Abstract
Introduction
The ongoing rise in the numbers of chronically ill people necessitates efforts for effective self-management. Goal setting and action planning are frequently used, as they are thought to support patients in changing their behavior. However, it remains unclear how goal setting and action planning in the context of self-management are defined in the scientific literature. This study aimed to achieve a better understanding of the various definitions used.
Methods
A scoping review was conducted, searching PubMed, Cinahl, PsychINFO and Cochrane. Inclusion and exclusion criteria were formulated to ensure the focus on goal setting/action planning and self-management. The literature was updated to December 2015; data selection and charting was done by two reviewers. A qualitative content analysis approach was used.
Results
Out of 9115 retrieved articles, 58 met the inclusion criteria. We created an overview of goal setting phases that were applied (preparation, formulation of goals, formulation of action plan, coping planning and follow-up). Although the phases we found are in accordance with commonly known frameworks for goal setting, it was striking that the majority of studies (n = 39, 67%) did not include all phases. We also prepared an overview of components and strategies for each goal setting phase. Interestingly, few strategies were found for the communication between patients and professionals about goals/action plans. Most studies (n = 35, 60%) focused goal setting on one single disease and on a predefined lifestyle behavior; nearly half of the articles (n = 27, 47%) reported a theoretical framework.
Discussion
The results might provide practical support for developers of interventions. Moreover, our results might encourage professionals to become more aware of the phases of the goal setting process and of strategies emphasizing on patient reflection. However, more research might be useful to examine strategies to facilitate communication about goals/action plans. It might also be worthwhile to develop and evaluate goal setting/action planning strategies for people with different and multiple chronic conditions.
Introduction
The increasing numbers of people living with one or more chronic conditions worldwide necessitate efforts to achieve effective self-management [1]. Based on the Expanded Chronic Care Model, self-management is defined as the degree to which a patient with a chronic condition is able to, and wants to, control his own daily life, by coping effectively with symptoms, treatments and lifestyle adjustments [2, 3]. Self-management support is defined as the support provided by healthcare professionals to enable patients to become good managers of their chronic conditions, tailored to their needs and capabilities [2, 4]. The aim of successful self-management is to enhance patient autonomy, to improve health status and consequently reduce the use of health services, leading to a decrease of the financial pressure on the healthcare sector [5, 6].
Self-management includes more than just coping with medical symptoms of a chronic illness and compliance with medical treatment. In addition to medical self-management, Corbin & Strauss (1988) describe two other forms: social and emotional self-management [7]. Social management refers to the ability of a patient to adjust his or her behavior so as to prevent negative outcomes and maintain or adjust life roles. Emotional self-management refers to dealing with emotional responses to a chronic condition, such as fear and depression, and coping with discomfort and disability [7].
Self-management support begins with the exploration of patients’ beliefs and values [8]. Depending on what is important to the patient, goals for the patient’s self-management can be set and actions can be planned [8]. Within the primary care sector, the term ‘collaborative goal setting’, defined as a process in which healthcare professionals and patients agree on health-related goals, is frequently used [9]. Action planning is defined as agreeing on a course of action for the patient (and/or the professional), including questions like what, when, where and how often [9, 10]. Goal setting and action planning are frequently applied in self-management support programs, as they are found to improve patients’ self-efficacy, help them change their behavior and improve their health outcomes [5, 10–12]. Moreover, there is increasing attention on coping planning, in close association with goal-setting and action planning [9, 13]. Coping planning is defined as the formulation of plans to overcome potential barriers to carrying out an action plan [13, 14]. Nowadays, European treatment guidelines for chronic conditions, like diabetes or COPD, recommend goal setting and action planning as methods for self-management support [15, 16]. However, professionals frequently encounter difficulties in the day-to-day practice of goal setting and action planning practice [17]. The process is perceived as time-consuming and the effort involved and the complexity are often underestimated [18, 19].
Literature about goal setting has mostly focused on the experiences and skills of professionals and patients [20–23]. In addition, two reviews of the evidence on goal setting and action planning have become available, focusing on the rehabilitation context and assessing the effects of goal setting and action planning on patients’ health outcomes [21, 24]. However, information about goal setting and action planning in the context of self-management is often lacking. A more thorough understanding of goal setting and action planning might provide practical support to those developing self-management programs. We therefore conducted a scoping review and formulated the following research question: How is goal setting and action planning within the context of self-management defined in the scientific literature?
Methods
Scoping review
For this scoping review, we adopted the methodological framework developed by Arksey & O’Malley (2005) [25]. We chose this approach as it allows for the inclusion of many different study designs which fits our aim to give a broad overview of the way researchers define goal setting and action planning [25]. In contrast to systematic reviews, the quality of evidence is not evaluated in a scoping review. Instead, it addresses broader topics and research questions [25]. Arksey & O’Malley suggest that there are five stages to a scoping review: (1) identifying the research question; (2) identifying relevant studies; (3) selecting studies; (4) charting the data; and (5) collating, summarizing and reporting the results [25].
Identifying relevant studies
The search strategy consisted of the following formula: goal setting/action planning AND method AND self-management. Search terms for ‘goal setting’ included the MeSH terms ‘Goals’ and ‘Patient Care Planning’, combined with free-text terms such as ‘goal setting’ and ‘goal planning’. Search terms for ‘method’ included the MeSH terms ‘Professional Practice’, ‘Technology’ and ‘Instrumentation’, combined with free text terms like ‘method*’ and ‘intervention*’. Finally, search terms for ‘self-management’ included the MeSH terms ‘Self Care’, ‘Disease Management’, ‘Patient Education’, ‘Patient Participation’, ‘Self-Help Groups’, ‘Personal Autonomy’, ‘Patient-Centered Care’ and ‘Patient Preference’ combined with free-text terms like ‘self-management support’ and ‘self-control’ (see Table 1 Search Strategy.).
Table 1. Search strategy.
| Goal setting/Action planning | Method | Self-management | |
|---|---|---|---|
| MeSH terms |
|
|
|
| Free-text terms |
|
|
|
The PubMed, Cinahl, PsychINFO and Cochrane databases were searched during September 2013 with no restriction on the date of publication. In addition, reference lists of relevant articles were screened to identify key articles that had been missed. The literature was subsequently updated to December 2015.
Selecting studies
The search was limited to adults (aged 19 years or older), English, Dutch, French and German articles and research involving humans. Study selection took place in three stages: first, titles were reviewed, followed by a review of abstracts and then full texts. Articles without an available abstract were directly included in the full-text review stage. Two researchers reviewed the articles. At each stage, a selection of 200 articles was reviewed by both reviewers to reach consensus about applying the inclusion and exclusion criteria. After that, each reviewer reviewed the articles independently.
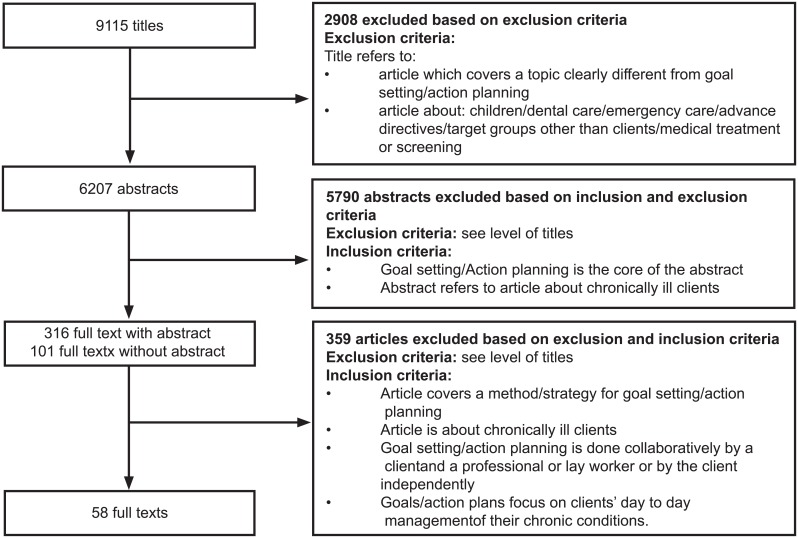
We formulated inclusion and exclusion criteria. Articles were included when: (a) the article focused on chronically ill patients, and (b) the terms ‘goal setting’ and/or ‘action planning’ or relevant synonyms were included, along with a definition of goal setting and/or action planning. To ensure that the articles defined goal setting and/or action planning within the context of self-management in the articles, additional inclusion criteria were formulated, building upon the self-management framework by Lorig & Holman (2003) [5]. The following criteria had to be met: (a) goal setting/action planning is done collaboratively by a patient and a professional or lay worker or independently by the patient, and (b) goals/action plans focus on patients’ day-to-day management of their chronic conditions. Articles were excluded when they focused on: (a) children/adolescents; (b) dental care; (c) emergency care, and/or (d) topics differing greatly from goal setting/action planning (e.g. learning goals of students, surgical interventions, coping with advanced directives) (Fig 1 Study selection.).
Fig 1. Study selection.
At each stage, we divided the articles into relevant (R), irrelevant (I) and doubtful (D). In order to validate the selection procedure, the inclusion and exclusion criteria were checked for consistency by the two reviewers.
