Abstract
Rationale:
Cervical nerve root injury is one of the complications of traumatic cervical spine fracture. Although one of the most effective treatments to reduce inflammation in nerve root injuries is the use of corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids and NSAIDs can inhibit bone healing. So, when nerve injury accompanies bone fractures, corticosteroids and NSAIDs have limitations as therapeutic agents. However, polydeoxyribonucleotide (PDRN) may be useful in the treatment of neuropathy or musculoskeletal pain patients with contraindication of the use of corticosteroids because of its anti-inflammatory effect, as revealed in previous studies. To the best of our knowledge, there has been no report of treatment of traumatic nerve root injury due to an articular process fracture with an ultrasound-guided cervical nerve root block (NRB) using PDRN.
Patients concerns:
A 54-year-old female patient with motor weakness of the left upper extremity and tingling sensation in the left neck and shoulder.
Diagnoses:
traumatic C5 nerve root injury due to a fracture of the left articular process in the C4 spine.
Intervention:
Ultrasound-guided C5 NRB using PDRN.
Outcomes:
Her motor weakness and sensory symptoms of the left upper extremity were significantly improved after treatment using an ultrasound-guided C5 NRB using PDRN.
Lessons:
Although it is impossible to draw a conclusion from a single case report, we suggest the ultrasound-guided NRB using PDRN could be a useful treatment for alleviating motor weakness and neuropathic pain caused by traumatic spinal nerve root injury in situations where corticosteroids cannot be used.
Keywords: PDRN, polydeoxyribonucleotide, STIR, traumatic spinal nerve root injury, ultrasound, ultrasound-guided cervical nerve root block
1. Introduction
Cervical nerve root injury is one of the complications of traumatic cervical spine fracture.[1] Although one of the most effective treatments to reduce inflammation in nerve root injury injuries[2] is the use of corticosteroids or nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids and NSAIDs can inhibit bone healing. Therefore, when nerve injury accompanies bone fractures as in this case, corticosteroids and NSAIDs have limitations as therapeutic agents.[3]
Recently, polydeoxyribonucleotide (PDRN) has begun to be used for neuropathic and musculoskeletal pain because of it its anti-inflammatory effects.[4,5] Although PDRN has not been studied for bone healing, it is known to promote wound healing through its collagen synthesis effects and by stimulating angiogenesis, unlike corticosteroids.[6] Moreover, PDRN is also known to have osteoblast-promoting properties,[7] and prevents cartilage loss.[8] Thus, PDRN may be useful in the treatment of neuropathy or musculoskeletal pain for patients who experience side effects of corticosteroids because its potential has been shown as an alternative substitute for corticosteroids in previous studies.[4,5,9] However, so far, there has been no report of treatment of traumatic nerve root injury due to fracture of the articular process in the cervical spine through ultrasound-guided cervical nerve root block (NRB) using PDRN. Therefore, we report a case of cervical root injury whose motor weakness and sensory symptoms were improved after ultrasound-guided cervical NRB using PDRN. This case series was approved by ethics committee of our hospital (Institutional Review Board of Daegu Fatima Hospital).
2. Case report
A 54-year-old female patient arrived in the emergency room complaining of neck and shoulder pain and weakness of the left upper extremity. She had slipped and hit the left side of her head and shoulders against the floor due to a sudden stop when she was standing at the door to get off a bus.
In the initial neurological examination, the patient's motor power of both the upper and lower extremities was normal except for the left shoulder elevation and elbow flexion, which were grade 2 (Medical Research Council grade) in the manual muscle test (MMT).[10] In computed tomography (CT) of the cervical spine, a fracture of the left articular process in the C4 spine was observed, and mild swelling and increased signal in the left C5 spinal nerve root were observed on coronal T2-weighted short tau inversion recovery (STIR) images (Fig. 1). The patient was admitted to the department of neurosurgery, and it was decided she would receive conservative treatment wearing a Philadelphia neck collar without surgery. Three weeks after the accident, she was transferred to the department of rehabilitation medicine for further rehabilitation because there was no significant improvement in the motor weakness.
Figure 1.
