Supplemental Digital Content is available in the text
Keywords: cervical intervertebral disc displacement, cervicalgia, Korean health insurance review and assessment service national patient sample data, medical status, sprain/strain of cervical spine, usual care
Abstract
Neck pain is a highly common condition and is the 4th major cause of years lived with disability. Previous literature has focused on the effect of specific treatments, and observations of actual practice are lacking to date. This study examined Korean health insurance review and assessment service (HIRA) claims data to the aim of assessing prevalence and comparing current medical practice and costs of cervical disorders in Korea.
Current practice trends were determined through assessment of prevalence, total expenses, per-patient expense, average days in care, average days of visits, sociodemographic characteristics, distribution of medical costs, and frequency of treatment types of high frequency cervical disorders (cervical sprain/strain, cervical intervertebral disc displacement [IDD], and cervicalgia).
Although the number of cervical IDD patients was few, total expenses, per-patient expense, average days in care, and average days of visits were highest. The proportion of women was higher than men in all 3 groups with highest prevalence in the ≥50s middle-aged population for IDD compared to sprain/strain. Primary care settings were commonly used for ambulatory care, of which approximately 70% chose orthopedic specialist treatment. In analysis of medical expenditure distribution, costs of visit (consultation) (22%–34%) and physical therapy (14%–16%) were in the top 3 for all 3 disorders. Although heat and electrical therapies were the most frequently used physical therapies, traction use was high in the cervical IDD group. In nonnarcotics, aceclofenac and diclofenac were the most commonly used NSAIDs, and pethidine was their counterpart in narcotics.
This study investigated practice trends and cost distribution of treatment regimens for major cervical disorders, providing current usage patterns to healthcare policy decision makers, and the detailed treatment reports are expected to be of use to clinicians and researchers in understanding current usual care.
1. Introduction
Neck pain is a highly common musculoskeletal disorder which is known to incur frequent work leaves, and heavy economic burden and disability,[1] and it is becoming increasingly prevalent worldwide. It is a condition of considerable significance at individual, household, and community levels,[2] and according to the 2010 Global Burden of Disease report, neck pain is the 4th major cause of years lived with disability following low back pain, major depressive disorder, and other musculoskeletal disorders.[3] Various epidemiological studies on neck pain have reported ranges of annual prevalence from 15% to 50%,[4–7] and a 2006 systematic review put average prevalence estimates at 37.2%.[4]
Neck pain may be classified to be of mechanical, neuropathic, or other origin (eg, of cardiac or vascular pathology). Mechanical pain generally indicates pain originating from spinal, ligamentous, or muscular structures, and examples include facet joint, discogenic, and fascial pain. Meanwhile, neuropathic pain refers to pain caused by trauma or diseases involving the peripheral nervous system, and radicular symptoms from intervertebral disc displacement (IDD) and spinal stenosis are some familiar examples.[8] Cervical sprain/strain/tension mainly relates to acute pain from soft tissue injury including muscles, tendons and ligaments, bringing about neck stiffness, fatigue, and range of motion restriction.[8] Cervical disc disorder with radiculopathy is one of the most common causes of neck and arm pain,[1,4,9] of which the main symptoms are upper extremity pain manifesting at various sites according to the level of IDD or nerve root compression.[10,11] Epidemiological data reports from Mayo Clinic put annual cervical radiculopathy incidence at 83 individuals per 100,000 in the general population.[12]
Although medical expenditure for such major cervical disorders as cervical sprain/strain/tension, cervical disc disorders with radiculopathy, and cervicalgia is steadily increasing along with escalating social and economic costs and burden, previous studies have tended to focus on outcome assessment of specific treatments or basic epidemiology research, overlooking real-world practice points such as medical expenditure difference by cervical disorder or treatments frequented in clinical practice.
Cervical disorders are a major cause of both personal suffering and collective social burden due to their high prevalence, and though highly prevalent cervical disorders such as cervical sprain/strain, cervical disc disorders with radiculopathy, and cervicalgia share common features, medical service use, primary treatment modalities, and medical costs may differ greatly. Therefore, in-depth comparison and analysis of disease attributes and their management should enable a more comprehensive understanding.
The healthcare system in Korea is implemented under the National Health Insurance program, which is compulsory by law and covers 47 million out of the South Korean population of 51 million as a universal social insurance program. This system is operated by a single insurer, the National Health Insurance Service, under the supervision of the Korean government, and all national health insurance claims data are required to be filed to the health insurance review and assessment service (HIRA) for reimbursement.[13] The aim of this study is to provide an informative report on cervical disorders to relevant specialists such as clinicians, researchers, and healthcare policy makers by assessing prevalence and characteristics, and current medical service usage including costs of interventions and surgery, hospitalization, physical therapy, and medication of high frequency cervical disorders (cervical sprain/strain, cervical disc disorders with radiculopathy, and cervicalgia) from HIRA claims data.
2. Methods
2.1. Data and subjects
The data used in this study is from the 2014 HIRA National Patient Sample (NPS) dataset, which is made available to researchers for research means by HIRA on an annual basis. National health insurance claims data are created when medical institutions file claims statements to HIRA in order to be reimbursed for the insurance benefit amount covered by the National Health Insurance Service after providing medical services to patients. The NPS dataset includes treatment and prescription details (ie, interventions, examinations, and medication), information on the provider (medical institution), and sociodemographic features of participants (eg, age, sex) from claims statements filed for the corresponding year as of the medical care commencement date, and is statistically sampled as secondary data from raw data removed of identifying individual and corporate information. Sex and age stratified (5 year intervals) systematic data sampling is conducted in 3% of total patients with any medical service use records for the past year for wider data accessibility and convenience due to the extensive total data amount, and equals approximately 1.4 million patients.[14] Multiple visits of individual patients within the dataset for the corresponding year are easily identified as each randomly extracted patient is coded with a randomly generated individual identifier, and all statistical analyses in this study were performed by patient count as opposed to number of visits/hospitalizations or treatment sessions to better illustrate individual medical service use and prescription history.
2.2. Cervical sprain/strain, cervical intervertebral disc displacement, and cervicalgia
The 6th revision of Korean standard classification of diseases (KCD) codes relating to cervical disorders were designated through literature review and researcher discussion as follows: S134 was included for the cervical sprain/strain group, M501 + M4722 + M4723 for the cervical disc disorder with radiculopathy group, and M542 + M502 + M503 + M508 + M509 for cervicalgia to define the 3 highest frequency cervical disorder groups. Only patients with both cervical disorder codes and relevant simple radiology records were included as a measure to ensure accurate coding identification (Fig. 1).
Figure 1.