Charting the data
A data-charting form was jointly developed by two reviewers to determine which variables to extract. The two reviewers independently charted the data, discussed the results and continuously updated the data-charting form in an iterative process.
This data-charting form contained descriptive variables (year of publication, study design, setting, target group) and information about the goal setting/action planning. We extracted information about the way authors defined goal setting and/or action planning and information about the way they intended to apply goal setting and/or action planning. For studies aiming to evaluate the effectiveness or feasibility of goal setting and/or action planning interventions, we also reviewed data on fidelity (i.e. the degree to which an intervention is delivered as intended).
Collating, summarizing and reporting the results
Focusing on disentangling goal setting and action planning, we applied a qualitative content analysis approach [26]. The analysis resulted in (1) an overview of goal setting phases (defined as steps of the goal setting/action planning process); (2) an overview of components (defined as activities performed in each of the goal setting phases) and (3) an overview of strategies (defined as techniques to put components into practice). The analysis also resulted in a description of the targets of goal setting/action planning, the theoretical underpinning and the mode of delivery of goal setting and/or action planning.
Results
Study characteristics
The search resulted in 9115 hits. After screening the titles, abstracts and full texts and correcting for duplicates, 58 articles met the inclusion criteria (see Fig 1 Study Selection.). Of the included articles, 46 (79%) were published in or after 2006, and most originated from the USA (n = 28, 48%) or Europe (n = 21, 36%). Most of the articles were RCTs (n = 25, 43%), pre-posttest trials (n = 13, 22%) or non-randomized controlled trials (n = 3, 5%). None of those intervention trials reported to have examined intervention fidelity. Six articles (10%) presented qualitative studies (e.g. use of a goal setting instrument to elicit patients’ goals, in order to study the content of these goals) and five articles (9%) described the development of an intervention (intervention development study) using mixed methods. The selection also included three case studies (5%), two study protocols (3%) and one literature study (2%). Fifty-four studies (93%) applied goal setting/action planning to patients suffering from one specific disease, mostly to those suffering from diabetes (n = 16, 28%) or neurological diseases (n = 10, 17%). Articles encompassed a wide range of settings (mostly primary care (n = 24, 41%), the community (n = 12, 21%) and the outpatient departments (n = 8, 14%)) (See Table 2 Summary of Study Characteristics.) (See Table 3 Study Characteristics.)
Table 2. Summary of study characteristics.
| Characteristic | Categories for each characteristic | Number of studies (n = 58) |
|---|---|---|
| Date of publication | Before 1990 (1978) | 1 |
| 1991–1995 | 0 | |
| 1996–2000 | 2 | |
| 2001–2005 | 9 | |
| 2006–2010 | 19 | |
| 2011–2015 | 27 | |
| Place of publication | USA | 28 |
| Europe | 21 | |
| Canada | 3 | |
| Australia | 2 | |
| Other | 4 | |
| Study design | RCT | 25 |
| Pre-posttest design | 13 | |
| Non-randomized controlled trial | 3 | |
| Qualitative design | 6 | |
| Intervention development study (using mixed methods) | 5 | |
| Case study | 3 | |
| Study protocol | 2 | |
| Literature study | 1 | |
| Target group | Diabetes | 16 |
| Neurological diseases | 10 | |
| Cardiovascular diseases | 7 | |
| Any chronic condition | 4 | |
| Mental illness | 4 | |
| Pain | 3 | |
| Rheumatoid arthritis | 2 | |
| Geriatric patients | 2 | |
| Asthma | 2 | |
| Cancer | 2 | |
| Other | 6 | |
| Setting | Primary care | 24 |
| Community | 12 | |
| Outpatient department | 9 | |
| Rehabilitation | 5 | |
| Hospital | 3 | |
| Residential care setting | 3 | |
| Pharmaceutical setting | 1 | |
| Other settings | 1 |
Table 3. Study characteristics.
| Author (year) | Study design | Research question | Patients | Professionals | Setting | Country |
|---|---|---|---|---|---|---|
| Arbour-Nicitopoulus et al. (2003) | RCT | To examine the effects of action and coping planning on physical activity and self-efficacy. | Spinal cord injury | Researcher | Community | Canada |
| Bacelar de Araujo Lourenco et al. (2013) | RCT | To assess the effect of action and coping planning on the adherence to drug treatment. | Coronary artery disease | researcher | Outpatient clinic | Brazil |
| Bearon et al. (2000) | Intervention Development Study | To describe the development and testing of the Personal Functional Goals (PFG) Checklist/Interview. | Geriatric patients | researcher | Primary care | USA |
| Becker et al. (2009) | RCT | To examine goal achievement over an 8-month period in women with fibromyalgia. | Fibromyalgia | nurse practitioner | Community | USA |
| Briggs-Early et al. (2009) | Qualitative design | To examine Latinos’ dietary behaviors used to achieve self-management goals. | Diabetes | nurse/ dietitian | Primary care | USA |
| Buechi et al. (2010) | Case study | To describe the implementation of Pictorial Representation of Illness and Self-measure (PRISM). | Psychiatric patients | psychotherapist | Psychiatric hospital | Switzer-land |
| Calfas et al. (2002) | RCT | To evaluate Patient-centered Assessment and Counseling for Exercise plus nutrition (PACE +). | Overweight | family physician/ nurse practitioner | Primary care | USA |
| Cho (2013) | RCT | To examine the effect of Health Contract Intervention on self-care behavior and physiological indices. | Renal dialysis patients | researcher | Outpatient hospital | Korea |
| Christiansen et al. (2010) | RCT | To evaluate a concise method for encouraging exercising in and consolidating behavioral changes. | Chronic back pain | psychologist | Outpatient rehabilitation | Germany |
| Chunchu et al. (2012) | Non-randomized controlled trial | To evaluate a team approach using a HER-based patient centered care plan (PCCP). | Any chronic condition | physician/ medical assistant | Primary care | USA |
| Corser et al. (2007) | Pre- posttest | To test the feasibility of a brief shared decision making goal setting intervention. | Diabetes | Nurse | Primary care | USA |
| Coote & MacLeod (2012) | RCT | To evaluate Goal setting and Planning Skills (GAP) in its individual, self-help format. | Depression | No professional | Community | UK |
| Custer et al. (2013) | Pre-posttest | To test a self-reported strategy that would assist in choosing goals and rating goal achievement. | Any chronic condition | Occupational therapists | Outpatient rehabilitation | USA |
| Davis & White (2008) | Pre-posttest | To test a pain self-management intervention, the Goal Attainment Pain Management Program (GAPAP). | Rheumatoid arthritis | Nurse | Residential care | USA |
| DeWalt et al. (2009) | Pre-posttest | To evaluate the Living with Diabetes Guide and a brief counseling intervention to set and achieve goals. | Diabetes | Research assistant | Primary care | USA |
| Dickman et al. (2012) | Pre-posttest | To evaluate changes in self-managing behavior following Shared Medical Appointments (SMAs). | Diabetes and hypertension | Nurse practitioner/ physician/ diabetes educator/medical assistant | Primary care | USA |
| Doughty et al. (2008) | Pre-posttest | To evaluate the delivery of a series of workshops on mental health recovery. | Mental illness | Mental health professional/ patients | Primary care | New Zeeland |
| Estabrooks et al. (2005) | RCT | To determine the frequency and effectiveness of goal choices and test goal setting theory hypotheses. | Diabetes | Physician | Primary care | USA |
| Evans-Hudnall et al. (2014) | RCT | To pilot a self-care treatment adapted for underserved racial/ethnic minority groups. | Stroke | Health educator | Hospital and community | USA |
| Fuchs et al. (2011) | Non-randomized controlled trial | To examine the effectiveness of the MOVO-Lisa intervention. | Orthopedic patients | Psychologist, physiotherapist | Outpatient rehabilitation | Germany |
| Glasgow et al. (2011) | RCT | To calculate various indices of website engagement. | Diabetes | Internist | Primary care | USA |
| Glasgow et al. (1996) | RCT | To evaluate an office-based intervention focused on behavioral issues for dietary self-management. | Diabetes | Internist | Primary care | USA |
| Glasgow et al. (2002) | RCT | To evaluate the effects of adding follow up components to a dietary goal-setting intervention. | Diabetes | Physician | Primary care | USA |
| Harris & Eng (2004) | Qualitative design | To identify goal priorities using a client-centered assessment. | Stroke | Occupational therapist | Community | Canada |
| Hart (1978) | RCT | To evaluate the effectiveness of setting goals in behavioral terms while monitoring attainment to goals. | Mental health problems | Psychotherapist | Community | USA |
| Holtrop et al. (2006) | RCT | To examine the types and influences of self-selected health behavior goals. | Cardio-vascular patients | Trained health educator | Hospital | USA |
