Abstract
Objective:
The aim of this study was to estimate the prevalence of hearing loss (HL), self-reported occupational noise exposure, and hearing protection usage among Canadians.
Methods:
In-person household interviews were conducted with 3666 participants, aged 16 to 79 years (1811 males) with 94% completing audiometry and distortion-product otoacoustic emission (DPOAE) evaluations. Occupational noise exposure was defined as hazardous when communicating with coworkers at an arm's length distance required speaking in a raised voice.
Results:
An estimated 42% of respondents reported hazardous occupational noise exposure; 10 years or more was associated with HL regardless of age, sex or education. Absent DPOAEs, tinnitus, and the Wilson audiometric notch were significantly more prevalent in hazardous workplace noise-exposed workers than in nonexposed. When mandatory, 80% reported wearing hearing protection.
Conclusions:
These findings are consistent with other industrialized countries, underscoring the need for ongoing awareness of noise-induced occupational HL.
High levels of occupational noise exposure pose a significant risk to health, safety, and hearing acuity.1–3 It has been estimated that worldwide, 16% to 24% of hearing impairment is work-related with quantification of the health impact estimated to be over 4 million disability-adjusted life-years (DALYs).4 The DALYs is a measure of the years lost from the ideal lifespan due to morbidity and premature death, and therefore represents the gap between the current and ideal situation where everyone achieves standard life expectancy in perfect health.4
A national British survey found that occupational noise exposure (so high that a speaker needed to shout to be heard at arm's length) was responsible for severe hearing difficulties in an estimated 153,000 men and 26,000 women, aged 35 to 64 years with persistent tinnitus far more prevalent (266,000 men, 84,000 women) than hearing difficulties.5 In the US, noise-induced hearing loss (NIHL) accounted for approximately 11% of all occupational illnesses.6 The 1999 to 2004 National Health and Nutrition Examination Survey (NHANES) found that 17% of US workers reported hazardous noise exposure in their workplace.7 Several surveys have defined self-reported “hazardous” occupational noise exposure as noise “so loud it required one to speak in a raised voice to be heard” and “at arm's length” as this vocal effort suggests noise exposures exceeding 85 to 90 dBA.5,7,8
The highest occupational noise exposures and hearing loss (HL) risks were found among mining and construction workers.7,9–11 According to Tak et al,7 76% of U.S. miners reported hazardous noise exposure, while Masterson et al10 reported a HL prevalence estimate of nearly 30% among U.S. miners; lumber and manufacturing were ranked second highest for noise exposure (55% for each)7 with corresponding high HL prevalence rates for these industries as documented in a retrospective study that analyzed 1,122,722 worker audiograms.10 However, many industry types not previously associated with excessive noise such as roofing, dry cleaning, telemarketing, and education have noise exposure levels above 85 dBA over 8 hours.12,13 Recently, health care and social assistance workers were found to have a high risk of HL, ranking third highest for HL incidence (7%) during 2006 to 2010 in a retrospective U.S. study of audiograms.11 Despite hearing conservation programs, some studies have shown that proper and diligent usage of hearing protection (HP) was rare14–16 and a Cochrane meta-analyses of 24 studies found little evidence for the effectiveness of HL prevention programs.17 Although there are a few industry-specific Canadian studies, HP usage in a representative working population encompassing a variety of workplaces is unknown. One study of Albertan construction workers (n = 299) found that approximately 50% (electricians, plumbers, pipefitters) “always” used HP compared with 70.5% of boilermakers, a higher noise occupation.18 These findings are consistent with a U.S. study wherein HP usage among construction workers (n = 400) was 50% of the time or less with consistent usage (95% or more of the time) even lower (3 to 25%).19 Among Canadian lumber mill workers exposed to between 85 and 95 dBA of occupational noise, over 8 to 12 hours, high self-reported HP usage was found (73 to 84% of the time), but the authors concluded this was unlikely to provide complete protection against NIHL.20
The negative consequences related to hazardous occupational noise exposure range from NIHL, where an audiometric “threshold dip” or “hearing notch” between 4 and 6 kHz is typically noted, to depression, social isolation, and increased risk of accidents in the workplace.2,21–24 Continued noise exposure can result in HL spreading to adjacent frequencies or the notch becoming more pronounced. Most HL is insidious in onset and therefore many workers may be unaware that they are losing their hearing.25 Audiometry is traditionally used to monitor hearing in industrial workplaces; however, distortion product otoacoustic emissions (DPOAE) testing has received attention as a promising hearing surveillance tool and a potential adjunct to the audiogram in the diagnosis and monitoring of occupational NIHL.26–29 Several occupational noise studies have found that DPOAEs can detect subtle changes in cochlear function, in particular early outer hair cell damage, allowing NIHL to be identified at an early stage before audiometric HL.26,30–33
In Canada, there are no population-based studies examining workplace noise exposures across industries and HL prevalence and/or tinnitus among workers. Tinnitus frequently coexists in individuals with NIHL34,35; however, it may also serve as a warning sign that hearing is at risk.36 A Swedish population-based study found that 31% of the working population and 36% of the nonworking population, aged 16 to 64 years, had HL and/or tinnitus using self-report.37 In those aged 40 years and younger, every fifth individual reported either tinnitus or HL, with severe hearing problems already present in those who reported exposure to work-related noise.37 In Canada, an informal estimate based on provincial insurance claim data found that 9000 Canadians had hearing impairment or tinnitus attributed to occupational noise exposure.38 In Quebec39 and British Columbia,40 up to 4300 and 150,000 workers, respectively, reported daily exposure to hazardous noise levels of 100 dB or greater; however, HL and/or tinnitus prevalence rates are unknown.
The present study, based on 2012 to 2013 Cycle 3 Canadian Health Measures Survey (CHMS) data, was designed to address knowledge gaps regarding occupational noise exposure and HL in Canadian workers. The CHMS Cycle 3 Hearing Module, modeled after NHANES, included direct audiologic measures and workplace noise questions for the first time allowing national estimates based on a representative sampling of Canadians to be presented. The objectives of this study were to provide prevalence estimates of a) self-reported exposure to hazardous workplace noise, b) HP usage, c) audiometric HL, d) absent DPOAEs, and e) self-reported tinnitus, in a representative Canadian working population.
METHODS
Participants
Recruitment of Cycle 3 CHMS participants took place between January 2012 and December 2013. In this ongoing cross-sectional survey, one or two individuals per household were randomly selected from households across five regions of Canada: Atlantic, Quebec, Ontario, Prairies, and British Columbia. The CHMS excludes full-time members of the Canadian Forces, residents of the three territories, First Nations Reserves and other Aboriginal settlements, certain remote regions, and institutional residents. Despite these exclusions, CHMS data are considered to be representative of the Canadian population. Each respondent has a weight that accounts for the age and sex distribution of the population, nonresponse, and the survey sampling strategy. These weights allow frequency calculations that are representative of the population and not just the sample itself.
Individuals were invited to complete a household questionnaire and to take part in a physical measures component including a hearing evaluation. Participants who agreed to take part in the physical measures component were allotted a $100 honorarium. The response rate for participants, aged 16 to 79 years, was 88.4% for the household questionnaire and 78.8% for the hearing evaluation component. Proxy interviews were accepted in cases of physical and/or intellectual impairment. See CHMS Data User Guide Cycle 341 for additional details. Figure 1 identifies exclusions and the derivation of the final unweighted study sample for audiometry.
FIGURE 1.
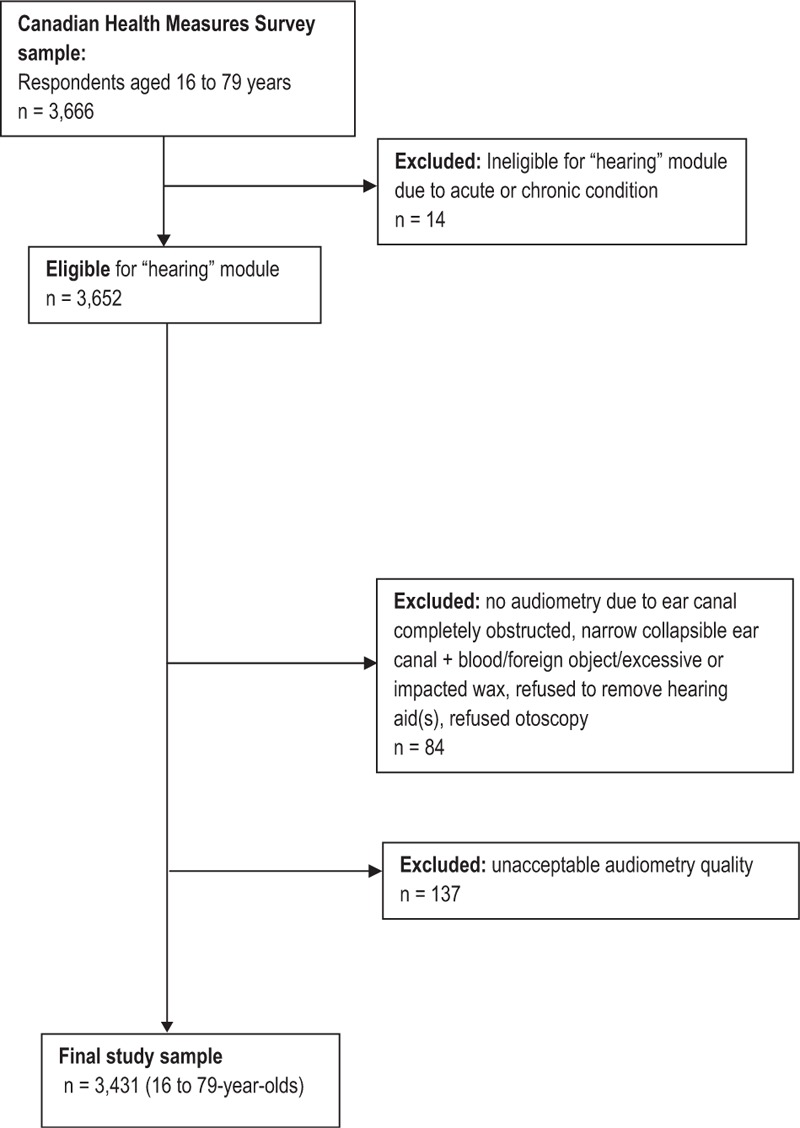
Final study sample (unweighted) for audiometry. The final study sample includes 3,431 16- to 79-Year-olds with valid audiometric results in both ears.
Household in-person interviews/questionnaires including occupation-related questions were administered to participants, aged 16 to 79 years (n = 3667). The analysis for hearing, based on individuals with valid bilateral audiometric results, comprised 3431 participants, representing 25.3 million Canadians (12.6 million males, 12.7 million females).
Data Collection
Household Questionnaire
Self-reported data were collected in-person, in English or French, using a computer-assisted personal interview to gather demographic, socioeconomic, health, and lifestyle information, including type of occupation and noise exposure history.41 To estimate past and current exposure to hazardous occupational noise, participants were asked: “At any time in your life, have you worked in a noisy environment? By noisy, I mean so loud that you and your co-workers had to speak in a raised voice to be understood by or communicate with someone standing an arm's length away.” Those who responded “yes” were asked if they currently worked in a noisy environment. Individuals who indicated either “no” or that they had never worked in a noisy environment were grouped together. Participants who replied affirmatively to having ever worked in a noisy environment at any time in their life were asked about 1) duration (less than 12 months, 1 to less than 5 years, 5 to less than 10 years, 10 years or more), 2) whether they were required to wear HP at work (yes, no), and 3) how often they used HP at work when in a noisy area (always, often, sometimes, rarely, never). The latter two variables were combined to group participants into four distinct groups based on whether they were required to and used HP (required and used always or often, required but did not use, not required but used, not required and not used).
Participants were also asked to indicate the source of loud noise at work. Due to small sample sizes, the following noise exposure categories were formed: Machinery (ie, bulldozers, backhoes, sawmill equipment) that included transportation noise sources (ie, trains, airplanes, cars, trucks); loud “people noise” was combined with concert music or other amplified music sources; noise from munitions (ie, guns, cannons) was combined with the “other” category, that is, unspecified loud noise sources.
Participants were also asked whether they had ever experienced tinnitus, described as “the presence of hissing, buzzing, ringing, rushing or roaring sounds in your ears when there is no other sound around you.” Those who replied affirmatively were asked when they last experienced tinnitus (within the last 7 days, 8 days to less than a month ago, 1 month to less than 6 months ago, 6 months to less than 1 year ago, 1 year ago or more). Individuals who experienced tinnitus in the past month were asked: “When it is quiet, do you experience these sounds in your ears?” (always, often, sometimes, rarely, never) and those who responded “always” or “often” were asked how long they had had tinnitus. Responses were dichotomized into “less than 5 years” or “5 years or longer.” Participants who had experienced tinnitus within the past year were asked: “Did this bother you? For example, did it affect your sleep, concentration or mood?” Participants who responded affirmatively to this question were categorized as having “bothersome” tinnitus.
Physical Measures
Participants were evaluated in a mobile examination clinic (MEC). The possibility that a temporary threshold shift (ie, a temporary increase in hearing threshold following loud noise exposure) may have influenced measurements was considered by asking participants to recall their exposure to loud noise/music in the 24 hours before testing. While loud noise/music exposure was reported by 7.8% of the study sample, no significant differences were observed in four frequency pure tone average HL between the exposed and nonexposed group.
All testing was carried out by health measures specialists with training/supervision provided by a certified audiologist who conducted periodic on-site visits to ensure quality control. Hearing tests, with the exception of otoscopy and tympanometry, were carried out while participants were seated in a portable audiometric booth (Eckel, AB-4230; Eckel Industries of Canada Ltd, Morrisburg, Ontario, Canada), with the door closed. Individuals who refused or had apparent cognitive deficits that could potentially interfere with testing were excluded from DPOAE testing and audiometric evaluation.
Ambient Sound Level Measurements
A Casella CEL-633 sound level meter monitored ambient sound pressure levels inside the sound booth. Testing was paused if sound pressure levels exceeded 55 dB for more than 2 seconds.
Hearing Evaluation Protocol
The testing consisted of otoscopy, tympanometry, DPOAEs, and audiometric evaluation (0.5 to 8 kHz). Before testing, a visual inspection of the pinna and ear canal was performed to identify possible signs of infection, obstruction, and other conditions/circumstances that might interfere with testing.
Otoscopy was performed using the Welch Allyn otoscope (Model 25020; Welch Allyn Inc, Skaneateles Falls, NY) to identify gross abnormalities, including the presence of blood, pus, excessive or impacted ear wax, a growth, tumor or foreign object in the ear canal, a collapsed ear canal, or other occlusion. Criteria for otoscopic exclusion included obstructed ear canal, acute pain or infection, open wounds or bandages covering the ear(s), refusal to remove hearing aid, or chronic abnormalities, including congenital atresia or microtia of the ear canal (one or both ears). No further testing was performed if the individual was excluded by otoscopy (see Fig. 1).
Tympanometry was conducted using the GSI 39 Auto Tympanometer (Grason-Stadler, Eden Prairie, MN). A normal tympanogram was defined as compliance between 0.2 and 1.8 cm3 with middle ear pressure between −150 and +50 daPa in an equivalent ear canal volume of between 0.75 and 2.0 cm3. Tympanometry was not administered when blood, pus or impacted wax, eardrum perforation, growth in the ear canal, and/or significant skin abnormality or discharge was observed during otoscopy.
Audiometric evaluation was carried out using a computer-controlled CCA-100 mini audiometer (Benson Medical Instruments, Minneapolis, MN) with insert earphones (EAR 5A case; 3M Auditory Systems, Indianapolis, IN). In cases where a participant was excluded from tympanometry for the reasons noted above, audiometry was performed using supra-aural headphones (TDH-39; Interacoustics USA, Eden Prairie, MN) instead of insert earphones. The audiometer was calibrated daily using the Bio-Acoustic simulator BAS-200 (Benson Medical Instruments, Minneapolis, MN), which served as a baseline. Hearing thresholds were assessed at 0.5, 1, 2, 3, 4, 6, and 8 kHz. Testing followed procedures recommended for standard audiometry using automatic mode, except when the respondent could not physically press the response button, had very slow response times, or when difficulties were noted with automatic mode. Manual mode was carried out using the modified Hughson–Westlake ascending method.42 To avoid interference with audiometric evaluation, subjects were asked to refrain from chewing.
DPOAE testing was conducted using the OtoRead Standard and Clinical-OAE instrument and OtoAccess software program. The OtoRead instrument indicates “Pass” or “Refer” following DPOAE test administration for each ear. “Refer” is equivalent to an absent DPOAE. The custom protocol set for the instrument required that the individual “Pass” three out of four test frequencies (2, 3, 4, and 5 kHz) using a signal-to-noise ratio of 6 dB. DPOAE was not administered when otoscopic examination could not be conducted or in cases of bilateral occlusions, presence of blood, a foreign object/substance in both ears, impacted wax in both ears, the participant was unwilling or unable to remove his/her hearing aids from both ears.
