Abstract
Acute interstitial nephritis (AIN) is a condition in which acute kidney injury (AKI) is characterized by the histological finding of interstitial inflammation. Hyponidd is an ayurvedic drug containing Momordica charantia, Gymnema sylvestre, Swertia chirata, etc., used for the treatment of Type 2 diabetes mellitus (DM) and polycystic ovarian disease as an insulin sensitizer. There are no case reports of AIN caused by this drug yet. We report a biopsy-proven case of AKI due to severe AIN associated with the use of hyponidd tablet in a 60-year-old male with DM and hypertension. As these types of various indigenous compounds are used as home remedies in our country, awareness about the possible adverse effects of these agents among physicians is very important in the early diagnosis and management.
Keywords: Acute interstitial nephritis, ayurvedic drug, tablet hyponidd
Introduction
Acute interstitial nephritis (AIN) is a renal lesion that causes a decline in creatinine clearance and is characterized by an inflammatory infiltrate in the kidney interstitium.[1] AIN has multiple etiologies such as autoimmune disorders and other systemic diseases (e.g., systemic lupus erythematosus, Sjögren's syndrome, and sarcoidosis), infections (e.g., Legionella, leptospirosis, and streptococcal organisms), idiopathic, and drug induced. Among them, drug-induced AIN accounts for about 60%–70% of cases.[2] A definitive diagnosis of AIN is made by renal biopsy and treatment is drug withdrawal and steroids in non-responding cases.
Case Report
A 60-year-old male presented with a history of decreased urine output and pedal edema of 1-week duration. He noted a decrease in urine output about 1 week back, which progressed to complete anuria in 2–3 days. There was no history of fever or rash but he developed edema in the course of 3-day period. There was no history of dysuria, gross hematuria, or abdominal pain. He was a known case of Type 2 diabetes mellitus (Type 2 DM) and systemic hypertension for 3 years and he was on tablet metformin (500 mg) and glimiperide (2 mg) combination twice a day and tablet atenolol (50 mg) and amlodipine (50 mg) combination once in a day for 2 years. He denied the intake of nonsteroidal anti-inflammatory drugs (NSAIDs) or any other over-the-counter drugs but has taken hyponidd one tablet once daily for 7 days before the onset of his symptoms. The physical examination revealed normal temperature, pulse rate of 90/min, and blood pressure (BP) of 170/100 mmHg in all the four limbs with bilateral pitting pedal edema. Systemic examination was normal. Fundus examination did not revealed any abnormality.
At the time of admission, urea was 177 mg/dl and serum creatinine was 9.1 mg/dl. There was no previous laboratory record available for renal function. Urine analysis showed numerous red blood cells (RBCs), with numerous white blood cells (WBCs) with no WBC or RBC cast and no eosinophills. Proteinuria was present, 2+ on dipstick, but as his output was <10 ml/day, quantification of proteinuria was not done. A renal ultrasound demonstrated normal-sized kidneys (right 10.1 cm and left 10.3 cm) without evidence of hydronephrosis or nephrolithiasis. Other investigations were as follows: hemoglobin (Hb): 10.9 g/dl, total leukocyte count: 12450/cmm, differential leukocyte count: P88 L10E2, peripheral platelet count: 4.1 lakhs, bilirubin: 0.8, serum albumin: 3.6, serum globulin: 3, serum glutamic pyruvic transaminase: 42, serum glutamic oxaloacetic transaminase: 32, serum calcium: 7.8, serum phosphate: 4.4, serum uric acid: 4.8, HIV negative, Hepatitis B surface antigen negative, and anti-HCV negative. Urine culture was sterile. Anti-neutrophil cytoplasmic antibodies were negative, and C3, C4 levels were normal, and antinuclear antibody and antiglomerular basement membrane antibody testings were not done. As the patient is a known diabetic and there were no previous renal function reports, our first differential diagnosis was acute on chronic kidney disease.
We kept the second possibility as severe acute tubular necrosis, and as urine showed proteinuria and RBCs, rapidly progressive, glomerulonephritis was considered as the third possibility.
