In this EMA study, we examined the association between momentary factors such as parental stress and depressed mood and food-related parenting practices.
Abstract
BACKGROUND:
Research suggests that stress and depressed mood are associated with food-related parenting practices (ie, parent feeding practices, types of food served at meals). However, current measures of parental stress, depressed mood, and food-related parenting practices are typically survey-based and assessed as static/unchanging characteristics, failing to account for fluctuations across time and context. Identifying momentary factors that influence parent food-related parenting practices will facilitate the development of effective interventions aimed at promoting healthy food-related parenting practices. In this study, we used ecological momentary assessment to examine the association between momentary factors (eg, stress, depressed mood) occurring early in the day and food-related parenting practices at the evening meal.
METHODS:
Children aged 5 to 7 years and their families (N = 150) from 6 racial and/or ethnic groups (n = 25 each African American, Hispanic/Latino, Hmong, American Indian, Somali, and white families) were recruited for this mixed-methods study through primary care clinics.
RESULTS:
Higher stress and depressed mood earlier in the day predicted pressure-to-eat feeding practices and fewer homemade foods served at meals the same night. Effect modification was found for certain racial and/or ethnic groups with regard to engaging in pressure-to-eat feeding practices (ie, America Indian, Somali) or serving fewer homemade meals (ie, African American, Hispanic/Latino) in the face of high stress or depressed mood.
CONCLUSIONS:
Clinicians may want to consider discussing with parents the influence stress and depressed mood can have on everyday food-related parenting practices. Additionally, future researchers should consider using real-time interventions to reduce parental stress and depressed mood to promote healthy parent food-related parenting practices.
What’s Known on This Subject:
Stress and depressed mood have been hypothesized to influence food-related parenting practices. However, stress, mood, and parenting practices are often measured as static and/or unchanging characteristics, failing to account for fluctuations across time and context.
What This Study Adds:
In this EMA study, we examined the association between momentary stress and depressed mood and food-related parenting practices. Higher parental stress and depressed mood earlier in the day predicted pressure-to-eat feeding practices and fewer homemade foods served at dinner the same night.
Previous studies have revealed that food-related parenting practices such as parent feeding practices and healthfulness of foods served at family meals are associated with child weight and weight-related outcomes.1–12 For example, controlling parent feeding practices such as restriction and pressure-to-eat have been found to be associated with overweight status,6–8 unhealthy diet quality,7–9 lower satiety responsiveness,10,11 and unhealthy weight control behaviors12 in children. Additionally, researchers have suggested that serving unhealthy foods at family meals (eg, energy dense foods, high-fat foods, sugar-sweetened beverages) is associated with more unhealthy diet quality and overweight status in children.1–5 Given the potential harmful outcomes associated with controlling parent feeding practices and unhealthy food served at family meals, it is important to find predictors of these food-related parenting practices. Two important factors that may increase a parent’s potential to engage in controlling feeding practices or to serve unhealthy foods at family meals are stress and depressed mood.
There is a large body of research that indicates elevated levels of stress contribute to a parent’s own unhealthy dietary intake,13,14 unhealthful food preparation,13 weight status,14 and weight control behaviors (eg, emotional eating).14–17 In addition, previous studies have revealed that depressed mood is associated with a parent’s excess weight and unhealthier lifestyle.18 However, little is known about whether a parent’s stress levels or depressed mood are associated with engaging in more or less controlling parent feeding practices with their children or serving more or less unhealthy foods at meals.19 Of the limited previous studies, results have revealed that maternal depressed mood was associated with increased risk of engaging in pressure-to-eat feeding practices20 and that stress was associated with parent controlling feeding practices with children.19 In addition, the authors of 1 study showed that parent depressed mood was associated with serving less healthy foods to adolescents at family meals.4 Although the authors of these previous studies suggest that there may be a connection between parental stress and depressed mood and food-related parenting practices, there are limitations with the research. For example, researchers for past studies have measured stress, depressed mood, and food-related parenting practices using self-report or static measures, which are prone to social desirability, lack of specificity, and assume food-related parenting practices do not fluctuate. Additionally, few studies have been focused on populations from diverse ethnic and/or racial and low socioeconomic status backgrounds, which is important given the high prevalence of both obesity and stress in these populations.21–23
With this study, we build on and expand the previous research in which researchers examined associations between parental stress and depressed mood and parent food-related parenting practices by using ecological momentary assessment (EMA) of both the exposure variables (ie, parental stress, depressed mood) and outcome variables (ie, parent feeding practices, healthfulness of foods served at dinner). EMA is a powerful technique that uses a smartphone-based Web application to record behaviors and/or ratings of stress, anxiety, hunger, etc. These recordings are made in the moment and in the participant’s daily life, allowing for observing behaviors as they unfold in the real world, moment-by-moment, to capture dynamic changes in behavior over time and across contexts.24–28 This approach avoids the limitations and biases inherent in retrospective recall. For example, momentary mechanisms preceding food-related parent feeding practices such as stress or depressed mood can be identified by using EMA and then targeted in interventions or discussed with parents during well-child visits to help them manage these feelings to reduce harmful food-related parenting practices. In addition, we include parents from minority, low-income, and immigrant population households, which will allow for understanding how stress and depressed mood operate similarly or differently with regard to food-related parenting practices in diverse families.
The main hypothesis tested in the current study is: high parental stress and depressed mood experienced earlier in the day is associated with controlling parent feeding practices (ie, restriction, pressure-to-eat) and less healthful foods (ie, preprepared foods, fast food) being served at family meals the same evening. In addition, an exploratory hypothesis being tested is: associations found between stress, depressed mood, and parent food-related practices will be modified by race and/or ethnicity. Results from the current study will help inform future interventions regarding momentary influences of food-related parenting practices. For example, understanding whether momentary stress and/or depressed mood are associated with a parent being more likely to engage in controlling feeding practices or to serving unhealthy foods at dinner the same day may inform the development of interventions that can intervene in real time to help parents engage in healthful food-related parenting practices in the face of high stress or depressive mood.