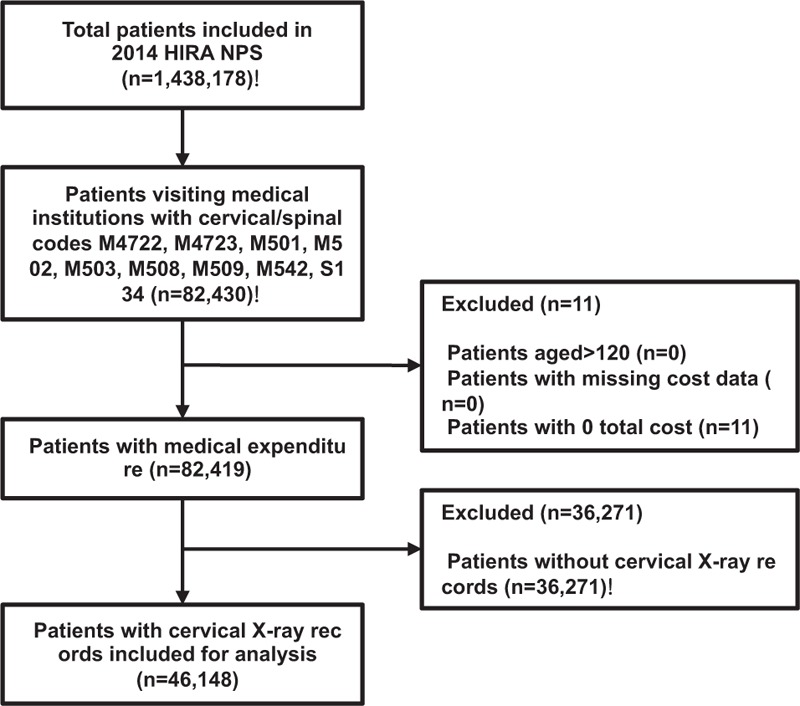
Flowchart of study inclusion and exclusion of cervical disorder patients. M4722, other spondylosis with radiculopathy, cervical region; M4723, other spondylosis with radiculopathy, cervicothoracic region; M501, cervical disc disorder with radiculopathy; M502, other cervical disc displacement; M503, other cervical disc degeneration; M508, other cervical disc disorders; M509, cervical disc disorder, unspecified; M542, cervicalgia; S134, sprain and strain of cervical spine. HIRA = health insurance review and assessment service, NPS = national patient sample.
2.3. Analysis
Sociodemographic characteristics by cervical disorder code were assessed by age, sex, public insurance scheme, medical institution type, and medical specialty. Age was classified into <20 years, 10 year intervals for ≥20 years, sex into men and women, public insurance scheme into National Health Insurance Service and Medicaid, and medical institution into 7 types: clinic, hospital, general hospital, tertiary hospital, long-term care hospital, public health center, and Korean medicine hospital. In accordance with medical law by order of the Korean Ministry of Health and Welfare, hospitals hold ≥30 beds for inpatient care, and general hospitals ≥300 beds, with at least 3 outpatient departments of internal medicine, surgery, pediatrics, and obstetrics and gynecology, and respective specialists in full-time employment. Tertiary hospitals specialize in advanced medical care for serious medical conditions with ≥20 departments as designated by the Ministry of Health and Welfare, and respective full-time specialists.[15] Medical specialty was listed in order of medical department frequency.
Total expenses were analyzed based on costs of visit (consultation), admission, medication, injections, anesthesia, physical therapy, psychotherapy, procedure/surgery, examination, and diagnostic and therapeutic radiology clause codes out of insured treatments as classified in the Korean Ministry of Health and Welfare notification. Medical expenditure is the costs accrued from treatment of national health insurance patients at medical institutions, and is shared by the National Health Insurance Service and patient through insurance benefit and patient copayment. HIRA decides the final benefit amount out of the claims filed by medical institutions.
Numbers of surgery, injection, physical therapy, and analgesics recipients were tallied based on the number of subjects with code records. As surgery codes are not prescribed singularly but together with procedure codes, procedure-related codes were excluded from procedure/surgery counts. Surgeries not limited to the cervical spine that may potentially include surgery pertaining to other regions were also excluded (eg, ostectomy and closed reduction of dislocation [radial head subluxation]). The 10 highest frequency injection intervention codes pertaining to the cervical spine and 9 highest frequency physical therapies were analyzed in order of decreasing frequency.
Analgesics were assessed by main component code used in cervical disorder in- and outpatients as converted into the 5-level anatomical therapeutic chemical (ATC) classification system codes. Analgesics categorization into nonnarcotics and narcotics followed the analgesics coding proposed in a previous Korea National Evidence-based Healthcare Collaborating Agency study.[14] ATC codes are employed for the systematic classification of pharmaceuticals and are managed by the WHO Collaborating Centre for Drug Statistics Methodology which is a WHO-affiliated organization, since its initial publishing in 1976.[16] ATC codes are structured into 5 levels, with the 1st level indicating anatomical main group, 2nd level therapeutic subgroup, 3rd level pharmacological subgroup, 4th chemical subgroup, and 5th level chemical substances, respectively.[17] Although ATC 5th level chemical substance classifications are generally the same as their chemical names, there are a few exceptions (eg, acetaminophen and paracetamol), and in these cases the study followed 5th level ATC code chemical substance names which are listed in Table S1 (see Table S1, Supplemental Digital Content 1 which illustrates the total analgesics use of sprain/strain of cervical spine, cervical IDD, and cervicalgia by 5th level ATC Classification System codes). However, unfortunately not all drugs are granted 5th level ATC codes, and 4 analgesics included in this study had ATC codes corresponding only to the 4th level. As not all analgesics could follow 5th level ATC codes, the 4 analgesics with no corresponding 5th level codes are presented using their chemical names (6 in Table S1) as exceptions. Regardless of dose, subjects with any drug prescription code were counted and included as drug treatment recipients.
2.4. Statistical analysis
Frequency and percentages (%) for sociodemographic characteristics and treatments (ie, surgery, injections, physical therapy, and prescribed analgesics substances) are presented for the patients included in the 3 groups (cervical sprain/strain, cervical IDD, and cervicalgia) through frequency analysis. In calculating percentages in number of patients for each respective category, the denominator was total number of patients for each disorder group, while categorical expense percentages were calculated by dividing by total expense. Total expense, average per-patient expense, and categorical expense were likewise determined for each disorder group. Analyses were conducted using Statistical package SAS version 9.3 (SAS Institute Inc., Cary, NC).
2.5. Ethics statement
The protocol was approved by the Institutional Review Board of Jaseng Hospital of Korean Medicine in Seoul, Korea (JASENG 2016-12-013). The study has been conducted according to the principles expressed in the Declaration of Helsinki. In the process of database construction, all personal information had been masked by HIRA.
