Abstract
Study Design:
Case description.
Objective:
Acute calcific tendinitis of the longus colli muscle is a rare clinical entity that causes severe neck pain. This entity is not well recognized due to its nonspecific presentation such as acute neck pain, neck stiffness, and odynophagia. The importance of this disease with a review of the literature is presented.
Summary of background data:
Acute calcific tendinitis of the longus colli muscle is an inflammatory condition caused by deposition of calcium hydroxyapatite in the superior oblique tendon fibers of the longus colli muscle. It can be misdiagnosed as other life-threatening conditions including retropharyngeal abscess, resulting in unnecessary medical or surgical interventions.
Methods:
We retrospectively reviewed the clinical data, radiological features, and laboratory reports of 8 patients who were diagnosed with acute calcific tendinitis of the longus colli muscle and seen at our institution between April 2008 and March 2015 in this article. We describe the clinical presentation, diagnosis, and treatment of acute calcific tendinitis of the longus colli muscle.
Results:
There were 5 men and 3 women who ranged in age from 41 to 49 years (mean age: 44.5 years). The associated symptoms included neck pain, stiffness, odynophagia, and headache. The duration of symptoms varied from 2 days to 1 week. All patients showed calcific deposition inferior to the anterior arch of the atlas, and prevertebral effusion extending from C1 to C4. All patients were treated with NSAIDs and immobilization with a cervical brace, and most patients showed complete resolution of symptoms within 1 week.
Conclusion:
We report 8 cases of acute calcific tendinitis of the longus colli, and describe the symptoms and radiological findings in detail. Awareness of this rare, benign, and self-limiting disease entity with characteristic radiologic findings is essential for early diagnosis and to avoid unnecessary medical and surgical interventions.
Keywords: longus colli, neck pain, tendinitis
Key Points
Acute calcific tendinitis of the longus colli muscle is a rare clinical entity that causes severe neck pain.
The disease can be diagnosed by computed tomography and resolved completely with medication and immobilization without aggressive treatment.
In this disease, early and correct diagnosis is required to avoid unnecessary medical and surgical intervention.
1. Introduction
Acute calcific tendinitis of the longus colli muscle is an inflammatory condition of the superior oblique tendons of the longus colli muscle, a neck flexor located in the upper cervical spine. It is a rare condition that causes severe neck pain, and it is also known as prevertebral calcific tendinitis or retropharyngeal calcific tendinitis. In 1964, it was first described by Hartley.[1] Its incidence is low; but this entity is underreported. Histopathologically, biopsy demonstrated a foreign-body inflammatory response to amorphous hydroxyapatite deposition in the longus colli muscle.[2] This finding is similar to calcific tendinitis of extremities like rotator cuff. The clinical symptoms are usually nonspecific and include acute neck pain and stiffness, limited cervical motion, or odynophagia. The diagnosis is usually made by detecting amorphous calcification anterior to C1-C2 level and prevertebral soft tissue swelling extending from C1 to C4 on plain radiographs and computed tomography (CT).
Although this entity has been reported previously, it can be easily overlooked or misdiagnosed due to its nonspecific presentation and infrequent incidence, and it can be confused with other serious pathologies, like retropharyngeal abscess, infectious spondylitis, or meningitis.[3]
Misdiagnosis of this entity could result in unnecessary medical or surgical interventions. We present 8 cases of acute calcific tendinitis of the longus colli, in which radiological findings have been described based on plain radiographs, CT, and magnetic resonance imaging (MRI). We review the relevant literature and highlight the characteristic features of this entity to help clinicians make an accurate diagnosis.
2. Materials and methods
We retrospectively evaluated the records of 8 patients with a diagnosis of acute calcific tendinitis of the longus colli, who visited Chonnam National University Hospital, South Korea, between April 2008 and March 2015. We present cases, including the clinical records, laboratory examinations including demographics, symptoms, physical examinations, treatment, and radiologic studies such as plain radiographs, CT, and MRI.
