Abstract
Background:
Esophageal duplication cysts (EDCs) are rare congenital anomalies that can be associated with symptomatic spinal abnormalities, but presentations due to EDC symptoms are rarely found in the presence of spinal abnormalities.
Case summary:
A 6-month-old infant weighing approximately 5.0 kg presented with a 2-month pulmonary infection and more recent difficulty swallowing and nutritional intolerance that did not improve with medical treatment. Contrast-enhanced chest computed tomography showed a well-defined, mediastinal, homogeneous, low-density cystic mass of 11.9 × 5.5 × 5.1 cm, compressing the liver and bending the trachea forward. Hemivertebrae were present (T4 and T3). Diagnostic laparoscopy was performed, but was converted to open surgery. After ensuring that the cyst was not within the abdominal cavity, thoracotomy was performed, and the cyst was completely resected. Pathophysiological examination revealed an EDC. The patient recovered well, without symptoms 6 months later.
Conclusions:
Overall, noninvasive imaging and diagnostic procedures may not be sufficient to define the exact location of an EDC. Although hemivertebrae were present, they were asymptomatic and did not require treatment; only the EDC induced nonspecific symptoms that disappeared after surgery.
Keywords: esophageal duplication cyst, hemivertebrae, infant
1. Introduction
Congenital esophageal duplication cysts (EDCs) are rare congenital anomalies and can be associated with other congenital anomalies such as small intestinal duplication, esophageal atresia distal to the duplication, and tracheoesophageal fistulas.[1] They are often associated with spinal abnormalities, including scoliosis and fusion, which help achieve correct diagnosis.[1] Neuroenteric cysts have been reported to be associated with butterfly vertebra, spina bifida, and hemivertebrae.[2] The incidence of congenital esophageal cysts is estimated at 1:8200, with 2:1 male predominance.[3,4] Patients with esophageal cysts usually present with pulmonary infection, respiratory distress, difficulty swallowing, and nutritional intolerance due to compression and infection. Most of these cysts are benign, with asymptomatic anomalies that occur during foregut formation; neurological complications are usually the reasons for initial investigation. The preferred treatment is complete surgical resection, and the operation is not difficult. Physicians should be familiar with this disease. We herein report a rare case of a large esophageal duplication cyst with hemivertebrae with an initial presentation of esophageal symptoms.
2. Case report
A 6-month-old Uighur Chinese male infant presented with a history of pulmonary infection for at least 2 months. He had received treatments for pneumonia, using aerosolized second-generation antibiotics. Difficulty swallowing and nutritional intolerance appeared after the onset of pulmonary infection. The infant was born at 38 weeks (3200 g and Apgar score of 9), through caesarean section to a second-time pregnant mother. Antenatal and perinatal histories were uneventful. There was no family history of congenital diseases. On physical examination, the right lung had voiceless percussion, and wheezing could be heard in both lungs. The infant had nutritional intolerance and funnel chest. At admission, chest X-ray was performed, and the patient was diagnosed with bronchopneumonia. The electroencephalogram, limb electromyogram, cardiac ultrasound, blood count, and routine biochemical parameters were all normal.
Barium swallow examination did not show substantial luminal narrowing or trace pressure (Fig. 1A). The day after admission, 3-dimensional computed tomography (CT) reconstruction demonstrated a cystic mass located in the posterior mediastinum. This mass displayed well-defined margins and was fluid-filled, but free of air-fluid levels. The cyst was 11.9 × 5.4 × 5.1 cm. The average wall thickness was 0.5 cm and increased from the extra-pleural space or enterocelia, isolated within the esophagus. The cyst compressed the fore lying trachea, right main bronchus, right inferior lobe (anteriorly), and liver (Fig. 1B). The hemivertebrae were located in the upper thoracic spine (T4 and T3) (Fig. 1C).
Figure 1.
