.11) | 0.63 (0.44 – 0.90)∼ | 1.14 (0.81 – 1.60) |
| $35,000 to $49,999 | 0.63 (0.39 – 1.03) | 0.73 (0.48 – 1.10) | 0.89 (0.59 – 1.33) |
| $20,000 to $34,999 | 0.45 (0.26 – 0.77)∼ | 0.53 (0.32 – 0.88)∼ | 1.01 (0.65 – 1.59) |
| $0 to $19,999 | 0.65 (0.38 – 1.12) | 0.63 (0.37 – 1.08) | 0.94 (0.58 – 1.55) |
| Health Insurance | |||
| Yes | Ref | Ref | Ref |
| No | 1.28 (0.82 – 2.01) | 0.93 (0.62 – 1.40) | 0.92 (0.62 – 1.35) |
| Regular Healthcare Provider | |||
| Yes | Ref | Ref | Ref |
| No | 0.86 (0.62 – 1.19) | 0.90 (0.67 – 1.21) | 1.25 (0.95 – 1.65) |
| General Health | |||
| Excellent/ Very good | Ref | Ref | Ref |
| Good | 1.10 (0.81 – 1.48) | 1.17 (0.88 – 1.55) | 1.12 (0.87 – 1.44) |
| Fair/Poor | 1.26 (0.81 – 1.96) | 1.05 (0.70 – 1.59) | 0.91 (0.63 – 1.32) |
| Number of Children under 18yrs old in Household | |||
| 0 | Ref | Ref | Ref |
| ≥ 1 | 1.11 (0.81 – 1.53) | 1.04 (0.77 – 1.40) | 1.05 (0.80 – 1.38) |
| Use Internet | |||
| Yes | Ref | Ref | Ref |
| No | 0.73 (0.48 – 1.11) | 0.80 (0.54 – 1.18) | 0.79 (0.54 – 1.17) |
p-value:
<0.0001
<0.01 ∼<0.05
OR = Adjusted Odds Ratios; CI = Confidence Interval; HPV = Human papillomavirus; HINTS = Health Information National Trends Survey
Models adjusted for age, gender, race, marital status, education, income level, health insurance, regular healthcare provider, general health, number of children under 18yrs old in household, internet use
Discussion
This study examined racial/ethnic and gender disparities in knowledge and awareness of HPV and the HPV vaccine among US adults using 2013 and 2014 HINTS data. This study found that 66% of American adults had heard of HPV and were aware of the HPV vaccine. When we conducted sensitivity analyses on only respondents between 18 and 55 years old and respondents who had children between 9 and 27 years old, HPV and vaccine awareness levels changed to approximately 70%. According to the 2005 HINTS data and before the approval of the HPV vaccine, Tiro et al found that 40% of women were aware of HPV vaccine.24 Shortly after the HPV vaccine was approved in 2006 and recommended for girls, results from the 2007 National Immunization Survey – Adult showed that 84.3% of women were aware of the vaccine.25 A recent study by Blake et al. (2015) using 2013 HINTS data reported that 68% of the adult population (both men and women) and 77% of women reported ever hearing of both HPV and the HPV vaccine.26 The level of awareness of HPV reported in our study is, to the best of the authors' knowledge, the lowest since vaccine licensure for a nationally representative study. One explanation is that there was a strong media following of the vaccine just before and right after the vaccine was licensed and recommended for use. It could be that the more time elapsed since the HPV vaccine recommendation the less likely individuals became to be actively aware of it. Approximately 99% of all HPV vaccines administered in the United States until 2014 were the quadrivalent HPV vaccine.27 It will be interesting, therefore, to see how the existence and approval of the nonavalent vaccine increases awareness and vaccine uptake after the transition from the quadrivalent to the nonavalent as the mainstay HPV vaccine in the United States.9,28
Although two-thirds of overall study population had heard of HPV and were aware of the HPV vaccine, we found notable gender differences. Women not only had higher knowledge of HPV, they were also 281% more likely to be aware of the HPV vaccine compared with men. This result held true even after the sensitivity analysis. A previous study in 2013 found that women were almost 5 times more likely to be aware of HPV vaccination than men.29 This gap in awareness held true in our study, despite the fact that the HPV vaccine has been available for use in young males since 2009, and has been recommended in eligible males since 2011. This lower awareness of HPV vaccine among men is also reflected in the current rate of HPV vaccine uptake, which is significantly lower among men than women.30
The gender gap in awareness of the HPV vaccine, in addition to decreased vaccine uptake, highlights the importance of increasing HPV awareness among men because men have an increasing burden of the virus and its associated cancers.31 The HPV vaccine provides protection against anogenital cancers that affect men, additionally demonstrating promise in protecting against oral HPV types associated with up to 90–95% of HPV-positive oropharyngeal cancer,32 so it is imperative that men are informed about the HPV vaccine. This is especially important considering the changing landscape in the incidence rates of HPV associated cancers. While fewer new cases of cervical cancers, for which the vaccine was originally developed, are reported each year, the rate of HPV-positive oropharyngeal cancer has grown by 225% in the last 3 decades.4 An increase in incidence of anal cancer