Definitions
HL was defined as an impairment of more than 20 dB HL for 16 to 18 year olds and at least 26 dB HL for 19 year olds or older, in one or more of the following pure tone averages: four frequency (0.5, 1, 2, and 4 kHz) pure tone average (FFPTA), high frequency (3, 4, 6, and 8 kHz) pure tone average (HFPTA), low frequency (0.5, 1, and 2 kHz) pure tone average (LFPTA). An adult HL threshold (≥26 dB) was applied to participants over 18 years olds in accordance with the American Academy of Audiologists (AAA) and the American Speech Language Hearing Association (ASHA) pediatric/childhood audiologic screening guidelines.43,44 Individuals with either bilateral or unilateral loss were classified as having hearing impairment. For bilateral HL, the average in the worse ear was used to categorize the degree of hearing impairment.
An audiometric “notch” was defined using two different definitions:
-
a)
Thresholds at 2 and 8 kHz are both minimally at hearing levels 10 dB lower or better than the threshold at 4 kHz, unilaterally or bilaterally.45
-
b)
Thresholds at 0.5 and 1 kHz are less than or equal to 15 dB, and the maximal threshold at 3, 4, or 6 kHz is greater than or equal to 15 dB higher or worse than the highest threshold for 0.5 and 1 kHz, and the threshold at 8 kHz is greater than or equal to 10 dB lower or better than the maximal threshold for 3, 4, or 6 kHz, unilaterally or bilaterally.46
“White collar” and “blue collar” occupations were categorized on the basis of a variant of the National Occupational Classification (NOC) developed jointly by Statistics Canada and Employment and Social Development Canada and utilized widely as a nationally accepted reference on occupations in Canada.47 Occupations in categories A to F (management, professional, technical and paraprofessional, administration and administrative support, sales, personal and customer information services) were classified as “white collar,” while jobs in categories G to J (industrial, construction and equipment operation trades, workers and laborers in transport and construction, natural resources, agriculture and related production occupations, occupations in manufacturing and utilities) were classified as “blue collar.”
Statistical Analysis
Weighted frequencies and cross-tabulations were used to explore work-related characteristics (noisy environment, HP) by demographic characteristics. Bivariate analyses included HL, the presence of an audiometric notch pattern (definition a or b) and absent DPOAE by selected demographic and work-related characteristics. All estimates were weighted at the person level to represent the population. Logistic regression was conducted to determine if longer duration in a noisy work environment was associated with HL, notch pattern, or absent DPOAE while controlling for demographic factors (sex, age, and household education). Analyses were conducted using SAS (version 9.3; SAS Institute Inc, Cary, NC) and SAS-Callable SUDAAN (version 11.0.0; SAS Institute Inc, Cary, NC) software. To account for the complex survey design, P values, 95% confidence intervals, and coefficients of variation (CVs) were estimated using the bootstrap technique with 11 degrees of freedom.48,49 Statistical significance was specified as a P value of less than 0.05. The CV is a measure of data quality and provides an indication of the scope of the sampling error associated with the estimate. The CV is obtained by dividing the standard error of the estimate by the estimate itself, and is expressed as a percentage of the estimate: SE/Estimate x 100 = CV. CV estimates between 16.6% and 33.3% were flagged “E” indicating a marginally acceptable estimate due to the high sampling variability associated with it, and advising users to interpret with caution. CV estimates that exceeded 33.3% were designated “F” indicating that these data could not be released as it is of questionable validity.
RESULTS
Hazardous Occupational Noise Exposure
Among participants, aged 16 to 79 years, an estimated 42% [95% confidence interval (95% CI), 36.5 to 47.8], representing 11.2 million Canadians, reported current or past hazardous occupational noise exposure, defined as “so loud that one had to speak in a raised voice to communicate with co-workers standing within an arm's length” with significantly more men (P < 0.01; 61%; 95% CI, 53.9 to 67.3) than women (24%; 95% CI, 17.4 to 30.9) reporting this exposure (Table 1). Approximately 14% (95% CI, 11.0 to 17.0) of participants representing 3.7 million Canadians reported that they currently were exposed to hazardous occupational noise, with significantly more men than women exposed (P < 0.01; 22% of men; 95% CI, 16.8 to 27.5; 6%E of women; 95% CI, 4.0 to 8.6). Participants without a post-secondary education were significantly more likely to have worked in a noisy environment (P < 0.05; 48% versus 41% for post-secondary graduates, respectively).
TABLE 1.
Self-Reported Prevalence of Occupational Noise Exposure in Canadians, Aged 16 to 79 years: Demographic Characteristics
| Currently Working in a Noisy Environment (n = 3,645) | Ever Worked in a Noisy Environment (n = 3,646) | Worked 5 or More Years in a Noisy Environment (Among 42% Who Had Worked in a Noisy Environment) | |||||||||||||||||||||||||
| 95% CI | 95% CI | 95% CI | |||||||||||||||||||||||||
| Characteristics | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * |
| ’000 | ’000 | ’000 | |||||||||||||||||||||||||
| Total | 454 | 3,667 | 13.7 | 1.3 | 11.0 | 17.0 | 1,500 | 11,240 | 42.0 | 2.6 | 36.5 | 47.8 | 735 | 5,321 | 47.4 | 2.0 | 43.0 | 51.8 | |||||||||
| Sex | |||||||||||||||||||||||||||
| Men | 352 | 2,876 | 21.7 | 2.4 | 16.8 | 27.5 | ‡ | 1,058 | 8,080 | 60.8 | 3.1 | 53.9 | 67.3 | ‡ | 540 | 4,253 | 52.7 | 3.1 | 45.8 | 59.4 | ‡ | ||||||
| Women† | 102 | 791 | E | 5.9 | 1.0 | 4.0 | 8.6 | E | 442 | 3,160 | 23.5 | 3.1 | 17.4 | 30.9 | 195 | 1,068 | 33.8 | 3.8 | 26.1 | 42.5 | |||||||
| Age group | |||||||||||||||||||||||||||
| 16–29 years† | 113 | 1,178 | 18.3 | 2.1 | 14.2 | 23.4 | 295 | 2,619 | 40.7 | 3.7 | 33.0 | 49.0 | 38 | 445 | E | 17.0 | 4.2 | 9.6 | 28.2 | E | |||||||
| 30–49 years | 216 | 1,590 | E | 16.8 | 3.7 | 10.2 | 26.5 | E | 612 | 4,333 | 45.8 | 5.0 | 35.2 | 56.8 | 270 | 1,848 | E | 42.7 | 4.6 | 32.9 | 53.1 | ‡ | |||||
| 50–79 years | 125 | 898 | E | 8.3 | 1.4 | 5.7 | 11.9 | E | ‡ | 593 | 4,288 | 39.5 | 2.5 | 34.2 | 45.1 | 427 | 3,028 | 70.6 | 3.1 | 63.5 | 76.9 | ‡ | |||||
| Education (highest level in household) | |||||||||||||||||||||||||||
| Post secondary or more† | 329 | 2,476 | 12.5 | 1.7 | 9.2 | 16.6 | 1,081 | 8,090 | 40.7 | 2.7 | 34.8 | 46.8 | 503 | 3,444 | 42.6 | 2.8 | 36.6 | 48.8 | |||||||||
| Less than post-secondary | 110 | 1,065 | E | 18.1 | 3.1 | 12.2 | 26.0 | E | 374 | 2,828 | 48.1 | 3.0 | 41.6 | 54.8 | * | 215 | 1,701 | 60.2 | 6.5 | 45.5 | 73.2 | ||||||
| Household income | |||||||||||||||||||||||||||
| <$50,000† | 142 | 1,142 | 12.2 | 1.8 | 8.7 | 16.9 | 614 | 4,123 | 44.1 | 3.2 | 37.3 | 51.2 | 326 | 2,134 | 51.8 | 4.8 | 41.2 | 62.2 | |||||||||
| $50,000–<$100,000 | 187 | 1,343 | E | 14.9 | 2.5 | 10.1 | 21.3 | E | 505 | 3,643 | 40.3 | 3.0 | 33.9 | 47.0 | 258 | 1,877 | 51.6 | 4.9 | 40.9 | 62.0 | |||||||
| $100,000 or more | 125 | 1,181 | E | 14.2 | 2.4 | 9.6 | 20.4 | E | 381 | 3,474 | 41.6 | 3.6 | 34.1 | 49.6 | 151 | 1,311 | 37.7 | 4.6 | 28.2 | 48.3 | |||||||
E use with caution (coefficient of variation 16.6–33.3%).
*Significantly different from estimate for reference category (P < 0.05).
†Reference category.
‡Significantly different from estimate for reference category (P < 0.01).
Source: 2012/2013 Canadian Health Measures Survey (Cycle 3).
Among participants who had ever worked in a noisy work environment, significantly more men (53%) than women (34%) had done so for at least 5 years or more (Table 1). Overall, an estimated 3.5 million Canadians have spent at least 10 years in noisy workplaces. Among those who worked in a noisy environment for less than 10 years, there were no significant differences between men and women (Table 2). However, among those who had ever worked in a noisy environment, men were significantly more likely than women to have done so for 10 years or more (P < 0.05; 36% compared with 20%E, respectively). Among individuals who had ever worked in a noisy workplace, 36% indicated that HP was required in their jobs and of those, 79.7% reported they “always” or “often” complied (Table 3). Overall, among those who had ever worked in a noisy environment, regardless of whether they were required to wear HP in their jobs, 38.2% indicated they “always” or “often” used HP (Table 3).
TABLE 2.
Self-Reported Occupational Noise Exposure Duration (in Years) Among Canadian Men and Women, Aged 16 to 79 Years
| Both Sexes† | Men† | Women† | |||||||||||||||||||||||
| 95% CI | 95% CI | 95% CI | |||||||||||||||||||||||
| n | N | CV | % | SE % | From | To | CV | n | N | CV | % | SE % | From | To | CV | n | N | CV | % | SE % | From | To | CV | * | |
| Time worked in a noisy environment | ’000 | ’000 | ’000 | ||||||||||||||||||||||
| Less than 1 year | 368 | 2,680 | 23.8 | 3.4 | 17.1 | 32.2 | 257 | 1,732 | 21.4 | 3.8 | 14.2 | 31.1 | E | 111 | 948 | 30.0 | 4.3 | 21.5 | 40.2 | ||||||
| 1 year to less than 5 years | 395 | 3,236 | 28.8 | 3.4 | 22.0 | 36.7 | 259 | 2,092 | 25.9 | 3.2 | 19.6 | 33.4 | 136 | 1,144 | E | 36.2 | 6.3 | 23.7 | 50.9 | E | |||||
| 5 years to less than 10 years | 211 | 1,806 | 16.1 | 1.3 | 13.4 | 19.1 | 136 | 1,382 | 17.1 | 1.7 | 13.7 | 21.1 | 75 | 424 | E | 13.4 | 2.3 | 9.1 | 19.3 | E | |||||
| 10 years or more | 524 | 3,516 | 31.3 | 2.1 | 26.9 | 36.0 | 404 | 2,871 | 35.5 | 3.4 | 28.4 | 43.4 | 120 | 644 | 20.4 | 3.5 | 13.7 | 29.3 | E | * | |||||
Number and percentage worked in a noisy environment by time worked and sex, household population aged 16–79 years, Canada excluding territories, 2012/2013.
E use with caution (coefficient of variation 16.6–33.3%).
*Significantly different from estimate for men (P < 0.05).
†Among respondents who have ever worked in a noisy environment.
Source: 2012/2013 Canadian Health Measures Survey (Cycle 3).
TABLE 3.
Self-Reported Hearing Protection Usage at Work Among Canadians, Aged 16 to 79 Years
| Always or Often Use Hearing Protection at Work, Among Workers‡ | Required to Use Hearing Protection at Work‡ | Always or Often Use Hearing Protection at Work, Among Those Required to Use Protection | Always or Often Use Hearing Protection at Work, Among Those Not Required to Use Protection | |||||||||||||||||||||||||||||||||
| 95% CI | 95% CI | 95% CI | 95% CI | |||||||||||||||||||||||||||||||||
| Characteristics | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * |
| ’000 | ’000 | ’000 | ’000 | |||||||||||||||||||||||||||||||||
| Total | 508 | 4,182 | 38.2 | 2.7 | 32.4 | 44.3 | 496 | 3,962 | 36.1 | 2.9 | 30.1 | 42.6 | 373 | 3,153 | 79.7 | 3.0 | 72.3 | 85.4 | 135 | 1,029 | E | 14.7 | 2.8 | 9.6 | 22 | E | ||||||||||
| Sex | ||||||||||||||||||||||||||||||||||||
| Men | 408 | 3,350 | 42.8 | 3.8 | 34.7 | 51.2 | * | 391 | 3,161 | 40.3 | 4.2 | 31.4 | 49.9 | 288 | 2,431 | 77.0 | 3.8 | 67.7 | 84.3 | 120 | 919 | E | 19.7 | 3.3 | 13.3 | 28 | E | |||||||||
| Women† | 100 | 832 | E | 26.6 | 5.2 | 16.8 | 39.6 | E | 105 | 801 | E | 25.7 | 4.9 | 16.4 | 37.8 | E | 85 | 722 | E | 90.1 | 5.1 | 72.0 | 97.0 | F | F | |||||||||||
| Age group | ||||||||||||||||||||||||||||||||||||
| 16–29 years† | 96 | 998 | E | 39.6 | 6.9 | 25.7 | 55.4 | E | 85 | 876 | E | 34.8 | 6.2 | 22.7 | 49.3 | E | 69 | 757 | E | 86.4 | 6.1 | 67.0 | 95.2 | 27 | 241 | E | F | |||||||||
| 30–49 years | 244 | 1.818 | E | 42.7 | 5.3 | 31.7 | 54.5 | 239 | 1,777 | E | 41.7 | 3.9 | 33.4 | 50.5 | 186 | 1,385 | E | 77.9 | 5.8 | 62.6 | 88.2 | F | F | |||||||||||||
| 50–79 years | 168 | 1,365 | 32.7 | 3.1 | 26.2 | 39.9 | 172 | 1,309 | 31.3 | 3.4 | 24.4 | 39.1 | 118 | 1,011 | 77.5 | 4.9 | 65.1 | 86.4 | 50 | 355 | E | 12.3 | 3.7 | 6.3 | 22.9 | E | ||||||||||
| Education (highest level in household) | ||||||||||||||||||||||||||||||||||||
| Post secondary or more† | 367 | 2,842 | 35.9 | 3.1 | 29.4 | 43 | 366 | 2,937 | 37.1 | 3.2 | 30.4 | 44.3 | 274 | 2,300 | 78.5 | 3.1 | 70.8 | 84.5 | 93 | 542 | E | 10.9 | 2.9 | 6 | 18.9 | E | ||||||||||
| Less than postsecondary | 128 | 1,210 | E | 44.5 | 4.9 | 34.2 | 55.3 | 119 | 945 | E | 34.7 | 5.0 | 24.7 | 46.3 | 93 | 790 | E | 83.6 | 6.3 | 65.1 | 93.3 | 35 | 420 | E | 23.6 | 5.1 | 14.3 | 36.5 | E | * | ||||||
| Household income | ||||||||||||||||||||||||||||||||||||
| <$50,000† | 189 | 1,533 | 38.6 | 3.7 | 30.9 | 47 | 181 | 1,241 | 31.2 | 3.0 | 25.0 | 38.3 | 135 | 987 | E | 79.9 | 5.5 | 65.2 | 89.4 | 54 | 545 | E | 20 | 5.5 | 10.5 | 34.8 | E | |||||||||
| $50,000–<$100,000 | 171 | 1,140 | 31.9 | 3.2 | 25.3 | 39.2 | 180 | 1,298 | 36.3 | 4.1 | 27.8 | 45.7 | 128 | 943 | 72.7 | 4.8 | 61.0 | 81.9 | 43 | 197 | E | 8.6 | 2.4 | 4.6 | 15.7 | E | ||||||||||
| $100,000 or more | 148 | 1,509 | E | 44.2 | 6.5 | 30.7 | 58.7 | 135 | 1,423 | E | 41.7 | 6.1 | 29.2 | 55.4 | 110 | 1,222 | E | 85.9 | 5.3 | 70.1 | 94.1 | 38 | 287 | E | 14.4 | 4.1 | 7.5 | 25.8 | E | |||||||
E use with caution (coefficient of variation 16.6–33.3%).
*Significantly different from estimate for reference category (P < 0.05).
†Reference category.
‡Among respondents who have ever worked in a noisy environment.
Source: 2012/2013 Canadian Health Measures Survey (Cycle 3).
“Blue collar” compared with “white collar” workers were significantly more likely to have 1) HL in one or more categories (FFPTA, HFPTA, LFPTA) (P < 0.05), 2) an absent DPOAE (P < 0.01), 3) a notch pattern consistent with both definitions (P < 0.01) (Tables 4 to 9).