3. Results
3.1. Total medical service use and expenditure in cervical sprain/strain, cervical intervertebral disc displacement, and cervicalgia patients
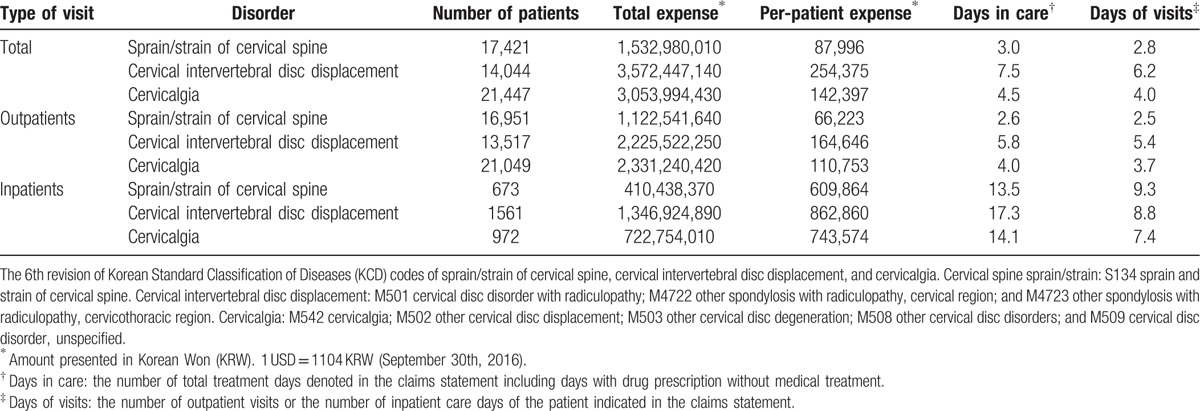
General medical service use in cervical sprain/strain, IDD, and cervicalgia patients is presented in Table 1. Cervical disc disorder with radiculopathy inpatients showed greater number of patients, total expense, per-patient expense, and more days in care compared to cervical sprain/strain or cervicalgia inpatients. Although the number of patients was smallest in cervical disc disorders with radiculopathy out of total patients (inpatients and outpatients), total expense, per-patient expense, average days in care, and average days of visits were highest. In outpatients, cervicalgia patients displayed highest number of patients and total expense, while per-patient expense, average days in care, and average days of visits were similarly highest in cervical disc disorders with radiculopathy. Although total expense was higher in outpatients than inpatients, per-patient expense was higher in inpatients than outpatients by 9, 5, and 10 times for cervical sprain/strain, cervical IDD, and cervicalgia groups, respectively.
Table 1.
Medical service usage for sprain/strain of cervical spine, cervical intervertebral disc displacement, and cervicalgia.
3.2. Patient characteristics by cervical diagnosis code
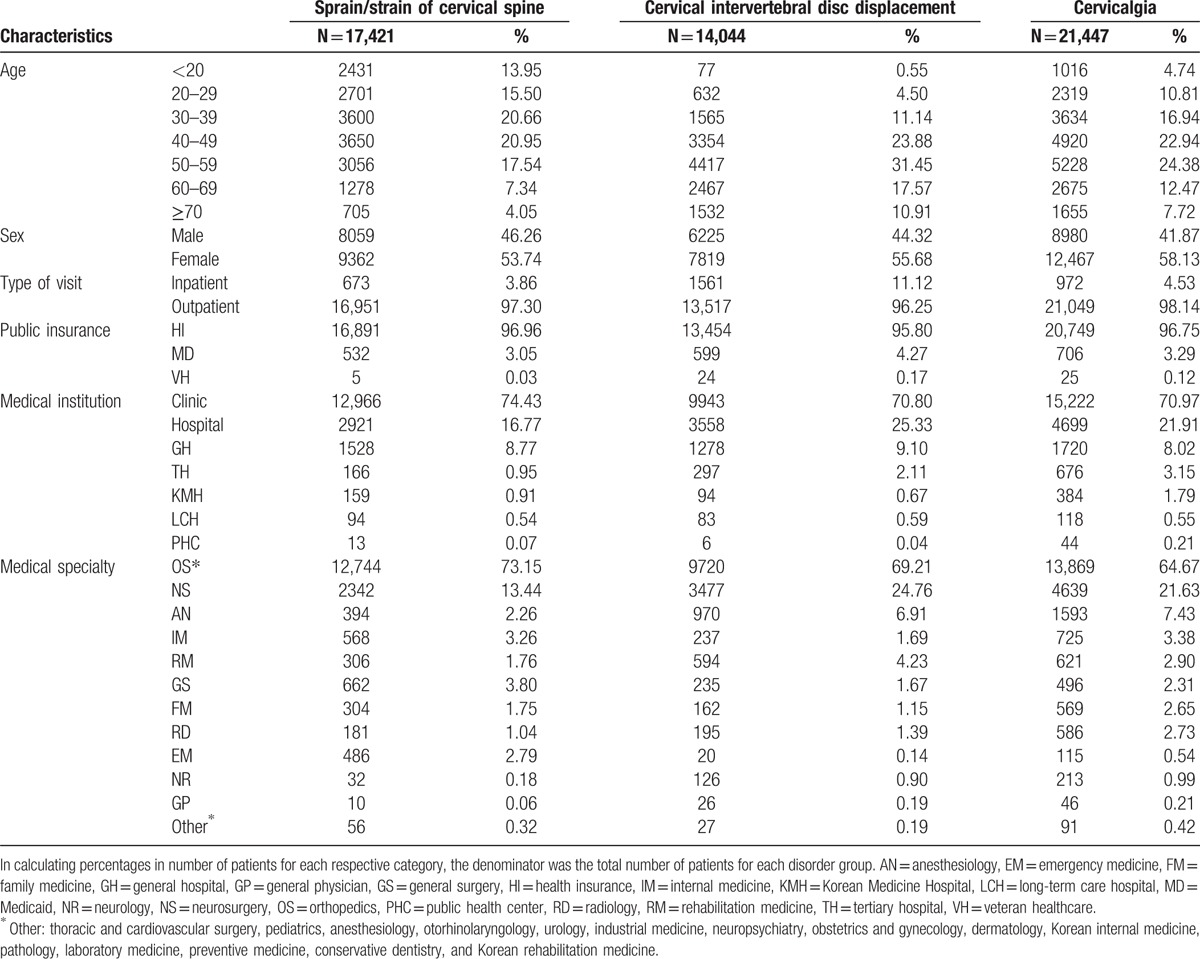
Although the percentage of cervical disc disorder with radiculopathy patients was high in patients aged 50 years or older, that for cervical sprain/strain patients was highest in ages 40 or younger. All 3 diseases showed higher proportions of women than men. Approximately 3% of the cervical sprain/strain group, 11% of the cervical IDD group, and 4% of the cervicalgia group received inpatient care, indicating that the majority of patients were outpatients. However, results demonstrate marked difference between groups with cervical disc disorder with radiculopathy patients undergoing inpatient care about 3 times more than cervical sprain/strain or cervicalgia patients. Regarding medical institutions, approximately 70% received medical attention at clinics, with the highest percentage visiting the orthopedic department, followed by neurosurgery in all 3 disorders, the sum of which equaled 80% to 90% of total patients. Although the 3rd most visited medical specialty was anesthesiology for cervical disc disorders with radiculopathy and cervicalgia, it was general surgery in the cervical sprain/strain group (Table 2).
Table 2.
Patient characteristics of sprain/strain of cervical spine, cervical intervertebral disc displacement, and cervicalgia.