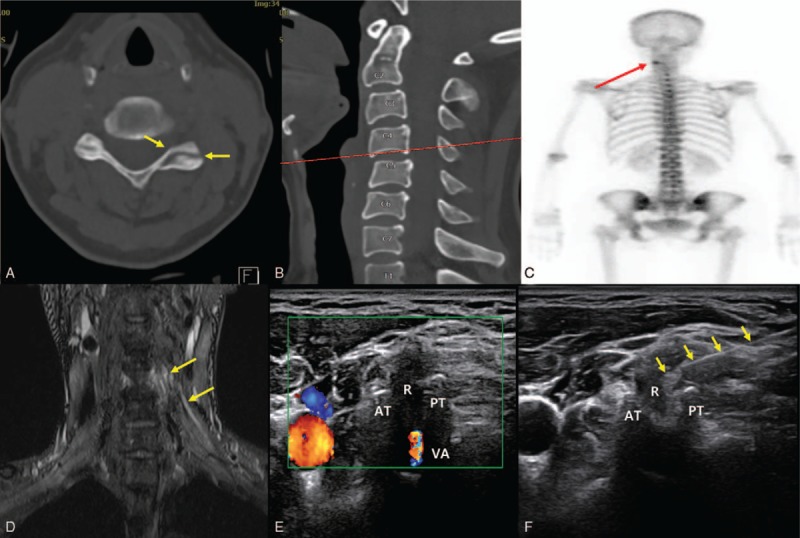
Computed tomography of the cervical spine. A fracture of the left articular process of the C4 spine was shown. (A, B) Increased uptake around the left articular process of the C4 spine was shown in bone scan scintigraphy. (C) Mild swelling and increased signal in the left C5 spinal nerve root was observed on coronal T2-weighted short tau inversion recovery (STIR) images. (D) An ultrasound-guided C5 cervical nerve root block using PDRN was performed. (E) A needle (arrow) was located around the C5 nerve root. AT = anterior tubercle, PT = posterior tubercle, R = C5 nerve root, VA = vertebral artery.
At the time of transfer to the department of rehabilitation, her motor weakness of the left shoulder elevation and elbow flexion were still grade 2 in MMT. She also complained of a tingling sensation in the left neck and shoulder, which she rated 5/10 on a numeric rating scale (NRS), despite taking pregabalin 150 mg. In a neurologic examination, the Hoffman sign and Babinski sign were negative on both sides, and deep tendon reflexes (DTR) of both the upper and lower extremities were all normal except for the left biceps jerk, which showed a decrease to 1+. In the electrophysiological study which was performed 3 weeks after the accident, the compound motor action potential (CMAP) amplitude of the left musculocutaneous, axillary, and the suprascapular nerve was decreased compared with the right side (Table 1). However, all nerve conduction studies (NCS) of all sensory nerves in both the upper extremities were within a normal range, including the left lateral antebrachial cutaneous nerve which is responsible for the dermatome of the C5 nerve. In the needle electromyography, denervation potentials and reduced interference patterns were shown in the left C5 paraspinalis muscle, rhomboid, deltoid, infraspinatus, and biceps brachii muscles (Table 2).
Table 1.
The nerve conduction studies at 3 weeks and 2 months after symptom onset.
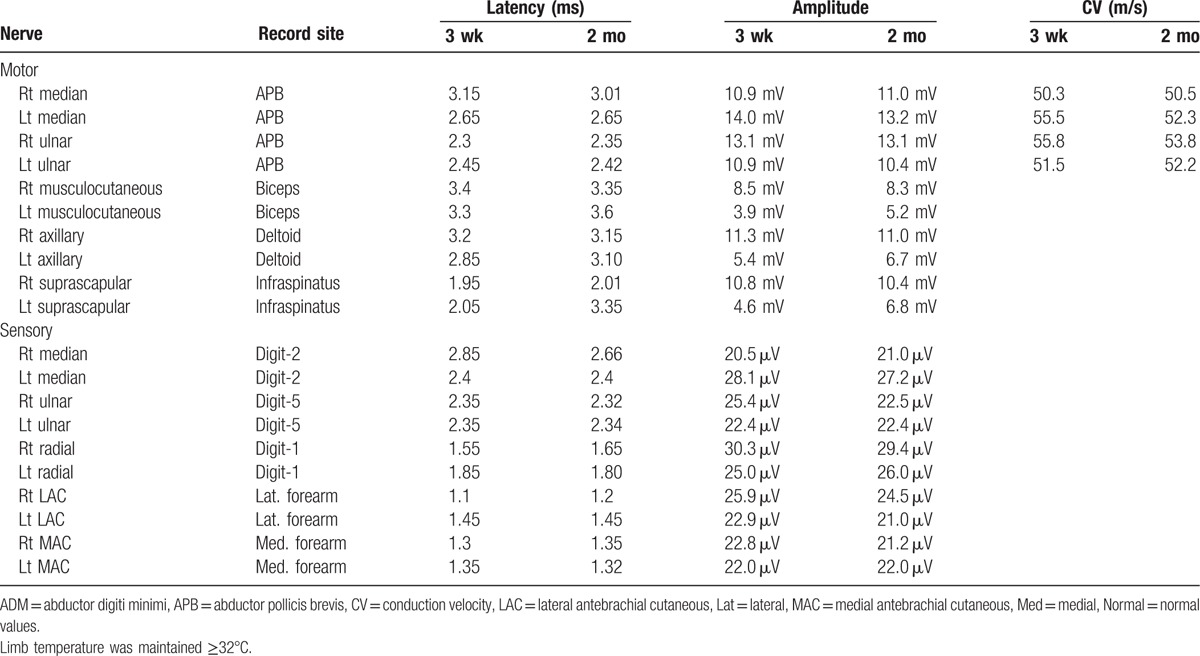
Table 2.
