Abstract
In the U.S., transgender and other gender minority (TG) youth are an at-risk group understudied in HIV prevention and treatment. This study sought to characterize the HIV prevention and care continua in a diverse sample of 181 sexually-active TG ages 16–24 years (mean age = 20.7 years; 76.8% trans feminine; 69.1% youth of color) recruited July–December 2015 in 14 U.S. cities. Overall, 30.9% reported living with HIV, of which 71.4% were on antiretroviral therapy (ART) and 55.0% were medication adherent; 65.6% were known to be virally suppressed. In multivariable models, medical gender affirmation was associated with lower odds of viral suppression. Medical gender affirmation and stigma in HIV care were each independently associated with elevated odds of having missed HIV care appointments. Among at-risk TG youth not living with HIV, only 8.2% had accessed pre-exposure prophylaxis (PrEP). Early biobehavioral prevention and treatment interventions are needed for TG youth.
Keywords: Transgender, HIV, Prevention, Adolescents
Introduction
Adolescents and emerging adults ages 13–24 years (“youth”) comprised 22% of all new HIV infections in the United States (U.S.) in 2014 [1]. The HIV prevention continuum is a framework that heuristically describes each step in the continuum of HIV biobehavioral prevention services, including HIV testing, behavioral risk reduction counseling and PrEP uptake, and emphasizes the importance and interconnected-ness of each prevention step to decrease HIV acquisition and transmission [2]. The HIV care continuum is a stage model to characterize health outcomes for individuals living with HIV, including linkage to care, retention in HIV care, and viral suppression (e.g., transmission risk reduction) [3]. Together these linked HIV prevention and care continua [4] offer an integrated and holistic model for conceptualizing a full range of engagement in HIV-related services and outcomes. This framework can be utilized to target and achieve national public health goals for the U.S. HIV epidemic, including for key populations of youth [5] who disproportionately struggle with engagement in primary and secondary HIV services relative to adults [6].
A gap in current U.S. HIV research is the lack of characterization of the full HIV prevention and case continua among transgender and other gender minority (TG) youth who have a current gender identity or expression different from their assigned sex at birth [7]. Although few data are available on the percentage of U.S. adolescents who are TG [8, 9], TG adults comprise an estimated 1.4 million individuals in the US [10]. TG adults assigned a male sex at birth who identify on the trans feminine (TF) gender spectrum, have long been known to be at high-risk for acquiring and transmitting HIV infection [11], and have an estimated 21.7% laboratory-confirmed HIV prevalence (meta-analysis), a 34.2-fold increased odds of HIV infection relative to the US general population [12]. This high prevalence of HIV is compounded by high rates of unrecognized HIV infection (i.e., > 10%) in TF individuals, with the largest percentage among young TF ages 29 years and younger [13]. Although less is known about HIV in TG individuals assigned female sex at birth who identify on the trans masculine gender spectrum (TM) [14], existing studies report a lower prevalence of HIV in this group (from 0 to 10%) [11, 15]. However, several studies document high levels of HIV-related sexual risk behaviors among TM adults (e.g., condomless sex and sexually transmitted infections; STIs), particularly among those who have sex with men [15–19], which could augment rates of HIV among TM in the future.
Between 2009 and 2014 in the U.S., more than one in 3 diagnoses in TF individuals were ages 13–24 years (8.3% ages 13–19 years, 28.0% ages 20–24 years); more than one in 5 were in TM (6.4% age 13–19, 16.6% ages 30–24) [20]. Community-based convenience samples have reported HIV prevalence between 5 [21, 22] and 20% [23, 24] in TF under ages 29 years. This suggests an already high HIV prevalence in some TG youth samples necessitating HIV secondary prevention and treatment efforts; and in other samples, a higher than U.S. general population rate of HIV infection with the need for HIV biobehavioral primary prevention and HIV testing efforts. Few studies have been identified in the published literature focused exclusively on characterizing HIV-related outcomes in TG youth living with HIV in the U.S [25]. Studies that include TG individuals are mostly comprised of adults older than emerging adulthood [26–29]. In addition, to our knowledge, there has been very limited research on HIV and related outcomes in nonbinary individuals (e.g., gender nonconforming, genderqueer, genderfluid, or any other gender different than their assigned sex at birth), either youth or adults. National HIV Surveillance System data from 2009 to 2014 found that 0.7% of HIV infections (n = 16) occurred in nonbinary transgender people; however, data were not disaggregated by other factors (e.g., age, sex assigned at birth, race, ethnicity) [20]. These data are urgently needed to reduce HIV incidence and improve health outcomes for diverse TG youth who are vulnerable to and living with HIV infection.
TG youth are a key population in the HIV epidemic not only due to being at high risk of HIV infection, but also because of challenges and barriers they face accessing needed HIV prevention, testing, treatment, and other healthcare services. Two social determinants of TG health that necessitate consideration in understanding and meeting the HIV-related healthcare needs of TG youth are gender affirmation and stigma. Gender affirmation refers to being recognized or affirmed in one’s gender identity or expression [30]. Gender-affirmative healthcare refers to healthcare services that are responsive to TG patient needs, including using correct pronouns (he/him/his, she/her/hers, they/them/their) and name (not necessarily the patient’s legal name or the name on their health insurance), and having access to medical gender affirmation therapies including cross-sex hormones and surgical interventions [31]. Medical gender affirmation has been shown to improve psychological health and quality of life for TG individuals [32, 33], including for TG adolescents and emerging adults [34–36]. Several studies have considered medical gender affirmation in HIV-related outcomes for TG people [26, 37–42]; in general, medical gender affirmation (e.g., hormones) has been shown to positively increase retention in HIV care for TF living with HIV. Medical gender affirmation data on the full range of TG youth (e.g., TF, TM, nonbinary) across the HIV prevention and continua are lacking.
