Abstract
Roots of Asparagus cochinchinesis have been widely used to treat fever, cough, kidney disease, breast cancer, inflammatory and brain disease, although the effects of their fermented products have not been assessed until now. To investigate the anti-inflammatory effects on macrophages of a butanol extract from A. cochinchinensis roots fermented with Weissella cibaria (BAW), alterations in the inducible nitric oxide synthase (iNOS)-mediated cyclooxygenase-2 (COX-2) induction pathway and inflammatory cytokine expression were measured in lipopolysaccharide (LPS)-activated RAW264.7 cells following pretreatment with BAW. Briefly, W. cibaria was selected from two bacterial strains for the fermentation of A. cochinchinensis roots based on its hyaluronidase inhibition and NO suppression rates. Following fermentation with W. cibaria, the level of various key components including total phenols and protodioscin were significantly enhanced in BAW. In addition, BAW exhibited high free radical scavenging activity (IC50=31.62 µg/ml) and induced a decrease of intracellular ROS production in RAW264.7 cells following DCFH-DA staining. Significant suppressions in the expression level of important members of the iNOS-mediated COX-2 induction pathway and the phosphorylation of mitogen-activated protein kinase members were detected. The expressions of pro-inflammatory and anti-inflammatory cytokines were recovered in BAW pretreated RAW264.7 cells. Overall, these results suggest that BAW may suppress inflammatory responses through differential regulation of the iNOS-mediated COX-2 induction pathway and inflammatory cytokine expressions in LPS-activated RAW264.7 cells.
Keywords: Asparagus cochinchinesis, Weissella cibaria, fermentation, inflammation, RAW264.7, cytokines
Introduction
Inflammation is a typical physiological response of an organism against various injurious insults including invading microorganisms, dust particles, altered self-cells, and transformed cancer cells (1). This response is usually classified into acute and chronic reactions according to the inflammatory process and cellular mechanisms (2). During an inflammatory response, a series of processes including dilation of venules and arterioles, enhanced blood vessel permeability, and blood flow with percolation of leukocytes into tissues have been detected in specific cells and tissues (3). Furthermore, inflammation could be associated with various chronic diseases including cancer, diabetes, obesity, autoimmune disease, inflammatory bowel disease, asthma, rheumatoid arthritis, and cardiovascular disease (2,4).
Meanwhile, several drug types including corticosteroids, NSAIDs, and biologics have been used to treat inflammatory diseases in humans, even though these drugs may have side effects and high cost. In particular, corticosteroids have long been used to treat rheumatoid arthritis, but they induce some serious side effects such as hypertension, Cushing's habitus, hyperglycemia, osteoporosis, and growth arrest (5). Therefore, natural products with anti-inflammatory activity have received a lot of attention as novel materials to overcome side effect problems (6). In particular, some natural products including Actinidia argute (7), Ampelopsis grossedentata (8), Artemisia annua Herba (9), Cheilanthes albomarginata (10) and Grateloupia lanceolate (11) have been shown to significantly reduce the expression of key inflammatory mediators.
Among these natural products, the anti-inflammatory activity of an A. cochinchinesis extract has been reported. The A. cochinchinesis extract significantly inhibited secretion of the pro-inflammatory cytokine, tumor necrosis factor (TNF)-α in LPS- and substance P-stimulated mouse astrocytes (12). In addition, aspacochinosides N, O, and P extracted from ethanol-treated A. cochinchinesis decreased NO concentration in LPS-stimulated BV-2 microglial cells. Moreover, an ethanol extract from A. cochinchinesis greatly decreased ectopic edema degree, ear thickness, cytokine secretion, and myeloperoxidase activity, which are considered indicators of skin inflammation progression, in a skin inflammation-induced mouse model treated with 12-O-tetradecanoyl-phorbol-13-acetate (13). A crude aqueous extract of A. cochinchinensis effectively inhibits TNF-α-induced cytotoxicity (14), as well as increases the spleen index and SOD activity and decreases malondialdehyde in mice (15). A recent study reported inhibitory effects of A. cochinchinensis in allergic asthma-associated airway remodeling. The standardized herbal formula PM014, which includes the roots of A. cochinchinensis, efficiently inhibited the number of total cells, eosinophils, neutrophils, macrophages, and lymphocytes in the bronchoalveolar lavage fluid of cockroach allergen-induced mice (16). However, the underlying mechanism by which the fermented roots of A. cochinchinensis exert their anti-inflammatory effects in macrophages has not yet been clearly identified, even though the effects of fermented extracts were investigated in antigen-stimulated macrophages.
In this study, we investigated the fundamental mechanisms responsible for anti-inflammatory activities of BAW in LPS-induced RAW264.7 microphage cells. The results provide novel data indicating that BAW may be associated with suppression of various chronic inflammation-related diseases through the regulation of the iNOS-mediated COX-2 induction pathway and cytokine expression.
Materials and methods
Preparation of BAW and butanol extract from A
cochinchinensis roots fermented with Lactobacillus plantarum (BAL). The roots of A. cochinchinensis used in this study were collected from plantations in the Go-Chang area of Korea and dried in a drying machine (Ilshinbiobase, Dongducheon, Korea) at 60°C. Voucher specimens of A. cochinchinensis roots (WPC-14-003) were deposited in the functional materials bank of the PNU-Wellbeing RIS Center at Pusan National University. These samples were also identified by Dr. Shin Woo Cha at the Herbal Crop Research Division, National Institute of Horticultural & Herbal Science.
Firstly, to prepare aqueous fractions of unfermented A. cochinchinensis (UnF), 20 g of freeze-dried A. cochinchinensis roots were ground to a powder and a hot water extract prepared with 1.2 l of deionized distilled water (dH20) for 2.5 h in a hot water extractor (DW-290, Daewoong, Kyunggi, Korea). After finishing aqueous extraction, samples were filtered through filter paper (Whatman No. 2, Whatman, Brentford, UK) and then evaporated by using a rotary vacuum evaporator (EYELA, N-1100 series, Tokyo, Japan). Finally, UnF was used for fermentation after freeze-drying. Yield from the hot water extraction process was 60.7%.
The two bacterial strains (W. cibaria and Lactobacillus plantarum) used in the fermentation process were provided by Professor Hong Joo Son, Department of Life Science and Environmental Biochemistry, Pusan National University. To prepare fermented products, UnF powder was dissolved with 1% (w/v) in dH2O (pH 5.3), and the mixture sterilized at 121°C for 15 min. After cooling at room temperature, W. cibaria or L. plantarum precultivated in lactobacilli MRS broth (Difco Laboratories, Detroit, MI) until the final cell density approached 107 CFU/ml (OD600=0.1) were inoculated [5% (v/v)] to the UnF mixture. The mixture was then incubated in a shaking incubator (VS-8480; Vision Scientific, Bucheon, Korea) at 37°C at 200 rpm/min for 4.3 d. Fermented A. cochinchinensis products of W. cibaria (FPW) or L. plantarum (FPL) were obtained from the mixtures solution fermented with W. cibaria or L. plantarum by using centrifugation at 12,000 × g for 10 min.
To obtain the n-butanol fractions of UnF (BUnF), FPW (BAW) and FPL (BAL), an equal volume of butanol was firstly added to UnF, FPW or FPL. After vigorous mixing and incubating, the butanol phase was collected from each mixture by centrifugation at 12,000 × g for 10 min. Butanol extraction was repeated three times, after which all butanol phases were combined, evaporated under a rotary vacuum evaporator, freeze-dried, and stored at −20°C until use.