Methods
Data for the current study are from Family Matters, a National Institutes of Health–funded study.29 Family Matters is a 5-year incremental (Phase I = 2014–2016; Phase II = 2017–2019), mixed-methods (eg, video-recorded tasks, EMA, interviews, surveys), longitudinal study designed to identify novel risk and protective factors for childhood obesity in the home environments of racially and/or ethnically diverse and primarily low-income children. Phase I included an in-depth, mixed-methods, cross-sectional examination of the family home environment of diverse families (n = 150). Phase II will be a longitudinal epidemiologic cohort study with diverse families (n = 1200).
Data in the current study are from Phase I of the Family Matters study. In Phase I, a mixed-methods analysis of the home environments of children ages 5 to 7 years from 6 racial and/or ethnic groups including African American, Hispanic/Latino, Hmong, American Indian, Somali, and white (n = 25 from each racial and/or ethnic group) was conducted to identify individual, dyadic, and familial risk and protective factors for childhood obesity. The University of Minnesota’s Institutional Review Board Human Subjects Committee approved all protocols used in both phases of the Family Matters study.
Recruitment and Eligibility Criteria
Eligible children (n = 150) and their families were recruited from the Minneapolis and St Paul, Minnesota areas between 2015 and 2016 via a letter sent to them by their family physician. Children were eligible to participate in the study if they were between the ages of 5 to 7 years, had a sibling between the ages of 2 to 12 years living in the same home, lived with their parent or primary guardian >50% of the time, shared at least 1 meal/day with the parent or primary guardian, and were from 1 of 6 racial and/or ethnic categories (African American, Hispanic/Latino, Hmong, American Indian, Somali, and white). The sample was intentionally stratified by race and/or ethnicity and weight status (overweight or obese = BMI ≥85th percentile; nonoverweight = BMI >5th percentile and <85th percentile) of the study child to identify potential weight- and/or race and/or ethnic-specific home environment factors related to obesity risk.
Procedures and Data Collection
A 10-day in-home observation was conducted with each family, including 2 in-home visits and an 8-day direct observational period in between home visits. The observational components included: (1) an interactive observational family task30,31 using a family board game with activities around family meal planning, meal preparation, and family physical activity to measure family functioning and parenting practices; (2) EMA24 surveys measuring parental stress, depressed mood, parent feeding practices, food preparation, parent modeling of eating and physical activity, and child dietary intake, physical activity, and sedentary behaviors; (3) child and parent accelerometry; (4) three 24-hour child dietary recalls; (5) a home food inventory; (6) built environment block audit; (7) objectively measured height and weight on all family members; (8) a parent-completed online survey; and (9) a parent interview. All study materials were translated into Spanish, Somali, and Hmong, and bilingual staff were available at all home visits, allowing families to participate in their preferred language. Because of the level of study involvement required, families were compensated with the iPad mini used to record EMA data (∼$300) and additional gift card opportunities (up to $100) if all elements of the study were completed (eg, 8 complete days of EMA, 3 complete dietary recalls, 4 complete days of accelerometry). This also increased the likelihood that the equipment was not misused or stolen.
The study sample included diverse families who were equally distributed across the 6 racial and/or ethnic groups recruited in the study (African American, Hispanic/Latino, Hmong, American Indian, Somali, white) (Table 1). Additionally, families were from low-income households, with 70% of families earning <$35 000 per year. The majority of participants were mothers (91%) who were ∼35 years old (mean = 34.5; SD = 7.1) with children aged 6 years (mean = 6.4; SD = 0.08). Over half of the mothers worked full- or part-time, and 61% had a high school diploma or less. Approximately half of the mothers were married, and 64% of households had 2 parents.
TABLE 1.