TABLE 4.
Prevalence of Audiometric Hearing Loss Among Working Canadians, Aged 16 to 79 Years: Demographics
| FFPTA (n = 3,431) | HFPTA (n = 3,431) | LFPTA (n = 3,431) | |||||||||||||||||||
| >20 dB (16–18 Years) | |||||||||||||||||||||
| >25 dB (19–79 Years) | 95% CI | 95% CI | 95% CI | ||||||||||||||||||
| Characteristics | n | N | % | SE % | From | To | n | N | % | SE % | From | To | n | N | % | SE % | From | To | * | ||
| ’000 | ’000 | ’000 | |||||||||||||||||||
| Total | 665 | 4,632 | 18.3 | 1.0 | 16.1 | 20.7 | 1,214 | 8,520 | 33.7 | 1.0 | 31.5 | 35.9 | 535 | 3,744 | 14.8 | 0.8 | 13.1 | 16.7 | |||
| Demographic characteristics | |||||||||||||||||||||
| Sex | |||||||||||||||||||||
| Men | 401 | 3,018 | 24.0 | 2.1 | 19.7 | 28.9 | ‡ | 695 | 4,895 | 38.9 | 2.1 | 34.5 | 43.5 | * | 291 | 2,212 | 17.6 | 1.3 | 14.9 | 20.6 | ‡ |
| Women† | 264 | 1,614 | 12.7 | 1.0 | 10.7 | 15.1 | 519 | 3,624 | 28.5 | 2.2 | 24.0 | 33.5 | 244 | 1,532 | 12.0 | 1.0 | 10.0 | 14.5 | |||
| Age group | |||||||||||||||||||||
| 16–29 years years† | 36 | 369 | 5.9 | 1.8 | 3.0 | 11.4 | e,E | 55 | 455 | 7.3 | 2.1 | 3.8 | 13.4 | e,E | 39 | 399 | 6.4 | 1.8 | 3.4 | 11.8 | e,E |
| 30–49 years | 98 | 805 | 9.1 | 1.5 | 6.3 | 13.0 | e | 199 | 1,386 | 15.7 | 2.2 | 11.5 | 21.1 | * | 95 | 842 | 9.5 | 1.3 | 7.1 | 12.7 | |
| 50–79 years | 531 | 3,458 | 33.8 | 1.7 | 30.3 | 37.6 | ‡ | 960 | 6,678 | 65.4 | 1.8 | 61.3 | 69.2 | ‡ | 401 | 2,502 | 24.5 | 1.5 | 21.4 | 27.8 | ‡ |
| Education (highest level in household) | |||||||||||||||||||||
| Post secondary or more† | 427 | 2,920 | 15.5 | 1.3 | 12.8 | 18.5 | 822 | 5,764 | 30.5 | 1.7 | 26.9 | 34.4 | 352 | 2,421 | 12.8 | 1.0 | 10.7 | 15.3 | |||
| Less than postsecondary | 219 | 1,560 | 28.4 | 2.9 | 22.5 | 35.2 | ‡ | 354 | 2,446 | 44.5 | 4.6 | 34.7 | 54.8 | * | 169 | 1,229 | 22.4 | 3.2 | 16.2 | 30.1 | * e |
| Household income | |||||||||||||||||||||
| <$50,000† | 338 | 2,316 | 26.8 | 2.0 | 22.6 | 31.4 | 565 | 3,544 | 41.0 | 2.5 | 35.6 | 46.6 | 281 | 1,819 | 21.0 | 1.8 | 17.4 | 25.3 | |||
| $50,000 to <$100,000 | 204 | 1,344 | 15.7 | 1.8 | 12.1 | 20.0 | ‡ | 392 | 2,668 | 31.1 | 1.4 | 28.2 | 34.2 | * | 146 | 1,019 | 11.9 | 1.4 | 9.1 | 15.4 | ‡ |
| $100,000 or more | 123 | 972 | 12.0 | 3.1 | 6.7 | 20.6 | ‡ e,E | 257 | 2,308 | 28.6 | 3.1 | 22.2 | 36.0 | * | 108 | 906 | 11.2 | 2.9 | 6.2 | 19.4 | * e,E |
Any hearing loss: FFPTA and/or HFPTA and/or LFPTA.
e, E use with caution (coefficient of variation 16.6–33.3%), population size and %, respectively.
f, F too unreliable to be published (coefficient of variation greater than 33.3%), population size and %, respectively.
DPOAE, distortion product otoacoustic emissions; FFPTA, four-frequency pure tone average over frequencies (0.5, 1, 2, and 4 kHz); HFPTA, high-frequency pure tone average over frequencies (3, 4, 6, and 8 kHz); LFPTA, low-frequency pure tone average over frequencies (0.5, 1, and 2 kHz).
*, ‡ Significantly different from estimate for reference category (P < 0.05) and (P < 0.01), respectively.
†Reference category.
Source: 2012/2013 Canadian Health Measures Survey (Cycle 3).
TABLE 9.
Prevalence of Audiometric Notch Among Working Canadians, Aged 16 to 79 Years: Occupational Noise Exposure Duration, Noise Sources, and Hearing Protection Usage
| §Notch (n = 3,431) | ||Notch (n = 3,431) | |||||||||||||
| 95% CI | 95% CI | |||||||||||||
| Characteristics | n | N | % | SE % | From | To | n | N | % | SE % | From | To | ||
| Occupational characteristics | ||||||||||||||
| Currently working in a noisy environment | ||||||||||||||
| Yes | 130 | 1,135 | 33.3 | 4.2 | 24.7 | 43.2 | *e | 88 | 516 | 15.2 | 3.5 | 8.9 | 24.7 | e,E |
| No† | 539 | 4,417 | 20.2 | 1.9 | 16.4 | 24.6 | 305 | 2,595 | 11.9 | 1.3 | 9.3 | 15.0 | ||
| Ever worked in a noisy environment | ||||||||||||||
| Yes | 348 | 2,781 | 26.0 | 2.9 | 20.2 | 32.8 | 224 | 1,770 | 16.6 | 2.0 | 12.6 | 21.5 | ‡ | |
| No† | 321 | 2,771 | 19.0 | 1.8 | 15.4 | 23.2 | 169 | 1,342 | 9.2 | 0.9 | 7.4 | 11.4 | ||
| Time worked in noisy environment | ||||||||||||||
| <12 months | 65 | 377 | 14.7 | 3.4 | 8.7 | 23.8 | ‡ e,E | f,F | ||||||
| 1 year to <5 years | 94 | 858 | 26.9 | 4.4 | 18.4 | 37.6 | E | 57 | 556 | 17.4 | 4.1 | 10.1 | 28.4 | e,F |
| 5 years to <10 years | 52 | 575 | 33.0 | 5.9 | 21.5 | 46.9 | e,E | f,F | ||||||
| 10 years or more† | 136 | 970 | 30.3 | 4.2 | 21.9 | 40.3 | 104 | 706 | 22.1 | 3.1 | 16.1 | 29.5 | e | |
| Used hearing protection at work | ||||||||||||||
| Always/often† | 138 | 1,209 | 30.2 | 4.9 | 20.5 | 42.0 | e | 89 | 760 | 19.0 | 4.7 | 10.7 | 31.3 | e,E |
| Sometimes/rarely/never | 209 | 1,568 | 23.5 | 2.7 | 18.1 | 29.8 | 135 | 1,010 | 15.1 | 1.6 | 11.9 | 19.0 | ||
| Hearing protection required/used | ||||||||||||||
| Yes/yes | 104 | 997 | 33.9 | 6.7 | 21.1 | 49.7 | e,E | 62 | 613 | 20.9 | 6.1 | 10.4 | 37.4 | e,E |
| Yes/no† | 32.9 | 10.9 | 14.2 | 59.2 | f,E | f,F | ||||||||
| No/yes | 19.2 | 6.4 | 8.8 | 36.9 | f,E | f,F | ||||||||
| No/no | 166 | 1,292 | 22.7 | 2.7 | 17.2 | 29.2 | 113 | 832 | 14.6 | 1.9 | 10.8 | 19.4 | ||
| Job category | ||||||||||||||
| White collar | 324 | 2,968 | 22.8 | 2.5 | 17.9 | 28.7 | * | 175 | 1,449 | 11.1 | 1.6 | 8.1 | 15.1 | ‡ |
| Blue collar† | 141 | 1,119 | 35.2 | 4.4 | 26.2 | 45.4 | e | 97 | 776 | 24.4 | 3.4 | 17.8 | 32.5 | e |
| Source of loud work noise | ||||||||||||||
| Machinery/transport | ||||||||||||||
| Yes | 281 | 2,416 | 27.8 | 3.3 | 21.2 | 35.6 | 191 | 1,581 | 18.2 | 2.2 | 13.8 | 23.7 | * | |
| No† | 67 | 366 | 18.2 | 3.9 | 11.1 | 28.5 | e,E | 9.4 | 2.8 | 4.7 | 17.7 | f,E | ||
| Music/people | ||||||||||||||
| Yes | 54 | 409 | 20.7 | 5.1 | 11.7 | 34.1 | e,E | 20 | 136 | 6.9 | 2.0 | 3.6 | 12.9 | ‡ e,E |
| No† | 294 | 2,372 | 27.2 | 3.6 | 20.1 | 35.7 | 204 | 1,634 | 18.7 | 2.5 | 13.9 | 24.8 | ||
| Other (munitions and/or other unspecified) | ||||||||||||||
| Yes | 20.9 | 5.2 | 11.7 | 34.6 | f,E | 17.2 | 5.0 | 8.7 | 31.2 | f,E | ||||
| No† | 307 | 2,543 | 26.6 | 3.1 | 20.4 | 33.9 | 198 | 1,574 | 16.5 | 2.0 | 12.5 | 21.4 | ||
Any hearing loss: FFPTA and/or HFPTA and/or LFPTA.
e, E use with caution (coefficient of variation 16.6–33.3%), population size and %, respectively.
f, F too unreliable to be published (coefficient of variation greater than 33.3%), population size and %, respectively.
DPOAE, distortion product otoacoustic emissions; FFPTA, four-frequency pure tone average over frequencies (0.5, 1, 2, and 4 kHz); HFPTA, high-frequency pure tone average over frequencies (3, 4, 6, and 8 kHz); LFPTA, low-frequency pure tone average over frequencies (0.5, 1, and 2 kHz).
*, ‡ significantly different from estimate for reference category (P < 0.05) and (P < 0.01), respectively.
†Reference category.
Audiometric notch definitions:
§Criteria for audiometric notch 1: (1) thresholds at 0.5 and 1 kHz of ≤15 dB, (2) maximal threshold at 3, 4, or 6 kHz ≥15 dB higher than the highest threshold for 0.5 and 1 kHz, and (3) threshold at 8 kHz ≥10 dB lower (better than) the maximal threshold for 3, 4, or 6 kHz. (Niskar et al46)
||Criteria for audiometric notch 2: thresholds at 2 and 8 kHz were both minimally at hearing levels 10-dB lower (better than) the threshold at 4 kHz (Wilson45).
Sources of Noise
The majority of participants (81%) who worked in a noisy workplace reported the noise source as either from machinery (ie, bulldozers, backhoes, or sawmill equipment) or transportation (ie, trains, planes, or road vehicles), with men significantly more likely than women to report these workplace noise sources (P < 0.01; 89% vs 62%, respectively) (Table 10). Approximately 18% overall reported loud “people or music noise” in the workplace, with women significantly more likely than men to report this workplace noise source (P < 0.01; 31% vs 13%, respectively). Furthermore, individuals aged 16 to 29 years were two to three times more likely than those in older age groups to report loud “people/music noise” as their main source of occupational noise.
TABLE 10.
Prevalence of Self-Reported Occupational Noise Exposure by Source of Noise Among Canadians, Aged 16 to 79 Years
| Machine/Transport§ | Music/People§ | Other§ | |||||||||||||||||||||||||
| 95% CI | 95% CI | 95% CI | |||||||||||||||||||||||||
| Characteristics | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * |
| ’000 | ’000 | ’000 | |||||||||||||||||||||||||
| Total | 1,166 | 9,129 | 81.2 | 1.6 | 77.3 | 84.6 | 279 | 2,056 | 18.3 | 1.4 | 15.5 | 21.5 | 190 | 1,171 | E | 10.4 | 1.6 | 7.4 | 14.5 | ||||||||
| Sex | |||||||||||||||||||||||||||
| Men | 913 | 7,179 | 88.9 | 1.7 | 84.6 | 92.0 | ‡ | 128 | 1,081 | 13.4 | 1.1 | 11.1 | 16.1 | ‡ | 119 | 763 | E | 9.4 | 1.5 | 6.6 | 13.3 | ||||||
| Women† | 253 | 1,950 | E | 61.7 | 3.6 | 53.6 | 69.2 | 151 | 974 | 30.8 | 3.2 | 24.3 | 38.3 | 71 | 407 | E | 12.9 | 3.2 | 7.3 | 21.8 | E | ||||||
| Age group | |||||||||||||||||||||||||||
| 16–29 years† | 210 | 1,934 | 73.9 | 5.8 | 59.5 | 84.5 | 83 | 854 | 32.6 | 5.0 | 22.6 | 44.5 | 36 | 300 | E | 11.5 | 2.7 | 6.7 | 18.9 | E | |||||||
| 30–49 years | 472 | 3,564 | 82.3 | 3.0 | 74.6 | 88.0 | 121 | 737 | E | 17.0 | 3.1 | 11.2 | 25.0 | E | * | 71 | 416 | E | 9.6 | 2.4 | 5.5 | 16.4 | E | ||||
| 50–79 years | 484 | 3,631 | 84.7 | 3.0 | 76.9 | 90.1 | 75 | 465 | E | 10.8 | 1.7 | 7.6 | 15.2 | ‡ | 83 | 454 | E | 10.6 | 2.0 | 7.0 | 15.8 | E | |||||
| Education (highest level in household) | |||||||||||||||||||||||||||
| Postsecondary or more† | 829 | 6,432 | 79.5 | 1.8 | 75.3 | 83.1 | 208 | 1,517 | 18.8 | 1.8 | 15.1 | 23.1 | 144 | 888 | E | 11.0 | 2.2 | 7.0 | 16.7 | E | |||||||
| Less than postsecondary | 304 | 2,447 | 86.5 | 3.9 | 75.3 | 93.1 | 60 | 501 | E | 17.7 | 5.1 | 9.1 | 31.6 | E | F | F | |||||||||||
| Household income | |||||||||||||||||||||||||||
| <$50,000† | 461 | 3,282 | 79.6 | 2.1 | 74.5 | 83.9 | 133 | 869 | 21.1 | 3.2 | 14.9 | 28.9 | 78 | 460 | E | 11.2 | 2.4 | 6.9 | 17.5 | E | |||||||
| $50,000 to <$100,000 | 392 | 2,847 | 78.2 | 3.0 | 70.9 | 84.0 | 85 | 795 | 21.8 | 2.8 | 16.3 | 28.6 | 71 | 396 | E | 10.9 | 2.8 | 6.0 | 18.8 | E | |||||||
| $100,000 or more | 313 | 3,000 | 86.4 | 2.1 | 81.1 | 90.3 | 61 | 392 | E | 11.3 | 2.1 | 7.4 | 16.8 | E | 41 | 314 | E | 9.0 | 2.3 | 5.1 | 15.5 | E | |||||
E use with caution (coefficient of variation 16.6–33.3%).
F too unreliable to be published (coefficient of variation greater than 33.3%).
*Significantly different from estimate for reference category (P < 0.05).
†Reference category.
‡Significantly different from estimate for reference category (P < 0.01).
§Among individuals who have ever worked in a noisy environment.
Source: 2012/2013 Canadian Health Measures Survey (Cycle 3).
Tinnitus
An estimated 43% of participants, representing 11.5 million Canadians, have experienced tinnitus at some point in their lives with men significantly more likely to have had tinnitus compared to women; P < 0.01; 48% versus 39%, respectively (men: 95% CI, 41.8 to 53.595; women: 95% CI, 35.0 to 42.8) (Table 11). Among those aged 16 to 29 years, over half (53%) reported tinnitus (at some point in their lives) compared with approximately 40% of individuals in the older age groups. While younger participants were more likely to have had tinnitus, among those who have experienced it, older participants were more likely to have experienced it “always,” “often,” or “sometimes” when it was quiet (84% vs 69% among 16 to 29 year olds). Overall, 35.3% of participants, aged 15 to 75 years, reported tinnitus within the past year (data not shown).
TABLE 11.
