Abstract
Fibrosis contributes to the development of many diseases and many target molecules are involved in fibrosis. Currently, the majority of fibrosis treatment strategies are limited to specific diseases or organs. However, accumulating evidence demonstrates great similarities among fibroproliferative diseases, and more and more drugs are proved to be effective anti-fibrotic therapies across different diseases and organs. Here we comprehensively review the current knowledge on the pathological mechanisms of fibrosis, and divide factors mediating fibrosis progression into extracellular and intracellular groups. Furthermore, we systematically summarize both single and multiple component drugs that target fibrosis. Future directions of fibrosis drug discovery are also proposed.
Keywords: fibrosis, drug, target, pathological mechanism, pharmacology
Introduction
Fibrosis, characterized by excess accumulation of extracellular matrix (ECM), is a common pathological process in many chronic diseases or injuries. Many irritations trigger the pro-fibrotic responses, including persistent infections, radiation, chemical agents, genetic disorders, and autoimmune diseases. The development of fibrosis is accompanied by the loss of a fraction of resident cells and their replacement by ECM, which would finally lead to tissue remodeling and organ failure. Fibrosis contributes to high morbidity and mortality in many diseases such as dilated cardiomyopathy and idiopathic pulmonary fibrosis (IPF) (Gulati et al., 2013; Hutchinson et al., 2015), and inevitably causes a prominent global clinical burden (Raimundo et al., 2016). For example, a study of medicare population aged 65 years and older showed that the incidence of IPF was around 93.7 cases per 100,000 person-years while the cumulative prevalence increased steadily to 494.5 cases per 100,000 person-years across 2001 to 2011 in US (Raghu et al., 2014). Besides, the mortality of non-alcoholic fatty liver disease (NAFLD) patients with a high probability of fibrosis was 69% higher than those without fibrosis (Kim et al., 2013).
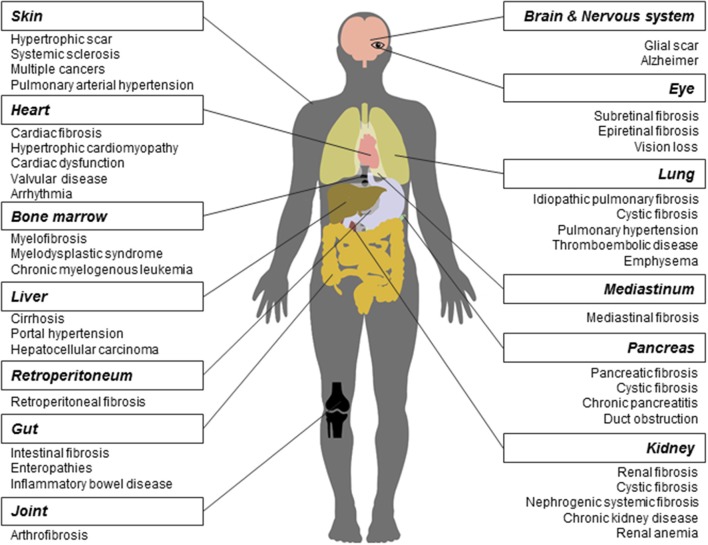
As a long-lasting pathological phenomenon, fibrosis occurs in various tissues and organs (Figure 1), more often in heart, lung, kidney, liver, skin (Rockey et al., 2015), and less frequently in other tissues and organs such as pancreas, intestine, eye (Wynn, 2008), nerve system (Kawano et al., 2012), mediastinum (Parish and Rosenow, 2002), retroperitoneum (Caiafa et al., 2013), joint and tendon (arthrofibrosis).
Figure 1.
Fibrosis and related diseases in various tissues and organs. Fibrosis is a pathological process that could occur in many tissues and organs and is associated with multiple diseases. Commonly reported fibrosis and associated diseases are listed.
Fibrosis contributes to the development of many diseases. First, many studies have demonstrated that the core mechanisms in fibrosis across various tissues and organs are similar. Wang and colleagues found that the interaction between transforming growth factor-β(TGF-β) and connective tissue growth factor signaling is required in kidney, liver, and lung fibrosis (Wang Q. et al., 2011). Makarev and colleagues identified a number of common pathways between lung and liver fibrogenesis, such as TGF-β, interleukin-6(IL-6), and integrin-linked kinase signaling (Makarev et al., 2016). Moreover, Wenzke and colleagues detected 90 genes, as well as several networks associated with connective tissue disorders, that play important roles in multi-organ fibrosis including lung, heart, liver, and kidney (Wenzke et al., 2012). On the basis of common pathogenesis across fibroproliferative diseases, some new drugs were proved effective in the treatment of fibrosis across different tissues and organs. For example, Pirfenidone has entered into the phase II clinical trial for treating the systemic sclerosis(SSc) (Khanna et al., 2016) and the phase III for IPF (King et al., 2014), respectively. Interferon drug Actimmune has been evaluated in patients with IPF (Skaria et al., 2015), liver (Muir et al., 2006), and cystic fibrosis (Moss et al., 2005).
Second, in different tissues and organs, multiple fibrotic diseases are related to each other. They are usually triggered by the same irritation and occur simultaneously. For example, heart and kidney together develop fibrosis (cardiorenal fibrosis) owing to the imbalance of natriuretic peptide system pathway and renin angiotensin aldosterone system/TGF-β1 pathway in aging (Sangaralingham et al., 2016). Chronic or acute renal failure may induce nephrogenic systemic fibrosis developed from thickening skin (Reiter et al., 2012) to impaired internal organs. In addition, cystic fibrosis, caused by gene mutation, could widely affect multiple organs, such as lung, kidney, and pancreas. Moreover, fibrosis is frequently a common pathological process in NAFLD and inflammatory bowel disease. Replacement of heart tissues by fibrotic protein could alter the ventricle size and shape, leading to hypertrophic cardiomyopathy (Khan and Sheppard, 2006). Cancers such as hepatocellular carcinoma share a series of risk factors with liver fibrosis (De Minicis et al., 2012).
Here we review the current knowledge on the pathological mechanisms of fibrosis and systematically summarize drugs targeting fibrosis in different fibroproliferative diseases. Future directions for fibrosis drug discovery are also proposed.
Pathogenesis of fibrosis
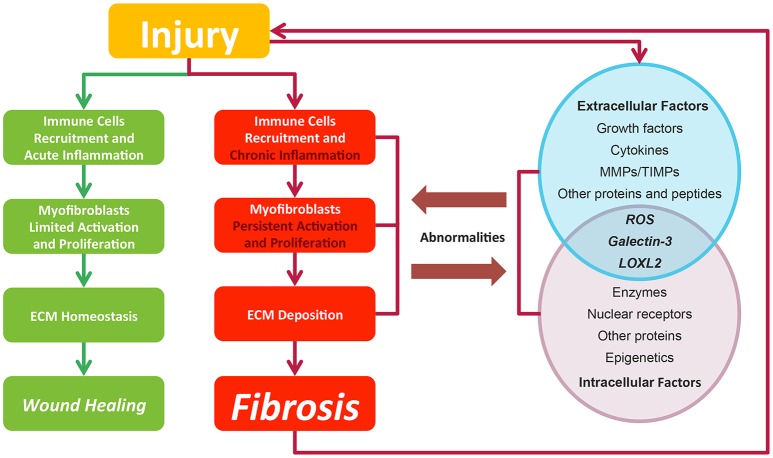
Fibrosis is considered as pathological outcomes of normal wound healing (Figure 2). When injuries occur and epithelial and/or endothelial cells are damaged, pro-inflammatory cytokines are released by the coagulation cascade for immune cell recruitment, mainly neutrophils and macrophages. These recruited immune cells function as the scavenger to remove tissue debris and dead cells, resulting in acute inflammation. Meanwhile, immune cells themselves release factors like chemokines and cytokines to amplify inflammatory reactions. Next, the released factors, such as TGF-β (Thannickal et al., 2003), platelet derived growth factor (PDGF) (Tang et al., 1996), interleukin-13 and interleukin-4 (Hashimoto et al., 2001), induce the limited activation and proliferation of myofibroblasts. Besides resident fibroblasts, myofibroblasts are derived from multiple cells (Hinz et al., 2007), including fibrocytes, epithelial cells via epithelial-mesenchymal transition (EMT), endothelial cells via endothelial-mesenchymal transition, pericytes, and smooth muscle cells related to blood vessels. In liver and pancreas, precursor cells like hepatic stellate cells (HSC) (Moreira, 2007) and pancreatic stellate cells (Apte et al., 2012) could also acquire myofibroblastic phenotype. Activated myofibroblasts migrate to injury sites, and their abilities to generate cell traction force enable them to stimulate wound closure (Li and Wang, 2011). Then, the balance of ECM synthesis and degradation could be achieved by myofibroblasts, resulting in ECM homeostasis. Finally, immune cells undergo apoptosis and epithelial/endothelial cells proliferate to regenerate injury sites, leading to wound healing.
Figure 2.
In normal wound healing condition, there is a series of ordered process: injury, immune cell recruitment and acute inflammation, myfibroblasts limited activation, and proliferation and ECM homeostasis, leading to wound closure after injury. While in pro-fibrotic condition, pathological process including chronic inflammation, myfibroblasts persistent activation, and proliferation and ECM deposition leading to fibrosis. Fibrosis itself could result in a secondary assault. Extracellular and intracellular factors interact with each other. Their abnormalities contribute to the fibrosis progression and in return are affected by pathological changes. Green lines and blocks represent normal wound healing while red lines and blocks represent fibrosis progression.
In contrast to normal wound healing process, the abnormalities of multiple factors could cause fibrosis (Biernacka et al., 2011) (Figure 2). Under some persistent stimuli, the overexpression of factors like pro-inflammatory cytokines or growth factors would overactivate (Kim et al., 2008) and interact with multiple kinases or nuclear receptors. The deficiencies of some factors would also contribute to fibrosis progression (Allen and Spiteri, 2002). Then, the abnormal signaling sustains to switch normal wound healing process to pro-fibrotic process, acting on the recruitment of excess immune cells, the induction of the myofibroblasts activation and proliferation and the promotion of ECM production. Pro-fibrotic process also promotes the activation of these factors conversely, thereby amplifying inflammatory responses and causing chronic inflammation. Finally, the sustained myofibroblasts activation would generate masses of ECM and tilt the balance in favor of synthesizing ECM to produce fibrosis. Furthermore, the pro-fibrotic process itself could contribute to secondary injury to the wound and cause a chronic vicious circle of pathological responses.
Below we divide factors modulating fibrosis progression into extracellular and intracellular groups, and discuss how they influence fibrosis progression.
Extracellular factors mediating the progression of fibrosis
The majority of the fibrosis-related extracellular factors are receptor-binding ligands, such as growth factors and cytokines. These factors target adjacent and distant cells in autocrine, paracrine, or endocrine signaling pathways. Then they bind to specific receptors on cell membrane and trigger the intracellular signaling, leading to pro-fibrotic cellular responses. Other extracellular factors, mainly enzymes such as matrix metalloproteinases (MMPs) could degrade ECM to prevent its excessive accumulation.
Growth factors contain a huge family of proteins that stimulate cell growth and proliferation. They are secreted by fibroblasts, immune cells, and epithelial/endothelial cells, and are able to orchestrate cellular responses. While epithelium/endothelium are damaged, cells in these tissues massively upregulate the production of growth factors to promote the proliferation of immune cells and fibroblasts. Among growth factors, TGF-β is the “master” modulator in fibrogensis (Meng et al., 2016), as it could provoke fibrosis through SMAD-dependent pathway (Lan, 2011) and SMAD-independent pathway related to a number of other pro-fibrotic reactions (Zhang, 2009). TGF-β signaling cascade results in differentiation of effector cells via inducing the expression of myofibroblasts hallmark α-hallmar muscle actin(α-SMA) (Sebe et al., 2008). In addition, TGF-β signaling leads to the transcription of collagen I and III genes (Fine and Goldstein, 1987; Chen et al., 1999) contributing to ECM accumulation. Interacting with TGF-β, many other growth factors have distinct roles in pro-fibrotic process. For example, PDGF induces HSC proliferation and type I collagen expression via downstream focal adhesion kinase/phosphoinositide 3-kinase/protein kinase B signaling (Reif et al., 2003). On the contrary, some growth factors have anti-fibrotic property, such as hepatocyte growth factor (HGF), the overexpression of which alleviates fibrosis in cardiomyopathic hamster through activation of MMP-1 and urokinase-type plasminogen activator (Taniyama et al., 2002). Excessive cytokines are usually secreted by immune cells, such as macrophages, neutrophils, and T cells in inflammation phase of wound healing. Compared with growth factors, cytokines tend to act as cell signaling transmitters to augment immunological responses and then lead to inflammation. One major type of cytokines is chemokines, which guide the recruitment of immune cells and fibroblasts to injury sites. Different immune cells are recruited by different chemokines. Neutrophils could be recruited by chemokine (C-X-C motif) ligand 1 and chemokine (C-X-C motif) ligand 8 by binding glycosaminoglycans with receptors in slightly different ways (Sawant et al., 2016). Chemokine (C-C motif) ligand 5 has been a major factor to induce the migration of HSC in liver fibrosis (Seki et al., 2009). Another type of cytokines is T cell cytokines, which are mainly secreted by activated T lymphocytes. They include interleukins, interferons and tumor necrosis factors (TNF), mediating adaptive immune responses and inflammation that might promote fibrosis. For example, IL-6 has been reported to shift the tissue repair to a chronic inflammatory state by signal transducer and activator of transcription 3(STAT3) signaling pathway in peritoneal fibrosis (Fielding et al., 2014). In contrast, some cytokines have anti-fibrotic effects. It has been reported that interferon-γ down-regulated the Adenosine A2A receptor signaling to prevent the production of type I collagen in HSC (Block and Cronstein, 2010). Moreover, some T cell cytokines, such as TNF-α, exhibit two-sided effects, pro-fibrotic or anti-fibrotic effect depending on the alternative status of macrophages and micro-environment (Redente et al., 2014).
MMPs are the extracellular endopeptidases degrading ECM including collagens, proteoglycans, laminins, and fibronectin. Tissue inhibitor of metalloproteinases (TIMPs) work as the inhibitors of MMPs. The balance of MMPs and TIMPs modulates the process throughout fibrosis development, including the formation of multiple cell injuries, the activation of latent cytokines and myofibroblasts and mainly, the maintenance of the homeostasis of ECM (Giannandrea and Parks, 2014). Some MMPs have pro-fibrotic functions whereas some have anti-fibrotic according to cell types and phases. The dysregulation of MMP-19 has been proved to cause the degradation of normal liver ECM and initiate liver injury (Jirouskova et al., 2012). Conversely, MMP-2 has been reported to cleave type I collagen and attenuate collagen deposition by HSC, inhibiting liver fibrosis (Radbill et al., 2011). As to TIMPs, they could inhibit or activate fibrosis via MMPs. For example, TIMP-3 inhibits MMPs to induce inflammation (Gill et al., 2010) in lung injury, and TIMP-1 has been found to play a dual role in liver fibrosis (Wang H. et al., 2011).
Other extracellular factors include a wide range of proteins and peptides. They mainly guide the differentiation of myofibroblasts, and are closely related to each other and growth factors. For example, the hedgehog (Hh) signaling pathway mediates EMT during the fetal development, and responds to injury through the repression of epithelial marker epithelial-cadherin by Snail and Twist. Overactivation of Hh signaling pathway contributes to biliary fibrosis and related liver fibrosis (Omenetti et al., 2008). In fibrotic kidney, the upregulated Wnt signaling has been reported to result in abundant of β-catenin. The signaling regulates genes such as Twist, LEF1 to induce EMT, thus to aggravate disease (He et al., 2009).