has also been reported, although not as high as HPV-associated oropharyngeal cancer.4,33 These increasing cancer rates create greater impetus to target interventions aimed at increasing awareness of HPV and HPV vaccine toward men. There are several factors that could have contributed to men's significantly lower HPV and HPV vaccine awareness. There is a 5-year lag between the time the HPV vaccine was recommended for girls (2006) and for boys (2011). Also, men generally consider HPV-related issues specific to women, especially because the HPV vaccine was initially heavily marketed toward cervical cancer prevention. With the increase in incidence of HPV-associated cancers in men, interventions aimed at increasing HPV vaccine coverage should target both men and women.34
The present study also showed racial/ethnic disparities in knowledge and awareness of HPV and HPV vaccine. Non-Hispanic Blacks had lower HPV awareness compared with non-Hispanic Whites. Non-Hispanic Blacks and Hispanics were also significantly less likely to be aware of the HPV vaccine compared with non-Hispanic Whites, despite the disproportionately higher burden of cervical cancer reported in these groups.5 Similarly, our sensitivity analyses showed that Non-Hispanic Blacks and Hispanics had lower HPV vaccine awareness. These findings are consistent with previous results which reported race differences in awareness about HPV and the HPV vaccine among women.21,22,26 Given that morbidity and mortality associated with cervical cancer is higher in non-Hispanic Black and Hispanic women compared with non-Hispanic Whites,5 our findings suggest that it is pertinent to develop culturally appropriate awareness campaigns, communication strategies, and interventions targeting minority groups to increase HPV-associated knowledge among them.35 Several studies have identified barriers to cancer prevention through HPV vaccination, including negative attitudes toward the vaccine, poor knowledge, poor access to care, general medical distrust, and concerns about long-term safety of the HPV vaccine.36,37 It is important to develop multilevel interventions that recognize the role of physicians, patients, and members of the community.38 Further research on the unique sociocultural barriers to HPV vaccination among Hispanics and non-Hispanic Blacks is needed to better understand the discrepancy between HPV awareness and vaccination uptake.
There are several studies that have found an association between increasing knowledge and HPV vaccine uptake;39,40 however, there are also studies that have shown no association, or an inverse association between increasing knowledge and receiving the HPV vaccine.15,16,41,42 It is therefore important that interventions are designed to facilitate the provision of adequate and reliable information to parents, especially information provided by a healthcare practitioner.43 Healthcare provider recommendation of HPV vaccine has been identified as the most important and influential predictor of vaccine uptake.44,45 However, one of our previous studies shows that electronic and print media, including the internet, is the most common source of HPV knowledge for members of the community rather than the physician's office.46 Healthcare providers should be a source of knowledge/awareness for their patients and physicians could increase HPV vaccine uptake by reducing missed clinical opportunities to educate parents and patients about the risks of HPV and the benefits of the HPV vaccine.47
Implications
Recently, both the American Society of Clinical Oncology (ASCO) and the American Cancer Society released statements on cancer prevention through HPV vaccination, adding voice to the call to increase HPV vaccine awareness and vaccine uptake across the United States.48,49 Since it has been shown that knowledge is an important predictor of HPV vaccine uptake,18,36 it is imperative to have current and reliable estimates of HPV knowledge and awareness so target interventions can be developed. Our study provides current estimates of and disparities in HPV awareness in a nationally representative sample. This will help inform what interventions are needed and more importantly what subgroups to target to help increase vaccine uptake. Otherwise, there is the potential to increase health inequalities if vaccine uptake is lower among already disadvantaged communities50 that are disproportionately affected by higher morbidity and mortality from HPV-associated disease and lower HPV-associated knowledge. In addition, if HPV vaccine coverage were high among women, that may confer herd protection for men, thus mitigating the need to achieve concurrent high vaccine coverage in men.51 However, herd protection has not been achieved in the US.52,53 Therefore, it may be important that more men continue to get vaccinated in view of the substantial male burden of HPV-associated diseases.