| Kjeken et al. (2014) | Study protocol | To evaluate goal attainment, health effects and the cost-effectiveness of a new rehabilitation program. | Rheumatoid arthritis | Rehabilitation team | Rehabilitation | Norway |
| Kroese et al. (2014) | Pre-posttest | To investigate long-term outcomes of a self-management intervention targeting proactive coping. | Diabetes | Instructed trainers | Primary care | Nether-lands |
| Luszczynska (2006) | Pre-posttest | To investigate relations between implementation intention, a planning strategy and physical activity. | Myocardial infarction | Researcher | Rehabilitation | Poland |
| Lyons et al. (2015) | Qualitative design | To identify goals and patterns of goal attainment and to understand what women were trying to achieve. | Cancer | Occupational therapist | Hospital | USA |
| Magar et al. (2005) | RCT | To evaluate an educational program. | Asthma | Family practice professional | Community | France |
| Mansson Lexell et al. (2014) | Pre-posttest | To assess self-perceived performance and satisfaction with performance of daily activities | Multiple sclerosis | Occupational therapist | Rehabilitation | Sweden |
| McConkey & Collins (2010) | Qualitative design | To examine a goal setting approach and to identify the variables that influenced goal achievement. | Learning disabilities | Researcher | Residential care setting | Northern Ireland |
| Morganstern et al. (2011) | Qualitative design | To evaluate the Quality of Life Appraisal Profile. | Cancer | Researcher | Primary care | USA |
| Mullis & Hay (2010) | Intervention development study | To develop a goal-based individualized assessment tool capable of defining meaningful change. | Low back pain | Researcher | Primary care | UK |
| Murphy & Boa (2012) | Case study | To describe the use of the ICF framework, alongside Talking Mats, to enable participation in in goal setting. | Communi-cation difficulties | Rehabilitation professional | Outpatient rehabilitation | UK |
| Naik et al. (2011) | RCT | To evaluate the effectiveness of 2 interventions on glycosylated hemoglobin (HbA1c) levels. | Diabetes | Physician | Primary care | USA |
| Nuovo et al. (2009) | Pre-posttest | To assess differences between women and men in developing an action plan. | Diabetes | Diabetes educator | Community | USA |
| O’Connor et al. (2008) | RCT | To conduct a self-management intervention focusing on professional led vs patient led goal setting. | Intermittent allergic rhinitis | Pharmacist or pharmacy assistant | Pharmacy | Australia |
| Pagels et al. (2015) | Pre-posttest | To evaluate the effects of a group-based, multidimensional and multidisciplinary support program. | Diabetes | Nurse | Outpatient clinic | Sweden |
| Power et al. (2011) | Case study | To describe the application of the ICF to communication assessment and goal setting. | Huntington disease | Researcher | Residential care setting | Australia |
| Schneider et al. (2011) | Non-randomized controlled trial | To examine perception of life coaching and person-centered planning for maintaining employment and managing chronic health issues. | Diabetes | Life coach | Community | USA |
| Schreurs et al. (2003) | Intervention development study | To describe the development of a intervention to enhance self-management. | Asthma, diabetes, heart failure | Nurse | Primary care | Nether-lands |
| Scobbie et al. (2010) | Literature study | To describe the development of a theory-based goal setting practice framework. | Neurological diseases | Rehabilitation team | Rehabilitation | UK |
| Sniehotta et al. (2005) | RCT | To examine two interventions addressing self-regulatory skills in their effects on physical exercise. | Coronary heart disease | No professional | Rehabilitation | Germany |
| Stuifbergen et al. (2003) | RCT | To examine the effectiveness of a wellness intervention on achieving health-related goals. | Multiple sclerosis | Nurse practitioner | Community | USA |
| Steurer-Stey et al. (2015) | RCT | To examine the addition of the Zurich Resource Management training to a patient education program. | Asthma | Health educator | Primary care | Switzer-land |
| Theunissen et al. (2003) | RCT | To study whether illness representations and action plans change when general practitioners are trained. | Hypertension | Physician | Primary care | Nether-lands |
| Thoolen et al. (2009) | RCT | To examine the effectiveness of a proactive intervention. | Diabetes | Nurse | Primary care | Nether-lands |
| Tielemans et al. (2014) | Study protocol | To describe the theoretical basis and the content of the treatment protocol for ‘Plan ahead!’ | Stroke | Rehabilitation professionals | Outpatient rehabilitation | Nether-lands |
| Tomori et al. (2012) | Intervention development study | To develop and evaluate an IPad application to promote shared decision making in goal setting. | Any chronic conditions | Occupational therapist | Not specified | Japan |
| Toto et al. (2015) | Pre-posttest | To determine the feasibility of generating patient-centered goals. | Geriatric patients | Rehabilitation team | Primary care | USA |
| Tripicchio et al. (2009) | Pre- posttest | To examine if training professionals in the OPN (Ozer, Payton & Nelson) method improves goal setting. | Any chronic condition | Physical therapist/ occupational therapists | Primary care | USA |
| Voils et al. (2013) | RCT | To evaluate the effectiveness of a telephone-delivered, spouse-assisted lifestyle intervention. | Coronary heart disease | Nurse | Primary care | USA |
| Walker et al. (2009) | Qualitative design | To examine and describe goal setting among people who participated in the pilot testing of WebEase | Epilepsy | No professional | Community | USA |
| Wolever et al. (2010) | RCT | To evaluate the effectiveness of integrative health coaching. | Diabetes | Coach | Community | USA |
| Van der Wulp et al. (2012) | RCT | To investigate a self-management coaching intervention. | Diabetes | Expert patients | Primary care | Nether-lands |
| Zhang et al. (2015) | Qualitative design | To enhance the understanding of patient motivation for self-care through the examination of their goals | Cardio-vascular patients | Researcher | Outpatient setting | Canada |
Targets of goal setting/action planning
With regard to the targets of goals and action plans, the articles showed great variation. Thirty-five studies (60%) aimed to support patients in setting goals or formulating action plans for one or more lifestyle behaviors [12, 13, 27–59]. Goal setting and action planning were mostly intended to improve physical activity (n = 21, 36%), healthy eating (n = 17, 29%), and/or medication adherence (n = 13, 22%). In these articles, the targets of goals/action plans had been predefined. Other articles (n = 9, 16%) focused more on everyday activities and participation [60–68] or on patients’ quality of life and well-being (n = 4, 7%) [69–72]. Nine of the articles (16%) did not describe in detail the goals they focused on, but reported that patients were asked to set health-related goals or goals for rehabilitation [14, 73–80]. One article focused on the development of an action plan for managing deterioration of mental well-being for people suffering from a mental illness [81].
Theoretical framework
Nearly half of the articles (n = 27, 47%) reported a theoretical framework for goal setting/action planning. The most commonly used theoretical frameworks to underpin the use of goal setting or action planning as a method to change a person’s behavior were behavior change theories. The Social Cognitive Theory [82], in which self-efficacy is described as the key concept for setting goals [83], was mentioned in 14 articles (24%). Other behavioral change theories that were referred to were: Self-Regulation Theory [84] (n = 5, 9%), Proactive Coping Theory [85] (n = 4, 7%), Health Action Process Approach [86] (n = 3, 5%), Self-Determination Theory [87] (n = 1, 2%) and the Theory of Planned Behavior [88] (n = 1, 2%). These theories were reported to be used because of their focus on overcoming the intention-behavior gap and on planning behavior. The theory of Locke & Latham [89] was used in four articles (7%) to underpin the importance of specificity and difficulty of goals [14, 29, 37, 52]. One article reported the use of the 5 A´s framework [30]. This framework (Assess, Advise, Agree, Assist, Arrange) is a process model for self-management support that puts goal setting and action planning at the center of self-management support [8]. Although theories were thus mentioned in nearly half of the articles (n = 27, 47%), fifteen articles (26%) offered minimal or no explanation of the relation between theory and the development, content and format of goal setting and action planning.
Goal setting phases and components
The five main goal setting phases identified were (1) preparation, (2) formulation of goals, (3) formulation of action plan, (4) coping planning, and (5) follow-up (for definitions of all phases see Table 4 Phases and Components.). Nineteen of the articles (33%) included all phases [12–14, 27–37, 69–71, 73, 74]. Different components were identified for the preparation, coping planning and follow-up phases (see Table 4 Phases and Components.).
Table 4. Phases and components.
