This study examines the utility of various growth charts, including a new modified CDC BMI z score chart, in tracking children with normal and problematic growth.
Abstract
OBJECTIVES:
To illustrate the difficulties in optimal growth monitoring of children with severe obesity or underweight by using the Centers for Disease Control and Prevention (CDC) 2000 age- and sex-specific BMI percentile growth charts. We also aimed to examine the utility of a new modified CDC BMI z score chart to monitor growth in children with normal and extreme BMI percentiles by using real-life clinical scenarios.
METHODS:
Modified BMI z score charts were created by using the 2000 CDC algorithm. Three cases of children with extreme BMI values and abnormal growth patterns were plotted by using the standard CDC 2000 clinical growth chart, the modified BMI z score chart, and the CDC BMI percentile chart, modified to include the percentage of the 95th percentile (%BMIp95) curves.
RESULTS:
Children with severe obesity could not be plotted on the standard CDC BMI percentile chart because their BMI points lay above the chart cutoff. Children with a low BMI (<3%) were also difficult to track on the standard BMI percentile chart. The addition of the %BMIp95 scale to the standard BMI percentile chart allowed tracking of severely obese children; however, it did not address severely underweight children and required a change of units within the chart when transitioning from normal to obese BMIs. The modified BMI z score chart allowed uniform tracking.
CONCLUSIONS:
The modified CDC z score chart is suitable for growth tracking of children with normal and extreme growth patterns; the measures correlate well with the %BMIp95, and the chart can be incorporated easily into existing electronic health record systems for clinical use.
What’s Known on This Subject:
With the increasing prevalence of childhood obesity, optimal methods for growth tracking are needed. The Centers for Disease Control (CDC) 2000 age- and sex-specific BMI percentile growth charts currently in use are inadequate for growth monitoring at extremes of BMI percentiles.
What This Study Adds:
Growth in children with normal and problematic growth was tracked by using CDC 2000 BMI growth charts, charts with additional curves depicting percent of the 95th percentile, and our proposed modified CDC BMI z score charts.
The global epidemic of childhood obesity is worsening. An estimated 41 million children worldwide under the age of 5 are either overweight or obese.1 In the United States, the prevalence of obesity among children and adolescents 2 to 19 years of age has stabilized over the past decade but remains high at ∼17%.2 More concerning is the increasing trend in severe obesity, especially among older children.3 This epidemic, combined with the existing challenge of tracking growth progress in underweight children, has presented a new predicament for clinicians as they struggle to identify an easy and meaningful method to monitor growth and interventions.
In 2000, the Centers for Disease Control and Prevention (CDC) published age- and sex-specific growth charts that are currently used by pediatric care providers in the United States for assessment of growth and nutritional status in children and adolescents 2 to 19 years of age.4 A serious limitation of these growth charts, however, is the inability to assess and track growth in children with very high BMI as well as children with very low BMI.5,6 The basic problem is that the standard z scores and percentiles based on age and sex are severely compressed at high BMI levels, so that very high or very low values are not well quantified, causing a relatively large change in BMI results from only a small change in BMI percentile or z score.6–8 Alternative charts have been proposed recently, including those using a percentage of the smoothed 95th BMI percentile (%BMIp95) for obese children.5
Z scores identify the distance and direction of deviation from the mean, and z scores are a standardized quantity reflecting the reference population that can be compared across age, sex, and anthropometric measures.9 The World Health Organization (WHO) has BMI-for-age z score charts for clinical use, wherein overweight is defined as a z score >2 SD and obesity is defined as a z score >3 SD above the mean.10 Conversely, BMIs-for-age < −2 SD and < −3 SD below the mean on the WHO charts are considered wasted and severely wasted, respectively.10,11 Currently, the CDC has not published z score charts for clinical growth tracking in children in the United States. However, age- and sex-specific BMI z scores can be calculated from the skewness, median, and coefficient of variation values provided by the CDC, which are derived from the smoothed percentile curves of the 2000 CDC growth charts.12
The age- and sex-specific BMI z score, or CDC BMI unmodified z score (BMIz), which is frequently used in research and current clinical practice, is inadequate for longitudinal growth tracking, especially among severely obese children.13 To address this problem, the CDC now provides “modified z scores” that are based on a fixed SD and are not bounded by upper or lower limits.14 Freedman and Berenson15 recently compared longitudinal tracking of multiple BMI metrics by using data from the Bogalusa Heart Study cohort; the authors found the tracking of BMI z scores to be weaker compared with that of %BMIp95 and adjusted (modified) BMI z scores especially among children with high BMI values.