Additionally, meeting the Healthy People goal of 80% coverage will require maintaining national programs, regulations, policies, and laws.54,55 Such national programs include the Vaccine for Children (VFC), which aims to cover the cost of the HPV vaccine for eligible individuals.12,56 Additionally, the Affordable Care Act (ACA) mandated insurance coverage for HPV vaccines.56 Yet, recent plans to repeal and replace the ACA57 may negatively affect the aforementioned initiative to promote vaccine coverage. With respect to clinical encounters, policies that encourage more physicians to discuss the HPV vaccine with eligible parents and patients will also help meet the Healthy People 2020 goal.45 There are currently no federal laws requiring the HPV vaccines, but several states have enacted legislations aimed at increasing HPV vaccination, and a few have passed HPV vaccine mandates (Virginia, Rhode Island, and Washington DC).55,56
Strengths and limitations
A major strength of this study is that it is one of the few studies assessing knowledge about HPV and the HPV vaccine in a nationally representative sample that include males. This has become increasingly important due to the many cancers caused by HPV in males, and due to the approval of the HPV vaccine for use among young boys. Limitations of the present study include the following. First, HINTS cycles do not assess current healthcare provider awareness, knowledge, and practices regarding HPV, as well as actual vaccination patterns. These variables could have explained some of the differences seen in our study. Second, the response rate was low, which could lead to biases in the data; however, significant efforts were made to reduce potential for bias through modality coverage and sampling.58 Further, recent evidence suggests that the potential for bias resulting from declining response rates may be less significant than previously assumed.59 Moreover, our findings may be a conservative estimate of the true burden of inadequate HPV-related knowledge as a low response rate actually reflects an under-representation of the problem we assessed.
Conclusion
Although knowledge and awareness about HPV and the HPV vaccine have increased compared with pre-vaccine years, this study reports a decrease, the lowest in a decade since the HPV vaccine was first licensed. This study also reports that there remain disparities among men and non-Hispanic Blacks and Hispanic ethnic groups. Deliberate interventions and health communications specifically targeting men, non-Hispanic Blacks and Hispanics are imperative to increase knowledge and awareness about HPV, the HPV vaccine, and HPV associated cancers to promote greater HPV vaccine uptake.
Materials and methods
Data
Data were obtained from the Health Information National Trends Survey (HINTS) 4, Cycle 3–4 administered by the National Cancer Institute. HINTS is a nationally-representative, publicly available, probability survey of adults aged 18 or older in the civilian non-institutionalized population of the United States. Cycle 3 data (response rate = 35.19%; N = 3,185) were collected from September through December 2013 and Cycle 4 data (response rate = 34.24%; N = 3,677) were collected from August through November 2014. Details of survey development, design, and methodology have been published elsewhere and are available online.60 All questionnaire items in the HINTS are psychometrically sound, having been cognitively tested before being administered. More information about the validation of the HINTS survey can be found here: https://hints.cancer.gov/faq.aspx. All HINTS questionnaires, data, and reports are available at http://hints.cancer.gov/hints4.aspx.
Dependent variables
In HINTS 4, Cycles 3 and 4, 5 HPV awareness and knowledge questions were asked of the entire sample, with embedded skip patterns, described below. The HPV awareness question posed to the entire sample was: “Have you ever heard of HPV? HPV stands for Human Papillomavirus. It is not HIV, HSV, or herpes” (yes/no). The following knowledge questions were asked only of those who answered “yes” to having ever heard of HPV: “Do you think HPV can cause cervical cancer?” (yes/no/not sure); “Do you think that HPV is a sexually transmitted disease (STD)?” (yes/no/not sure); and “Do you think that HPV will often go away on its own without treatment?” (yes/no/not sure). In the logistic regression analysis, responses to the 3 follow-up questions were dichotomized to be “yes” versus “no,” which was made up of “no” and “not sure.” The HPV vaccine awareness question posed to the entire sample without a skip pattern was: “A vaccine to prevent HPV infection is available and is called the cervical cancer vaccine or HPV shot. Before today, have you ever heard of the cervical cancer vaccine or HPV shot?” (yes/no). The same questions and responses were used for HPV and HPV vaccine knowledge and awareness across both data set sets. There was no statistically significant difference between the number of participants who had heard of HPV in the HINTS 4 Cycle 3 (66.4%) and HINTS 4 Cycle 4 (63.6%) data sets (p = 0.6781). Similarly, there was no statistically significant difference between the number of participants who were aware of the HPV vaccine in the HINTS 4 Cycle 3 (66.4) and HINTS 4 Cycle 4 (62.7) data sets (p = 0.5844).