Intracellular factors mediating the progression of fibrosis
Intracellular factors, mainly multiple kinases, propagate the signaling received by cells through phosphorylation and other pathways. A common consequence of the signaling is that, transcription activators or inhibitors translocate into nucleus to regulate fibrosis-related gene expression and cell responses. In certain inflammatory pathways, intracellular factors also modulate the expression of extracellular factors, such as growth factors and cytokines, and secrete them out of cells to amplify inflammatory responses. Besides, epigenetic factors are emerging as a new way to affect fibrosis-related gene expression.
Intracellular factors include a number of kinases. In inflammation phase, many upstream factors, such as TGF-β, TNF-α, and epidermal growth factors initiate mitogen-activated protein kinase (MAPK) pathway. An element of MAPK pathway, mitogen-activated protein kinase-activated protein kinase-2 mediates myofibroblasts differentiation and regulates the gene expression of several matrix proteins such as col1a2, col3a1, and lox (Vittal et al., 2013). Another important intracellular signaling, mechanistic target of rapamycin (mTOR) pathway is activated by Wnt and TNF-α. Then, mTOR pathway activates ribosomal protein S6 kinase β-1 and modulates protein p21 or p27, which regulates the cell cycle of many cells including fibroblasts. In addition, the inhibition of mTOR pathway reduces collagen deposition and cardiac fibrosis (Chen et al., 2012). Besides serving as amplifiers of signal transduction, some intracellular enzymes such as cathepsin K, which belongs to lysosomal cysteine proteases, have been proved to be able to degrade ECM in lysosome after phagocytosis (Fukumori et al., 2003; Buhling et al., 2004).
Nuclear receptors are receptors located in cytoplasm and nucleus that could receive signals from intracellular ligands and bind to DNA to regulate gene expression. For example, peroxisome proliferator activated receptor γ(PPAR-γ), may directly regulate type I collagen gene (Yang et al., 2006) and block TGF-β signaling (Ghosh et al., 2009). Another nuclear receptor, farnesoid-X receptor (FXR), exhibits anti-fibrotic effect via the reduction of proliferating cholangiocytes and subsequent reduction of TGF-β (Liu et al., 2003). The activation of FXR also decreases a series of pro-fibrotic factors including TIMP-1, collagens, α-SMA, and MMP-2 (Zhang et al., 2009).
Nowadays, epigenetics including microRNAs, DNA methylation and lncRNAs, are found involved in machinery of pro-fibrotic process mainly through regulating fibrosis-related gene expression. Some microRNAs are found to negatively regulate translation of ECM components. Among them, miR-21 induces extracellular-signal regulated kinase/MAPK activity via the inhibition of Spry1 to protect cardiac fibroblasts survival (Thum et al., 2008). It has been reported that the levels of DNA methylation at specific CpG sites of pro-fibrotic genes (PPARα, PPARδ, TGFβ1, Collagen1A1, and PDGFα) differ among different fibrosis stages in NAFLD (Zeybel et al., 2015).
There are factors that affect fibrosis process both extra- and intracellularly, including reactive oxygen species (ROS), galectin-3 and lysyl oxidase homolog 2 (LOXL2). ROS can be generated through tissue injuries, cell damages and NADPH oxidase activities. Extracellular ROS targets latency-associated peptides and then activates TGF-β signaling while intracellular oxidative stress induces p53-dependent apoptosis in lung fibrosis via the caspases-9/3 activation in mitochondria (Cheresh et al., 2013). As to galectin-3, extracellular galectin-3 induces T cell apoptosis and plays a dual function inside and outside cells (Li et al., 2014). Another factor LOXL2 is generally considered as extracellular enzyme that promotes collagen production and crosslink with collagen fibers in response to mechanical stress (Yang et al., 2016). While on the other hand, intracellular LOXL2 has been reported to induce EMT in carcinoma progression (Peinado et al., 2005).
Many studies proved that different fibroproliferative diseases share common underlying mechanisms (Wenzke et al., 2012). The existence of common mechanisms facilitates the complete interpretation of fibrosis pathogenesis and enhances our understanding of fibrosis-related diseases. On this basis, it is necessary to reconsider targets involved in these mechanisms and evaluate their potential roles in fibrosis treatment across tissues and organs.
Drugs and targets in fibrosis
Motivated by huge clinical burdens, continuous intense researches on drug targeting fibrosis have been conducted, many of which have led to clinical trials. Due to the strong associations between inflammation and fibrosis, more efforts have been devoted to anti-inflammation drugs in the past few years (Dinwiddie, 2005). Nowadays, new targets and drugs for fibrosis are constantly emerging with the progress in understanding fibrosis pathology. Here we summarize them in Tables 1–4, including single (Tables 1–3) and multi component (Table 4) drugs with their verified and potential targets in fibrosis.
Table 1.
Single-component drugs targeting extracellular factors.
| Target | Drug | Clinical trialb | Reference | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | Target or mechanism type | Target or mechanism | Organsa | Drug Name | Mechanism | Class | Disease | Phase | Reference/Trial identifierc |
| Growth factors | Extracellular TGF-β signaling | TGF-βd | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | SHP-627 (FT011) | Inhibitor | Small molecule | Cardiac fibrosis | Preclinical | Zhang et al., 2012 |
| Hydronidone (F351) | Inhibitor | Small molecule | Liver fibrosis | 2(unknown) | NCT02499562 | ||||
| PXS-25 | Inhibitor | Small molecule | IPFd | Preclinical | Maldonado et al., 2009; Wong et al., 2011 | ||||
| Disitertide (P-144) | Inhibitor | Small molecule | Skin fibrosis | 2(completed) | NCT00574613 | ||||
| Fresolimumab (GC-1008) | Inhibitor | Monoclonal antibody | IPF; SScd | 1(completed); 1(completed) | NCT00125385; NCT01284322 | ||||
| LY2382770 | Inhibitor | Monoclonal antibody | Diabetic kidney disease | 2(terminated) | NCT01113801 | ||||
| Integrin αvβ6 | STX-100 | Inhibitor | Monoclonal antibody | IPF | 2(completed) | NCT01371305 | |||
| CWHM-12 | Inhibitor | Small molecule | Liver fibrosis; Lung fibrosis | Preclinical | Henderson et al., 2013 | ||||
| ALK5d | SB-431542 | Antagonist | Small molecule | Pulmonary fibrosis | Preclinical | Koh et al., 2015 | |||
| BMP-7d | THR-184 | Agonist | Small molecule | Renal fibrosis | 2(completed) | NCT01830920 | |||
| CTGFd | CTGF | PF-06473871 | Inhibitor | Small molecule | Hypertrophic scar | 2(completed) | NCT01730339 | ||
| RXI-109 | Inhibitor | Small molecule | Hypertrophic scar | 2(completed) | NCT02030275 | ||||
| FG-3019 | Inhibitor | Monoclonal antibody | IPF | 2(active, not recruiting) | NCT01890265 | ||||
| PDGFd/VEGFd | PDGFRd | Imatinib | Antagonist | Small molecule | Nephrogenic systemic fibrosis; SSc; IPF | Approved| 2(completed); 2(completed); 3(completed) | NCT00677092; NCT00613171; NCT00131274 | ||
| BOT-191 | Antagonist | Small molecule | Liver fibrosis | Preclinical | van Dijk et al., 2015 | ||||
| Nilotinib (AMN-107) | Antagonist | Small molecule | SSc | Approved| 2(completed) | NCT01166139 | ||||
| Dasatinib | Antagonist | Small molecule | Scleroderma pulmonary fibrosis | Approved| 2(completed) | NCT00764309 | ||||
| VEGFRd/PDGFR | Nintedanib (BIBF-1120) | Antagonist | Small molecule | Scleroderma; IPF | Approved| 3(recruiting); 3(completed) | NCT02597933; NCT01335464 | |||
| Sorafenib (BAY 43-9006) | Antagonist | Small molecule | Extensive keloids | Approved| 2(terminated) | NCT01425216 | ||||
| TNFd | TNF | Thalidomide | Inhibitor | Small molecule | IPF | Approved| 2(completed) | NCT00162760 | ||
| Pomalidomide | Inhibitor | Small molecule | IPF | Approved| 2(withdrawn) | NCT01135199 | ||||
| Etanercept | Inhibitor | Recombinant protein | IPF | Approved| 2(completed) | NCT00063869 | ||||
| Belimumab | Inhibitor | Monoclonal antibody | SSc | Approved| 2(completed) | NCT01670565 | ||||
| HGFd | HGF | Liver, Kidney, Lung, Heart, Skin | Refanalin (BB-3) | Stimulant | Small molecule | Liver fibrosis; IPF | Preclinical | Fallowfield, 2011 | |
| Cytokines | Interleukin | IL-13d | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | Dectrekumab (QAX-576) | Inhibitor | Monoclonal antibody | IPF; IPF secondary to SSc | 2(terminated); 2(terminated) | NCT01266135; NCT00581997 |
| Tralokinumab | Inhibitor | Monoclonal antibody | IPF | 2(terminated) | NCT01629667 | ||||
| IL-1R1 | Liver, Kidney, Lung, Heart, Skin, Gut | Anakinra | Antagonist | Recombinant protein | Cystic fibrosis | Approved| Preclinical | Iannitti et al., 2016 | ||
| IL-1βR | Rilonacept | Antagonist | Recombinant protein | SSc | Approved| 2(active, not recruiting) | NCT01538719 | |||
| IL-13/IL-4 | SAR156597 | Inhibitor | Monoclonal antibody | SSc; IPF | 2(recruiting); 2(completed) | NCT02921971; NCT01529853 | |||
| CC chemokine | CCL2d | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | Carlumab (CNTO-888) | Inhibitor | Monoclonal antibody | IPF | 2(completed) | NCT00786201 | |
| Bindarit | Inhibitor | Small molecule | Myocardial fibrosis; Renal fibrosis | Preclinical | Lin et al., 2009; Zhu et al., 2009 | ||||
| CCR5d | Liver, Kidney, Lung | Maraviroc | Antagonist | Small molecule | Liver fibrosis | Approved| Preclinical | Gonzalez et al., 2014 | ||
| CCR2 | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | RS-504393 | Antagonist | Small molecule | Renal fibrosis | Preclinical | Kitagawa et al., 2004 | ||
| Interferon | IFN-γRd | Actimmune | Stimulant | Interferon | IPF; Liver fibrosis; Cystic fibrosis | Approved| 3(completed); 2(completed); 2(completed) | NCT00047658; NCT00043303; NCT00043316 | ||
| IFN-α | Liver, Kidney, Lung | Interferon alpha oral lozenge | Stimulant | Interferon | Pulmonary fibrosis | 2(completed) | NCT01442779 | ||
| MMPd/TIMPd | MMP/TIMP | MMP-2/MMP-9/TIMP-1 | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | Batimastat(BB-49) | Inhibitor | Small molecule | IPF | Preclinical | Corbel et al., 2001 |
| MMP/TIMP | Marimastat | Inhibitor | Small molecule | Liver fibrosis | Approved| Preclinical | de Meijer et al., 2010 | |||
| Other proteins and peptides | Endothelin | ET-1 receptord | Liver, Kidney, Lung, Heart, Skin, Gut | Macitentan | Antagonist | Small molecule | IPF | Approved| 2(completed) | NCT00903331 |
| Bosentan | Antagonist | Small molecule | IPF; SSc; | Approved| 3(completed); 3(completed); 4(completed) | NCT00070590; NCT00319696; NCT01395732 | ||||
| Ambrisentan | Antagonist | Small molecule | IPF; SSc | Approved| 3(terminated); 4(unknown) | NCT00879229; NCT01051960 | ||||
| Sparsentan (RE-021) | Antagonist | Small molecule | Focal segmental glomerulosclerosis | 2(active, not recruiting) | NCT01613118 | ||||
| Atrasentan | Antagonist | Small molecule | Renal fibrosis | Preclinical | Samad et al., 2015 | ||||
| Angiotensin II | AT1 receptord | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | Losartan | Antagonist | Small molecule | Liver fibrosis; Cystic fibrosis | Approved| 4(completed); 2(not yet recruiting) | NCT00298714; NCT03206788 | |
| GPCRd | LPARd | Liver, Kidney, Lung, Skin | BMS-986020 | Antagonist | Small molecule | SSc; IPF | 2(withdrawn); 2(completed) | NCT02588625; NCT01766817 | |
| SAR-100842 | Antagonist | Small molecule | SSc | 2(completed) | NCT01651143 | ||||
| PAR1d | Liver, Kidney, Lung, Heart, Pancreas, Skin | PAR1 antagonism | Antagonist | Small molecule | Liver fibrosis | Preclinical | Fiorucci et al., 2004 | ||
| CB1 receptord | Liver | Curcumin* | Antagonist | Small molecule | Liver fibrosis; Renal fibrosis; IPF | Preclinical | Smith et al., 2010; Zhang et al., 2013; Sun et al., 2017 | ||
| Silymarin* | Antagonist | Small molecule | Liver fibrosis | Preclinical | Tsai et al., 2008; Zhang et al., 2013 | ||||
| CB2 receptord | β-caryophyllene* | Agonist | Small molecule | Liver fibrosis | Preclinical | Calleja et al., 2013; Mahmoud et al., 2014 | |||
| Prostacyclin receptor | Liver, Kidney, Lung, Heart, Pancreas | Beraprost | Agonist | Small molecule | Renal fibrosis; Cardiac fibrosis | Preclinical | Chen et al., 2014 | ||
| Iloprost | Agonist | Small molecule | SSc | Approved| 2(completed) | NCT00109681 | ||||
| Treprostinil | Agonist | Small molecule | IPF; SSc | Approved| 2(terminated); 2(completed) | NCT00703339; NCT00775463 | ||||
| VIP receptor | Lung | Aviptadil | Agonist | Peptide hormone | Cystic fibrosis | Preclinical | Mathioudakis et al., 2013 | ||
| Leukocyte elastase | Leukocyte elastase | Sivelestat | Inhibitor | Small molecule | IPF | Preclinical | Takemasa et al., 2012 | ||
| TAFId | TAFI | Liver, Kidney, Lung | UK-396082 | Inhibitor | Small molecule | Renal fibrosis | Preclinical | Atkinson et al., 2015 | |
| Relaxin | Relaxin receptor | Liver, Kidney, Lung, Heart, Skin | Serelaxin | Stimulant | Peptide hormone | Cardiac fibrosis; Renal fibrosis | Preclinical | Samuel et al., 2014; Huuskes et al., 2015 | |
| SAPd | SAP (mimic) | PRM-151 | Stimulant | Recombinant protein | IPF | 2(active, not recruiting) | NCT02550873 | ||
| Integrin α | Integrin α5 | Liver | Dioscin* | Inhibitor | Small molecule | Liver fibrosis | Preclinical | Liu et al., 2015; Zhang et al., 2015a,b; Gu et al., 2016; Xu et al., 2017; Yin et al., 2017 | |
| TGMd | TGM2 | Kidney, Lung | NTU281 | Inhibitor | Small molecule | Renal fibrosis | Preclinical | Johnson et al., 2007 | |
Drug belongs to monomer extracted from natural products.
Organs that had study report of corresponding targets in fibrosis treatment.
Clinical trial resource are from http://Clinicaltrials.gov.
Trial Identifier is the clinical trail identifier of corresponding drug
TGF-β, transforming growth factor-β; IPF, idiopathic pulmonary fibrosis; SSc, systematic sclerosis; ALK5, TGF-β receptor 1; BMP-7, bone morphogenetic protein 7; CTGF, connective tissue growth factor; PDGF, platelet-derived growth factor; PDGFR, platelet-derived growth factor receptor; VEGF, vascular endothelial growth factor; VEGFR, vascular endothelial growth factor receptor; TNF, tumor necrosis factor; HGF, hepatocyte growth factor; IL-13, interleukin-13; CCL2, chemokine (C-C motif) ligand 2; CCR5, C-C chemokine receptor type 5; IFN-γR, interferon-γ receptor; MMP, matrix metalloproteinase; TIMP, tissue inhibitor of metalloproteinase; ET-1 receptor, endothelin-1 receptor; AT1 receptor, angiotensin II receptor type 1; GPCR, G protein-coupled receptor; LPAR, lysophosphatidic acid receptor; PAR1, protease-activated receptor 1; CB1 receptor, cannabinoid receptor type 1; TAFI, thrombin activatable fibrinolysis inhibitor; SAP, serum amyloid P; VIP, vasoactive intestinal peptide; TGM2, transglutaminase.
