Abstract
AIM
To perform a meta-analysis on laparoscopic hepatectomy VS conventional liver resection for treating hepatolithiasis.
METHODS
We conducted a systematic literature search on PubMed, Embase, Web of Science and Cochrane Library, and undertook a meta-analysis to compare the efficacy and safety of laparoscopic hepatectomy VS conventional open liver resection for local hepatolithiasis in the left or right lobe. Intraoperative and postoperative outcomes (time, estimated blood loss, blood transfusion rate, postoperative intestinal function recovery time, length of hospital stay, postoperative complication rate, initial residual stone, final residual stone and stone recurrence) were analyzed systematically.
RESULTS
A comprehensive literature search retrieved 16 publications with a total of 1329 cases. Meta-analysis of these studies showed that the laparoscopic approach for hepatolithiasis was associated with significantly less intraoperative estimated blood loss [weighted mean difference (WMD): 61.56, 95% confidence interval (CI): 14.91-108.20, P = 0.01], lower blood transfusion rate [odds ratio (OR): 0.41, 95%CI: 0.22-0.79, P = 0.008], shorter intestinal function recovery time (WMD: 0.98, 95%CI: 0.47-1.48, P = 0.01), lower total postoperative complication rate (OR: 0.52, 95%CI: 0.39-0.70, P < 0.0001) and shorter stay in hospital (WMD: 3.32, 95%CI: 2.32-4.32, P < 0.00001). In addition, our results showed no significant differences between the two groups in operative time (WMD: 21.49, 95%CI: 0.27-43.24, P = 0.05), residual stones (OR: 0.79, 95%CI: 0.50-1.25, P = 0.31) and stone recurrence (OR: 0.34, 95%CI: 0.11-1.08, P = 0.07). Furthermore, with subgroups analysis, our results proved that the laparoscopic approach for hepatolithiasis in the left lateral lobe and left side could achieve satisfactory therapeutic effects.
CONCLUSION
The laparoscopic approach is safe and effective, with less intraoperative estimated blood loss, fewer postoperative complications, reduced length of hospital stay and shorter intestinal function recovery time than with conventional approaches.
Keywords: Hepatolithiasis, Laparoscopic hepatectomy, Conventional liver resection, Systematic review, Meta-analysis
Core tip: Application of the laparoscopic approach in symptomatic hepatolithiasis has gradually attracted more attention. However, its advantages over the open approach are still unclear. We analyzed 16 articles, comprising 1329 patients, to compare the two techniques for treating hepatolithiasis. We concluded that the laparoscopic approach is safe, effective and feasible for liver resection, with less intraoperative estimated blood loss, fewer postoperative complications, reduced length of hospital stay and shorter intestinal function recovery time than with conventional approaches.
INTRODUCTION
Hepatolithiasis is a gallstone disorder that involves the intrahepatic biliary duct (IHD), which may occur alone or accompanying extrahepatic gallstones. IHD stones may occur in any segments of the liver, and are particularly prevalent in the left lateral segment[1]. A recent report has shown that only 0.6%-1.3% of patients have intrahepatic stones in western countries, being more prevalent in eastern countries, especially Southeast Asia[2]. Hepatolithiasis over a long period of time may cause secondary cholangitis-originated cirrhosis and even cholangiocarcinoma[1,3], which can seriously affect the health and quality of life of patients.
There are many approaches to treat this disease, including percutaneous transhepatic cholangioscopic lithotripsy, IHD exploration and hepatectomy[4-7]. Among these treatment methods, hepatectomy is considered the most radical option for hepatolithiasis. In the past, open hepatectomy was preferred, with bile duct exploration and stone removal[8,9]. In recent years, with the development of laparoscopic technology and refinement of laparoscopic instruments, laparoscopic hepatectomy is now identified as a safe and flexible technique for hepatolithiasis.
However, few meta-analyses have evaluated the efficacy and safety of the laparoscopic approaches and open surgery that are routinely used in hepatolithiasis. It is unclear whether laparoscopic hepatectomy can be performed as effectively and safely as conventional hepatectomy or is superior to it in treating hepatolithiasis in the left or right hepatic lobes. Here, we performed a meta-analysis to assess the safety and efficacy of laparoscopic hepatectomy for treating intrahepatic bile duct stones. Furthermore, we evaluated left lateral sectionectomy and left hemihepatectomy by performing subgroups analysis.
MATERIALS AND METHODS
Search strategy and criteria
This meta-analysis was performed to compare laparoscopic hepatectomy and conventional open hepatectomy for hepatolithiasis. In January 2017, PubMed, Embase, Web of Science and Cochrane Library were searched for studies comparing laparoscopic hepatectomy with open liver resection for hepatolithiasis. There were no restrictions on publication date, type or language. Search terms were confined to Title/Abstract: “hepatolithiasis” OR “intrahepatic stone” AND “laparoscopic” OR “laparoendoscopic”. The reference lists of all selected articles were manually searched to determine if they should be included. Two reviewers browsed the titles and abstracts independently. Articles were included if they: (1) compared the outcomes of laparoscopic and open approaches for hepatolithiasis; and (2) reported at least some of the outcomes that we were interested in. Articles were excluded if they were submitted by the same authors or they reported duplicate data, to avoid duplication of patient populations. Editorials, case reports, conference abstracts and animal studies were excluded.
Data management
Data from the included studies were summarized by two of the authors independently. They were blinded to journals of publication, authors and study institutions of all available articles. Any disagreements between the reviewers were settled by the senior author. Perioperative outcomes were compared, including operative time, estimated blood loss (EBL), intraoperative transfusion, length of hospital stay (LOS), time to oral intake and postoperative complications. Outcomes regarding residual rate of intrahepatic stones containing initial residual, final residual and stone recurrence were also analyzed.
Quality assessment and statistical analysis
The level of evidence of these articles was estimated using the UK Cochrane Centre of Evidence (2009)[10]. The methodological quality of randomized controlled trials (RCTs) was assessed by the Cochrane Risk of Bias Tool[11]. The modified Newcastle-Ottawa scale was used to assess the quality of retrospective studies, which consists of three factors: patient selection, comparability of the study groups, and assessment of outcome[12-14]. The maximum total score on this scale was 9, and studies with scores ≥ 7 were defined as high quality[12].
All data were pooled with the Cochrane Collaboration’s Review Manager 5.3 (Cochrane Collaboration, Oxford, United Kingdom). Mean differences and 95% confidence intervals (CIs) were calculated to pool functional outcomes. Statistical heterogeneity among studies was assessed using the χ2 test with significance set at P < 0.1, and heterogeneity was quantified using the I2 statistic. A fixed-effects model was used routinely only if there was obvious heterogeneity among the included literature[15].
Subgroups and publication bias
Intrahepatic duct stones were located in different liver segments. Patients were subgrouped by type of operation, including left lateral sectionectomy (LLS), left hemihepatectomy (LH) and right hepatectomy (RH). Subgroup analysis was performed to compare outcomes resulting from different excision extension. Funnel plots were used to signify the publication bias. If outcomes were associated with significant heterogeneity, a random-effects model was used to minimize bias.
RESULTS
Characteristics of selected articles
The literature search identified 515 articles, 115 from PubMed, 187 from Embase and 213 from Web of Science; no studies were available in Cochrane Library (Figure 1). Of the 515 identified articles, 203 were duplications, 194 did not focus on hepatolithiasis, 40 were not comparative studies, 35 were case reports, 4 were conference abstracts and 2 were editorials. The full text of the remaining 36 articles was carefully reviewed. Twenty more were excluded, including 2 case reports, 5 that were not comparative studies and 13 that had no data of interest. Finally, 16 articles were included in our meta-analysis[16-31]. The characteristics of the selected articles are shown in Table 1.
Figure 1.