Considering these latest research findings, we propose a uniform modified BMI z score chart that could be used to track BMI in all categories of growth, from severe underweight to severe obesity, without changing units or adding clinical complexity. These modified BMI z score charts could be easily integrated into existing electronic health record systems and would be ideal for both primary care and pediatric subspecialty use.
The objectives of this study are as follows: (1) to describe methods used to construct BMI-for-age z score growth charts by using the modified z score software program provided by the CDC, which allows for quantifying extreme BMI values; (2) to describe methods to construct 2000 CDC BMI-for-age–based percentile charts by inclusion of additional curves depicting %BMIp95; and (3) to present actual clinical case scenarios of children with growth problems and plot BMI-for-age by using 2000 CDC BMI-for-age percentile charts that are currently in clinical use, the 2000 CDC charts with the addition of %BMIp95 growth lines for characterizing growth in children with BMI percentiles in the upper extremes, and our proposed modified BMI z score charts.
Methods
The growth charts proposed by Gulati et al5 that allow for tracking of severe obesity (BMI >36) were created by using the 2000 CDC growth chart as the base, with the addition of new percentile curves above the 95th percentile. These new percentile curves were calculated by multiplying the age- and sex-specific BMI at the 95th percentile by values from 1.1 through 2.0 to derive the 110% to 200% BMIp95.
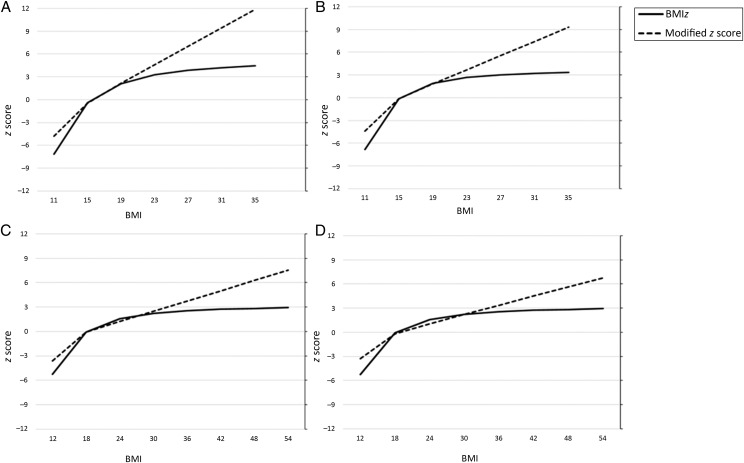
We created the age- and sex-specific modified BMI z score charts by using the statistical program provided by CDC.16,17 The modified BMI z scores are based on extrapolating one-half of the distance between 0 and +2 z scores.14 To further illustrate the difference in how BMI is represented on a plot using BMIz and modified BMI z score methods, we plotted different BMI values less than and greater than the median in a hypothetical girl and boy of 5.5 and 12.5 years of age, respectively (Fig 1). It is evident from this figure that the BMIz curve plateaus at the upper extreme and is exaggerated at the lower extreme, whereas the modified BMI z curve shows a linear distribution at both extremes. In the middle range of BMI representing most normal weight children, the BMIz and modified BMI z are nearly identical.
FIGURE 1.
BMI tracking of children by using BMIz and modified BMI z score methods for (A) a 5.5-year-old boy, (B) a 5.5-year-old old girl, (C) a 12.5-year-old boy, and (D) a 12.5-year-old girl.