Hyaluronidase inhibition assay
The inhibition activity of hyaluronidase against BUnF, BAW, and BAL was investigated by using a colorimetric assay based on the modified Morgan-Elson method (17–19) which measures the amount of N-acetyl-D-glucosamine produced from sodium hyaluronate. Briefly, 12 µl of BUnF, BAW, or BAL were mixed with 12 µl of hyaluronidase (10 mg/ml) in 0.1 M sodium acetate buffer (pH 3.5), then incubated in a water bath at 37°C. After pre-incubation for 20 min, the sample and hyaluronidase solution mixture was added to 12 µl of 12.5 mM calcium chloride to activate the hyaluronidase and then incubated for 20 min. To the activated hyaluronidase solution, 24 µl of sodium hyaluronate (6 mg/ml) dissolved in 0.1 M sodium acetate buffer (pH 3.5) was added and incubated for an additional 40 min. Next, the solution was amended with 12 µl of 0.4 N NaOH and 0.4 M potassium tetraborate, then vortexed, boiled for 3 min, and placed on ice to terminate the hyaluronidase activity. Subsequently, 360 µl of DMAB solution (p-dimethylaminobenzaldehyde 4 g in a solution of acetic acid 350 ml mixed with 50 ml of 10 N HCl) was added, and the sample placed in a 37°C water bath for 20 min. The absorbance of each test tube at 540 nm was measured by using a microplate reader (Tecan Sunrise, Tecan, Hombrechtikon, Switzerland). Hyaluronidase inhibition activity was estimated by determining differences in the absorbance values of the sample solutions.
Analysis of bioactive compounds in BUnF and BAW
The concentration of three bioactive compounds including total phenols and crude saponins in BUnF and BAW were measured as previously described. The amount of total phenols in BAW was determined according to the Folin-Ciocalteu method (20). Briefly, BUnF and BAW (20 µl) was mixed with 100 µl of 0.2 N Folin-Ciocalteu reagent for 5 min, after which 300 µl of 20% sodium carbonate was added. Following incubation at room temperature for 2 h, the absorbance of the reaction mixture was measured at 765 nm. A calibration curve was generated with Gallic acid as the standard. Total phenolic content was expressed in milligrams of gallic acid equivalents per gram of BAW.
The total crude saponins amount was detected as described previously (21). Briefly, BUnF and BAW dissolved in 30 ml dH2O was repeatedly extracted with ethyl ether (50 ml) to remove lipid soluble substances. After collection of the aqueous layer, samples were further extracted with n-butanol (30 ml) three times. This layer was then concentrated by vacuum evaporation and lyophilization by using circulation extraction equipment (IKA Labortechnik, Seoul, Korea). Finally, total crude saponins was calculated by using the equation: crude saponin (mg/g)=A-B/S, where, A is the dry weight of the n-butanol layer (mg), B is the weight of the flask (mg), and S is the weight of the solid volume of the sample (g).
High performance liquid chromatography (HPLC) analysis
Protodioscin, a saponin, was identified in BUnF and BAW by using an ILC 3000 HPLC system (Interface Engineering Co. Ltd., Seoul, Korea) equipped with a Corona® CAD® detector (ESA Biosciences, Inc., Chelmsford, MA, USA). Chromatographic separation was performed on a CapCell PAK MG C18 (4.6×250 mm, particle size 5 µm; Shiseido Co., Ltd., Tokyo, Japan). The mobile phase consisted of solvent A (dH2O) and solvent B (acetonitrile) prepared by using a gradient elution program: 0–25 min with 30–90% solvent B and 25–40 min with 90% solvent B. A flow rate of 1.0 ml/min was used for sample analysis. The nebulizer gas was compressed nitrogen. Gas flow rate and gas pressure were maintained at 1.53 l/min and 35±2 psi, respectively. The output signal of the detector was recorded by using Clarity™ chromatography software (DataApex, Prague, Czech Republic).
Free radical scavenging activity
The scavenging activity of the 2,2-diphenyl-1-picrylhydrazyl (DPPH) radical against BAW was measured as previously described (22). Briefly, each sample (100 µl) in eight different concentrations of BAW (7.8 to 1,000 µg/ml) was mixed with 100 µl of 0.1 mM DPPH (Sigma-Aldrich Co., St. Louis, MO, USA) in 95% ethanol solution or 100 µl of 95% ethanol solution, then incubated for 30 min at room temperature. Next, the absorbance of the reaction mixture was measured at 517 nm by using a Versa-max plate reader (Molecular Devices, Sunnyvale, CA, USA). The DPPH radical scavenging activity of the BAW was expressed as the percent decrease in absorbance relative to that in the control. The IC50 value is defined as the concentration of substrate that produces a 50% loss in DPPH activity.
Cell viability assay
The RAW264.7 cell line used in this study consists of macrophage cells originating from the Abelson murine leukemia virus-induced tumor provided by the Korean Cell Line Bank (Seoul, Korea). The RAW264.7 cells were grown with Dulbecco's Modified Eagle's Medium (DMEM, Thermo Scientific, Waltham, MA, USA) containing 10% fetal bovine serum (FBS, S001-01, Welgene, Gyeongsan-si, Korea), L-glutamine, penicillin, and streptomycin (Thermo Scientific) in a humidified incubator at 37°C under 5% CO2 and 95% air.
Cell viability was determined by using tetrazolium compound 3-[4,5-dimethylthiazol-2-yl]-2,5-diphenyltetrazolium bromide (MTT) (Sigma-Aldrich Co.). To determine cell viability, RAW264.7 cells were seeded at a density of 5×104 cells/0.2 ml and grown for 24 h in a 37°C incubator. When the cells attained 70–80% confluence, they were either untreated (No) or treated with DMSO (Vehicle), or pretreated with 100 µg/ml (BAWLo) or 200 µg/ml (BAWHi) of BAW dissolved in DMSO. Following incubation for 24 h, the supernatants were discarded, after which 0.2 ml of fresh MEM media and 50 µl of MTT solution [2 mg/ml in phosphate buffered saline (PBS)] were added to each well. The cells were then incubated at 37°C for 4 h. Formazan precipitate was dissolved in DMSO, after which the absorbance at 570 nm was read directly in the wells by using a Molecular Devices VERSA max Plate reader (Sunnyvale, CA, USA). The morphological features of RAW264.7 cells in each treated group were observed by using a microscope (Leica Microsystems, Switzerland).
NO concentration analysis
NO concentration in the culture supernatant of RAW264.7 cells was measured by using Griess reagent [1% sulfanilamide, 5% phosphoric acid, 0.1% N-(1-naphthyl) ethylenediamine dihydrochloride; Sigma-Aldrich Co.] as described previously (23). Briefly, RAW264.7 cells were treated with Vehicle or BAW (100 or 200 µg/ml) for 2 h followed by LPS (1 µg/ml) for 24 h. Following collection of the supernatant, each sample (100 µl) was mixed with the same volume of Griess reagent and incubated at room temperature for 10 min. The absorbance was read at 540 nm by using a VersaMax microplate reader (Molecular Devices).
Analysis of intracellular ROS level
Intracellular ROS levels in RAW264.7 cells were measured by staining with 2′,7′-dichlorofluorescein diacetate (DCFH-DA; Sigma-Aldrich Co.), which is a cell permeable, nonfluorescent agent that can be deacetylated by intracellular esterases to form nonfluorescent DCFH. In the presence of ROS, DCFH is converted to highly fluorescent DCF intracellularly. Briefly, RAW364.7 cells were seeded at 5×105 cells/2 ml in 6-well plates, then grown with two different concentrations of BAW for 2 h in a 37°C incubator. After washing once with 1× PBS, the cells were incubated with 1 µg/ml of LPS for another 24 h. Next, cells were incubated with 25 µM DCFH-DA for 30 min at 37°C. Finally, the cells were washed twice with PBS, after which the green fluorescence was observed at 200× magnification via fluorescence microscopy (Eclipse TX100, Nikon, Tokyo, Japan).