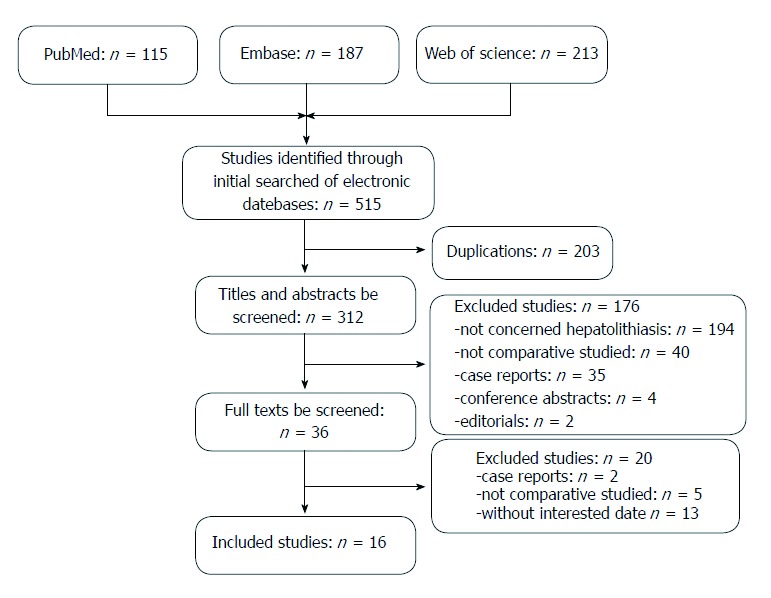
Flow chart showing study retrieval and selection process.
Table 1.
Characteristics of included studies
| Ref. | Level of evidence | Design |
Patient No. |
Location of stone | F/U, mo | Matching | Quality score | |
| LH | OH | LH/OH | ||||||
| Cai et al[16], 2007 | 3b | Re | 29 | 22 | L+R | 16.1/16.1 | 1,2,3,4,5 | 7 |
| Ding et al[17], 2015 | 2b | RCT | 49 | 49 | L | Perioperative | 1,2,3,5 | RCT |
| Li, H et al[18], 2008 | 4 | Re | 14 | 20 | L+R | Perioperative | 1,2 | 5 |
| Jin et al[19], 2015 | 3b | Re | 96 | 105 | L | 18-90 | 1,2,3,6,7 | 5 |
| Kim et al[20], 2015 | 3a | Re | 17 | 17 | R | 35/35 | 1,3,4,5 | 7 |
| Lee et al[21], 2014 | 3b | Re | 7 | 9 | L | 12.1/11.1 | 1,2,4,6 | 6 |
| Li, J et al[22], 2014 | 3b | Re | 35 | 40 | L+R | 41/41 | 1,2,3 | 6 |
| Li, Y et al[23], 2015 | 3b | Re | 23 | 22 | L+R | 15-51 | 1,2,3,6 | 5 |
| Namgoong et al[24], 2014 | 3b | Re | 37 | 112 | L | NA | 1,2,3,4 | 7 |
| Peng et al[25], 2016 | 3a | Re | 36 | 39 | L | 18.9/20 | 1,2,3,4 | 7 |
| Shin et al[26], 2015 | 3b | Re | 40 | 54 | L | 46.8/75.7 | 1,2,6 | 5 |
| Song et al[27], 2010 | 3b | Re | 7 | 10 | L | Perioperative | 1,2,3,4,5 | 7 |
| Tian et al[28], 2013 | 3b | Re | 116 | 78 | L+R | 29/29 | 1,2,4 | 6 |
| Tu et al[29], 2010 | 3b | Re | 28 | 33 | L | 17/17 | 1,2,3,4 | 7 |
| Ye et al[30], 2015 | 3a | Re | 46 | 51 | L | 33/33 | 1,2,3,4 | 7 |
| Zhou et al[31], 2013 | 3b | Re | 44 | 44 | L+R | 24/24 | 1,2,3,4,5,6,7 | 7 |
1: Age; 2: Sex; 3: Liver function; 4: Previous upper surgery history; 5: Surgeon experience; 6: Body mass index; 7: American Society of Anesthesiologists score. F/U: Follow-up, mean or median or range, month; L: Left intrahepatic; LH: Laparoscopic hepatectomy; NA: Not available; OH: Open hepatectomy; R: Right intrahepatic; RCT: Randomized controlled trail; Re: Retrospective.
Of the 1329 patients included in the 16 articles, 624 were treated with the laparoscopic approach and 705 with the open approach (Table 2). All 16 studies were retrospective except for 1 RCT (level of evidence: 2b)[17]. Among the remaining 15 studies, 3 compared contemporary series of patients (level of evidence: 3a)[20,25,30], 11 were retrospective case-control studies (level of evidence: 3b)[16,19,21-24,26-29,31], and 1 was a retrospective study using historical series as controls (level of evidence: 4)[18] (Table 3).
Table 2.
Results of meta-analysis in laparoscopic hepatectomy vs open hepatectomy
| Outcomes of interest | Study, n | LH, n | OH, n | WMD/OR (95%CI) | P |
Study heterogeneity |
P | ||
| χ2 | df | I2, % | |||||||
| Operative time, min | 15 | 589 | 665 | 21.49 (-0.27, 43.24) | 0.05 | 227.54 | 14 | 94 | < 0.001 |
| Estimated blood loss, mL | 13 | 575 | 646 | -61.56 (-108.2, -14.91) | 0.01 | 124.6 | 12 | 90 | < 0.001 |
| Intraoperative transfusion | 9 | 450 | 525 | 0.41 (0.22, 0.79) | 0.008 | 13.36 | 8 | 40 | 0.10 |
| Length of hospital stay, d | 15 | 609 | 685 | -3.32 (-4.32, -2.32) | < 0.001 | 75.37 | 14 | 81 | < 0.001 |
| Postoperative complications | 16 | 624 | 705 | 0.52 (0.39, 0.70) | < 0.001 | 10.10 | 15 | 0 | 0.81 |
| Time to oral intake, d | 7 | 210 | 289 | -0.98 (-1.48, -0.47) | < 0.001 | 188.28 | 6 | 97 | < 0.001 |
| Initial residual stone | 12 | 517 | 604 | 0.79 (0.50, 1.25) | 0.31 | 3.96 | 11 | 0 | 0.97 |
| Final residual stone | 5 | 136 | 146 | 0.34 (0.11, 1.08) | 0,07 | 2.92 | 4 | 0 | 0.57 |
| Stone recurrence | 12 | 530 | 604 | 0.63 (0.34, 1.16) | 0.14 | 4.08 | 11 | 0 | 0.97 |
df: Degrees of freedom; LH: Laparoscopic hepatectomy; OH: Open hepatectomy; WMD/OR: Weight mean difference/odds ratio.
Table 3.