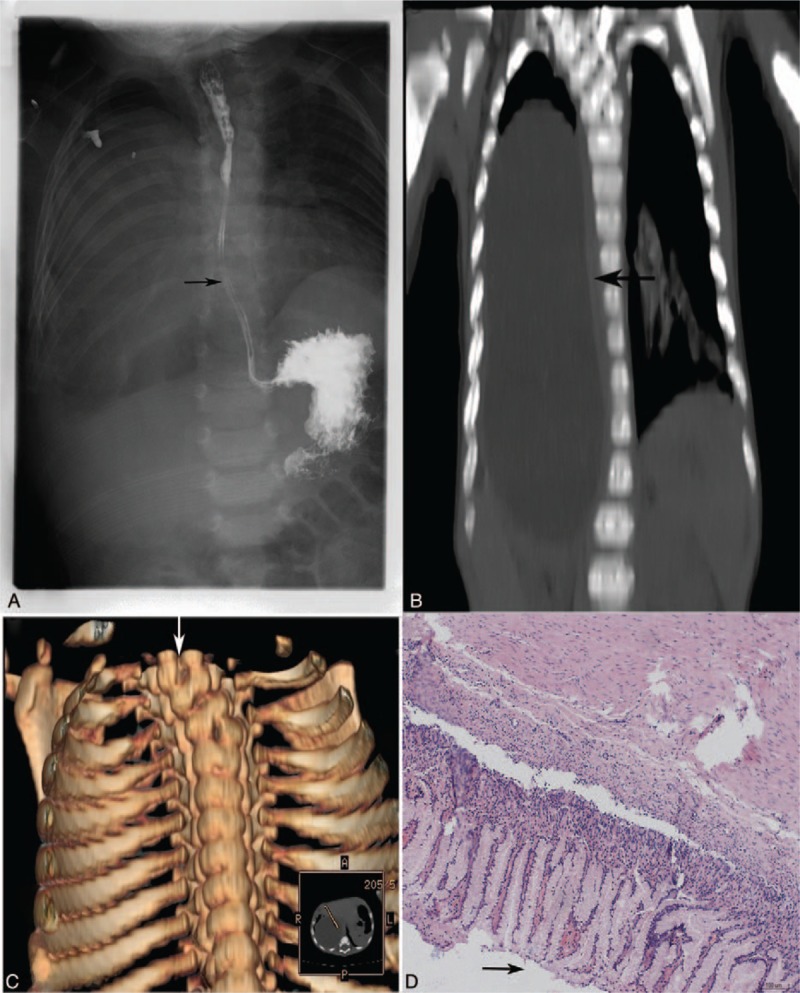
Imaging findings of a case with esophageal duplication cyst with asymptomatic hemivertebrae. In this 6-month-old male infant, barium swallow examination was inconclusive (A). Computed tomography scan showed an esophageal duplication cyst (arrow), whose coronal is depicted. The cyst was 11.9 × 5.4 × 5.1 cm, with an average wall thickness of 0.5 cm, compressing the trachea, right main bronchus, right inferior lobe (anteriorly), and liver (B). Three-dimensional computed tomography reconstruction showed hemivertebrae located in the upper thoracic spine (T4 and T3) (C). Histopathological examination after hematoxylin and eosin staining showed gastrointestinal-type mucosa (magnification, ×40) (D).
Because the cyst was oversized and compressed both the right main bronchus and liver, we performed a diagnostic laparoscopy 7 days upon admission, but this remained inconclusive regarding the exact localization and extent of the cyst. Laparoscopy was converted to open surgery, and the cyst was confirmed to protrude in the abdominal cavity from the thoracic cavity. Then, anterolateral thoracotomy was performed. The cyst was dissected from the adjacent tissues and completely excised. We withdrew about 150 mL of a clear, jelly-like fluid from the cyst. Closed tube drainage was performed for 3 days, and discontinued when chest X-ray showed improvement. The patient was discharged 6 days later when chest X-ray showed improvement of bronchopneumonia, without change in the condition of the spine. The infant recovered uneventfully. Histopathological examination after hematoxylin and eosin staining of the cyst showed gastrointestinal-type mucosa with well-developed muscularis propria and serosa (Fig. 1D).
Since neurological examinations were normal, no treatment for hemivertebrae was undertaken at that time. The infant showed normal growth and development at 6-month follow-up. No X-ray was performed at that time.
Informed consent was obtained from the patient's parents.
3. Discussion
Esophageal duplication cysts are rare, benign mediastinal masses that occur in the 6th week of embryonic life.[5] They can be associated with symptomatic spinal abnormalities, but presentations due to esophageal duplication cyst symptoms are rarely found in the presence of spinal abnormalities. We reported the case of a 6-month-old infant who presented with respiratory tract infection symptoms, which were later demonstrated to be caused by a large esophageal duplication cyst accompanied by asymptomatic hemivertebrae. This case suggests that noninvasive imaging and diagnostic procedures may not be sufficient to identify the exact localization of esophageal duplication cysts. Although hemivertebrae were present, they were asymptomatic and did not require treatment; only the esophageal duplication cyst induced nonspecific symptoms that disappeared after surgery. A previously published case was also incidentally diagnosed with esophageal duplication cyst after being investigated for respiratory tract symptoms, but this case had no spinal deformity.[6]
Esophageal duplication cysts are rare (incidence of 1:8200).[7] They can be associated with spinal abnormalities, but the patients usually present with symptoms of spinal abnormalities and are incidentally diagnosed with esophageal duplication.[1,2,4,8] In the present study, the esophageal duplication cyst was very large, which led to an original misdiagnosis of common bile duct cysts or pancreatic pseudocysts, and laparoscopic surgical exploration was then performed. Fortunately, the finally diagnosed esophageal duplication cyst only required minimal surgery and could be performed during the same operating time.