Clinical Scenarios Plotted by Using Different Growth Charts
To illustrate the differences in growth trends among children with problematic growth patterns involving both severe underweight and severe obesity, we selected 3 clinical cases from a pediatric endocrinology clinic at a children’s hospital and plotted changes in BMI using all 3 growth charts. Two of the 3 children had excessive weight, and the third was an underweight child.
The institutional review board at Phoenix Children’s Hospital granted a waiver of informed consent for this study.
Results
Case 1
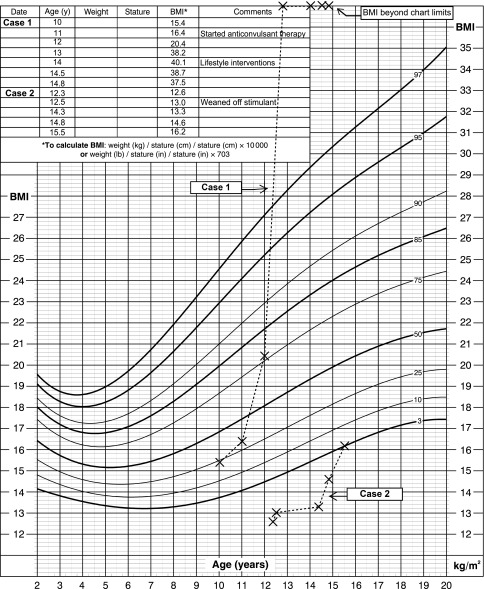
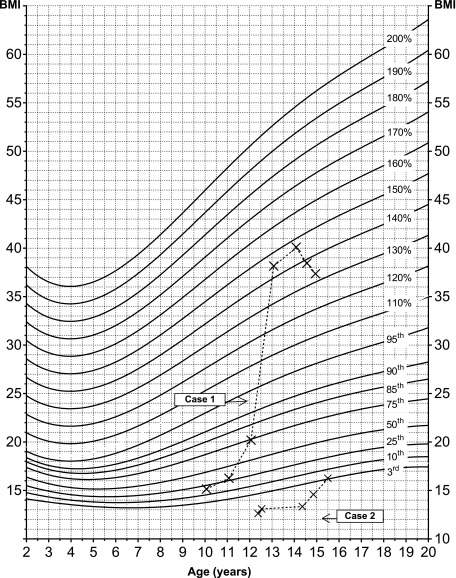
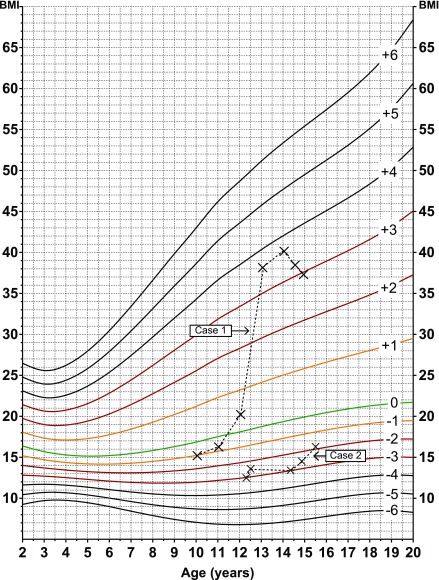
A 13-year-old girl was referred to the pediatric endocrine specialty clinic for evaluation and management of excessive weight gain. She developed rapid weight gain after starting anticonvulsant medications at age 11 years. At age 13.5 years, intensive lifestyle interventions were initiated, which resulted in a downward tracking of her weight. In Fig 2, her BMI at yearly visits from ages 10 to 14 years and at 2 additional visits between ages 14 to 15 years was plotted by using the 2000 CDC BMI-for-age percentile chart for girls. In Figs 3 and 4, the plot was illustrated by using an age- and sex-specific 2000 CDC percentile chart with %BMIp95 and the modified BM z score chart. With either of these charts, more extreme BMIs can be tracked, although the modified BMI z score chart uses a uniform unit of measurement and provides more continuous tracking. By using the modified BMI z score chart (Fig 4), it is possible to see that the patient started in the normal weight category at a z score slightly > −1 at age 10 years. Her BMI increased dramatically within 4 years, and peaked at > +3 SD by age 14, before beginning a downtrend to a z score of +3 SD. This change is also illustrated in the %BMIp95 chart, which reveals that her BMI peaked at ∼130% of the 95th percentile (Fig 3) before she began a downtrend, remaining >120% of the 95th percentile for her age and sex. When she transitioned from normal weight into the obesity category, the quantitative measure changed from percentile to percent of the 95th percentile.