Independent variables
Gender and race/ethnicity were the primary independent variables of interest. Gender was assessed with the question: “Are you male or female?” Race/Ethnicity was operationalized for this study as Hispanic, non-Hispanic Black, non-Hispanic White, and “Other race,” which combines low-frequency responses for American Indian/Alaska Native, Asian Indian, Chinese, Filipino, Japanese, Korean, Vietnamese, other Asian, Native Hawaiian, Guamanian or Chamorro, Samoan, and other Pacific Islander.
Covariates
Covariates assessed were selected based on previous literature,26 including age, marital status, income, education, health insurance, whether the respondent had a usual healthcare provider, self-reported general health condition, number of children in household, and Internet use. Covariates were categorized as follows: age (18 – 34, 35 – 49, 50 – 64, and 65 years or older); marital status (married/living as married, widowed/divorced/separated, and never married); education (less than high school, high school graduate, some college, and college graduate or higher); income (< $20,000, $20,000 – $34,999; $35,000 – $49,999; $50,000 – $74,999; $75,000 – $99,999; and ≥ $100,000); health insurance (yes/no); had a regular healthcare provider (yes/no); general health condition (excellent/very good, good, and fair/poor); number of children in household <18 years old (zero, one or more); and Internet use (“Do you ever go online to access the Internet or World Wide Web, or to send and receive e-mail?” [yes/no]).
Statistical analysis
Our study was a secondary analysis of the HINTS data. Analyses were performed using SAS (Version 9.4) procedures which incorporate survey sampling weights to account for the complex sampling design used in HINTS and to provide representative estimates of the US population (SAS Institute Inc., Cary, NC). Weighted, unadjusted prevalence estimates (n, %) were used to assess overall awareness and knowledge of HPV. Weighted, multivariable logistic regression models using listwise deletion were used to evaluate if there were gender and racial disparities in HPV awareness and knowledge, controlling for covariates (age, gender, race, marital status, education, income level, health insurance, regular healthcare provider, general health, number of children under 18 years old in household, internet use) selected based on previous literature.26 To evaluate if inclusion of older respondents biased the estimation of knowledge and awareness of HPV and the vaccine, we conducted 2 sensitivity analyses. In the first sensitivity analysis, we limited data to respondents between 18 and 55 years old. We selected an upper age limit of 55 because the average age of mothers giving birth to their first child in the US is 26.3 years61 and men are on the average 3 years older than women at the time of their first child62 and so when the upper age limit of the vaccine (26 years) is added to those numbers they add up to 55 years old. In the second sensitivity analysis, we limited data to respondents who had children aged between 9 and 27 years old. Respondents with children who are age-eligible for the HPV vaccine should be aware of it. All analyses were 2 tailed and statistical significance was determined using p < 0.05.
Disclosure of potential conflicts of interest
There are no conflicts of interest for all authors.
Acknowledgments
Part of this work was presented at the at the Eighth Annual AACR Conference on the Science of Cancer Health Disparities in Racial/Ethnic Minorities and the Medically Under-served, November 2015, Atlanta, GA; and the 37th Annual Meeting & Scientific Sessions of the Society of Behavioral Medicine, March 2016, Washington DC.
Authors' contributions
Conception and design: E. Adjei Boakye, N. Osazuwa-Peters
Development of methodology: E. Adjei Boakye, B.B. Tobo, N. Osazuwa-Peters
Acquisition of data: E. Adjei Boakye, B.B. Tobo
Analysis and interpretation of data (e.g., statistical analysis, biostatistics, computational analysis): E. Adjei Boakye, B.B. Tobo, R.P. Rojek
Writing, review, and/or revision of the manuscript: E. Adjei Boakye, B.B. Tobo, R.P. Rojek, K. A. Mohammed, C. J. Geneus, N. Osazuwa-Peters
Study supervision: E. Adjei Boakye, N. Osazuwa-Peters
Other (final approval of the version to be published): All authors