Prevalence of Self-Reported Tinnitus Among Canadians Aged 16 to 79 Years: Demographics, Duration of Occupational Noise Exposure, Hearing Protection Usage, “Blue Collar,” “White Collar” Workers
| Ever Experienced Tinnitus§ | Tinnitus When Quiet|| (Always, Often, Sometimes) | |||||||||||||||||
| 95% CI | 95% CI | |||||||||||||||||
| Characteristics | n | N | CV | % | SE % | From | To | CV | * | n | N | CV | % | SE % | From | To | CV | * |
| ’000 | ’000 | |||||||||||||||||
| Total | 1,654 | 11,539 | 43.2 | 1.8 | 39.3 | 47.2 | 568 | 3,881 | 72.0 | 3.1 | 64.7 | 78.3 | ||||||
| Demographic characteristics | ||||||||||||||||||
| Sex | ||||||||||||||||||
| Men | 857 | 6,319 | 47.6 | 2.7 | 41.8 | 53.5 | ‡ | 287 | 1,951 | 67.6 | 4.8 | 56.3 | 77.2 | |||||
| Women† | 797 | 5,220 | 38.8 | 1.8 | 35.0 | 42.8 | 281 | 1,930 | 77.0 | 3.1 | 69.5 | 83.1 | ||||||
| Age group | ||||||||||||||||||
| 16–29 years† | 468 | 3,398 | 52.9 | 2.7 | 46.9 | 58.8 | 117 | 1,044 | E | 68.5 | 6.4 | 53.2 | 80.6 | |||||
| 30–49 | 589 | 3,747 | 39.6 | 2.4 | 34.4 | 45.1 | ‡ | 147 | 726 | E | 53.5 | 6.1 | 40.2 | 66.3 | ||||
| 50–79 | 597 | 4,394 | 40.6 | 2.6 | 35.0 | 46.4 | ‡ | 304 | 2,111 | 84.1 | 2.6 | 77.4 | 89.1 | * | ||||
| Education (highest level in household) | ||||||||||||||||||
| Postsecondary or more† | 1,221 | 8,218 | 41.4 | 1.5 | 38.1 | 44.7 | 409 | 2,722 | 73.5 | 3.9 | 64.2 | 81.1 | ||||||
| Less than postsecondary | 375 | 2,855 | 48.6 | 3.5 | 41.1 | 56.2 | * | 141 | 998 | E | 66.5 | 5.6 | 53.3 | 77.5 | ||||
| Household income | ||||||||||||||||||
| <$50,000† | 641 | 3,835 | 41.0 | 2.3 | 36.0 | 46.3 | 246 | 1,414 | E | 73.0 | 4.7 | 61.4 | 82.1 | |||||
| $50,000 to <$100,000 | 553 | 4,376 | 48.4 | 3.1 | 41.6 | 55.3 | 191 | 1,681 | 79.3 | 4.3 | 68.1 | 87.2 | ||||||
| $100,000 or more | 460 | 3,328 | 39.9 | 2.7 | 34.2 | 45.9 | 131 | 787 | 58.9 | 6.3 | 44.6 | 71.8 | ||||||
| Occupational characteristics | ||||||||||||||||||
| Currently working in a noisy environment | ||||||||||||||||||
| Yes | 250 | 2,029 | 55.4 | 5.3 | 43.6 | 66.6 | * | 77 | 430 | E | 55.2 | 9.2 | 35.2 | 73.7 | E | |||
| No† | 1,404 | 9,510 | 41.3 | 2.0 | 37.0 | 45.7 | 491 | 3,451 | 74.8 | 3.5 | 66.3 | 81.8 | ||||||
| Ever worked in a noisy environment | ||||||||||||||||||
| Yes | 791 | 5,744 | 51.1 | 2.9 | 44.8 | 57.4 | ‡ | 291 | 1,959 | 75.1 | 4.5 | 64.0 | 83.7 | |||||
| No† | 863 | 5,795 | 37.4 | 2.3 | 32.5 | 42.7 | 277 | 1,922 | 69.0 | 5.1 | 56.8 | 79.0 | ||||||
| Time worked in noisy environment | ||||||||||||||||||
| <12 months | 202 | 1,259 | E | 47.0 | 5.0 | 36.2 | 58.1 | 54 | 278 | E | 70.1 | 8.0 | 50.3 | 84.4 | ||||
| 1 year to <5 years | 208 | 1,739 | 53.8 | 5.5 | 41.6 | 65.5 | 65 | 635 | E | 75.3 | 11.6 | 43.6 | 92.3 | |||||
| 5 years to <10 years | 114 | 970 | 53.7 | 7.0 | 38.4 | 68.4 | 40 | 261 | E | 68.1 | 13.1 | 36.1 | 89.0 | E | ||||
| 10 years or more† | 266 | 1,774 | 50.5 | 3.7 | 42.4 | 58.7 | 132 | 785 | E | 79.8 | 5.9 | 63.8 | 89.8 | |||||
| Used hearing protection at work | ||||||||||||||||||
| Always/often† | 268 | 2,274 | 53.7 | 4.1 | 44.6 | 62.6 | 90 | 653 | E | 70.2 | 6.3 | 54.8 | 82.1 | |||||
| Sometimes/rarely/never | 523 | 3,470 | 49.6 | 3.7 | 41.6 | 57.6 | 201 | 1,306 | 77.9 | 3.9 | 68.2 | 85.2 | ||||||
| Hearing protection required/used | ||||||||||||||||||
| Yes/yes | 191 | 1,675 | E | 53.2 | 4.8 | 42.7 | 63.5 | 60 | 525 | E | 69.0 | 7.4 | 50.9 | 82.7 | ||||
| Yes/no† | 64 | 449 | E | 55.8 | 11.6 | 31.0 | 78.0 | E | 24 | 208 | E | 83.7 | 10.8 | 47.2 | 96.7 | |||
| No/yes | 71 | 576 | E | 56.0 | 9.0 | 36.4 | 73.9 | F | 73.9 | 9.5 | 49.0 | 89.3 | ||||||
| No/no | 437 | 2,853 | 47.8 | 3.3 | 40.6 | 55.1 | 166 | 1,051 | 76.3 | 5.3 | 62.7 | 86.1 | ||||||
| Job category | ||||||||||||||||||
| White collar | 791 | 5,836 | 43.2 | 1.8 | 39.2 | 47.4 | 230 | 1,865 | 73.3 | 2.8 | 66.8 | 78.9 | ||||||
| Blue collar† | 210 | 1,472 | E | 42.4 | 5.7 | 30.7 | 55.1 | 60 | 244 | E | 48.9 | 13.1 | 23.3 | 75.1 | E | |||
E use with caution (coefficient of variation 16.6–33.3%).
F too unreliable to be published (coefficient of variation greater than 33.3%).
*Significantly different from estimate for reference category (P < 0.05).
†Reference category.
‡Significantly different from estimate for reference category (P < 0.01).
§Universe: all respondents aged 16–79 years.
||Universe: respondents who had tinnitus within the past month; “current tinnitus.”
Source: 2012/2013 Canadian Health Measures Survey (Cycle 3).
Of those who “ever worked in a noisy environment,” 51% had experienced tinnitus at some point in their lives compared with 41% who had “never experienced a noisy workplace.” Participants who currently worked in a noisy environment were more likely to report tinnitus (55%) than those in quieter environments (41%). However, for “blue collar” and “white collar” workers who reported having experienced tinnitus at some point in their lives, similar estimates of tinnitus were found (42.4% and 43.2%, respectively). Among participants whose tinnitus occurred within the past month, 19% (95% CI, 14.0 to 24.0) reported “bothersome” tinnitus, defined as affecting their sleep, concentration, or mood.
Hearing Loss, Notch Pattern, and Absent DPOAE
Among working Canadians, approximately 35% (95% CI, 33.2 to 37.6) of participants, aged 16 to 79 years, had measured HL on the basis of one or more PTA, including FFPTA, HFPTA, or LFPTA (Tables 4 to 9). Approximately 18% (95% CI, 16.1 to 20.7) had FFPTA HL, 34% (95% CI, 31.5 to 35.9) had HFPTA HL, while 15% (95% CI, 13.1 to 16.7) had LFPTA HL. Among participants who reported ever having worked in a noisy environment, 38% (95% CI, 33.9 to 42.2) had HL in one or more PTA compared with 33.5% (95% CI, 29.7 to 37.6) who never worked in such an environment. No significant differences in HL were found between those who currently worked in a noisy environment and those who did not. However, individuals who reported ever working in a noisy workplace were significantly more likely (P < 0.05 for FFPTA; P < 0.01 for LFPTA) to have HL than those who reported never working in such an environment, where a higher prevalence of both FFPTA HL (22%; 95% CI, 17.5 to 26.3, compared with 16%; 95% CI, 13.6 to 18.7, respectively) and LFPTA HL (18%; 95% CI, 15.2 to 21.5 compared with 12%; 95% CI, 10.5 to 14.5, respectively) was observed. Also, individuals who reported ever working a noisy environment were significantly more likely to have the Wilson audiometric notch45 than those who never worked in a noisy environment (16.6%: 95% CI, 12.6 to 21.5, compared with 9.2%; 95% CI, 7.4 to 11.4, respectively). Although a greater prevalence of participants who reported ever working in a noisy environment than those who never worked in such an environment also demonstrated the Niskar notch46 (26%; 95% CI, 20.2 to 32.8 vs 19%; 95% CI, 15.4 to 23.2, respectively), there was no significant difference observed. When duration of occupational exposure was considered, individuals who worked in a noisy environment for 10 years or more were significantly more likely to have HL in one or more PTA categories (FFPTA, HFPTA, LFPTA) than those with shorter durations of occupational noise exposure. For example, 46% of people with 10 or more years in a noisy work environment had FFPTA compared with 13% of those who had worked in a noisy environment for less than a year. Men, low household income participants, 50 to 79 year olds, and individuals with less than post-secondary education were more likely to have HL in one or more PTA categories (FFPTA, HFPTA, LFPTA).
When these demographic factors and duration in a noisy work environment were considered together, being male and increasing age generally remained significantly associated with HL (P < 0.05) (Table 12). Lower education was only associated with FFPTA HL whereby those from households with less than post-secondary education had higher odds of having FFPTA than those from households with post-secondary education [odds ratio (OR): 1.8; 95% CI, 1.2 to 2.7]. Working in a noisy environment remained significantly associated (P < 0.05) with both FFPTA and LFPTA HL when demographic factors were taken into account. The odds of having FFPTA and LFPTA were higher (2.0 and 2.2-fold, respectively) for individuals who had worked in a noisy environment for 10 years or more than for those who had never worked in a noisy environment. In the bivariate analysis, associations were evident between some demographic factors and noisy work environment duration with the presence of a notch pattern (Table 12). However, when considered together, only sex was significantly associated with having a notch whereby men had nearly twice the odds compared with women of having a notch using the definition by Niskar et al46 (OR: 1.8; 95% CI, 1.1 to 2.9). Also, the odds of having an absent DPOAE were nearly four times higher for men (OR: 3.7; 95% CI, 2.1 to 6.8) compared with women and increased by a factor of 1.1 for every 1-year increase in age.
TABLE 12.
Adjusted Odds Ratios Relating Hearing Loss, Audiometric Notch, and Absent DPOAE to Selected Characteristics Among Canadians, Aged 16 to 79 Years
| Hearing Loss, Notch, and DPOAE | ||||||||||||||||||
| FFPTA | HFPTA | LFPTA | Any HL | Audiometric Notch‡ | Absent DPOAE | |||||||||||||
| 95% Confidence Interval | 95% Confidence Interval | 95% Confidence Interval | 95% Confidence Interval | 95% Confidence Interval | 95% Confidence Interval | |||||||||||||
| Adjusted Odds Ratio | From | To | Adjusted Odds Ratio | From | To | Adjusted Odds Ratio | From | To | Adjusted Odds Ratio | From | To | Adjusted Odds Ratio | From | To | Adjusted Odds Ratio | From | To | |
| Sex | ||||||||||||||||||
| Men | 2.2 | 1.3 | 3.8* | 2.1 | 1.0 | 4.2* | 1.3 | 0.9 | 1.8 | 2.2 | 1.1 | 4.2* | 1.8 | 1.1 | 2.9* | 3.7 | 2.1 | 6.8* |
| Women† | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — |
| Age (continuous) | 1.1 | 1.1 | 1.1* | 1.1 | 1.1 | 1.1* | 1.1 | 1.0 | 1.1* | 1.1 | 1.1 | 1.1* | 1.0 | 1.0 | 1.0 | 1.1 | 1.1 | 1.1* |
| Education (highest level in household) | ||||||||||||||||||
| Postsecondary or more† | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — |
| Less than postsecondary | 1.8 | 1.2 | 2.7* | 1.8 | 0.9 | 3.7 | 1.7 | 1.0 | 2.9 | 1.8 | 0.9 | 3.7 | 1.1 | 0.8 | 1.6 | 1.1 | 0.6 | 1.9 |
| Time worked in a noisy environment | ||||||||||||||||||
| Never† | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — | 1.0 | — | — |
| Up to 10 years | 0.7 | 0.4 | 1.3 | 0.8 | 0.4 | 1.6 | 1.1 | 0.8 | 1.7 | 0.9 | 0.5 | 1.8 | 1.2 | 0.7 | 2.1 | 0.9 | 0.5 | 1.5 |
| 10 years or more | 2.0 | 1.1 | 3.7* | 1.5 | 0.7 | 3.0 | 2.2 | 1.5 | 3.1* | 1.4 | 0.7 | 2.8 | 1.3 | 0.7 | 2.4 | 1.6 | 0.7 | 3.7 |
Any HL: FFPTA and/or HFPTA and/or LFPTA.
Hearing loss thresholds: >20 dB (child/youth 16–18 years).
>25 dB (adult 19–79 years).
FFPTA, four-frequency pure tone average over frequencies (0.5, 1, 2, and 4 kHz); LFPTA, low-frequency pure tone average over frequencies (0.5, 1, and 2 kHz).
HFPTA: high frequency pure tone average over frequencies (3, 4, 6, and 8 kHz).
*Significantly different from estimate for reference category (P < 0.05).
†Reference category.
‡Criteria for audiometric notch 1: (1) thresholds at 0.5 and 1 kHz of ≤15 dB, (2) maximal threshold at 3, 4, or 6 kHz ≥15 dB higher than the highest threshold for 0.5 and 1 kHz, and (3) threshold at 8 kHz ≥10 dB lower (better than) the maximal threshold for 3, 4, or 6 kHz. (Niskar et al46).
Source: 2012/2013 Canadian Health Measures Survey (Cycle 3).
DISCUSSION
This is the first study to provide national prevalence estimates regarding occupational noise, audiometric HL, and HP usage among representative Canadian workers. More than 4 out of every 10 Canadians, between the ages of 16 and 79 years, reported being exposed to hazardous workplace noise, either in a present or past job. Of these individuals, 38% of workers (an estimated 4 million Canadians) had some degree of measured HL compared with 33.5% who reported not being exposed to hazardous workplace noise. This is somewhat higher than reported in a U.S. study50 based on a 2007 National Health Interview Survey (NHIS), which found that among individuals who had ever been exposed to loud workplace noise, 30% self-reported hearing difficulty compared with 10% of those not exposed (P < 0.0001).50 However, the higher prevalence of measured HL in the present study compared to the self-reported hearing difficulty prevalence reported by Masterson et al50 is not unexpected given the findings by Feder et al51 showing a large disparity between self-reported and measured HL in an adult population.
In the present study, the odds of having a measured HL for FFPTA and LFPTA was twice as high for workers who worked in a noisy workplace for 10 years or more compared with those who had never worked in such an environment, even after adjusting for age and sex. Although we would have expected the same finding for HFPTA HL, this was not the case. There may be several explanations for this finding, one of which may be related to the use of HP in those exposed to a noisy work environment for 10 years or more. It is possible that HP usage in these workers protected them from developing HFPTA HL; however, further research examining this specific issue would be needed. Another explanation may be related to sample size. The addition of Cycle 4 hearing data, and analyses of the combined dataset (approximately 7000 respondents), may show higher odds for high-frequency HFPTA HL.