Western blot analysis
Total homogenate of RAW264.7 cells obtained by using Pro-Prep Protein Extraction Solution (iNtRON Biotechnology, Seongnam, Korea) was centrifuged at 13,000 rpm/min for 5 min, then the concentration of total protein was quantified by using a SMARTTM BCA protein assay kit (Thermo Scientific) for western blotting. Briefly, the proteins were separated by 4–20% sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) for 2 h, after which resolved proteins were transferred to nitrocellulose membranes for 2 h at 40 V. Each membrane was then incubated overnight separately at 4°C with the following primary antibodies: SAPK/JNK antibody (Cell Signaling Technology, Danvers, MA, USA), p-SAPK/JNK (Thr183/Tyr185) antibody (Cell Signaling Technology), ERK1 (K-23) antibody (Santa Cruz Biotechnology, Inc. Santa Cruz, CA, USA), p-p44/42 MAPK (Erk1/2) (Thr202/Tyr204) antibody (Cell Signaling Technology), p38 MAPK antibody (Cell Signaling Technology), p-p38 MAP Kinase (Thr180/Tyr182) antibody (Cell Signaling Technology), and anti-actin antibody (Sigma-Aldrich Co.). Next, the membranes were washed with washing buffer (137 mM NaCl, 2.7 mM KCl, 10 mM Na2HPO4, and 0.05% Tween 20) and incubated with 1:1,000 diluted horseradish peroxidase (HRP)-conjugated goat anti-rabbit IgG (Invitrogen, Carlsbad, CA, USA) at room temperature for 1 h. Finally, membrane blots were developed by using Amersham ECL Select western blotting detection reagent (GE Healthcare, Little Chalfont, UK). The chemiluminescence signals that originated from specific bands were detected by using FluorChemi®FC2 (Alpha Innotech, San Leandro, CA, USA).
Enzyme-linked immunosorbent assay (ELISA) for IL-6 cytokine
The concentration of cytokine IL-6 in the culture supernatant of RAW264.7 cells treated with BAW was determined by using an IL-6 ELISA kit (Biolegend, San Diego, CA, USA) according to the manufacturer's instructions. Briefly, RAW264.7 cells were treated with two different concentrations of BAW (100 or 200 µg/ml) for 2 h, followed by 1 µg/ml of LPS for 24 h. After collection of the supernatant, 100 ml of serial dilutions of the culture supernatant were added to a 96-well plate coated with anti-IL-6 antibody and then incubated for 2 h at room temperature. After five washes with wash solution (PBS, 0.05% and Tween-20, pH 7.4), 100 µl of avidin-horseradish peroxidase solution was added to each well, and the plates were allowed to develop at 37°C for 2 h. After five washes with wash solution, the plate was maintained at 37°C for 30 min to react with 100 µl of substrate solution. The reaction was then stopped by the addition of 100 µl of blocking solution, after which the absorbance at 450 nm was read with a VersaMax microplate reader (Molecular Devices).
RT-PCR analysis for cytokine gene expression
The mRNA levels of iNOS, COX-2, TNF-α, IL-1β, and IL-6 were measured by RT-PCR as previously described (24). First, total RNA molecules were purified by removing media from a subset group of cells and then homogenizing the cells in RNAzol CS104 (Tel-Test Inc., Friendswood, USA). The isolated RNA was then quantified by using UV spectroscopy. Expressions of the target genes were assessed by using RT-PCR with 5 µg of total RNA from cells of each group. Next, 500 ng of oligo-dT primer (Invitrogen, Carlsbad, CA, USA) were annealed at 70°C for 10 min. The complementary DNA (cDNA), which was used as the template for further amplification, was synthesized by the addition of deoxyadenosine triphosphate (dATP), deoxycytidine triphosphate (dCTP), deoxyguanosine triphosphate (dGTP), and deoxythymidine triphosphate (dTTP) with 200 units of reverse transcriptase (Superscript II, Invitrogen, 200 U/µl). Next, 10 pmol of the sense and antisense primers were added, and the reaction mixture was subjected to 28–32 cycles of amplification. Amplification was conducted in a Perkin-Elmer Thermal Cycler and used the following cycle: 30 sec at 94°C, 30 sec at 62°C, and 45 sec at 72°C. The primer sequences for target gene expression identification were as follows: iNOS, sense primer: 5′-CACTTGGAGTTCACCCAGT-3′, anti-sense primer: 5′-ACCACTCGTACTTGGGATGC-3′; COX-2, sense primer: 5′-CAGGTCATTGGTGGAGAGGTGTATC-3′, anti-sense primer: 5′-CCAGGAGGATGGAGTTGTTGTAGAG-3′; TNF-α, sense primer: 5′-CCTGTAGCCCACGTCGTAGC-3′, anti-sense primer: 5′-TTGACCTCAGCGCTGACTTG-3′; IL-1β, sense primer: 5′-GCACATCAACAAGAGCTTCAGGCAG-3′, anti-sense primer: 5′-GCTGCTTGTGAGGTGCTGATGTAC-3′; and IL-6, sense primer: 5′-TTGGGACTGATGTTGTTGACA-3′, anti-sense primer: 5′-TCATCGCTGTTGATACAATCAGA-3′. The experiment was repeated three times, and all samples were analyzed in triplicate. The final RT-PCR products were separated on 1–2% agarose gel and then visualized by ethidium bromide staining. The densities of specific bands were quantified by using the Kodak Electrophoresis Documentation and Analysis System 120 (Eastman Kodak, Rochester, NY).
Statistical analysis
One-way ANOVA was used to identify significant differences between No-treated and LPS-treated groups (SPSS for Windows, Release 10.10, Standard Version, Chicago, IL, USA). Differences in the responses of the Vehicle+LPS-treated group and the BAW+LPS-treated groups were evaluated by using a post hoc test (SPSS for Windows, Release 10.10, Standard Version). All values are reported as the mean ± standard deviation (SD) and a P-value of <0.05 was considered significant.
Results
Selection of bacterial strain for optimal fermentation
To enhance the anti-inflammatory activity of A. cochinchinensis roots, fermentation technique was firstly applied to these roots using two bacterial strains (W. cibaria and L. plantarum). Anti-inflammatory activity and toxicity were measured in the two final products (BAW and BAL) obtained from fermented A. cochinchinensis roots using butanol extraction. As shown Table I, a significance alternation was detected in hyaluronidase inhibition rate and suppression rate of NO concentration. Hyaluronidase inhibition rate was dramatically enhanced after fermentation although this level was slightly higher with 18–21% in BAW than BAL. A similar pattern to that observed for the hyaluronidase inhibition rate was also observed in the suppression rate of NO concentration. After fermentation, the suppression rate of NO concentration was increased regardless of their concentration. But, the increase of these level was greater with 57–64% in BAW than BAL. Meanwhile, any significance differences were not detected in cell viability of group treated with BUnF, BAW and BAL. Therefore, the present results suggest that the fermentation with W. cibaria can successfully change from the roots of A. cochinchinensis to the fermented products with high anti-inflammatory activity and non-toxicity. Also, above results showed that BAW can be considered as the better candidate for suppressing the inflammatory response.
Table I.
Hyaluronidase inhibition rate, suppression rate of NO concentration and cell viability of butanol extracts of A. cochinchinensis fermented with W. cibaria and L. platarum.
| Category | Type of A. cochinchinensis | Dose | BAW (Weissella cibaria) | BAL (Lactobacillus plantarum) | |
|---|---|---|---|---|---|
| Hyaluronidase inhibition rate (%) | BUnF | Low | ND | ||
| High | 4.14±0.3 | ||||
| BF | Low | 26.95±3.5a,b | 22.43±2.7a | ||
| High | 28.35±2.9a,b | 23.96±3.4a | |||
| Suppression rate of NO concentration (%) | BUnF | Low | 7.7±1.1 | ||
| High | 13.7±1.6 | ||||
| BF | Low | 22.7±2.8a,b | 14.2±1.6 | ||
| High | 23.1±3.1a,b | 14.3±1.8 | |||
| Cell viability (%) | BUnF | Low | 92±11 | ||
| High | 97±12 | ||||
| BF | Low | 103±11 | 100±9 | ||
| High | 98±8 | 98±10 |
BUnF, Butanol extracts of unfermented A. cochinchinensis; BF, Butanol extracts of fermented A. cochinchinensis; BAW, Butanol extracts of A. cochinchinensis fermented with W. cibaria for 4.3 days; BAL, Butanol extracts of A. cochinchinensis fermented with L. plantarium for 4.3 days; Low, Low concentration of extracts; High, High concentration of extracts; ND, Not detected.