References
- [1].Dunne EF, Markowitz LE, Saraiya M, Stokley S, Middleman A, Unger ER, Williams A, Iskander J. CDC grand rounds: reducing the burden of HPV-associated cancer and disease. MMWR Morbidity Mortality Weekly Report. 2014;63(4):69-72. PMID:24476977 [PMC free article] [PubMed] [Google Scholar]
- [2].Burd EM. Human papillomavirus and cervical cancer. Clin Microbiol Rev. 2003;16(1):1-17. doi: 10.1128/CMR.16.1.1-17.2003. PMID:12525422 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Jemal A, Simard EP, Dorell C, Noone AM, Markowitz LE, Kohler B, Eheman C, Saraiya M, Bandi P, Saslow D, et al.. Annual Report to the Nation on the Status of Cancer, 1975–2009, featuring the burden and trends in human papillomavirus (HPV)–associated cancers and HPV vaccination coverage levels. J Natl Cancer Inst. 2013;105(3):175-201. doi: 10.1093/jnci/djs491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, et al.. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011;29(32):4294-4301. doi: 10.1200/JCO.2011.36.4596. PMID:21969503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].American Cancer Society Cancer Statistics Center: Cancer Type – Cervix. 2017; https://cancerstatisticscenter.cancer.org/#/cancer-site/Cervix. (accessed 13 June 2017)
- [6].Howlader N, Noone AM, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Statistics Review, 1975-2014. 2017. Bethesda, MD: National Cancer Institute. https://seer.cancer.gov/csr/1975_2014/ [Google Scholar]
- [7].Markowitz LE, Dunne EF, Saraiya M, Chesson HW, Curtis CR, Gee J, Bocchini JA Jr, Unger E. Human papillomavirus vaccination: recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2014;63:1-30. PMID:25167164 [PubMed] [Google Scholar]
- [8].Petrosky E, Bocchini JA Jr, Hariri S, Chesson H, Curtis CR, Saraiya M, Unger ER, Markowitz LE. Use of 9-valent human papillomavirus (HPV) vaccine: updated HPV vaccination recommendations of the Advisory Committee on Immunization Practices. MMWR. 2015;64:300-304. PMID:25811679 [PMC free article] [PubMed] [Google Scholar]
- [9].Angelo LB. Immunization update 2017. Pharmacy Today. 2017;23(5):56-64. doi: 10.1016/j.ptdy.2017.04.029. [DOI] [Google Scholar]
- [10].Palefsky JM. Human papillomavirus-related disease in men: not just a women's issue. J Adolesc Health. 2010;46(4 Suppl):S12-19. doi: 10.1016/j.jadohealth.2010.01.010. PMID:20307839 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Centers for Disease Control and Prevention Recommendations on the use of quadrivalent human papillomavirus vaccine in males–Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morbidity Mortality Weekly Report. 2011;60(50):1705-1708. PMID:22189893 [PubMed] [Google Scholar]
- [12].Reagan-Steiner S National, regional, state, and selected local area vaccination coverage among adolescents aged 13–17 years—United States, 2015. MMWR Morbidity Mortality Weekly Report. 2016;65:850-8. doi: 10.15585/mmwr.mm6533a4. PMID:27561081 [DOI] [PubMed] [Google Scholar]
- [13].Rambout L, Tashkandi M, Hopkins L, Tricco AC. Self-reported barriers and facilitators to preventive human papillomavirus vaccination among adolescent girls and young women: A systematic review. Prev Med. 2014;58(0):22-32. doi: 10.1016/j.ypmed.2013.10.009. PMID:24176938 [DOI] [PubMed] [Google Scholar]
- [14].Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, Smith J. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197-204. doi: 10.1097/OLQ.0b013e3181f12dbf. PMID:20838362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Jacobson RM, Agunwamba AA, St Sauver JL, Finney Rutten LJ. The most effective and promising population health strategies to advance human papillomavirus vaccination. Expert Rev Vaccines. 2016;15(2):257-269. doi: 10.1586/14760584.2016.1116947. PMID:26559567 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Walling EB, Benzoni N, Dornfeld J, Bhandari R, Sisk BA, Garbutt J, Colditz G. Interventions to Improve HPV Vaccine Uptake: A Systematic Review. Pediatrics. 2016;138(1):e20153863. doi: 10.1542/peds.2015-3863. PMID:27296865 [DOI] [PubMed] [Google Scholar]
- [17].Read DS, Joseph MA, Polishchuk V, Suss AL. Attitudes and perceptions of the HPV vaccine in Caribbean and African-American adolescent girls and their parents. J Pediatric Adolescent Gynecol. 2010;23(4):242-245. doi: 10.1016/j.jpag.2010.02.002. [DOI] [PubMed] [Google Scholar]