| Phase | Definition | Component |
|---|---|---|
| Preparation | Patients engage in activities prior to setting goals and making action plans (independently or with support from a professional). | Patient education (about the disease or relevant disease-related behaviors/factors) |
| Patient reflection (on current behavior and attitudes) | ||
| Identification of topics for setting goals | ||
| Formulation of goals | Patients’ goals are made explicit and are written down (independently or with support from a professional). | |
| Formulation of action plan | Patients’ action plans are made explicit and are written down (independently or with support from a professional). | |
| Coping planning | Patients explicitly formulate plans that describe how potential barriers to carrying out an action plan could be overcome (independently or with support from a professional). | Identification of barriers to carrying out the action plan |
| Identification of facilitators for carrying out the action plan | ||
| Assessment of confidence about carrying out the action plan | ||
| Formulation of strategies to overcome barriers | ||
| Follow-up | Patients actively work on achieving their goals and/or are supported in working on their goals and carrying out their action plans. | Patients’ self-monitoring of progress towards goal achievement |
| Support for the patients | ||
| Evaluation of progress or achievement |
The preparation phase was described in 49 of the 58 included articles (85%), and three components were identified: (1) patient education (about the disease or relevant disease-related behaviors/factors) (n = 22, 38%); (2) patient reflection (on current behaviors or attitudes) (n = 24, 41%); and (3) identification of topics for setting goals (any kind of topic or problem the patient wants to set a goal for) (n = 15, 26%). The formulation of goals was also reported in 49 articles (85%). The 9 articles (16%) that omitted the goal formulation phase incorporated the formulation of an action plan for a goal that was preset and identical for all participants [38–45, 81] (e.g. to increase physical activity). The formulation of an action plan was discussed in 38 articles (66%). The 20 articles (44%) that did not include the formulation of an action plan encouraged patients to set short-term behavioral goals, which were formulated as actions (e.g. feasible and measureable behavior goals for a lifestyle behavior). Thirty articles (52%) incorporated the phase of coping planning. Within this phase, our analysis revealed four components: (1) identification of barriers (factors that might impede goal achievement) (n = 24, 41%); (2) identification of facilitators (factors that might enhance goal achievement) (n = 6, 10%); (3) assessment of confidence (patient’s confidence about carrying out the action plan) (n = 7, 12%); and (4) formulation of strategies to overcome barriers (plans to overcome problems while working on goals) (n = 21, 36%). Forty-two articles (72%) mentioned a follow-up phase. In the follow-up phase, three components were identified: (1) patient self-monitoring (monitoring of progress in goal achievement by the patient) (n = 17, 29%); (2) support (practical or emotional support) for the patient (n = 17, 29%); and (3) evaluation of progress or achievement (interim evaluation of the progress and/or evaluation of goal achievement) (n = 25, 43%) (See S1 Table Overview of Phases and Components for each included Article).
Strategies
This section describes strategies that were mentioned in the articles for the different phases of the goal setting process. Strategies were defined as practical techniques to put a phase or component into practice (See S2 Table Overview of Mode of Delivery, Phases, Components and Strategies for each included Article).
Strategies for preparation
In the preparation phase, patients were often educated by means of written or visual materials (like workbooks, brochure, video’s or a website) (n = 13, 22%) [12, 30, 34, 36, 37, 46–50, 69, 74, 75] and/or in group meetings (n = 7, 12%) [42, 46, 47, 51–53, 74]. Patient reflection or self-assessment of their current status or behavior was usually done independently by the patients, without the help of a professional, by means of questionnaires (on paper or on a computer) (n = 5, 9%) [27, 29, 33, 54, 55] or self-care logs/diaries (n = 4, 7%) [28, 30, 37, 42]. Bearon et al. (2000) used ladder rating as a visual technique to reflect on the patient’s present status in acht self-selected functional areas (60). Five other articles (9%) investigated techniques for patient reflection on positive and negative aspects of changing behavior [27, 31, 40, 45, 90]. Three of these articles (5%) used mental contrasting or mental simulation as a strategy (for more explanation see S2 Table) [40, 45, 90]. Six articles (10%) discussed the exploration of patients’ overall perspectives on life and health [56, 60, 70, 72, 73, 76]. Patients were asked to reflect on their wishes in life, their hopes and fears or values for health, using in-depth interviews [60, 73, 76] or instruments like the Brief Quality of Life Appraisal profile [70], the Personal Value Care Sort [72] or the Wheel of Health [56] (for more explanation see S2 Table). Exchanging experiences with a group of peer patients was reported in four articles (7%) [54, 74, 81, 90]. Thirteen other articles (22%) focused on patients’ problems in everyday life and described individual interviews to identify and analyze these problems [34, 43, 57, 61–65, 71, 77–79]. Three of these articles (5%) used the Canadian Occupational Performance Measurement (COPM), a standardized outcome measure designed to capture a patient’s self-perception of performance in everyday living over time [61, 62, 65] (for more explanation see S2 Table). In addition, three articles (5%) used motivational interviewing to identify topics for discussion [57, 71, 80] and one article described the use of the visual instrument Talking Mats [63](for more explanation see S2 Table).
Strategies for formulation of goals
With regard to strategies for goal formulation, 16 articles (26%) focused on strategies for goal formulation using established criteria for effective goal setting [12–14, 32, 34, 35, 37, 48–51, 56, 58, 66, 71, 78]. In these articles, patients were stimulated to set specific, achievable, measurable, realistic, time-bound and behavioral goals (SMART criteria). However, the SMART criteria were only explicitly mentioned in three articles (5%) [37, 49, 71]. Scobbie et al. (2011) added that goals needed to be challenging for the patient [14]. Two other articles (3%) described encouraging patients to focus on long-term goals, often concerning their participation or life goals [56, 66]. Documenting patients’ goals was described in 19 articles (33%). In 11 of these articles (19%), goals were written down for the patient in records, cards or worksheets [27–29, 33, 55, 64, 66, 67, 75, 76, 78]. Cho et al (2013) and Tomori et al. (2012) used the method of contracting to document goals. Goals were written in the form of a contract, which was signed by both the professional and the patient [28, 67]. Six articles (10%) used patient workbooks or manuals in which patients could write down their goals [12, 13, 53, 69, 74, 80]. In five articles (9%) this was supported by group meetings or individual meetings with a professional [12, 13, 53, 74, 80]. Another reported strategy was the use of checklists for goals (n = 5, 9%) [32, 55, 59, 60, 68]. Checklists for goals, like the Personal Goals Checklist [60] or the Goals for Occupational Therapy List [68] (for more explanation see S2 Table) were used to encourage patients to select items from a list of pre-formulated goals. Five of the included articles (9%) described the use of the Goal Attainment Scaling (GAS) instrument as a strategy to set goals. GAS is a method that supports patients to set specific goals and to score the extent to which goals are achieved (for more explanation see S2 Table) [47, 51, 65, 78, 79].
Strategies for formulation of an action planning
Eight articles (14%) also described characteristics for action plans, four of them (7%) mentioning the formulation of implementation intentions as a strategy [31, 39–41]. Implementation intentions include the three action plan characteristics of indicating when, where and how the action is to be carried out. Four other articles (7%) applied the same criteria to patients’ action plans, but did not explicitly mention the implementation intention strategy [14, 33, 38, 44]. The documentation of action plans was reported in 12 articles (21%) [29, 33, 35, 36, 38, 41, 43, 44, 50, 54, 67, 78]. Nuovo et al. (2009) used a decision wheel to explore topics to talk about and to produce an action plan, which was then written on the back of the wheel [43]. This action plan incorporated the following components: When will I do it? Where will I do it? How often will I do it? What might get in the way? What can I do about it? [43] (for more explanation see S2 Table). Other strategies that were described included discussing and rating the level of difficulty of actions [70], discussing action plans with peers [52], and mental contrasting as a method to imagine possible actions [45] (for more explanation see S2 Table). Voils et al. (2013) involved spouses by developing a specific behavioral plan for spouses to support the patients’ goal achievement [36]. Doughty et al. (2008) described the use of a personal crisis plan for a possible deterioration of mental well-being for patients suffering from mental illnesses [81] (for more explanation see S2 Table).
Strategies for coping planning
Nine articles (16%) described strategies used for coping planning. In contrast to goals and action plans, coping plans were only documented in five articles (9%). If documented, they were always written down together with the action plans [29, 35, 38, 43, 44]. Four articles (7%) mentioned the use of motivational interviewing and the use of cognitive behavioral principles of problem solving as strategies to set coping plans [30, 40, 51, 55] (for more explanation see S2 Table).
Strategies for follow-up
Patients’ self-monitoring was almost always done using logbooks or diaries (n = 8, 14%) [13, 31, 34, 38, 44, 47, 50, 71]. Support for the patient (i.e. encouragement of patients by professionals and/or peer(s) to keep working on goals or action plans) was done via telephone or e-mail in six articles (10%) [27, 32, 39, 53, 55, 80]. In three articles (5%), support was provided in group sessions [32, 39, 52]. Kroese et al. (2014) described an extensive phase of goal reinforcement by means of three ‘booster sessions’ to enhance the attainability of goals and to discuss patient’s higher-order overarching goals [58] (for more explanation see S2 Table). Six articles (10%) used telephone calls to review progress and update goals or actions [12, 29, 31, 36, 38, 47]. In four articles (7%), review of progress was done within individual or group meetings [43, 50, 75, 76]. Five articles described the use of the GAS instrument to measure goal attainment (9%) [47, 51, 53, 78, 79] (for more explanation see S2 Table). Two articles (3%) involved measuring satisfaction about goal attainment by using the COPM [62] or Goal Satisfaction Rating [68] (for more explanation see S2 Table). Hart (1978) reported using an interview with a person from the patient’s social environment who was significant to the patient’s goal, as external validation of the patient’s self-reporting [78]. One article specifically emphasized patients’ future goal planning by means of follow-up calls [69]. The follow-up calls were intended to stimulate the patients to continue goal setting [69].
Mode of delivery
Goal setting phases, components and strategies varied significantly in terms of their duration, ranging from a single individual goal setting/action planning session to several meetings distributed over a year. The number of meetings with patients ranged from one to nine, and in 40 articles (69%), goal setting/action planning was applied at individual level or incorporated a mixture of individual and group sessions. Two articles (3%) presented goal setting/action planning as part of the usual/routine long-term care and therefore did not report the number of meetings [14, 73]. Forty-eight articles (83%) described face-to-face goal setting/action planning by a healthcare professional or researcher. In two articles (3%), the goal setting/action planning was supported by other (expert) patients, either only by expert patients [57] or by expert patients together with a healthcare professional [81]. Four articles (7%) described goal setting/action planning being provided by telephone calls and/or e-mail [34, 36, 48, 56]. In four other articles (7%), patients were taught to set their goals without the help of a professional, using a manual [44, 69] or a website [32, 37] (See S2 Table).