Family Matters Study Phase I Demographic Characteristics (N = 150)
| Participant Characteristics | Primary Caregiver (N = 150), n (%) | Child (N = 150), n (%) |
|---|---|---|
| Female sex | 137 (91) | 71 (47) |
| Age in years (SD) | 34.5 (7.1) | 6.4 (0.8) |
| Adult BMI (BMI percentile child) | 30.9 (7.2) | 75.9 (23.1) |
| Weight status | ||
| Nonoverweight | 35 (23) | 77 (51) |
| Overweight or obese | 115 (77) | 73 (49) |
| Race and/or ethnicity | ||
| Asian (Hmong) | 25 (17) | 25 (17) |
| Black or African American | 22 (15) | 25 (17) |
| Hispanic/Latino | 23 (15) | 25 (17) |
| American Indian or Alaskan native | 21 (14) | 25 (17) |
| Somali | 25 (17) | 25 (17) |
| White | 27 (18) | 25 (17) |
| Multiracial or other | 7 (5) | — |
| Household Characteristics | ||
| Household structure | ||
| 1 parent (no other adults) | 37 (25) | — |
| 1 parent (w/ other adults) | 18 (12) | — |
| 2 parents (no other adults) | 78 (52) | — |
| 2 parents (w/ other adults) | 17 (11) | — |
| Primary caregiver marital status | ||
| Married | 78 (51) | — |
| Committed dating relationship or engaged | 31 (21) | — |
| Casually dating | 2 (1) | — |
| Separated or divorced | 6 (4) | — |
| Widowed | 1 (1) | — |
| Single or never married | 31 (21) | — |
| Missing | 1 (1) | — |
| Educational attainment | ||
| Middle school or junior high | 15 (10) | — |
| Some high school | 17 (11) | — |
| High school or GED | 60 (40) | — |
| Vocational, technical, trade certificate program, or associate degree | 28 (18) | — |
| College degree (eg, bachelor, masters, or doctorate) | 25 (16) | — |
| Other | 4 (3) | — |
| Missing | 1 (1) | — |
| Primary caregiver work status | ||
| Working full-time | 63 (42) | — |
| Working part-time | 32 (21) | — |
| Stay-at-home caregiver | 25 (17) | — |
| Currently unemployed, seeking work | 18 (12) | — |
| Not working for pay (unable to work, retired, student, etc) | 11 (7) | — |
| Not applicable | 1 (1) | — |
| Household income | ||
| <$20 000 | 50 (33) | — |
| $20 000–$34 999 | 55 (37) | — |
| $35 000–$49 999 | 16 (11) | — |
| $50 000–$74 999 | 12 (8) | — |
| $75 000–$99 999 | 7 (5) | — |
| $100 000 or more | 9 (6) | — |
| Missing | 1 (1) | — |
| Household income source (all that apply) | ||
| Wages from self | 85 (57) | — |
| Wages from other guardian | 34 (23) | — |
| Another family member | 14 (10) | — |
| Unemployment compensation | 4 (3) | — |
| Worker’s compensation | 0 (0) | — |
| Social Security | 11 (7) | — |
| Public assistance (eg, MFIP) | 34 (23) | — |
| Alimony and/or child support | 17 (11) | — |
| Other sources | 21 (14) | — |
Percentages may not sum to exactly 100% because of rounding. GED, General Education Diploma; MFIP, Minnesota Family Investment Program; —, not applicable.
Measures
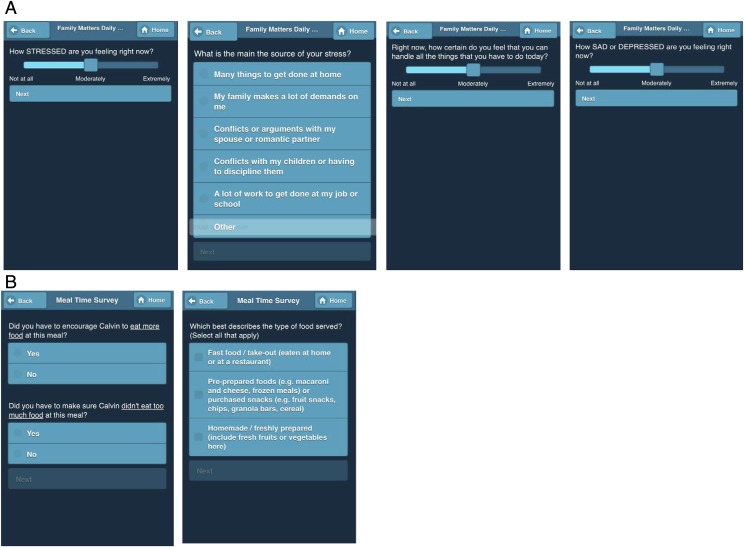
Multiple daily measures of EMA over 8 days were collected on parents. Standardized EMA data collection protocols from previous studies24 were used in the study including: (1) signal contingent, (2) event contingent, and (3) end-of-day EMA messaging.24 iPad minis were provided to parents to enter responses to the EMA surveys during the 8-day observation period. Screen shots of example EMA questions are shown in Fig 1.
FIGURE 1.
Screenshots of signal- and event-contingent EMA survey questions answered by Family Matters participants (names have been changed to protect confidentiality). A, Signal contingent questions. B, Event contingent questions.
Signal contingent recordings were researcher initiated and were used in a stratified random manner so that each parent was prompted via a text message to fill out a survey 4 times a day within a 3-hour time block (eg, 7–10 am, 11–2 pm, 3–6 pm, 7–10 pm). The surveys expired after 1 hour. The timing of EMA prompts was adjusted for parent shift work and wake times to accommodate parents’ differing life situations. The signal contingent recordings allowed for examining different contexts that occurred day-to-day, moment-by-moment, in families’ lives. Questions asked on the signal contingent surveys included parent modeling of eating, physical activity and sedentary behavior, parental stress levels and depressed mood, and parent feeding practices.
Event contingent recordings were self-initiated by parents whenever an eating occasion (ie, child and at least 1 other person were eating) occurred. In addition, the parent had to be present for the meal and indicate who was eating the meal together (eg, child, parent, sibling). Parents were asked to fill out information about the type of food served at the meal occasion, what the child actually ate, parent feeding practices, child eating behaviors, pickiness, meal atmosphere, food preparation and planning, and other meal logistics (eg, how long the meal lasted, where it occurred).
The end-of-day recording was completed before sleep to capture any events not reported since the last recording and to get end-of-day measures. All EMA responses were time-stamped. Participants were assigned additional days of EMA if several EMA prompts were missed within a day to obtain a minimum of 8 full days of EMA data with at least 4 complete EMA responses per day (ie, at least 2 signal contingent responses; at least 1 event contingent response; 1 end-of-day response).
All exposure (ie, parental stress, parental depressed mood) and outcome variables (types of food served at dinner, parent feeding practices) are presented in Table 2.
TABLE 2.