Quality of cohort studies evaluated by modified Newcastle-Ottawa scale
| Ref. |
Selection |
Comparability |
Outcomes |
Quality score | |||||
| Definition of cases | Representativeness | Selection of controls | Definition of controls | Comparable for 1, 2, 3, 4 | Comparable for 5, 6, 7 | Assessment of outcomes | Integrity of follow-up | ||
| Cai et al[16], 2007 | Yes | No | No | Yes | Yes | 5 | Yes | Yes | 7 |
| Li, H et al[18], 2008 | Yes | No | No | Yes | 1, 2 | 5 | Yes | Yes | 5 |
| Jin et al[19], 2015 | Yes | No | No | Yes | 1, 2, 3 | No | Yes | Yes | 5 |
| Kim et al[20], 2015 | Yes | Yes | No | Yes | 1, 3, 4 | 6, 7 | Yes | Yes | 7 |
| Lee et al[21], 2014 | Yes | No | No | Yes | 1, 2, 4 | 5 | Yes | Yes | 6 |
| Li, J et al[22], 2014 | Yes | No | No | Yes | 1, 2, 3 | 6 | Yes | Yes | 6 |
| Li, Y et al[23], 2015 | Yes | No | No | Yes | 1, 2, 3 | No | Yes | Yes | 5 |
| Namgoong et al[24], 2014 | Yes | No | No | Yes | Yes | 6 | Yes | Yes | 7 |
| Peng et al[25], 2016 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | 7 |
| Shin et al[26], 2015 | Yes | No | No | Yes | 1, 2 | No | Yes | Yes | 5 |
| Song et al[27], 2010 | Yes | No | No | Yes | Yes | 6 | Yes | Yes | 7 |
| Tian et al[28], 2013 | Yes | No | No | Yes | 1, 2, 4 | 5 | Yes | Yes | 6 |
| Tu et al[29], 2010 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | 7 |
| Ye et al[30], 2015 | Yes | Yes | No | Yes | Yes | No | Yes | Yes | 7 |
1: Age; 2: Sex; 3: Liver function; 4: Previous upper surgery history; 5: Surgeon experience; 6: Body mass index; 7: American Society of Anesthesiologists score.
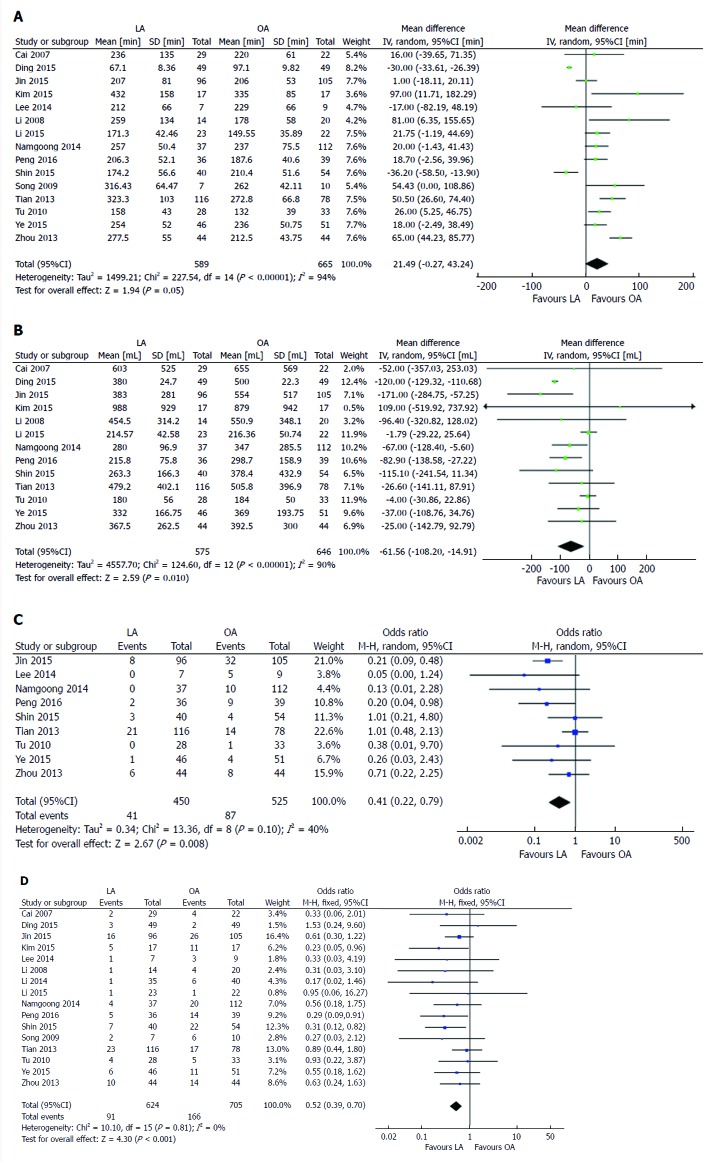
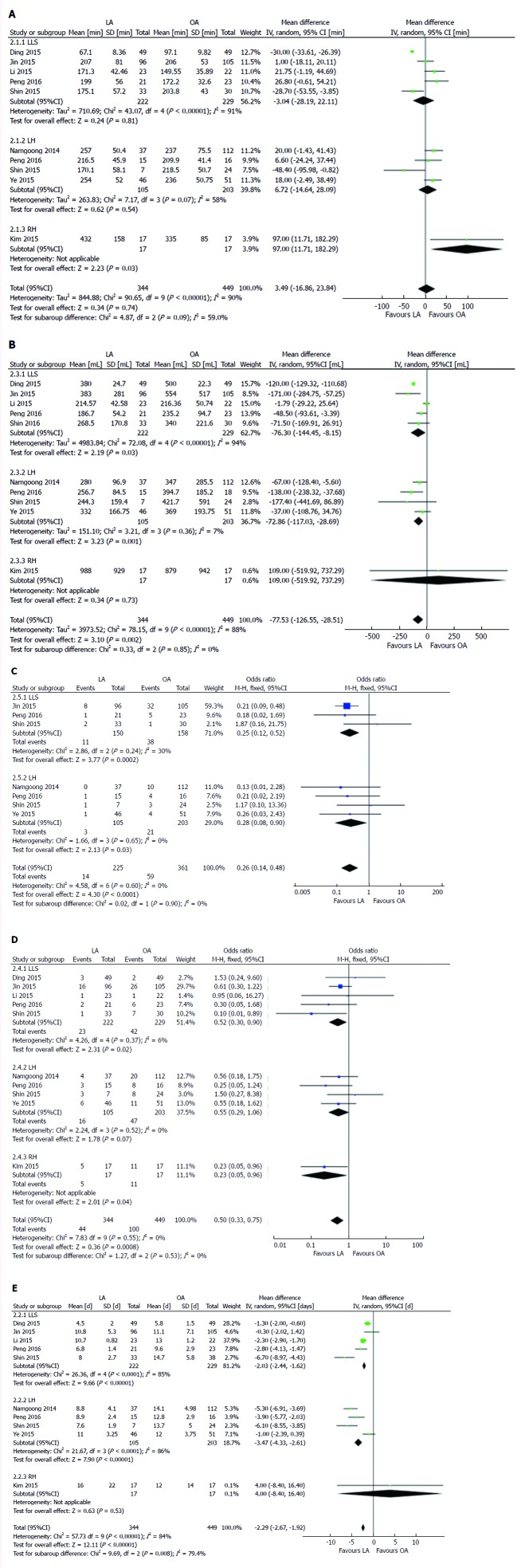
Duration of operation in the 15 studies[16-21,23-31] was similar between the two groups [weighted mean difference (WMD): 21.49, 95%CI: -0.27 to 43.24, P = 0.05] (Figure 2A). EBL was analyzed among 1221 patients from 13 studies[16-20,23-26,28-31], and less EBL was found in the laparoscopic group (WMD: -61.56, 95% CI: -108.2 to -14.91, P = 0.01) (Figure 2B). Intraoperative transfusion was analyzed in 9 articles[19,21,24-26,28-31], showing lower transfusion rate in the laparoscopic group [odds ratio (OR): 0.41, 95%CI: 0.22-0.79, P = 0.008) (Figure 2C). All 16 articles[16-31] were analyzed for postoperative complications, indicating that the rate was significantly lower in the laparoscopic group (OR: 0.52, 95%CI: 0.39-0.70, P < 0.001) (Figure 2D). Seven articles[16,22-25,27,31] reported time to oral intake, with a significantly shorter time for recovery of bowel movement in the laparoscopic group (WMD: -0.98, 95%CI: -1.48 to -0.47, P < 0.001) (Figure 3A). Fifteen studies[16,17,19-31], including 1294 patients, evaluated LOS, which was significantly shorter in the laparoscopic group (WMD: -3.32, 95% CI: -4.32 to -2.32, P < 0.001) (Figure 3B). No significant difference was found in initial and final residual rate (P = 0.31 and 0.07, respectively) (Figure 3C and D). Twelve studies[16,19-22,24-26,28-31] reported stone recurrence rate, with no significant difference between the two groups (OR: 0.63, 95%CI: 0.34-1.16, P = 0.14) (Figure 3E).