The second social determinant known to uniquely influence TG individuals’ is stigma, including in healthcare contexts and settings [43–49]. TG stigma can also manifest in social and economic marginalization and exclusion for TG youth and contribute to the high rates of unstable housing/homelessness (e.g., due to discrimination in housing, rejection from family, and other stigma-related stressors) [21, 24], sex work (e.g., to obtain an income in the face of economic marginalization) [23], and substance abuse to cope with mistreatment [50, 51] documented among TG youth. Inadequate housing, economic marginalization, and substance use are known barriers to healthcare engagement and HIV treatment adherence for cisgender and TG adults living with HIV, and for cisgender youth [1, 52]. Research exploring the role of individual, interpersonal, and structural barriers to engaging in primary and secondary HIV services is warranted in TG youth, including measures to assess experiences of stigma in HIV prevention and testing, and HIV care and treatment settings.
The primary aim of this study is to characterize TG youth experiences of engagement in the HIV prevention and care continua by gender identity and by HIV serostatus. Guided by gender affirmation [38] and gender minority stress [53] frameworks in the context of a developmental socio-ecological framework [54], the secondary goal is to examine whether and how gender affirmation and stigma are linked to specific HIV prevention and care continua outcomes in this youth population. We hypothesized that medical gender affirmation (e.g., hormones) would be positively associated with better HIV-related outcomes, and that stigma would be negatively associated with these outcomes. To our knowledge, this is the first study to explore the full range of HIV-related outcomes along the prevention and care continua among diverse TG youth across the U.S. These data are urgently needed to improve HIV-related health outcomes for at-risk TG and TG youth living with HIV infection.
Methods
Between July and December 2015, 187 diverse TG adolescents and emerging adults ages 16–24 years were recruited and enrolled in a Affirming Voices for Action (AVA), a mixed-methods study conducted across 14 U.S. cities (Tampa, Los Angeles, Washington D.C., Philadelphia, Chicago, New York, New Orleans, Miami, Memphis, Houston, Detroit, Baltimore, Boston, and Denver). The goal of the study was to characterize the HIV prevention and care continua (e.g., prevention, testing, and diagnosis, linkage to care, engagement in care, retention in care, ART initiation, ART adherence, and viral suppression) in a diverse sample of TG youth across the U.S., and to assess TG youth experiences with accessing services along the HIV prevention and care continua, including barriers and facilitators to service engagement. The current article draws from quantitative survey data. Of 186 TG youth with survey data, five youth were missing data on assigned sex at birth and/or current gender identity and therefore excluded from analyses. The final data analytic sample size for this article is 181 TG youth.
TG Youth Community Engagement
The study was conducted in line with the community-based participatory research principles of cooperative and participatory engagement from stakeholders, collaborative participation, and representation from community members, and dissemination of findings to stakeholders [55–57]. A Youth Advisory Board (YAB) was convened comprised of diverse TG youth (in terms of age, race, ethnicity, and gender identity) at three geographically diverse sites—Detroit, Los Angeles, and Boston (3–4 youth per site). The YAB met monthly in-person at each local site, and quarterly these meetings included a video conference across the three sites with the project director and at least one PI present during each in-person and virtual meeting. YAB members received a stipend for their participation in each meeting. The YAB was a vital part of the study team providing insight on the study protocol, study branding and recruitment, measure development and selection, interview guides, implementation, feasibility and acceptability of study procedures, and dissemination activities.
Recruitment and Eligibility
Potential participants were purposively sampled from 14 Adolescent Medicine Trials Unit (AMTU) sites. Youth currently engaged in care at an AMTU site (defined as receiving HIV specialty medical services at an ATN site or their affiliates; youth living with HIV infection) and those not currently engaged in care at an AMTU site (not receiving HIV specialty medical services; youth living with HIV, not living with HIV, or with HIV unknown status) were sampled to ensure broad range of participation, including individuals not currently engaged in ATN research. For TG youth engaged in care, AMTU staff at each of the study sites recruited potential participants from their patient population or collaborative community partners. For TG youth not engaged in care, AMTU staff at each of the study sites recruited participants from their Community Advisory Boards, Connect-to-Protect Coalition [58], and community partners. Advised by the YAB, the study team engaged local TG communities in the catchment areas of each of the AMTU sites. A Transgender Community Specialist, who was a member of the TG community, was hired to build connections with community groups. The research team was comprised of diverse individuals specialized in adolescent and emerging adult health and in LGBTQ health, and was connected nationally and internationally to TG communities. The study team conducted training with each site to improve capacity to recruit youth and local resources specific to the catchment area of their clinic or hospital to facilitate community engagement and cultural humility of AMTU sites [59].
Eligibility for participation was: (a) do not solely identify with sex assigned at birth (may identify as trans, transgender, trans woman, trans man, man, woman, gender nonconforming, genderqueer, or any other gender, so long as their current gender identity and/or expression do not match their sex assigned at birth); (b) self-report being ages 16–24 years inclusive at time of consent; (c) able to understand both written and spoken English; (d) willing to participate in a quantitative survey and in-depth face-to-face qualitative interview about TG identity and personal experiences seeking HIV prevention, testing, and treatment services; and (e) able to understand and willing to provide signed informed consent for study participation.