Exposure and Outcomes Variables Used in the Analysis
| Exposure Variables | |
| Parental stress | Parental stress was measured via signal contingent EMA surveys by using items adapted from the daily health diary.32 Parents were asked about their current level of stress (ie, how stressed are you feeling right now?), the main source of stress (ie, what is the main source of your stress?; response options, eg, a lot of work to get done at job or school, conflicts or arguments with my spouse or romantic partner), and their perceived ability to cope with stress32 (ie, right now, how certain do you feel that you can handle all the things that you have to do today?) since they woke up or since the last survey. EMA-reported stress before noon (ie, morning stress) was analyzed as a continuous random variable with Likert scale values ranging from 0 to 4 (0, “not at all”; 1, “a little”; 2, “moderately”; 3, “quite a bit”; 4, “extremely”). Multiple morning stress observations on signal contingent EMA surveys were averaged by participant and by observation day if the stress measure occurred before noon to ensure temporal ordering of the predictor variable. |
| Parent depressed mood | Parent depressed mood was measured during signal contingent EMA surveys by using an item adapted from Kessler-6 measure of depressive symptoms.33 Parents were asked about their current level of depressed mood (ie, how sad or depressed are you feeling right now?). EMA-reported depressed mood before noon (ie, morning stress) was also analyzed as a continuous random variable with Likert scale values ranging from 0 to 4 (0, “not at all”; 1, “a little”; 2, “moderately”; 3, “quite a bit”; 4, “extremely”). Temporal ordering was handled for morning depressive symptoms in the same way as the morning stress measure. |
| Outcome Variables | |
| Parent feeding practices | Parent restriction and pressure-to-eat parent feeding practices were measured during event contingent (ie, meal occasions) EMA surveys by using 2 items modeled after the child feeding questionnaire.34 Parent restriction (ie, did you have to make sure [child’s name] didn’t eat too much food at this meal?) and pressure-to-eat (ie, did you have to encourage [child’s name] to eat more food at this meal?) feeding practices at meal occasions were measured as a dichotomous variable (0, “no”; 1, “yes”). Dinner and snacking event contingent meal occasions occurring at 4 pm or later were included for analysis (ie, breakfast and lunch meal occasions were excluded to avoid reverse causation). Evening feeding practices were averaged at the participant and observation day level and treated as a binomial outcome variable ranging between 0 and 1 in all quantitative analyses. If a participant reported pressuring feeding practices at 2 of 3 meal occasions, the binomial outcome variable at the day level would be equal to 0.667 (ie, 2 meal occasions in which the feeding practice was observed divided by the 3 total meals occurring that day after 4 pm at dinner or snacking occasions). |
| Type of foods served at meals | The type of foods served at meals was assessed during event contingent EMA surveys (ie, which best describes the type of food served at the meal?), adapted from previous survey research questions. Response options included: homemade, preprepared or fast food. Parents could report multiple types of foods served at any one meal occasion.4,35 The proportion of evening meal occasions (at the participant, observation day level) in which the food type was present was operationalized as a binomial outcome variable in the same way as the parent feeding practices variable (ie, range 0–1). Like the example provided above, if the daily proportion of fast food at evening dinner and snacking meal occasions was equal to 0.667, then two-thirds of 1 day’s evening meal occasions had fast food item present. Parents could report multiple types of foods served at any 1 meal occasion. Lunch meals were excluded to ensure temporal ordering of early parental stress and later-day parent feeding practices and type of foods served at meals. |
Statistical Analysis
Descriptive and inferential statistics were used to examine how morning stress and depressed mood related to evening feeding practices and separately to the daily composition of food types (homemade, preprepared, and fast food) served at evening dinner and snacking meal occasions. The 2 predictor variables (stress and depressive symptoms before noon) were analyzed as continuous random variables. The outcome variables (evening feeding practices and proportion of food types present at those meal occasions) were evaluated with generalized estimating equations with a binomial variance family and logistic link and with Gaussian variance family and identity link respectively. Robust SEs were used and the covariance structure was initially set to independent. These analyses were performed for the full sample, and separately for each of the 6 race and/or ethnic groups to evaluate differences in subpopulation response to level of stress or mood (ie, effect moderation). All models were adjusted for family level race (regardless of whether the observation day occurred on a weekday or weekend) and the primary caregiver’s and child’s age, sex, and weight status and/or BMI. All analyses were performed in Stata 13.1SE (StataCorp, College Station, TX).
Results
Stress and Depressed Mood Levels
Overall, population average stress (0.67 ± 0.95) and depressed mood (0.45 ± 0.85) were low in this sample. Average stress levels were highest among African Americans (0.91 ± 1.1), whites (0.79 ± 0.80), and Hispanics/Latinos (0.68 ± 1.0) and lowest among American Indians (0.48 ± 0.90), Somalis (0.55 ± 0.85), and Hmong (0.61 ± 0.92) participants. Depressed mood showed some similar and some different subpopulation patterns. African Americans (0.65 ± 1.0), Somalis (0.55 ± 0.90), and Hmong (0.48 ± 0.80) had a higher average level of depressed mood, whereas whites (0.29 ± 0.46), American Indians (0.36 ± 0.85), and Hispanics/Latinos (0.42 ± 0.95) reported lower levels of depressed mood. African Americans reported the most stressed and depressed mood and American Indians reported the lowest stress and second lowest depressed mood relative to the rest of the sample.
Parent Feeding Practices
With regard to parent feeding practices, a 1-unit increase in stress earlier in the day was associated with 45% greater odds of parents engaging in pressure-to-eat feeding practices at dinner the same night, after controlling for sociodemographics, weight status, and weekday or weekend observation (Table 3). Additionally, a 1-unit increase in depressed mood earlier in the day was associated with 42% greater odds of parents engaging in pressure-to-eat parent feeding practices at dinner the same night (Table 3). There were no significant associations found between parental stress, depressed mood, and parent food restriction.
TABLE 3.