Single-component drugs targeting extracellular factors mediating fibrosis
Nowadays, most approved and investigational drugs are single-component drugs, which only contain one organic component and have distinct targets. As we described previously, fibrosis progression results from a combination of the abnormalities of extracellular and intracellular factors. Drugs targeting extracellular factors are prevalent, about 60% of known targets are receptors located on cell membrane mainly because the extracellular targets are accessible and serve as upstream signals (Overington et al., 2006), and so are the targets of fibrosis-related drugs. The binding of receptors and ligands triggers the downstream signaling, thus the blockade of receptors or ligands is considered to be an effective choice to alleviate fibrosis (Table 1).
The majority of anti-fibrosis drugs targeting extracellular factors are inhibitors of ligands such as growth factors, cytokines and MMPs. Most inhibitors could directly bind to the active sites of targets. The majority of approved inhibitor drugs in Table 1 target TNF, which are widely used in fibrosis-related diseases and could suppress the action of TNF through multiple mechanisms. These drugs include small molecules Thalidomide and Pomalidomide (Weingartner et al., 2012), recombinant protein Etanercept and monoclonal antibodies Belimumab. Thalidomide and Etanercept have completed the phase II trial in IPF (Raghu et al., 2008; Horton et al., 2012) while Belimumab has completed the phase II trial in SSc. Besides, some inhibitor drugs targeting growth factors are still under investigation. For example, Disitertide, a synthetic peptide derived from TGF-β type III receptor, inhibits the binding of TGF-β and its receptor and exhibit anti-fibrotic function (Ezquerro et al., 2003). Drugs that inhibit interleukins are always monoclonal antibodies. Tralokinumab, a human IgG4 monoclonal antibody, shows pro-apoptotic effects via IL-induced apoptotic factors in IPF (Murray et al., 2014). Many natural products act as inhibitor drugs like Dioscin, which is a monomer extracted from Dioscoreae Rhizoma and could ameliorate liver fibrosis (Liu et al., 2015; Zhang et al., 2015a,b; Gu et al., 2016; Xu et al., 2017; Yin et al., 2017). In addition, some preclinical drugs inhibit MMPs, like Marimastat, which simultaneously down-regulates MMPs gene expression and MMPs activities. However, Marimastat reduces inflammation and liver injuries while increases fibrosis in mice model. This may result from the indiscriminative inhibition of MMPs, some of which function to degrade ECM (de Meijer et al., 2010).
Compared with inhibitor drugs, antagonists achieve the same inhibition effect by targeting cell membrane receptors to dampen downstream signaling. These small molecules bind to receptors without effectively activating them. The receptors of PDGF, vascular endothelial growth factor, endothelin (ET), and angiotensin all have approved antagonist drugs. An antagonist for tyrosine kinase receptors of PDGF, Imatinib, has showed protective effect by reducing differentiation of resting fibroblasts in SSc mice model (Akhmetshina et al., 2009). However, it did not show efficacy in phase II clinical trial in IPF (Daniels et al., 2010) and the high-dose of Imatinib may lead to severe adverse events (Khanna et al., 2011). Macitentan, a dual antagonist of ETA and ETB receptor, is beneficial for lung fibrosis. Similarly, another drug Losartan targeting angiotensin II receptor has been evaluated in IPF patients (Couluris et al., 2012). Some preclinical antagonist drugs including Maraviroc (Gonzalez et al., 2014), Atrasentan (Ritter et al., 2014), and PAR1 antagonists (Fiorucci et al., 2004) were under investigation for fibrosis treatment.
On the contrary, many drugs exert their therapeutic effects by activating their targets. Many anti-fibrotic receptors can be targets of these exogenous agonists that augment the downstream biological responses to suppress fibrosis. An approved agonist drug in this category is Iloprost, which can reverse right ventricle fibrosis by re-establishing collagen balance (Gomez-Arroyo et al., 2015). Another agonist of vasoactive intestinal peptide, Treprostinil, reduces inflammation and collagen deposition (Manitsopoulos et al., 2015). Other anti-fibrotic agonists for cell membrane receptors include Aviptadil, INT-767 (Baghdasaryan et al., 2011) and Beraprost (Kaneshige et al., 2007).
Moreover, a few drugs are synthetic proteins that bind receptors to serve as stimulants and perform the same functions as native proteins. An approved drug, synthetic interferon-γ, Actimmune, has completed phase II or phase III study in multiple fibrosis including IPF (Skaria et al., 2015), liver fibrosis (Muir et al., 2006), and cystic fibrosis (Moss et al., 2005). Another stimulant Refanalin, a HGF mimetic, is a potential drug for liver fibrosis (Fallowfield, 2011; Pellicoro et al., 2014).
Single-component drugs targeting intracellular factors mediating fibrosis
Compared with extracellular factors, intracellular targets are less popular owing to their inaccessibility. Drugs targeting intracellular factors are less varied because most of them are small molecules. Small molecules could readily translocate into cytoplasm while large molecules such as monoclonal antibodies face more challenges to cross the plasma membrane (Imai and Takaoka, 2006). Nevertheless, more and more studies concerned intracellular factors as targets in recent years, and numerous candidate targets are identified in cytoplasm, nucleus, and mitochondrion. Many approaches, including increasing membrane permeation, combination with supercharged proteins and activating transport through receptors, were implemented to deliver drugs across cell membrane (Mitragotri et al., 2014).
Fibrosis drugs targeting intracellular factors are summarized and classified into four categories: enzymes, nuclear receptors, other proteins, and epigenetics (Table 2). Many drugs acting through intracellular factors are also inhibitors. These drugs inhibit a wide range of kinases located in cytoplasm, and consequently suppress the translocation of transcription factors that drive the expression of pro-fibrotic genes. Rapamycin and Sirolimus are approved drugs that inhibit mTOR. Rapamycin prevents the activation of macrophages and myofibroblasts and the subsequent release of TGF-β in chronic kidney disease (CKD) (Chen et al., 2012). Sirolimus shows anti-inflammatory and anti-fibrotic effects in IPF (Tulek et al., 2011). Besides kinases, there are many other intracellular proteins that serve as potential targets for fibrosis management. Pirfenidone, one of the IPF drugs, has completed phase III trial in IPF patients with alleviated disease progression and acceptable side effects (King et al., 2014). The potential mechanism of Pirfenidone is inhibiting the nuclear accumulation of intracellular proteins SMAD2/3 to regulate TGF-β signaling (Choi et al., 2012). Other approved inhibitor drugs include Ruxolitinib for bone marrow fibrosis (Wilkins et al., 2013), Paquinimod for SSc (Stenstrom et al., 2016), and Pentoxifylline (Okunieff et al., 2004) combined with vitamin E (Jacobson et al., 2013).
Table 2.
Single-component drugs targeting intracellular factors.
| Target | Drug | Clinical trialb | Reference | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Group | Target or mechanism type | Target or mechanism | Organsa | Drug Name | Mechanism | Class | Disease | Phase | Reference/Trial identifierc |
| Enzymes | mTORd | mTORC1/2d | Liver, Kidney, Lung, Heart, Skin, Gut | Rapamycin (Sirolimus)* | Inhibitor | Small molecule | Renal interstitial fibrosis | Approved| 3(completed) | NCT01079143 |
| Palomid-529 (RES-529) | Inhibitor | Small molecule | Macular degeneration | 1(completed) | NCT01033721 | ||||
| JAK-STATd | JAK1/JAK2d | Ruxolitinib | Inhibitor | Small molecule | Myelofibrosis | Approved| 3(completed) | NCT00952289 | ||
| Baricitinib | Inhibitor | Small molecule | Renal interstitial fibrosis | Preclinical | Breyer and Susztak, 2016 | ||||
| PI3K-Aktd | Akt | Liver, Kidney, Lung, Heart, Skin | Omipalisib (GSK2126458) | Inhibitor | Small molecule | IPFd | 1(completed) | NCT01725139 | |
| FAK1d | Liver, Kidney, Lung, Heart, Pancreas, Skin | PF-562271 | Inhibitor | Small molecule | Pulmonary fibrosis; Cardiac fibrosis; Liver fibrosis | Preclinical | Lagares et al., 2012; Fan et al., 2015; Zhao et al., 2017 | ||
| MAPKd | JNKd | Tanzisertib (CC-930) | Inhibitor | Small molecule | IPF | 2(terminated) | NCT01203943 | ||
| MAPK | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | MMI-0100 | Inhibitor | Small molecule | IPF; Cardiac fibrosis | Preclinical | Xu et al., 2014 | ||
| NF-κBd | IKKd | IMD-1041 | Inhibitor | Small molecule | Cardiac fibrosis | Preclinical | Tanaka et al., 2012 | ||
| Bardoxolone methyl (CDDO-Me) | Inhibitor | Small molecule | Pulmonary hypertension | 2(recruiting) | NCT02036970 | ||||
| NF-κB | Antisense NF-κB | Inhibitor | Antisense oligonucleotide | Intestinal fibrosis | Preclinical | Lawrance et al., 2003 | |||
| Baicalein* | Inhibitor | Small molecule | Renal fibrosis; IPF | Preclinical | Gao et al., 2013; Wang et al., 2015 | ||||
| Sulfasalazine | Inhibitor | Small molecule | Liver fibrosis; Pancreatic fibrosis | Approved| Preclinical | Chavez et al., 2012; Wang et al., 2016 | ||||
| cAMP-PKAd | ROCKd | Y-27632 | Inhibitor | Small molecule | Renal fibrosis; Liver fibrosis | Preclinical | Tada et al., 2001 | ||
| Non-kinase enzyme | 26S protease | Liver, Kidney, Lung, Heart | Bortezomib | Inhibitor | Small molecule | SSc pulmonary fibrosis | Approved| 2(recruiting) | NCT02370693 | |
| Caspase | Liver, Kidney, Lung, Heart, Skin | Emricasan | Inhibitor | Small molecule | Liver fibrosis | Preclinical | Barreyro et al., 2015 | ||
| VX-166 | Inhibitor | Small molecule | Liver fibrosis | Preclinical | Witek et al., 2009 | ||||
| Z-VAD-fmk | Inhibitor | Small molecule | Pulmonary fibrosis | Preclinical | Kuwano et al., 2001 | ||||
| PDEd | Kidney, Heart | CTP-499 | Inhibitor | Small molecule | Diabetic nephropathy | 1(completed) | NCT01328821 | ||
| Cathepsin B | Liver, Lung, Heart, Pancreas | VBY-376 | Inhibitor | Small molecule | Liver fibrosis | Preclinical | Alkhouri et al., 2011 | ||
| CA-074Me | Inhibitor | Small molecule | Pancreatic fibrosis; Cardiac fibrosis; Pulmonary fibrosis | Preclinical | Lerch and Halangk, 2006; Liu et al., 2013; Zhang et al., 2015 | ||||
| S100A9 | Liver, Lung, Heart, Skin | Paquinimod | Inhibitor | Small molecule | SScd | 2(completed) | NCT01487551 | ||
| Procollagen-proline dioxygenase | Liver, Lung | HOE-077 | Inhibitor | Small molecule | Liver fibrosis | Preclinical | Matsumura et al., 1997 | ||
| Nuclear receptors | PPARd | PPAR-γ | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | Rosiglitazone | Agonist | Small molecule | Liver fibrosis; | Approved| 2(completed) | NCT00492700 |
| Elafibranor (GFT-505) | Agonist | Small molecule | Liver fibrosis | 3(recruiting) | NCT02704403 | ||||
| Saroglitazar | Agonist | Small molecule | Liver fibrosis | 2(recruiting) | NCT03061721 | ||||
| Pioglitazone | Agonist | Small molecule | Cystic fibrosis; Liver fibrosis | Approved| 1(completed); 1(completed) | NCT00719381; NCT01454336 | ||||
| Docosahexaenoic acid* | Agonist | Small molecule | Liver fibrosis; Pulmonary fibrosis | Preclinical | Depner et al., 2013; Zhao et al., 2014 | ||||
| FXRd | FXR | Liver, Kidney, Lung, Gut | INT-767 | Agonist | Small molecule | Liver fibrosis | Preclinical | Baghdasaryan et al., 2011 | |
| PX-102 | Agonist | Small molecule | Liver fibrosis | Preclinical | Ali et al., 2015 | ||||
| Obeticholic acid* (INT-747) | Agonist | Small molecule | Liver fibrosis | Approved| 3(recruiting) | NCT02548351 | ||||
| Turofexorate isopropyl (WAY-362450) | Agonist | Small molecule | Liver fibrosis | Preclinical | Zhang et al., 2009 | ||||
| GW4064 | Agonist | Small molecule | Liver fibrosis | Preclinical | Liu et al., 2003 | ||||
| GRd | GR | Liver, Lung, Heart, Skin | Triamcinolone | Agonist | Small molecule | Keloid scarring | Approved| 1(terminated) | NCT01978301 | |
| ERd | ERβ | Liver | Genistein* | Agonist | Small molecule | Pulmonary fibrosis; Liver fibrosis | Preclinical | Salas et al., 2008; Nadadur et al., 2012 | |
| Other proteins | Intracellular TGF-βd signaling | SMAD2/3 | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | Pirfenidone | Inhibitor | Small molecule | IPF; SSc | Approved| 3(completed); 2(completed) | NCT00287729; NCT01933334 |
| SMAD3/4 | Pentoxifylline | Inhibitor | Small molecule | Skin fibrosis | Approved| 2(completed) | NCT00001437 | |||
| SMAD3 | SIS-3 | Inhibitor | Small molecule | Renal fibrosis | Preclinical | Meng et al., 2015 | |||
| Glycyrrhizin* | Inhibitor | Small molecule | Liver fibrosis | 3(terminated) | NCT00686881 | ||||
| Epigenetics | miRNA | miR-21 | Anti-miR-21 | Inhibitor | Oligonucleotide | IPF; Renal fibrosis | Preclinical | Liu et al., 2010; Chau et al., 2012 | |
| methylation | Transmethylation | Liver, Kidney, Lung, Heart, Skin, Gut | Ademetionine (SAM) | Inhibitor | Small molecule | Liver fibrosis | Approved| Unknown | NCT02231333 | |
| BMPER (gene) | Lung | DNA methylation | Inhibitor | Methylation | IPF | Preclinical | Huan et al., 2015 | ||
Drug belongs to monomer extracted from natural products.
Organs that had study report of corresponding targets in fibrosis treatment.
Clinical trial resource are from http://Clinicaltrials.gov.
Trial Identifier is the clinical trail identifier of corresponding drug.
mTOR, mechanistic target of rapamycin; mTORC1, mechanistic target of rapamycin complex 1; JAK-STAT, janus kinase/signal transducers and activators of transcription; PI3K-Akt, phosphoinositide 3-kinase/protein kinase B; IPF, idiopathic pulmonary fibrosis; FAK1, focal adhesion kinase 1; MAPK, mitogen-activated protein kinase; JNK, c-Jun N-terminal kinases; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells; IKK, I-kappa B kinase; cAMP-PKA, cyclic AMP- protein kinase A signaling; ROCK, rho-associated protein kinase; PDE, phosphodiesterase; SSc, systematic sclerosis; PPAR, peroxisome proliferator-activated receptor; FXR, farnesoid X receptor; GR, glucocorticoid receptor; ER, estrogen receptor; TGF-β, transforming growth factor-β.