Study Procedure
Participants completed written informed consent; a waiver of consent was obtained for youth under ages 18 years due to disclosure issues that may present themselves for TG youth and youth living with HIV infection (e.g., potential risk of abuse or ejection from the home if parents/guardians are not away of their gender identity or HIV status).
Study participation involved completing a quantitative survey via computer-assisted self-interview and participating an in-depth face-to-face qualitative interview with a highly-trained interviewer about TG identity and personal experiences seeking HIV prevention, testing, and treatment services to understand facilitators and barriers TG youth experience at each stage of the HIV prevention and care continua. The study visit took approximately 2.5 h to complete and participants were monetarily compensated for their time in accordance with local site standards and norms related to study participation. All study activities were approved at the Institutional Review Boards at the 14 AMTU sites, as well as investigators’ institutions.
Measures
Sex, Gender, and Medical Gender Affirmation
A “two-step” method was used to capture assigned sex at birth (step 1) and current gender identity (step 2) [60]. “What sex were you assigned at birth, meaning what the doctor put on your original birth certificate?” Response options were “female” or “male”. “What is your current gender identity?” with six response options: “female”, “male”, “trans female/trans woman”, “trans male/trans man”, “genderqueer/gender nonconforming”, “a gender not listed here”. Respondents were cross-classified using the sex and gender questions. A variable was created for gender identity spectrum to compare youth who were trans feminine (TF; assigned a male sex at birth whose current gender identity was not male) to youth who were trans masculine (TM; assigned a female sex at birth who responded their current gender identity was not female). Another variable was operationalized as binary gender identity (female, male, trans female/trans woman, trans male/trans man) versus nonbinary gender identity (genderqueer/gender nonconforming, a gender not listed). Youth were asked about medical gender affirmation, including hormones (e.g., estrogen, testosterone) and surgical interventions (e.g., breast augmentation, facial feminization, etc.). Medical gender affirmation was operationalized as hormones and/or surgery (yes/no). Non-prescription hormone use (yes/no) was also queried.
Demographics, Psychosocial, and Sexual Health
Age was queried in years. For ethnicity, youth were asked if they were of Hispanic (Spanish) or Latino heritage (yes/no). Ethnicity was coded as Latino/Hispanic (yes/no). Racial background was asked in a “check all that apply” format with the categories: American Indian, Alaska Native, Asian, Native Hawaiian, Pacific Islander (other than Native Hawaiian), Black or African American, White, Other. Race was operationalized as youth of color (four categories: Black or African American, American Indian/Alaska Native, Asian/Native Hawaiian/Pacific Islander, another race) vs white (non-Hispanic). Youth were asked current student status (yes/no), family poverty (ever received assistance from the Aids to Families with Dependent Children (AFDC), Temporary Assistance for Needy Families (TANF), food stamps, or free lunch programs; yes/no), lifetime history of being homeless (yes/no), lifetime history of sex work (yes/no). Substance use was assessed using the validated 6-item CRAFFT where a score 2 + was considered a positive screen for problematic substance use [61, 62.] Youth were asked to select the gender of their sexual partners (male, female, and/or transgender) in the last 6 months. They were also asked about condomless sex in the context of substance use in last 6 months: “in the last 6 months after [drinking alcohol, smoking marijuana, using other drugs besides alcohol and marijuana] did you have vaginal or anal sex without a condom, even though you had intended to use a condom? With male, female, or transgender partners.” A binary variable for condomless sex in the last 6 months was created for each substance (alcohol, marijuana, and other drugs).
HIV Prevention Continuum
Youth were asked to self-report HIV testing and HIV serostatus. Participants were asked if they had ever been tested for HIV, and the result of their most recent HIV test (response options were positive, negative, unknown, don’t know). HIV status was operationalized as living with HIV (positive), not living with HIV (negative), or HIV status unknown (youth who had never been tested for HIV, answered HIV status as unknown or don’t know). Youth were asked whether or not they had used primary HIV prevention services or programming (e.g., risk reduction counseling, demonstrations on how to properly use condoms, programs for couples or groups focused on reducing the risk of acquiring HIV) in their lifetime and in the last 6 months (yes/no). Youth who reported accessing HIV prevention services in the last 6 months were asked how specific these were “to your needs as a transgender or gender nonconforming person” with response options 1 = very specific to 4 = not at all specific. Responses were dichotomized as “not at all specific” and compared to all others responses that were considered to have some degree of youth-perceived competency in meeting TG needs (i.e., trans-friendly). Biomedical HIV prevention was queried, including lifetime and past 6 month use of PrEP, and lifetime post-exposure prophylaxis use (PEP) utilization.
HIV Care Continuum
Measures for the HIV care continuum were consistent with those used to measure engagement in the HIV continuum of care within previous ATN studies [63]. Youth living with HIV were asked whether they had ever disclosed their HIV serostatus to anyone (yes/no). Youth living with HIV were asked whether or not they had utilized secondary HIV prevention services or programming in the last 6 months (yes/no). A follow-up question was asked about the extent to which these services met their needs (“how specific were they to your needs as a transgender or gender nonconforming person?”) with responses ranging from 1 = very specific to 4 = not very specific and were dichotomized as not very specific vs all other (considered trans-friendly). Youth living with HIV were asked about HIV medication use ever and currently to treat HIV infection (yes/no). Adherence was assessed by asking youth about the last 7 days taking HIV medications [64]. One or more doses missed were categorized as not fully adherent during the last 7 days. Youth living with HIV were asked whether they knew their most recent viral load is (yes/no), and if yes what their most recent viral load was (responses: 1 = undetectable, 2 = 75–5000, 3 = 5000–10,000, 4 = above 10,000). Viral non-suppression was defined as youth reporting any detectable viral load. Youth were asked how long ago they had blood drawn to learn their VL with responses ranging from 1 = less than 3 months ago to 5 = more than 12 months ago. Youth with recent viral load less than 3 months ago (yes/no) were compared to others. Retention in HIV care was assessed by asking youth how many doctor’s appointments they missed in the last 6 months (responses ranged from 0 to 20). Two dichotomous variables were operationalized: missing two or more appointments; missing one appointment (yes/no).