Bivariate and Adjusted Associations Between Morning Stress and Mood Levels With Evening Food Pressuring and Restrictive Feeding Practices (N = 150 Caregivers; N = 1044 Meal Occasions)
| Independent Predictor: Stress | OR | 95% CI | P | Independent Predictor: Mood | OR | 95% CI | P |
|---|---|---|---|---|---|---|---|
| Full sample adjusted analyses | |||||||
| Pressure to eat | 1.45 | (1.08 to 1.94) | .013* | Pressure to eat | 1.42 | (1.01 to 1.99) | .043* |
| Restriction | 1.26 | (0.96 to 1.64) | .091 | Restriction | 1.24 | (0.96 to 1.58) | .096 |
| Stratified by race and/or ethnicity | |||||||
| African American (N = 25, N = 170 meals) | African American (N = 25, N = 170 meals) | ||||||
| Pressure to eat | 1.46 | (0.45 to 4.74) | .531 | Pressure to eat | 1.05 | (0.51 to 2.14) | .894 |
| Restriction | 1.02 | (0.56 to 1.84) | .951 | Restriction | 1.04 | (0.56 to 1.93) | .892 |
| White (N = 25, N = 182 meals) | White (N = 25, N = 182 meals) | ||||||
| Pressure to eat | 0.90 | (0.56 to 1.44) | .661 | Pressure to eat | 0.49 | (0.19 to 1.26) | .140 |
| Restriction | 0.47 | (0.19 to 1.16) | .100 | Restriction | 0.81 | (0.16 to 4.21) | .807 |
| Hmong (N = 25, N = 185 meals) | Hmong (N = 25, N = 185 meals) | ||||||
| Pressure to eat | 1.14 | (0.67 to 1.95) | .633 | Pressure to eat | 1.09 | (0.55 to 2.13) | .811 |
| Restriction | 1.42 | (0.78 to 2.60) | .253 | Restriction | 1.27 | (0.70 to 2.31) | .438 |
| Hispanic/Latino (N = 25, N = 178 meals) | Hispanic/Latino (N = 25, N = 178 meals) | ||||||
| Pressure to eat | 1.12 | (0.76 to 1.63) | .566 | Pressure to eat | 1.09 | (0.61 to 1.97) | .764 |
| Restriction | 0.97 | (0.60 to 1.56) | .888 | Restriction | 0.97 | (0.48 to 1.94) | .925 |
| American Indian (N = 25, N = 162 meals) | American Indian (N = 25, N = 162 meals) | ||||||
| Pressure to eat | 2.64 | (1.49 to 4.67) | .001* | Pressure to eat | 2.40 | (1.29 to 4.49) | .006* |
| Restriction | 1.19 | (0.61 to 2.32) | .614 | Restriction | 1.24 | (0.76 to 2.00) | .390 |
| Somali (N = 25, N = 167 meals) | Somali (N = 25, N = 167 meals) | ||||||
| Pressure to eat | 2.02 | (1.05 to 3.91) | .036* | Pressure to eat | 1.55 | (0.79 to 3.02) | .203 |
| Restriction | 1.49 | (0.80 to 2.77) | .210 | Restriction | 1.06 | (0.63 to 1.80) | .819 |
Adjusted models include covariates: primary caregiver and/or child age, sex, and weight status; family race; weekend or weekday observation. Interpretation example: a 1-unit increase in morning stress was associated with 45% greater odds of pressure-to-eat feeding practices (OR: 1.45, 95% CI: 1.08 to 1.94, P = .013) the same night at dinner, after controlling for all other covariates in the adjusted models. Effect modification interpretation: the relationship between stress and pressure-to-eat feeding practices was strongest for American Indian caregivers (OR: 2.64, 95% CI: 1.49 to 4.67, P = .001) and for Somali caregivers (OR: 2.02, 95% CI: 1.05 to 3.91, P = .36).
P < .05.
Effect modification results indicated that the relationship between parental stress, depressed mood, and pressure-to-eat feeding practices was strongest for American Indian parents (odds ratio [OR]: 2.64, 95% confidence interval [CI]: 1.49 to 4.67, P = .001) and for Somali parents (OR: 2.02, 95% CI: 1.05 to 3.91, P = .036; Table 3).
Foods Served at Family Meals
With regard to types of foods served at dinner, a 1-unit increase in stress earlier in the day was associated with a decrease in the proportion of dinner meals in which homemade foods were served (mean response: −0.05, 95% CI: −0.08 to −0.01, P = .008), after controlling for sociodemographics, BMI, and weekday or weekend observation (Table 4). In addition, a 1-unit increase in depressed mood earlier in the day was negatively associated with serving homemade foods (mean response: −0.06, 95% CI: −0.09 to −0.02, P = .004) and positively associated with serving preprepared foods (mean response: 0.05, 95% CI: 0.01 to 0.08, P = .025) at dinner the same night (Table 4).
TABLE 4.