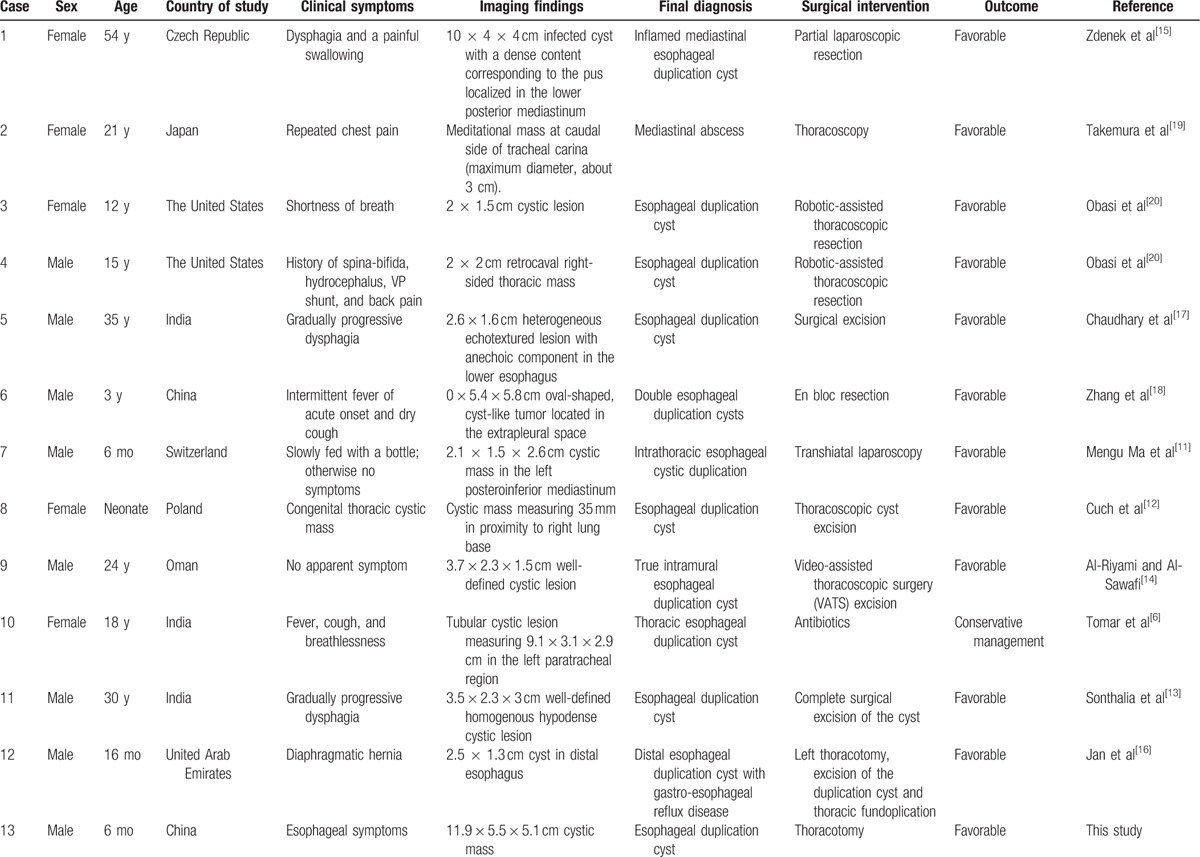
Only 10% of esophageal cysts interact with the lumen of the esophagus.[9] There have been very few cases in which the cyst is connected to the lower half of the esophagus, and large cysts of this type usually compress the lower half of the esophagus.[10] In the present case, barium swallow examination was inconclusive, which led to an incorrect diagnosis. The cyst was completely and successfully resected from the adjacent tissues by open surgery. A previous case was reported to have been operated by laparoscopy,[11] but laparoscopy was inconclusive in the present case. The exact diagnosis could be made only after pathological examination. Such cysts can lead to complications such as hemorrhage, infection, and malignancies, and are found in both genders, virtually all ethnicities, and a wide range of ages, as shown in Table 1.[6,11–20] In the current case, the cyst was very large, and might have gone unnoticed because it was initially asymptomatic until it reached a large volume that obstructed the respiratory airways. In addition, the child might have not been followed up closely after birth by an experienced pediatrician. This stresses the importance of regular postnatal examinations. Complete surgical excision is typically curative because recurrence is rare.[6,21] The present case recovered well.
Table 1.
Demographic data, clinical and image findings, surgical interventions, and outcomes in selected cases with esophageal duplication cysts.
Because the neurological functions were normal and the patient was asymptomatic, no spinal surgery was undertaken. The infant had normal growth and development at 6-month follow-up.