- [18].Cummings T, Kasting ML, Rosenberger JG, Rosenthal SL, Zimet GD, Stupiansky NW. Catching Up or Missing Out? Human Papillomavirus Vaccine Acceptability Among 18-to 26-Year-old men who have sex with men in a US National Sample. Sex Transm Dis. 2015;42(11):601-6doi: 10.1097/OLQ.0000000000000358. PMID:26462183 [DOI] [PubMed] [Google Scholar]
- [19].Lai JY, Tinker AV, Cheung WY. Factors influencing the willingness of US women to vaccinate their daughters against the human papillomavirus to prevent cervical cancer. Medical Oncol. 2013;30(2):582. doi: 10.1007/s12032-013-0582-z. [DOI] [PubMed] [Google Scholar]
- [20].Licht AS, Murphy JM, Hyland AJ, Fix BV, Hawk LW, Mahoney MC. Is use of the human papillomavirus vaccine among female college students related to human papillomavirus knowledge and risk perception? Sexually Transmitted Infect. 2010;86(1):74-78. doi: 10.1136/sti.2009.037705. [DOI] [PubMed] [Google Scholar]
- [21].Kontos EZ, Emmons KM, Puleo E, Viswanath K. Contribution of communication inequalities to disparities in human papillomavirus vaccine awareness and knowledge. Am J Public Health. 2012;102(10):1911-1920. doi: 10.2105/AJPH.2011.300435. PMID:22970692 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kobetz E, Dunn Mendoza A, Menard J, Finney Rutten L, Diem J, Barton B, Kornfeld J, McKenzie N. One size does not fit all: differences in HPV knowledge between Haitian and African American women. Cancer Epidemiol Biomarkers Prev. 2010;19(2):366-370. doi: 10.1158/1055-9965.EPI-09-1180. PMID:20142238 [DOI] [PubMed] [Google Scholar]
- [23].Patel PR, Berenson AB. Sources of HPV vaccine hesitancy in parents. Hum Vaccin Immunother. 2013;9(12):2649-2653. doi: 10.4161/hv.26224. PMID:23982270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Tiro JA, Meissner HI, Kobrin S, Chollette V. What do women in the U.S. know about human papillomavirus and cervical cancer? Cancer Epidemiol Biomarkers Prev. 2007;16(2):288-294. doi: 10.1158/1055-9965.EPI-06-0756. PMID:17267388 [DOI] [PubMed] [Google Scholar]
- [25].Jain N, Euler GL, Shefer A, Lu P, Yankey D, Markowitz L. Human papillomavirus (HPV) awareness and vaccination initiation among women in the United States, National Immunization Survey—Adult 2007. Preventive Med. 2009;48(5):426-431. doi: 10.1016/j.ypmed.2008.11.010. [DOI] [PubMed] [Google Scholar]
- [26].Blake KD, Ottenbacher AJ, Finney Rutten LJ, Grady MA, Kobrin SC, Jacobson RM, Hesse B. Predictors of human papillomavirus awareness and knowledge in 2013: gaps and opportunities for targeted communication strategies. Am J Preventive Medi. 2015;48(4):402-410. doi: 10.1016/j.amepre.2014.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Advisory Committee on Immunization Practices (ACIP) Summary Report. June 24–25, 2015. http://www.cdc.gov/vaccines/acip/meetings/downloads/min-archive/min-2015-06.pdf
- [28].Chesson HW, Laprise J-F, Brisson M, Markowitz LE. Impact and cost-effectiveness of 3 doses of 9-valent human papillomavirus (HPV) vaccine among US females previously vaccinated with 4-valent HPV vaccine. J Infect Dis. 2016;213(11):1694-1700. doi: 10.1093/infdis/jiw046. PMID:26908738 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Marlow LA, Zimet GD, McCaffery KJ, Ostini R, Waller J. Knowledge of human papillomavirus (HPV) and HPV vaccination: an international comparison. Vaccine. 2013;31(5):763-769. doi: 10.1016/j.vaccine.2012.11.083. PMID:23246310 [DOI] [PubMed] [Google Scholar]
- [30].Stokley S, Jeyarajah J, Yankey D, Cano M, Gee J, Roark J, Curtis RC, Markowitz L. Human papillomavirus vaccination coverage among adolescents, 2007–2013, and postlicensure vaccine safety monitoring, 2006-2014–United States. MMWR Morbidity Mortal Wkly Rep. 2014;63(29):620-624 [PMC free article] [PubMed] [Google Scholar]