FIGURE 2.
Two to 20 years: female patients. BMI-for-age percentiles. The BMI of a female patient (Case 1) who transitioned from having normal weight to having severe obesity between the ages of 10 to 14 years was plotted by using the CDC 2000 BMI-for-age-sex growth chart, and the BMI of a female patient (Case 2) with underweight problems was plotted by using the CDC 2000 BMI-for-age-sex growth chart. Source: developed by the National Center for Health Statistics in collaboration with the National Center for Chronic Disease Prevention and Health Promotion (http://www.cdc.gov/growthcharts).
FIGURE 3.
Two to 20 years: female patients, continued. BMI-for-age %BMIp95. The BMI of a female patient (Case 1) who transitioned from having normal weight to having severe obesity between the ages of 10 to 14 years was plotted by using a modified 2000 CDC percentile chart with %BMIp95, and the BMI of a female patient (Case 2) with underweight problems was plotted by using a modified 2000 CDC percentile chart with %BMIp95.
FIGURE 4.
Two to 20 years: female patients, continued. BMI-for-age z scores calculated by using the modified BMI z score. The BMI of a female patient (Case 1) who transitioned from having normal weight to having severe obesity between the ages of 10 to 14 years was plotted by using a modified BMI-for-age z score chart, and the BMI of a female patient (Case 2) with underweight problems was plotted by using a modified BMI-for-age z score chart.
Case 2
A 12-year-old girl with a history of attention deficit hyperactivity disorder was on stimulant therapy until 12 years of age, when she was referred to the specialty clinic for evaluation of growth failure. The patient had a severe loss of appetite and poor caloric intake, resulting in low body weight for age and poor weight gain. After weaning her from stimulants and implementing an optimized diet plan, her growth improved. Figure 2 illustrates the corresponding BMI changes in this patient plotted by using the conventional 2000 CDC percentile growth chart. Her growth was also plotted on the %BMIp95 chart (Fig 3); the plot is identical to the 2000 CDC BMI-for-age chart and tracks mostly below the third percentile, so it cannot be well quantified, creating a challenge for optimal tracking in these low percentiles. By using the modified BMI z score method in Fig 4, we note that the growth line has an upward trend toward the median from just < −3 SD to just > −2 SD, crossing 2 z lines over a 14-month period. By the WHO interpretation,11 the child has improved from a “severely wasted” category to being within normal limits.11
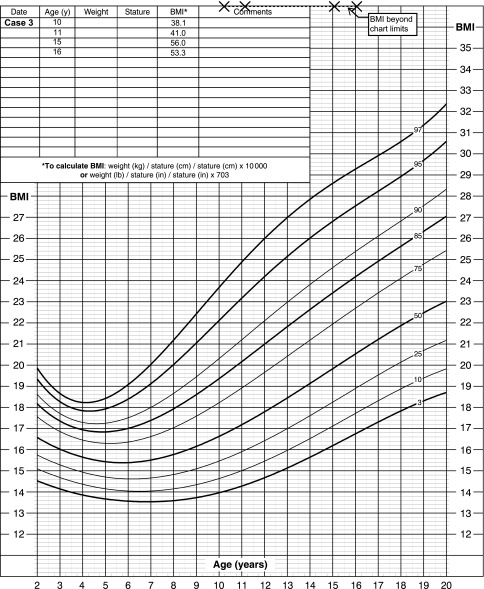
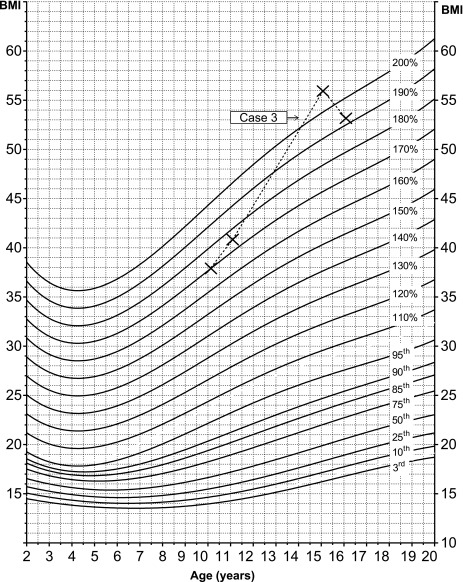