In addition, there are also some nuclear receptors located in cytoplasm and nucleus, which could be activated by small molecule agonists, such as PPAR. Rosiglitazone, a PPAR-γ agonist, has anti-fibrotic effect as a consequence of activating MMP-1 and elevating HGF expression in patients with systemic sclerosis-related interstitial lung disease (Bogatkevich et al., 2012). Other approved PPAR targeting drugs like Elafibranor and Pioglitazone, have entered phase II and phase I studies, respectively. Obeticholic acid is an approved drug entering phase III study that decreases inflammation and fibrosis in NASH patients via activating FXR signaling (Verbeke et al., 2016).
Epigenetics are very different types of fibrosis therapies. The most studied epigenetics-based therapy for fibrosis is microRNA. MicroRNA could be neutralized by specific anti-miRNA oligonucleotides delivered into cells. Among them, anti-miR-21 has been reported to inhibit miR-21 activity and ameliorate fibrosis progression through PPAR signaling in CKD (Chau et al., 2012). Another strategy is the intervention of DNA methylation for proteins such as BMP endothelial cell precursor-derived regulator (BMPER), which acts as the regulator of fibroblasts activation. Altering methylation on BMPER gene has been reported to decrease BMPER level and thus to inhibit fibroblasts activity (Huan et al., 2015). Besides, some drugs targeting both extracellular and intracellular factors are also incorporated (Table 3). A majority of them are antioxidants, including an approved drug N-acetylcysteine (Zhang et al., 2014).
Table 3.
Single-component drugs targeting both extra- and intracellular factors.
| Target | Drug | Clinical trialb | Reference | |||||
|---|---|---|---|---|---|---|---|---|
| Target or mechanism type | Target or mechanism | Organsa | Drug Name | Mechanism | Class | Disease | Phase | Reference/Trial identifierc |
| LOXd | LOXL2d | Liver, Kidney, Lung, Heart, Skin, Gut | β-aminopropionitrile (BAPN) | Inhibitor | Small molecule | Cardiac fibrosis | Preclinical | Martinez-Martinez et al., 2016 |
| Simtuzumab (GS-6624) | Inhibitor | Monoclonal antibody | Liver fibrosis; IPFd | 2(completed); 2(terminated) | NCT01452308; NCT01769196 | |||
| ROSd | NOX1d/NOX4 | Liver, Kidney, Lung, Heart, Pancreas, Skin | GM-CT-01 | Inhibitor | Polymer | Liver fibrosis | Preclinical | Traber and Zomer, 2013 |
| GR-MD-02 | Inhibitor | Polymer | Liver fibrosis | 2(completed) | NCT02421094 | |||
| GCS-100 | Inhibitor | Polymer | Renal fibrosis | 2(completed) | NCT01843790 | |||
| ROS | GKT137831 | Inhibitor | Small molecule | Liver fibrosis | Preclinical | Aoyama et al., 2012 | ||
| N-acetylcysteine* | Inhibitor | Small molecule | IPF | Approved| Preclinical | Demedts et al., 2005; Zhang et al., 2014 | |||
| Mitoquinone | Inhibitor | Small molecule | Liver fibrosis | Preclinical | Vilaseca et al., 2017 | |||
| Salvianolic acid B* | Inhibitor | Small molecule | Liver fibrosis; Renal fibrosis; IPF | Preclinical | Liu et al., 2002, 2016; Pan et al., 2011 | |||
| Resveratrol* | Inhibitor | Small molecule | Liver fibrosis | 3(completed) | NCT02030977 | |||
| Vitamin (mimic) | Liver, Kidney, Lung, Heart, Pancreas, Skin, Gut | Pyridoxamine | Inhibitor | Small molecule | Renal fibrosis | 2(completed) | NCT00320060 | |
| α-tocopherol | Inhibitor | Small molecule | IPF | Approved| Preclinical | Deger et al., 2007 | |||
| Collagen (mimic) | Liver, Kidney, Lung, Skin | IW001 | Inhibitor | Collagen | IPF | 1(completed) | NCT01199887 | |
Drug belongs to monomer extracted from natural products.
Organs that had study report of corresponding targets in fibrosis treatment.
Clinical trial resource are from http://Clinicaltrials.gov.
Trial Identifier is the clinical trail identifier of corresponding drug.
LOX, lysyl oxidase; LOXL2, lysyl oxidase homolog 2; IPF, idiopathic pulmonary fibrosis; ROS, reactive oxygen species; NOX1, NADPH oxidase 1.
Multi-component drugs used for fibrosis
Differed from single-component drugs that target a single protein or other simple targets, multi-component drugs contain more than one active ingredient. Traditional Chinese medicines (TCM) therapies, usually appeared as herbal formula, have been studied for thousands of years as multi-component drugs (Wang et al., 2012). Nowadays, single compound acting on multiple targets and multiple compounds acting on multiple targets are popular strategies in drug development (Hopkins, 2008). Fibrosis includes numerous complicated pathological pathways. Multi-component drugs, aiming at different targets, have the advantage in modulating these pathways simultaneously and producing synergistic effects. Moreover, multi-component drugs are expected to provide great resources for discovering new effective drug molecules. Many studies have revealed the pharmacology of multi-component drugs in the fibrosis treatment (Feng et al., 2009; Yang et al., 2009; Li and Kan, 2017) (Table 4). For example, Fuzhenghuayu capsule (FZHY), a well-known multi-component drug for treating liver fibrosis, inhibits liver fibrosis and improves liver function in patients via inhibition of nuclear factor kappa-B kinase subunit β/nuclear factor κF and TGF-β signaling (Liu et al., 2005). Another emerging multi-component drug, Qishenyiqi (QSYQ), is under phase II clinical trial for ischemic heart failure. QSYQ attenuates cardiac fibrosis via IL-6/STAT3 and TNF-α/nuclear factor kappa-light-chain-enhancer of activated B cells (NFκB) signalings and anti-apoptosis activities (Wang et al., 2017). Multi-component drugs act on different physiological reactions associated with fibrosis, such as inflammation and angiogenesis, leading to a systematic improvement of disease. Qushi Huayu Decoction (QHD) is a multitargeting drug that alleviates fibrosis by reducing ROS via the induction of glutathione and modulating lipid metabolism and gut barrier function (Feng et al., 2017).
Table 4.
Multi-component drugs.
| Drug | Clinical triala | Reference | ||
|---|---|---|---|---|
| Drug Name | Mechanism | Disease | Phase | Reference/Trial identifierb |
| Fuzhenghuayu capsule (FZHY) | TGF-βc/MMP-2c | Liver fibrosis | 2(completed); 4(recruiting) | NCT00854087; NCT02241616 |
| Qishenyiqi (QSYQ) | TNFc/TGF-β/β-Catenin | Ischemic heart failure | 2(recruiting) | NCT02875639 |
| Qushi Huayu Decoction (QHD) | ROSc | Liver fibrosis | Preclinical | Feng et al., 2017 |
| Herbal compound 861 (Cpd 861) | TGF-β/MMP-1/TIMP-1c | Liver fibrosis | Preclinical | Hou et al., 2016 |
| Xiao-Chai-Hu Tang (XCHT) | IL-6c/TNF-α/Bax protein | Liver cancer | 2(completed) | NCT00040898; Zhou et al., 2012 |
| Dahuangzhechong pill (DHZCP) | α-SMAc/TNF-α/IL-13/p38 MAPKc/ERKc | Liver fibrosis | Preclinical | Cai et al., 2010 |
| Han-dan-gan-le | ROS/collagen | Liver fibrosis | Preclinical | Li et al., 1998 |
| Qianggan-Rongxian Decoction | − | Liver fibrosis | Preclinical | Li et al., 2008 |
| Yi-gan-kang granule | type I collagen/TIMP-1 | Liver fibrosis | Preclinical | Yao et al., 2005 |
| Ginkgo biloba extract | TGF-β | Liver fibrosis | Preclinical | Ding et al., 2005 |
| Rosa laevigata Michx (RLTS) | ROS/CYP2Elc/TGF-β/SMAD/FAKc-PI3Kc-Aktc-p70S6Kc/MAPK | Liver fibrosis | Preclinical | Dong et al., 2015 |
| Liuweiwuling (LWWL) tablets | TGF-β/SMAD/ NF-κBc | Liver fibrosis | Preclinical | Liu et al., 2017 |
| Xuefuzhuyu (XFZY) decoction | HIF-Yc/DDAHc/ADMAc/VEGFc | Liver fibrosis | Preclinical | Zhou et al., 2014 |
| Diwu Yanggan (DWYG) | TGF-β/BMP-7c | Liver fibrosis | Preclinical | Shen et al., 2014 |
| Ocimum gratissimum extracts (OGEs) | ROS/α-SMA | Liver fibrosis | Preclinical | Chiu et al., 2014 |
| Yin-Chiao-San (YCS) | ROS/TNF-α | IPFc | Preclinical | Yen et al., 2007 |
| Renshen pingfei decoction | TGF-β/SMAD3 | IPF | Preclinical | Chen et al., 2016 |
| Hu-qi-yin | TGF-β | IPF | Preclinical | Zhou et al., 2007 |
| Decoction for Strengthening Qi and Replenishing Lung (DSQRL) | – | IPF | Preclinical | Zhang et al., 2008 |
| Modified Kushen Gancao Formula (mKG) | TGF-β/IL-6/IL-17A | IPF | Preclinical | Gao et al., 2016 |
| Sho-seiryu-to (TJ-19) | ROS | IPF | Preclinical | Yang et al., 2010 |
| Hochu-ekki-to (TJ-41) | IL-5/IL-4/IFN-γ | IPF | Preclinical | Tajima et al., 2007 |
| Shenlong Decoction | MMsP/TIMPs | IPF | Preclinical | Lu et al., 2010 |
| Yupingfeng | HMGB1c/TGF-β | IPF | Preclinical | Cui et al., 2015 |
| Danggui–Buxue–Tang (DBTG) | TNF-α/TGF-β | IPF | Preclinical | Lv et al., 2012 |
Clinical trial resource are from http://Clinicaltrials.gov.
Trial Identifier is the clinical trail identifier of corresponding drug.
TGF-β, transforming growth factor-β; MMP-2, matrix metalloproteinase 2; TNF, tumor necrosis factor; ROS, reactive oxygen species; TIMP, tissue inhibitor of metalloproteinase; IL-6, interleukin-6; α-SMA, α-smooth muscle actin; MAPK, mitogen-activated protein kinase; ERK, extracellular signal-regulated kinase; PDGF-BB, platelet-derived growth factor-BB; IPF, idiopathic pulmonary fibrosis; HMGB1, high mobility group box 1; CYP2E1, cytochrome P450 2E1; FAK, focal adhesion kinase; PI3K, phosphatidylinositol-3-kinase; Akt, amino kinase terminal; p70S6K, 70-kDa ribosomal S6 Kinase; NF-κB, nuclear factor kappa-light-chain-enhancer of activated B cells; HIF-α, hypoxia inducible factors; DDAH, dimethylarginine dimethylaminohydrolase; ADMA, asymmetric dimethylarginine; VEGF, vascular endothelial grow factor; BMP-7, bone morphogenetic protein 7.
With multiple targets being discovered, it becomes apparent that more common targets will be shared across many fibrotic diseases with common mechanisms, though some proteins will not express in special conditions. Meanwhile, there will be more chance for drug repositioning, which indicate common drugs will be shared across different targets andfibroproliferative diseases.
Perspective
Fibrosis is a common pathological process in many diseases, causing a great clinical burden in recent years. The development of state-of-the-art technologies facilitate discovery of fibrosis therapies. Multi-omics analysis provides a more convenient and systematic way for researching on disease mechanisms (Fernandes and Husi, 2017). The seamless combination of traditional transcriptomics approaches with emerging technologies, including proteomics (Ordureau et al., 2014), metabolomics (Shah et al., 2012), and metagenomics (Jiao et al., 2017), will offer unprecedented opportunities to precisely elucidating and dissecting fibrosis mechanisms. Nowadays, the application of cryo-electron microscopy (cryo-EM) in macromolecular structure determination make it easier to identify drug targets (Zheng et al., 2015). Compared with traditional X-ray crystallography, cryo-EM has advantage in determining the structure of more complex and flexible receptors (Huang et al., 2016; Zhang et al., 2017). Finally, with the advent of the era of big data, artificial intelligence technology, especially deep learning, provides more accurate algorithms for drug repositioning (LeCun et al., 2015; Alaimo et al., 2016). The continuous development and application of the above technologies and methods will make it possible to identify and discover more common mechanisms, targets and drugs in fibrosis.
Author contributions
RZ and LZ conceived and designed the project. Each author has contributed significantly to the submitted work. XL drafted the manuscript. LZ, BW, MY, and RZ revised the manuscript. All authors read and approved the final manuscript.
Conflict of interest statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest. The reviewer XT and handling Editor declared their shared affiliation.
Acknowledgments
This work was supported by National Natural Science Foundation of China 31200986 (to RZ), 41530105 (to RZ), Natural Science Foundation, the Shanghai Committee of Science and Technology 16ZR1449800 (to RZ), a departmental start-up fund (to LZ), the Peter and Tommy Fund, Inc., Buffalo, NY (to LZ), and Funds from the University at Buffalo Community of Excellence in Genome, Environment and Microbiome (GEM) (to LZ). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Glossary
Abbreviations
- ECM
extracellular matrix
- IPF
idiopathic pulmonary fibrosis
- NAFLD
non-alcoholic fatty liver disease
- TGF-β
transforming growth factor-β
- IL-6
interleukin-6
- SSc
systemic sclerosis
- PDGF
platelet derived growth factor
- EMT
epithelial-mesenchymal transition
- HSC
hepatic stellate cell
- MMPs
matrix metalloproteinases
- α-SMA
α-smooth muscle actin
- HGF
hepatocyte growth factor
- TNF
tumor necrosis factor
- STAT3
signal transducer and activator of transcription 3
- TIMPs
tissue inhibitor of metalloproteinases
- Hh signaling
hedgehog signaling
- mTOR
mechanistic target of rapamycin
- MAPK
mitogen-activated protein kinase
- PPAR-γ
peroxisome proliferator activated receptor γ
- FXR
farnesoid-X receptor
- LOXL2
lysyl oxidase homolog 2
- ROS
reactive oxygen species
- CKD
chronic kidney disease
- ET
endothelin
- BMPER
BMP endothelial cell precursor-derived regulator
- TCM
traditional Chinese medicines
- FZHY
Fuzhenghuayu capsule
- NFκB
nuclear factor kappa-light-chain-enhancer of activated B cells
- QSYQ
Qishenyiqi
- QHD
Qushi Huayu Decoction.
- cryo-EM
cryo-electron microscopy.