Adjusted Associations of Morning Stress and Mood on the Proportion of Food Categories Served at Snack and Dinner Evening Meal Occasions
| Independent Predictor: Stress | Mean | 95% CI | P | Independent Predictor: Mood | Mean | 95% CI | P |
|---|---|---|---|---|---|---|---|
| Full sample adjusted analyses | |||||||
| Fast food | 0.01 | (−0.01 to 0.03) | .149 | Fast food | 0.00 | (–0.02 to 0.02) | .967 |
| Preprepared foods | 0.02 | (−0.01 to 0.06) | .182 | Preprepared foods | 0.05 | (0.01 to 0.08) | .025* |
| Homemade foods | –0.05 | (−0.08 to −0.01) | .008* | Homemade foods | −0.06 | (–0.09 to –0.02) | .004* |
| Stratified by race and/or ethnicity | |||||||
| African American | African American | ||||||
| Fast food | 0.04 | (−0.01 to 0.08) | .116 | Fast food | −0.02 | (−0.08 to 0.04) | .485 |
| Preprepared foods | 0.03 | (−0.04 to 0.11) | .389 | Preprepared foods | 0.10 | (0.03 to 0.17) | .008* |
| Homemade foods | –0.10 | (−0.16 to −0.04) | .001* | Homemade foods | −0.09 | (−0.16 to −0.02) | .008* |
| White | White | ||||||
| Fast food | 0.01 | (−0.02 to 0.04) | .509 | Fast food | 0.03 | (−0.05 to 0.11) | .466 |
| Preprepared foods | 0.03 | (−0.04 to 0.09) | .427 | Preprepared foods | −0.02 | (−0.13 to 0.09) | .755 |
| Homemade foods | –0.02 | (−0.09 to 0.05) | .555 | Homemade foods | 0.00 | (−0.14 to 0.14) | .967 |
| Hmong | Hmong | ||||||
| Fast food | –0.01 | (−0.03 to 0.01) | .319 | Fast food | −0.02 | (−0.05 to 0.00) | .080 |
| Preprepared foods | 0.04 | (−0.03 to 0.10) | .270 | Preprepared foods | 0.04 | (−0.04 to 0.13) | .296 |
| Homemade foods | –0.02 | (−0.09 to 0.05) | .527 | Homemade foods | −0.02 | (−0.11 to 0.07) | .682 |
| Hispanic/Latino | Hispanic/Latino | ||||||
| Fast food | 0.00 | (−0.04 to 0.04) | .897 | Fast food | −0.01 | (–0.04 to 0.02) | .522 |
| Preprepared foods | 0.05 | (−0.04 to 0.14) | .306 | Preprepared foods | 0.12 | (0.04 to 0.20) | .003* |
| Homemade foods | –0.07 | (−0.17 to 0.03) | .161 | Homemade foods | −0.12 | (−0.19 to −0.06) | <.001* |
| American Indian | American Indian | ||||||
| Fast food | –0.04 | (−0.07 to 0.00) | .038* | Fast food | −0.01 | (−0.06 to 0.04) | .655 |
| Preprepared foods | 0.07 | (0.00 to 0.14) | .053 | Preprepared foods | 0.04 | (−0.04 to 0.12) | .344 |
| Homemade foods | –0.04 | (−0.11 to 0.02) | .223 | Homemade foods | −0.05 | (−0.12 to 0.02) | .164 |
| Somali | Somali | ||||||
| Fast food | 0.07 | (−0.01 to 0.15) | .069 | Fast food | 0.04 | (−0.03 to 0.12) | .254 |
| Preprepared foods | –0.04 | (−0.14 to 0.05) | .342 | Preprepared foods | −0.02 | (−0.11 to 0.06) | .631 |
| Homemade foods | –0.03 | (−0.11 to 0.04) | .381 | Homemade foods | −0.02 | (−0.09 to 0.05) | .572 |
Adjusted models include covariates: primary caregiver age and BMI, family race, weekend or weekday observation. Interpretation example: a 1-unit increase in depressed mood earlier in the day was negatively associated with serving homemade foods (mean response: −0.06, 95% CI: −0.09 to −0.02, P = .004) but was positively associated with serving preprepared foods the same night at dinner (mean response: 0.05, 95% CI: 0.01 to 0.08, P = .025), after controlling for all other covariates in the adjusted models. Effect modification interpretation example: in the African American subpopulation analysis, a 1-unit increase in stress levels earlier in the day was negatively associated with serving homemade foods the same night at dinner (mean response: −0.10, 95% CI: −0.16 to −0.04, P = .001).
P < .05.
Effect modification results indicated that the relationship between parental stress, depressed mood, and the proportion of dinner meals with homemade food was strongest for African American parents and Hispanic/Latino parents. For example, a 1-unit increase in stress earlier in the day was negatively associated with serving homemade foods at dinner meals (mean response: −0.10, 95% CI: −0.16 to −0.04, P = .001) and a 1-unit increase in depressed mood earlier in the day was negatively associated with serving homemade food at dinner (mean response: −0.09, 95% CI: −0.16 to −0.02, P = .008) and positively associated with serving preprepared foods at dinner (mean response: 0.10, 95% CI: 0.03 to 0.17, P = .008) for African American parents (Table 4).
Discussion
Overall, the results of the current study indicated that parental stress and depressed mood experienced earlier in the day were associated with food-related parenting practices at dinner the same night, with some exceptions. The results of the current study both confirm and extend previous research. The findings in the current study related to parental depressed mood support previous studies revealing that maternal depressed mood is associated with parent pressure-to-eat feeding practices.20 Findings related to stress extend previous studies in the field whose results reveal that stress earlier in the day is associated with parent engagement in pressure-to-eat feeding practices the same night but not parent restriction. One potential explanation of this finding is that restriction of foods may require more parental energy to engage in than pressure-to-eat; thus, a parent who is experiencing stress or depressive symptoms may not engage in restriction as readily as pressure-to-eat feeding practices. Additionally, results indicate that certain populations (ie, American Indian, Somali) are at higher risk of engaging in pressure-to-eat feeding practices when experiencing high stress levels or depressed mood.
Results of the current study also extend previous research by showing that high parental stress and depressed mood experienced earlier in the day are associated with a lower prevalence of homemade foods being served at dinner meals and a higher prevalence of preprepared foods being served at dinner meals the same night. Additionally, results reveal that certain racial and/or ethnic groups (ie, African American, Hispanic/Latino) are at higher risk of serving less homemade food when experiencing high levels of stress or depressive symptoms.