3.3. Medical expense distribution for cervical sprain/strain, cervical intervertebral disc displacement, and cervicalgia
Treatment expense per group was analyzed according to the following 10 subgroups: costs of visit (consultation), admission, medication, injection, anesthesia, physical therapy, psychotherapy, procedure/surgery, examination, and diagnostic and therapeutic radiology (Table 3).
Table 3.
Cost distribution of sprain/strain of cervical spine, cervical intervertebral disc displacement, and cervicalgia.
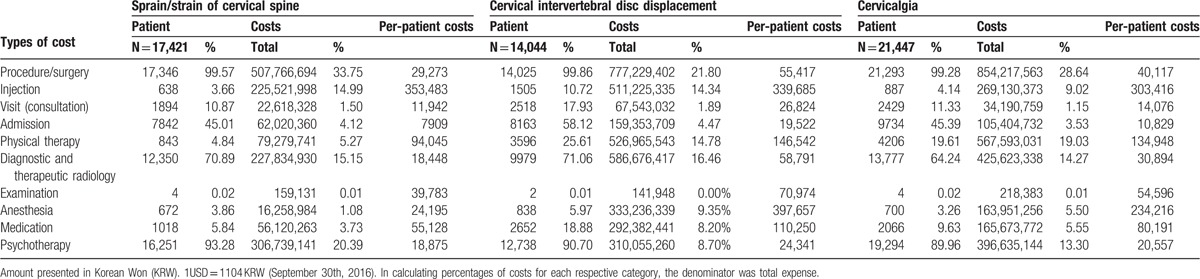
In analysis of total expense, costs of visit (consultation) (33.75%), diagnostic and therapeutic radiology (20.39%), physical therapy (15.15%), and admission (14.99%) took up highest percentages in decreasing order in cervical sprain/strain, while costs of visit (consultation) (21.80%), physical therapy (16.46%), anesthesia (14.78%), and admission (14.34%) in cervical disc disorders with radiculopathy, and costs of visit (consultation) (28.64%), anesthesia (19.03%), physical therapy (14.27%), and diagnostic and therapeutic radiology (13.30%) were highest in cervicalgia. Over 99% of all 3 patient groups paid for costs of visit (consultation), which constituted the largest proportion in total expenses. Although the proportion of diagnostic and therapeutic radiology was low, taking 6th place out of the 10 subcategories in total expenses for cervical disc disorders with radiculopathy following physical therapy, anesthesia, and admission, diagnostic and therapeutic radiology took 2nd place after costs of visit (consultation) in cervical sprain/strain. Also, although anesthesia took 2nd and 3rd place in total expense at approximately 20% and 15% in cervicalgia and cervical disc disorder with radiculopathy, respectively, the percentage for anesthesia out of total expense was very low at 5% in cervical sprain/strain. Physical therapy was 2nd in costs for cervical disc disorder with radiculopathy, and 3rd in cervical sprain/strain and cervicalgia, each accounting for a similar percentage of 15% of total expenses in all groups. Meanwhile, medication took 8th place in the cervical sprain/strain group, and 9th in the IDD and cervicalgia groups comprising about 1% of total expenses.
In analysis of per-patient expense, costs for admission were highest in the cervical sprain/strain group, followed by anesthesia and examination. The counterpart for the cervical disc disorder with radiculopathy group was procedure/surgery, followed by admission and anesthesia, and for the cervicalgia group was admission, followed by procedure/surgery and anesthesia.
3.4. Usual care excluding analgesics
Table 4 lists usual care in surgery, injections, and physical therapy. The 2 main surgery codes of highest frequency were arthrodesis of the cervical spine using an anterior technique, and open discectomy (including laminectomy) in cervical IDD and cervicalgia.
Table 4.
Usual care of sprain/strain of cervical spine, cervical intervertebral disc displacement, and cervicalgia.
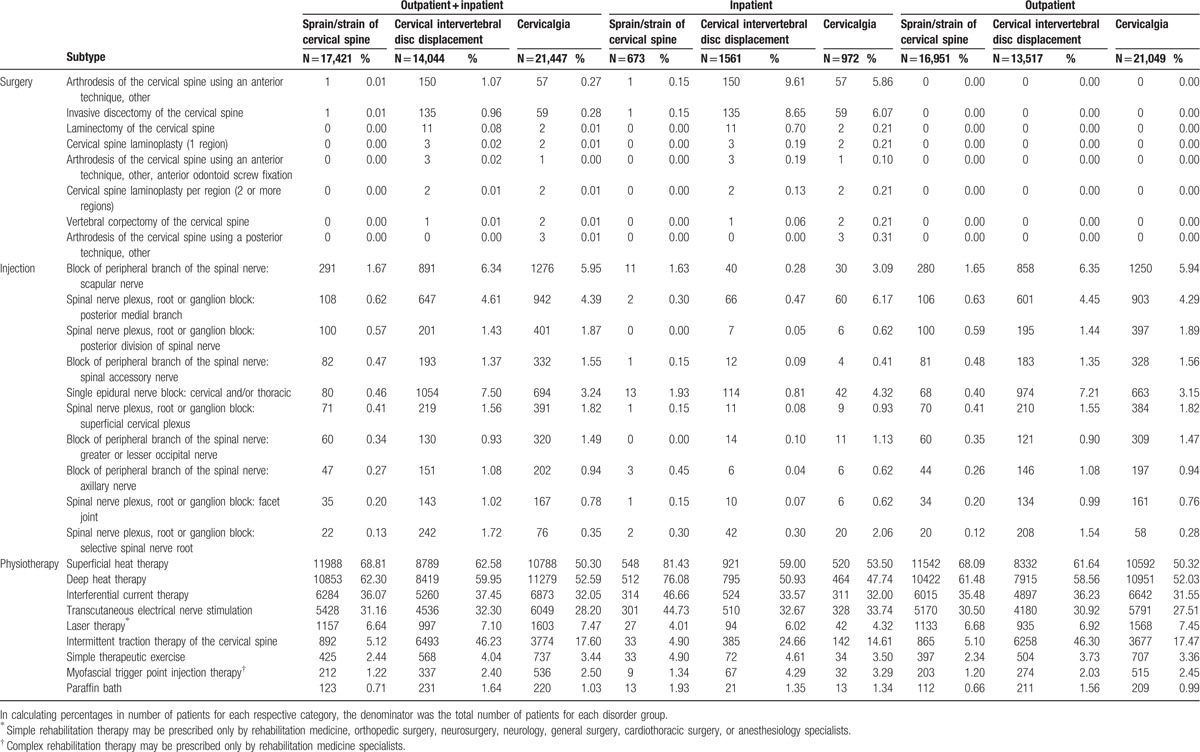
The most frequently prescribed intervention code in injections for the cervical sprain/strain and cervicalgia total patient and outpatient groups was block of scapular nerve branch of the spinal nerve, and for the cervical IDD total patient, inpatient, and outpatient groups was epidural nerve block (single block, cervical, and/or thoracic).