Gender Affirmation and Stigma in HIV Prevention and Care Continua Settings
Due to a dearth of available measures for use with TG youth in HIV research, the study team and the YAB collaborated to develop, design, and refine scales to assess gender affirmation in HIV prevention and care, and stigma in HIV prevention and care (4 scales) [65]. For each scale (described below), preliminary measure performance was assessed with an exploratory factor analysis (EFA) to test that the items loaded onto a single factor (estimated eigenvalue and percent variance explained [PVE]) and internal consistency reliability (Cronbach’s alpha [α]).
Gender Affirmation
Respondents were asked about gender affirmation in HIV healthcare service settings: “In the past 12 months, how supported have you felt in your gender identity or gender expression at place(s) where you accessed HIV-related services?” Response options ranged from 1 = not at all supported to 4 = very supported. HIV Prevention: HIV-uninfected and unknown serostatus youth were asked about HIV prevention (1 item) and HIV testing (1 item). The two items were highly correlated (r = 0.64; p < 0.0001), loaded onto a single factor (eigenvalue = 1.64; PVE = 82.1%), and had acceptable reliability (α = 0.78). HIV Care Settings: Youth living with HIV were asked about HIV care (1 item), HIV medications (1 item), and other support services (1 item). These three items were highly correlated (r = 0.77–0.83; p < 0.0001), loaded onto a single factor (eigenvalue = 2.64; PVE = 88.2%), and had excellent reliability (α = 0.92). The items were summed for HIV prevention and for HIV care settings.
Stigma
Stigma in specific HIV prevention and care continua settings was assessed by asking youth: “During the past 12 months, how often have you been treated negatively because of your gender identity or gender expression at the place(s) where you have accessed HIV-related services?” Response options were on a Likert scale from 1 = never treated negatively to 5 = very often treated negatively. HIV Prevention and Testing: HIV-uninfected and unknown serostatus youth were asked about HIV prevention and HIV testing services (2 items). These items were highly correlated (r = 0.53; p < 0.0001), loaded onto a single factor (Eigenvalue = 1.53; PVE = 76.5%), and had acceptable reliability (α = 0.69). HIV Care Settings: Youth living with HIV were asked about HIV care, HIV medications, and other support services (3 items). These items were highly correlated (r = 0.45–0.74; p < 0.0001), loaded onto a single factor (eigenvalue = 2.17; PVE = 72.4%), and had good reliability (α = 0.81). The items were summed for HIV prevention and HIV care settings to create separate scales.
Statistical Analysis
Descriptive statistics (mean, standard deviation, frequencies, and proportions) were estimated for all variables of interest. Cross-tabs by gender identity category (TF vs. TM) were examined to characterize the distribution of variables by gender identity across the full HIV continuum of prevention and care. Cross-tabs were conducted by HIV status comparing youth living with HIV to youth not living with HIV or not knowing their current HIV status. Analyses by HIV status were restricted to TF youth given the distribution of HIV infection in the sample (see results). Bivariate comparisons were conducted including χ2 for proportions and t-tests for continuous variables with appropriate tests for equality of variances.
Multivariable logistic regression models were then fit to model HIV prevention and care continua outcomes. Four dichotomous outcomes were modeled for HIV testing and primary prevention: ever tested for HIV infection, primary HIV prevention ever, primary HIV prevention last 6 months, primary HIV prevention trans-friendly. Models included age (continuous in years), gender identity spectrum (TF vs TM), race/ethnicity (YOC vs white non-Hispanic), housing status (homeless ever vs never), medical gender affirmation (hormones and/or surgery yes vs none), CRAFFT score (continuous), gender affirmation in primary HIV prevention and testing (continuous), stigma in primary HIV preventing and testing (continuous). Analyses were then restricted to youth living with HIV (all TF) to model six dichotomous outcomes for HIV care: secondary HIV prevention last 6 months, secondary HIV prevention trans-friendly, medication adherence last 7 days, virally suppressed, missed two or more appointments, missed any appointments. Models included age (continuous in years), race/ethnicity (YOC vs. white non-Hispanic), medical gender affirmation vs none, gender affirmation in HIV care (continuous), stigma in HIV care (continuous). The AIC (Akaike Information Criterion) was used in model selection to identify the most robust and parsimonious statistical model for each outcome [66.] The final fitted model for ever tested for HIV infection was not adjusted for housing status or substance use to ensure goodness-of-model fit. The models for secondary HIV prevention trans-friendly and viral suppression were not adjusted for race (youth of color vs white non-Hispanic) in order to avoid overfitting the models. SAS 9.4.1 was used for all analyses with statistical significance at the alpha 0.05-level.