“Blue collar” workers in the present study had a significantly higher prevalence of any PTA HL than “white collar” workers, with the rate of FFPTA HL being nearly double, which is consistent with the findings reported by Rubak et al.52 This Danish population-based study found 30% of industrial trade workers, aged 20 to 45 years, had HL at twice the prevalence of the reference population (office workers and residents exposed to traffic noise) with a four-fold increase among construction workers, despite the restricted age group and more stringent HL threshold (20 dB threshold, PTA: 2, 3, 4 kHz) than used in the present study.52 The exclusion of individuals over age 45 in the Danish study52 likely underestimated HL prevalence in that study. A German study (n = 4958) reported that male construction workers, aged 40 to 64 years, had a 1.5-fold increased prevalence of HL (sum of HL at 2, 3, 4 kHz greater than 105 dB in at least 1 ear) compared with “white collar workers” classified as office workers, architects, and engineers.53 The high HL threshold, the exclusion of subjects under 40 and over 64 years of age, and the testing of only three audiometric frequencies (2, 3, 4 kHz averaged) likely reduced the HL prevalence findings reported by Arndt et al.53
The present study results support previous research showing that males are more likely to be exposed to hazardous workplace noise and have a higher prevalence of HL than female workers,5,7,10 which is likely due to the traditional employment of men in high noise occupational industries such as construction, mining, lumber, and manufacturing. Interestingly, there were no significant differences in the proportion of men and women who worked in hazardous workplace noise environments for less than 10 years. This may be an indication of more women beginning to enter male-dominated, high-noise occupations; however, more research would be needed to corroborate these findings. Furthermore, the present study finding that individuals from households with an annual income of less than $50,000 per year had a significantly higher prevalence of any one or more PTA HL than individuals from higher income households supports previous research in this area37,54 and may be related to the difficulty that low-income groups experience in accessing health care and treatment.55,56
Occupational NIHL
Occupational NIHL develops insidiously over time and is the result of continuous or intermittent noise exposure and duration.57 The time lag that occurs between work-related hearing damage and the presentation of symptoms can be several years, depending on the duration and intensity of the noise exposure. However, some studies have reported surprisingly high NIHL prevalence rates among young workers suggesting that NIHL may already be present even before employment.58,59 A Dutch survey of construction workers found that 7.6% of workers under age 25 were diagnosed with NIHL, while other studies reported prevalence rates ranging from 14.4% to 16.0%.58,59 In a large scale retrospective study (n = 29,644) of Dutch construction workers in which hearing thresholds of workers (noise-exposed and nonexposed) were compared with ISO-1999 predictions, the authors found that NIHL was present at the start of employment and increased at the same rate as predicted for longer exposure durations.60 It may be that leisure noise exposure is a contributing factor to NIHL in young workers as well as in workers of all ages. As Rabinowitz3 notes, most estimates of occupational noise exposure used to determine the prevalence of HL “fail to approximate meaningfully the size of the population exposed to potentially damaging noise outside of work.” However, in two studies that considered nonoccupational exposure, there were no substantial overall differences in noise exposure reported, except in a subset of workers. Neitzel et al61 considered nonoccupational activities in a longitudinal study involving 266 construction workers, using dosimetry measurements and activity cards over 530 subject days. The researchers found minimal additional exposure for most workers compared with occupational noise found in construction; however, for a subset who frequently participated in noisy activities, nonoccupational noise may have contributed significantly to overall noise exposure levels.61 In a population-based study involving 788 workers from high noise exposure trades, using data from portable dosimeters, it was found that average leisure time noise levels had no effect on HL estimates—levels were comparable for the noise-exposed and reference populations (below 70 dBA).52 However, the composition of different tradeworkers in the aforementioned study52 may have been associated with lower occupational noise levels compared to the study by Neitzel et al,61 which comprised only construction workers.
There is some evidence that having NIHL can lead to a greater number of workplace accidents.2 In a large retrospective Quebec study of blue-collar workers (n = 52,982), which examined audiograms and accident claims, even the slightest degree of NIHL, leading to not hearing a warning signal or being confounded by its masking effect, accounted for up to 15.6% of “passive” accidents, defined as the worker “becoming the involuntary recipient of some mechanical energy” with no direct or full participation in the accident.2 Communication difficulties, cognitive failure, and worker fatigue are some of the factors associated with the risk of accidents for workers, with and without HL, exposed to high occupational noise conditions.57,62–64
Audiometric Notch
One well-documented characteristic of occupational NIHL is not only a “notch” in the audiogram typically at 4 kHz but may also be observed at 3 kHz and more variably at 6 kHz depending on the frequency range of the noise exposure.65 A notch can broaden and affect adjacent frequencies with continued noise exposure that has given rise to different audiometric notch definitions.57,65 The present study found that although a higher prevalence of noise-exposed individuals for both current and past workplaces showed the Niskar audiometric notch configuration46 than the Wilson notch,45 the latter was more sensitive in differentiating between individuals who reported “ever being exposed” to hazardous workplace noise and those who did not. A significantly higher prevalence of workers who responded affirmatively to this question showed the Wilson audiometric notch configuration45 than those who did not report this exposure (Table 9). Similarly, a higher prevalence of individuals reporting exposure to “machinery” and “people/music noise” in the workplace than those not exposed to these sources showed the Wilson audiometric notch45; this notch also yielded a stronger association (P < 0.01) between “blue collar” versus “white collar” workers than the Niskar notch definition46 (P < 0.05). These findings support the conclusion by McBride et al65 that in conjunction with an accurate noise exposure history, the 4-kHz notch is a well-established clinical sign that is valuable in confirming a NIHL diagnosis. Our study findings indicate that the Wilson audiometric notch definition45 may be a more sensitive parameter; however, further research is needed to corroborate these results.
DPOAE
The use of DPOAE testing has shown promise in early identification of NIHL in that low-level or absent DPOAEs could be indicative of NIHL susceptibility.66 Cochlear status in individuals exposed to industrial workplace noise compared with nonexposed workers has increasingly been the subject of research. There have been studies showing the vulnerability of the cochlea to long-term noise exposure and increased susceptibility of outer hair cell damage compared with inner hair cells, likely due to their location, structure, and specific metabolism.67–69 Some studies have shown DPOAEs to be more sensitive than audiometry in determining subclinical cochlear damage, specifically in high-frequency outer hair cells, manifested by decreased amplitudes or absent DPOAEs.28,70–72
In the present study, individuals with 10 years or more of hazardous workplace noise exposure were significantly more likely to have absent DPOAEs than those with shorter duration exposures, which is consistent with audiometric results. Likewise, “blue collar” workers had a significantly higher prevalence of absent DPOAEs than “white collar” workers. In general, our findings that DPOAEs can identify cochlear damage and are consistent with audiometric results are congruent with studies involving noise-exposed workers compared with controls29; however, no significant differences were observed between the prevalence of absent DPOAEs and audiometric HL for any PTA.
Several studies have found reduced emissions in DPOAEs, including notches at 4 to 6 kHz, associated with chronic noise exposure, showing a greater sensitivity of DPOAEs in identifying cochlear damage than the audiogram.26,27,73,74 However, as the present study did not include data for specific frequency and amplitude emission levels during DPOAE testing, it was not possible to identify early subclinical damage and compare with audiometric results for differing durations of occupational noise exposure. However, it is clear that research in this area would be beneficial. As Forshaw27 and the American College of Occupational and Environmental Medicine (ACOEM) statement on NIHL have indicated,75 the use of OAE emissions is an emerging audiologic technology, identified as one of the research priorities for shedding light on current knowledge gaps.
Hazardous Workplace Exposure
In the present study, individuals who reported hazardous workplace noise exposure for 10 years or more had higher odds of having HL than those who were exposed for shorter durations with the odds of HL doubled when compared with those who had never worked in such an environment, regardless of age, sex, or education level. This demarcation of 10 years or more is consistent with population-based study findings by Palmer et al,5 where the risk of HL rose for men as a function of duration with the greatest risk observed at 10 or more years of noisy workplace exposure (where one had to shout to be heard at arm's length). However, Palmer et al5 reported a higher prevalence ratio for severe hearing difficulty (3.8) and for persistent tinnitus, such that noise-exposed men over the age of 35 had a prevalence ratio of 2.6 compared with those who were never exposed to loud occupational noise. One explanation for the high prevalence ratio may be the much larger sample size (n = 21,201) in the study by Palmer et al5 than the present study sample, and their inclusion of members of the armed services (n = 993). In addition, as HL in the study by Palmer et al 5 was self-reported, the high tinnitus prevalence may have been an indication of HL not realized by the individual. Lastly, the mail-in questionnaire used in the study by Palmer et al5 may have led to a potential bias in that more individuals with hearing impairment may have returned the questionnaire. Overall, it is likely that the HL prevalence ratio reported by Palmer et al5 represents an underestimate given previous findings showing a large disparity between self-reported HL and audiometric results,51 their exclusion of retired individuals over age 64, and those with mild to moderate HL.
In examining the prevalence of self-reported exposure to occupational noise, a NHANES study reported that 17% of U.S. workers were exposed to hazardous noise in their current job,7 which is somewhat higher than the 14% reported in the present study. The larger sample size included in the NHANES weighted analysis (n = 9275) may account for this difference as well as the slightly different hazardous noise exposure definition. The NHANES hazardous workplace noise exposure definition of “by loud noise I mean noise so loud that you have to speak in a raised voice to be heard” 7 was similar to the present study, with the exception of the distance condition used in the current study question, “so loud that one had to speak in a raised voice to communicate with co-workers standing within an arm's length.” The NHANES definition may have led to a greater number of participants answering affirmatively to this question compared with the present study, which stipulated “within an arm's length.”
The present study found that just over one-third of men (35.5%) and under a quarter of women (20.4%) had worked in a noisy job for 10 years or more, which is nearly double the percentage for men (16%) and six-fold more for women (3%) reported in a British population-based study, using a similar definition of hazardous workplace noise (where there was a need to shout to be heard at arm's length).5 This may reflect differences in workplace occupations between Canada and Britain or may signify a change in the numbers of individuals working in high noise occupations. When comparing those currently exposed to hazardous workplace noise with the NHANES study,7 the present study findings are fairly consistent (21.7% compared with 26.3% NHANES for men; 5.9% compared with 6.7% NHANES for women).
Hearing Protection Usage
The current study found that nearly twice as many participants reported they “sometimes,” “rarely,” or “never” used HP compared with their American counterparts reported by NHANES (60% vs 34%).7 However, an important difference that may partially account for the higher percentage found in the present study are the response categories and the question itself. The NHANES study used a dichotomous “Yes/No” response for the question, “In this (current) job, do you ever wear protective hearing devices?” whereas the present study had five response categories (always, often, sometimes, rarely, never) for the question “How often do/did you use hearing protection at work when in a noisy area?” with the latter three categories collapsed to indicate routine nonuse of HP. In terms of workers who were required to use HP in their workplace, the present study found that 20% indicated they “sometimes,” “rarely,” or “never” wore HP, representing an estimated 809,000 Canadians. This is similar to findings by study by Hessel18 in which 24% to 27% of Albertan electricians, plumbers, and pipefitters (n = 198) reported “never, seldom or sometimes” wearing HP, while only 12% of boilermakers (n = 101) reported this. The higher noise exposure for boilermakers may explain the higher HP compliance rate of 70.5% who reported “always” wearing HP. A high HP compliance rate of nearly 100% was also observed in Canadian lumber mill workers; however, compliance dropped to 84% when noise exposure was at or above 95 dBA, and to 60% in those exposed under 85 dBA.20 This pattern was also observed in a Danish population-based study wherein 75% of workers exposed to more than 85 dBA and 42% of workers exposed to 80 to 84 dBA, respectively, reported using HP.52 As the current study relied on self-reported workplace noise exposure, associations with specific noise levels cannot be made. However, this phenomenon along with other reasons for nonuse of HP may be worth exploring. Studies that have probed reasons for nonusage have cited improper fitting of HP, sizing problems, and comfort as factors,76–78 many of which can also lower HP effectiveness due to suboptimal attenuation 19,57 such that even with high compliance, workers may not be completely protected from NIHL.
There are only a few population-based studies examining HP usage.7,52 Two industry-specific U.S. surveys were conducted, primarily involving male tradeworkers (n = 98) and firefighters (n = 425). The average HP usage was marginally above 50%, even though 98% indicated they were supposed to wear HP.76 Similarly, for firefighters, respondents only used HP 34% of the time it was required.79 Although the present population-based study encompassed a larger age range (16 to 79 years) of both genders working in various noisy occupations, it appears that the present study findings are consistent with many previous studies showing that HP is often not worn consistently, even when occupationally required.
For construction workers, there are many unique factors affecting HP usage such as high variability of noise exposure as workers move in and out of noisy areas, exposure to complex combinations of noise sources, employment at multiple job sites each day, and the likelihood of being self-employed, placing the onus on the worker to take greater responsibility for their own health and safety19,80,81; other causes of irregular HP usage include hindrance to communication and discomfort.82,83 Studies have found an array of factors associated with HP usage such as risk perception, perceived susceptibility to HL, noise annoyance, perceived self-efficacy, and perceived benefits or barriers.77,78,84 The insidious nature of HL and the fact that it is often not noticed until the loss is significant render the risk as “invisible”85; this may have the effect of limiting perceived risk, thereby weakening the motivation of the individual to use HP.
Tinnitus
Tinnitus can be a debilitating chronic condition for some individuals, negatively impacting sleep and quality of life, while for others it is a minor annoyance.86 The necessity of evaluating tinnitus using self-report and the various definitions of tinnitus used in surveys leads to challenges in estimating the prevalence of this condition.86 According to Moller,86 “the greatest challenge lies in defining the tinnitus,” as this condition has many forms in terms of strength and character and is changeable within the same individual over the course of one day and across several days.86–88 Nonetheless, the National Center for Health Statistics89 estimated that tinnitus affected up to 30% of the adult U.S. population at some time in their lives, while other studies in Britain, Sweden, Italy, Scotland, Japan, and Norway have reported prevalence estimates ranging from 10% to 20%.68,90–95 In a cohort of Australians (n = 1300; aged 11 to 35 years), a higher tinnitus prevalence of 64% was reported.96 The present study finding of 43.2% of Canadians “ever having experienced” tinnitus is somewhat higher than found in previous population-based studies but lower than the Australian study,96 which assessed a younger age cohort. The differing tinnitus definitions, the use of mail-in questionnaires versus face-to-face interviews, and the age groups involved are all factors to consider when examining tinnitus prevalence rates across studies.
Approximately one-third of Canadians, aged 16 to 79 years, reported tinnitus within the previous year, which is somewhat higher than estimates by NHANES97 (25.3%) of 20 to 69 year olds and a Korean population-based study98 (21.4%) of 20 to 97 year olds, both of which used the same question: “In the past 12 months, have you ever had ringing, roaring, or buzzing in your ears?” This may be due to the differing age groups and/or the tinnitus question itself. The current study presented a preamble definition before the question (“Tinnitus is the presence of hissing, buzzing, ringing, rushing or roaring sounds in your ears when there is no other sound around you”) following which participants were asked if they experienced it. Concurrent with both aforementioned studies,97,98 the current study findings indicate that while tinnitus is generally higher in older age groups, it is also frequently reported by young adults; just over half of 16 to 29 year olds in the present study and approximately 20% of 21 to 30 year olds in the NHANES study97 and 20 to 29 year olds in the Korean study98 (14.6% men; 19.6% women) reported tinnitus. It has been speculated that this may be due to the increased participation in noisy leisure activities and the use of personal listening devices by adolescent and young adult populations.99
Masterson et al50 found that among U.S. workers who had ever or currently worked in a noisy environment (defined as needing to speak in a raised voice to be heard), 19% and 15%, respectively, reported tinnitus in the previous 12 months. This is much lower than the present study findings wherein among participants who were exposed to hazardous workplace noise within the past 12 months, 55% reported tinnitus. This wide discrepancy is likely due to the use of “bothered” and the time reference of “5 minutes or more” in the definition used by Masterson et al50: “In the past 12 months, have you been bothered by ringing, roaring, or buzzing in your ears or head that lasts for 5 minutes or more?” These results are more consistent with the present study findings wherein “bothersome” tinnitus, defined as tinnitus affecting sleep, concentration, or mood, was found in 19% of participants (who reported tinnitus within the past year), but without considering occupational noise exposure.
In fact, “bothersome” tinnitus prevalence in a population may be of the most importance due its association with lower quality of life and work capacity as well as negative mental health outcomes.99–101 The prevalence of “troubling,” “bothersome,” or “moderately annoying” tinnitus in other population-based studies ranges from 4.4% to 17.4%,90,95,100–107 with the wide variation likely due to the differing definitions and age groups studied. Nonetheless, a review of tinnitus studies found that despite variable prevalence rates, approximately 20% of tinnitus sufferers reported their condition as a “severe” annoyance,86 which can translate to a significant proportion of a population. Bothersome tinnitus often includes sleep disturbance that is a common complaint affecting between 25% and 70% of tinnitus sufferers.108–111 The present study found that among those who had tinnitus within the previous year, 19% of participants, representing 1,752,000 Canadians, indicated that it affected their sleep, concentration, or mood. Although this is a small subset of those who have tinnitus, it is nonetheless a significant proportion of individuals reporting a serious form of tinnitus.