- [31].Palefsky JM. Human papillomavirus-related disease in men: not just a women's issue. J Adolescent Health. 2010;46(4):S12-S19. doi: 10.1016/j.jadohealth.2010.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Gillison ML, Chaturvedi AK, Lowy DR. HPV prophylactic vaccines and the potential prevention of noncervical cancers in both men and women. Cancer. 2008;113(S10):3036-3046. doi: 10.1002/cncr.23764. PMID:18980286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Nelson RA, Levine AM, Bernstein L, Smith DD, Lai LL. Changing patterns of anal canal carcinoma in the United States. J Clin Oncol. 2013;31(12):1569-75. doi: 10.1200/JCO.2012.45.2524. PMID:23509304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Osazuwa-Peters N, Adjei Boakye E, Mohammed KA, Tobo BB, Geneus CJ, Schootman M. Not just a woman's business! Understanding men and women's knowledge of HPV, the HPV vaccine, and HPV-associated cancers. Prev Med. 2017;99:299-304. doi: 10.1016/j.ypmed.2017.03.014. PMID:28341458 [DOI] [PubMed] [Google Scholar]
- [35].Vanderpool RC, Dressler EV, Stradtman LR, Crosby RA. Fatalistic beliefs and completion of the HPV vaccination series among a sample of young Appalachian Kentucky women. J Rural Health. Spring 2015;31(2):199-205. doi: 10.1111/jrh.12102. PMID:25640763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [36].Reiter PL, Katz ML, Paskett ED. Correlates of HPV vaccination among adolescent females from Appalachia and reasons why their parents do not intend to vaccinate. Vaccine. 2013;31(31):3121-3125. doi: 10.1016/j.vaccine.2013.04.068. PMID:23664990 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Holman DM, Benard V, Roland KB, Watson M, Liddon N, Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168(1):76-82. doi: 10.1001/jamapediatrics.2013.2752. PMID:24276343 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Paskett ED, Krok-Schoen JL, Pennell ML, Tatum CM, Reiter PL, Peng J, Bernardo BM, Weier RC, Richardson MS, Katz ML. Results of a Multilevel Intervention Trial to Increase Human Papillomavirus (HPV) Vaccine Uptake among Adolescent Girls. Cancer Epidemiol Biomarkers Prev. 2016;25(4):593-602. doi: 10.1158/1055-9965.EPI-15-1243. PMID:27196093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [39].Brewer NT, Gottlieb SL, Reiter PL, McRee AL, Liddon N, Markowitz L, Smith J. Longitudinal predictors of human papillomavirus vaccine initiation among adolescent girls in a high-risk geographic area. Sex Transm Dis. 2011;38(3):197-204. doi: 10.1097/OLQ.0b013e3181f12dbf. PMID:20838362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Grandahl M, Oscarsson M, Stenhammar C, Neveus T, Westerling R, Tyden T. Not the right time: why parents refuse to let their daughters have the human papillomavirus vaccination. Acta paediatrica (Oslo, Norway: 1992). 2014;103(4):436-441. doi: 10.1111/apa.12545. PMID:24460679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Krawczyk A, Knauper B, Gilca V, Dubé E, Perez S, Joyal-Desmarais K, Rosberger Z. Parents' decision-making about the human papillomavirus vaccine for their daughters: I. Quantitative results. Hum Vaccin Immunother. 2015;11(2):322-329. doi: 10.1080/21645515.2014.1004030. PMID:25692455 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Gerend MA, Weibley E, Bland H. Parental response to human papillomavirus vaccine availability: uptake and intentions. J Adolesc Health. 2009;45(5):528-531. doi: 10.1016/j.jadohealth.2009.02.006. PMID:19837361 [DOI] [PubMed] [Google Scholar]
- [43].Perez S, Tatar O, Shapiro GK, Dubé E, Ogilvie G, Guichon J, Gilca V, Rosberger Z. Psychosocial determinants of parental human papillomavirus (HPV) vaccine decision-making for sons: Methodological challenges and initial results of a pan-Canadian longitudinal study. BMC Public Health. 2016;16(1):1223. doi: 10.1186/s12889-016-3828-9. PMID:27919239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].Ylitalo KR, Lee H, Mehta NK. Health care provider recommendation, human papillomavirus vaccination, and race/ethnicity in the US National Immunization Survey. Am J Public Health. 2013;103(1):164-169. doi: 10.2105/AJPH.2011.300600. PMID:22698055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Mohammed KA, Geneus CJ, Osazuwa-Peters N, Adjei Boakye E, Tobo BB, Burroughs TE. Disparities in provider recommendation of human papillomavirus vaccination for US adolescents. J Adolescent Health. 2016;59(5):592-598. doi: 10.1016/j.jadohealth.2016.06.005 [DOI] [PubMed] [Google Scholar]
- [46].Osazuwa-Peters N, Wang DD, Namin A, John VM, O'Neill M, Patel PV, Varvares M. Sexual behavior, HPV knowledge, and association with head and neck cancer among a high-risk group. Oral Oncol. 2015;51(5):452-456. doi: 10.1016/j.oraloncology.2015.01.011. PMID:25683135 [DOI] [PubMed] [Google Scholar]