Results
Descriptive Characteristics of the Sample
Table 1 presents descriptive characteristics of the study sample, comparing trans feminine (76.8%; n = 139) and trans masculine (23.2%; n = 42) youth. The mean age of the sample was 20.7 (SD = 2.2). Overall, 75.1% endorsed a binary gender identity and 24.9% a nonbinary identity. The majority of the sample (69.1%) were youth of color, and the proportion of TF youth of color was statistically significantly higher than in TM (75.5 vs. 47.6%; p = 0.0006). TF were less likely to have medically affirmed their gender (hormones and/or surgery) compared to TM (48.2 vs. 66.7%; p = 0.036). About half (50.3%) of youth sampled reported having been homeless or marginally housed at some time in their life. Overall, 45.3% of youth reported lifetime sex work, with a higher proportion of TF than TM (51.1 vs. 26.2%; p = 0.005). TG youth had sexual partners of diverse genders. A higher proportion of TF vs TM reported male sex partners (74.8% vs 33.3%; p < 0.0001); a higher proportion of TM reported female sex partners (40.5 vs. 10.8%; p < 0.0001). The most heterogeneous distribution of sexual partners was in TM who reported 33.3% male, 40.5% female, and 28.6% TG sex partners. Rates of condomless sex in the last 6 months during substance use ranged from 18.8 to 24.1%. No statistically significant differences by gender identity were found for condomless sex.
Table 1.
Descriptive characteristics of the overall sample of US transgender youth (n = 181) with comparisons of trans feminine and trans masculine youth
| Total sample (n = 181) 100.0% |
Trans feminine (n = 139) 76.8% |
Trans masculine (n = 42) 23.2% |
Test statistica | p value | ||||
|---|---|---|---|---|---|---|---|---|
| Age in years, Mean (SD) (range 16–24) | 20.69 (2.23) | 20.82 (2.24) | 20.26 (2.18) | − 1.43 (179) | 0.156 | |||
| Gender identity | ||||||||
| Binary (TG woman, TG man) | 136 | 75.1 | 108 | 77.7 | 28 | 66.7 | 2.10 (1) | 0.147 |
| Non-binary (genderqueer, genderfluid) | 45 | 24.9 | 31 | 22.3 | 14 | 33.3 | – | – |
| Medical gender affirmation | 95 | 52.5 | 67 | 48.2 | 28 | 66.7 | 4.41 (1) | 0.036 |
| Non-prescription hormone use ever | 30 | 32.3 | 25 | 38.5 | 5 | 17.9 | 3.80 (1) | 0.051 |
| Latino/hispanic ethnicity | 52 | 28.7 | 37 | 26.6 | 15 | 35.7 | 1.30 (1) | 0.2254 |
| Race | ||||||||
| White youth | 56 | 30.9 | 34 | 24.5 | 22 | 52.4 | 11.77 (1) | 0.0006 |
| Youth of color | 125 | 69.1 | 105 | 75.5 | 20 | 47.6 | – | – |
| Black or African American | 117 | 64.6 | 102 | 73.4 | 15 | 35.7 | 20.02 (1) | < 0.0001 |
| American Indian/Alaska Native | 16 | 8.8 | 15 | 10.8 | 1 | 2.4 | 2.83 (1) | 0.124 |
| Asian/Native Hawaiian/Pacific Islander | 10 | 5.5 | 4 | 2.9 | 6 | 14.3 | 8.04 (1) | 0.011 |
| Another race | 12 | 6.6 | 9 | 6.5 | 3 | 7.1 | 0.02 (1) | 0.879 |
| Current student | 88 | 48.6 | 63 | 45.3 | 25 | 59.5 | 2.60 (1) | 0.107 |
| Low family SES | 97 | 53.6 | 75 | 54.0 | 22 | 52.4 | 0.03 (1) | 0.858 |
| Homeless ever | 91 | 50.3 | 74 | 53.2 | 17 | 40.5 | 2.10 (1) | 0.147 |
| Sex work ever | 82 | 45.3 | 71 | 51.1 | 11 | 26.2 | 8.06 (1) | 0.005 |
| Substance use | ||||||||
| CRAFFT score, mean (SD) (range 0–6) | 2.66 (1.95) | 2.58 (1.94) | 2.95 (2.00) | 1.10 (179) | 0.285 | |||
| CRAFFT positive screen (Score 2 +) | 119 | 65.8 | 88 | 63.3 | 31 | 73.8 | 1.58 (1) | 0.209 |
| HIV testing history | ||||||||
| Ever tested for HIV | 167 | 92.3 | 133 | 95.7 | 34 | 80.9 | 9.81 (1) | 0.005 |
| Never tested for HIV | 14 | 7.7 | 6 | 4.3 | 8 | 19.1 | ||
| HIV status | ||||||||
| HIV-infected | 56 | 30.9 | 56 | 40.3 | 0 | 0.0 | 25.30 (2) | <0.0001 |
| HIV-uninfected | 103 | 56.9 | 70 | 50.4 | 33 | 78.6 | ||
| HIV status unknown | 22 | 12.1 | 13 | 9.3 | 9 | 21.4 | ||
| Primary prevention services | ||||||||
| Primary HIV prevention ever (n = 121) | 66 | 54.6 | 50 | 63.3 | 16 | 38.1 | 7.02 (1) | 0.008 |