References
- Akhmetshina A., Venalis P., Dees C., Busch N., Zwerina J., Schett G., et al. (2009). Treatment with imatinib prevents fibrosis in different preclinical models of systemic sclerosis and induces regression of established fibrosis. Arthritis Rheum. 60, 219–224. 10.1002/art.24186 [DOI] [PubMed] [Google Scholar]
- Alaimo S., Giugno R., Pulvirenti A. (2016). Recommendation techniques for drug-target interaction prediction and drug repositioning. Methods Mol. Biol. 1415, 441–462. 10.1007/978-1-4939-3572-7_23 [DOI] [PubMed] [Google Scholar]
- Ali A. H., Carey E. J., Lindor K. D. (2015). Recent advances in the development of farnesoid X receptor agonists. Ann Transl Med 3:5. 10.3978/j.issn.2305-5839.2014.12.06 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alkhouri N., Carter-Kent C., Feldstein A. E. (2011). Apoptosis in nonalcoholic fatty liver disease: diagnostic and therapeutic implications. Expert Rev. Gastroenterol. Hepatol. 5, 201–212. 10.1586/egh.11.6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen J. T., Spiteri M. A. (2002). Growth factors in idiopathic pulmonary fibrosis: relative roles. Respir. Res. 3:13. 10.1186/rr162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aoyama T., Paik Y. H., Watanabe S., Laleu B., Gaggini F., Fioraso-Cartier L., et al. (2012). Nicotinamide adenine dinucleotide phosphate oxidase in experimental liver fibrosis: GKT137831 as a novel potential therapeutic agent. Hepatology 56, 2316–2327. 10.1002/hep.25938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Apte M. V., Pirola R. C., Wilson J. S. (2012). Pancreatic stellate cells: a starring role in normal and diseased pancreas. Front. Physiol. 3:344. 10.3389/fphys.2012.00344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkinson J. M., Pullen N., Da Silva-Lodge M., Williams L., Johnson T. S. (2015). Inhibition of thrombin-activated fibrinolysis inhibitor increases survival in experimental kidney fibrosis. J. Am. Soc. Nephrol. 26, 1925–1937. 10.1681/ASN.2014030303 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baghdasaryan A., Claudel T., Gumhold J., Silbert D., Adorini L., Roda A., et al. (2011). Dual farnesoid X receptor/TGR5 agonist INT-767 reduces liver injury in the Mdr2-/- (Abcb4-/-) mouse cholangiopathy model by promoting biliary HCO(-)(3) output. Hepatology 54, 1303–1312. 10.1002/hep.24537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barreyro F. J., Holod S., Finocchietto P. V., Camino A. M., Aquino J. B., Avagnina A., et al. (2015). The pan-caspase inhibitor Emricasan (IDN-6556) decreases liver injury and fibrosis in a murine model of non-alcoholic steatohepatitis. Liver Int. 35, 953–966. 10.1111/liv.12570 [DOI] [PubMed] [Google Scholar]
- Biernacka A., Dobaczewski M., Frangogiannis N. G. (2011). TGF-beta signaling in fibrosis. Growth Factors 29, 196–202. 10.3109/08977194.2011.595714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Block E. T., Cronstein B. N. (2010). Interferon-gamma inhibits adenosine A2A receptor function in hepatic stellate cells by STAT1-mediated repression of adenylyl cyclase. Int. J. Interferon Cytokine Mediat. Res. 2010, 113–126. 10.2147/ijicmr.s8860 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogatkevich G. S., Highland K. B., Akter T., Silver R. M. (2012). The PPARgamma agonist rosiglitazone is antifibrotic for scleroderma lung fibroblasts: mechanisms of action and differential racial effects. Pulm. Med. 2012:545172. 10.1155/2012/545172 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breyer M. D., Susztak K. (2016). The next generation of therapeutics for chronic kidney disease. Nat. Rev. Drug Discov. 15, 568–588. 10.1038/nrd.2016.67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhling F., Rocken C., Brasch F., Hartig R., Yasuda Y., Saftig P., et al. (2004). Pivotal role of cathepsin K in lung fibrosis. Am. J. Pathol. 164, 2203–2216. 10.1016/S0002-9440(10)63777-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cai H. B., Sun X. G., Liu Z. F., Liu Y. W., Tang J., Liu Q., et al. (2010). Effects of dahuangzhechong pills on cytokines and mitogen activated protein kinase activation in rats with hepatic fibrosis. J. Ethnopharmacol. 132, 157–164. 10.1016/j.jep.2010.08.019 [DOI] [PubMed] [Google Scholar]
- Caiafa R. O., Vinuesa A. S., Izquierdo R. S., Brufau B. P., Ayuso Colella J. R., Molina C. N. (2013). Retroperitoneal fibrosis: role of imaging in diagnosis and follow-up. Radiographics 33, 535–552. 10.1148/rg.332125085 [DOI] [PubMed] [Google Scholar]
- Calleja M. A., Vieites J. M., Montero-Melendez T., Torres M. I., Faus M. J., Gil A., et al. (2013). The antioxidant effect of beta-caryophyllene protects rat liver from carbon tetrachloride-induced fibrosis by inhibiting hepatic stellate cell activation. Br. J. Nutr. 109, 394–401. 10.1017/S0007114512001298 [DOI] [PubMed] [Google Scholar]
- Chau B. N., Xin C., Hartner J., Ren S., Castano A. P., Linn G., et al. (2012). MicroRNA-21 promotes fibrosis of the kidney by silencing metabolic pathways. Sci. Transl. Med. 4:121ra118. 10.1126/scitranslmed.3003205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chavez E., Castro-Sanchez L., Shibayama M., Tsutsumi V., Moreno M. G., Muriel P. (2012). Sulfasalazine prevents the increase in TGF-beta, COX-2, nuclear NFkappaB translocation and fibrosis in CCl4-induced liver cirrhosis in the rat. Hum. Exp. Toxicol. 31, 913–920. 10.1177/0960327112438928 [DOI] [PubMed] [Google Scholar]
- Chen F., Wang P. L., Fan X. S., Yu J. H., Zhu Y., Zhu Z. H. (2016). Effect of Renshen Pingfei Decoction, a traditional Chinese prescription, on IPF induced by Bleomycin in rats and regulation of TGF-beta1/Smad3. J. Ethnopharmacol. 186, 289–297. 10.1016/j.jep.2016.03.051 [DOI] [PubMed] [Google Scholar]
- Chen G., Chen H., Wang C., Peng Y., Sun L., Liu H., et al. (2012). Rapamycin ameliorates kidney fibrosis by inhibiting the activation of mTOR signaling in interstitial macrophages and myofibroblasts. PLoS ONE 7:e33626. 10.1371/journal.pone.0033626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen S. J., Yuan W., Mori Y., Levenson A., Trojanowska M., Varga J. (1999). Stimulation of type I collagen transcription in human skin fibroblasts by TGF-beta: involvement of Smad 3. J. Invest. Dermatol. 112, 49–57. 10.1046/j.1523-1747.1999.00477.x [DOI] [PubMed] [Google Scholar]
- Chen Y., Yang S., Yao W., Zhu H., Xu X., Meng G., et al. (2014). Prostacyclin analogue beraprost inhibits cardiac fibroblast proliferation depending on prostacyclin receptor activation through a TGF beta-Smad signal pathway. PLoS ONE 9:e98483. 10.1371/journal.pone.0098483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheresh P., Kim S. J., Tulasiram S., Kamp D. W. (2013). Oxidative stress and pulmonary fibrosis. Biochim. Biophys. Acta 1832, 1028–1040. 10.1016/j.bbadis.2012.11.021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiu Y. W., Chao P. Y., Tsai C. C., Chiou H. L., Liu Y. C., Hung C. C., et al. (2014). Ocimum gratissimum is effective in prevention against liver fibrosis in vivo and in vitro. Am. J. Chin. Med. 42, 833–852. 10.1142/S0192415X14500530 [DOI] [PubMed] [Google Scholar]
- Choi K., Lee K., Ryu S. W., Im M., Kook K. H., Choi C. (2012). Pirfenidone inhibits transforming growth factor-beta1-induced fibrogenesis by blocking nuclear translocation of Smads in human retinal pigment epithelial cell line ARPE-19. Mol. Vis. 18, 1010–1020. [PMC free article] [PubMed] [Google Scholar]
- Corbel M., Caulet-Maugendre S., Germain N., Molet S., Lagente V., Boichot E. (2001). Inhibition of bleomycin-induced pulmonary fibrosis in mice by the matrix metalloproteinase inhibitor batimastat. J. Pathol. 193, 538–545. 10.1002/path.826 [DOI] [PubMed] [Google Scholar]
- Couluris M., Kinder B. W., Xu P., Gross-King M., Krischer J., Panos R. J. (2012). Treatment of idiopathic pulmonary fibrosis with losartan: a pilot project. Lung 190, 523–527. 10.1007/s00408-012-9410-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cui W., Li L., Li D., Mo X., Zhou W., Zhang Z., et al. (2015). Total glycosides of Yupingfeng protects against bleomycin-induced pulmonary fibrosis in rats associated with reduced high mobility group box 1 activation and epithelial-mesenchymal transition. Inflamm. Res. 64, 953–961. 10.1007/s00011-015-0878-x [DOI] [PubMed] [Google Scholar]
- Daniels C. E., Lasky J. A., Limper A. H., Mieras K., Gabor E., Schroeder D. R., et al. (2010). Imatinib treatment for idiopathic pulmonary fibrosis: randomized placebo-controlled trial results. Am. J. Respir. Crit. Care Med. 181, 604–610. 10.1164/rccm.200906-0964OC [DOI] [PubMed] [Google Scholar]
- de Meijer V. E., Sverdlov D. Y., Popov Y., Le H. D., Meisel J. A., Nose V., et al. (2010). Broad-spectrum matrix metalloproteinase inhibition curbs inflammation and liver injury but aggravates experimental liver fibrosis in mice. PLoS ONE 5:e11256. 10.1371/journal.pone.0011256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Minicis S., Marzioni M., Saccomanno S., Rychlicki C., Agostinelli L., Trozzi L., et al. (2012). Cellular and molecular mechanisms of hepatic fibrogenesis leading to liver cancer. Transl. Gastrointest. Cancer 1, 88–94. 10.3978/j.issn.2224-4778.2011.12.05 [DOI] [Google Scholar]
- Deger Y., Yur F., Ertekin A., Mert N., Dede S., Mert H. (2007). Protective effect of alpha-tocopherol on oxidative stress in experimental pulmonary fibrosis in rats. Cell Biochem. Funct. 25, 633–637. 10.1002/cbf.1362 [DOI] [PubMed] [Google Scholar]
- Demedts M., Behr J., Buhl R., Costabel U., Dekhuijzen R., Jansen H. M., et al. (2005). High-dose acetylcysteine in idiopathic pulmonary fibrosis. N. Engl. J. Med. 353, 2229–2242. 10.1056/NEJMoa042976 [DOI] [PubMed] [Google Scholar]
- Depner C. M., Philbrick K. A., Jump D. B. (2013). Docosahexaenoic acid attenuates hepatic inflammation, oxidative stress, and fibrosis without decreasing hepatosteatosis in a Ldlr(-/-) mouse model of western diet-induced nonalcoholic steatohepatitis. J. Nutr. 143, 315–323. 10.3945/jn.112.171322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ding J., Yu J., Wang C., Hu W., Li D., Luo Y., et al. (2005). Ginkgo biloba extract alleviates liver fibrosis induced by CCl in rats. Liver Int. 25, 1224–1232. 10.1111/j.1478-3231.2005.01169.x [DOI] [PubMed] [Google Scholar]
- Dinwiddie R. (2005). Anti-inflammatory therapy in cystic fibrosis. J. Cyst. Fibros 4(Suppl. 2), 45–48. 10.1016/j.jcf.2005.05.010 [DOI] [PubMed] [Google Scholar]
- Dong D., Yin L., Qi Y., Xu L., Peng J. (2015). Protective effect of the total saponins from Rosa laevigata michx fruit against carbon tetrachloride-induced liver fibrosis in rats. Nutrients 7, 4829–4850. 10.3390/nu7064829 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ezquerro I. J., Lasarte J. J., Dotor J., Castilla-Cortazar I., Bustos M., Penuelas I., et al. (2003). A synthetic peptide from transforming growth factor β type III receptor inhibits liver fibrogenesis in rats with carbon tetrachloride liver injury. Cytokine 22, 12–20. 10.1016/s1043-4666(03)00101-7 [DOI] [PubMed] [Google Scholar]
- Fallowfield J. A. (2011). Therapeutic targets in liver fibrosis. Am. J. Physiol. Gastrointest. Liver Physiol. 300, G709–G715. 10.1152/ajpgi.00451.2010 [DOI] [PubMed] [Google Scholar]
- Fan G. P., Wang W., Zhao H., Cai L., Zhang P. D., Yang Z. H., et al. (2015). Pharmacological inhibition of focal adhesion kinase attenuates cardiac fibrosis in mice cardiac fibroblast and post-myocardial-infarction models. Cell. Physiol. Biochem. 37, 515–526. 10.1159/000430373 [DOI] [PubMed] [Google Scholar]
- Feng Q., Liu W., Baker S. S., Li H., Chen C., Liu Q., et al. (2017). Multi-targeting therapeutic mechanisms of the Chinese herbal medicine QHD in the treatment of non-alcoholic fatty liver disease. Oncotarget 8, 27820–27838. 10.18632/oncotarget.15482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Feng Y., Cheung K. F., Wang N., Liu P., Nagamatsu T., Tong Y. (2009). Chinese medicines as a resource for liver fibrosis treatment. Chin. Med. 4:16. 10.1186/1749-8546-4-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernandes M., Husi H. (2017). Establishment of a integrative multi-omics expression database CKDdb in the context of chronic kidney disease (CKD). Sci. Rep. 7:40367. 10.1038/srep40367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fielding C. A., Jones G. W., McLoughlin R. M., McLeod L., Hammond V. J., Uceda J., et al. (2014). Interleukin-6 signaling drives fibrosis in unresolved inflammation. Immunity 40, 40–50. 10.1016/j.immuni.2013.10.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fine A., Goldstein R. H. (1987). The effect of transforming growth factor-beta on cell proliferation and collagen formation by lung fibroblasts. J. Biol. Chem. 262, 3897–3902. [PubMed] [Google Scholar]
- Fiorucci S., Antonelli E., Distrutti E., Severino B., Fiorentina R., Baldoni M., et al. (2004). PAR1 antagonism protects against experimental liver fibrosis. Role of proteinase receptors in stellate cell activation. Hepatology 39, 365–375. 10.1002/hep.20054 [DOI] [PubMed] [Google Scholar]
- Fukumori T., Takenaka Y., Yoshii T., Kim H. R., Hogan V., Inohara H., et al. (2003). CD29 and CD7 mediate galectin-3-induced type II T-cell apoptosis. Cancer Res. 63, 8302–8311. [PubMed] [Google Scholar]
- Gao Y., Lu J., Zhang Y., Chen Y., Gu Z., Jiang X. (2013). Baicalein attenuates bleomycin-induced pulmonary fibrosis in rats through inhibition of miR-21. Pulm. Pharmacol. Ther. 26, 649–654. 10.1016/j.pupt.2013.03.006 [DOI] [PubMed] [Google Scholar]