Contrary to expectations, the present study findings were similar for “blue collar” and “white collar” workers who had ever experienced tinnitus, 42.4% and 43.2%, respectively. This may be compared with a Swedish population-based study37 wherein a similar prevalence of tinnitus in workers versus nonworkers was reported, 26% and 30%, respectively, using the question: “Have you during the most recent time experienced sound in any of the ears, without there being an external source (so-called tinnitus) lasting more than 5 minutes? (no, yes sometimes, yes often, yes all the time).” Also, in the aforementioned study, there was little difference between workers and nonworkers with regard to moderately or severely “bothersome” tinnitus prevalence, 30% and 37%, respectively, using the question: “How much do you feel that the tinnitus sounds worry, bother or upset you? (not at all, a little, moderately, severely).”37 This may be an indication that nonoccupational exposures play a role in the pervasiveness of tinnitus.96
One of the risk factors for developing tinnitus is exposure to loud noise, in addition to HL and aging97 with other risk factors being sex, personality type, work stress, head injury, exposure to toxins, and otological diseases.86 A population-based Korean study found that the odds of tinnitus was approximately 1.5 times higher in those exposed to occupational noise than those who were not.98 Similarly, a U.S. NHIS (2007) found that among workers who had ever been exposed to occupational noise, the prevalence of hearing difficulty was 23% (compared with 7% nonexposed), the prevalence of tinnitus was 15% while 9% had both.50 Furthermore, occupation was reported to have a marked effect on bothersome tinnitus in a population-based Norwegian study.93 In the present study, among those who reported current exposure to hazardous workplace noise, just over half had tinnitus, while one-third had some measured HL. This may be an indication of compromised hearing in a higher percentage of workers than found using audiometric evaluation. Although tinnitus is not as well understood as HL, these two conditions share many risk factors and some causal etiologies.112 One tinnitus progression theory suggests that cochlear changes may trigger central auditory system changes with speculation that those who report tinnitus but not hearing difficulty have subclinical auditory damage.112,113
Indeed, tinnitus often coexists with HL and in isolation is seen as a warning sign of potential HL. Shargorodsky et al97 reported that participants with hearing impairment were two to three times more likely to report frequent tinnitus than those with no hearing impairment. Furthermore, the presence of tinnitus and/or NIHL has implications for worker safety, as they are often associated with impaired speech discrimination and a higher risk of accidents in the workplace.2,22,114,115
Limitations
One limitation of the present study is the absence of a nonoccupational noise exposure estimate and its contribution to the overall noise exposure of workers. Second, noise exposure in this study was not directly measured but recalled by participants that may have led to inaccuracies with regard to noise exposure levels and durations. Third, the lack of data for individual DPOAE test frequencies did not allow analysis of emission strength that may have shown changes in cochlear function compared with audiometry. Fourth, an estimate of conductive HL was not possible which may have affected the overall prevalence of HL in this study. Lastly, the relatively small sample size for the CHMS Cycle 3 resulted in a more limited analysis in certain cases where cell sizes were small. The release of CHMS Cycle 4 data will allow a comparison between datasets and provide a larger sample size when Cycle 3 and 4 are combined.
CONCLUSION
These study findings address a knowledge gap by providing national estimates of hazardous workplace noise exposure, and a snapshot of hearing health, acuity, and HP usage in the Canadian working population. An estimated 42% of respondents, representing 11.2 million Canadians, are exposed to hazardous workplace noise defined as so loud that workers had to speak in a raised voice to communicate with someone standing an arm's length away. An estimated one-third of workers, substantially more men than women, had some degree of measured HL, with a similar proportion showing cochlear hair cell damage evidenced by absent DPOAEs.
A strong effect was observed for 10 years or more of hazardous workplace noise exposure where the odds of having HL were doubled compared with never having worked in such an environment, regardless of age, sex, or education level. A significantly higher prevalence of “blue collar” workers had HL, absent DPOAEs, and a 4-kHz audiometric notch than “white collar” workers. Although the reasons were outside the scope of this study, just over half of Canadians overall reported not using HP while exposed to hazardous workplace noise, while for those required to use HP at work, 80% reported doing so. Beyond the impact on NIHL, there are potential health and safety implications for workers for whom HP is not mandatory, which may be worth exploring in future studies.
The Wilson audiometric notch45 was found to be more sensitive than the Niskar audiometric notch46 in that a clear differentiation was observed between “blue collar” and “white collar” workers and between those ever having been exposed to hazardous occupational noise and those who were not. Tinnitus, which is often associated with HL and also serves as a warning sign of potential hearing damage, was reported by over one-third of Canadians as having experienced it at some point in their lives and by over one-half currently working in a noisy workplace. In addition, just under a quarter of tinnitus sufferers indicated that it affected their sleep, concentration, or mood. Despite the limitations highlighted, foremost being the unknown contribution of leisure noise exposure, these study findings provide a scientific knowledge base on the status of hearing health and acuity in the Canadian working population.
TABLE 5.
Prevalence of Audiometric Hearing Loss Among Working Canadians, Aged 16 to 79 Years: Occupational Noise Exposure Duration, Noise Sources, and Hearing Protection Usage
| FFPTA (n = 3,431) | HFPTA (n = 3,431) | LFPTA (n = 3,431) | |||||||||||||||||||
| 95% CI | 95% CI | 95% CI | |||||||||||||||||||
| Characteristics | n | N | % | SE % | From | To | n | N | % | SE % | From | To | n | N | % | SE % | From | To | |||
| Currently working in a noisy environment | |||||||||||||||||||||
| Yes | 71 | 602 | 17.7 | 3.2 | 11.7 | 25.9 | e,E | 133 | 1,040 | 30.5 | 3.6 | 23.2 | 39.0 | 52 | 523 | 15.4 | 2.8 | 10.1 | 22.6 | e,E | |
| No† | 594 | 4,030 | 18.4 | 1.0 | 16.2 | 20.8 | 1,081 | 7,480 | 34.2 | 1.0 | 31.9 | 36.5 | 483 | 3,221 | 14.7 | 1.1 | 12.5 | 17.3 | |||
| Ever worked in a noisy environment | |||||||||||||||||||||
| Yes | 313 | 2,305 | 21.6 | 2.0 | 17.5 | 26.3 | * | 532 | 3,766 | 35.2 | 1.9 | 31.2 | 39.5 | 249 | 1,939 | 18.1 | 1.4 | 15.2 | 21.5 | ‡ | |
| No† | 352 | 2,327 | 15.9 | 1.2 | 13.6 | 18.7 | 682 | 4,753 | 32.6 | 1.7 | 28.9 | 36.4 | 286 | 1,805 | 12.4 | 0.9 | 10.5 | 14.5 | |||
| Time worked in noisy environment | |||||||||||||||||||||
| <12 months | 12.6 | 3.9 | 6.3 | 23.8 | ‡ f,E | 66 | 375 | 14.7 | 3.4 | 8.6 | 23.9 | ‡ e,E | 14.1 | 4.0 | 7.4 | 25.2 | ‡ f,E | ||||
| 1 year to <5 years | 43 | 264 | 8.3 | 2.1 | 4.6 | 14.4 | ‡ e,E | 91 | 781 | 24.5 | 3.3 | 17.9 | 32.6 | ‡ e | 36 | 275 | 8.6 | 2.0 | 5.2 | 14.0 | ‡ e,E |
| 5 years to <10 years | 37 | 251 | 14.4 | 3.3 | 8.6 | 23.2 | ‡ e,E | 80 | 577 | 33.1 | 4.5 | 24.1 | 43.5 | ‡ e | 30 | 190 | 10.9 | 2.7 | 6.2 | 18.6 | ‡ e,E |
| 10 years or more† | 194 | 1,466 | 45.8 | 4.4 | 36.4 | 55.5 | 294 | 2,031 | 63.5 | 3.8 | 54.7 | 71.4 | 144 | 1,112 | 34.8 | 2.6 | 29.2 | 40.7 | |||
| Used hearing protection at work | |||||||||||||||||||||
| Always/often† | 95 | 827 | 20.6 | 3.8 | 13.6 | 30.1 | e,E | 166 | 1,303 | 32.5 | 5.2 | 22.2 | 44.9 | e | 79 | 742 | 18.5 | 3.3 | 12.3 | 27.0 | e,E |
| Sometimes/rarely/never | 218 | 1,478 | 22.1 | 1.8 | 18.4 | 26.4 | 365 | 2,458 | 36.8 | 1.9 | 32.7 | 41.0 | 170 | 1,197 | 17.9 | 1.7 | 14.5 | 21.9 | |||
| Hearing protection required/used | |||||||||||||||||||||
| Yes/yes | 62 | 514 | 17.5 | 3.4 | 11.2 | 26.3 | e,E | 111 | 872 | 29.7 | 5.5 | 19.2 | 42.8 | e,E | 52 | 456 | 15.5 | 3.0 | 10.0 | 23.4 | e,E |
| Yes/no† | f,F | 57 | 375 | 48.4 | 7.9 | 31.9 | 65.2 | e | 29.6 | 9.5 | 13.4 | 53.3 | f,E | ||||||||
| No/yes | 29.3 | 7.3 | 16.0 | 47.3 | f,E | 50 | 402 | 39.7 | 9.2 | 22.1 | 60.5 | e,E | 26.9 | 7.7 | 13.5 | 46.5 | f,E | ||||
| No/no | 178 | 1,210 | 21.2 | 2.1 | 17.0 | 26.2 | 296 | 2,043 | 35.8 | 1.9 | 31.8 | 40.1 | 138 | 935 | 16.4 | 2.2 | 12.1 | 21.8 | |||
| Job category | |||||||||||||||||||||
| White collar | 177 | 1,396 | 10.7 | 1.1 | 8.6 | 13.3 | * | 381 | 2,993 | 23.0 | 2.1 | 18.7 | 28.0 | * | 158 | 1,360 | 10.5 | 1.1 | 8.3 | 13.2 | |
| Blue collar† | 83 | 612 | 19.2 | 3.3 | 13.0 | 27.5 | e,E | 164 | 1,176 | 37.0 | 4.5 | 27.7 | 47.3 | e | 61 | 493 | 15.5 | 2.7 | 10.4 | 22.5 | e,E |
| Source of loud work noise | |||||||||||||||||||||
| Machinery/transport | |||||||||||||||||||||
| Yes | 261 | 1,952 | 22.5 | 2.5 | 17.5 | 28.4 | 442 | 3,213 | 37.0 | 2.4 | 32.0 | 42.3 | 202 | 1,625 | 18.7 | 1.9 | 14.8 | 23.3 | |||
| No† | 52 | 353 | 17.6 | 4.2 | 10.1 | 28.8 | e,E | 90 | 553 | 27.5 | 4.6 | 18.6 | 38.7 | e,E | 47 | 314 | 15.6 | 4.3 | 8.2 | 27.7 | e,E |
| Music/people | |||||||||||||||||||||
| Yes | f,F | 67 | 432 | 21.9 | 4.5 | 13.6 | 33.4 | * e,E | f,F | ||||||||||||
| No† | 277 | 2,049 | 23.5 | 2.5 | 18.4 | 29.5 | 465 | 3,334 | 38.2 | 2.5 | 32.9 | 43.9 | 219 | 1,713 | 19.6 | 2.1 | 15.4 | 24.6 | |||
| Other (munitions and/or other unspecified) | |||||||||||||||||||||
| Yes | 51 | 269 | 23.6 | 4.3 | 15.6 | 34.2 | e,E | 77 | 415 | 36.4 | 5.5 | 25.3 | 49.2 | e | 40 | 199 | 17.5 | 4.6 | 9.6 | 29.8 | e,E |
| No† | 262 | 2,036 | 21.3 | 2.2 | 16.9 | 26.6 | 455 | 3,351 | 35.1 | 2.0 | 30.9 | 39.5 | 209 | 1,740 | 18.2 | 1.5 | 15.1 | 21.8 | |||
Any hearing loss: FFPTA and/or HFPTA and/or LFPTA.
e, E use with caution (coefficient of variation 16.6–33.3%), population size and %, respectively.
f, F too unreliable to be published (coefficient of variation greater than 33.3%), population size and %, respectively.
DPOAE, distortion product otoacoustic emissions; FFPTA, four-frequency pure tone average over frequencies (0.5, 1, 2, and 4 kHz); HFPTA, high-frequency pure tone average over frequencies (3, 4, 6, and 8 kHz); LFPTA, low-frequency pure tone average over frequencies (0.5, 1, and 2 kHz).
*, ‡ significantly different from estimate for reference category (P < 0.05) and (P < 0.01), respectively.
†Reference category.
TABLE 6.
Prevalence of Audiometric Hearing Loss, Among Working Canadians, Aged 16 to 79 Years: Demographics
| Any Hearing Loss (n = 3,431) | Absent DPOAE (n = 3,068/newfaildp) | |||||||||||||
| 95% CI | 95% CI | |||||||||||||
| Characteristics | n | N | % | SE % | from | to | n | N | % | SE % | From | To | ||
| ’000 | ’000 | |||||||||||||
| Total | 1,271 | 8,951 | 35.4 | 1.0 | 33.2 | 37.6 | 928 | 6,274 | 28.5 | 1.4 | 25.5 | 31.8 | ||
| Demographic characteristics | ||||||||||||||
| Sex | ||||||||||||||
| Men | 725 | 5,235 | 41.6 | 2.1 | 36.9 | 46.4 | ‡ | 586 | 4,182 | 38.9 | 2.3 | 33.9 | 44.1 | ‡ |
| Women† | 546 | 3,716 | 29.2 | 2.2 | 24.6 | 34.4 | 342 | 2,092 | 18.6 | 2.0 | 14.7 | 23.3 | ||
| Age group | ||||||||||||||
| 16–29 years† | 66 | 564 | 9.0 | 2.1 | 5.3 | 14.8 | e,E | 34 | 254 | 4.8 | 1.0 | 3.0 | 7.7 | e,E |
| 30–49 years | 229 | 1,650 | 18.7 | 2.1 | 14.5 | 23.7 | ‡ | 177 | 1,444 | 18.8 | 2.7 | 13.6 | 25.5 | ‡ |
| 50–79 years | 976 | 6,737 | 65.9 | 1.7 | 62.0 | 69.7 | ‡ | 717 | 4,577 | 50.5 | 2.4 | 45.1 | 55.8 | ‡ |
| Education (highest level in household) | ||||||||||||||
| Postsecondary or more† | 866 | 6,068 | 32.1 | 1.6 | 28.7 | 35.7 | 633 | 4,332 | 26.6 | 2.1 | 22.2 | 31.4 | ||
| Less than postsecondary | 366 | 2,572 | 46.8 | 4.4 | 37.3 | 56.6 | * | 265 | 1,690 | 34.7 | 3.9 | 26.7 | 43.7 | |
| Household income | ||||||||||||||
| <$50,000† | 587 | 3,692 | 42.7 | 2.3 | 37.8 | 47.8 | 419 | 2,777 | 36.8 | 3.2 | 30.1 | 44.1 | ||
| $50,000 to <$100,000 | 410 | 2,860 | 33.3 | 1.3 | 30.4 | 36.3 | * | 311 | 2,039 | 27.4 | 2.4 | 22.4 | 33.1 | * |
| $100,000 or more | 274 | 2,399 | 29.7 | 3.4 | 22.9 | 37.6 | * | 198 | 1,458 | 20.8 | 3.5 | 14.1 | 29.6 | ‡e,E |
Any hearing loss: FFPTA and/or HFPTA and/or LFPTA.
e, E use with caution (coefficient of variation 16.6–33.3%), population size and %, respectively.
f, F too unreliable to be published (coefficient of variation greater than 33.3%), population size and %, respectively.
DPOAE, distortion product otoacoustic emissions; FFPTA, four-frequency pure tone average over frequencies (0.5, 1, 2, and 4 kHz); HFPTA, high-frequency pure tone average over frequencies (3, 4, 6, and 8 kHz); LFPTA, low-frequency pure tone average over frequencies (0.5, 1, and 2 kHz).
*, ‡ significantly different from estimate for reference category (P < 0.05) and (P < 0.01), respectively.
†Reference category.
TABLE 7.