The needle electromyography at 3 weeks and 2 months after symptom onset.
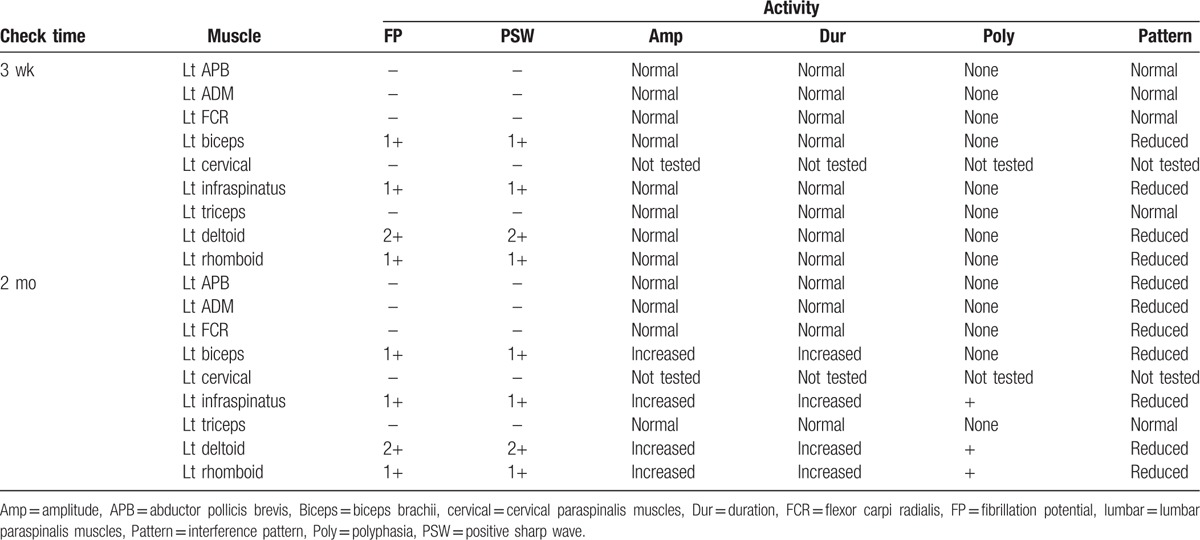
After the explanation about the anti-inflammatory effect of PDRN, the patient provided written informed consent for its use. After obtaining informed consent from the patient, an ultrasound-guided left C5 nerve root block (NRB) using 5.625 mg/3 mL of PDRN (Rejuvenex PDRN, Pharma Research Products, South Korea) was performed[11] (Fig. 1). Although there was no significant improvement in the motor power of the left upper extremity, her neck and left shoulder pain improved from NRS 5 to 2 after the first injection. One week after the first injection, a second ultrasound-guided C5 NRB using PDRN was performed. On the second day following the second injection, the motor power of the left shoulder elevation and elbow flexion improved from grade 2 to 3, and her neck and left shoulder pain also improved to NRS 1. Two weeks after the second injection, the motor weakness of her left shoulder elevation and elbow flexion were improved to grade 4, and her neck and left shoulder pain had nearly disappeared. In the follow-up electrophysiological study which was performed 2 months after the accident, the CMAP amplitude of the left musculocutaneous, axillary, and suprascapular nerve also showed improvement, although there were still denervation potentials in the left rhomboid, deltoid, infraspinatus, and biceps brachii muscles (Table 1).
3. Discussion
PDRN is a mixture of deoxyribonucleotide polymers with chain lengths ranging from 50 to 2000 bp.[12] PDRN is obtained from sperm salmon or trout through an extraction process. PDRN is an adenosine A2A agonist and has been demonstrated to have anti-inflammatory effects in several previous studies.[4,5] In this case, it is considered that the patient with motor weakness and neuropathic pain showed significant improvement after 2 PDRN injections because of the anti-inflammatory effect of PDRN.