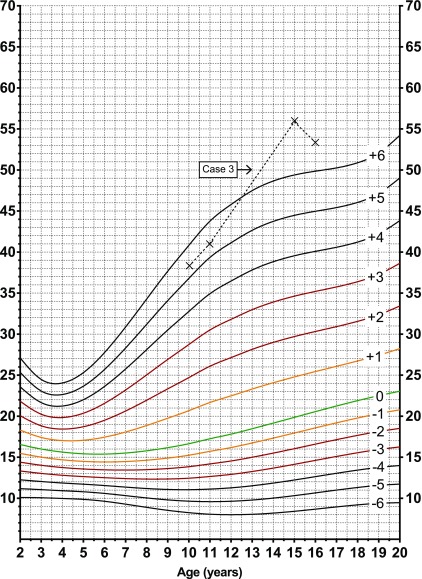
Case 3
A 15-year-old boy with no known underlying chronic medical problems was referred to the endocrine specialty clinic for excessive weight gain. He indulged in high consumption of calorie-dense foods, compounded by a sedentary lifestyle. Intensive lifestyle modifications were implemented that resulted in a slight reduction in BMI. His BMI could not be plotted by using the 2000 CDC clinical BMI-for-age percentile chart because all the BMI values exceeded 35 and were beyond the limit of the chart (Fig 5). Figure 6 shows how his BMI was tracked by using the %BMIp95 chart, and Fig 7 shows the plot using the modified BMI z score chart. In both the modified BMI z score chart and the %BMIp95 chart, a similar change in growth pattern and points of change are shown.
FIGURE 5.
Two to 20 years: male patient. BMI-for-age percentiles. Shown here are the BMI plots of a male patient (Case 3) with severe obesity who demonstrated an improvement in BMI that could not be tracked by using the CDC 2000 BMI-for-age-sex growth chart. Source: developed by the National Center for Health Statistics in collaboration with the National Center for Chronic Disease Prevention and Health Promotion (http://www.cdc.gov/growthcharts).
FIGURE 6.
Two to 20 years: male patient, continued. BMI-for-age %BMIp95. Shown here are the BMI plots of a male patient (Case 3) with severe obesity who demonstrated improvement in BMI that could be tracked by using a modified 2000 CDC percentile chart with %BMIp95.
FIGURE 7.
Two to 20 years: male patient, continued. BMI-for-age z scores calculated by using the modified BMI z score. Shown here are the BMI plots of a male patient (Case 3) with severe obesity who showed improvement in BMI that was adequately tracked by using a modified BMI-for-age z score chart.
Discussion
The reference population data for the 2000 CDC growth charts currently used for assessment of growth and nutritional status of children in the United States were obtained from nationally representative surveys conducted between 1963 and 1994.18 Since then, we have witnessed an obesity epidemic, with one-third of children now considered overweight or obese. The prevalence rates of class 2 (BMI ≥120% of the 95th percentile or BMI ≥35) and class 3 (BMI ≥140% of the 95th percentile or BMI ≥40) obesity have risen significantly and are estimated to be 5.9% and 2.1%, respectively.3 The inadequacies in optimal tracking of severely obese and underweight children by using current growth charts are problematic, especially in clinical settings where periodic growth monitoring is essential for assessing the effectiveness of therapeutic interventions.