Out of physical therapies, superficial heat therapy, deep heat therapy, interferential current therapy, and transcutaneous electrical nerve stimulation could be considered to constitute usual care with at least 1 out of 4 cervical disorder patients receiving 1 or more of these treatments. Superficial heat therapy was most frequently prescribed in the cervical sprain/strain and cervical IDD total patient, inpatient, and outpatient groups, and it is worth note that intermittent traction therapy was administered in approximately 46% of cervical intervertebral disc displacement total patient and outpatient groups, following superficial heat therapy and deep heat therapy, which is different from cervical sprain/strain and cervicalgia patient group patterns, and approximately 25% of inpatients also, which is about 6 times higher than traction use of cervical sprain/strain and 1.8 times higher than that of cervicalgia. The use of laser therapy, simple therapeutic exercise, myofascial trigger point injection therapy, and paraffin bath were low in all 3 groups at ≤7%.
3.5. Analgesics use out of usual care
In analgesics including nonnarcotics and narcotics used for cervical disorders, the ATC 5th level classification codes for the top 12 nonnarcotic (with total 1000+ prescription cases in the 3 disorder groups), and top 3 narcotic chemical substances (with total 100+ prescription cases in the 3 disorder groups) out of total 41 nonnarcotics and 9 narcotics are listed in Table 5. The nonnarcotic used most frequently in the 3 disorders was aceclofenac, which showed consistent use of 20% to 30% in the in- and outpatient groups of all 3 disorders. Diclofenac and tramadol were also chemical substances of common use in the 3 groups, and while outpatient prescription rates were low, that for inpatients were highest. Contrastingly, chlorphenesin carbamate and dexibuprofen showed low inpatient prescription rates, and high outpatient rates. In total patients, aceclofenac, tramadol, and meloxicam displayed higher usage in the cervical disc disorder with radiculopathy patient groups compared to the other 2 groups, and diclofenac, loxoprofen sodium hydrate, and talniflumate exhibited higher usage in the cervical sprain/strain group than the other groups. Pethidine was the most frequently prescribed narcotic and showed a distinctively higher prescription rate in inpatients compared to total patients, with especially high rates in the cervical disc disorder with radiculopathy inpatient group (8.14%).
Table 5.
Multifrequency analgesics use in sprain/strain of cervical spine, cervical intervertebral disc displacement, and cervicalgia (according to 5th level anatomical therapeutic chemical [ATC] classification system codes).
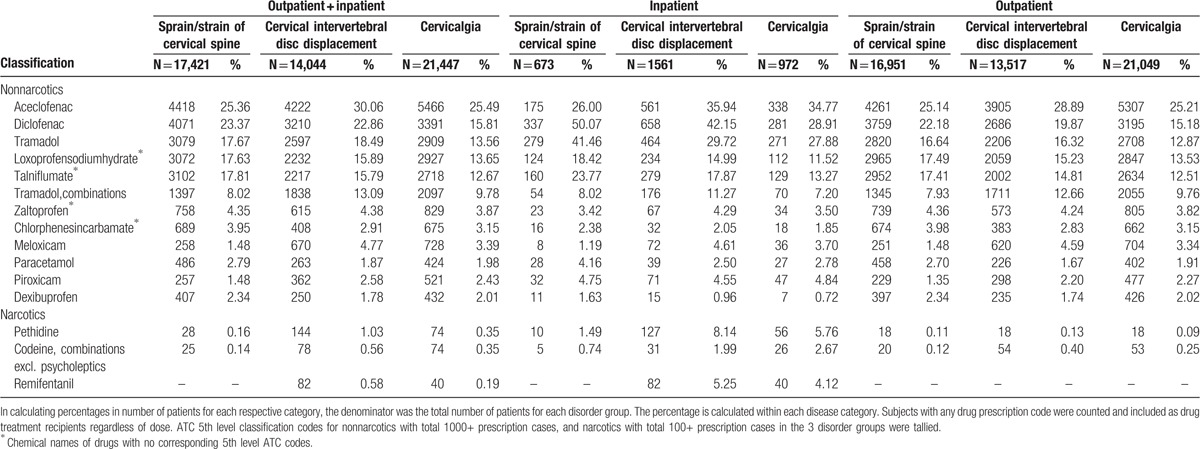
Table 5 identifies only highest frequency chemical substances, and the complete list of chemical substances used in cervical disorders can be verified in Table S1. ATC 5th level codes may be grouped into 4th level classifications, which showed that the 4 classifications of acetic acid derivatives and related substances, other opioids, propionic acid derivatives, other antiinflammatory and antirheumatic agents, and nonsteroids were most commonly used out of nonnarcotics, and the 2 categories of phenylpiperidine derivatives and natural opium alkaloids were most common in narcotics (see Table S2, Supplemental Digital Content 2 which illustrates the total analgesics use of sprain/strain of cervical spine, cervical IDD, and cervicalgia by 4th level ATC Classification System codes).
4. Discussion
This study showed that total expense, per-patient expense, average days in care, and average days of visits were higher in the cervical disc disorder with radiculopathy group compared to the other 2 disorder groups. These findings suggest that the treatment concentration and economic costs are higher in the cervical disc disorder with radiculopathy patient group than the cervical sprain/strain or cervicalgia patient groups. All the 3 groups of cervical sprain/strain, cervical IDD, and cervicalgia exhibited far larger per-patient expense, average days in care, and average days of visits in inpatients than outpatients. These differences may be reflective of greater severity in inpatients compared to outpatients, or of surgical practice. Table 4 depicts how all surgical treatments were performed in inpatients and indicates that surgery incurs considerable social and economic costs.
Cervical sprain/strain, cervical disc disorder with radiculopathy, and cervicalgia group prevalence were all higher in women than men, which are in line with previous studies.[4–7] The reason for this gender difference is probably multifactorial involving such factors as gender-based occupation, working hours, form of labor/work, and housework, in addition to the fact that women are generally of smaller build than men and have less muscular structure in the neck. Similarly, the reason why prevalence of cervical disc disorder with radiculopathy is highest in 50 seconds patients may be interpreted as due to the progression of degenerative change beginning from mid-30s.
Although most patients were outpatients and ≥70% visited clinics as clinics have highest accessibility as primary care institutions, and nearly 70% of total cervical spine patient treatment was conducted at orthopedic surgery departments as opposed to general practice. It can be conjectured that many physicians in Korea undergo specialty training and practice as primary caregivers.
In treatment expenses, costs of visit (consultation) constituted 33.75%, 21.80%, and 28.64% out of total expenses in the cervical sprain/strain, cervical disc disorder with radiculopathy, and cervicalgia groups, respectively. The number of patients charged with costs of visit (consultation) in all 3 groups exceeded 99%, which probably explains the largest incurrence out of total expenses. Considering that physical therapy and anesthesia take 2nd or 3rd place in the cervical disc disorder with radiculopathy and cervicalgia patient groups, it can be inferred that cost of anesthesia for surgery, nerve blocks for pain alleviation, and rehabilitation and physical therapy is high. Meanwhile, both the number of patients and total expense for anesthesia in the cervical sprain/strain patient group was considerably lower at 4% to 5%. This may be because the relative severity of disease is lighter than the other 2 groups.