Discussion
This scoping review aimed to disentangle how goal setting and action planning are defined within the context of the patient self-management literature. We found 58 articles reporting on phases, components and strategies for goal setting/action planning, which differed greatly in terms of their duration (from a single goal setting session to several meetings distributed over one year). The analysis resulted in an overview of five goal setting phases (preparation, formulation of goals, formulation of action plan, coping planning and follow-up). Although the goal-setting phases we found are in accordance with commonly used definitions and frameworks for goal setting [8, 10, 21], the majority of articles did not include all phases of the goal setting process. As most articles did not give any explanation for the inclusion of phases (neither from a theoretical nor from other viewpoints), the rationale for their use or non-use remains unclear. In addition, we have created an overview of different components within the goal setting phases and an overview of practical strategies to put components into practice. Interestingly, the largest numbers of strategies were found for the phase prior to formulating goals and action plans, and for the follow-up phase. We found few articles focusing on the communication or discussions about goals/action plans or on possibilities to tailor the goal setting/action planning to the individual patient. This is in line with our finding that goal setting and action planning mostly concentrated on a single disease and focused on the improvement of one or more predefined lifestyle behaviors. Although half of the articles reported a theoretical framework for goal setting/action planning, the relation between the theory and the definition, content and format of goal setting and action planning was usually not clearly stated.
The majority of the articles included in this review (n = 35, 60.3%) focused on lifestyle improvement (e.g. increasing physical activity or improving diet). Patients were encouraged to set their own goals and action plans within the lifestyle domain, but the overall nature of their goals was predefined. Moreover, most of the goal setting strategies were designed for people with one specific chronic condition and excluded people with different conditions or suffering from multi-morbidity. In addition, few articles started the goal setting process with an exploration of patients’ values, allowing them to set goals that differ from the predefined nature of goals. Self-management support models highlight the importance of starting self-management support with an exploration of the patients’ values and beliefs [8, 91]. Patients with chronic conditions want to be listened to and are more motivated to work on their self-management when their individual values, needs and preferences are taken into account [92, 93]. Focusing self-management programs on one single disease might carry the risk of narrowing self-management to complying with medical instructions and lifestyle regulations, without much attention for the individual patient’s values [94]. This contrasts with the holistic character of the definition of self-management, which highlights the equal importance of social self-management (i.e. adjusting behavior to prevent negative outcomes and maintaining or adjusting life roles) and emotional self-management (i.e. dealing with emotional responses to a chronic condition and coping with discomfort and disability) [7]. In addition, the interrelations between patients’ different goals (e.g. that dealing with medical symptoms is frequently related to adjusting social roles) might be disregarded [95–97]. Although self-management programs exist for different chronic conditions [98], more research into self-management goal setting and action planning, including patients with different chronic conditions or people with multi-morbidity, might be useful, allowing for the integration of the patients’ values and setting self-management goals at different levels.
In line with this, we also found that few articles elaborated on strategies for tailoring goal setting/action planning to the individual patient’s readiness to change. Literature about self-management and goal setting emphasizes that chronically ill patients often go through an adaptation process, in which they learn to adapt to their condition and change their behavior accordingly [99]. Patients in different phases of their behavior change process might require different approaches for self-management goal setting and action-planning as regards forms of communication and the intensity of support [100, 101]. Earlier research has shown that self-management programs are frequently designed for individuals who are ready to change [101]. These programs might only reach a minority of those in need [101]. More research into the way self-management goal setting and action planning can be tailored to the individual patient’s adaptation process might be useful.
With regard to the strategies identified in this review, it is worth noting that a large variety of articles focused on characteristics of goals or action plans or on instruments facilitating goal setting, like the GAS [102] or the COPM [103]. Few articles focused on discussion and communication about goals, action plans or coping plans, or on strategies for the decision making process. Although principles of motivational interviewing [104] and cognitive behavior theory principles [105] were mentioned as communication strategies in some articles, they often failed to describe how these strategies were used to decide on goals, action plans or coping plans. This is surprising, since goal-setting is frequently regarded as a complex interactional activity, in which professionals and patients can face many communication problems [17]. Earlier research has shown that patients and professionals often find it difficult to make shared decisions about goals or actions [106–108]. Difficulties often relate to dealing with conflicting perspectives and priorities, ensuring patient participation, exploring the patient’s perspective and agreeing on goals and plans [17, 106, 107]. The findings of the present review indicate that uncertainty remains about the communication practices that are applied in setting goals, action plans and coping plans.
Our review has several strengths. First, we used a comprehensive search strategy across multiple databases with no date restrictions, minimizing the risk of having missed scientific articles about self-management goal setting/action planning. In addition, the process of including articles and extracting charting data was done by two researchers, to enhance the trustworthiness [26]. However, the results of the review may also have been subject to certain limitations. First, in our search we used a combination of keywords for the different concepts, but self-management, goal setting and action planning are broad concepts whose terminology varies greatly. It is possible that we have missed articles that used other terms with similar meanings. On the other hand, we checked reference lists to minimize this potential shortcoming. Second, we limited our search to databases of peer-reviewed, scientific articles. Books and grey literature were not included. As a result, we may have missed some publications describing self-management goal setting/action planning. However, we were especially interested in ways in which goal setting and action planning are defined in the scientific literature, and we did not expect to find this within books and grey literature. In future research it would be worthwhile to review goal setting/action planning fidelity, in order to explore barriers and facilitators for implementation.
Another problem we faced was that scientific publications are frequently restricted in terms of words and space, so most of the articles included, especially those on intervention trials, lacked a comprehensive description of their intervention. This restriction in the number of words might also be responsible for the minimal descriptions of the relation between the theoretical framework used and the definitions of goal setting and action planning. It is therefore possible that our overview of phases, components and strategies is incomplete and also that more authors than we found used a theoretical basis for their definition of goal setting/action planning. We attempted to minimize this risk by checking the references for other sources providing more detailed descriptions. In future studies, it might be worthwhile to actively approach the authors of the included studies for additional information.
Conclusion and implications
This scoping review assessed how self-management goal setting and action planning are defined. Although we focused on goal setting/action planning as described in the scientific literature, we think that our results might also encourage health care professionals to become more aware of:
the entire goal setting process, especially of the importance of the phase prior to setting goals and action plans and the follow up-phase;
possibilities to support patients in preparing for goal setting and working on goals by applying strategies focusing on patients’ self-reflection (e.g. logbooks, questions about values for health, visual methods);
possibilities to support patients (and professionals) in identifying and formulating goals/action plans using certain instruments (e.g. Talking mats, GAS, COPM).
This scoping review also resulted in some implications for research. More research might be useful to investigate:
goal setting and action planning for people suffering from different conditions or multi-morbidity;
strategies for tailoring self-management goal setting and action planning to the patient’s readiness to change;
communication strategies for goal setting and action planning that help patients and professionals overcome possible interactional difficulties (such as patient participation and agreement on goals).
effectiveness of goal setting/action planning on patients’ behavior and medical outcomes. Those studies should investigate intervention fidelity in order to gain a better understanding of how and why an intervention works.
Supporting information
(PDF)
(PDF)
Acknowledgments
We would like to thank Yvonne Schlenter for supporting the data selection and data extraction process.
Data Availability
All relevant data are within the paper and its supporting information files.