- Gao Y., Yao L. F., Zhao Y., Wei L. M., Guo P., Yu M., et al. (2016). The chinese herbal medicine formula mKG suppresses pulmonary fibrosis of mice induced by bleomycin. Int. J. Mol. Sci. 17:238. 10.3390/ijms17020238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghosh A. K., Bhattacharyya S., Wei J., Kim S., Barak Y., Mori Y., et al. (2009). Peroxisome proliferator-activated receptor-gamma abrogates Smad-dependent collagen stimulation by targeting the p300 transcriptional coactivator. FASEB J. 23, 2968–2977. 10.1096/fj.08-128736 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giannandrea M., Parks W. C. (2014). Diverse functions of matrix metalloproteinases during fibrosis. Dis. Model. Mech. 7, 193–203. 10.1242/dmm.012062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill S. E., Huizar I., Bench E. M., Sussman S. W., Wang Y., Khokha R., et al. (2010). Tissue inhibitor of metalloproteinases 3 regulates resolution of inflammation following acute lung injury. Am. J. Pathol. 176, 64–73. 10.2353/ajpath.2010.090158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez-Arroyo J., Sakagami M., Syed A. A., Farkas L., Van Tassell B., Kraskauskas D., et al. (2015). Iloprost reverses established fibrosis in experimental right ventricular failure. Eur. Respir. J. 45, 449–462. 10.1183/09031936.00188013 [DOI] [PubMed] [Google Scholar]
- Gonzalez E. O., Boix V., Deltoro M. G., Aldeguer J. L., Portilla J., Montero M., et al. (2014). The effects of Maraviroc on liver fibrosis in HIV/HCV co-infected patients. J. Int. AIDS Soc. 17(4 Suppl. 3):19643. 10.7448/IAS.17.4.19643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gu L., Tao X., Xu Y., Han X., Qi Y., Xu L., et al. (2016). Dioscin alleviates BDL- and DMN-induced hepatic fibrosis via Sirt1/Nrf2-mediated inhibition of p38 MAPK pathway. Toxicol. Appl. Pharmacol. 292, 19–29. 10.1016/j.taap.2015.12.024 [DOI] [PubMed] [Google Scholar]
- Gulati A., Jabbour A., Ismail T. F., Guha K., Khwaja J., Raza S., et al. (2013). Association of fibrosis with mortality and sudden cardiac death in patients with nonischemic dilated cardiomyopathy. JAMA 309, 896–908. 10.1001/jama.2013.1363 [DOI] [PubMed] [Google Scholar]
- Hashimoto S., Gon Y., Takeshita I., Maruoka S., Horie T. (2001). IL-4 and IL-13 induce myofibroblastic phenotype of human lung fibroblasts through c-Jun NH2-terminal kinase-dependent pathway. J. Allergy Clin. Immunol. 107, 1001–1008. 10.1067/mai.2001.114702 [DOI] [PubMed] [Google Scholar]
- He W., Dai C., Li Y., Zeng G., Monga S. P., Liu Y. (2009). Wnt/beta-catenin signaling promotes renal interstitial fibrosis. J. Am. Soc. Nephrol. 20, 765–776. 10.1681/ASN.2008060566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson N. C., Arnold T. D., Katamura Y., Giacomini M. M., Rodriguez J. D., McCarty J. H., et al. (2013). Selective αv integrin depletion identifies a core, targetable molecular pathway that regulates fibrosis across solid organs. Nat. Med. 19, 1617–1624. 10.1038/nm.3282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hinz B., Phan S. H., Thannickal V. J., Galli A., Bochaton-Piallat M. L., Gabbiani G. (2007). The myofibroblast: one function, multiple origins. Am. J. Pathol. 170, 1807–1816. 10.2353/ajpath.2007.070112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hopkins A. L. (2008). Network pharmacology: the next paradigm in drug discovery. Nat. Chem. Biol. 4, 682–690. 10.1038/nchembio.118 [DOI] [PubMed] [Google Scholar]
- Horton M. R., Santopietro V., Mathew L., Horton K. M., Polito A. J., Liu M. C., et al. (2012). Thalidomide for the treatment of cough in idiopathic pulmonary fibrosis: a randomized trial. Ann. Intern. Med. 157, 398–406. 10.7326/0003-4819-157-6-201209180-00003 [DOI] [PubMed] [Google Scholar]
- Hou F., Liu R., Liu X., Cui L., Wen Y., Yan S., et al. (2016). Attenuation of liver fibrosis by herbal compound 861 via upregulation of BMP-7/Smad signaling in the bile duct ligation model rat. Mol. Med. Rep. 13, 4335–4342. 10.3892/mmr.2016.5071 [DOI] [PubMed] [Google Scholar]
- Huan C., Yang T., Liang J., Xie T., Cheng L., Liu N., et al. (2015). Methylation-mediated BMPER expression in fibroblast activation in vitro and lung fibrosis in mice in vivo. Sci. Rep. 5:14910. 10.1038/srep14910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang X., Luan B., Wu J., Shi Y. (2016). An atomic structure of the human 26S proteasome. Nat. Struct. Mol. Biol. 23, 778–785. 10.1038/nsmb.3273 [DOI] [PubMed] [Google Scholar]
- Hutchinson J., Fogarty A., Hubbard R., McKeever T. (2015). Global incidence and mortality of idiopathic pulmonary fibrosis: a systematic review. Eur. Respir. J. 46, 795–806. 10.1183/09031936.00185114 [DOI] [PubMed] [Google Scholar]
- Huuskes B. M., Wise A. F., Cox A. J., Lim E. X., Payne N. L., Kelly D. J., et al. (2015). Combination therapy of mesenchymal stem cells and serelaxin effectively attenuates renal fibrosis in obstructive nephropathy. FASEB J. 29, 540–553. 10.1096/fj.14-254789 [DOI] [PubMed] [Google Scholar]
- Iannitti R. G., Napolioni V., Oikonomou V., De Luca A., Galosi C., Pariano M., et al. (2016). IL-1 receptor antagonist ameliorates inflammasome-dependent inflammation in murine and human cystic fibrosis. Nat. Commun. 7:10791. 10.1038/ncomms10791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai K., Takaoka A. (2006). Comparing antibody and small-molecule therapies for cancer. Nat. Rev. Cancer 6, 714–727. 10.1038/nrc1913 [DOI] [PubMed] [Google Scholar]
- Jacobson G., Bhatia S., Smith B. J., Button A. M., Bodeker K., Buatti J. (2013). Randomized trial of pentoxifylline and vitamin E vs standard follow-up after breast irradiation to prevent breast fibrosis, evaluated by tissue compliance meter. Int. J. Radiat. Oncol. Biol. Phys. 85, 604–608. 10.1016/j.ijrobp.2012.06.042 [DOI] [PubMed] [Google Scholar]
- Jiao N., Baker S. S., Chapa-Rodriguez A., Liu W., Nugent C. A., Tsompana M., et al. (2017). Suppressed hepatic bile acid signalling despite elevated production of primary and secondary bile acids in NAFLD. Gut. [Epub ahead of print]. 10.1136/gutjnl-2017-314307 [DOI] [PubMed] [Google Scholar]
- Jirouskova M., Zbodakova O., Gregor M., Chalupsky K., Sarnova L., Hajduch M., et al. (2012). Hepatoprotective effect of MMP-19 deficiency in a mouse model of chronic liver fibrosis. PLoS ONE 7:e46271. 10.1371/journal.pone.0046271 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson T. S., Fisher M., Haylor J. L., Hau Z., Skill N. J., Jones R., et al. (2007). Transglutaminase inhibition reduces fibrosis and preserves function in experimental chronic kidney disease. J. Am. Soc. Nephrol. 18, 3078–3088. 10.1681/ASN.2006070690 [DOI] [PubMed] [Google Scholar]
- Kaneshige T., Saida Y., Tanaka R., Soda A., Fukushima A., Ida N., et al. (2007). Effect of long-term administration of a prostacyclin analogue (beraprost sodium) on myocardial fibrosis in Dahl rats. J. Vet. Med. Sci. 69, 1271–1276. 10.1292/jvms.69.1271 [DOI] [PubMed] [Google Scholar]
- Kawano H., Kimura-Kuroda J., Komuta Y., Yoshioka N., Li H. P., Kawamura K., et al. (2012). Role of the lesion scar in the response to damage and repair of the central nervous system. Cell Tissue Res. 349, 169–180. 10.1007/s00441-012-1336-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan R., Sheppard R. (2006). Fibrosis in heart disease: understanding the role of transforming growth factor-beta in cardiomyopathy, valvular disease and arrhythmia. Immunology 118, 10–24. 10.1111/j.1365-2567.2006.02336.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khanna D., Albera C., Fischer A., Khalidi N., Raghu G., Chung L., et al. (2016). An Open-label, phase II study of the safety and tolerability of pirfenidone in patients with scleroderma-associated interstitial Lung Disease: the LOTUSS trial. J. Rheumatol. 43, 1672–1679. 10.3899/jrheum.151322 [DOI] [PubMed] [Google Scholar]
- Khanna D., Saggar R., Mayes M. D., Abtin F., Clements P. J., Maranian P., et al. (2011). A one-year, phase I/IIa, open-label pilot trial of imatinib mesylate in the treatment of systemic sclerosis-associated active interstitial lung disease. Arthritis Rheum. 63, 3540–3546. 10.1002/art.30548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim D., Kim W. R., Kim H. J., Therneau T. M. (2013). Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology 57, 1357–1365. 10.1002/hep.26156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim L., Kim D. K., Yang W. I., Shin D. H., Jung I. M., Park H. K., et al. (2008). Overexpression of transforming growth factor-beta 1 in the valvular fibrosis of chronic rheumatic heart disease. J. Korean Med. Sci. 23, 41–48. 10.3346/jkms.2008.23.1.41 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King T. E., Jr., Bradford W. Z., Castro-Bernardini S., Fagan E. A., Glaspole I., Glassberg M. K., et al. (2014). A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N. Engl. J. Med. 370, 2083–2092. 10.1056/NEJMoa1402582 [DOI] [PubMed] [Google Scholar]
- Kitagawa K., Wada T., Furuichi K., Hashimoto H., Ishiwata Y., Asano M., et al. (2004). Blockade of CCR2 ameliorates progressive fibrosis in kidney. Am. J. Pathol. 165, 237–246. 10.1016/S0002-9440(10)63292-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koh R. Y., Lim C. L., Uhal B. D., Abdullah M., Vidyadaran S., Ho C. C., et al. (2015). Inhibition of transforming growth factor-beta via the activin receptor-like kinase-5 inhibitor attenuates pulmonary fibrosis. Mol. Med. Rep. 11, 3808–3813. 10.3892/mmr.2015.3193 [DOI] [PubMed] [Google Scholar]
- Kuwano K., Kunitake R., Maeyama T., Hagimoto N., Kawasaki M., Matsuba T., et al. (2001). Attenuation of bleomycin-induced pneumopathy in mice by a caspase inhibitor. Am. J. Physiol. Lung Cell. Mol. Physiol. 280, L316–L325. [DOI] [PubMed] [Google Scholar]
- Lagares D., Busnadiego O., Garcia-Fernandez R. A., Kapoor M., Liu S., Carter D. E., et al. (2012). Inhibition of focal adhesion kinase prevents experimental lung fibrosis and myofibroblast formation. Arthritis Rheum. 64, 1653–1664. 10.1002/art.33482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lan H. Y. (2011). Diverse roles of TGF-β/Smads in renal fibrosis and inflammation. Int. J. Biol. Sci. 7, 1056–1067. 10.7150/ijbs.7.1056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawrance I. C., Wu F., Leite A. Z., Willis J., West G. A., Fiocchi C., et al. (2003). A murine model of chronic inflammation-induced intestinal fibrosis down-regulated by antisense NF-κB. Gastroenterology 125, 1750–1761. 10.1053/j.gastro.2003.08.027 [DOI] [PubMed] [Google Scholar]
- LeCun Y., Bengio Y., Hinton G. (2015). Deep learning. Nature 521, 436–444. 10.1038/nature14539 [DOI] [PubMed] [Google Scholar]
- Lerch M. M., Halangk W. (2006). Human pancreatitis and the role of cathepsin B. Gut 55, 1228–1230. 10.1136/gut.2006.092114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li B., Wang J. H. (2011). Fibroblasts and myofibroblasts in wound healing: force generation and measurement. J. Tissue Viability 20, 108–120. 10.1016/j.jtv.2009.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C. H., Pan L. H., Yang Z. W., Li C. Y., Xu W. X. (2008). Preventive effect of Qianggan-Rongxian Decoction on rat liver fibrosis. World J. Gastroenterol. 14, 3569–3573. 10.3748/wjg.14.3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li C. X., Li L., Lou J., Yang W. X., Lei T. W., Li Y. H., et al. (1998). The protective effects of traditional Chinese medicine prescription, han-dan-gan-le, on CCl4-induced liver fibrosis in rats. Am. J. Chin. Med. 26, 325–332. 10.1142/S0192415X98000361 [DOI] [PubMed] [Google Scholar]
- Li L. C., Kan L. D. (2017). Traditional Chinese medicine for pulmonary fibrosis therapy: progress and future prospects. J. Ethnopharmacol. 198, 45–63. 10.1016/j.jep.2016.12.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li L. C., Li J., Gao J. (2014). Functions of galectin-3 and its role in fibrotic diseases. J. Pharmacol. Exp. Ther. 351, 336–343. 10.1124/jpet.114.218370 [DOI] [PubMed] [Google Scholar]
- Lin J., Zhu X., Chade A. R., Jordan K. L., Lavi R., Daghini E., et al. (2009). Monocyte chemoattractant proteins mediate myocardial microvascular dysfunction in swine renovascular hypertension. Arterioscler. Thromb. Vasc. Biol. 29, 1810–1816. 10.1161/ATVBAHA.109.190546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu A., Gao X., Zhang Q., Cui L. (2013). Cathepsin B inhibition attenuates cardiac dysfunction and remodeling following myocardial infarction by inhibiting the NLRP3 pathway. Mol. Med. Rep. 8, 361–366. 10.3892/mmr.2013.1507 [DOI] [PubMed] [Google Scholar]
- Liu G., Friggeri A., Yang Y., Milosevic J., Ding Q., Thannickal V. J., et al. (2010). miR-21 mediates fibrogenic activation of pulmonary fibroblasts and lung fibrosis. J. Exp. Med. 207, 1589–1597. 10.1084/jem.20100035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu H., Dong F., Li G., Niu M., Zhang C., Han Y., et al. (2017). Liuweiwuling tablets attenuate BDL-induced hepatic fibrosis via modulation of TGF-beta/Smad and NF-kappaB signaling pathways. J. Ethnopharmacol. 210, 232–241. 10.1016/j.jep.2017.08.029 [DOI] [PubMed] [Google Scholar]
- Liu M., Xu Y., Han X., Yin L., Xu L., Qi Y., et al. (2015). Dioscin alleviates alcoholic liver fibrosis by attenuating hepatic stellate cell activation via the TLR4/MyD88/NF-kappaB signaling pathway. Sci. Rep. 5:18038. 10.1038/srep18038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P., Hu Y. Y., Liu C., Xu L. M., Liu C. H., Sun K. W., et al. (2005). Multicenter clinical study on Fuzhenghuayu capsule against liver fibrosis due to chronic hepatitis B. World J. Gastroenterol. 11, 2892–2899. 10.3748/wjg.v11.i19.2892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu P., Hu Y. Y., Liu C., Zhu D. Y., Xue H. M., Xu Z. Q., et al. (2002). Clinical observation of salvianolic acid B in treatment of liver fibrosis in chronic hepatitis B. World J. Gastroenterol. 8, 679–685. 10.3748/wjg.v8.i4.679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Q., Chu H., Ma Y., Wu T., Qian F., Ren X., et al. (2016). Salvianolic acid B attenuates experimental pulmonary fibrosis through inhibition of the TGF-beta signaling pathway. Sci. Rep. 6:27610. 10.1038/srep27610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Binz J., Numerick M. J., Dennis S., Luo G., Desai B., et al. (2003). Hepatoprotection by the farnesoid X receptor agonist GW4064 in rat models of intra- and extrahepatic cholestasis. J. Clin. Invest. 112, 1678–1687. 10.1172/JCI18945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu X. D., Pang L. J., Wang L. L., Nan M. H., Ma Z. (2010). Effects of Chinese herbal medicine Shenlong Decoction on mRNA expressions of matrix metalloproteinase-2 and tissue inhibitor of metalloproteinase-1 in lung tissue of rats with pulmonary fibrosis induced by bleomycin. Zhong Xi Yi Jie He Xue Bao 8, 961–967. 10.3736/jcim20101008 [DOI] [PubMed] [Google Scholar]