- [47].Vadaparampil ST, Kahn JA, Salmon D, Lee JH, Quinn GP, Roetzheim R, Bruder K, Malo TL, Proveaux T, Zhao X, et al.. Missed clinical opportunities: provider recommendations for HPV vaccination for 11–12 year old girls are limited. Vaccine. 2011;29(47):8634-8641. doi: 10.1016/j.vaccine.2011.09.006. PMID:21924315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Bailey HH, Chuang LT, duPont NC, Eng C, Foxhall LE, Merrill JK, Wollins DS, Blanke CD. American Society of Clinical Oncology Statement: Human Papillomavirus Vaccination for Cancer Prevention. J Clin Oncol. 2016;34(15):1803-1812. doi: 10.1200/JCO.2016.67.2014. PMID:27069078 [DOI] [PubMed] [Google Scholar]
- [49].Saslow D, Andrews KS, Manassaram‐Baptiste D, Loomer L, Lam KE, Fisher-Borne M, Smith RA, Fontham ET. Human papillomavirus vaccination guideline update: American Cancer Society Guideline endorsement. CA. 2016;66(5):375-8. PMID:27434803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Fisher H, Trotter CL, Audrey S, MacDonald-Wallis K, Hickman M. Inequalities in the uptake of human papillomavirus vaccination: a systematic review and meta-analysis. Int J Epidemiol. 2013;42(3):896-908. doi: 10.1093/ije/dyt049. PMID:23620381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Brisson M, van de Velde N, Franco EL, Drolet M, Boily MC. Incremental impact of adding boys to current human papillomavirus vaccination programs: role of herd immunity. J Infect Dis. 2011;204(3):372-376. doi: 10.1093/infdis/jir285. PMID:21742835 [DOI] [PubMed] [Google Scholar]
- [52].Markowitz LE, Liu G, Hariri S, Steinau M, Dunne EF, Unger ER. Prevalence of HPV after introduction of the vaccination program in the United States. Pediatrics. 2016;137(3):e20151968. doi: 10.1542/peds.2015-1968. PMID:26908697 [DOI] [PubMed] [Google Scholar]
- [53].Tarney C, Pagan M, Klaric J, Beltran T, Han J. HPV Vaccination Does Not Provide Herd Immunity for Unvaccinated Women or Cross-Protection for Nonvaccine HPV Types [12].Obstetrics and gynecology. 2016;127 Suppl 1:4s [Google Scholar]
- [54].U.S. Department of Health and Human Services Healthy People 2020 topics & objectives: immunization and infectious diseases. 2013; https://www.healthypeople.gov/2020/topics-objectives/topic/immunization-and-infectious-diseases/objectives
- [55].Osazuwa-Peters N. Human papillomavirus (HPV), HPV-associated oropharyngeal cancer, and HPV vaccine in the United States–do we need a broader vaccine policy? Vaccine. 2013;31(47):5500-5505. doi: 10.1016/j.vaccine.2013.09.031. PMID:24095883 [DOI] [PubMed] [Google Scholar]
- [56].Keim-Malpass J, Mitchell EM, DeGuzman PB, Stoler MH, Kennedy C. Legislative activity related to the human papillomavirus (HPV) vaccine in the United States (2006-2015): a need for evidence-based policy. Risk Management Healthcare Policy. 2017;10:29-32. doi: 10.2147/RMHP.S128247. PMID:28331378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- [57].Hirsch JA, Rosenkrantz AB, Nicola GN, Harvey HB, Duszak R Jr, Silva E 3rd, Barr RM, Klucznik RP, Brook AL, Manchikanti L. Contextualizing the first-round failure of the AHCA: down but not out. J Neurointerventional Surg. 2017;9(6):595-600. doi: 10.1136/neurintsurg-2017-013136. [DOI] [PubMed] [Google Scholar]
- [58].Cantor D. CK, Crystal-Mansour S, Davis T, Dipko S, Sigman R. Health Information National Trends Survey (HINTS) 2007: Final report. Rockville, MD: Westat; 2009. [Google Scholar]
- [59].Fahimi M, Link M, Mokdad A, Schwartz DA, Levy P. Tracking chronic disease and risk behavior prevalence as survey participation declines: statistics from the behavioral risk factor surveillance system and other national surveys. Preventing Chronic Dis. 2008;5(3):A80. [PMC free article] [PubMed] [Google Scholar]
- [60].National Cancer Institute Health Information National Trends Survey. 2014; http://hints.cancer.gov/hints4.aspx. Accessed October10, 2015
- [61].Mathews TJ, Hamilton BE. Mean age of mothers is on the rise: United States, 2000–2014. NCHS Data Brief. 2016;232:1-8 [PubMed] [Google Scholar]
- [62].NCFMR Family Profiles Fatherhood in the U.S.: Men's Age at First Birth, 1987–2010 https://www.bgsu.edu/content/dam/BGSU/college-of-arts-and-sciences/NCFMR/documents/FP/FP-11-04.pdf. Accessed 10/8/2016