2.1. Results and case
There were 5 men and 3 women who ranged in age from 41 to 49 years (mean age: 44.5 years) (Table 1). The associated symptoms included continuous neck pain (100%), neck stiffness (100%), odynophagia (swallowing difficulty due to sore throat; 87.5%), and occipital headache (75%). The duration of symptoms varied from 2 days to 1 week. None of the patients had relevant underlying disease in the past, including any infections. All patients had limited range of motion (ROM) of the neck and febrile sense without fever.
Table 1.
Clinical characteristic of acute calcific tendinitis of longus colli: 8 cases.
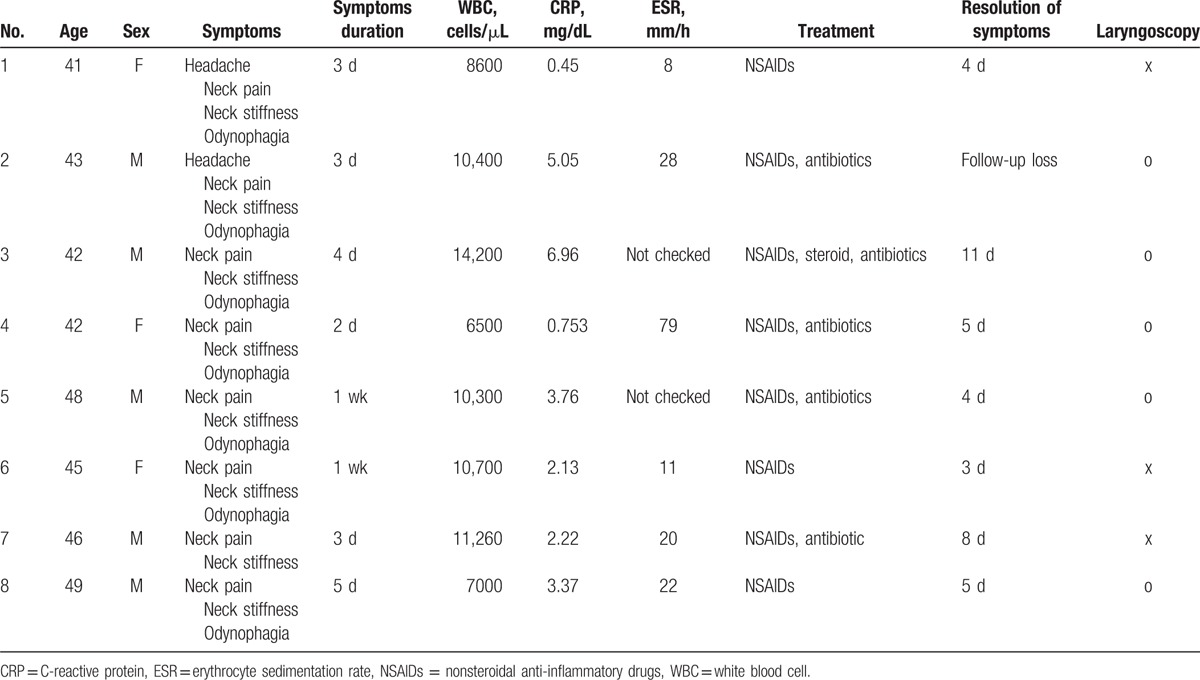
Except for 2 patients, laboratory data including white blood cell (WBC) count, C-reactive protein (CRP), and erythrocyte sedimentation rate (ESR) were available in all the other patients. The WBC count (reference range <10,800 cells/μL) remained normal in 6 patients. The CRP (reference range <1 mg/dL) was elevated in 6 patients. The ESR (reference range <20 mm/h) was increased in 3 patients.
All patients showed calcific deposition anterior to the atlas or dens, which is the insertion site of the superior oblique tendon of the longus colli, and prevertebral effusion from C1 to C4 (Fig. 1).
Figure 1.