P<0.05 compared to the No treated group.
P<0.05 compared to the BAL treated group.
Change of key components in A. cochinchinensis after fermentation with W. cibaria
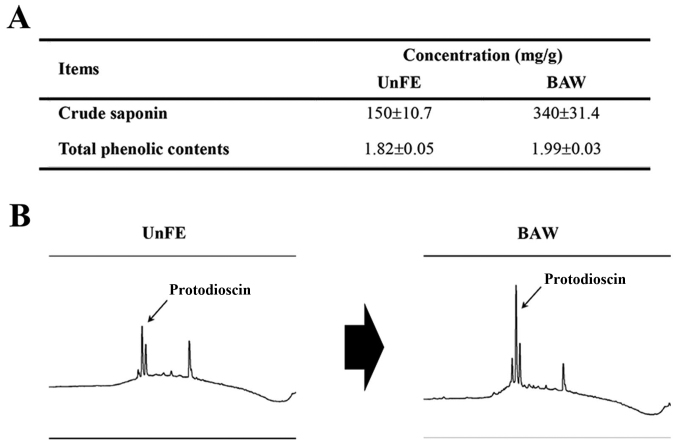
To identify the key components altered by fermentation, the concentration of several key components were analyzed in BUnF and BAW. As shown in Fig. 1A, BUnF contained significantly different concentrations of total phenolic compounds (1.82 mg/g) and total crude saponins (150 mg/g). After fermentation, the total phenolic and crude saponin concentrations in BAW were significantly increased with 9.3, 126.6%, respectively. Furthermore, the protodioscin concentration, detected as a sharp specific peak in the HPLC curve, was also higher in BAW (Fig. 1B). These results demonstrate that concentrations of several key components that associated with high anti-oxidative capacity can be increased in the extracts of roots of A. cochinchinensis after fermentation with W. cibaria.
Figure 1.
Change in components composition before and after fermentation. (A) Concentrations of two key components were measured under the conditions described in Materials and methods. (B) Chromatograms of protodioscin were obtained by performing high performance liquid chromatography of BAW. The peak height/area reflects the concentration of protodioscin in BAW.
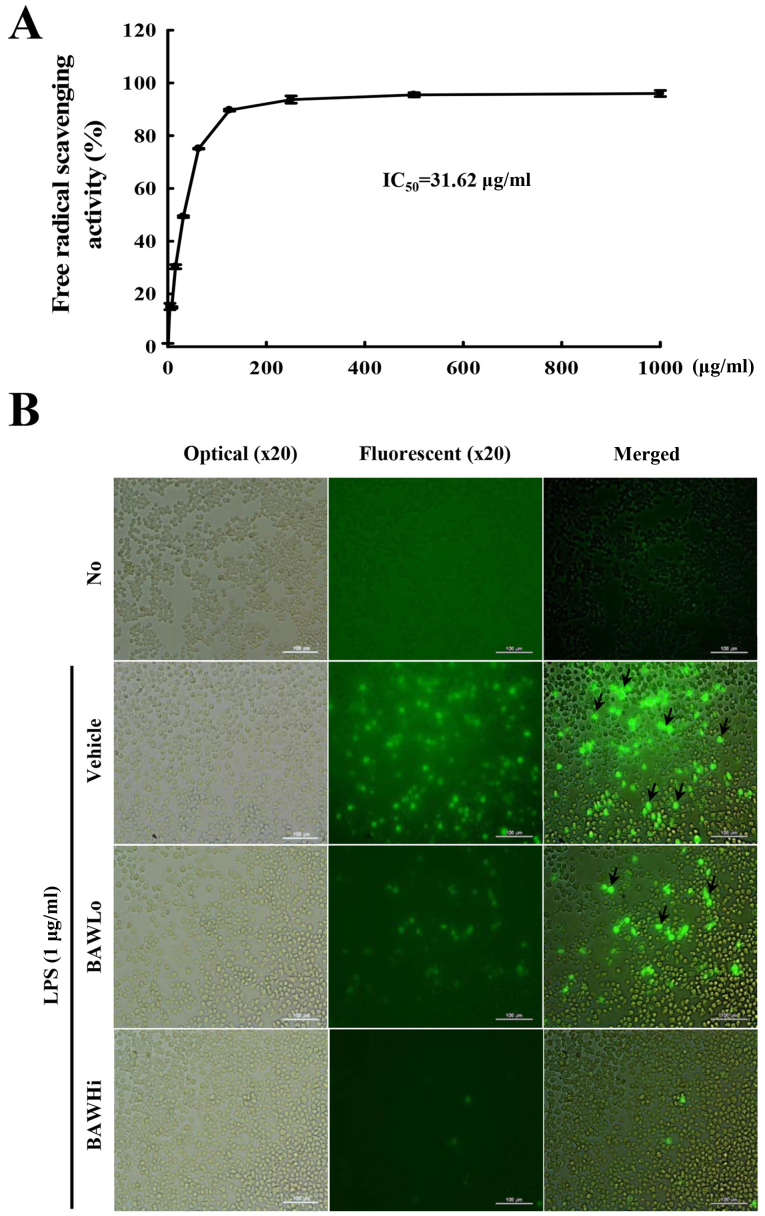
Antioxidative capacity of BAW
To investigate the antioxidative capacity of BAW, alterations in DPPH scavenging activity and the inhibitory activity of intracellular ROS production were measured in RAW264.7 cells treated with BAW. The scavenging activity against the DPPH radical was gradually enhanced with the increase in BAW concentration (7.8 and 1,000 µg/ml), and the IC50 value for BAW was 31.62 µg/ml (Fig. 2A). In addition, the intracellular level of ROS was notably enhanced after LPS treatment. However, the ROS level markedly decreased with depending on BAW concentration increase in LPS+BAWLo and LPS+BAWHi treated group (Fig. 2B). These results indicate that BAW may have a high anti-oxidative capacity that is obtained via suppression of intracellular ROS production and DPPH radical scavenging activity.
Figure 2.
Antioxidant activity of BAW. (A) DPPH radical scavenging activity was assayed in a mixture containing different concentrations of BAW. IC50 reflects the substrate concentration required to produce a 50% reduction in DPPH activity. (B) Determination of intracellular ROS production. After DCFH-DA treatment, green fluorescence in subset groups of cells was observed at 200× magnification using a fluorescence microscope (Eclipse TX100, Nikon, Tokyo, Japan). Arrows indicate cells stained with DCFH-DA.
Suppression effects on the iNOS-mediated COX-2 induction pathway
The signaling pathway for iNOS-mediated COX-2 induction has a key role during the inflammation process (25). Thus, we investigated the suppressive effects of BAW on the potential iNOS-mediated COX-2 induction pathway in LPS-activated Raw264.7 cells after BAW pretreatment. Firstly, we observed that the enhanced NO concentration after LPS treatment was dramatically decreased in the BAW-treated group (Fig. 3A). Also, the levels of the iNOS and COX-2 gene transcripts were higher in the Vehicle+LPS-treated group than that in the No-treated group. However, these levels were slightly decreased in BAWHi+LPS-treated Raw264.7 cells (Fig. 3B). These results suggest that BAW pretreatment can recover the signaling pathway for iNOS-mediated COX-2 induction during the inflammatory process.
Figure 3.