Surgical interventions are usually considered for cervical disc disorder with radiculopathy when conservative methods fail, and of anterior and posterior discectomy techniques, anterior discectomy is performed frequently.[18] Arthrodesis of the cervical spine using anterior techniques has been shown to be effective for cervical radiculopathy and myelopathy, and degenerative cervical disorders such as disc disorders, and is common practice in neurosurgery and orthopedic departments.[19,20] However, various clinical studies have reported joint hypermobility and degenerative change, and increased intradiscal pressure at adjacent segments following arthrodesis.[20–23] The outcomes of this study also demonstrate how arthrodesis using anterior techniques and open discectomy (including laminectomy) is used at high percentages in the cervical disc disorder with radiculopathy patient group, and the benefits and harms should be given due consideration when establishing surgical treatment plans. Moreover, surgical costs are high, and while admission costs were highest in per-patient expense for cervical sprain/strain and cervicalgia patient groups, those for procedure/surgery were highest in the cervical disc disorder with radiculopathy patient group. In order to effectively cut down on socioeconomic costs exemplified by total expense and per-patient expenses in cervical disorder patients, further research on appropriate treatment and costs for high-expenditure items such as procedure/surgery and admission are required. Moreover, patients of higher severity tend to receive more surgery, injections, and inpatient care, and therefore national awareness campaigns and educational programs through the combined efforts of relevant healthcare providers and authorities towards prevention of development and further progression of cervical disorders are necessitated.
Heat therapy and electric therapy were utilized at high percentages in this study, and these results suggest that these modalities may be considered to be basic physical therapies to be used for cervical sprain/strain, cervical IDD, and cervicalgia patients. Heat therapy is known to be effective for relieving various musculoskeletal pains by promoting resolution of inflammation through increased metabolic activity and blood circulation, and by alleviating muscle spasms and rigidity by raising local body temperature.[24] Electric therapy encompasses such modalities as interferential current therapy (ICT) and transcutaneous electrical nerve stimulation (TENS), and the reported effects of ICT include increased pressure pain threshold (PPT)[25] and decreased pain sensitivity in myalgia patients[26] along with reduced swelling, and various applications to tissue and bone regeneration.[27,28] Meanwhile, studies on high-frequency TENS at 100 Hz have resulted in improved muscle power, fatigue, and balancing ability[29] by means of increased gamma aminobutyric acid (GABA), an inhibitory neurotransmitter, and release in the spinal cord.[30]
A point worth note is that intermittent traction therapy of the cervical spine was performed in approximately 46% of cervical disc disorder with radiculopathy total patient and outpatient groups, and 25% in the inpatient group, which was noticeably higher than the cervical sprain/strain and cervicalgia patient groups. These results demonstrate that the cervical disc disorders with radiculopathy group patients show disease-specific tendencies and receive intermittent traction therapy more than cervical sprain/strain or cervicalgia patients, which are more pronounced in outpatients than inpatients. Laser therapy and therapeutic exercise are classified as simple rehabilitation treatment methods, and myofascial trigger point injection therapy as complex rehabilitation therapy. All other physical therapy items belong in the basic physiotherapy category. Altough there are no particular restrictions in administering basic physiotherapy, simple and complex rehabilitation therapy prescription authorization is limited to relevant medical specialists, and these licensing limitations may be partly accountable for in the relatively low prescription rate.
Aceclofenac and diclofenac were shown to be the nonnarcotic analgesics most frequently prescribed for cervical disorders in Korea out of ATC 5th level classifications. Diclofenac is an NSAID that is widely used for chronic inflammatory diseases such as arthritis. Aceclofenac is structurally similar with diclofenac, but has been proven to be a safer and more effective alternative.[31] It is surmised that aceclofenac was used at a higher rate than diclofenac in this study because of fewer adverse events. Tramadol was the medicine prescription of 3rd highest frequency out of total prescriptions and appeared to be mainly used as an alternative to commonly used NSAIDs, aceclofenac, and diclofenac. Tramadol possesses mild opioid activity, acting on the central nervous system,[32] and is used to effectively manage chronic patients who show unsatisfactory response to NSAIDs.[33] Tramadol was shown to be used more frequently in inpatients than outpatients, suggesting that it is used more often in severe cases as opposed to mild cases.
Pethidine was the most often used narcotic for cervical disorders in Korea. Pethidine is a synthesized opioid also known as meperidine, extracted from phenyl pyridine, and is generally used to manage severe cases of pain.[34] Although it has been known to cause nausea and vomiting in overdose,[35] adverse events are not limited to pethidine, and most opioids have been linked with adverse effects that may affect physical function, causing vertigo or drowsiness, and therefore require caution in prescription.[36] Still, use of pethidine has been declining in favor of other opioid analgesics in the United States in light of these adverse events.[37] These results also show that pethidine has a very low prescription rate of <0.1% in outpatients where management of drug administration is more challenging, and most prescriptions were for inpatients in this study.
Approximately 98% of the Korean population receives national health insurance coverage, and national health insurance claims statement data may be considered to be representative of the Korean population and its healthcare system. The national health insurance claims data were analyzed to assess and compare healthcare use and medical expenditure of major cervical disorder patients in Korea, and provided a breakdown of the composition of usual care for each disorder. Currently, there is a paucity of studies comparing medical service use and usual care of common cervical disorders, and this study holds significance in that it is the first study to provide a comprehensive analysis of specific healthcare usage for cervical sprain/strain, cervical IDD, and cervicalgia in Korea. The strengths and implications of this study can be largely divided into the following 3 aspects: 1st, these results may provide practitioners with general guidelines in administering usual care including pharmacological care for cervical disorder treatment and management; 2nd, as a comprehensive analysis of characteristics, medical expenses, and medical service use of major cervical disorders from nationally representative data, these results may be used as referential data when planning national healthcare policies, and appropriating national health insurance fees and budgets relating to cervical disorders; and 3rd, from a research perspective, these findings provide a basic guide to pragmatic studies on cervical disorder treatment which set usual care as active controls. Moreover, given that evidence-based standard care and real-world usual care tend to be discrepant with additional divergences by country and culture, this current report further serves as a window into high-frequency medical service use from a healthcare data source representative of Korea and holds international relevance such as for clinicians, researchers, and healthcare policy makers.