Prevalence of Audiometric Hearing Loss, Absent DPOAE Among Working Canadians, Aged 16 to 79: Occupational Noise Exposure Duration, Noise Sources, and Hearing Protection Usage
| Any Hearing Loss (n = 3,431) | Absent DPOAE (n = 3,068) | |||||||||||||
| 95% CI | 95% CI | |||||||||||||
| Characteristics | n | N | % | SE % | From | To | n | N | % | SE % | From | To | ||
| Currently working in a noisy environment | ||||||||||||||
| Yes | 140 | 1,132 | 33.2 | 3.6 | 25.9 | 41.5 | 113 | 972 | 31.3 | 4.4 | 22.5 | 41.6 | e | |
| No† | 1,131 | 7,819 | 35.7 | 1.1 | 33.3 | 38.2 | 815 | 5,302 | 28.1 | 1.5 | 25.0 | 31.5 | ||
| Ever worked in a noisy environment | ||||||||||||||
| Yes | 558 | 4,058 | 38.0 | 1.9 | 33.9 | 42.2 | 437 | 3,028 | 32.7 | 2.1 | 28.3 | 37.5 | * | |
| No† | 713 | 4,893 | 33.5 | 1.8 | 29.7 | 37.6 | 491 | 3,246 | 25.5 | 2.0 | 21.3 | 30.3 | ||
| Time worked in noisy environment | ||||||||||||||
| <12 months | 77 | 526 | 20.5 | 3.8 | 13.4 | 30.2 | ‡ e,E | 16.2 | 4.9 | 8.0 | 30.1 | ‡ f,E | ||
| 1 year to <5 years | 94 | 823 | 25.8 | 3.7 | 18.5 | 34.7 | ‡ e | 73 | 508 | 19.9 | 3.7 | 13.0 | 29.3 | ‡ E |
| 5 years to <10 years | 84 | 642 | 36.8 | 3.5 | 29.5 | 44.7 | ‡ e | 57 | 451 | 29.6 | 5.0 | 19.8 | 41.7 | ‡ e,E |
| 10 years or more† | 302 | 2,067 | 64.6 | 3.7 | 56.1 | 72.2 | 248 | 1,727 | 56.1 | 4.6 | 45.9 | 65.8 | ||
| Used hearing protection at work | ||||||||||||||
| Always/often† | 178 | 1,495 | 37.3 | 4.8 | 27.4 | 48.4 | e | 126 | 1,019 | 30.3 | 5.1 | 20.3 | 42.7 | e,E |
| Sometimes/rarely/never | 379 | 2,558 | 38.3 | 1.6 | 34.8 | 41.9 | 310 | 2,004 | 34.0 | 1.9 | 29.9 | 38.4 | ||
| Hearing protection required/used | ||||||||||||||
| Yes/yes | 122 | 1,048 | 35.6 | 5.0 | 25.6 | 47.1 | e | 95 | 782 | 29.3 | 6.5 | 17.3 | 45.2 | e,E |
| Yes/no† | 60 | 444 | 57.2 | 7.4 | 40.8 | 72.2 | e | 50.3 | 9.8 | 29.9 | 70.5 | f,E | ||
| No/yes | 51 | 417 | 41.3 | 9.5 | 22.9 | 62.5 | e,E | 28 | 224 | 33.4 | 8.2 | 18.2 | 53.1 | e,E |
| No/no | 305 | 2,060 | 36.1 | 1.9 | 32.1 | 40.3 | * | 257 | 1,651 | 32.4 | 2.8 | 26.6 | 38.9 | |
| Job category | ||||||||||||||
| White collar | 410 | 3,266 | 25.1 | 1.7 | 21.5 | 29.1 | * | 288 | 1,826 | 16.8 | 1.5 | 13.7 | 20.4 | ‡ |
| Blue collar† | 171 | 1,210 | 38.0 | 4.8 | 28.2 | 48.9 | e | 134 | 1,075 | 38.9 | 5.8 | 27.2 | 52.0 | E |
| Source of loud work noise | ||||||||||||||
| Machinery/transport | ||||||||||||||
| Yes | 463 | 3,491 | 40.2 | 2.3 | 35.4 | 45.3 | 355 | 2,535 | 34.1 | 2.8 | 28.1 | 40.6 | ||
| No† | 95 | 567 | 28.2 | 4.7 | 19.1 | 39.6 | e,E | 82 | 493 | 27.1 | 5.5 | 16.8 | 40.7 | e,E |
| Music/people | ||||||||||||||
| Yes | 71 | 444 | 22.5 | 4.6 | 14.0 | 34.1 | * e,E | 61 | 386 | 22.2 | 5.2 | 12.9 | 35.6 | e,E |
| No† | 487 | 3,614 | 41.4 | 2.4 | 36.2 | 46.9 | 376 | 2,642 | 35.2 | 2.7 | 29.6 | 41.2 | ||
| Other (munitions and/or other unspecified) | ||||||||||||||
| Yes | 80 | 432 | 37.9 | 5.7 | 26.3 | 51.0 | e | 60 | 311 | 30.7 | 5.6 | 19.9 | 44.1 | e,E |
| No† | 478 | 3,626 | 38.0 | 1.8 | 34.0 | 42.1 | 377 | 2,717 | 33.0 | 2.3 | 28.2 | 38.2 | ||
Any hearing loss: FFPTA and/or HFPTA and/or LFPTA.
e, E use with caution (coefficient of variation 16.6–33.3%), population size and %, respectively.
f, F too unreliable to be published (coefficient of variation greater than 33.3%), population size and %, respectively.
DPOAE, distortion product otoacoustic emissions; FFPTA, four-frequency pure tone average over frequencies (0.5, 1, 2, and 4 kHz); HFPTA, high-frequency pure tone average over frequencies (3, 4, 6, and 8 kHz); LFPTA, low-frequency pure tone average over frequencies (0.5, 1, and 2 kHz).
*, ‡ significantly different from estimate for reference category (P < 0.05) and (P < 0.01), respectively.
†Reference category.
TABLE 8.
Prevalence of Audiometric Notch Among Working Canadians, Aged 16 to 79 Years: Demographics
| §Notch (n = 3,431) | ||Notch (n = 3,431) | |||||||||||||
| 95% CI | 95% CI | |||||||||||||
| Characteristics | n | N | % | SE % | From | To | n | N | % | SE % | From | To | ||
| ’000 | ’000 | |||||||||||||
| Total | 670 | 5,558 | 22.0 | 1.6 | 18.6 | 25.7 | 394 | 3,118 | 12.3 | 1.1 | 10.1 | 14.9 | ||
| Demographic characteristics | ||||||||||||||
| Sex | ||||||||||||||
| Men | 414 | 3,468 | 27.5 | 2.6 | 22.2 | 33.6 | ‡ | 304 | 2,400 | 19.1 | 1.9 | 15.2 | 23.7 | ‡ |
| Women† | 256 | 2,090 | 16.4 | 2.0 | 12.6 | 21.2 | 90 | 717 | 5.6 | 0.8 | 4.1 | 7.8 | ||
| Age group | ||||||||||||||
| 16–29 years† | 103 | 933 | 14.9 | 2.6 | 10.0 | 21.7 | e,E | f,F | ||||||
| 30–49 | 297 | 2,024 | 22.9 | 2.8 | 17.4 | 29.6 | * | 170 | 1,241 | 14.0 | 1.1 | 11.7 | 16.7 | |
| 50–79 | 270 | 2,602 | 25.5 | 2.4 | 20.6 | 31.0 | * | 190 | 1,563 | 15.3 | 2.5 | 10.6 | 21.5 | e |
| Education (highest level in household) | ||||||||||||||
| Postsecondary or more† | 504 | 3,998 | 21.2 | 1.6 | 17.8 | 25.0 | 299 | 2,212 | 11.7 | 1.2 | 9.4 | 14.5 | ||
| Less than postsecondary | 139 | 1,400 | 25.5 | 3.3 | 18.9 | 33.4 | 84 | 851 | 15.5 | 2.4 | 10.8 | 21.7 | e | |
| Household income | ||||||||||||||
| <$50,000† | 232 | 1,746 | 20.2 | 2.8 | 14.8 | 26.9 | 146 | 1,217 | 14.1 | 1.2 | 11.7 | 16.9 | ||
| $50,000 to <$100,000 | 235 | 1,799 | 21.0 | 2.0 | 16.9 | 25.7 | 143 | 907 | 10.6 | 1.2 | 8.2 | 13.6 | * | |
| $100,000 or more | 203 | 2,013 | 24.9 | 2.5 | 19.8 | 30.9 | 105 | 993 | 12.3 | 2.3 | 8.0 | 18.5 | e,E | |
Any hearing loss: FFPTA and/or HFPTA and/or LFPTA.
e, E use with caution (coefficient of variation 16.6–33.3%), population size and %, respectively.
f, F too unreliable to be published (coefficient of variation greater than 33.3%), population size and %, respectively.
DPOAE, distortion product otoacoustic emissions; FFPTA, four-frequency pure tone average over frequencies (0.5, 1, 2, and 4 kHz); HFPTA, high-frequency pure tone average over frequencies (3, 4, 6, and 8 kHz); LFPTA, low-frequency pure tone average over frequencies (0.5, 1, and 2 kHz).
*, ‡ significantly different from estimate for reference category (P < 0.05) and (P < 0.01), respectively.
†Reference category.
Audiometric notch definitions: §Criteria for audiometric notch 1: (1) thresholds at 0.5 and 1 kHz of ≤15 dB, (2) maximal threshold at 3, 4, or 6 kHz ≥15 dB higher than the highest threshold for 0.5 and 1 kHz, and (3) threshold at 8 kHz ≥10 dB lower (better than) the maximal threshold for 3, 4, or 6 kHz. (Niskar et al46); ||Criteria for audiometric notch 2: thresholds at 2 and 8 kHz were both minimally at hearing levels 10 dB lower (better than) than the threshold at 4 kHz (Wilson45).
Footnotes
This research was funded by Statistics Canada and Health Canada.
This study was approved by the Health Canada and Public Health Agency of Canada Review Ethics Board (Protocol #2005-0025).
The authors have no conflicts of interest.
REFERENCES
- 1.World Health Organization. Occupational noise: assessing the burden of disease from work-related hearing impairment at national and local levels. Environmental Burden of Disease Series, Number 9 2004; Geneva, Switzerland: World Health Organization, 1–33. [Google Scholar]
- 2.Picard M, Girard SA, Simard M, Larocque R, Leroux T, Turcotte F. Association of work-related accidents with noise exposure in the workplace and noise-induced hearing loss based on the experience of some 240,000 person-years of observation. Accident Analysis Prev 2008; 40:1644–1652. [DOI] [PubMed] [Google Scholar]
- 3.Rabinowitz PM. Le Prell CG, Henderson D, Fay RR, Popper AN. The public health significance of noise-induced hearing loss. Noise-Induced Hearing Loss: Scientific Advances. New York, NY: Springer Science+Business Media; 2012. 13–25. [Google Scholar]
- 4.Nelson DI, Nelson RY, Concha-Barrientos M, Fingerhut M. The global burden of occupational noise-induced hearing loss. Am J Ind Med 2005; 48:446–458. [DOI] [PubMed] [Google Scholar]
- 5.Palmer KT, Griffin MJ, Syddall HE, Davis A, Pannett B, Coggon D. Occupational exposure to noise and the attributable burden of hearing difficulties in Great Britain. Occup Environ Med 2002; 59:634–639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bureau of Labor, Statistics. Workplace Injuries and Illnesses in 2005. Washington, DC: United States Department of Labor; 2006. [Google Scholar]
- 7.Tak SW, Davis RR, Calvert GM. Exposure to hazardous workplace noise and the use of hearing protection devices among US workers: NHANES, 1999–2004. Am J Indust Med 2009; 52:358–371. [DOI] [PubMed] [Google Scholar]
- 8.Health, Safety Executive. Noise at Work, Guidance on Regulations. London, UK: HMSO; 1989. [Google Scholar]
- 9.Engdahl B, Tambs K. Occupation and the risk of hearing impairment—results from the Nord-Trondelag study on hearing loss. Scand J Work Environ Health 2010; 36:250–257. [DOI] [PubMed] [Google Scholar]
- 10.Masterson E, Tak S, Themann CL, et al. Prevalence of hearing loss in the United States by industry. Am J Indust Med 2013; 56:670–681. [DOI] [PubMed] [Google Scholar]
- 11.Masterson E, Deddens JA, Themann CL, Bertke S, Calvert GM. Trends in worker hearing loss by industry sector, 1981-2010. Am J Indust Med 2015; 56:670–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Reilly MJ, Rosenman KD, Kalinowski DJ. Occupational noise-induced hearing loss surveillance in Michigan. J Occup Environ Med 1998; 40:667–674. [DOI] [PubMed] [Google Scholar]
- 13.Workers’ Compensation Board. Noise Survey Project Report: Workers’ Compensation Board of British Columbia. Vancouver, British Columbia: WorksafeBC Hearing Loss Prevention Section; 2002. [Google Scholar]
- 14.Gunderson E, Moline J, Catalano P. Risks of developing noise-induced hearing loss in employees of urban music clubs. Am J Indust Med 1997; 31:75–79. [DOI] [PubMed] [Google Scholar]
- 15.Ologe FE, Akande TM, Olajide TG. Noise exposure, awareness, attitudes and use of hearing protection in a steel rolling mill in Nigeria. Occup Med 2005; 55:487–489. [DOI] [PubMed] [Google Scholar]
- 16.Rabinowitz PM, Sircar KD, Tarabar S, Galusha D, Slade MD. Hearing loss in migrant agricultural workers. J Agromed 2005; 10:9–17. [DOI] [PubMed] [Google Scholar]
- 17.Verbeek JH, Kateman E, Morata TC, Dreschler WA, Mischke C. Interventions to prevent occupational noise-induced hearing loss (Review). Cochrane Database Syst Rev:CD006396; 2012: 1–109. [DOI] [PubMed] [Google Scholar]
- 18.Hessel PA. Hearing loss among construction workers in Edmonton, Alberta, Canada. J Occup Environ Med 2000; 42:40–46. [DOI] [PubMed] [Google Scholar]
- 19.Lusk SL, Kerr MJ, Kauffman SA. Use of hearing protection and perceptions of noise exposure and hearing loss among construction workers. Am Indust Hyg J 1998; 59:466–470. [DOI] [PubMed] [Google Scholar]
- 20.Davies H. Occupational noise exposue and hearing protector use in Canadian lumber mills. J Occup Environ Hyg 2009; 6:32–41. [DOI] [PubMed] [Google Scholar]
- 21.Girard SA, Leroux T, Courteau M, Picard M, Turcotte F, Richer O. Occupational noise exposure and noise-induced hearing loss are associated with work-related injuries leading to admission to hospital. Inj Prev 2014; 0:1–5. [DOI] [PubMed] [Google Scholar]
- 22.Girard SA, Picard M, Davis AC, et al. Multiple work-related accidents: tracing the role of hearing status and noise exposure. Occup Environ Med 2009; 66:319–324. [DOI] [PubMed] [Google Scholar]
- 23.Hetu R, Getty L, Quoc HT. Impact of occupational hearing loss on the lives of workers. Occup Med 1995; 10:495–512. [PubMed] [Google Scholar]
- 24.Zwerling C, Sprince NL, Davis CS, Whitten PS, Wallace RB, Heeringa SG. Occupational injuries among older workers with disabilities: a prospective Cohort Study of the Health and Retirement Survey, 1992 to 1994. Am J Public Health 1998; 88:1691–1695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institute for Occupational Safety and Health (NIOSH). NIOSH Publications and Products: Occupationally-Induced Hearing Loss; 2010. Publication No. 2010-136 Accessed September 20, 2015. [Google Scholar]
- 26.Attias J, Horovitz G, El-Hatib N, et al. Detection and clinical diagnosis of noise-induced hearing loss by otoacoustic emissions. Noise Health 2001; 3:19–31. [PubMed] [Google Scholar]
- 27.Forshaw C. Report of an International Expert Symposium on the usefulness of Otoacoustic Emissions (OAE) Testing in Occupational Health Surveillance. Manchester, UK: Corporate Medical Unit, Health & Safety Executive; 2011. [Google Scholar]
- 28.Prasher D, Sulkowski W. The role of otoacoustic emissions in screening and evaluation of noise damage. Int J Occup Med Environ Health 1999; 12:183–192. [PubMed] [Google Scholar]
- 29.Seixas NS, Kujawa SG, Norton S, Sheppard L, Neitzel R, Slee A. Predictors of hearing threshold levels and distortion product otoacoustic emissions among noise exposed young adults. Occup Environ Med 2004; 61:899–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Atchariyasathian V, Chayarpham S, Saekhow S. Evaluation of noise-induced hearing loss with audiometer and distortion product otoacoustic emissions. J Med Assoc Thai 2008; 91:1066–1071. [PubMed] [Google Scholar]
- 31.Baradarnfar MH, Karamifar K, Mehrparvar AH, et al. Amplitude changes in otoacoustic emissions after exposure to industrial noise. Noise Health 2012; 14:28–31. [DOI] [PubMed] [Google Scholar]
- 32.Lapsley Miller JA, Marshall L, Heller LM. A longitudinal study of changes in evoked otoacoustic emissions and pure tone thresholds as measured in a hearing conservation program. Int J Audiol 2004; 43:307–322. [DOI] [PubMed] [Google Scholar]
- 33.Plinkert PK, Hemmert W, Wagner W, Just K, Zenner HP. Monitoring noise susceptibility: sensitivity of otoacoustic emissions and subjective audiometry. Br J Audiol 1999; 33:367–382. [DOI] [PubMed] [Google Scholar]
- 34.Mazurek B, Olze H, Haupt H, Szczepek AJ. The more the worse: the grade of noise-induced hearing loss associates with the severity of tinnitus. Int J Environ Res Public Health 2010; 7:3071–3079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Savastano M. Tinnitus with or without hearing loss: are its characteristics different? Euro Arch Oto-Rhino-Laryng 2008; 265:1295–1300. [DOI] [PubMed] [Google Scholar]
- 36.World Health Organization. The global burden of disabling hearing impairment: a call to action. 2014; Geneva: Bulletin WHO, 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hasson D, Theorell T, Westerlund H, Canlon B. Prevalence and characteristics of hearing problems in a working and non-working Swedish population. J Epidemiol Community Health 2010; 64:453–460. [DOI] [PubMed] [Google Scholar]
- 38.Health Canada. Noise from Machinery Intended for the Workplace; Environmental and Workplace Health. 2010. Available at: http://www.hc-sc.gc.ca/ewh-semt/noise-bruit/machinery-machines-eng.php [Google Scholar]