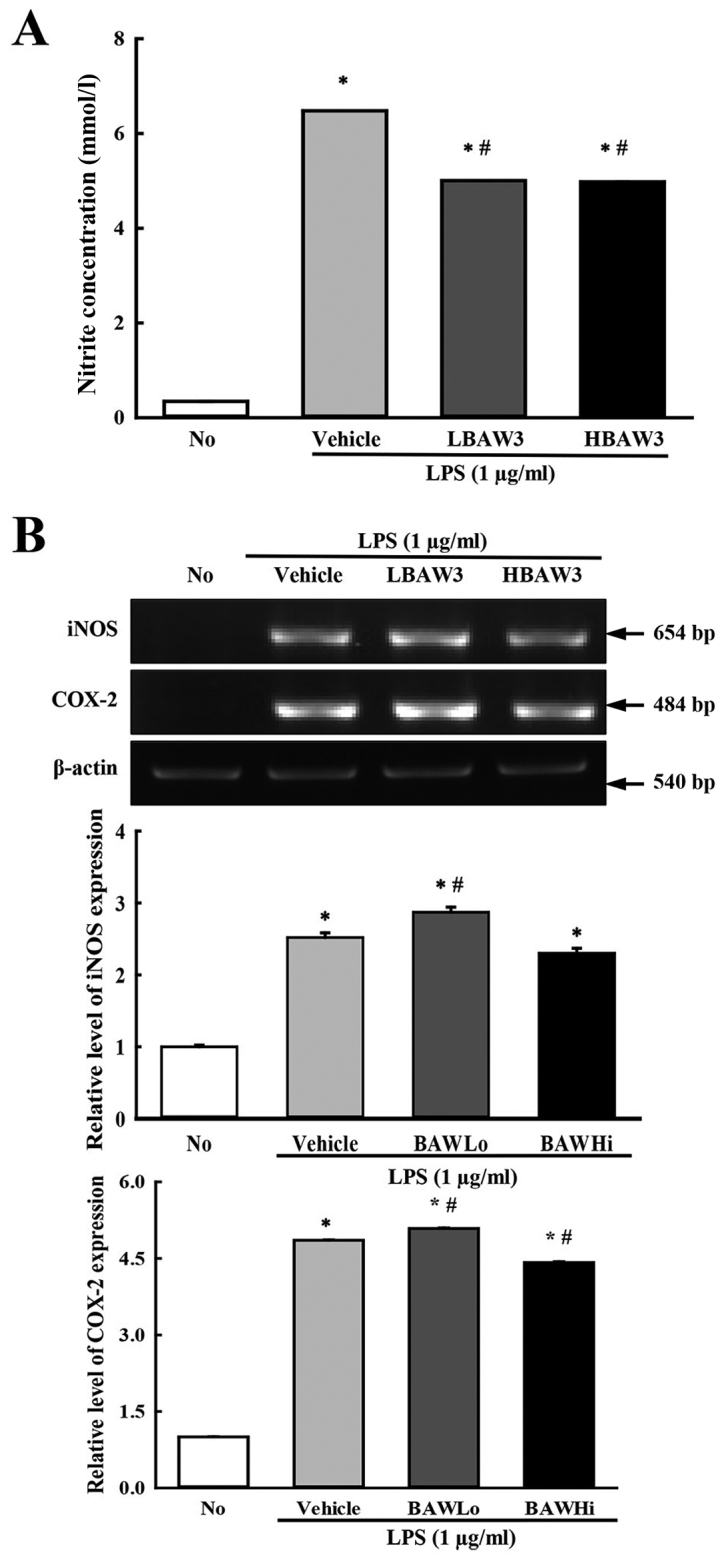
Determination of NO concentration as well as COX-2 and iNOS expressions. (A) NO concentration. The level of NO was determined by using a NO assay kit and supernatant collected from LPS-activated RAW264.7 cells treated with different concentrations of BAW. Triplicate trials per group were evaluated by NO assay. (B) RT-PCR analysis. Changes in the transcript levels of COX-2 and iNOS were examined by RT-PCR in the No-, Vehicle+LPS- and BAW+LPS-treated groups using specific primers. The data shown represent the means ± SD of three replicates. *P<0.05 relative to the No-treated group. #P<0.05 relative to the Vehicle+LPS-treated group.
To investigate whether alteration of iNOS and NO level accompanies a change in the MAP kinase pathway, the phosphorylation levels of ERK, JNK and p38 were measured in LPS-stimulated RAW 264.7 cells treated with BAW. As shown in Fig. 4, the phosphorylation levels of the three members were higher after LPS activation with various ratios than they were after No treatment. However, the levels of only ERK and JNK were significantly decreased after BAW pretreatment, while the level of p38 was continuously increased with depending on BAW concentration (Fig. 4). Therefore, the present data suggest that the suppression of iNOS and NO induced by BAW treatment may exert it regulatory activity by controlling the ERK and JNK in MAP kinase pathway.
Figure 4.
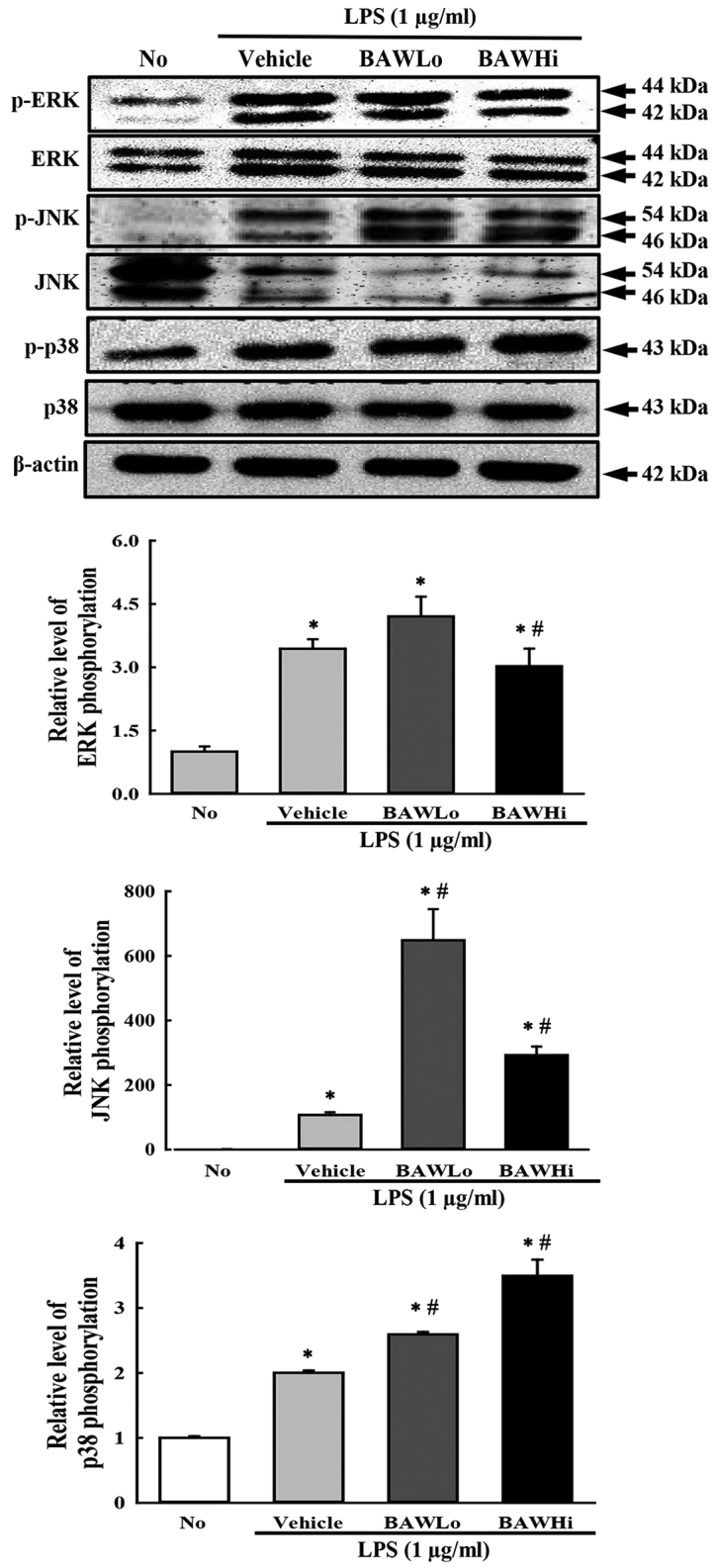
Expression of three members of the MAP kinase signaling pathway. Nitrocellulose membranes containing 30 µg of total protein from RAW264.7 cells were incubated with antibodies specific to p-ERK, ERK, p-JNK, JNK, p38, p-p38, and β-actin, followed by horseradish peroxidase-conjugated goat anti-rabbit IgG. After the intensity of each band was determined by using an imaging densitometer, the relative levels of the six proteins were calculated based on the intensity of actin protein. The data represent the means ± SD of three replicates. *P<0.05 compared to the No-treated group. #P<0.05 compared to the Vehicle+LPS-treated group.