To address the more pervasive issue of severe obesity, Flegal et al7 suggested that a practical approach would be to express high BMI values as a %BMIp95, rather than imputing high percentiles that are unreliable at the tails of the distribution. On the basis of this method, the American Heart Association defined severe obesity in children aged ≥2 years as having a BMI ≥120% BMIp95 for age and sex, or as having a BMI ≥35 (the definition of class 2 obesity in adults), whichever is lower.19 In 2012, Gulati et al5 built on this concept and proposed new growth charts that are convenient for clinical tracking of severely obese children and adolescents. Although the %BMIp95 method of characterizing severe obesity has been gaining favor, there is an obvious discontinuity in the units of measurement between the nonobese and obese groups. It also addresses only children in the upper extremes, and does not create a unified chart to track growth in children in the lower extremes. Z score charts do not have this limitation. However, in the current commonly used CDC BMI z scores, the power transformation to achieve normality results in a severe compression of the distribution of z scores, primarily at the upper end. To address the extreme values of growth indicators considered biologically implausible before the obesity epidemic, the CDC has since introduced a modified z score program.14 By using this method, the BMI of an individual is expressed relative to the median BMI in units of 1/2 the distance between 0 and +2 z scores.14 The advantage of this method is that assumptions are not made beyond the limits of observed values in the reference sample, and values can be tracked outside of the −3 to +3 SD range. The CDC documentation includes a description of the modified z score as a tool for identifying “implausible” values, that is, probable data errors. It is becoming increasingly clear, however, that many, if not nearly all, of these high values are real, representing severely obese children.20
We previously used the modified z score method to characterize secular trends in childhood obesity in an American Indian population.21 Although the CDC has developed a software program that calculates modified BMI z scores, it has not developed z score growth charts. To demonstrate the clinical utility of using a modified BMI z score chart, in the current study, we used illustrative cases from a pediatric endocrinology clinic to plot BMI changes in children with severe obesity and found that both %BMIp95 and modified CDC z score charts track growth changes in severely obese children satisfactorily. The modified BMI z score chart can also be used to track children who fall below the third percentile on standard charts. Among underweight children, the modified BMI z score chart was more informative than the 2000 CDC standard BMI% chart in this study. Recently, Freedman and Berenson15 compared different BMI metrices for longitudinal growth tracking in children. Modified BMI z values were substituted for BMI z values beyond <−1.88 (third percentile) or >1.88 (97th percentile).15 We have shown in Fig 1, however, that even within the ±1.88 SD range, the curves derived by using both methods are nearly identical. Hence, using a single modified BMI z score chart would be a simple and preferred replacement to the standard percentile and %BMIp95 charts. In addition, we recommend redefining weight categories based on z scores, as has been described in WHO z score growth charts.10,11
Although the authors of previous studies questioned the validity of BMI z scores in severe obesity and their weak association with other adiposity measures, these inferences were based largely on the compressed BMI z scores.6,13 By using data from the NHANES to compare BMI z scores, modified BMI z scores, %BMIp95, and the change in the smoothed 95th BMI percentile with indirect measures of adiposity that included circumferences, skinfolds, and fat mass, we found that BMIz had a weaker correlation with adiposity measures than %BMIp95 and the change in the smoothed 95th BMI percentile among the severely obese children13 This observation was made primarily because of the attenuation of the CDC’s estimated z scores from skewness, median, and coefficient of variation parameters, as explained previously.
Severe obesity is associated with substantial health risks, including a greater risk of diabetes and cardiovascular disease.22 In 1 study of American Indian youth, BMI was strongly associated with adiposity estimated from dual-energy radiograph absorptiometry, and BMI was as strongly associated with cardiovascular and metabolic risk factors as were dual-energy radiograph absorptiometry estimates.23 Childhood BMI also predicted early adult mortality.24 The modified BMI z score and %BMIp95 are also highly correlated in this population of American Indian children and adolescents aged 5 to 17 years (Spearman r = 0.99, P < .0001; S.K.T. et al, unpublished observations).