Figure 2.
Forest plots comparing operative outcomes between laparoscopic and open liver resection for hepatolithiasis. A: Operative time; B: Intraoperative blood loss; C: Intraoperative transfusion; D: Postoperative complications.
Figure 3.
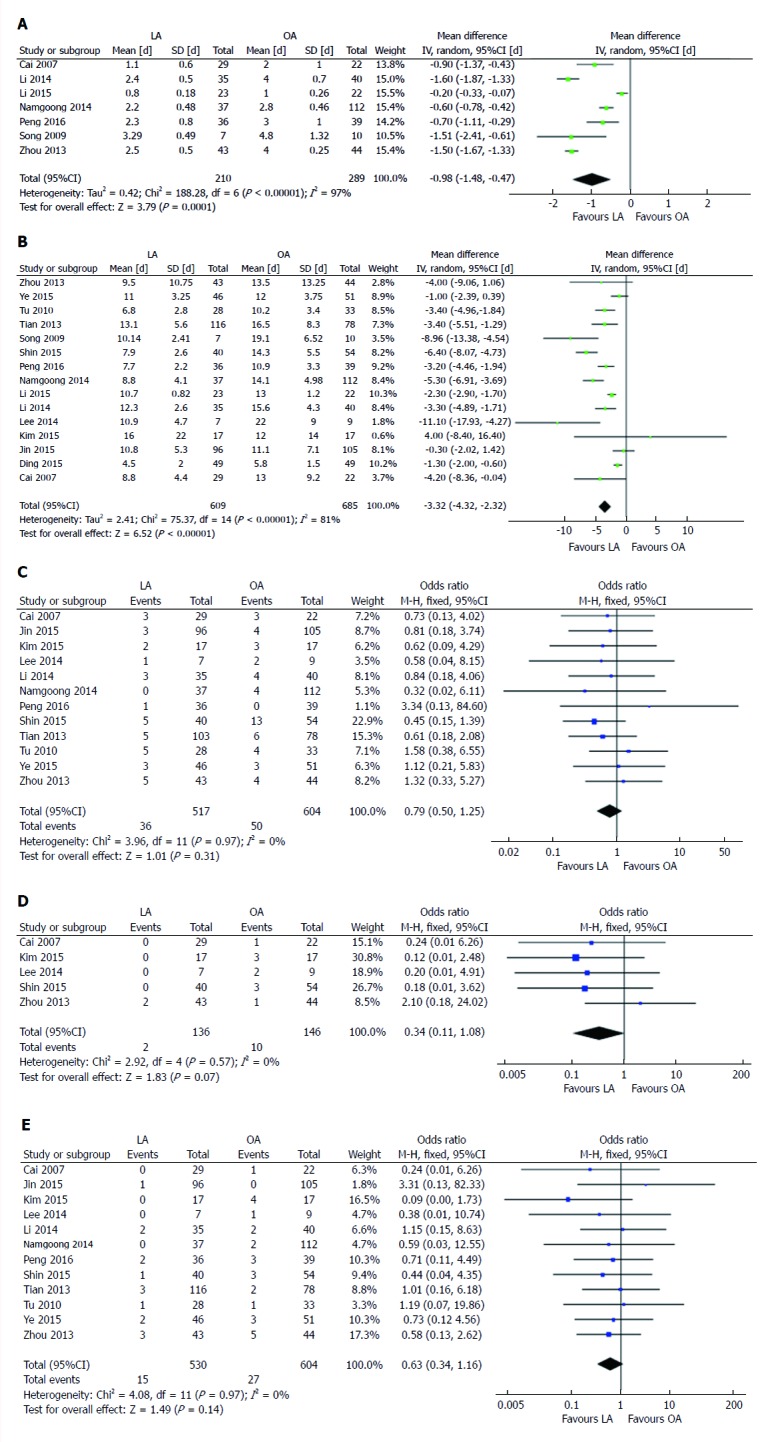
Forest plots comparing postoperative outcomes between laparoscopic and open liver resection for hepatolithiasis. A: Time to oral intake; B: Length of postoperative hospital stay.
Subgroup analysis
Operative time, EBL, LOS, intraoperative transfusion, postoperative complications, initial residual stone and stone recurrence were included in subgroup analysis. In the subgroup assessment of operative time, 8 studies[17,19,20,23-26,30] with 793 patients were included. Pooled data of 5 studies[17,19,23,25,26] showed no significant difference in operating time in patients who underwent LLS by laparoscopic and open approach (WMD: -3.04, 95%CI: -28.19 to 22.11, P = 0.81) (Figure 4A). Pooled analysis of 4 studies[24-26,30] evaluating patients who underwent left hemihepatectomy showed no significant difference between the two groups (WMD: 6.72, 95% CI: -14.64 to 28.09, P = 0.54). In contrast, patients who underwent right hepatectomy tended to have a shorter operating time in the laparoscopic group (WMD: 97.00, 95%CI: 11.71-182.29, P = 0.03)[20].
Figure 4.
Forest plots and subgroup meta-analysis of operative time (A), blood loss during operation (B), intraoperative transfusion rate (C), postoperative complication rate (D) and length of hospital stay (E). IV: Inverse variance method; LA: Laparoscopic approach; LH: Left hemihepatectomy; LLS: Left lateral sectionectomy; OA: Open approach; RH: Right hemihepatectomy; SD: Standard deviation.
Five studies[17,19,23,25,26] compared estimated blood loss for LLS, and showed significantly less blood loss for laparoscopic hepatectomy compared to open liver resection (WMD: -76.30, 95%CI: -144.45 to -8.15, P = 0.03) (Figure 4B). Four studies[24-26,30] comparing EBL for left hemihepatectomy found significantly less blood loss in the laparoscopic group (WMD: -72.86, 95%CI: -116.03 to -28.69, P = 0.001). One study[20] analyzed EBL for right hepatectomy, and indicated no significant difference between the two groups (WMD: 109.0, 95%CI: -519.92 to 737.92, P = 0.73).
Intraoperative transfusion was analyzed in 3 studies[19,25,26] of left lateral sectionectomy, and showed a lower transfusion rate for the laparoscopic approach (OR: 0.25, 95%CI: 0.12-0.52, P < 0.001) (Figure 4C). Similarly, 4 studies[24-26,30] comparing left hemihepatectomy indicated a lower transfusion rate for the laparoscopic approach (OR: 0.28, 95%CI: 0.08-0.90, P = 0.03).
Postoperative complication rate was analyzed in 8 studies[17,19,20,23-26,30], of which 5 involved LLS, 4 left hemihepatectomy[24-26,30] and 1 right liver resection[20] (Figure 4D). It revealed that the laparoscopic approach resulted in fewer postoperative complications than LLS and RH (P = 0.02 and 0.04, respectively). However, it suggested no significant difference between the two groups for left hemihepatectomy (OR: 0.55, 95%CI: 0.29-1.06, P = 0.07).
Eight studies[17,19,20,23-26,30] were included in the subgroup analysis of LOS. Five[17,19,23,25,26] evaluated LLS, showing shorter LOS in the laparoscopic group (WMD: -2.03, 95%CI: -2.44 to -1.62, P < 0.001) (Figure 4E). Four studies[24-26,30] revealed that patients in the laparoscopic left hemihepatectomy group spent less time in hospital (WMD: -3.47, 95%CI: -4.33 to -2.61, P < 0.001). One article[20] suggested no significant difference between the two operative approaches for right hepatectomy (WMD: 4.0, 95%CI: -8.40 to 16.40, P = 0.53).