Results from the current study may inform future research and recommendations for health care clinicians that work with children and families. For example, future intervention researchers may want to consider using momentary intervention techniques such as ecological momentary intervention methods to intervene in real time with parents to help them engage in healthful food-related parenting practices in the face of high stress or depressed mood. Additionally, intervention researchers may want to consider tailoring interventions with specific populations (ie, African American, Hispanic/Latino, American Indian, Somali) to address stress and depressed mood to increase healthful food-related parenting practices.
In addition, results from the current study may be used by health care clinicians to identify specific groups of children who may be at higher risk of experiencing pressure-to-eat feeding practices or for being served less healthy foods at dinner. For example, in many primary care clinics, parents are screened for depressed mood. When parents report high levels of depressed mood, health care clinicians may want to educate parents and/or provide resources for parents regarding food-related parenting practices in the face of high stress and/or depressed mood. Furthermore, health care clinicians may want to consider educating parents during well-child visits regarding the momentary influences that stress and depressed mood can have on behaviors such as what types of food one serves at dinner or parent feeding practices. Many parents may be unaware that their stress levels or depressed mood could influence what they serve their child for dinner or their own parent feeding practices.
There were both strengths and limitations of the current study. Strengths of the current study include the use of EMA to measure behaviors at multiple time points within and across days over an 8-day period. Additionally, EMA was used to measure both exposure (ie, parental stress and depressed mood) and outcome variables (parent feeding practices, types of food served at meals) across time and context. Furthermore, the sample included racially and/or ethnically and socioeconomically diverse participants as well as immigrant populations. There were also limitations of the current study; 1 includes the use of items from scales that have not been used with EMA or immigrant populations. Additionally, although the overall sample size was relatively small (n = 150), this study was a mixed-methods study that allowed for in-depth measurements of family behaviors that would not have been feasible with a larger sample size. Additionally, because EMA was conducted over an 8-day period, with 4 surveys each day, there are over 1000 data points, which increases the precision of our analyses.
Conclusions
Results of the current study indicated that high levels of parental stress and depressed mood earlier in the day predicted pressure-to-eat feeding practices, less homemade food, and more preprepared foods at meals the same night. Additionally, these findings were stronger for some racial and/or ethnic groups. Recommendations for future research include developing interventions using ecological momentary intervention to target momentary factors in real time that influence food-related feeding practices such as stress and depressed mood to promote healthful food-related parenting practices. Health care providers may also want to use study findings to guide their anticipatory guidance with parents during well-child visits regarding the influence that stress and depressed mood can have on everyday food-related parenting practices. In addition, given the study findings, these messages may need to be tailored to specific groups (eg, African American, Hispanic/Latino, American Indian, Somali).
Glossary
- CI
confidence interval
- EMA
ecological momentary assessment
- OR
odds ratio
Footnotes
Dr Berge is the principal investigator on the grant and conceptualized the manuscript, assisted with data analysis and interpretation, and wrote all drafts of the manuscript; Mr Tate conducted the data analysis and critically reviewed the manuscript; Ms Trofholz assisted with data acquisition and interpretation of the data and critically reviewed the manuscript; Dr Fertig assisted with the conceptualization of the manuscript and the data analysis and critically reviewed the manuscript; Dr Miner assisted with the data analysis of the manuscript and critically reviewed the manuscript; Dr Crow assisted with the conceptualization of the manuscript and critically reviewed the manuscript; Dr Neumark-Sztainer assisted in conceptualizing the manuscript, contributed to the design of the study, and critically reviewed the manuscript; and all authors gave final approval of this version to be published and agree to be accountable for all aspects of the work regarding the accuracy or integrity of any part of the work.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grant R01HL126171 from the National Heart, Lung, and Blood Institute (principal investigator: Dr Berge). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Larson N, Eisenberg ME, Berge JM, Arcan C, Neumark-Sztainer D. Ethnic/racial disparities in adolescents’ home food environments and linkages to dietary intake and weight status. Eat Behav. 2015;16:43–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Loth KA, MacLehose RF, Larson N, Berge JM, Neumark-Sztainer D. Food availability, modeling and restriction: how are these different aspects of the family eating environment related to adolescent dietary intake? Appetite. 2016;96:80–86 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cullen KW, Baranowski T, Owens E, Marsh T, Rittenberry L, de Moor C. Availability, accessibility, and preferences for fruit, 100% fruit juice, and vegetables influence children’s dietary behavior. Health Education Behav. 2003;30(5):615–626 [DOI] [PubMed] [Google Scholar]
- 4.Neumark-Sztainer D, MacLehose R, Loth K, Fulkerson JA, Eisenberg ME, Berge J. What’s for dinner? Types of food served at family dinner differ across parent and family characteristics. Public Health Nutr. 2014;17(1):145–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Trofholz AC, Tate AD, Draxten ML, et al. . What’s being served for dinner? An exploratory investigation of the associations between the healthfulness of family meals and child dietary intake. J Acad Nutr Diet. 2017;117(1):102–109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Food-related parenting practices and adolescent weight status: a population-based study. Pediatrics. 2013;131(5). Available at: www.pediatrics.org/cgi/content/full/131/5/e1443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Birch LL, Fisher JO. Mothers’ child-feeding practices influence daughters’ eating and weight. Am J Clin Nutr. 2000;71(5):1054–1061 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Birch LL, Davison KK. Family environmental factors influencing the developing behavioral controls of food intake and childhood overweight. Pediatr Clin North Am. 2001;48(4):893–907 [DOI] [PubMed] [Google Scholar]