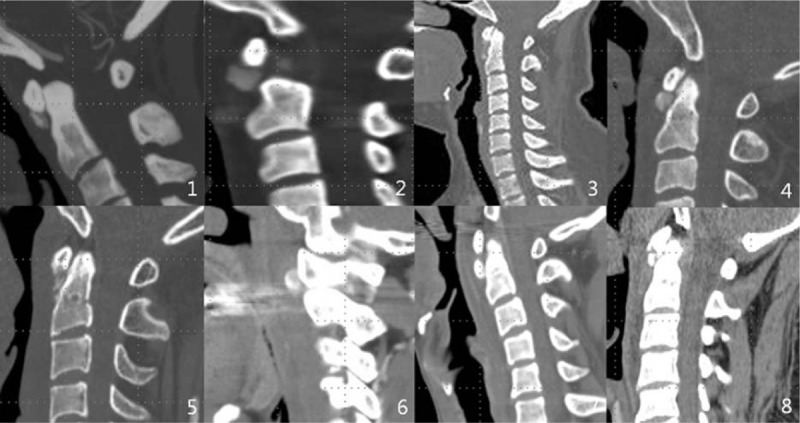
CT of all patients: showed calcific deposition in anterior aspect of atlas or axis; the insertion site of superior oblique tendon of longus colli and prevertebral effusion. Each image is labeled to cross-reference with Table 1 demographics.
All patients were treated with nonsteroidal anti-inflammatory drugs (NSAIDs) and a cervical brace was recommended for immobilization. Unfortunately, 62.5% patients were treated with antibiotics, as this condition was confused with a retropharyngeal abscess.
Of the patients, 75% showed complete resolution of symptoms within 1 week. The patients who were treated with NSAIDs 2 days after presentation showed resolution of symptoms 1 week after from the time on medication.
The clinical characteristics of acute calcific tendinitis of the longus colli in 8 patients are summarized in Table 1.
2.2. Case
A 41-year-old woman presented with a 3-day history of headache, neck pain, neck stiffness, and odynophagia. There was no history of trauma, relevant underlying disease, or recent illness. On physical examination, ROM of the neck was quite limited, in all directions especially extension. Region of headache was occipital, neck was aching with tenderness and pain exacerbated by movement. Odynophagia developed while swallowing, and pain worsened when opening the mouth. She had tenderness along sternocleidomastoid muscle and posterior neck. There was no radiating pain or any abnormal oropharyngeal lesion. On laboratory testing, inflammatory markers including WBC (8600 cells/μL), CRP (0.45 mg/dL), and ESR (8 mm/h) remained within the normal range. The initial plain x-rays of the cervical spine revealed mild diffuse swelling in the retropharyngeal space (Fig. 2). Because of severe occipital headache, she was admitted and brain CT with angiography was performed, and an amorphous calcific deposit anterior to the C1-2 joint with mild prevertebral soft tissue thickening was detected inadvertently. MRI showed soft tissue swelling and fluid collection in the retropharyngeal space. There were no findings of abscess, spondylitis, or unknown traumatic injury.
Figure 2.

The x-ray revealed diffuse swelling on the retropharyngeal space. Neck CT showed calcific deposit on C1-2 joint. MRI showed a nodular lesion which located the insertion site of superior oblique tendon of longus colli (white arrow) and retropharyngeal fluid.
Based on the characteristic imaging findings and the patient's clinical presentation, the patient was diagnosed with acute calcific tendinitis of the longus colli, and treated with NSAIDs and soft cervical collar for immobilization. Within 2 days from the initiation of treatment, the symptoms were reduced. Plain x-ray and CT performed at 1 week after presentation revealed reduction in the calcific deposit and retropharyngeal soft tissue swelling (Fig. 3). After 10 days of admission, she had fully recovered.
Figure 3.
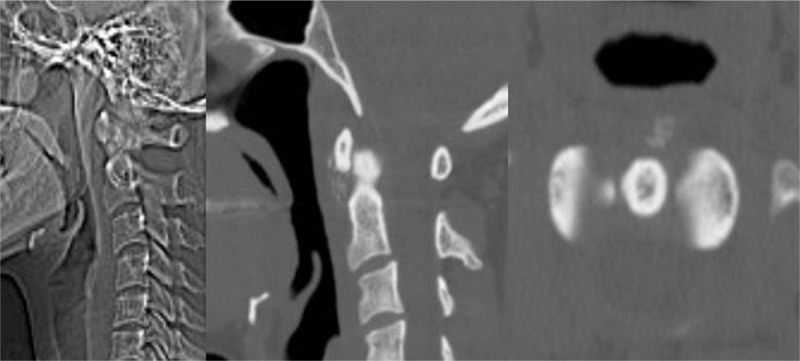
Radiologic examination at 1 wk after presentation. X-ray and CT of neck revealed reduced calcific deposit and retropharyngeal soft tissue swelling.