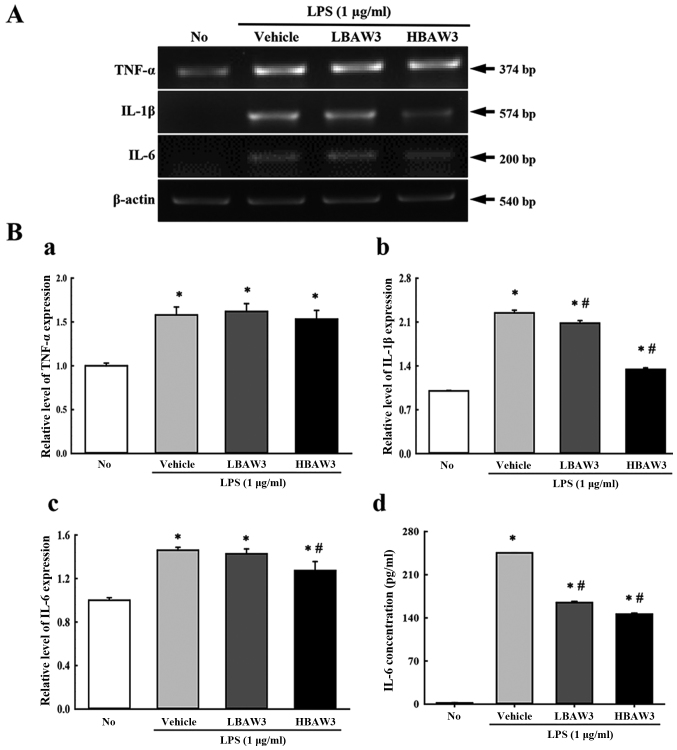
Suppression of the expression of inflammatory cytokines
To investigate alteration of the expression of pro-inflammatory and anti-inflammatory cytokines during an anti-inflammatory response induced with BAW treatment, the transcript levels of TNF-α, IL-1β, and IL-6 were measured by performing RT-PCR of LPS-activated Raw264.7 cells. Among the three cytokines, IL-1β and IL-6 showed a suppression pattern in the BAW+LPS-treated group. In contrast, the TNF-α transcript maintained a constant level (Fig. 5A and B). Furthermore, the concentration of IL-6 in the culture supernatant of LPS-activated Raw264.7 cells was measured by ELISA in order to confirm the RT-PCR results. The IL-6 concentrations in the culture supernatant completely reflected the results for the IL-6 transcripts, although a few differences were observed in the BAWLo+LPS-treated group (Fig. 5B). Therefore, these results indicate that BAW pretreatment suppresses the enhancement of pro-inflammatory cytokine expressions that were induced by LPS treatment in RAW264.7 cells.
Figure 5.
Measurement of pro-inflammatory and anti-inflammatory cytokines. The mRNA levels of the TNF-α (A and Ba), IL-1β (A and Bb), and IL-6 (A and Bc) genes were examined by RT-PCR in the No-, Vehicle+LPS-, BAWLo+LPS-, and BAWHi+LPS-treated group using specific primers. (Bd) IL-6 concentration in the culture supernatant. After collection of culture supernatant from RAW264.7 cells co-treated with BAW+LPS, IL-6 concentrations were measured by using a IL-6 ELISA kit that could detect IL-6 at 9.3 pg/ml. The data shown represent the means ± SD of three replicates. *P<0.05 relative to the No-treated group. #P<0.05 relative to the Vehicle+LPS-treated group.
Discussion
Fermentation techniques have been widely applied in the production of various high value substances because fermentation can provide economic and environmental advantages to individuals and industry (26). Moreover, many products produced by fermentation show therapeutic effects against several inflammatory diseases (27–29). In an effort to identify novel fermentation-derived candidates for the treatment of inflammatory disease, we investigated the anti-inflammatory effects of BAW in LPS-activated RAW264.7 cells. Our results demonstrated that BAW with its high anti-oxidative activity could significantly suppress the inflammatory response in LPS-activated RAW 264.7 macrophages through regulation of iNOS-mediated Cox-2 induction pathway and inflammatory cytokines expression. Thus, BAW may be considered a potential anti-inflammatory drug for use in the treatment of various chronic inflammatory diseases.
The roots of A. cochinchinesis have long been considered a therapeutic drug for various disease because their anti-inflammatory, diuretic, antiseptic, antitussive, antibacterial, nervine, sialogoue, antipyretic, and stomachic effects. In addition, they are used in combination with other natural products to treat the lungs, spleen, immune system, and aging (15,30). Furthermore, the above functions of A. cochinchinesis can be associated with some functional compounds including β-sitosterol (31), daucosterol (32), n-ethatriacontanoic acid (33), palmitic acid (34), 9-heptacosylene (35), smilagenin (36), diosgenin (37), sarsasapogenin-3-O-β-D-glucoside feeding grapes imidacloprid (38), 5-methoxy methyl furfural, yame sapogenin, diosgenin-3-O-β-D imidacloprid feeding glucose glycosides (39,40), aspacochioside D (41), iso-agatharesinoside (42) and seven steroidal saponins (43). Concentration enhancement of the above compounds has been an important issue in several recent studies. However, a fermentation technique has not been applied previously to A. cochinchinesis roots as a method to increase the concentration of functional compounds and produce novel beneficial compounds. In this study, the roots of A. cochinchinesis were fermented with W. cibaria and L. plantarum for 4.3 days. After fermentation, the hyaluronidase inhibition rate and NO suppression rate enhancement was greater in the fermentation product from W. cibaria than it was in that fermented with L. plantarum. Furthermore, the concentration of total phenols and crude saponins were significantly increased by 9.3 and 126.6% in BAW, and an increased protodioscin peak was detected. The results, therefore, indicate that the functional compounds in the roots of A. cochinchinesis may be successfully enhanced by fermenting the roots with W. cibaria.
Extracts from many fermented natural products can effectively suppress an LPS-stimulated inflammatory response. The production of pro-inflammatory mediators such as NO, iNOS, COX-2, TNF-α, and IL-6 is inhibited by the treatment of Oyaksungisan (OY) and Sipjeondaebotang (SJ) fermented by Lactobacillus (28,44), fermented Rhizoma coptidis (29), and three fermented herbs (Rhizome Atractylodes macrocephalae, Massa Medicata Fermentata, and Dolichoris Semen) (45) in LPS-stimulated RAW264.7 cells. Also, a fermented barley extract can effectively suppress oxidative stress in LPS-induced inflammation, while fermented red ginseng extract and fermented soybean extract can inhibit the production of NO in the same cells (30,46,47). Similar inhibitory effects on the production of pro-inflammatory mediators were observed in our BAW-based study, although the inhibition rate and solvent used for extraction were different. Furthermore, BAW pretreatment suppressed the level of NO, iNOS, COX-2, IL-6, IL-1β, and TNF-α in LPS-activated macrophage cells. However, additional research is needed to elucidate the key factors within BAW that control the regulation of pro-inflammatory mediators.
The iNOS and COX-2 proteins can be considered key factors when investigating the therapeutic effects of anti-inflammatory drugs because their expression can be induced by a variety of pro-inflammatory stimuli such as LPS and TNF-α in many disease conditions (48,49). Furthermore, NO production induced by iNOS expression is regulated via COX-2 expression through the MAPK signaling pathway, which has a critical role in the regulation of cell growth and differentiation, as well as in the control of cellular responses to cytokines and stresses (50,51). Some fermented natural products induce significant alteration of the iNOS-mediated COX-2 induction pathway in RAW264.7 cells. After the treatment of fermented OY extracts (27), fermented SJ extract (27), fermented soybean extract (47), and fermented RG extract (46), the levels of NO and COX-2 were significantly decreased in RAW264.7 cells. In the present study, our results for the iNOS-mediated COX-2 induction pathway obtained from BAW-treated RAW264.7 cells were very similar to those of previous studies, although some differences in the suppression of MAP kinases were observed. These differences might be due to factors such as the innate composition of, and the key molecules within, the herbal medicine.