- Lv J., Zhao Z., Chen Y., Wang Q., Tao Y., Yang L., et al. (2012). The chinese herbal decoction danggui buxue tang inhibits angiogenesis in a rat model of liver fibrosis. Evid. Based Complement. Alternat. Med. 2012:284963. 10.1155/2012/284963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mahmoud M. F., Swefy S. E., Hasan R. A., Ibrahim A. (2014). Role of cannabinoid receptors in hepatic fibrosis and apoptosis associated with bile duct ligation in rats. Eur. J. Pharmacol. 742, 118–124. 10.1016/j.ejphar.2014.08.021 [DOI] [PubMed] [Google Scholar]
- Makarev E., Izumchenko E., Aihara F., Wysocki P. T., Zhu Q., Buzdin A., et al. (2016). Common pathway signature in lung and liver fibrosis. Cell Cycle 15, 1667–1673. 10.1080/15384101.2016.1152435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maldonado F., Kottom T., Limper A. (2009). PXS-25, a Mannose-6-phosphate derivative, is effective in decreasing the production of extracellular matrix by TGF-beta stimulated fibroblasts. Am. Thoracic. Soc. 179:A3471 10.1164/ajrccm-conference.2009.179.1 [DOI] [Google Scholar]
- Manitsopoulos N., Kotanidou A., Magkou C., Ninou I., Tian X., Aidinis V., et al. (2015). Treprostinil administration attenuates bleomycin-induced lung fibrosis in mice. Eur. Respir. Soc.. 46:PA3837 10.1183/13993003.congress-2015.PA3837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinez-Martinez E., Rodriguez C., Galan M., Miana M., Jurado-Lopez R., Bartolome M. V., et al. (2016). The lysyl oxidase inhibitor (beta-aminopropionitrile) reduces leptin profibrotic effects and ameliorates cardiovascular remodeling in diet-induced obesity in rats. J. Mol. Cell. Cardiol. 92, 96–104. 10.1016/j.yjmcc.2016.01.012 [DOI] [PubMed] [Google Scholar]
- Mathioudakis A., Chatzimavridou-Grigoriadou V., Evangelopoulou E., Mathioudakis G. (2013). Vasoactive intestinal Peptide inhaled agonists: potential role in respiratory therapeutics. Hippokratia 17, 12–16. [PMC free article] [PubMed] [Google Scholar]
- Matsumura Y., Sakaida I., Uchida K., Kimura T., Ishihara T., Okita K. (1997). Prolyl 4-hydroxylase inhibitor (HOE 077) inhibits pig serum-induced rat liver fibrosis by preventing stellate cell activation. J. Hepatol. 27, 185–192. [DOI] [PubMed] [Google Scholar]
- Meng X. M., Nikolic-Paterson D. J., Lan H. Y. (2016). TGF-beta: the master regulator of fibrosis. Nat. Rev. Nephrol. 12, 325–338. 10.1038/nrneph.2016.48 [DOI] [PubMed] [Google Scholar]
- Meng X. M., Tang P. M., Li J., Lan H. Y. (2015). TGF-beta/Smad signaling in renal fibrosis. Front. Physiol. 6:82 10.3389/fphys.2015.00082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitragotri S., Burke P. A., Langer R. (2014). Overcoming the challenges in administering biopharmaceuticals: formulation and delivery strategies. Nat. Rev. Drug Discov. 13, 655–672. 10.1038/nrd4363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira R. K. (2007). Hepatic stellate cells and liver fibrosis. Arch. Pathol. Lab. Med. 131, 1728–1734. 10.1043/1543-2165(2007)131[1728%3AHSCALF]2.0.CO%3B2 [DOI] [PubMed] [Google Scholar]
- Moss R. B., Mayer-Hamblett N., Wagener J., Daines C., Hale K., Ahrens R., et al. (2005). Randomized, double-blind, placebo-controlled, dose-escalating study of aerosolized interferon gamma-1b in patients with mild to moderate cystic fibrosis lung disease. Pediatr. Pulmonol. 39, 209–218. 10.1002/ppul.20152 [DOI] [PubMed] [Google Scholar]
- Muir A. J., Sylvestre P. B., Rockey D. C. (2006). Interferon gamma-1b for the treatment of fibrosis in chronic hepatitis C infection. J. Viral Hepat. 13, 322–328. 10.1111/j.1365-2893.2005.00689.x [DOI] [PubMed] [Google Scholar]
- Murray L. A., Zhang H., Oak S. R., Coelho A. L., Herath A., Flaherty K. R., et al. (2014). Targeting interleukin-13 with tralokinumab attenuates lung fibrosis and epithelial damage in a humanized SCID idiopathic pulmonary fibrosis model. Am. J. Respir. Cell Mol. Biol. 50, 985–994. 10.1165/rcmb.2013-0342OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nadadur R., Umar S., Matori H., Iorga A., Mai D., Amjedi M., et al. (2012). Genistein therapy reverses lung inflammation and fibrosis during severe pulmonary hypertension through estrogen receptor beta. Biophys. J. 102:140a 10.1016/j.bpj.2011.11.772 [DOI] [Google Scholar]
- Okunieff P., Augustine E., Hicks J. E., Cornelison T. L., Altemus R. M., Naydich B. G., et al. (2004). Pentoxifylline in the treatment of radiation-induced fibrosis. J. Clin. Oncol. 22, 2207–2213. 10.1200/JCO.2004.09.101 [DOI] [PubMed] [Google Scholar]
- Omenetti A., Porrello A., Jung Y., Yang L., Popov Y., Choi S. S., et al. (2008). Hedgehog signaling regulates epithelial-mesenchymal transition during biliary fibrosis in rodents and humans. J. Clin. Invest. 118, 3331–3342. 10.1172/JCI35875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ordureau A., Sarraf S. A., Duda D. M., Heo J. M., Jedrychowski M. P., Sviderskiy V. O., et al. (2014). Quantitative proteomics reveal a feedforward mechanism for mitochondrial PARKIN translocation and ubiquitin chain synthesis. Mol. Cell 56, 360–375. 10.1016/j.molcel.2014.09.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Overington J. P., Al-Lazikani B., Hopkins A. L. (2006). How many drug targets are there? Nat. Rev. Drug Discov. 5, 993–996. 10.1038/nrd2199 [DOI] [PubMed] [Google Scholar]
- Pan R. H., Xie F. Y., Chen H. M., Xu L. Z., Wu X. C., Xu L. L., et al. (2011). Salvianolic acid B reverses the epithelial-to-mesenchymal transition of HK-2 cells that is induced by transforming growth factor-beta. Arch. Pharm. Res. 34, 477–483. 10.1007/s12272-011-0317-7 [DOI] [PubMed] [Google Scholar]
- Parish J. M., Rosenow E. C., III. (2002). Mediastinal granuloma and mediastinal fibrosis. Semin. Respir. Crit. Care Med. 23, 135–143. 10.1055/s-2002-25302 [DOI] [PubMed] [Google Scholar]
- Peinado H., Del Carmen Iglesias-de la Cruz M., Olmeda D., Csiszar K., Fong K. S., Vega S., et al. (2005). A molecular role for lysyl oxidase-like 2 enzyme in snail regulation and tumor progression. EMBO J. 24, 3446–3458. 10.1038/sj.emboj.7600781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pellicoro A., Ramachandran P., Iredale J. P., Fallowfield J. A. (2014). Liver fibrosis and repair: immune regulation of wound healing in a solid organ. Nat. Rev. Immunol. 14, 181–194. 10.1038/nri3623 [DOI] [PubMed] [Google Scholar]
- Radbill B. D., Gupta R., Ramirez M. C., DiFeo A., Martignetti J. A., Alvarez C. E., et al. (2011). Loss of matrix metalloproteinase-2 amplifies murine toxin-induced liver fibrosis by upregulating collagen I expression. Dig. Dis. Sci. 56, 406–416. 10.1007/s10620-010-1296-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raghu G., Brown K. K., Costabel U., Cottin V., du Bois R. M., Lasky J. A., et al. (2008). Treatment of idiopathic pulmonary fibrosis with etanercept: an exploratory, placebo-controlled trial. Am. J. Respir. Crit. Care Med. 178, 948–955. 10.1164/rccm.200709-1446OC [DOI] [PubMed] [Google Scholar]
- Raghu G., Chen S. Y., Yeh W. S., Maroni B., Li Q., Lee Y. C., et al. (2014). Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001–11. Lancet Respir Med 2, 566–572. 10.1016/S2213-2600(14)70101-8 [DOI] [PubMed] [Google Scholar]
- Raimundo K., Chang E., Broder M. S., Alexander K., Zazzali J., Swigris J. J. (2016). Clinical and economic burden of idiopathic pulmonary fibrosis: a retrospective cohort study. BMC Pulm. Med. 16:2. 10.1186/s12890-015-0165-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Redente E. F., Keith R. C., Janssen W., Henson P. M., Ortiz L. A., Downey G. P., et al. (2014). Tumor necrosis factor-alpha accelerates the resolution of established pulmonary fibrosis in mice by targeting profibrotic lung macrophages. Am. J. Respir. Cell Mol. Biol. 50, 825–837. 10.1165/rcmb.2013-0386OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif S., Lang A., Lindquist J. N., Yata Y., Gabele E., Scanga A., et al. (2003). The role of focal adhesion kinase-phosphatidylinositol 3-kinase-akt signaling in hepatic stellate cell proliferation and type I collagen expression. J. Biol. Chem. 278, 8083–8090. 10.1074/jbc.M212927200 [DOI] [PubMed] [Google Scholar]
- Reiter T., Ritter O., Prince M. R., Nordbeck P., Wanner C., Nagel E., et al. (2012). Minimizing risk of nephrogenic systemic fibrosis in cardiovascular magnetic resonance. J. Cardiovasc. Magn. Reson. 14:31. 10.1186/1532-429X-14-31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ritter C., Zhang S., Finch J. L., Liapis H., Suarez E., Ferder L., et al. (2014). Cardiac and renal effects of atrasentan in combination with enalapril and paricalcitol in uremic rats. Kidney Blood Press. Res. 39, 340–352. 10.1159/000355811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rockey D. C., Bell P. D., Hill J. A. (2015). Fibrosis–a common pathway to organ injury and failure. N. Engl. J. Med. 372, 1138–1149. 10.1056/NEJMra1300575 [DOI] [PubMed] [Google Scholar]
- Salas A. L., Montezuma T. D., Farina G. G., Reyes-Esparza J., Rodriguez-Fragoso L. (2008). Genistein modifies liver fibrosis and improves liver function by inducing uPA expression and proteolytic activity in CCl4-treated rats. Pharmacology 81, 41–49. 10.1159/000107968 [DOI] [PubMed] [Google Scholar]
- Samad M. A., Kim U. K., Kang J. J., Ke Q., Kang P. M. (2015). Endothelin A receptor antagonist, atrasentan, attenuates renal and cardiac dysfunction in Dahl salt-hypertensive rats in a blood pressure independent manner. PLoS ONE 10:e0121664. 10.1371/journal.pone.0121664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samuel C. S., Bodaragama H., Chew J. Y., Widdop R. E., Royce S. G., Hewitson T. D. (2014). Serelaxin is a more efficacious antifibrotic than enalapril in an experimental model of heart disease. Hypertension 64, 315–322. 10.1161/HYPERTENSIONAHA.114.03594 [DOI] [PubMed] [Google Scholar]
- Sangaralingham S. J., Wang B. H., Huang L., Kumfu S., Ichiki T., Krum H., et al. (2016). Cardiorenal fibrosis and dysfunction in aging: imbalance in mediators and regulators of collagen. Peptides 76, 108–114. 10.1016/j.peptides.2016.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawant K. V., Poluri K. M., Dutta A. K., Sepuru K. M., Troshkina A., Garofalo R. P., et al. (2016). Chemokine CXCL1 mediated neutrophil recruitment: role of glycosaminoglycan interactions. Sci. Rep. 6:33123. 10.1038/srep33123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sebe A., Leivonen S. K., Fintha A., Masszi A., Rosivall L., Kahari V. M., et al. (2008). Transforming growth factor-beta-induced alpha-smooth muscle cell actin expression in renal proximal tubular cells is regulated by p38beta mitogen-activated protein kinase, extracellular signal-regulated protein kinase1,2 and the Smad signalling during epithelial-myofibroblast transdifferentiation. Nephrol. Dial. Transplant 23, 1537–1545. 10.1093/ndt/gfm789 [DOI] [PubMed] [Google Scholar]
- Seki E., De Minicis S., Gwak G. Y., Kluwe J., Inokuchi S., Bursill C. A., et al. (2009). CCR1 and CCR5 promote hepatic fibrosis in mice. J. Clin. Invest. 119, 1858–1870. 10.1172/jci37444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shah S. H., Kraus W. E., Newgard C. B. (2012). Metabolomic profiling for the identification of novel biomarkers and mechanisms related to common cardiovascular diseases: form and function. Circulation 126, 1110–1120. 10.1161/CIRCULATIONAHA.111.060368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen X., Cheng S., Peng Y., Song H., Li H. (2014). Attenuation of early liver fibrosis by herbal compound “Diwu Yanggan” through modulating the balance between epithelial-to-mesenchymal transition and mesenchymal-to-epithelial transition. BMC Complement. Altern. Med. 14:418. 10.1186/1472-6882-14-418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skaria S. D., Yang J., Condos R., Smaldone G. C. (2015). Inhaled interferon and diffusion capacity in Idiopathic Pulmonary Fibrosis (IPF). Sarcoidosis Vasc. Diffuse Lung Dis. 32, 37–42. [PubMed] [Google Scholar]
- Smith M. R., Gangireddy S. R., Narala V. R., Hogaboam C. M., Standiford T. J., Christensen P. J., et al. (2010). Curcumin inhibits fibrosis-related effects in IPF fibroblasts and in mice following bleomycin-induced lung injury. Am. J. Physiol. Lung Cell. Mol. Physiol. 298, L616–L625. 10.1152/ajplung.00002.2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stenstrom M., Nyhlen H. C., Torngren M., Liberg D., Sparre B., Tuvesson H., et al. (2016). Paquinimod reduces skin fibrosis in tight skin 1 mice, an experimental model of systemic sclerosis. J. Dermatol. Sci. 83, 52–59. 10.1016/j.jdermsci.2016.04.006 [DOI] [PubMed] [Google Scholar]
- Sun X., Liu Y., Li C., Wang X., Zhu R., Liu C., et al. (2017). Recent advances of curcumin in the prevention and treatment of renal fibrosis. Biomed Res. Int. 2017:2418671. 10.1155/2017/2418671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tada S., Iwamoto H., Nakamuta M., Sugimoto R., Enjoji M., Nakashima Y., et al. (2001). A selective ROCK inhibitor, Y27632, prevents dimethylnitrosamine-induced hepatic fibrosis in rats. J. Hepatol. 34, 529–536. 10.1016/S0168-8278(00)00059-3 [DOI] [PubMed] [Google Scholar]
- Tajima S., Bando M., Yamasawa H., Ohno S., Moriyama H., Terada M., et al. (2007). Preventive effect of hochu-ekki-to, a Japanese herbal medicine, on bleomycin-induced lung injury in mice. Respirology 12, 814–822. 10.1111/j.1440-1843.2007.01146.x [DOI] [PubMed] [Google Scholar]
- Takemasa A., Ishii Y., Fukuda T. (2012). A neutrophil elastase inhibitor prevents bleomycin-induced pulmonary fibrosis in mice. Eur. Respir. J. 40, 1475–1482. 10.1183/09031936.00127011 [DOI] [PubMed] [Google Scholar]