Funding Statement
This paper was funded by Stichting Innovatie Alliantie (PRO-3-36) (http://www.regieorgaan-sia.nl) and Zuyd University of Applied Sciences. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.World Health Organization. Global status report on noncommunicable diseases. 2014. http://apps.who.int/iris/bitstream/10665/148114/1/9789241564854_eng.pdf?ua=1
- 2.Wagner EH, Bennett SM, Austin BT, Greene SM, Schaefer JK, Von Korff M. Finding common ground: Patient-centeredness and evidence-based chronic illness care. J Altern and Complement Med. 2005;11(Suppl 1): 7–15. [DOI] [PubMed] [Google Scholar]
- 3.Barr VJ, Robinson S, Marin-Link B, Underhill L, Dotts A, Ravensdale D, et al. The expanded Chronic Care Model: An integration of concepts and strategies from population health promotion and the Chronic Care Model. Hosp Q. 2003;7(1): 73–82. [DOI] [PubMed] [Google Scholar]
- 4.Bodenheimer T, MacGregor K, Sharifi C. Helping Patients Manage Their Chronic Conditions. 2005. California Health Care Foundation. http://www.chcf.org/~/media/MEDIA%20LIBRARY%20Files/PDF/PDF%20H/PDF%20HelpingPatientsManageTheirChronicConditions.pdf
- 5.Lorig KR, Holman HR. Self-Management Education: History, Definition, Outcomes and Mechanisms. Ann Behav Med. 2003; 26(1): 1–7. [DOI] [PubMed] [Google Scholar]
- 6.Lawn S, Schoo A. Supporting self-management of chronic health conditions: common approaches. Patient Educ Couns. 2010; 80(2): 205–211. doi: 10.1016/j.pec.2009.10.006 [DOI] [PubMed] [Google Scholar]
- 7.Corbin J, Strauss J. Unending work and care: Managing chronic illness at home. Jossey-Bass; San Francisco, CA: 1988. [Google Scholar]
- 8.Bodenheimer T, Grumbach K. Self-Management Support for People with Chronic Illness In: Shanahan JF, Brown RY. Improving Primary Care—Strategies and tools for a better practice. New York: The MacGraw-Hill Companies; 2007. p.79–98. [Google Scholar]
- 9.Bodenheimer T, Hadley MA. Goal-setting for behavior change in primary care: An exploration and status report. Patient Educ Couns. 2009;76(2): 174–180. doi: 10.1016/j.pec.2009.06.001 [DOI] [PubMed] [Google Scholar]
- 10.Lorig K. Action Planning: A Call To Action. J Am Board Fam Med. 2006;19(3): 324–325. [DOI] [PubMed] [Google Scholar]
- 11.Langford AT, Sawyer DR, Gioimo S, Brownson CA, O’Toole ML. Patient-centered goal setting as a tool to improve diabetes self-management. Diabetes Educ. 2007;33(Suppl 6): 139–144. [DOI] [PubMed] [Google Scholar]
- 12.DeWalt DA, Davis TC, Wallace AS, Seligman HK, Bryant-Shilliday B, Arnold CL, et al. Goal setting in diabetes self-management: taking the baby steps to success. Patient Educ Couns. 2009;77(2): 218–223. doi: 10.1016/j.pec.2009.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thoolen BJ, de Ridder D, Bensing J, Gorter K, Rutten G. Beyond good intentions: The role of proactive coping in achieving sustained behavioral change in the context of diabetes management. Psychol Health. 2009;24(3): 237–254. doi: 10.1080/08870440701864504 [DOI] [PubMed] [Google Scholar]
- 14.Scobbie L, Dixon D, Wyke S. Goal setting and action planning in the rehabilitation setting: development of a theoretically informed practice framework. Clin Rehabil. 2010;25(5): 468–482. doi: 10.1177/0269215510389198 [DOI] [PubMed] [Google Scholar]
- 15.Rutten GEHM, de Grauw WJC, Nijpels G, Gouds-Waard AN, Uitewaal PJM, van der Does FEE, et al. [Dutch College of General Practitioners—Guidelines for Diabetes Mellitus Type 2]. Huisarts Wet. 2006;49(3): 137–152. (Dutch). https://www.nhg.org/standaarden/volledig/nhg-standaard-diabetes-mellitus-type-2 [Google Scholar]
- 16.The National Collaborating Centre for Chronic Conditions. Rheumatoid Arthritis—National clinical guideline for management and treatment in adults. 2009. London: https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0009576/pdf/PubMedHealth_PMH0009576.pdf [Google Scholar]
- 17.Parry RH. Communication during goal-setting in physiotherapy treatment session. Clin Rehabil. 2004;18(6): 668–682. doi: 10.1191/0269215504cr745oa [DOI] [PubMed] [Google Scholar]
- 18.Blakeman T, Macconald W, Bower P, Gately C, Chew-Graham C. A qualitative study of GP’s attitudes to self-management of chronic disease. Br J Gen Pract. 2006;56(527): 407–414. [PMC free article] [PubMed] [Google Scholar]
- 19.MacGregor K, Handley M, Wong S, Sharifi C, Gjeltema K, Schillinger D, et al. Behavior-Change Action Plans in Primary Care: A Feasibility Study of Clinicians. I Am Board Fam Med. 2006;19(3): 215–223. [DOI] [PubMed] [Google Scholar]
- 20.Wade DT. Editorial: Goal setting in rehabilitation: an overview of what, why and how. Clin Rehabil. 2009;23(4): 291–295. doi: 10.1177/0269215509103551 [DOI] [PubMed] [Google Scholar]
- 21.Rosewilliam S, Roskell CA, Pandyan AD. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal-setting in stroke rehabilitation. Clin Rehabil. 2011;25(6): 1–14. [DOI] [PubMed] [Google Scholar]
- 22.Young CA, Manmathan GP, Ward JC. Perceptions of goal-setting in a neurological rehabilitation unit: A qualitative study of patients, carers and staff. J Rehabil Med. 2008;40(3): 190–194. doi: 10.2340/16501977-0147 [DOI] [PubMed] [Google Scholar]
- 23.Playford ED, Siegert RJ, Levack WMM, Freeman J. Areas of consensus and controversy about goal setting in rehabilitation: a conference report. Clin Rehabil. 2009;23(4): 334–344. doi: 10.1177/0269215509103506 [DOI] [PubMed] [Google Scholar]
- 24.Levack WM, Taylor K, Siegert RJ, Dean SG, McPherson KM, Weatherall M. Is goal planning in rehabilitation effective? A systematic review. Clin Rehabil. 2006;20(739): 739–755. [DOI] [PubMed] [Google Scholar]
- 25.Arksey H, O’Malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1): 19–32. [Google Scholar]
- 26.Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5 (1): 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Calfas KJ, Sallis JF, Zabinski MF, Wilfley DE, Rupp J, Prochaska JJ, et al. Preliminary evaluation of a multicomponent program for nutrition and physical activity change in primary care: PACE+ for adults. Prev Med. 2002;34(2): 153–161. doi: 10.1006/pmed.2001.0964 [DOI] [PubMed] [Google Scholar]
- 28.Cho MK. Effect of health contract intervention on renal dialysis patients in Korea. Nurs Health Sci. 2013;15(1): 86–93. doi: 10.1111/nhs.12003 [DOI] [PubMed] [Google Scholar]
- 29.Estrabrooks PA, Nelson CC, Xu S, King D, Bayliss EA, Gaglio B, et al. The frequency and behavioral outcomes of goal choices in the self-management of diabetes. Diabetes Educ. 2005;31(3): 391–400. doi: 10.1177/0145721705276578 [DOI] [PubMed] [Google Scholar]
- 30.Evans-Hudnall GL, Stanley MA, Clark AN, Bush AL, Resnicow K, Liu Y, et al. Improving secondary stroke self-care among underserves ethnic minority individuals: A randomized clinical trial of a pilot intervention. J Behav Med. 2014;37(2): 196–204. doi: 10.1007/s10865-012-9469-2 [DOI] [PubMed] [Google Scholar]
- 31.Fuchs R, Goehner W, Seelig H. Long-term effects of a psychological group intervention on physical exercise and health: the MoVo concept. J Phys Act Health. 2011;8(6): 794–803. [DOI] [PubMed] [Google Scholar]
- 32.Glasgow RE, Christiansen SM, Kurz D, King DK, Woolley T, Faber AJ, et al. Engagement in a diabetes self-management website: usage patterns and generalizability of program use. J Med Internet Res. 2011;13(1): e9 doi: 10.2196/jmir.1391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Glasgow RE, Toobert DJ, Hampson SE. Effects of a brief office-based intervention to facilitate diabetes dietary self-management. Diabetes Care. 1996;19(8): 835–41. [DOI] [PubMed] [Google Scholar]
- 34.Lyons KD, Svensborn IA, Kornblith AB, Hegel MT. A content analysis of functional recovery strategies of breast cancer survivors. OTJR (Thorofare NJ). 2015;35(2): 73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Steurer-Stey C, Storch M, Benz S, Hobi B, Steffen-Bürgi B, Steurer J, et al. Motivational training improves self-efficacy but nog short-term adherence with asthma self-management: A randomized controlled trial. Prim Health Care Res Dev. 2015;16(1): 32–41. doi: 10.1017/S1463423613000480 [DOI] [PubMed] [Google Scholar]
- 36.Voils CI, Coffman CJ, Yancy WS Jr, Weinberger M, Jeffreys AS, Datta S, et al. A randomized controlled trial to evaluate the effectiveness of couples: a spouse-assisted lifestyle change intervention to improve low-density lipoprotein cholesterol. Prev Med. 2012;56(1): 46–52. doi: 10.1016/j.ypmed.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 37.Walker ER, Wexler B, Dilorio C, Escoffery C, McCarty F, Yeager KA. Content and characteristics of goals created during a self-management intervention for people with epilepsy. J Neurosci Nurs. 2009;41(6): 312–21. [DOI] [PubMed] [Google Scholar]