3. Discussion
Acute calcific tendinitis of the longus colli muscle is a rare clinical entity. The suggested pathogenesis of this condition is the deposition of calcium hydroxyapatite crystals and an aseptic inflammatory process in the tendon of the longus colli muscle.[4] The longus colli muscle is located in the prevertebral area and consists of 3 portions: superior oblique, vertical, and inferior oblique fibers. Superior oblique fibers originate from the anterior tubercles of the transverse processes of C3 to C5 vertebrae and fuse into a single tendon that inserts into the anterior tubercle of the atlas. Typically, the calcium deposit accumulates in the superior oblique fibers of the longus colli muscle, mainly at the C1-C2 level.[2] Hence, acute calcific tendinitis of the longus colli is a type of calcium hydroxyapatite deposition disease (CHAD), which typically involves the large joints, such as the hip or shoulder joint.[5,6] The cause of calcific deposit is unclear, but repetitive trauma, recent injury, tissue necrosis, or ischemia may play a role.[7,8] It has been suggested that rupture of the capsule causes release of calcific hydroxyapatite crystals into the tissue, resulting in an acute inflammatory response that provokes neck pain, muscle spasm, and local inflammation. When calcium is absorbed from the tissue, inflammation and the patient's symptoms resolve.[9,10] Duration of symptoms and time to resolve is mostly <1 month. This infers acute characteristic of disease.
The true incidence is still unknown because this condition is probably underdiagnosed.[8,11,12] With the frequent use of CT, its true incidence is probably higher than previously thought. It has been reported in adults between the ages of 21 and 81 years with the predominant age range being 30 to 60 years.[10,12–15] The sex incidence is equal.[15,16] The common presenting symptoms are acute to subacute onset of neck pain and stiffness, and it is often associated with odynophagia. The odynophagia is due to the close proximity of the retropharyngeal space to the pharyngeal constrictors.[17] Physical examination shows paraspinal muscle spasm with the head held in slight flexion. The ROM is extremely limited, especially in extension. The patient may be afebrile or may have a low-grade fever. Previous review of literature reports that neck pain (94%), limited range of neck motion (45%), odynophagia (45%), and neck stiffness (42%) are major symptoms at present.[7] In our cases, all patients suffered from neck pain and neck stiffness. Laboratory tests may show inflammatory signs, such as mild leukocytosis, mild elevation of the ESR, and confusing retropharyngeal infection.[1,2] Sometimes, occipital headache is the presenting symptom which may be caused by the greater and lesser occipital nerve irritation by reactive muscle spasm.[13] Clinically, many cases may have been treated as tension-type headache or some other disorder.[16] To exclude the other causes of acute neck pain, such as traumatic injury, retropharyngeal abscess, infectious spondylitis, or meningitis, the diagnostic imaging work-up should be performed.