- 9.Fisher JO, Mitchell DC, Smiciklas-Wright H, Birch LL. Parental influences on young girls’ fruit and vegetable, micronutrient, and fat intakes. J Am Diet Assoc. 2002;102(1):58–64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Birch LL, Fisher JO, Davison KK. Learning to overeat: maternal use of restrictive feeding practices promotes girls’ eating in the absence of hunger. Am J Clin Nutr. 2003;78(2):215–220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fisher JO, Birch LL. Restricting access to palatable foods affects children’s behavioral response, food selection, and intake. Am J Clin Nutr. 1999;69(6):1264–1272 [DOI] [PubMed] [Google Scholar]
- 12.Loth KA, MacLehose RF, Fulkerson JA, Crow S, Neumark-Sztainer D. Are food restriction and pressure-to-eat parenting practices associated with adolescent disordered eating behaviors? Int J Eat Disord. 2014;47(3):310–314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Devine CM, Connors MM, Sobal J, Bisogni CA. Sandwiching it in: spillover of work onto food choices and family roles in low- and moderate-income urban households. Soc Sci Med. 2003;56(3):617–630 [DOI] [PubMed] [Google Scholar]
- 14.Wardle J, Steptoe A, Oliver G, Lipsey Z. Stress, dietary restraint and food intake. J Psychosom Res. 2000;48(2):195–202 [DOI] [PubMed] [Google Scholar]
- 15.Arnow B, Kenardy J, Agras WS. The Emotional Eating Scale: the development of a measure to assess coping with negative affect by eating. Int J Eat Disord. 1995;18(1):79–90 [DOI] [PubMed] [Google Scholar]
- 16.Loth K, van den Berg P, Eisenberg ME, Neumark-Sztainer D. Stressful life events and disordered eating behaviors: findings from Project EAT. J Adolesc Health. 2008;43(5):514–516 [DOI] [PubMed] [Google Scholar]
- 17.Lattimore PJ. Stress-induced eating: an alternative method for inducing ego-threatening stress. Appetite. 2001;36(2):187–188 [DOI] [PubMed] [Google Scholar]
- 18.Castillo F, Francis L, Wylie-Rosett J, Isasi CR. Depressive symptoms are associated with excess weight and unhealthier lifestyle behaviors in urban adolescents. Child Obes. 2014;10(5):400–407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.El-Behadli AF, Sharp C, Hughes SO, Obasi EM, Nicklas TA. Maternal depression, stress and feeding styles: towards a framework for theory and research in child obesity. Br J Nutr. 2015;113(suppl):S55–S71 [DOI] [PubMed] [Google Scholar]
- 20.Goulding AN, Rosenblum KL, Miller AL, et al. . Associations between maternal depressive symptoms and child feeding practices in a cross-sectional study of low-income mothers and their young children. Int J Behav Nutr Phys Act. 2014;11:75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of obesity and trends in body mass index among US children and adolescents, 1999-2010. JAMA. 2012;307(5):483–490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ogden CL, Carroll MD, Lawman HG, et al. . Trends in obesity prevalence among children and adolescents in the United States, 1988-1994 through 2013-2014. JAMA. 2016;315(21):2292–2299 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shiffman S, Stone AA, Hufford MR. Ecological momentary assessment. Annu Rev Clin Psychol. 2008;4:1–32 [DOI] [PubMed] [Google Scholar]
- 25.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol. 2010;15(pt 1):1–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Dunton GF, Intille SS, Wolch J, Pentz MA. Children’s perceptions of physical activity environments captured through ecological momentary assessment: a validation study. Prev Med. 2012;55(2):119–121 [DOI] [PubMed] [Google Scholar]
- 27.Dunton GF, Liao Y, Intille SS, Spruijt-Metz D, Pentz M. Investigating children’s physical activity and sedentary behavior using ecological momentary assessment with mobile phones. Obesity (Silver Spring). 2011;19(6):1205–1212 [DOI] [PubMed] [Google Scholar]
- 28.De Young KP, Lavender JM, Crosby RD, et al. . Bidirectional associations between binge eating and restriction in anorexia nervosa. An ecological momentary assessment study. Appetite. 2014;83:69–74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berge JM, Trofholz A, Tate AD, et al. . Examining unanswered questions about the home environment and childhood obesity disparities using an incremental, mixed-methods, longitudinal study design: the Family Matters study. Contemp Clin Trials. 2017;62:61–76 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Melby JN, Conger RD. The Iowa family interaction rating scales: instrument summary In: Kerig PK, Lindahl KM, eds. Family Observational Coding Systems: Resources for Systemic Research. Mahway, NJ: Lawrence Ehrlbaum Associates; 2001:33–58 [Google Scholar]
- 31.Berge JM, Mendenhall TJ, Doherty WJ. Using Community-based Participatory Research (CBPR) to target health disparities in families. Fam Relat. 2009;58(4):475–488 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dunton GF, Liao Y, Dzubur E, et al. . Investigating within-day and longitudinal effects of maternal stress on children’s physical activity, dietary intake, and body composition: protocol for the MATCH study. Contemp Clin Trials. 2015;43:142–154 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kessler RC, Green JG, Gruber MJ, et al. . Screening for serious mental illness in the general population with the K6 screening scale: results from the WHO World Mental Health (WMH) survey initiative. Int J Methods Psychiatr Res. 2010;19(suppl 1):4–22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Birch LL, Fisher JO, Grimm-Thomas K, Markey CN, Sawyer R, Johnson SL. Confirmatory factor analysis of the child feeding questionnaire: a measure of parental attitudes, beliefs and practices about child feeding and obesity proneness. Appetite. 2001;36(3):201–210 [DOI] [PubMed] [Google Scholar]
- 35.Boutelle KN, Fulkerson JA, Neumark-Sztainer D, Story M, French SA. Fast food for family meals: relationships with parent and adolescent food intake, home food availability and weight status. Public Health Nutr. 2007;10(1):16–23 [DOI] [PubMed] [Google Scholar]