Modified BMI z scores are useful in quantifying values that lie beyond the percentile ranges and provide uniformity in characterizing growth trends in severe obesity without the discontinuity in units of measurement between obese and nonobese groups that occurs with the recently-proposed %BMIp95 charts.5 Children who are growing normally are expected to remain between −2 SD and +2 SD z scores of a specific anthropometric measure and consistently track along the same z score without crossing z score lines over time.10 A deviation may indicate risk on the basis of the direction of change toward or away from the median.10 Another benefit of modified z scores is the ability to track children on the opposite end of the weight spectrum. These children may be well below the third percentile on the standard BMI chart, and tracking their progress on standard charts is challenging. By using modified z scores, it is easier to determine if they are moving closer to, or farther from, the median. For ease of reading, we drafted our modified z score charts from −5 SD to +6 SD. However, these values can be altered infinitely to fit a specific clinical case. Lastly, an additional potential advantage of z scores is that they can be easily adapted and integrated into existing electronic health record systems. We have also color-coded the z score lines from −3 to +3 to help pediatric health providers in explaining growth patterns to parents. The only limitation we see to adopting the modified z score is that users will not be used to it and may confuse it with the traditional growth charts based on percentiles or with the unmodified z score that results in a compression of high values of BMI.
Conclusions
As the search continues for an optimal method of characterizing children with normal growth as well as growth problems who fall at the extremes of the spectrum of BMIs, we demonstrate, using clinical cases, the utility of plotting BMI using the modified z score method compared with methods using the %BMIp95 and standard BMI percentile 2000 CDC growth charts. The %BMIp95 statistic has the disadvantage of complexity because of its discontinuity at the 95th percentile, and the standard growth charts based on percentiles suffer from compression at the extremes because percentiles are bounded by 0 and 100, regardless of how low or high the BMI is. The modified z score charts, on the other hand, are conceptually and computationally simpler, accommodate high and low BMIs, and may be more useful in clinical settings as well as in epidemiologic studies. The modified BMI z chart should therefore be strongly considered as a replacement for the current CDC 2000 BMI percentile charts as well as the recently proposed %BMIp95 growth charts.
Acknowledgments
We acknowledge Ms Sayuko Kobes, Ms Dorota Wasak, Ms Mary Hoskin, and Mr Sanil Reddy for their assistance with the study.
Glossary
- BMIz
Centers for Disease Control and Prevention BMI unmodified z score
- CDC
Centers for Disease Control and Prevention
- WHO
World Health Organization
- %BMIp95
percentage of the smoothed 95th BMI percentile
Footnotes
Dr Chambers conceptualized the study, collected patient data, assisted in study design, and assisted in drafting the manuscript; Dr Tanamas and Ms Clark assisted is study design, assisted with creation of the growth charts, and critically reviewed the manuscript; Drs Dunnigan, Nelson, and Hanson assisted with the study design and critically reviewed the manuscript; Dr Kapadia obtained study data and critically reviewed the manuscript; Dr Knowler assisted in study design, including the creation of the growth charts, and critically reviewed the manuscript; Dr Sinha conceptualized the study, assisted in study design, and drafted the initial manuscript; and all authors approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by the Intramural Research Program of the National Institute of Diabetes and Digestive and Kidney Diseases. Funded by the National Institutes of Health (NIH).