The imaging modality of choice is CT of the cervical spine, because CT easily detects calcific deposition inferior to the anterior arch of the atlas and prevertebral effusion extending from C1 to C4—the 2 distinct characteristics in diagnosis of acute calcific tendinitis of the longus colli. Plain radiographs of the cervical spine reveal amorphous calcification anterior to C1-C2 level and prevertebral soft tissue swelling. However, the subtle amorphous calcific deposit is not always visible on plain radiographs, and only diffuse soft tissue swelling may provide a clue for diagnosis. MRI may be more useful for demonstrating edematous swelling or fluid collection in the retropharyngeal space. However, the representation of calcification by MRI is inferior to that by CT. Despite the insensitivity of MRI to demonstrate calcific deposition within the tendon, it can provide useful information that helps to exclude spondylitis or epidural abscess.[2,18,19]
Awareness of this disease entity with characteristic radiologic findings can prevent inappropriate medical and surgical treatment. This condition is usually confused with a retropharyngeal abscess. In 5 patients of our series, the initial diagnosis was retropharyngeal abscess, and the Ear, Nose, and Throat Department performed a fibroscopic examination, which revealed a patent airway and no drainable abscess. Then, these patients were transferred to our department after laryngoscopic work-up. There are 3 main differentiating features of acute calcific tendinitis of the longus colli from retropharyngeal abscess: the lack of enhancement surrounding the effusion; the absence of suppurative inflammatory retropharyngeal lymph nodes; and the presence of pathognomonic calcification in the longus colli muscle.[6,7,13]
Acute calcific tendinitis of the longus colli is a self-limiting condition that resolves spontaneously after 1 to 2 weeks.[2,11,20] Resolution of symptoms can be easily achieved by taking NSAIDs and cervical immobilization, preventing movement triggering pain.[2,3,7,21] Improvement of symptoms frequently occurs within 3 to 5 days after initiation of treatment, and complete resolution usually occurs within 3 weeks. Sometimes, the patients with severe symptoms get relief from a short course of steroid therapy. Invasive examination and treatment procedure should be avoided. If symptoms persist for >2 weeks, another cause should be sought.[10] The calcium deposit is dissolved and soft tissue swelling is usually resolved within a month on plain radiographs or CT.[5] In our presented case, the calcific deposition also resolved as the symptoms resolved.
We presented 8 cases of acute calcific tendinitis of the longus colli, which was resolved by conservative treatment. In patients with neck pain and stiffness, limited cervical motion, and odynophagia, this entity should be kept in mind as a differential diagnosis. We performed physical examination for meningeal sign using Kerning maneuver and Brudzinski maneuver, but no patient showed any sign. CT scan is the gold standard for diagnosis. After CT scans reveal an amorphous calcific deposit and soft tissue swelling, which indicate acute calcific tendinitis, invasive diagnostic and therapeutic procedures such as laryngoscopy, biopsy, or antibiotics are not necessary. The absence of enhancement surrounding the effusion can be helpful in distinguishing a reactive effusion from an abscess. Conservative treatment with NSAIDs and a soft neck collar for immobilization is quite helpful in reducing the symptoms. Awareness of this rare, benign, and self-limiting disease entity with characteristic radiologic findings is essential for early diagnosis and to avoid unnecessary medical and surgical interventions.
Our case description has several limitations. Except one, all the patients with resolved symptoms visited hospital just 1 time and did not take CT scan due to cost. And a prescription like antibiotics that was not needed was added. Further studies need to be performed prospectively with large numbers of subjects for validating the effectiveness of conservative treatment.
4. Conclusion
We report 8 cases of acute calcific tendinitis of the longus colli, and describe the symptoms and radiological findings in detail. Awareness of this rare, benign, and self-limiting disease entity with characteristic radiologic findings and laboratory reports showing a high ESR and a low CRP is essential for early diagnosis and to avoid unnecessary medical and surgical interventions.
Footnotes
Abbreviations: CHAD = calcium hydroxyapatite deposition disease, CRP = C-reactive protein, CT = computed tomography, ESR = erythrocyte sedimentation rate, MRI = magnetic resonance imaging, NSAIDs = nonsteroidal anti-inflammatory drugs, ROM = range of motion, WBC = white blood cell.
This study was supported by a grant (CRI13902-21) Chonnam National University Hospital Biomedical Research Institute.
The authors report no conflicts of interest.