- Tanaka T., Ogawa M., Suzuki J., Sekinishi A., Itai A., Hirata Y., et al. (2012). Inhibition of IkappaB phosphorylation prevents load-induced cardiac dysfunction in mice. Am. J. Physiol. Heart Circ. Physiol. 303, H1435–H1445. 10.1152/ajpheart.00290.2012 [DOI] [PubMed] [Google Scholar]
- Tang W. W., Ulich T. R., Lacey D. L., Hill D. C., Qi M., Kaufman S. A., et al. (1996). Platelet-derived growth factor-BB induces renal tubulointerstitial myofibroblast formation and tubulointerstitial fibrosis. Am. J. Pathol. 148, 1169–1180. [PMC free article] [PubMed] [Google Scholar]
- Taniyama Y., Morishita R., Aoki M., Hiraoka K., Yamasaki K., Hashiya N., et al. (2002). Angiogenesis and antifibrotic action by hepatocyte growth factor in cardiomyopathy. Hypertension 40, 47–53. 10.1161/01.hyp.0000020755.56955.bf [DOI] [PubMed] [Google Scholar]
- Thannickal V. J., Lee D. Y., White E. S., Cui Z., Larios J. M., Chacon R., et al. (2003). Myofibroblast differentiation by transforming growth factor-beta1 is dependent on cell adhesion and integrin signaling via focal adhesion kinase. J. Biol. Chem. 278, 12384–12389. 10.1074/jbc.M208544200 [DOI] [PubMed] [Google Scholar]
- Thum T., Gross C., Fiedler J., Fischer T., Kissler S., Bussen M., et al. (2008). MicroRNA-21 contributes to myocardial disease by stimulating MAP kinase signalling in fibroblasts. Nature 456, 980–984. 10.1038/nature07511 [DOI] [PubMed] [Google Scholar]
- Traber P. G., Zomer E. (2013). Therapy of experimental NASH and fibrosis with galectin inhibitors. PLoS ONE 8:e83481. 10.1371/journal.pone.0083481 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsai J. H., Liu J. Y., Wu T. T., Ho P. C., Huang C. Y., Shyu J. C., et al. (2008). Effects of silymarin on the resolution of liver fibrosis induced by carbon tetrachloride in rats. J. Viral Hepat. 15, 508–514. 10.1111/j.1365-2893.2008.00971.x [DOI] [PubMed] [Google Scholar]
- Tulek B., Kiyan E., Toy H., Kiyici A., Narin C., Suerdem M. (2011). Anti-inflammatory and anti-fibrotic effects of sirolimus on bleomycin-induced pulmonary fibrosis in rats. Clin. Invest. Med. 34:E341. 10.25011/cim.v34i6.15894 [DOI] [PubMed] [Google Scholar]
- van Dijk F., Olinga P., Poelstra K., Beljaars L. (2015). Targeted therapies in liver fibrosis: combining the best parts of platelet-derived growth factor BB and interferon gamma. Front. Med. 2:72. 10.3389/fmed.2015.00072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbeke L., Mannaerts I., Schierwagen R., Govaere O., Klein S., Vander Elst I., et al. (2016). FXR agonist obeticholic acid reduces hepatic inflammation and fibrosis in a rat model of toxic cirrhosis. Sci. Rep. 6:33453. 10.1038/srep33453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilaseca M., Garcia-Caldero H., Lafoz E., Ruart M., Lopez-Sanjurjo C. I., Murphy M. P., et al. (2017). Mitochondria-targeted antioxidant mitoquinone deactivates human and rat hepatic stellate cells and reduces portal hypertension in cirrhotic rats. Liver Int. 37, 1002–1012. 10.1111/liv.13436 [DOI] [PubMed] [Google Scholar]
- Vittal R., Fisher A., Gu H., Mickler E. A., Panitch A., Lander C., et al. (2013). Peptide-mediated inhibition of mitogen-activated protein kinase-activated protein kinase-2 ameliorates bleomycin-induced pulmonary fibrosis. Am. J. Respir. Cell Mol. Biol. 49, 47–57. 10.1165/rcmb.2012-0389OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang H., Lafdil F., Wang L., Yin S., Feng D., Gao B. (2011). Tissue inhibitor of metalloproteinase 1 (TIMP-1) deficiency exacerbates carbon tetrachloride-induced liver injury and fibrosis in mice: involvement of hepatocyte STAT3 in TIMP-1 production. Cell Biosci. 1:14. 10.1186/2045-3701-1-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Q., Usinger W., Nichols B., Gray J., Xu L., Seeley T. W., et al. (2011). Cooperative interaction of CTGF and TGF-beta in animal models of fibrotic disease. Fibrogenesis Tissue Repair 4:4. 10.1186/1755-1536-4-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang W., Zhou P. H., Xu C. G., Zhou X. J., Hu W., Zhang J. (2015). Baicalein attenuates renal fibrosis by inhibiting inflammation via down-regulating NF-kappaB and MAPK signal pathways. J. Mol. Histol. 46, 283–290. 10.1007/s10735-015-9621-8 [DOI] [PubMed] [Google Scholar]
- Wang Y. R., Tian F. L., Yan M. X., Fan J. H., Wang L. Y., Kuang R. G., et al. (2016). Sulfasalazine inhibits inflammation and fibrogenesis in pancreas via NF-kappaB signaling pathway in rats with oxidative stress-induced pancreatic injury. Drug Des. Devel. Ther. 10, 1743–1751. 10.2147/DDDT.S107679 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- Wang Y., Fan X., Qu H., Gao X., Cheng Y. (2012). Strategies and techniques for multi-component drug design from medicinal herbs and traditional Chinese medicine. Curr. Top. Med. Chem. 12, 1356–1362. 10.2174/156802612801319034 [DOI] [PubMed] [Google Scholar]
- Wang Y., Lin W., Li C., Singhal S., Jain G., Zhu L., et al. (2017). Multipronged therapeutic effects of chinese herbal medicine qishenyiqi in the treatment of acute myocardial infarction. Front. Pharmacol. 8:98. 10.3389/fphar.2017.00098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weingartner S., Zerr P., Tomcik M., Palumbo-Zerr K., Distler A., Dees C., et al. (2012). Pomalidomide is effective for prevention and treatment of experimental skin fibrosis. Ann. Rheum. Dis. 71, 1895–1899. 10.1136/annrheumdis-2012-201784 [DOI] [PubMed] [Google Scholar]
- Wenzke K. E., Cantemir-Stone C., Zhang J., Marsh C. B., Huang K. (2012). Identifying common genes and networks in multi-organ fibrosis. AMIA Jt Summits Transl. Sci. Proc. 2012, 106–115. [PMC free article] [PubMed] [Google Scholar]
- Wilkins B. S., Radia D., Woodley C., Farhi S. E., Keohane C., Harrison C. N. (2013). Resolution of bone marrow fibrosis in a patient receiving JAK1/JAK2 inhibitor treatment with ruxolitinib. Haematologica 98, 1872–1876. 10.3324/haematol.2013.095109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witek R. P., Stone W. C., Karaca F. G., Syn W. K., Pereira T. A., Agboola K. M., et al. (2009). Pan-caspase inhibitor VX-166 reduces fibrosis in an animal model of nonalcoholic steatohepatitis. Hepatology 50, 1421–1430. 10.1002/hep.23167 [DOI] [PubMed] [Google Scholar]
- Wong M. G., Panchapakesan U., Qi W., Silva D. G., Chen X. M., Pollock C. A. (2011). Cation-independent mannose 6-phosphate receptor inhibitor (PXS25) inhibits fibrosis in human proximal tubular cells by inhibiting conversion of latent to active TGF-beta1. Am. J. Physiol. Renal Physiol. 301, F84–F93. 10.1152/ajprenal.00287.2010 [DOI] [PubMed] [Google Scholar]
- Wynn T. A. (2008). Cellular and molecular mechanisms of fibrosis. J. Pathol. 214, 199–210. 10.1002/path.2277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., Yates C. C., Lockyer P., Xie L., Bevilacqua A., He J., et al. (2014). MMI-0100 inhibits cardiac fibrosis in myocardial infarction by direct actions on cardiomyocytes and fibroblasts via MK2 inhibition. J. Mol. Cell. Cardiol. 77, 86–101. 10.1016/j.yjmcc.2014.09.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu L., Yin L., Tao X., Qi Y., Han X., Xu Y., et al. (2017). Dioscin, a potent ITGA5 inhibitor, reduces the synthesis of collagen against liver fibrosis: Insights from SILAC-based proteomics analysis. Food Chem. Toxicol. 107(Pt A), 318–328. 10.1016/j.fct.2017.07.014 [DOI] [PubMed] [Google Scholar]
- Yang C. Q., Sun P. Y., Ding D. Z., Moriuchi H., Ishitsuka Y., Irikura M., et al. (2010). The ethical Kampo formulation Sho-seiryu-to (TJ-19) prevents bleomycin-induced pulmonary fibrosis in rats. Biol. Pharm. Bull. 33, 1438–1442. 10.1248/bpb.33.1438 [DOI] [PubMed] [Google Scholar]
- Yang J., Cui Y., Kolb M. (2009). How useful is traditional herbal medicine for pulmonary fibrosis? Respirology 14, 1082–1091. 10.1111/j.1440-1843.2009.01644.x [DOI] [PubMed] [Google Scholar]
- Yang J., Savvatis K., Kang J. S., Fan P., Zhong H., Schwartz K., et al. (2016). Targeting LOXL2 for cardiac interstitial fibrosis and heart failure treatment. Nat. Commun. 7:13710. 10.1038/ncomms13710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L., Chan C. C., Kwon O. S., Liu S., McGhee J., Stimpson S. A., et al. (2006). Regulation of peroxisome proliferator-activated receptor-gamma in liver fibrosis. Am. J. Physiol. Gastrointest. Liver Physiol. 291, G902–G911. 10.1152/ajpgi.00124.2006 [DOI] [PubMed] [Google Scholar]
- Yao X. X., Jiang S. L., Tang Y. W., Yao D. M., Yao X. (2005). Efficacy of Chinese medicine Yi-gan-kang granule in prophylaxis and treatment of liver fibrosis in rats. World J. Gastroenterol. 11, 2583–2590. 10.3748/wjg.v11.i17.2583 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yen F. L., Wu T. H., Liao C. W., Lin C. C. (2007). A kampo medicine, Yin-Chiao-san, prevents bleomycin-induced pulmonary injury in rats. Phytother. Res. 21, 251–258. 10.1002/ptr.2056 [DOI] [PubMed] [Google Scholar]
- Yin L., Qi Y., Xu Y., Xu L., Han X., Tao X., et al. (2017). Dioscin inhibits HSC-T6 cell migration via adjusting SDC-4 expression: insights from iTRAQ-based quantitative proteomics. Front. Pharmacol. 8:665. 10.3389/fphar.2017.00665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zeybel M., Hardy T., Robinson S. M., Fox C., Anstee Q. M., Ness T., et al. (2015). Differential DNA methylation of genes involved in fibrosis progression in non-alcoholic fatty liver disease and alcoholic liver disease. Clin. Epigenetics 7:25. 10.1186/s13148-015-0056-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang H. Q., Yau Y. F., Wong M. S., Man O. Y., He Y. Y., Chan N., et al. (2008). Chinese medicine formula DSQRL versus glucocorticoids for the treatment of experimental pulmonary fibrosis. J. Ethnopharmacol. 116, 318–324. 10.1016/j.jep.2007.11.039 [DOI] [PubMed] [Google Scholar]
- Zhang L., Fu X. H., Yu Y., Shui R. H., Li C., Zeng H. Y., et al. (2015). Treatment with CA-074Me, a Cathepsin B inhibitor, reduces lung interstitial inflammation and fibrosis in a rat model of polymyositis. Lab. Invest. 95, 65–77. 10.1038/labinvest.2014.135 [DOI] [PubMed] [Google Scholar]
- Zhang L., He Y. L., Li Q. Z., Hao X. H., Zhang Z. F., Yuan J. X., et al. (2014). N-acetylcysteine alleviated silica-induced lung fibrosis in rats by down-regulation of ROS and mitochondrial apoptosis signaling. Toxicol. Mech. Methods 24, 212–219. 10.3109/15376516.2013.879974 [DOI] [PubMed] [Google Scholar]
- Zhang S., Wang J., Liu Q., Harnish D. C. (2009). Farnesoid X receptor agonist WAY-362450 attenuates liver inflammation and fibrosis in murine model of non-alcoholic steatohepatitis. J. Hepatol. 51, 380–388. 10.1016/j.jhep.2009.03.025 [DOI] [PubMed] [Google Scholar]
- Zhang X., Han X., Yin L., Xu L., Qi Y., Xu Y., et al. (2015a). Potent effects of dioscin against liver fibrosis. Sci. Rep. 5:9713. 10.1038/srep09713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang X., Xu L., Yin L., Qi Y., Xu Y., Han X., et al. (2015b). Quantitative chemical proteomics for investigating the biomarkers of dioscin against liver fibrosis caused by CCl4 in rats. Chem. Commun. 51, 11064–11067. 10.1039/c4cc09160d [DOI] [PubMed] [Google Scholar]
- Zhang X., Yan C., Hang J., Finci L. I., Lei J., Shi Y. (2017). An atomic structure of the human spliceosome. Cell 169, 918 e914–929 e914. 10.1016/j.cell.2017.04.033 [DOI] [PubMed] [Google Scholar]
- Zhang Y. E. (2009). Non-Smad pathways in TGF-beta signaling. Cell Res. 19, 128–139. 10.1038/cr.2008.328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y., Edgley A. J., Cox A. J., Powell A. K., Wang B., Kompa A. R., et al. (2012). FT011, a new anti-fibrotic drug, attenuates fibrosis and chronic heart failure in experimental diabetic cardiomyopathy. Eur. J. Heart Fail. 14, 549–562. 10.1093/eurjhf/hfs011 [DOI] [PubMed] [Google Scholar]
- Zhang Z., Guo Y., Zhang S., Zhang Y., Wang Y., Ni W., et al. (2013). Curcumin modulates cannabinoid receptors in liver fibrosis in vivo and inhibits extracellular matrix expression in hepatic stellate cells by suppressing cannabinoid receptor type-1 in vitro. Eur. J. Pharmacol. 721, 133–140. 10.1016/j.ejphar.2013.09.042 [DOI] [PubMed] [Google Scholar]
- Zhao H., Chan-Li Y., Collins S. L., Zhang Y., Hallowell R. W., Mitzner W., et al. (2014). Pulmonary delivery of docosahexaenoic acid mitigates bleomycin-induced pulmonary fibrosis. BMC Pulm. Med. 14:64. 10.1186/1471-2466-14-64 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao X. K., Yu L., Cheng M. L., Che P., Lu Y. Y., Zhang Q., et al. (2017). Focal adhesion kinase regulates hepatic stellate cell activation and liver fibrosis. Sci. Rep. 7:4032. 10.1038/s41598-017-04317-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng H., Handing K. B., Zimmerman M. D., Shabalin I. G., Almo S. C., Minor W. (2015). X-ray crystallography over the past decade for novel drug discovery - where are we heading next? Expert Opin. Drug Discov. 10, 975–989. 10.1517/17460441.2015.1061991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhou X. M., Zhang G. C., Li J. X., Hou J. (2007). Inhibitory effects of Hu-qi-yin on the bleomycin-induced pulmonary fibrosis in rats. J. Ethnopharmacol. 111, 255–264. 10.1016/j.jep.2006.11.029 [DOI] [PubMed] [Google Scholar]
- Zhou Y. N., Sun M. Y., Mu Y. P., Yang T., Ning B. B., Ren S., et al. (2014). Xuefuzhuyu decoction inhibition of angiogenesis attenuates liver fibrosis induced by CCl(4) in mice. J. Ethnopharmacol. 153, 659–666. 10.1016/j.jep.2014.03.019 [DOI] [PubMed] [Google Scholar]
- Zhou Y. X., Qiu Y. Q., Xu L. Q., Guo J., Li L. J. (2012). Xiao-Chai-Hu Tang in treating model mice with D-galactosamine-induced liver injury. Afr. J. Tradit. Complement. Altern. Med. 9, 405–411. 10.4314/ajtcam.v9i3.16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu X. Y., Chade A. R., Krier J. D., Daghini E., Lavi R., Guglielmotti A., et al. (2009). The chemokine monocyte chemoattractant protein-1 contributes to renal dysfunction in swine renovascular hypertension. J. Hypertens. 27, 2063–2073. 10.1097/HJH.0b013e3283300192 [DOI] [PMC free article] [PubMed] [Google Scholar]