As for initial residual stone and stone recurrence, subgroup analysis suggested no significant difference between the two approaches. P value for initial residual rate in the different subgroups was 0.09, 0.99 and 0.63, respectively (Figure 5). P value for postoperative stone recurrence rate in the different subgroups was 0.99, 0.53 and 0.11, respectively.
Figure 5.
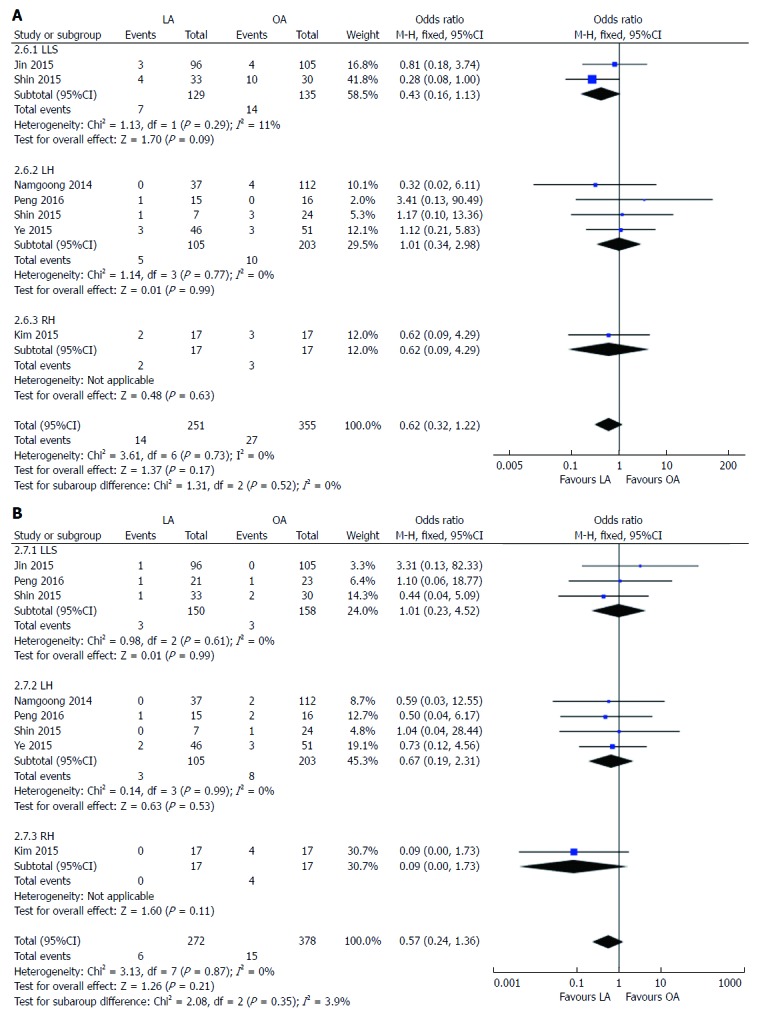
Forest plots and subgroup meta-analysis of initial residual stone rate (A) and stone recurrence rate (B). IV: Inverse variance method; LA: Laparoscopic approach; LH: Left hemihepatectomy; LLS: Left lateral sectionectomy; OA: Open approach; RH: Right hemihepatectomy; SD: Standard deviation.
Sensitivity analysis and publication bias
The RCT and 8 retrospective studies that scored seven stars or more on the modified Newcastle-Ottawa scale were included in sensitivity analysis (Table 4). No significant changes were found in any of the outcomes. The degree of between-study heterogeneity decreased for operative time, EBL, intraoperative transfusion, LOS and time to oral intake. The degree of between-study heterogeneity remained significant for operating time, EBL, LOS and time to oral intake.
Table 4.
Sensitivity analysis in laparoscopic hepatectomy vs open hepatectomy
| Outcomes of interest | Study, n | LH, n | OH, n | WMD/OR (95%CI) | P |
Study heterogeneity |
P | ||
| χ2 | df | I2, % | |||||||
| Operative time, min | 11 | 416 | 464 | 26.58 (-1.78, 54.94) | 0.07 | 201.48 | 10 | 95 | < 0.001 |
| Estimated blood loss, mL | 9 | 402 | 445 | -56.21 (-108.00, -4.43) | 0.03 | 73.92 | 9 | 88 | < 0.001 |
| Intraoperative transfusion | 7 | 314 | 366 | 0.47 (0.23, 0.97) | 0.04 | 8.03 | 6 | 25 | 0.24 |
| Length of hospital stay, d | 12 | 450 | 504 | -3.47 (-4.67, -2.27) | < 0.001 | 47.8 | 11 | 77 | < 0.001 |
| Postoperative complications | 12 | 451 | 504 | 0.55 (0.38, 0.78) | < 0.001 | 8.33 | 11 | 0 | 0.68 |
| Time to oral intake, d | 6 | 187 | 267 | -1.12 (-1.56, -0.68) | < 0.001 | 70.78 | 5 | 93 | < 0.001 |
| Initial residual stone | 10 | 381 | 445 | 0.90 (0.53, 1.53) | 0.71 | 2.74 | 9 | 0 | 0.97 |
| Final residual stone | 5 | 136 | 146 | 0.34 (0.11, 1.08) | 0,07 | 2.92 | 4 | 0 | 0.57 |
| Stone recurrence | 10 | 394 | 445 | 0.59 (0.31, 1.15) | 0.12 | 3.01 | 9 | 0 | 0.96 |
df: Degrees of freedom; LH: Laparoscopic hepatectomy; OH: Open hepatectomy; WMD/OR: Weight mean difference/odds ratio.
The funnel plot of postoperative complications showed that all articles included in this meta-analysis lay inside the 95% CIs and were symmetrically distributed around the center line, indicating a lack of obvious publication bias (Figure 6).
Figure 6.
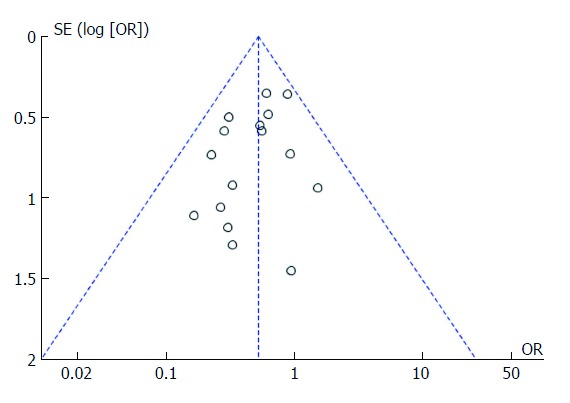
Funnel plot presenting meta-analysis of postoperative complication rate.
DISCUSSION
Treatment for symptomatic hepatolithiasis is still an intractable clinical problem. With appropriate therapy, a variety of complications would be avoided, including cholangitis, biliary stricture, recurrent stones, cirrhosis and even cholangiocarcinoma[32]. Traditionally, open hepatectomy was identified as the best method for this disease[33,34]. However, as laparoscopic approaches have been increasingly used in abdominal surgery over the past two decades, laparoscopic hepatectomy for hepatolithiasis has been considered as standard practice for appropriate cases. Yet, laparoscopic hepatectomy for hepatolithiasis still has not been widely accepted, mainly due to the lack of convincing evidence by adequate comparison of surgical outcomes and long-term quality of life. Nevertheless, numerous studies[16,35] have reported the efficacy, safety and flexibility of laparoscopic hepatectomy for hepatolithiasis. In the current study, we aimed to conduct an extensive worldwide review and meta-analysis to evaluate whether laparoscopic liver surgery can replace open traditional approaches for symptomatic hepatolithiasis.