References
- [1].Hartley J. Acute cervical pain associated with retropharyngeal calcium deposit. A case report. J Bone Joint Surg Am 1964;46:1753–4. [PubMed] [Google Scholar]
- [2].Ring D, Vaccaro AR, Scuderi G, et al. Acute calcific retropharyngeal tendinitis. Clinical presentation and pathological characterization. J Bone Joint Surg Am 1994;76:1636–42. [DOI] [PubMed] [Google Scholar]
- [3].Bladt O, Vanhoenacker R, Bevernage C, et al. Acute calcific prevertebral tendinitis. JBR-BTR 2008;91:158–9. [PubMed] [Google Scholar]
- [4].Eastwood JD, Hudgins PA, Malone D. Retropharyngeal effusion in acute calcific prevertebral tendinitis: diagnosis with CT and MR imaging. AJNR Am J Neuroradiol 1998;19:1789–92. [PMC free article] [PubMed] [Google Scholar]
- [5].Tezuka F, Sakai T, Miyagi R, et al. Complete resolution of a case of calcific tendinitis of the longus colli with conservative treatment. Asian Spine J 2014;8:675–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Chung T, Rebello R, Gooden EA. Retropharyngeal calcific tendinitis: case report and review of literature. Emerg Radiol 2005;11:375–80. [DOI] [PubMed] [Google Scholar]
- [7].Park R, Halpert DE, Baer A, et al. Retropharyngeal calcific tendinitis: case report and review of the literature. Semin Arthritis Rheum 2010;39:504–9. [DOI] [PubMed] [Google Scholar]
- [8].Jiménez S, Millán JM. Calcific retropharyngeal tendinitis: a frequently missed diagnosis. Case report. J Neurosurg Spine 2007;6:77–80. [DOI] [PubMed] [Google Scholar]
- [9].Southwell K, Hornibrook J, O’Neill-Kerr D. Acute longus colli calcific tendonitis causing neck pain and dysphagia. Otolaryngol Head Neck Surg 2008;138:405–6. [DOI] [PubMed] [Google Scholar]
- [10].Razon RV, Nasir A, Wu GS, et al. Retropharyngeal calcific tendonitis: report of two cases. J Am Board Fam Med 2009;22:84–8. [DOI] [PubMed] [Google Scholar]
- [11].Zibis AH, Giannis D, Malizos KN, et al. Acute calcific tendinitis of the longus colli muscle: case report and review of the literature. Eur Spine J 2013;22(suppl 3):S434–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Levy Z, Carroll J, Farley H. Benign nuchal rigidity: the emergency department evaluation of acute prevertebral calcific tendonitis. West J Emerg Med 2012;13:114–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Ellika SK, Payne SC, Patel SC, et al. Acute calcific tendinitis of the longus colli: an imaging diagnosis. Dentomaxillofac Radiol 2008;37:121–4. [DOI] [PubMed] [Google Scholar]
- [14].Estimable K, Rizk C, Pujalte GG. A rare case of neck pain: acute longus colli calcific tendinitis in a possibly immunocompromised individual. J Am Board Fam Med 2015;28:146–50. [DOI] [PubMed] [Google Scholar]
- [15].Kupferman TA, Rice CH, Gage-White L. Acute prevertebral calcific tendinitis: a nonsurgical cause of prevertebral fluid collection. Ear Nose Throat J 2007;86:164–6. [PubMed] [Google Scholar]
- [16].Wakabayashi Y, Hori Y, Kondoh Y, et al. Acute calcific prevertebral tendonitis mimicking tension-type headache. Neurol Med Chir (Tokyo) 2012;52:631–3. [DOI] [PubMed] [Google Scholar]
- [17].Omezzine SJ, Hafsa C, Lahmar I, et al. Calcific tendinitis of the longus colli: diagnosis by CT. Joint Bone Spine 2008;75:90–1. [DOI] [PubMed] [Google Scholar]
- [18].Mihmanli I, Karaarslan E, Kanberoglu K. Inflammation of vertebral bone associated with acute calcific tendinitis of the longus colli muscle. Neuroradiology 2001;43:1098–101. [DOI] [PubMed] [Google Scholar]
- [19].Patel TK, Weis JC. Acute neck pain in the emergency department: consider longus colli calcific tendinitis vs meningitis. Am J Emerg Med 2017;35:943.e3–4. [DOI] [PubMed] [Google Scholar]
- [20].Park SY, Jin W, Lee SH, et al. Acute retropharyngeal calcific tendinitis: a case report with unusual location of calcification. Skeletal Radiol 2010;39:817–20. [DOI] [PubMed] [Google Scholar]
- [21].Harnier S, Kuhn J, Harzheim A, et al. Retropharyngeal tendinitis: a rare differential diagnosis of severe headaches and neck pain. Headache 2008;48:158–61. [DOI] [PubMed] [Google Scholar]