Recently, ultrasound-guided CRB has been known to be effective, with a similar effectiveness to fluoroscopy-guided CRB, and has been widely used due to its advantages of minimizing intravascular injuries and radiation exposure.[11,13] In the case of a cervical root injury, therefore, ultrasound-guided CRB will allow safe PDRN injection around the injured cervical nerve root. Although it is impossible to draw a conclusion from a single case report, we suggest the ultrasound-guided CRB using PDRN could be a useful treatment for alleviating motor weakness and neuropathic pain caused by traumatic spinal nerve root injury in situations where corticosteroids cannot be used.
Footnotes
Abbreviations: CMAP = compound motor action potential, CT = computed tomography, DTR = deep tendon reflexes, MMT = manual muscle test, NRB = nerve root block, NRS = numeric rating scale, NSAIDs = nonsteroidal anti-inflammatory drugs, PDRN = polydeoxyribonucleotide, STIR = short tau inversion recovery.
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Science, ICT and Future Planning (NRF-2017R1D1A1B03033127). No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the authors or upon any organization with which the authors are associated.
The authors have no conflicts of interest to disclose.
References
- [1].Ducreux D, Lacour M, Cazejust J, et al. [Traumatic cord and nerve root injuries: imaging features at the acute and chronic phases]. J Radiol 2010;91:1010–21. [DOI] [PubMed] [Google Scholar]
- [2].Al-Bishri A, Forsgren S, Al-Thobaiti Y, et al. Effect of betamethasone on the degree of macrophage recruitment and nerve growth factor receptor p75 immunoreaction during recovery of the sciatic nerve after injury: an experimental study in rats. Br J Oral Maxillofac Surg 2008;46:455–9. [DOI] [PubMed] [Google Scholar]
- [3].Sato S, Kim T, Arai T, et al. Comparison between the effects of dexamethasone and indomethacin on bone wound healing. Jpn J Pharmacol 1986;42:71–8. [DOI] [PubMed] [Google Scholar]
- [4].Yoon YC, Lee DH, Lee MY, et al. Polydeoxyribonucleotide injection in the treatment of chronic supraspinatus tendinopathy: a case-controlled, retrospective, comparative study with 6-month follow-up. Arch Phys Med Rehabil 2017;98:874–80. [DOI] [PubMed] [Google Scholar]
- [5].Lim TH, Cho HR, Kang KN, et al. The effect of polydeoxyribonucleotide prolotherapy on posterior tibial tendon dysfunction after ankle syndesmotic surgery: a case report. Medicine 2016;95:e5346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Jeong W, Yang CE, Roh TS, et al. Scar prevention and enhanced wound healing induced by polydeoxyribonucleotide in a rat incisional wound-healing model. Int J Mol Sci 2017;18:1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Guizzardi S, Galli C, Govoni P, et al. Polydeoxyribonucleotide (pdrn) promotes human osteoblast proliferation: a new proposal for bone tissue repair. Life Sci 2003;73:1973–83. [DOI] [PubMed] [Google Scholar]
- [8].Bitto A, Polito F, Irrera N, et al. Polydeoxyribonucleotide reduces cytokine production and the severity of collagen-induced arthritis by stimulation of adenosine a((2)a) receptor. Arthritis Rheum 2011;63:3364–71. [DOI] [PubMed] [Google Scholar]
- [9].Kang KN, Kim TW, Koh JW, et al. Effect of transforaminal epidural polydeoxyribonucleotide injections on lumbosacral radiculopathy: a case report. Medicine 2017;96:e7174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Park D, Seong MY, Kim HY, et al. Spinal cord injury during ultrasound-guided c7 cervical medial branch block. Am J Phys Med Rehabil 2017;96:e111–4. [DOI] [PubMed] [Google Scholar]
- [11].Park D. Precise target site of ultrasound-guided c5 cervical root block. Am J Phys Med Rehabil 2017;96:e198–9. [DOI] [PubMed] [Google Scholar]
- [12].Altavilla D, Bitto A, Polito F, et al. Polydeoxyribonucleotide (PDRN): a safe approach to induce therapeutic angiogenesis in peripheral artery occlusive disease and in diabetic foot ulcers. Cardiovasc Hematol Agents Med Chem 2009;7:313–21. [DOI] [PubMed] [Google Scholar]
- [13].Park D. Ultrasound-guided s1 transforaminal epidural injection using the in-plane approach and color doppler imaging. Am J Phys Med Rehabil 2017;[Epub ahead of print]. [DOI] [PubMed] [Google Scholar]