- 38.Arbour-Nicitopoulus KP, Ginis KA, Latimer AE. Planning, leisure-time physical activity, and coping self-efficacy in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90(12): 2003–2011. doi: 10.1016/j.apmr.2009.06.019 [DOI] [PubMed] [Google Scholar]
- 39.Lourenco LB, Rodrigues RC, Ciol MA, Sao-Joao TM, Cornelio ME, Dantas RA, et al. A randomized controlled trial of the effectiveness of planning strategies in the adherence to medication for coronary artery disease. J Adv Nurs. 2014;70(7): 16–28. [DOI] [PubMed] [Google Scholar]
- 40.Christiansen S, Oettingen G, Dahme B, Klinger R. A short goal-pursuit intervention to improve physical capacity: a randomized clinical trial in chronic back pain patients. Pain. 2010;149(3): 444–452. doi: 10.1016/j.pain.2009.12.015 [DOI] [PubMed] [Google Scholar]
- 41.Luszczynska A. An implementation intentions intervention, the use of a planning strategy, and physical activity after myocardial infarction. Soc Sci Med. 2006;62(4): 900–908. doi: 10.1016/j.socscimed.2005.06.043 [DOI] [PubMed] [Google Scholar]
- 42.Magar Y, Vervloet D, Steenhouwer F, Smaga S, Mechin H, Rocca Serra JP, et al. Assessment of a therapeutic education program for asthma patients: ‘Un soufflé nouveau’. Patient Educ Couns. 2005;58(1): 41–46. doi: 10.1016/j.pec.2004.05.016 [DOI] [PubMed] [Google Scholar]
- 43.Nuovo J, Balsbaugh T, Levich B. Gender differences in the selection of an action plan for patients with type 2 diabetes mellitus. The patient: Patient-Centered Outcomes Research. 2009;2(3): 203–208 [DOI] [PubMed] [Google Scholar]
- 44.Sniehotta FF, Scholz U, Schwarzer R, Fuhrmann B, Kiwus U, Völler H. Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. Int J Behav Med. 2005;12(4): 244–255. doi: 10.1207/s15327558ijbm1204_5 [DOI] [PubMed] [Google Scholar]
- 45.Theunissen NCM, de Ridder DTD, Bensing JM, Rutten GEHM. Manipulation of patient-provider interaction: Discussing illness representations or action plans concerning adherence. Patient Educ Couns. 2003;51(3): 247–258. [DOI] [PubMed] [Google Scholar]
- 46.Corser W, Holmes-Rovner M, Lein C, Gossain V. A shared decision-making primary care intervention for type 2 diabetes. Diabetes Educ. 2007;33(4): 700–708. doi: 10.1177/0145721707304086 [DOI] [PubMed] [Google Scholar]
- 47.Davis GC, White TL. A goal attainment pain management program for older adults with arthritis. Pain Manag Nurs. 2008;9(4): 171–179 doi: 10.1016/j.pmn.2008.02.007 [DOI] [PubMed] [Google Scholar]
- 48.Holtrop JS, Corser W, Jones G, Brooks G, Holmes—Rovner M, Stommel M. Health behavior goals of cardiac patients after hospitalization. Am J Health Behav. 2006;30(4): 387–399. [DOI] [PubMed] [Google Scholar]
- 49.Pagels AA, Hylander B, Alvarsson M. A multi-dimensional support program for patients with diabetic kidney disease. J Ren Care. 2015;41(3): 187–194. doi: 10.1111/jorc.12114 [DOI] [PubMed] [Google Scholar]
- 50.Schreurs KM, Colland VT, Kuijer RG, de Ridder DT, van Elderen T. Development, content, and process evaluation of ha short self-management intervention in patients with chronic diseases requiring self-care behaviors. Patient Educ Couns. 2003;51(2): 133–141. [DOI] [PubMed] [Google Scholar]
- 51.Becker H, Stuifbergen A, Taxis C, Beal CC, Pierini DM. The use of goal attainment scaling to facilitate and assess individualized change in a wellness intervention for women with fibromyalgia syndrome. J Holist Nurs. 2009;27(4): 232–240. doi: 10.1177/0898010109339525 [DOI] [PubMed] [Google Scholar]
- 52.Naik AD, Palmer N, Petersen NJ, Street RL Jr, Rao R, Suarez-Almazor M, et al. Comparative effectiveness of goal setting in diabetes mellitus group clinics: randomized clinical trial. Arch Intern Med. 2011;171(5): 453–459. doi: 10.1001/archinternmed.2011.70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Stuifbergen AK, Becker H, Timmerman GM, Kulberg V. The Use of Individualized Goal Setting to Facilitate Behavior Change in Women with Multiple Sclerosis. Journal Neurosci Nurs. 2003;35(2): 94–100. [DOI] [PubMed] [Google Scholar]
- 54.Dickman K, Pintz C, Gold K, Kivlahan C. Behavior changes in patients with diabetes and hypertension after experiencing shared medical appointments. J Am Acad of Nurse Pract. 2012;24(1): 43–51. [DOI] [PubMed] [Google Scholar]
- 55.Glasgow RE, Toobert DJ, Hampson SE, Strycker LA. Implementation, generalization and long-term results of the “choosing well” diabetes self-management intervention. Patient Educ Couns. 2002;48(2): 115–122. [DOI] [PubMed] [Google Scholar]
- 56.Wolever RQ, Dreusicke M, Fikkan J, Hawkins TV, Yeung S, Wakefield J, et al. Integrative health coaching for patients with type 2 diabetes: A randomized clinical trial. Diabetes Educ. 2010;36(4):629–639. doi: 10.1177/0145721710371523 [DOI] [PubMed] [Google Scholar]
- 57.Van der Wulp I, de Leeuw JRJ, Gorter KJ, Rutten GEHM. Effectiveness of peer-led self-management coaching for patients recently diagnosed with Type 2 diabetes mellitus in primary care: a randomized controlled trial. Diabetes Med. 2012;29(10): 390–397. [DOI] [PubMed] [Google Scholar]
- 58.Kroese FM, Adriaanse MA, Vinkers CDW, van de Schoot R, de Ridder DTD. The effectiveness of a proactive coping intervention targeting self-management in diabetes patients. Psychol Health. 2014;29(1): 110–125. [DOI] [PubMed] [Google Scholar]
- 59.Briggs Early K, Armstrong Shultz J, Evans M, Corbett CF, Nicholson Butkus S, Massey L. Dietary goal attainment measures and psychosocial factors among Mexican Americans and non-Hispanic whites with type 2 diabetes. Ecol Food Nutr. 2012;51(3): 227–246. doi: 10.1080/03670244.2012.674446 [DOI] [PubMed] [Google Scholar]
- 60.Bearon LB, Crowley GM, Chandler J, Robbins MS, Studenski S. Personal functional goals: A new approach to assessing patient-centered outcomes. J Appl Gerontol. 2000;19 (3): 326–344. [Google Scholar]
- 61.Harris JE, Eng JJ. Goal priorities identified through client-centered measurement in individuals with chronic stroke. Physiother Can. 2004;56(3): 171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Manson Lexell EM, Flansbjer UB, Lexell J. Self-perceived performance and satisfaction with performance of daily activities in persons with multiple sclerosis following interdisciplinary rehabilitation. Disabil Rehabil. 2014;36(5): 373–378. doi: 10.3109/09638288.2013.797506 [DOI] [PubMed] [Google Scholar]
- 63.Murphy J, Boa S. Using the WHO-ICF with Talking Mats to Enable Adults with Long-term Communication Difficulties to Participate in Goal Setting. AAC. 2012;28(1): 52–60. doi: 10.3109/07434618.2011.653828 [DOI] [PubMed] [Google Scholar]
- 64.Power E, Anderson A, Togher L. Applying the WHO ICF-framework to communication assessment and goal setting in Huntington’s disease: a case discussion. J Commun Disord. 2011;44(3): 261–275. doi: 10.1016/j.jcomdis.2010.12.004 [DOI] [PubMed] [Google Scholar]
- 65.Toto PE, Skidmore ER, Terhorst L, Rosen J, Weiner DK. Goal Attainment Scaling (GAS) in geriatric primary care: a feasibility study. Arch Gerontol Geriater. 2014;60(1): 16–21. [DOI] [PubMed] [Google Scholar]
- 66.McConkey R, Collins S. Using personal goal setting to promote the social inclusion of people with intellectual disability living in supported accommodation. J Intellect Disabil Res. 2009;54(2): 135–143. doi: 10.1111/j.1365-2788.2009.01224.x [DOI] [PubMed] [Google Scholar]
- 67.Tomori K, Uezu S, Kinjo S, Ogahara K, Nagatani R, Higashi T. Utilization of the iPad application: Aid for Decision-making in Occupation Choice. Occup Ther Int. 2011;19(2): 88–97. doi: 10.1002/oti.325 [DOI] [PubMed] [Google Scholar]
- 68.Custer MG, Huebner RA, Freudenberger L, Nichols LR. Client-Chosen Goals in Occupational Therapy: Strategy and Instrument Pilot. Occup Ther Health Care. 2013;27(1): 58–70. doi: 10.3109/07380577.2012.747120 [DOI] [PubMed] [Google Scholar]
- 69.Coote HM, Macleod AK. A self-help, positive goal-focused intervention to increase well-being in people with depression. Clin Psychol Psychother. 2012; 19(4): 305–315. doi: 10.1002/cpp.1797 [DOI] [PubMed] [Google Scholar]
- 70.Morganstern BA, Bochner B, Dalbagni G, Shabsigh A, Rapkin B. The psychological context of quality of life: a psychometric analysis of a novel idiographic measure of bladder cancer patients’ personal goals and concerns prior to surgery. Health Qual Life Outcomes. 2011;9: 10 doi: 10.1186/1477-7525-9-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Schneider JI, Hashizume J, Heak S, Maetani L, Ozaki RR, Watanabe DL. Identifying challenges, goals and strategies for success for people with diabetes through life coaching. Journal of Vocational Rehabilitation. 2011;34(2): 129–139. [Google Scholar]