- 39.Legris M, Poulin P. Noise exposure profile among heavy equipment operators, associated laborers, and crane operators. Am Ind Hyg Assoc J 1998; 59:774–778. [DOI] [PubMed] [Google Scholar]
- 40.Workers’ Compensation Board (WCB). Occupational Health and Safety Regulation Victoria: Workers’ Compensation of British Columbia. Victoria, British Columbia: Queens Printer; 1998. [Google Scholar]
- 41.Statistics Canada. Canadian Health Measures Survey Data User Guide: Cycle 3. 2015. Available at: http://www23.statcan.gc.ca/imdb-bmdi/document/5071_D4_T9_V2-eng.htm Accessed October 19, 2015. [Google Scholar]
- 42.Carhart R, Jerger JF. Preferred method for clinical determination of pure-tone thresholds. J Speech Hear Disord 1959; 24:330–345. [Google Scholar]
- 43.American Academy of Audiology (AAA) Clinical Practice Guidelines. Childhood Hearing Screening. 2011. Available at: http://www.cdc.gov/ncbddd/hearingloss/documents/aaa_childhood-hearing guidelines_2011.pdf Accessed August 21, 2014. [Google Scholar]
- 44.American Speech Language Hearing Association (ASHA). Guidelines for Audiologic Screening. 1997. Available at: http://www.asha.org/policy.pdf Accessed August 21, 2014. [Google Scholar]
- 45.Wilson RH. Some observations on the nature of the audiometric 4000 Hz notch: data from 3430 veterans. J Am Acad Audiol 2011; 22:23–33. [DOI] [PubMed] [Google Scholar]
- 46.Niskar AS, Kieszak SM, Holmes AE, Esteban E, Rubin C, Brody DJ. Estimated prevalence of noise-induced hearing threshold shifts among children 6 to 19 years of age: the Third National Health and Nutrition Examination Survey, 1988–1994, United States. Pediatrics 2001; 108:40–43. [DOI] [PubMed] [Google Scholar]
- 47.Statistics Canada. National Occupational Classification (NOC). Catalogue no. 12-588-X; 2011. Available at: http://www.statcan.gc.ca/pub/12-583-x/12-583-x2011001-eng.pdf Accessed September 22, 2015. [Google Scholar]
- 48.Rao JNK, Wu CFJ, Yue K. Some recent work on resampling methods for complex surveys. Survey Methodol (Statistics Canada, Catalogue 12-001) 1992; 18:209–217. [Google Scholar]
- 49.Rust KF, Rao JNK. Variance estimation for complex surveys using replication techniques. Stat Methods Med Res 1996; 5:281–310. [DOI] [PubMed] [Google Scholar]
- 50.Masterson E, Tak S, Themann CL, Luckhaupt SE, Li J, Calvert GM. Hearing difficulty and tinnitus among U.S. workers and non-workers in 2007. Am J Indust Med 2016; 59:290–300. [DOI] [PubMed] [Google Scholar]
- 51.Feder K, Michaud D, Ramage-Morin P, McNamee J, Beauregard Y. Prevalence of hearing loss among Canadians aged 20 to 79: audiometric results from the 2012/2012 Canadian Health Measures Survey. Health Rep 2015; 26:10–17. [PubMed] [Google Scholar]
- 52.Rubak T, Kock SA, Koefoed-Nielsen B, Bonde JP, Kolstad HA. The risk of noise-induced hearing loss in the Danish workforce. Noise Health 2006; 8:80–87. [DOI] [PubMed] [Google Scholar]
- 53.Arndt V, Rothenbacher D, Brenner H, et al. Older workers in the construction industry: results of a routine health examination and a five year follow up. J Occup Environ Med 1996; 53:686–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilson DH, Walsh PG, Sanchez L, et al. The epidemiology of hearing impairment in an Australian adult population. Int J Epidemiol 1999; 28:247–252. [DOI] [PubMed] [Google Scholar]
- 55.Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Aff 2002; 21:60–76. [DOI] [PubMed] [Google Scholar]
- 56.Raphael D. Anderson J. Poverty, income inequality and health in Canada. Social Justice Series. Toronto, CA: CSJ Foundation for Research and Education; 2002. 1–20. [Google Scholar]
- 57.Kirchner DB, Evenson E, Dobie RA, et al. ACOEM Guidance Statement: occupational noise-induced hearing loss. J Occup Environ Med 2012; 54:106–108. [DOI] [PubMed] [Google Scholar]
- 58.Rabinowitz PM, Slade MD, Galusha D, Dixon-Ernst C, Cullen MR. Trends in the prevalence of hearing loss among young adults entering an industrial workforce 1985 to 2004. Ear Hear 2006; 27:369–375. [DOI] [PubMed] [Google Scholar]
- 59.Seixas N, Goldman B, Sheppard L, Neitzel R, Norton S, Kujawa SG. Prospective noise induced changes to hearing among construction industry apprentices. Occup Environ Med 2005; 62:309–317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Leensen MCJ, van Dulvenbooden JC, Dreschler WA. A retrospective analysis of noise-induced hearing loss in the Dutch construction industry. Int Arch Occup Environ Health 2011; 84:577–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Neitzel R, Seixas N, Goldman B, Daniell W. Contributions of non-occupational activities to total noise exposure of construction workers. Ann Occup Hyg 2004; 48:463–474. [DOI] [PubMed] [Google Scholar]
- 62.Moll van Charrente AW, Mulder PG. Perceptual ability and the risk of industrial accidents. Am J Epidemiol 1990; 131:653–663. [DOI] [PubMed] [Google Scholar]
- 63.Palmer KT, Harris EC, Coggon D. Chronic health problems and risk of accidental injury in the workplace: a systematic literature review. Occup Environ Med 2008; 65:757–764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Poulsen OM, Breum NO, Ebbehoj N, et al. Collection of domestic waste. Review of occupational health problems and their possible causes. Sci Total Environ 1995; 170:1–19. [DOI] [PubMed] [Google Scholar]
- 65.McBride DI, Williams S. Audiometric notch as a sign of noise induced hearing loss. Occup Environ Med 2001; 58:46–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Lapsley Miller JA, Marshall L. Robinette MS, Glattke TJ. Otoacoustic emissions as a preclinical measure of NIHL and susceptibility to NIHL. Otoacoustic Emissions, Clinical Application 3rd ed.New York: Thieme; 2007. 321–341. [Google Scholar]
- 67.Clark WW, Bohne BA. Effects of noise on hearing. JAMA 1999; 281:1658–1659. [DOI] [PubMed] [Google Scholar]
- 68.Quaranta A, Assennato G, Sallustio V. Epidemiology of hearing problems among adults in Italy. Scand Audiol 1996; 42:9–13. [PubMed] [Google Scholar]
- 69.Wong ACY, Ryan AF. Mechanisms of sensorineural cell damage, death and survival in the cochlea. Front Aging Neurosci 2015; 7:1–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Probst R, Lonsbury-Martin BL, Martin GK. A review of otoacoustic emissions. JASA 1991; 89:2027–2067. [DOI] [PubMed] [Google Scholar]
- 71.Attias J, Furst M, Furman V, et al. Noise-induced otoacoustic emission loss with or without hearing loss. Ear Hear 1995; 16:612–618. [DOI] [PubMed] [Google Scholar]
- 72.Helleman HW, Jansen EJM, Dreschler WA. Otoacoustic emissions in a hearing conservation program: general applicability in longitudinal monitoring and the relation to changes in pure-tone thresholds. Int J Audiol 2010; 49:410–419. [DOI] [PubMed] [Google Scholar]
- 73.Balatsouras DG. The evaluation of noise-induced hearing loss with distortion product otoacoustic emissions. Med Sci Monit 2004; 10:218–222. [PubMed] [Google Scholar]
- 74.Marques FP, da Costa EA. Exposure to occupational noise: otoacoustic emissions test alterations. Braz J Otorhinolaryngol 2006; 72:362–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.American College of Occupational, Environmental Medicine. ACOEM Evidence-Based Statement: Noise-Induced Hearing Loss. J Occup Environ Med 2003; 45:579–581. [DOI] [PubMed] [Google Scholar]
- 76.Lusk SL, Kelemen MJ. Predicting use of hearing protection: a preliminary study. Public Health Nurs 1993; 10:189–196. [DOI] [PubMed] [Google Scholar]
- 77.Lusk SL, Ronis DL, Hogan MM. Test of the Health Promotion Model as a causal model of construction workers’ use of hearing protection. Res Nurs Health 1997; 20:183–194. [DOI] [PubMed] [Google Scholar]
- 78.Melamed S, Rabinowitz S, Feiner M, Weisber E, Ribak J. Usefulness of the protection motivation theory in explaining hearing protection device use among male industrial workers. Health Psychol 1996; 15:209–215. [DOI] [PubMed] [Google Scholar]
- 79.Hong O, Chin DL, Samo DG. Hearing loss and use of hearing protection among career firefighters in the United States. J Occup Environ Med 2013; 55:960–965. [DOI] [PubMed] [Google Scholar]
- 80.Franks JR. Noise in the construction industry and its effect on hearing. Hearing Instr 1990; 41:18–21. [Google Scholar]
- 81.Hager LD. Sound exposure profiling: a noise monitoring alternative. Am Ind Hyg Assoc J 1998; 59:414–418. [Google Scholar]
- 82.Suter AH. Construction noise: exposure, effects, and the potential for remediation; a review and analysis. Am Indust Hyg Assoc J 2002; 63:768–789. [DOI] [PubMed] [Google Scholar]
- 83.Neitzel R, Seixas N. Effectiveness of hearing protection use among construction workers. J Occup Environ Hyg 2005; 2:227–238. [DOI] [PubMed] [Google Scholar]
- 84.Kerr M, Brosseau L, Johnson CS. Noise levels of selected construction tasks. Am Ind Hyg Assoc J 2002; 63:334–339. [DOI] [PubMed] [Google Scholar]
- 85.Arezes PM, Miguel AS. Hearing protection use in industry: the role of risk perception. Safety Sci 2005; 43:253–267. [Google Scholar]
- 86.Moller AR. Moller AR, Langguth B, DeRidder D, Kleinjung T. Epidemiology of tinnitus in adults. Textbook of Tinnitus. New York: Springer Science; 2010. 29–37. [Google Scholar]
- 87.Heller A. Classification and epidemiology of tinnitus. Otolaryngol Clin North Am 2003; 36:239–248. [DOI] [PubMed] [Google Scholar]
- 88.Tyler RS. Tinnitus Handbook. San Diego, CA: Singular Thomson Learning; 2000: 1–464. [Google Scholar]
- 89.National Center for Health Statistics. Hearing Status Among Adults, United States, 1960–1962. Washington, DC: US Department of Health, Education and Welfare; 1968. [Google Scholar]
- 90.Axelsson A, Ringdahl A. Tinnitus: a study of its prevalence and characteristics. Br J Audiol 1989; 23:53–62. [DOI] [PubMed] [Google Scholar]
- 91.Coles RR. Epidemiology of tinnitus: prevalence. J Laryngol Otol Suppl 1984; 9:7–15. [DOI] [PubMed] [Google Scholar]
- 92.Davis AC. The prevalence of hearing impairment and reported hearing disability among adults in Great Britain. Int J Epidemiol 1989; 18:911–917. [DOI] [PubMed] [Google Scholar]
- 93.Engdahl B, Krog NH, Kvestad E, Hoffman HJ, Tambs K. Occupation and the risk of bothersome tinnitus: results from a prospective cohort study (HUNT). BMJ Open 2012; 2:1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Fujii K, Nagata C, Nakamura K, et al. Prevalence of tinnitus in community-dwelling Japanese adults. J Epidemiol 2011; 21:299–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Hannaford PC, Simpson JA, Bisset AF, Davis A, McKerrow W, Mills R. The prevalence of ear, nose and throat problems in the community: results from a national cross-sectional postal survey in Scotland. Fam Pract 2005; 22:227–233. [DOI] [PubMed] [Google Scholar]
- 96.Carter L. Prevalence of Hearing Loss and its Relationship to Leisure-Sound Exposure. Final Report. New South Wales, Australia: Department of Health Aging, National Acoustic Laboratories, Research Division of Australian Hearing; 2011: 1–60. [Google Scholar]
- 97.Shargorodsky J, Curhan GC, Wildon RF. Prevalence and characteristics of tinnitus among US adults. Am J Med 2010; 123:711–718. [DOI] [PubMed] [Google Scholar]
- 98.Park RJ, Moon JD. Prevalence and risk factors of tinnitus: the Korean National Health and Nutrition Examination Survey 2010–2011, a cross-sectional study. Clin Otolaryngol 2014; 39:89–94.24612912 [Google Scholar]
- 99.Scientific Committee on Emerging and Newly Identified Health Risks (SCENIHR). Potential Health Risks of Exposure to Noise From Personal Music Players and Mobile Phone Including a Music Playing Function. European Commission; Brussels, Belgium: Directorate-General for Health & Consumers; 2008. [Google Scholar]
- 100.Erlandsson SI, Hallberg LRM. Prediction of quality of life in patients with tinnitus. Br J Audiol 2000; 34:11–20. [DOI] [PubMed] [Google Scholar]
- 101.Holmes S, Padgham ND. Ringing in the ears”: narrative review of tinnitus and its impact. Biolog Res Nurs 2011; 13:97–108. [DOI] [PubMed] [Google Scholar]
- 102.Krog NH, Engdahl B, Tambs K. The association between tinnitus and mental health in a general population sample: results from the HUNT Study. J Psychosom Res 2010; 69:289–298. [DOI] [PubMed] [Google Scholar]
- 103.Adams P, Marano M. Current Estimates from the National Health Interview Survey, 1994. In: Vital and health statistics. Hyattsville, MD: National Center for Health Statistics; 1995. [PubMed] [Google Scholar]
- 104.Benson V, Marano M. Current estimates from the National Health Interview Survey 1995, In: Vital and health statistics. Hyattsville, MD: National Center for Health Statistics; 1998. [PubMed] [Google Scholar]
- 105.Davis AC. Hearing in Adults: The Prevalence and Distribution of Hearing Impairment and Reported Hearing Disability in the MRC Institute of Hearing Research's National Study of Hearing. London: Whurr Publishers Ltd; 1995. [Google Scholar]
- 106.Ries P. Prevalence and Characteristics of Persons With Hearing Trouble: United States, 1990-91, in Vital and Health Statistics. Hyattsville, MD: National Center for Health Statistics; 1994. [PubMed] [Google Scholar]
- 107.Nondahl DK, Cruickshanks KJ, Wiley TL, Klein R, Klein BE, Tweed TS. Prevalence and 5-year incidence of tinnitus among older adults: the epidemiology of hearing loss study. J Am Acad Audiol 2002; 13:323–331. [PubMed] [Google Scholar]
- 108.Izuhura K, Wada K, Nakamura K, et al. Association between tinnitus and sleep disorders in the general Japanese population. Ann Otolog Rhino Laryngol 2013; 122:701–706. [DOI] [PubMed] [Google Scholar]
- 109.Langguth B. A review of tinnitus symptoms beyond “ringing in the ears”: a call to action. Curr Med Res Opinion 2011; 27:1635–1643. [DOI] [PubMed] [Google Scholar]
- 110.Meikle MB, Creedon TA, Griest SE. Tinnitus Archive, 2nd ed. 2004. Available at: http://www.tinnitusarchive Accessed September 26, 2015. [Google Scholar]
- 111.Sanchez L, Stephens D. A tinnitus problem questionnaire in a clinic population. Ear Hear 1997; 18:210–217. [DOI] [PubMed] [Google Scholar]
- 112.Tan CM, Lecluyse W, McFerran D, Meddis R. Tinnitus and patterns of hearing loss. J Assoc Res Otolaryngol 2013; 14:275–282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Schaette R, McAlpine D. Tinnitus with a normal audiogram: physiological evidence for hidden hearing loss and computational model. J Neurosci 2011; 31:13452–13457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Melamed S, Luz J, Green MS. Noise exposure, noise annoyance and their relation to psychological distress, accident and sickness absence among blue collar workers: the Cordiss Study. Israel J Med Sci 1992; 28:629–635. [PubMed] [Google Scholar]
- 115.Cantley LF, Galusha D, Cullen MR, et al. Does tinnitus, hearing asymmetry, or hearing loss predispose to occupational injury risk? Int J Audiol 2015; 54 suppl 1:s30–s36. [DOI] [PMC free article] [PubMed] [Google Scholar]