In conclusion, esophageal duplication cysts are relatively rare and may have no specific symptoms. A combination of multiple medical imaging techniques, such as esophagography, CT scan, and barium swallow examination can assist in diagnosing esophageal duplication cysts and defining their relationships with the neighboring anatomy. Curative surgery is not difficult and is needed to provide strong clinical evidence for diagnosis. Complete surgical excision is typically curative because recurrence is rare.
Footnotes
Abbreviations: CT = computed tomography, EDC = esophageal duplication cyst.
YL and LZ have contributed equally to this study.
This study was supported by Public Welfare Industry Research Subject (No. 201402007).
The authors have no conflicts of interest to disclose.
References
- [1].Khan MU, Saidy KM, Ousulimane DM, et al. Posterior mediastinal gastroenteric cyst in neonate. Saudi Med J 2004;25:955–7. [PubMed] [Google Scholar]
- [2].Laurent F, Latrabe V, Lecesne R, et al. Mediastinal masses: diagnostic approach. Eur Radiol 1998;8:1148–59. [DOI] [PubMed] [Google Scholar]
- [3].Arbona JL, Fazzi JG, Mayoral J. Congenital esophageal cysts: case report and review of literature. Am J Gastroenterol 1984;79:177–82. [PubMed] [Google Scholar]
- [4].Sethi GK, Marsden J, Johnson D. Duplication cysts of the esophagus. South Med J 1974;67:616–8. [DOI] [PubMed] [Google Scholar]
- [5].Dai ZJ, Kang HF, Lin S, et al. Esophageal cancer with esophageal duplication cyst. Ann Thorac Surg 2013;96:e15–6. [DOI] [PubMed] [Google Scholar]
- [6].Tomar LR, Mannar V, Pruthi S, et al. Asymptomatic thoracic esophageal duplication cyst in a young adult with bronchiectasis. Lung India 2015;32:404–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Kim YW, Sohn TI, Shim HS, et al. Intra-abdominal esophageal duplication cyst in an adult. Yonsei Med J 2005;46:859–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Kapoor K, Jajoo M, Dublish S, et al. A rare cause of wheezing in an infant: esophageal duplication cyst. Indian J Crit Care Med 2014;18:464–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Nelms CD, White R, Matthews BD, et al. Thoracoabdominal esophageal duplication cyst. J Am Coll Surg 2002;194:674–5. [DOI] [PubMed] [Google Scholar]
- [10].Liu R, Adler DG. Duplication cysts: diagnosis, management, and the role of endoscopic ultrasound. Endosc Ultrasound 2014;3:152–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Mengu Ma T, Vasseur Maurer S, Reinberg O. Transhiatal laparoscopic resection of intrathoracic esophageal duplication in a 6-month-old boy. Ann Thorac Surg 2014;97:e81–3. [DOI] [PubMed] [Google Scholar]
- [12].Cuch B, Nachulewicz P, Wieczorek AP, et al. Esophageal duplication cyst treated thoracoscopically during the neonatal period: clinical case report. Medicine (Baltimore) 2015;94:e2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sonthalia N, Jain SS, Surude RG, et al. Congenital esophageal duplication cyst: a rare cause of dysphagia in an adult. Gastroenterol Res 2016;9:79–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Al-Riyami S, Al-Sawafi Y. True intramural esophageal duplication cyst. Oman Med J 2015;30:469–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Zdenek K, Vladimir P, Marketa H, et al. Partial laparoscopic resection of inflamed mediastinal esophageal duplication cyst. Surg Laparosc Endosc Percutan Tech 2007;17:311–2. [DOI] [PubMed] [Google Scholar]
- [16].Jan IA, Al Nuaimi A, Al Hamoudi B, et al. Distal esophageal duplication cyst with gastro-esophageal reflux disease: a rare association and a management challenge. J Coll Physicians Surg Pak 2016;26:148–50. [PubMed] [Google Scholar]
- [17].Chaudhary V, Rana SS, Sharma V, et al. Esophageal duplication cyst in an adult masquerading as submucosal tumor. Endosc Ultrasound 2013;2:165–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Zhang Z, Jin F, Wu H, et al. Double esophageal duplication cysts, with ectopic gastric mucosa: a case report. J Cardiothorac Surg 2013;8:221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Takemura M, Yoshida K, Morimura K. Thoracoscopic resection of thoracic esophageal duplication cyst containing ectopic pancreatic tissue in adult. J Cardiothorac Surg 2011;6:118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Obasi PC, Hebra A, Varela JC. Excision of esophageal duplication cysts with robotic-assisted thoracoscopic surgery. JSLS 2011;15:244–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Abu-Zaid A, Azzam A. Images in clinical medicine. Esophageal duplication cyst. N Engl J Med 2014;371:e36. [DOI] [PubMed] [Google Scholar]