Taken together, the results of the present study indicate that the antioxidant and anti-inflammatory activity of the roots of A. cochinchinensis can be enhanced by fermentation with W. cibaria. In addition, the results provide novel evidence that BAW may suppress inflammatory responses through the regulation of iNOS-mediated COX-2 induction pathway and inflammatory cytokine expression.
Acknowledgements
The present study was supported by grants to Dr. Dae Youn Hwang from the Korea Institute of Planning Evaluation for Technology of Food, Agriculture, Forestry and Fisheries (114034–03-1-HD030).
References
- 1.Krishnamoorthy S, Honn KV. Inflammation and disease progression. Cancer Metastasis Rev. 2006;25:481–491. doi: 10.1007/s10555-006-9016-0. [DOI] [PubMed] [Google Scholar]
- 2.Arulselvan P, Fard MT, Tan WS, Gothai S, Fakurazi S, Norhaizan ME, Kumar SS. Role of antioxidants and natural products in inflammation. Oxid Med Cell Longev. 2016;2016:5276130. doi: 10.1155/2016/5276130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henson PM, Larsen GL, Henson JE, Newman SL, Musson RA, Leslie CC. Resolution of pulmonary inflammation. Fed Pro. 1984;43:2799–2806. [PubMed] [Google Scholar]
- 4.Gautam R, Jachak SM. Recent developments in anti-inflammatory natural products. Med Res Rev. 2009;29:767–820. doi: 10.1002/med.20156. [DOI] [PubMed] [Google Scholar]
- 5.Parker KL, Schimmer BP. Genetics of the development and function of the adrenal cortex. Rev Endocr Metab Disord. 2001;2:245–252. doi: 10.1023/A:1011580314588. [DOI] [PubMed] [Google Scholar]
- 6.Ravipati AS, Zhang L, Koyyalamudi SR, Jeong SC, Reddy N, Bartlett J, Smith PT, Shanmugam K, Münch G, Wu MJ, et al. Antioxidant and anti-inflammatory activities of selected Chinese medicinal plants and their relation with antioxidant content. BMC Complement Altern Med. 2012;12:173. doi: 10.1186/1472-6882-12-173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim HY, Hwang KW, Park SY. Extracts of Actinidia arguta stems inhibited LPS-induced inflammatory responses through nuclear factor-κB pathway in Raw 264.7 cells. Nutr Res. 2014;34:1008–1016. doi: 10.1016/j.nutres.2014.08.019. [DOI] [PubMed] [Google Scholar]
- 8.Hou XL, Tong Q, Wang WQ, Shi CY, Xiong W, Chen J, Liu X, Fang JG. Suppression of inflammatory responses by dihydromyricetin, a flavonoid from Ampelopsis grossedentata, via inhibiting the activation of NF-κB and MAPK signaling pathways. J Nat Prod. 2015;78:1689–1696. doi: 10.1021/acs.jnatprod.5b00275. [DOI] [PubMed] [Google Scholar]
- 9.Oh YC, Jeong YH, Kim T, Cho WK, Ma JY. Anti-inflammatory effect of Artemisiae annuae herba in lipopolysaccharide-stimulated RAW 264.7 cells. Pharmacogn Mag. 2014;10(Suppl 3):S588–S595. doi: 10.4103/0973-1296.139793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lamichhane R, Kim SG, Poudel A, Sharma D, Lee KH, Jung HJ. Evaluation of in vitro and in vivo biological activities of Cheilanthes albomarginata Clarke. BMC Complement Altern Med. 2014;14:342. doi: 10.1186/1472-6882-14-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kim DH, Kim ME, Lee JS. Inhibitory effects of extract from G. lanceolata on LPS-induced production of nitric oxide and IL-1β via down-regulation of MAPK in macrophages. Appl Biochem Biotechnol. 2015;175:657–665. doi: 10.1007/s12010-014-1301-8. [DOI] [PubMed] [Google Scholar]
- 12.Kim H, Lee E, Lim T, Jung J, Lyu Y. Inhibitory effect of Asparagus cochinchinensis on tumor necrosis factor-alpha secretion from astrocytes. Int J Immunopharmacol. 1998;20:153–162. doi: 10.1016/S0192-0561(98)00022-8. [DOI] [PubMed] [Google Scholar]
- 13.Lee DY, Choo BK, Yoon T, Cheon MS, Lee HW, Lee YA, Kim HK. Anti-inflammatory effects of Asparagus cochinchinensis extract in acute and chronic cutaneous inflammation. J Ethnopharmacol. 2009;121:28–34. doi: 10.1016/j.jep.2008.07.006. [DOI] [PubMed] [Google Scholar]
- 14.Koo HN, Jeong HJ, Choi JY, Choi SD, Choi TJ, Cheon YS, Kim KS, Kang BK, Park ST, Chang CH, et al. Inhibition of tumor necrosis factor-alpha-induced apoptosis by Asparagus cochlnchinensis in HepG2 cells. J Ethnopharmacol. 2000;73:137–143. doi: 10.1016/S0378-8741(00)00287-7. [DOI] [PubMed] [Google Scholar]
- 15.Xiong D, Yu LX, Yan X, Guo C, Xiong Y. Effects of root and stem extracts of Asparagus cochinchinensis on biochemical indicators related to aging in the brain and liver of mice. Am J Chinese Med. 2011;39:719–726. doi: 10.1142/S0192415X11009159. [DOI] [PubMed] [Google Scholar]
- 16.Jung KH, Choi HL, Park S, Lee G, Kim M, Min JK, Min BI, Bae H. The effects of the standardized herbal formula PM014 on pulmonary inflammation and airway responsiveness in a murine model of cockroach allergen-induced asthma. J Ethnopharmacol. 2014;155:113–122. doi: 10.1016/j.jep.2014.04.029. [DOI] [PubMed] [Google Scholar]
- 17.Elson LA, Morgan WTJ. A colorimetric method for the determination of glucosamine and chondrosamine. Biochem J. 1933;27:1824–1828. doi: 10.1042/bj0271824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaegawa H, Matsumoto H, Endo K, Satoh T, Nonaka GI, Noshioka I. Inhibitory effects of tannins on hyaluronidase activation and on the degranulation from rat mesentery mast cells. Chem Pharm Bull. 1985;33:5079–5082. doi: 10.1248/cpb.33.5079. [DOI] [PubMed] [Google Scholar]
- 19.Lee KK, Kim JH, Cho JJ, Choi JD. Inhibitory effects of 150 plant extracts on elastase activity and their anti-inflammatory effects. Int J Cosmet Sci. 1999;21:71–82. doi: 10.1046/j.1467-2494.1999.181638.x. [DOI] [PubMed] [Google Scholar]
- 20.Singleton VL, Rossi JA. Colorimetry of total phenolics with phosphomolybdic-phosphotungstic acid reagents. Am J Enol Vitic. 1965;16:144–158. [Google Scholar]
- 21.Hassan SM, Al Aqil AA, Attimarad M. Determination of crude saponin and total flavonoids content in guar meal. Adv Med Plant Res. 2013;1:24–28. [Google Scholar]
- 22.Oh H, Ko EK, Kim DH, Jan KK, Park SE, Lee HS, Kim YC. Secoiridoid glucosides with free radical scavenging activity from the leaves of Syringa dilatata. Phytother Res. 2003;17:417–419. doi: 10.1002/ptr.1148. [DOI] [PubMed] [Google Scholar]
- 23.Jie S, Xueji Z, Mark B, Harry F. Measurement of nitric oxide production in biological systems by using griess reaction assay. Sensors. 2003;3:276–284. doi: 10.3390/s30800276. [DOI] [Google Scholar]