An earlier meta-analysis performed by Peng et al[36] in 2016 focused on left-sided hepatectomy for hepatolithiasis. It included studies of patients with hepatolithiasis in the left lobe and left lateral lobe that underwent laparoscopic or open hepatectomy. It included 8 studies, 1 RCT and 7 non-randomized trials. The conclusion was that the laparoscopic approach was a safe procedure for patients with hepatolithiasis. However, there were several limitations to that study. First, only 8 studies were included, comparing surgical outcomes between the two methods. Second, the authors concluded the advantages of laparoscopic surgery for patients without any subgroup analysis. Furthermore, although hepatolithiasis is prevalent in the left-sided liver, stones may occur in any segment of the liver. The study only included studies that compared the safety and efficacy of laparoscopic and open approaches in left hemihepatectomy and left lateral segmentectomy for hepatolithiasis.
Our meta-analysis of an RCT and 15 retrospective studies, including 1329 patients, compared the efficacy and flexibility of two methods for hepatolithiasis. We showed that the laparoscopic approach was better than the open approach for both right and left sides of the liver, with significantly lower intraoperative blood loss and blood transfusion rate, shorter intestinal function recovery time, shorter LOS, and lower postoperative complication rate. However, no significant differences in operation time, residual stone and stone recurrence were found.
With respect to surgical outcomes, patient safety should be determined first in the application of any procedure. From the pooled data of postoperative complication rate, EBL and intraoperative blood transfusion, our results indicated that patients who underwent laparoscopic liver resection had better perioperative outcomes than those treated with the open approach.
In term of intraoperative outcomes, our study demonstrated that, compared with the open approach, laparoscopic hepatectomy for patients with hepatolithiasis had advantages of lower blood loss and less transfusion. Laparoscopic parenchymal dissection and the high intra-abdominal pressure during laparoscopic hepatectomy attained by pneumoperitoneum result in lower intraoperative blood loss[37]. Moreover, laparoscopy provided a magnified view of the liver, which contributed to bleeding control. Therefore, fewer patients undergoing laparoscopic surgery were in need of intraoperative transfusion. However, operating time did not differ significantly between the two approaches. This suggests that laparoscopic techniques are still a challenge for hepatic surgeons. The surgeons’ experience had an impact on hepatic lobe dissection under laparoscopy, which contributed significantly to operating time[38,39]. The laparoscopic approach required frequent installation and removal of laparoscopic devices, resulted in additional operative time. In addition, the dissimilarity of the operating procedures in different institutions would have affected the result.
As for postoperative outcomes, the pooled outcomes of 16 studies with 1329 patients revealed that few patients experienced postoperative complications, including wound-related, vascular and biliary complications. Furthermore, fewer postoperative complications appeared in patients who underwent laparoscopic hepatectomy. In laparoscopic liver resection, the vessels and hepatic bile duct could be identified more precisely with the amplification effect of laparoscopy, and the probability of bile duct injury was reduced. Preoperative magnetic resonance cholangiopancreatography would help to reduce postoperative bile leak. With respect to postoperative recovery, the pooled outcomes of 7 studies suggested that the laparoscopic approach was associated with shorter time to oral intake and intestinal function recovery. Minimal incision, better intraoperative outcomes, and faster intestinal function recovery were confirmed to be in favor of shorter hospital stay in patients undergoing laparoscopic hepatectomy. Future well-designed studies should be performed to confirm these potential benefits.
Long-term outcomes after any procedure should also be taken into account. Our meta-analysis and subgroup analysis both showed that, compared with open surgery, there were no significant differences in residual stone rate and hepatolithiasis recurrence rate between the laparoscopic and open approaches. On the one hand, it means that there is no correlation between selection of the surgical procedure and stone residual/recurrent rate. Indeed, the generation and development of hepatolithiasis may have mainly been caused by anatomical variation and dietary habits in different regions[40,41]. Hepatolithiasis is likely to recur even if no residual stones exist after radical hepatectomy. On the other hand, it is known that the severity of abdominal adhesion after laparoscopic liver resection is significantly less than after open surgery[42]. Even though the patients have recurrence of intrahepatic bile duct stones, it would be easier for them to receive effective and safe treatment.
We conducted subgroup analysis, including left lateral hepatectomy, left hemihepatectomy and right hepatectomy for hepatolithiasis, to avoid the influence of heterogeneity. Similar outcomes were found for postoperative complication rate, blood loss and intraoperative blood transfusion, whereas EBL in the subgroup of right hepatectomy did not differ between the two surgical approaches. Sensitivity analysis was also performed to assess the impact of study quality on the estimates. A meta-analysis of RCTs would be ideal. However, with ethical concerns and patient expectations, this kind of study is difficult to conduct. This situation highlights the importance of the present meta-analysis. Although only 1 RCT was included in the present study, most of the other studies were of high quality, and the results could be considered credible and evidential.
The present study confirmed that the laparoscopic approach was better than the open approach for hepatolithiasis. However, our meta-analysis had several limitations that should be taken into account. First, although there was no evidence of publication bias, all the included studies were retrospective studies, except for one RCT. This increased the risk of bias for inadequate random sequencing and blinding. Second, the different levels of surgical expertise would have affected the final outcomes, and multicenter studies with large patient samples are required. Third, the included studies were in English, Chinese and Korean, which could have caused language selection bias. Finally, only studies performed in eastern countries were included in our meta-analysis, which could have resulted in regional selection bias. Further studies are needed to overcome the above-mentioned limitations and confirm our findings.
Nevertheless, the results of this meta-analysis are encouraging, as laparoscopic surgical techniques are frequently applied in abdominal surgery. Moreover, sufficient data on a large patient cohort that underwent liver resection for treatment of hepatolithiasis have been accumulated, allowing evaluation by meta-analysis. Multiple strategies were used to identify applicable studies, with strict criteria used for study inclusion and evaluation. Subgroup analysis was performed to minimize heterogeneity. Future studies comparing laparoscopic and open approaches for treatment of intrahepatic bile duct stones should include larger numbers of patients, with a longer follow-up period.
In summary, this meta-analysis demonstrated that laparoscopic surgery was technically feasible and safe, and superior to open surgery for treatment of hepatolithiasis. Subgroups analysis showed consistent results, except for EBL during right hepatectomy. The laparoscopic approach provides a favorable option for patients seeking curative treatment for hepatolithiasis.
COMMENTS
Background
Hepatectomy has become an established treatment modality for patients with hepatolithiasis. With laparoscopic approach widely used in hepatic surgery in recent years, laparoscopic hepatectomy for treating symptomatic hepatolithiasis attracted more and more attention. Despite this, no consensus is available in the literature about which of these two approaches is more beneficial to the patient.
Research frontiers
Laparoscopy is applied in hepatic surgery more and more frequently. It has been reported about no less safety and efficacy of laparoscopic hepatectomy for liver cancer compared to the conventional approach. The worldwide research is directed towards a type of technique to guaranteeing the safety of patients with benign liver disease.
Innovations and breakthroughs
In this study, the authors investigate the perioperative outcomes of laparoscopic hepatectomy and conventional liver resection by pooling data from the literature. This is the first report of a meta-analysis comparing these two kinds of surgical approaches with large sample size comprehensively.
Applications
This work allows understanding the role of two surgical techniques for treating hepatolithiasis.
Peer-review
This systematic review and meta-analysis adds useful information for practice and research, and probably for policy.