| Primary HIV prevention, last 6 months (n = 66) | 47 | 71.2 | 37 | 74.0 | 10 | 62.5 | 0.78 (1) | 0.527 |
| Primary HIV prevention trans-friendly (n = 66) | 36 | 54.5 | 30 | 60.0 | 6 | 37.5 | 2.48 (1) | 0.153 |
| PrEP ever (n = 121) | 10 | 8.2 | 10 | 12.7 | 0 | 0.0 | 5.80 (1) | 0.015 |
| PrEP, last 6 months (n = 10) | 5 | 50.0 | 5 | 100.0 | 0 | 0.0 | – | – |
| PEP ever (n = 121) | 5 | 4.1 | 5 | 6.5 | 0 | 0.0 | 2.78 (1) | 0.162 |
| Scales | ||||||||
| Gender affirmation in HIV prevention and testing (range 1–10) | 5.36 (2.38) | 5.78 (2.38) | 4.50 (2.18) | − 2.80 (114) | 0.006 | |||
| Stigma in HIV prevention and testing (range 1–12) | 3.42 (2.68) | 3.29 (2.59) | 3.68 (2.89) | 0.71 (113) | 0.479 | |||
| Gender of sexual partners, last 6 months | ||||||||
| Male partner | 118 | 65.2 | 104 | 74.8 | 14 | 33.3 | 24.46 (1) | < 0.0001 |
| Female partner | 32 | 17.7 | 15 | 10.8 | 17 | 40.5 | 19.53 (1) | < 0.0001 |
| Transgender partner | 34 | 18.8 | 22 | 15.8 | 12 | 28.6 | 3.43 (1) | 0.064 |
| Condomless sex during substance use, last 6 months | ||||||||
| Alcohol (n = 181) | 40 | 22.1 | 34 | 24.5 | 6 | 14.3 | 1.94 (1) | 0.205 |
| Marijuana (n = 112) | 27 | 24.1 | 24 | 27.0 | 3 | 13.0 | 1.94 (1) | 0.273 |
| Other drug(s) (n = 74) | 14 | 18.8 | 11 | 20.0 | 3 | 15.8 | 0.16 (1) | 0.254 |
Bold values indicate statistical significance at the alpha 0.05 level
Continuous variables: Bivariate t-test statistics. We tested for equality of variances and did not reject the null hypothesis that variances were equal; a Pooled estimate for equal variances was utilized. Frequency and proportions: Chi-sqare (χ2) test statistics with degrees of freedom (df) are presented
HIV Prevention and Care Continua
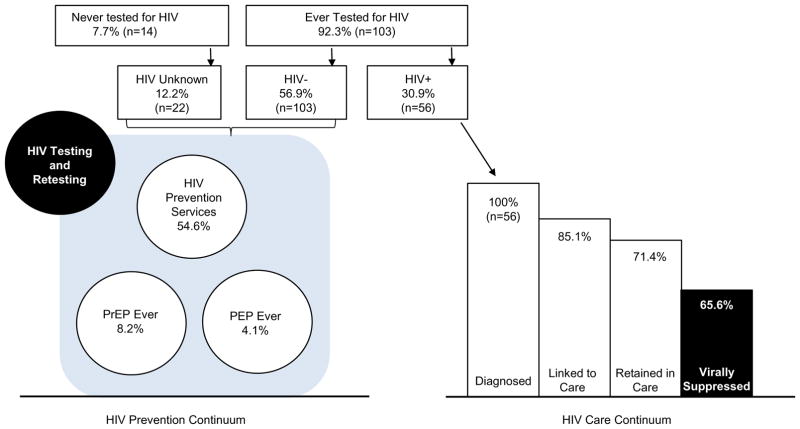
Figure 1 visually illustrates the HIV prevention and care continua in the sample. Overall, prevalence of HIV infection was 30.9% (n = 56/181 cases, self-reported). All HIV cases were in TF, thus HIV prevalence in TF was 40.3% (n = 56/139). Among TF youth living with HIV, 10.7% (6/56) had never disclosed HIV status to anyone.
Fig. 1.
HIV prevention and care continua in transgender youth. Estimation of viral suppression estimation: Among TF living with HIV who knew their viral load (57.1%; n = 32), 65.6% (21/32) reported virolologic suppression. Overall, the proportion of TF living with HIV who were virologically suppressed was 37.5% (21/56), regardless of whether or not they knew their viral load, were on ART, or were adherent to ART
Modified from: http://www.jiasociety.org/index.php/jias/article/view/21263/html#CIT0001_21263
HIV Prevention Continuum
As shown in Table 1, more than 1 in 10 (12.2%) of TG youth sampled did not know their HIV status, and 7.7% had never been tested for HIV in their lifetime. A higher proportion of TF had ever been tested for HIV than TM (95.7 vs. 80.9%; p = 0.005). Among youth not living with HIV or having an unknown HIV status, 54.6% had ever accessed HIV primary prevention services. A significantly higher proportion of TF than TM had accessed prevention services (63.3 vs. 38.1%; p = 0.008). Of these, 71.2% had accessed these services in the last 6 months. Approximately half (54.5%) described these services as trans-friendly. PrEP uptake was low (8.2%), as was use of PEP (4.1%) in the sample.
HIV Care Continuum
TF youth living with HIV were compared to those not living with HIV (presented in Table 2). Relative to TF not living with HIV or not knowing their HIV status, TF youth living with HIV were slightly older, a lower proportion had medically affirmed their gender (35.7 vs. 56.5%; p = 0.02), a lower proportion were currently a student (32.1 vs. 54.2%; p = 0.01), and a higher proportion had ever engaged in sex work (62.5 vs. 43.4%; p = 0.03).
Table 2.