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.United Nations Children’s Fund, World Health Organization, World Bank . Levels and Trends in Child Malnutrition: UNICEF-WHO-World Bank Joint Child Malnutrition Estimates. Washington, DC: World Bank; 2015 [Google Scholar]
- 2.Ogden CL, Carroll MD, Kit BK, Flegal KM. Prevalence of childhood and adult obesity in the United States, 2011-2012. JAMA. 2014;311(8):806–814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Skinner AC, Skelton JA. Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012. JAMA Pediatr. 2014;168(6):561–566 [DOI] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention Clinical growth charts. Available at: https://www.cdc.gov/growthcharts/clinical_charts.htm. Accessed on April 3, 2017
- 5.Gulati AK, Kaplan DW, Daniels SR. Clinical tracking of severely obese children: a new growth chart. Pediatrics. 2012;130(6):1136–1140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Woo JG. Using body mass index Z-score among severely obese adolescents: a cautionary note. Int J Pediatr Obes. 2009;4(4):405–410 [DOI] [PubMed] [Google Scholar]
- 7.Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90(5):1314–1320 [DOI] [PubMed] [Google Scholar]
- 8.Freedman DS, Butte NF, Taveras EM, Goodman AB, Ogden CL, Blanck HM. The limitations of transforming very high body mass indexes into z-scores among 8.7 million 2- to 4-year-old children. J Pediatr. 2017;188:50–56.e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang Y, Chen H-J. Use of percentiles and Z-scores in anthropometry In:Preedy VR, ed. Handbook of Anthropometry: Physical Measures of Human Form in Health and Disease. New York, NY: Springer Science+Business Media, LLC; 2012:29–48 [Google Scholar]
- 10.World Health Organization Training Course on Child Growth Assessment. Geneva, Switzerland: World Health Organization; 2008 [Google Scholar]
- 11.World Health Organization WHO Child Growth Standards: Length/Height-for-Age, Weight-for-Age, Weight-for-Length, Weight-for-Height, and Body Mass Index-for-Age: Methods and Development. Geneva, Switzerland: World Health Organization, Department of Nutrition for Health and Development; 2006 [Google Scholar]
- 12.Flegal KM, Cole TJ. Construction of LMS Parameters for the Centers for Disease Control and Prevention 2000 Growth Charts. National Health Statistics Reports; No 63. Hyattsville, MD: National Center for Health Statistics; 2013 [PubMed] [Google Scholar]
- 13.Freedman DS, Butte NF, Taveras EM, et al. . BMI z-scores are a poor indicator of adiposity among 2- to 19-year-olds with very high BMIs, NHANES 1999-2000 to 2013-2014. Obesity (Silver Spring). 2017;25(4):739–746 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Centers for Disease Control and Prevention Modified z-scores in the CDC growth charts. Available at: https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/biv-cutoffs.pdf Accessed on April 3, 2017
- 15.Freedman DS, Berenson GS. Tracking of BMI z scores for severe obesity. Pediatrics. 2017;140(3):e20171072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention A SAS program for the 2000 CDC growth charts (ages 0 to <20 years). Available at: https://www.cdc.gov/nccdphp/dnpao/growthcharts/resources/sas.htm. Accessed on April 3, 2017
- 17.Centers for Disease Control and Prevention Percentile data files with LMS values. Available at: https://www.cdc.gov/growthcharts/percentile_data_files.htm. Accessed on April 3, 2017
- 18.Kuczmarski RJ, Ogden CL, Guo SS, et al. . 2000 CDC growth charts for the United States: methods and development. Vital Health Stat 11. 2002; (246):1–190 [PubMed] [Google Scholar]
- 19.Kelly AS, Barlow SE, Rao G, et al. ; American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young, Council on Nutrition, Physical Activity and Metabolism, and Council on Clinical Cardiology . Severe obesity in children and adolescents: identification, associated health risks, and treatment approaches: a scientific statement from the American Heart Association. Circulation. 2013;128(15):1689–1712 [DOI] [PubMed] [Google Scholar]
- 20.Freedman DS, Lawman HG, Skinner AC, McGuire LC, Allison DB, Ogden CL. Validity of the WHO cutoffs for biologically implausible values of weight, height, and BMI in children and adolescents in NHANES from 1999 through 2012. Am J Clin Nutr. 102(5): 1000–1006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Vijayakumar P, Wheelock KM, Kobes S, et al. . Secular changes in physical growth and obesity among southwestern American Indian children over four decades [published online ahead of print December 6, 2016]. Pediatr Obes. doi: 10.1111/ijpo.12199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015;373(14):1307–1317 [DOI] [PubMed] [Google Scholar]
- 23.Lindsay RS, Hanson RL, Roumain J, Ravussin E, Knowler WC, Tataranni PA. Body mass index as a measure of adiposity in children and adolescents: relationship to adiposity by dual energy x-ray absorptiometry and to cardiovascular risk factors. J Clin Endocrinol Metab. 2001;86(9):4061–4067 [DOI] [PubMed] [Google Scholar]
- 24.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362(6):485–493 [DOI] [PMC free article] [PubMed] [Google Scholar]