The diagnostic classification system currently used in HIRA is not well equipped to define pain exclusive to the cervical spine, and while subjects were limited to those with primary and X-ray diagnoses clearly related to cervical disorders, defining the patient population solely based on administrative coding may be controversial. Although the initial inclusion criteria were set as patients with a primary KCD code for cervical disorders, X-ray results were additionally included to improve precision in patient identification in view of expert opinion that KCD codes are largely for administrative means and that primary and secondary diagnostic codes may not directly correspond to primary and secondary diagnosis, respectively, and that X-rays are routinely conducted in Korea. This selection method follows that of a previous report issued by the National Evidence-based Health Care Collaborating Agency using the same data source which included lumbar X-rays in defining chronic LBP patients.[38] Nonetheless, this may be considered a methodological limitation as it leads to exclusion of cervical disorder patients without X-ray results in the course of aiming to improve identification precision. Researchers utilizing national health insurance claims data in future studies need to give careful consideration to valid diagnostic coding and participant selection. Park et al[39] previously reported that diagnostic coding tends to be more accurate in patients suffering from more severe medical conditions compared to milder conditions, in inpatients rather than outpatients, and in general hospitals than clinics. As the inclusion and exclusion criteria of this study followed administrative coding, whether the given codes were concordant with clinical symptoms cannot be confirmed. In addition, as analgesic intake was identified through prescription codes in outpatients, whether or not patients actually took the medication as indicated could not be verified. These limitations are shared by all studies using claims data. Moreover, if the medical service recipient were diagnosed with administrative codes other than cervical disorders, it will be unclear whether the surgery, injections, analgesics, and physical therapy codes were prescribed for cervical disorder treatment purposes. The authors accordingly excluded extracted treatment items that appeared to be unrelated to the cervical spine in an attempt to enhance precision, but this may be viewed as an additional limitation regarding data coding and selection. In addition, over-the-counter medicine and medical service items not covered by national insurance are not included in claims data, and this may act as a limitation in accurately portraying general medical usage in Korea. For example, the Korean medical system recognizes both conventional and Korean medicine, and Korean medicine is commonly used for such musculoskeletal disorders as cervical or lumbar spine disorders. The 2011 HIRA NPS analysis results show that the usage rate of Korean medicine for nonspecific back pain is high at 28.8%.[40] However, the 2014 HIRA NPS dataset used in this study does not contain Korean medicine usage data, and therefore provides a partial window into current medical service use for musculoskeletal disorders. Along these lines, the Korean medicine hospitals reported in Table 2 in medical institution distribution denote conventional medicine clinics set up in Korean medicine hospitals and therefore require caution in interpretation. Although this study did not apply weights for the population, as 3% of total patients were extracted, the total population may be estimated by multiplying 33.3 to the patient numbers and expenditures. An additional limitation is that this study is a cross-sectional study of the 2014 dataset which covers the period of 1 year, and following the patients through to long-term follow-up is not an available option. In order to further elucidate disease properties regarding natural history and prognosis, cohort studies using claims data should also be considered.
Numerous previous studies report use of usual care for neck pain treatment.[41,42] However, many do not discuss the contents or give individual mention to physical therapy, analgesics or antiinflammatory agents, NSAIDs, consultation with general practitioners, rest, exercise, education, manipulation, electrotherapy, and acupuncture treatments,[43–48] but with no specific treatment composition or consistent guidelines for treatment and management of cervical disorders. It appears that a more systematic and structured composition of usual care is called for. The analysis results of the most frequently used treatments for cervical sprain/strain, cervical disc disorder with radiculopathy, and cervicalgia patients in Korea may be used as basic data in implementing usual care.
This study uses national health insurance claims data provided by HIRA to assess the medical expenses and current treatment of cervical sprain/strain, cervical disc disorder with radiculopathy, and cervicalgia in Korea. This study holds significance in that the analysis of medical expenditure distribution in cervical disorders offers a rational healthcare policy guideline regarding cervical disorders to decision makers, and the detailed analysis and comparison of usual care for cervical disorders (ie, surgery, injections, physical therapy, and analgesics) provides clinicians and researchers with a current window into usual practice patterns.
Supplementary Material
Acknowledgments
The authors thank the Traditional Korean Medicine R&D program funded by the Ministry of Health & Welfare through the Korea Health Industry Development Institute (KHIDI) (HB16C0035) for the support.
Footnotes
Abbreviations: ATC = anatomical therapeutic chemical, HIRA = health insurance review and assessment service, NPS = national patient sample, IDD = intervertebral disc displacement, KCD = Korean standard classification of diseases.
Funding/support: This study was supported by the Traditional Korean Medicine R&D program funded by the Ministry of Health & Welfare through the Korea Health Industry Development Institute (KHIDI) (HB16C0035).
The authors have no conflicts of interest to disclose.
Supplemental Digital Content is available for this article.
References
- [1].Son KM, Cho NH, Lim SH, et al. Prevalence and risk factor of neck pain in elderly Korean community residents. J Korean Med Sci 2013;28:680–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Hoy D, Protani M, De R, et al. The epidemiology of neck pain. Best Pract Res Clin Rheumatol 2010;24:783–92. [DOI] [PubMed] [Google Scholar]
- [3].Murray CJ, Abraham J, Ali MK, et al. The state of US health, 1990–2010: burden of diseases, injuries, and risk factors. JAMA 2013;310:591–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Fejer R, Kyvik KO, Hartvigsen J. The prevalence of neck pain in the world population: a systematic critical review of the literature. Eur Spine J 2006;15:834–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Hogg-Johnson S, van der Velde G, Carroll LJ, et al. The burden and determinants of neck pain in the general population: results of the bone and joint decade 2000–2010 task force on neck pain and its associated disorders. JManipulative Physiol Ther 2009;32:S46–60. [DOI] [PubMed] [Google Scholar]
- [6].Binder A. Neck pain syndromes. Clinical Evidence 2007. [Google Scholar]
- [7].Fernández-de-las-Peñas C, Hernández-Barrera V, Alonso-Blanco C, et al. Prevalence of neck and low back pain in community-dwelling adults in spain: a population-based national study. Spine 2011;36:E213–9. [DOI] [PubMed] [Google Scholar]
- [8].White K, Hudgins TH, Alleva JT. Cervical sprain/strain definition. Dis Mon 2009;55:724–8. [DOI] [PubMed] [Google Scholar]