Footnotes
Manuscript source: Unsolicited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: China
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Supported by National Natural Science Foundation of China, No. 81372243, No. 81570593 and No. 81370575; Key Scientific and Technological Projects of Guangdong Province, No. 2014B020228003 and No. 2014B030301041; Natural Science Foundation of Guangdong Province, No. 2015A030312013; Science and Technology Planning Project of Guangzhou, No. 201400000001-3, No. 201508020262 and No. 2014J4100128; Science and Technology Planning Project of Guangdong Province, No. 2017A020215178.
Conflict-of-interest statement: The authors declare that there are no conflicts of interest related to this report.
Data sharing statement: No additional data are available.
Peer-review started: July 10, 2017
First decision: July 28, 2017
Article in press: August 15, 2017
P- Reviewer: Lee HC, Pani SP, Specchia ML S- Editor: Qi Y L- Editor: Filipodia E- Editor: Huang Y
Contributor Information
Hui Li, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China.
Jun Zheng, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China.
Jian-Ye Cai, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China.
Shi-Hui Li, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China.
Jun-Bin Zhang, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China.
Xiao-Ming Wang, Department of Hepatobiliary Surgery, Yijishan Hospital affiliated to Wannan Medical College, Wuhu 241001, Anhui Province, China.
Gui-Hua Chen, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China.
Yang Yang, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China.
Gen-Shu Wang, Department of Hepatic Surgery and Liver Transplantation Center of the Third Affiliated Hospital, Organ Transplantation Institute, Sun Yat-sen University, Organ Transplantation Research Center of Guangdong Province, Guangzhou 510630, Guangdong Province, China; Guangdong Key Laboratory of Liver Disease Research, Key Laboratory of Liver Disease Biotherapy and Translational Medicine of Guangdong Higher Education Institutes, the Third Affiliated Hospital of Sun Yat-sen University, Guangzhou 510630, Guangdong Province, China. wgsh168@163.com.
References
- 1.Lee SE, Jang JY, Lee JM, Kim SW. Selection of appropriate liver resection in left hepatolithiasis based on anatomic and clinical study. World J Surg. 2008;32:413–418. doi: 10.1007/s00268-007-9355-1. [DOI] [PubMed] [Google Scholar]
- 2.Yang T, Lau WY, Lai EC, Yang LQ, Zhang J, Yang GS, Lu JH, Wu MC. Hepatectomy for bilateral primary hepatolithiasis: a cohort study. Ann Surg. 2010;251:84–90. doi: 10.1097/SLA.0b013e3181b2f374. [DOI] [PubMed] [Google Scholar]
- 3.Li SQ, Liang LJ, Peng BG, Hua YP, Lv MD, Fu SJ, Chen D. Outcomes of liver resection for intrahepatic stones: a comparative study of unilateral versus bilateral disease. Ann Surg. 2012;255:946–953. doi: 10.1097/SLA.0b013e31824dedc2. [DOI] [PubMed] [Google Scholar]
- 4.Jan YY, Chen MF, Wang CS, Jeng LB, Hwang TL, Chen SC. Surgical treatment of hepatolithiasis: long-term results. Surgery. 1996;120:509–514. doi: 10.1016/s0039-6060(96)80071-7. [DOI] [PubMed] [Google Scholar]
- 5.Cheung MT, Kwok PC. Liver resection for intrahepatic stones. Arch Surg. 2005;140:993–997. doi: 10.1001/archsurg.140.10.993. [DOI] [PubMed] [Google Scholar]
- 6.Huang MH, Chen CH, Yang JC, Yang CC, Yeh YH, Chou DA, Mo LR, Yueh SK, Nien CK. Long-term outcome of percutaneous transhepatic cholangioscopic lithotomy for hepatolithiasis. Am J Gastroenterol. 2003;98:2655–2662. doi: 10.1111/j.1572-0241.2003.08770.x. [DOI] [PubMed] [Google Scholar]
- 7.Lee SK, Seo DW, Myung SJ, Park ET, Lim BC, Kim HJ, Yoo KS, Park HJ, Joo YH, Kim MH, et al. Percutaneous transhepatic cholangioscopic treatment for hepatolithiasis: an evaluation of long-term results and risk factors for recurrence. Gastrointest Endosc. 2001;53:318–323. doi: 10.1016/s0016-5107(01)70405-1. [DOI] [PubMed] [Google Scholar]
- 8.Feng ZQ, Huang ZQ, Xu LN, Liu R, Zhang AQ, Huang XQ, Zhang WZ, Dong JH. Liver resection for benign hepatic lesions: a retrospective analysis of 827 consecutive cases. World J Gastroenterol. 2008;14:7247–7251. doi: 10.3748/wjg.14.7247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uchiyama K, Onishi H, Tani M, Kinoshita H, Kawai M, Ueno M, Yamaue H. Long-term prognosis after treatment of patients with choledocholithiasis. Ann Surg. 2003;238:97–102. doi: 10.1097/01.sla.0000077923.38307.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Manterola C, Asenjo-Lobos C, Otzen T. [Hierarchy of evidence: levels of evidence and grades of recommendation from current use] Rev Chilena Infectol. 2014;31:705–718. doi: 10.4067/S0716-10182014000600011. [DOI] [PubMed] [Google Scholar]
- 11.Yoshii A, Plaut DA, McGraw KA, Anderson MJ, Wellik KE. Analysis of the reporting of search strategies in Cochrane systematic reviews. J Med Libr Assoc. 2009;97:21–29. doi: 10.3163/1536-5050.97.1.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fan X, Lin T, Xu K, Yin Z, Huang H, Dong W, Huang J. Laparoendoscopic single-site nephrectomy compared with conventional laparoscopic nephrectomy: a systematic review and meta-analysis of comparative studies. Eur Urol. 2012;62:601–612. doi: 10.1016/j.eururo.2012.05.055. [DOI] [PubMed] [Google Scholar]
- 13.Taggart DP, D’Amico R, Altman DG. Effect of arterial revascularisation on survival: a systematic review of studies comparing bilateral and single internal mammary arteries. Lancet. 2001;358:870–875. doi: 10.1016/S0140-6736(01)06069-X. [DOI] [PubMed] [Google Scholar]
- 14.Wells GA, Shea BJ, O’Connell D, Peterson J, Welch V, Losos M, Tugwell P. The Newcastle-Ottawa Scale (NOS) for Assessing the Quality of Non-Randomized Studies in Meta-Analysis. Applied Engineering Agriculture. 2000;18:727–734. [Google Scholar]
- 15.Higgins Jp T, Green S. Cochrane Handbook for Systematic Reviews of Interventions. Version 5.1. 0: Wiley-Blackwell; 2011. [Google Scholar]
- 16.Cai X, Wang Y, Yu H, Liang X, Peng S. Laparoscopic hepatectomy for hepatolithiasis: A feasibility and safety study in 29 patients. Surg Endosc. 2007;21:1074–1078. doi: 10.1007/s00464-007-9306-9. [DOI] [PubMed] [Google Scholar]
- 17.Ding G, Cai W, Qin M. Pure laparoscopic versus open liver resection in treatment of hepatolithiasis within the left lobes: A randomized trial study. Surgical Laparoscopy. Surg Laparosc Endosc Percutan Tech. 2015;25:392–394. doi: 10.1097/SLE.0000000000000120. [DOI] [PubMed] [Google Scholar]