BP control was achieved over the next 2 days with oral medications and hemodialysis was done. A kidney biopsy was performed on the 3rd day of admission. The biopsy showed areas of interstitial edema with marked infiltration composed of mononuclear cells, eosinophils, few polymorphs, and macrophages [Figure 1]. The infiltrates surrounded individual tubules. Evidence of tubulitis and destruction of tubular epithelium with detached necrotic tubular cells and casts in lumen of tubules were consistent with acute tubulointerstitial nephritis. Mild interstitial fibrosis (15%–20%), along with patches of atrophic tubules and hyalinosis of arterioles, were also present. The glomeruli were unremarkable in light microscopy except for mild mesangial hypercellularity, and immunofluorescence microscopy was negative for IgG, IgM, IgA, C3, C4, C1q, kappa, and lambda. Offending drug was withdrawn immediately, and renal replacement therapy was started in the form of hemodialysis. The patient remained anuric, so on the 6th day, oral steroids were started at 1 mg/kg dose, 60 mg/day for 1 week, and then tapered and stopped at 28 days. After about 20 days of the onset of symptom (after 1 week of steroids), he started to have urine output, which progressively increased. The patient was discharged after 1 more week when he became dialysis independent and his urine output became normal. At discharge, his creatinine was 3.1 mg/dl and urine was showing 1+ protein and 5–10 WBCs, and there was no RBCs. At 2 months, his creatinine is still 1.8 mg/dl.
Figure 1.
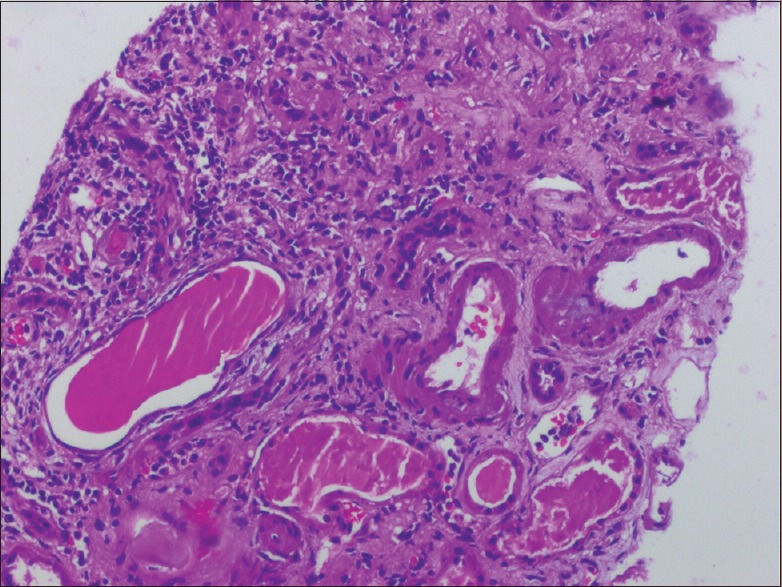
The biopsy image showing areas of interstitial edema with marked infiltration composed of mononuclear cells, eosinophils, few polymorphs, and macrophages
Discussion
AIN is a common cause of acute kidney injury (AKI). The most common cause of AIN is drugs. The first major description of drug-induced AIN was published by Baldwin et al. in a 1968 report of seven patients with AIN secondary to treatment with meticillin (also known as methicillin) or penicillin.[3] In a 2004 report of pooled data from three large studies, a drug-induced etiology emerged as the most common cause of AIN, underlying 91 of the 128 cases (71.1%).[4] The most common class of drug associated with AIN is NSAIDs, followed by antibiotics and proton pump inhibitors. The mechanism involved in the pathogenesis of drug-induced AIN is thought to be a drug-evoked allergic reaction.[5] The clinical features of AIN are highly variable with the classical triad of fever, rash, and eosinophilia, which is rarely seen.[6] The renal failure is usually nonoliguric and associated with a slow progressive rise of creatinine over days.[7] However, in severe forms of disease, the patient can present with oliguric renal failure and a rapid rise of creatinine.[7] Even though laboratory evidences in the form of eosinophilia, increased erythrocyte sedimentation rate, C-reactive protein, urinary eosinophils, etc., may provide some clue to diagnosis, the diagnosis is basically confirmed by a kidney biopsy only.[5] The treatment is mainly supportive with withdrawal of the offending agent. Even though evidences based on randomized controlled trials are lacking, steroids may be used in the treatment of resistant cases.[2,5,8]
Hyponidd tablets are ayurvedic tablets commonly used for the treatment of diabetes, conjunctivitis, joint pain, muscle pain, constipation, jaundice, and other conditions. Hyponidd tablet contains the following active ingredients: Cassia auriculata, Curcuma longa, Emblica officinalis, Eugenia jambolana, Gymnema sylvestre, Melia azadirachta, Momordica charantia, Pterocarpus marsupium, Swertia chirata, Tinospora cordifolia, and Yashad bhasma.[9] We referred to the criteria of Naranjo et al. to report an adverse drug event. A score of 6 was derived using these criteria, rating this adverse reaction as “probable.” Nephrotoxicity was attributed to this drug on the basis of the criteria of Naranjo et al., clinical onset of AKI, absence of any other nephrotoxic drugs being administered, and histopathological findings on the renal biopsy.[10] Among the various ingredients in tablet hyponidd, M. charantia and G. sylvestre have shown to produce nephrotoxicity in animal studies and both these agents are very commonly used in the management of Type 2 DM in ayurvedic practice. M. charantia in rats is found to produce tubular cell necrosis and degeneration and glomerular basement thickening.[11] Rat studies of G. sylvestre have shown that G. sylvestre produces cellular infiltration, degenerative changes, and necrosis of tubular epithelium.[12] The proposed mechanisms of kidney injury are - (1) direct toxic effect of the drug and (2) an immunologically mediated indirect injury.[12] Even though the multiple ingredients were present in the offending drug in our case, because of these data from animal studies, we presume that M. charantia and G. sylvestre could be the agents that produced AIN in our patient.