Comparing trans feminine youth living with HIV infection (n = 56) and not living with HIV infection (n = 83)
| HIV-infected (n = 56) | HIV-uninfected or HIV unknown (n = 83) | Test statistic | p-value | |||
|---|---|---|---|---|---|---|
| Age in years, mean (SD) (range 16–24) | 21.34 (1.88) | 20.47 (2.40) | − 2.28 (137) | 0.024 | ||
| Gender identity | ||||||
| Binary | 40 | 71.4 | 68 | 81.9 | 2.13 (1) | 0.145 |
| Non-binary | 16 | 28.6 | 15 | 18.1 | ||
| Medical gender affirmation | 20 | 35.7 | 47 | 56.6 | 5.86 (1) | 0.024 |
| Non-prescription hormone use ever | 12 | 60.0 | 13 | 28.9 | 5.66 (1) | 0.017 |
| Latino/Hispanic ethnicity | 14 | 25.0 | 23 | 27.7 | 0.13 (1) | 0.723 |
| Race | ||||||
| White | 11 | 19.6 | 23 | 27.7 | 1.18 (1) | 0.319 |
| Youth of color | 45 | 80.4 | 60 | 72.3 | ||
| Black or African American | 45 | 80.4 | 57 | 68.7 | 2.34 (1) | 0.171 |
| American Indian/Alaska Native | 6 | 10.7 | 9 | 10.8 | 0.01 (1) | 0.219 |
| Asian/Native Hawaiian/Pacific Islander | 2 | 3.6 | 2 | 2.4 | 0.16 (1) | 0.352 |
| Another race | 3 | 5.4 | 6 | 7.2 | 0.19 (1) | 0.740 |
| Current student | 18 | 32.1 | 45 | 54.2 | 6.57 (1) | 0.010 |
| Low family SES | 35 | 62.5 | 40 | 48.2 | 2.76 (1) | 0.097 |
| Ever homeless | 32 | 57.1 | 42 | 50.6 | 0.57 (1) | 0.491 |
| Sex work ever | 35 | 62.5 | 36 | 43.4 | 4.90 (1) | 0.027 |
| Substance use | ||||||
| CRAFFT score, mean (SD) (range 0–6) | 2.96 (2.13) | 2.31 (1.76) | − 1.96 (137) | 0.052 | ||
| CRAFFT positive screen (Score 2 +) | 36 | 64.3 | 52 | 62.7 | 0.04 (1) | 0.845 |
| Gender of sexual partners, last 6 months | ||||||
| Male partner | 46 | 83.2 | 58 | 70.0 | 2.67 (1) | 0.102 |
| Female partner | 6 | 10.7 | 9 | 10.8 | 0.01 (1) | 0.981 |
| Transgender Partner | 10 | 17.9 | 12 | 14.5 | 0.29 (1) | 0.640 |
| Condomless sex during substance use, last 6 months | ||||||
| Alcohol (n = 139) | 11 | 19.6 | 23 | 27.7 | 1.18 (1) | 0.278 |
| Marijuana (n = 89) | 11 | 27.5 | 13 | 26.5 | 0.01 (1) | 0.918 |
| Other drug(s) (n = 74) | 6 | 22.2 | 5 | 17.9 | 0.16 (1) | 0.746 |
Bold values indicate statistical significance at the alpha 0.05 level
Table 3 presents secondary HIV prevention and care continuum indicators. One in three (33.9%) TF living with HIV had accessed secondary HIV prevention services in the last 6 months, of which 73.7% described the services as trans-friendly. 83.9% of TF living with HIV had initiated ART, of which 85.1% were still currently taking ART. About two-thirds (62.5%) self-reported being adherent to their ART medications last weekend and 55.0% reported being adherent over the last week. Only 57.1% (n = 32) of TF youth living with HIV knew their viral load, of which 65.6% (n = 21) were virologically suppressed. In terms of engagement in care, 8.6% had missed two or more medical appointments in the last 6 months.
Table 3.
Secondary HIV prevention and the HIV care continuum among trans feminine youth living with HIV (n = 56)
| n | % | |
|---|---|---|
| Secondary HIV prevention services | ||
| Secondary HIV prevention, last 6 months (n = 56) | 19 | 33.9 |
| Secondary HIV prevention, trans friendly (n = 19) | 14 | 73.7 |
| HIV medication use and adherence | ||
| Initiation of HIV medications (n = 56) | 47 | 83.9 |
| Currently taking HIV medications (n = 47) | 40 | 85.1 |
| Medication adherent, last weekend (40) | 25 | 62.5 |
| Medication adherent, last 7 Days (n = 40) | 22 | 55.0 |
| Viral load suppression | ||
| Know viral load (n = 56) | 32 | 57.1 |
| Last blood draw to learn viral load < 3 months ago (n = 32) | 24 | 75.0 |
| Virally suppressed (n = 32)a | 21 | 65.6 |
| Retention in care | ||
| Missed two or more appointments, last 6 months (n = 56) | 16 | 28.6 |
| Missed Any Appointments, Last 6 Months (n = 56) | 19 | 33.9 |
| Gender affirmation and stigma scales, mean (SD): | ||
| Gender affirmation HIV care, medications, other support services (range 3–13) | 9.41 (3.31) | |
| Stigma HIV care, medications, other support services (range 1–15) | 5.05 (3.48) | |
Overall, 37.5% (21/56) of TF youth living with HIV were virologically suppressed
Gender Affirmation and Stigma: Modeling HIV Prevention and Care Continua
Four multivariable logistic regression models were fit to examine gender affirmation and stigma in HIV prevention continuum outcomes, which are presented in Table 4. Higher gender affirmation scores and higher stigma scores were each statistically significantly associated with an increased odds of having accessed primary HIV prevention services ever. Experiencing stigma in HIV prevention and testing settings was negatively associated with endorsing having received primary HIV prevention services that were trans-friendly; such that as the frequency of stigma increased, the odds of reporting trans-friendly services meeting their prevention needs as a TG individuals decreased. Older age and being a youth of color vs white (non-Hispanic) were also associated with an increased odds of reporting trans-friendly prevention services in the past 12 months. Gender affirmation and stigma did not statistically predict other outcomes. However, being a youth of color and ever being homeless were each significantly and positively associated with having accessed HIV prevention services in the last 6 months.