- 18.Li H, Mao HX, Yu DS. [Laparoscopic anatomical hepatectomies for intrahepatic bile duct stone] Zhongguo Yi Xue Ke Xue Yuan Xue Bao. 2008;30:465–468. [PubMed] [Google Scholar]
- 19.Jin RA, Wang Y, Yu H, Liang X, Cai XJ. Total laparoscopic left hepatectomy for primary hepatolithiasis: Eight-year experience in a single center. Surgery. 2016;159:834–841. doi: 10.1016/j.surg.2015.09.022. [DOI] [PubMed] [Google Scholar]
- 20.Kim YK, Han H-S, Yoon Y-S, Cho JY, Lee W. Laparoscopic Approach for Right-Sided Intrahepatic Duct Stones: A Comparative Study of Laparoscopic Versus Open Treatment. World J Surg. 2015;39:1224–1230. doi: 10.1007/s00268-015-2942-7. [DOI] [PubMed] [Google Scholar]
- 21.Lee SE, Choi YS. Initial experience of laparoscopic hepatectomy for intrahepatic duct (IHD) stones: Comparison with open hepatectomy. HPB. 2014;16:359. [Google Scholar]
- 22.Li J, Lu B, Cai X, Huang Y, Lu W, Huang F, Jin X, Yan Y. Comparative study of clinical effects of laparoscopic hepatectomy versus open hepatectomy for treating hepatolithiasis. Chongqing Yiyao. 2014;43:4891–4894. [Google Scholar]
- 23.Li Y, Wei D, Wang K, Huang S, Zhu H, Li X, Zhang X, Zou H. Laparoscopic versus open left lateral hepatic lobectomy plus choledochoscopic stone extraction for left lobe hepatolithiasis. Zhonghua Puwaike Zazhi. 2015;24:1070–1076. [Google Scholar]
- 24.Namgoong JM, Kim KH, Park GC, Jung DH, Song GW, Ha TY, Moon DB, Ahn CS, Hwang S, Lee SG. Comparison of laparoscopic versus open left hemihepatectomy for left-sided hepatolithiasis. Int J Med Sci. 2014;11:127–133. doi: 10.7150/ijms.7516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Peng L, Xiao J, Liu Z, Zhu J, Wan R, Xiao W, Li Y. Laparoscopic left-sided hepatectomy for the treatment of hepatolithiasis: A comparative study with open approach. Int J Surg. 2017;40:117–123. doi: 10.1016/j.ijsu.2017.02.068. [DOI] [PubMed] [Google Scholar]
- 26.Shin YC, Jang JY, Kang MJ, Jung W, Chang J, Chang YR, Kim SW. Comparison of laparoscopic versus open left-sided hepatectomy for intrahepatic duct stones. Surg Endosc. 2016;30:259–265. doi: 10.1007/s00464-015-4200-3. [DOI] [PubMed] [Google Scholar]
- 27.Song YJ, Kim KJ, Moon HG, Jeong SH, Ju YT, Jung E-J, Lee YJ, Hong SC, Choi SE, Ha WS, et al. The Feasibility of Laparoscopic Hepatectomy for the Patients with Left Intrahepatic Stones. J Korean Surg Society. 2010;78:35–40. [Google Scholar]
- 28.Tian J, Li JW, Chen J, Fan YD, Bie P, Wang SG, Zheng SG. Laparoscopic hepatectomy with bile duct exploration for the treatment of hepatolithiasis: An experience of 116 cases. Dig Liver Dis. 2013;45:493–498. doi: 10.1016/j.dld.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 29.Tu JF, Jiang FZ, Zhu HL, Hu RY, Zhang WJ, Zhou ZX. Laparoscopic vs open left hepatectomy for hepatolithiasis. World J Gastroenterol. 2010;16:2818–2823. doi: 10.3748/wjg.v16.i22.2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ye X, Ni K, Zhou X, Xie K, Hong X. Laparoscopic versus open left hemihepatectomy for hepatolithiasis. J Surg Res. 2015;199:402–406. doi: 10.1016/j.jss.2015.06.021. [DOI] [PubMed] [Google Scholar]
- 31.Zhou F, Shao JH, Zou SB, Huang MW, Yin XB, Yu X. Laparoscopic hepatectomy is associated with a higher incident frequency in hepatolithiasis patients. Surg Today. 2013;43:1371–1381. doi: 10.1007/s00595-012-0425-0. [DOI] [PubMed] [Google Scholar]
- 32.Lin CC, Lin PY, Ko CJ, Chen YL, Chen ST, Kuo SJ. Hepatic resection for bilateral hepatolithiasis: a 20-year experience. ANZ J Surg. 2013;83:978–984. doi: 10.1111/j.1445-2197.2012.06283.x. [DOI] [PubMed] [Google Scholar]
- 33.Gagner M, Rogula T, Selzer D. Laparoscopic liver resection: benefits and controversies. Surg Clin North Am. 2004;84:451–462. doi: 10.1016/j.suc.2003.11.002. [DOI] [PubMed] [Google Scholar]
- 34.Yoon YS, Han HS, Shin SH, Cho JY, Min SK, Lee HK. Laparoscopic treatment for intrahepatic duct stones in the era of laparoscopy: laparoscopic intrahepatic duct exploration and laparoscopic hepatectomy. Ann Surg. 2009;249:286–291. doi: 10.1097/SLA.0b013e31818eea56. [DOI] [PubMed] [Google Scholar]
- 35.Huang C, Li G, Zou S, Fang L, Huang M, Wang K, Lou S. Clinical efficacy of laparoscopic left hemihepatectomy for the treatment of intrahepatic bile duct stones. Zhonghua Xiaohua Waike Zazhi. 2015;14:152–154. [Google Scholar]
- 36.Peng L, Xiao J, Liu Z, Li Y, Xiao W. Laparoscopic Versus Open Left-Sided Hepatectomy for Hepatolithiasis: A Systematic Review and Meta-Analysis. J Laparoendosc Adv Surg Tech A. 2017;27:951–958. doi: 10.1089/lap.2016.0357. [DOI] [PubMed] [Google Scholar]
- 37.Eiriksson K, Fors D, Rubertsson S, Arvidsson D. High intra-abdominal pressure during experimental laparoscopic liver resection reduces bleeding but increases the risk of gas embolism. Br J Surg. 2011;98:845–852. doi: 10.1002/bjs.7457. [DOI] [PubMed] [Google Scholar]
- 38.Langenhuijsen J, Birtle A, Klatte T, Porpiglia F, Timsit MO. Surgical Management of Adrenocortical Carcinoma: Impact of Laparoscopic Approach, Lymphadenectomy, and Surgical Volume on Outcomes-A Systematic Review and Meta-analysis of the Current Literature. Eur Urol Focus. 2016;1:241–250. doi: 10.1016/j.euf.2015.12.001. [DOI] [PubMed] [Google Scholar]
- 39.Wu TJ, Wang F, Lin YS, Chan KM, Yu MC, Lee WC. Right hepatectomy by the anterior method with liver hanging versus conventional approach for large hepatocellular carcinomas. Br J Surg. 2010;97:1070–1078. doi: 10.1002/bjs.7083. [DOI] [PubMed] [Google Scholar]
- 40.Kitagawa Y, Nimura Y, Hayakawa N, Kamiya J, Nagino M, Uesaka K, Oda K, Ohta A, Jan YY, Cheng LP, et al. Intrahepatic segmental bile duct patterns in hepatolithiasis: a comparative cholangiographic study between Taiwan and Japan. J Hepatobiliary Pancreat Surg. 2003;10:377–381. doi: 10.1007/s00534-002-0834-3. [DOI] [PubMed] [Google Scholar]
- 41.Shaffer EA. Gallstone disease: Epidemiology of gallbladder stone disease. Best Pract Res Clin Gastroenterol. 2006;20:981–996. doi: 10.1016/j.bpg.2006.05.004. [DOI] [PubMed] [Google Scholar]
- 42.Stommel MW, Ten Broek RP, Strik C, Slooter GD, Verhoef C, Grünhagen DJ, van Duijvendijk P, Bemelmans MH, den Dulk M, Sietses C, et al. Multicenter Observational Study of Adhesion Formation after Open-and Laparoscopic Surgery for Colorectal Cancer. Ann Surg. 2017 doi: 10.1097/SLA.0000000000002175. Epub ahead of print. [DOI] [PubMed] [Google Scholar]