- 24.Kim JE, Park SH, Kwak MH, Go J, Koh EK, Song SH, Sung JE, Lee HS, Hong JT, Hwang DY. Characterization of changes in global genes expression in the distal colon of loperamide-induced constipation SD rats in response to the laxative effects of Liriope platyphylla. PLoS One. 2015;10:e0129664. doi: 10.1371/journal.pone.0129664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ishimura N, Bronk SF, Gores GJ. Inducible nitric oxide synthase upregulates cyclooxygenase-2 in mouse cholangiocytes promoting cell growth. Am J Physiol Gastrointest Liver Physiol. 2004;287:G88–G95. doi: 10.1152/ajpgi.00539.2003. [DOI] [PubMed] [Google Scholar]
- 26.Rahman M. Medical application of fermentation technology. Adv Mat Res. 2013;810:127–157. [Google Scholar]
- 27.Oh YC, Cho WK, Jeong YH, Im GY, Yang MC, Ma JY. Fermentation improves anti-inflammatory effect of sipjeondaebotang on LPS-stimulated RAW 264.7 cells. Am J Chin Med. 2012;40:813–831. doi: 10.1142/S0192415X12500619. [DOI] [PubMed] [Google Scholar]
- 28.Bose S, Jeon S, Eom T, Song MY, Kim H. Evaluation of the in vitro and in vivo protective effects of unfermented and fermented Rhizoma coptidis formulations against lipopolysaccharide insult. Food Chem. 2012;135:452–459. doi: 10.1016/j.foodchem.2012.05.007. [DOI] [PubMed] [Google Scholar]
- 29.Giriwono PE, Shirakawa H, Hokazono H, Goto T, Komai M. Fermented barley extract supplementation maintained antioxidative defense suppressing lipopolysaccharide-induced inflammatory liver injury in rats. Biosci Biotechnol Biochem. 2011;75:1971–1976. doi: 10.1271/bbb.110374. [DOI] [PubMed] [Google Scholar]
- 30.Xiao PG. Modern Chinese Materia Medica. Chemical Industry Press; Beijing: 2002. p. 150. [Google Scholar]
- 31.Liu YZ, Qu FY, Zhang PX. EfBFct of chloroform extract of Tiandong on the brain antioxidation of D-galactose-induced senile mice. Heilongjiang Med Pharm. 2001;24:7–8. [Google Scholar]
- 32.Ni JM, Zhao R, Wang R. Comparison on amino acid content in prepared and unprepared Asparagus cochinchinensis. Chin Tradit Herb Drugs. 1992;23:182–183. [Google Scholar]
- 33.Tenji K, Junzo S. Studies on the constituents of Asparagi Radix. I. On the structures of furostanol oligosides of Asparagus cochinchinensis (Lour.) Merr. Chem Pharm Bull. 1979;27:3086–3094. doi: 10.1248/cpb.27.3086. [DOI] [Google Scholar]
- 34.Liang ZZ, Aquino R, De Simone F, Dini A, Schettino O, Pizza C. Oligofurostanosides from Asparagus cochinchinensis. Planta Med. 1988;54:344–346. doi: 10.1055/s-2006-962453. [DOI] [PubMed] [Google Scholar]
- 35.Yang YC, Huang SY, Shi JG. Two new furostanol glycosides from Asparagus cochinchinensis. Chin Chem Lett. 2002;13:1185–1188. [Google Scholar]
- 36.Cong PZ, Keman S. Handbook of analytical chemistry-mass volume. Chemical Industry Publishing House; Beijing: 2000. pp. 296–298. [Google Scholar]
- 37.Gong YH. 13C NMR chemical shifts of natural organic compounds. Yunnan Science and Technology Publishing House; Kunming: 1986. p. 252. [Google Scholar]
- 38.Yang MH. Steroidal sapogenins of dioscorea. Chin Tradit Herb Drugs. 1981;12:43–44. [Google Scholar]
- 39.Xu CL, Chen HS, Tan XQ. Studies on the active constituents of Asparagi radix. Nat Prod Res Dev. 2005;17:128–130. [Google Scholar]
- 40.Shen Y, Chen HS, Wang Q. Studies on chemical constituents of Asparagus cochinchinensis. J Second Med Univ. 2007;28:1241–1244. [Google Scholar]
- 41.Shen Y, Xu CL, Xuan WD, Li HL, Liu RH, Xu XK, Chen HS. A new furostanol saponin from Asparagus cochinchinensis. Arch Pharm Res. 2011;34:1587–1591. doi: 10.1007/s12272-011-1001-7. [DOI] [PubMed] [Google Scholar]
- 42.Li XN, Chu C, Cheng DP, Tong SQ, Yan JZ. Norlignans from Asparagus cochinchinensis. Nat Prod Commun. 2012;7:1357–1358. [PubMed] [Google Scholar]
- 43.Zhu GL, Hao Q, Li RT, Li HZ. Steroidal saponins from the roots of Asparagus cochinchinensis. Chin J Nat Med. 2014;12:213–217. doi: 10.1016/S1875-5364(14)60035-2. [DOI] [PubMed] [Google Scholar]
- 44.Oh YC, Cho WK, Oh JH, Im GY, Jeong YH, Yang MC, Ma JY. Fermentation by Lactobacillus enhances anti-inflammatory effect of Oyaksungisan on LPS-stimulated RAW 264.7 mouse macrophage cells. BMC Complement Altern Med. 2012;12:17. doi: 10.1186/1472-6882-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bose S, Song MY, Nam JK, Lee MJ, Kim H. In vitro and in vivo protective effects of fermented preparations of dietary herbs against lipopolysaccharide insult. Food Chem. 2012;134:758–765. doi: 10.1016/j.foodchem.2012.02.175. [DOI] [PubMed] [Google Scholar]
- 46.Jung HJ, Choi H, Lim HW, Shin D, Kim H, Kwon B, Lee JE, Park EH, Lim CJ. Enhancement of anti-inflammatory and antinociceptive actions of red ginseng extract by fermentation. J Pharm Pharmacol. 2012;64:756–762. doi: 10.1111/j.2042-7158.2012.01460.x. [DOI] [PubMed] [Google Scholar]
- 47.Lee WH, Wu HM, Lee CG, Sung DI, Song HJ, Matsui T, Kim HB, Kim SG. Specific oligopeptides in fermented soybean extract inhibit NF-κB-dependent iNOS and cytokine induction by toll-like receptor ligands. J Med Food. 2014;17:1239–1246. doi: 10.1089/jmf.2013.3070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Endo K, Yoon BI, Pairojkul C, Demetris AJ, Sirica AE. ERBB-2 overexpression and cyclooxygenase-2 up-regulation in human cholangiocarcinoma and risk conditions. Hepatology. 2002;36:439–450. doi: 10.1053/jhep.2002.34435. [DOI] [PubMed] [Google Scholar]
- 49.Jaiswal M, LaRusso NF, Burgart LJ, Gores GJ. Inflammatory cytokines induce DNA damage and inhibit DNA repair in cholangiocarcinoma cells by a nitric oxide-dependent mechanism. Cancer Res. 2000;60:184–190. [PubMed] [Google Scholar]
- 50.Hemish J, Nakaya N, Mittal V, Enikolopov G. Nitric oxide activates diverse signaling pathways to regulate gene expression. J Biol Chem. 2003;278:42321–42329. doi: 10.1074/jbc.M308192200. [DOI] [PubMed] [Google Scholar]
- 51.Berghe W Vanden, Plaisance S, Boone E, Debosscher K, Schmitz ML, Fiers W, Haegeman G. p38 and extracellular signal-regulated kinase mitogen-activated protein kinase pathways are required for nuclear factor-kappaB p65 transactivation mediated by tumor necrosis factor. J Biol Chem. 1998;273:3285–3290. doi: 10.1074/jbc.273.6.3285. [DOI] [PubMed] [Google Scholar]