Conclusion
M. charantia and G. sylvestre are commonly used agents in the treatment of DM in ayurvedic practice. In addition, in the Indian subcontinent, juices and extracts of plants are commonly used for the control of blood sugar as a form of grandma's remedy. Many a times, the patients may not be disclosing the fact that they have consumed these preparations for glycemic control. Hence, a careful interrogation into the drug history is very important. Awareness of this adverse effect from this frequently prescribed drug is necessary for the clinicians.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Bahaa Aldeen M, Talibmamury N, Alalusi S, Nadham O, Omer AR, Smalligan RD. When coke is not hydrating: Cocaine-induced acute interstitial nephritis. J Investig Med High Impact Case Rep. 2014:2. doi: 10.1177/2324709614551557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perazella MA, Markowitz GS. Drug-induced acute interstitial nephritis. Nat Rev Nephrol. 2010;6:461–70. doi: 10.1038/nrneph.2010.71. [DOI] [PubMed] [Google Scholar]
- 3.Baldwin DS, Levine BB, McCluskey RT, Gallo GR. Renal failure and interstitial nephritis due to penicillin and methicillin. N Engl J Med. 1968;279:1245–52. doi: 10.1056/NEJM196812052792302. [DOI] [PubMed] [Google Scholar]
- 4.Baker RJ, Pusey CD. The changing profile of acute tubulointerstitial nephritis. Nephrol Dial Transplant. 2004;19:8–11. doi: 10.1093/ndt/gfg464. [DOI] [PubMed] [Google Scholar]
- 5.Rossert JA, Fischer EA. Acute interstitial nephritis. In: Johnson RJ, Feehally J, Floege J, editors. Comprehensive Clinical Nephrology. 5th ed. Philadelphia: Elsevier Saunders; 2015. pp. 728–36. [Google Scholar]
- 6.Rossert J. Drug-induced acute interstitial nephritis. Kidney Int. 2001;60:804–17. doi: 10.1046/j.1523-1755.2001.060002804.x. [DOI] [PubMed] [Google Scholar]
- 7.Kodner CM, Kudrimoti A. Diagnosis and management of acute interstitial nephritis. Am Fam Physician. 2003;67:2527–34. [PubMed] [Google Scholar]
- 8.González E, Gutiérrez E, Galeano C, Chevia C, de Sequera P, Bernis C, et al. Early steroid treatment improves the recovery of renal function in patients with drug-induced acute interstitial nephritis. Kidney Int. 2008;73:940–6. doi: 10.1038/sj.ki.5002776. [DOI] [PubMed] [Google Scholar]
- 9. [Last accessed on 2016 Nov 10]. Available from: http://www.mims.com/india/drug/info/hyponidd/hyponidd%20tab .
- 10.Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, Roberts EA, et al. A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther. 1981;30:239–45. doi: 10.1038/clpt.1981.154. [DOI] [PubMed] [Google Scholar]
- 11.Mardani S, Nasri H, Hajian S, Ahmadi A, Kazemi R, Rafieian-Kopaei M. Impact of Momordica charantia extract on kidney function and structure in mice. J Nephropathol. 2014;3:35–40. doi: 10.12860/jnp.2014.08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sujin RM, Subin RM, Mahesh R, Mary JV. The effect of anti-diabetics in kidney of rats. Ethnobotanical Lealf. 2009;13:689–701. [Google Scholar]