- 72.Zhang KM, Dindoff K, Arnold JMO, Lane J, Swartzman LC. What matters to patients with heart failure? The influence of non-health-related goals on patient adherence to self-care management. Patient Educ Couns. 2015;98(8): 927–934. doi: 10.1016/j.pec.2015.04.011 [DOI] [PubMed] [Google Scholar]
- 73.Chunchu K, Mauksch L, Charles C, Ross V, Pauwels J. A patient centered care plan in the EHR: improving collaboration and engagement. Fam Syst Health. 2012;30(3): 199–209. doi: 10.1037/a0029100 [DOI] [PubMed] [Google Scholar]
- 74.Tielemans NS, Schepers VPM, Visser-Meily JMA, van Erp J, Eijkenaar M, van Heugten CM. The Restore4Stroke self-management intervention ‘Plan ahead!’: rationale and description of the treatment protocol based on proactive action planning. Clin Rehabil. 2014;28(6): 530–540. doi: 10.1177/0269215513514460 [DOI] [PubMed] [Google Scholar]
- 75.O’Connor J, Seeto C, Saini B, Bosnic-Anticevich S, Krass I, Armour C, et al. Healthcare professional versus patient goal setting in intermittent allergic rhinitis. Patient Educ Couns. 2007;70(1): 111–117. doi: 10.1016/j.pec.2007.09.004 [DOI] [PubMed] [Google Scholar]
- 76.Tripicchio B, Bykerk K, Wegner C, Wegner J. Increasing patient participation: the effects of training physical and occupational therapists to involve geriatric patients in the concerns-clarification and goal-setting processes. J Phys Ther Educ. 2009;23(1): 55–63. [Google Scholar]
- 77.Buchi S, Straub S, Schwager U. [Shared decision-making and individualized goal setting—a pilot trial using PRISM (Pictorial Representation of Illness and Self Measure) in psychiatric inpatients]. Praxis. 2010;99(24): 1467–1477. German doi: 10.1024/1661-8157/a000320 [DOI] [PubMed] [Google Scholar]
- 78.Hart RR. Therapeutic Effectiveness of Setting and Monitoring Goals. J Consult Clin Psychol. 1978;46(6): 1242–1245. [DOI] [PubMed] [Google Scholar]
- 79.Mullis R, Hay EM. Goal scaling for low back pain in primary care: development of a semi-structured interview incorporating minimal important change. J Eval Clin Pract. 2010;16(6): 1209–1214. doi: 10.1111/j.1365-2753.2009.01296.x [DOI] [PubMed] [Google Scholar]
- 80.Kjeken I, Berdal G, Bo I, Dager T, Dingsor A, Hagfors J, et al. Evaluation of a structured goal planning and tailored follow-up program in rehabilitation for patients with rheumatic diseases: Protocol for a pragmatic, stepped-wedge cluster randomized trial. BMC Musculoskelet Disord. 2014;15:153 doi: 10.1186/1471-2474-15-153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Doughty C, Tse S, Duncan N, McIntyre L. The Wellness Recovery Action Plan (WRAP): workshop evaluation. Australas Psychiatry 2008, 16(6): 450–456. doi: 10.1080/10398560802043705 [DOI] [PubMed] [Google Scholar]
- 82.Bandura A. Social foundations of thought and action: A social cognitive theory. Englewood Cliffs, New Jersey: Prentice-Hall, Inc; 1986. [Google Scholar]
- 83.Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2): 191–215. [DOI] [PubMed] [Google Scholar]
- 84.Leventhal H, Leventhal EA, Contrada R. Self-regulation, health, and behavior: A perceptual-cognitive approach. Psychol Health. 1998;13(4): 717–733. [Google Scholar]
- 85.Aspinwall LG, Taylor SE. A stitch in time: self-regulation and proactive coping. Psychol Bull. 1997;121(3): 417–436. [DOI] [PubMed] [Google Scholar]
- 86.Schwarzer R. Self-efficacy: Thought control of action. Washington DC: Hemisphere; 1992. [Google Scholar]
- 87.Deci El, Ryan RM. Intrinsic motivation and self-determination in human behavior. New York: Plenum; 1985. [Google Scholar]
- 88.Aijzen I. The Theory of Planned Behavior. Organizational Behavior and Human Decision processes. 1991;50(2): 179–211. [Google Scholar]
- 89.Locke EA, Latham GP. Building a practically useful theory of goal-setting and task motivation: A 35-year Odyssey. Am Psychol. 2002;57(9): 705–717. [DOI] [PubMed] [Google Scholar]
- 90.Thoolen BJ, de Ridder D, Bensing J, Gorter K, Rutten G. Beyond good intentions: The role of proactive coping in achieving sustained behavioral change in the context of diabetes management. Psychol Health. 2009;24(3): 237–254. doi: 10.1080/08870440701864504 [DOI] [PubMed] [Google Scholar]
- 91.Glasgow Re, Emont S, Miller DC. Assessing delivery of the five ‘As’ for patient-centered counseling. Health Promot Int. 2006;21(3): 245–255. doi: 10.1093/heapro/dal017 [DOI] [PubMed] [Google Scholar]
- 92.Bayliss EA, Edwards AE, Steiner JF, Main DS. Processes of care desired by elderly patients with multi-morbidities. Fam Pract. 2008;25(4): 287–293. doi: 10.1093/fampra/cmn040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Rijken M, Bekkema N, Boeckxstaens P, Schellevis FG, de Maeseneer JM, Groenewegen PP. Chronic Disease Management Programs: an adequate response to patients’ needs? Health Expect. 2012;17(5): 608–621. doi: 10.1111/j.1369-7625.2012.00786.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Cramm JM, Nieboer AP. Disease management: The need for a focus on broader self-management abilities and quality of life. Popul Health Manag. 2015;18(4): 246–255. doi: 10.1089/pop.2014.0120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Lenzen SA, Daniels R, van Bokhoven MA, Weijden T, Beurskens A. Setting goals in chronic care: Shared decision making as self-management support by the family physician. Eur J Gen Pract. 2014;21(2): 138–144. doi: 10.3109/13814788.2014.973844 [DOI] [PubMed] [Google Scholar]
- 96.Barlow J, Edwards R, Turner A. The experience of attending a lay-led, chronic disease self-management program from the perspective of participants with multiple sclerosis. Psychol Health. 2009;24(10): 1167–1180. doi: 10.1080/08870440802040277 [DOI] [PubMed] [Google Scholar]
- 97.Brown VA, Bartholomew LK, Naim AD. Management of chronic hypertension in older men: An exploration of patient goal setting. Patient Educ Couns. 2007;69(1–3): 93–99. doi: 10.1016/j.pec.2007.07.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Lorig K, Sobel DS, Stewart AL, Brown BW, Bandura A, Ritter P, et al. Evidence suggesting that a chronic disease self-management program can improve health status while reducing hospitalization: a randomized trial. Med Care. 1999;37(1): 5–14. [DOI] [PubMed] [Google Scholar]
- 99.Peolsson M, Hyden LC, Satterlund Larson U. Living with Chronic Pain: a dynamic learning process. Scand J Occup Ther. 2000;7(3): 114–125. [Google Scholar]
- 100.Keefe FJ, Lefebvre JC, Kerns RD, Rosenberg R, Beaupre P, Prochaska J, et al. Understanding the adoption of arthritis self-management: stages of change profiles among arthritis patients. Pain. 2000;87(3): 303–313. [DOI] [PubMed] [Google Scholar]
- 101.Jones H, Edwards L, Vallis TM, Ruggiero L, Rossi SR, Rossi JS, et al. Changes in diabetes self-care behaviors make a difference in glycemic control. Diabetes Care. 2003;26(3): 732–737. [DOI] [PubMed] [Google Scholar]
- 102.Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil. 2009;23(4): 362–370. doi: 10.1177/0269215508101742 [DOI] [PubMed] [Google Scholar]
- 103.Carswell A, McColl MA, Baptiste S, Law M, Polataijko H, Pollock N. The Canadian Occupational Performance Measure: A research and clinical literature review. Can J Occup Ther. 2004;71(4): 210–222. doi: 10.1177/000841740407100406 [DOI] [PubMed] [Google Scholar]
- 104.Miller WR, Rollnick S. Motivational Interviewing, Helping People Change. New York: The Guilford Press; 2013. [Google Scholar]
- 105.Sage N, Sowden M, Chorlonton E, Edeleanu A. CBT for Chronic Illness and Palliative Care—A Workbook and Toolkit. Southern Gate, Chichester: John Wiley & Sons Ltd, The Atrium; 2008. [Google Scholar]
- 106.Elwyn G, Edwards A, Kinnersley P. Shared decision-making in primary care: the neglected second half of the consultation. Br J of Gen Pract. 1999; 49(443): 477–482. [PMC free article] [PubMed] [Google Scholar]
- 107.Baker SM, Marshak HH, Rice GT, Zimmermann GJ. Patient Participation in Physical Therapy Goal Setting. J Am Phys Ther Assoc. 2001;81(5): 1118–1126. [PubMed] [Google Scholar]
- 108.Plant SE, Tyson SF, Kirk S, Parson J. What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis. Clin Rehabil. 2016, 30(9): 921–930. doi: 10.1177/0269215516655856 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its supporting information files.