- [9].Carette S, Fehlings MG. Cervical radiculopathy. N Engl J Med 2005;353:392–9. [DOI] [PubMed] [Google Scholar]
- [10].Abbed KM, Coumans J-VC. Cervical radiculopathy: pathophysiology, presentation, and clinical evaluation. Neurosurgery 2007;60:S1–28. [DOI] [PubMed] [Google Scholar]
- [11].Springer, Wiesel SW, Lauerman WC, Scherping SC., Jr The spine. Essentials of Orthopedic Surgery. 2007;pp. 276–332. [Google Scholar]
- [12].Radhakrishnan K, Litchy WJ, O’Fallon WM, et al. Epidemiology of cervical radiculopathy. Brain 1994;117:325–35. [DOI] [PubMed] [Google Scholar]
- [13].Sohn M, Jung M. Effects of public and private health insurance on medical service utilization in the National Health Insurance System: National panel study in the Republic of Korea. BMC Health Serv Res 2016;16:503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Lee SM, Han SK, Kim JH, et al. Clinical Effectiveness of Injection Therapy for Chronic Low Back Pain. Seoul: National Evidence-based Healthcare Collaborating Agency; 2010. [Google Scholar]
- [15].World Health Organization. Ministry of Health and Welfare. Republic of Korea: Health Service Delivery Profile; 2012. [Google Scholar]
- [16].Methodology WCCfDS. ATC/DDD Methodology: History. http://www.whocc.no/atc_ddd_methodology/history/. Accessed November 4, 2017. [Google Scholar]
- [17].Methodology WCCfDS. ATC: Structure and principles. http://www.whocc.no/atc/structure_and_principles/. Accessed November 4, 2017. [Google Scholar]
- [18].Clark CR. The Cervical Spine. 4th ed.Philadelphia, PA: Lippincott Williams & Wilkins; 2005. [Google Scholar]
- [19].Thomas AZ, Thomas BO. The use of freeze-dried allograft bone for anterior cervical fusions. Spine 1991;16:726–9. [DOI] [PubMed] [Google Scholar]
- [20].Goffin J, Geusens E, Vantomme N, et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 2004;17:79–85. [DOI] [PubMed] [Google Scholar]
- [21].Eck JC, Humphreys SC, Lim TH, et al. Biomechanical study on the effect of cervical spine fusion on adjacent-level intradiscal pressure and segmental motion. Spine 2002;27:2431–4. [DOI] [PubMed] [Google Scholar]
- [22].Fuller DA, Kirkpatrick JS, Emery SE, et al. A kinematic study of the cervical spine before and after segmental arthrodesis. Spine 1998;23:1649–56. [DOI] [PubMed] [Google Scholar]
- [23].Goffin J, van Loon J, Van Calenbergh F, et al. Long-term results after anterior cervical fusion and osteosynthetic stabilization for fractures and/or dislocations of the cervical spine. J Spinal Disord 1995;8:500–8. discussion 499. [PubMed] [Google Scholar]
- [24].Pagel P, Kersten J, Farber N. Michlovitz SL, Nolan T, et al. Heat therapy modalities: beyond fake and lake. Modalities for Therapeutic Intervention. 4th ed.. Philadelphia, PA: F.A. Davis Company; 2005. 61–78. [Google Scholar]
- [25].Roberta CV, Stella P, Daiane QG, et al. Effects of carrier frequency of interferential current on pressure pain threshold and sensory comfort in humans. Arch Phys Med Rehabil 2013;94:95–102. [DOI] [PubMed] [Google Scholar]
- [26].Jorge FC, Susan AO, David JM, et al. A preliminary investigation into the effects of active interferential current therapy and placebo on pressure pain sensitivity: a random crossover placebo controlled study. Physiotherapy 2011;97:291–301. [DOI] [PubMed] [Google Scholar]
- [27].Ganne JM. Stimulation of bone healing with interferential therapy. Aust J Physiother 1988;34:9–20. [DOI] [PubMed] [Google Scholar]
- [28].Ganne JM, Speculand B, Mayne LH, et al. Interferential therapy to promote union of mandibular fractures. Aust N Z J Surg 1979;49:81–3. [DOI] [PubMed] [Google Scholar]
- [29].Cho HY, Lee SH, In TS, et al. Effects of transcutaneous electrical nerve stimulation (TENS) on changes in postural balance and muscle contraction following muscle fatigue. J Phys ther Sci 2011;23:899–903. [Google Scholar]
- [30].Maeda Y, Lisi TL, Vance CG, et al. Release of GABA and activation of GABA A in the spinal cord mediates the effects of TENS in rats. Brain Res 2007;1136:43–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Sharma G, Singh J, Anand D, et al. Aceclofenac: species-dependent metabolism and newer paradigm shift from oral to non-oral delivery. Curr Top Med Chem 2017;17:107–19. [DOI] [PubMed] [Google Scholar]
- [32].Scott LJ, Perry CM. Tramadol. Drugs 2000;60:139–76. [DOI] [PubMed] [Google Scholar]
- [33].Inage K, Orita S, Yamauchi K, et al. Low-dose tramadol and non-steroidal anti-inflammatory drug combination therapy prevents the transition to chronic low back pain. Asian Spine J 2016;10:685–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Shipton E. Should New Zealand continue signing up to the pethidine protocol. N Z Med J 2006;119:U1875. [PubMed] [Google Scholar]
- [35].McKee KC, Nazif DMM, Jackson MDL, et al. Dose-responsive characteristics of meperidine sedation in preschool children. Sleep 1990;1:3. [PubMed] [Google Scholar]
- [36].Avouac J, Gossec L, Dougados M. Efficacy and safety of opioids for osteoarthritis: a meta-analysis of randomized controlled trials. Osteoarthritis Cartilage 2007;15:957–65. [DOI] [PubMed] [Google Scholar]
- [37].McCaig LF, Burt CW. National Hospital Ambulatory Medical Care Survey: 2003 Emergency Department Summary: Advance Data from Vital and Health Statistics: National Center for Health Statistics; 2005;27. [Google Scholar]
- [38].Lee SM, Han SK, Kim JH, et al. Clinical effectiveness of injection therapy for chronic low back pain: Korean National Evidence-based Health Care Collaborating Agency, 2010:1–232. [Google Scholar]
- [39].Park B, Seong J, Park G, et al. Studying on improving diagnosis codes in National Health Insurance claims data. Seoul: Health Insur ance Review and Assessment Service 2003. [Google Scholar]
- [40].Ahn Y-J, Shin J-S, Lee J, et al. Evaluation of use and cost of medical care of common lumbar disorders in Korea: cross-sectional study of Korean Health Insurance Review and Assessment Service National Patient Sample data. BMJ Open 2016;6:e012432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].van Geest S, Kuijper B, Oterdoom M, et al. CASINO: surgical or nonsurgical treatment for cervical radiculopathy, a randomised controlled trial. BMC Musculoskelet Dis 2014;15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Blödt S, Pach D, Roll S, et al. Effectiveness of app-based relaxation for patients with chronic low back pain (Relaxback) and chronic neck pain (Relaxneck): study protocol for two randomized pragmatic trials. Trials 2014;15:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Pfister DG, Cassileth BR, Deng GE, et al. Acupuncture for pain and dysfunction after neck dissection: results of a randomized controlled trial. J Clin Oncol 2010;28:2565–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].MacPherson H, Tilbrook H, Richmond S, et al. Alexander Technique lessons or acupuncture sessions for persons with chronic neck pain: a randomized trial. Ann Intern Med 2015;163:653–62. [DOI] [PubMed] [Google Scholar]
- [45].MacPherson H, Tilbrook HE, Richmond SJ, et al. Alexander technique lessons, acupuncture sessions or usual care for patients with chronic neck pain (ATLAS): study protocol for a randomised controlled trial. Trials 2013;14:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Jull G, Kenardy J, Hendrikz J, et al. Management of acute whiplash: a randomized controlled trial of multidisciplinary stratified treatments. PAIN 2013;154:1798–806. [DOI] [PubMed] [Google Scholar]
- [47].Williams NH, Wilkinson C, Russell I, et al. Randomized osteopathic manipulation study (ROMANS): pragmatic trial for spinal pain in primary care. Fam Pract 2003;20:662–9. [DOI] [PubMed] [Google Scholar]
- [48].Hudson JS, Ryan CG. Multimodal group rehabilitation compared to usual care for patients with chronic neck pain: a pilot study. Man Ther 2010;15:552–6. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