Table 4.
HIV testing and primary prevention: multivariable logistic regression models
| Ever tested for HIV infection (n = 115) | Primary HIV prevention ever (n = 122) | Primary HIV prevention, Last 6 months (n = 65) | Primary HIV prevention trans-friendly, last 6 months (n = 66) | |||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age in years (continuous) | 1.22 (0.80, 1.87) | 0.502 | 1.25 (0.90, 1.73) | 0.182 | 0.95 (0.70, 1.28) | 0.715 | 1.39 (1.03, 1.88) | 0.030 |
| Trans feminine vs. trans masculine | 4.86 (0.72, 33.06) | 0.359 | 2.99 (0.62, 14.45) | 0.173 | 0.76 (0.16, 3.67) | 0.729 | 0.54 (0.10, 2.81) | 0.462 |
| Youth of color vs. white (non-Hispanic) Youth | 1.77 (0.29, 10.74) | 0.106 | 2.09 (0.45, 9.65) | 0.345 | 4.56 (1.11, 18.65) | 0.035 | 7.32 (1.66, 32.24) | 0.009 |
| Homeless ever vs. never | – | – | 0.31 (0.07, 1.31) | 0.112 | 4.36 (1.02, 18.62) | 0.047 | 2.35 (0.67, 8.31) | 0.185 |
| Medical gender affirmation vs. none | 4.22 (0.66, 27.21) | 0.130 | 0.71 (0.15, 3.30) | 0.659 | 2.97 (0.77, 11.50) | 0.114 | 0.52 (0.15, 1.84) | 0.312 |
| CRAFFT score (continuous) | – | – | 1.36 (0.90, 2.04) | 0.143 | 0.83 (0.55, 1.26) | 0.378 | 0.83 (0.56, 1.25) | 0.376 |
| Gender affirmation in primary HIV prevention and testing (continuous) | 1.10 (0.73, 1.66) | 0.657 | 3.60 (2.06, 6.29) | < 0.0001 | 1.04 (0.77, 1.40) | 0.796 | 1.04 (0.77, 1.42) | 0.786 |
| Stigma in primary HIV prevention and testing (continuous) | 0.91 (0.65, 1.28) | 0.579 | 1.81 (1.31, 2.50) | 0.0004 | 0.81 (0.64, 1.02) | 0.075 | 0.69 (0.52, 0.91) | 0.009 |
Final model for ever tested for HIV infection outcome was not adjusted for homelessness or substance use (CRAFFT score) in order to obtain the most robust and parsimonious statistical model
Bold values indicate statistical significance at the alpha 0.05 level
Results from six models are shown in Table 5 with HIV care continuum outcomes. Higher stigma scores were positively associated with lack of engagement and retention in care, both missing two or more medical appointments in the last 6 months, and any missing appointments. Gender affirmation in HIV care was not associated with any HIV care continuum outcomes; however, medical gender affirmation was associated with lower odds of viral suppression. Among TF youth who had medically affirmed their gender 36.4% were virally suppressed as compared to 80.9% achieving viral suppression in TF who had not medically affirmed their gender.
Table 5.
Secondary HIV prevention, medication adherence, viral suppression, retention in care: multivariable logistic regression models
| Secondary HIV prevention, last 6 months (n = 56) | Secondary prevention trans-friendly (n = 19) | Medication adherent, last 7 days (n = 40) | Virally suppressed (n = 32) | Missed two or more appointments (n = 56) | Missed Any Appointments (n = 56) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|
|||||||
| OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | OR (95% CI) | p-value | |
| Age in years (continuous) | 1.04 (0.75, 1.44) | 0.839 | 1.10 (0.43, 2.81) | 0.841 | 0.86 (0.59, 1.23) | 0.405 | 1.15 (0.67, 2.99) | 0.611 | 1.09 (0.74, 1.59) | 0.667 | 1.06 (0.74, 1.50) | 0.759 |
| Youth of color vs. white non-Hispanic | 0.82 (0.20, 3.39) | 0.789 | – | – | 1.04 (0.18, 6.15) | 0.966 | – | 1.44 (0.24, 8.50) | 0.687 | 0.97 (0.20, 4.77) | 0.966 | |
| Medical gender affirmation vs. none | 1.14 (0.35, 3.68) | 0.829 | 1.44 (0.06, 37.83) | 0.828 | 0.66 (0.16, 2.71) | 0.568 | 0.06 (0.01, 0.53) | 0.011 | 7.83 (1.82, 33.80) | 0.006 | 5.68 (1.53, 21.06) | 0.009 |
| Gender affirmation in HIV care | 1.00 (0.83, 1.20) | 0.991 | 1.87 (0.93, 3.74) | 0.079 | 0.87 (0.64, 1.18) | 0.372 | 1.26 (0.93, 1.71) | 0.135 | 0.96 (0.77, 1.19) | 0.702 | 1.02 (0.83, 1.25) | 0.887 |
| Stigma in HIV care | 0.94 (0.78, 1.13) | 0.513 | 2.20 (0.78, 6.17) | 0.136 | 0.77 (0.58, 1.03) | 0.082 | 0.90 (0.67, 1.20) | 0.461 | 1.28 (1.04, 1.59) | 0.022 | 1.25 (1.03, 1.53) | 0.027 |
Final models for secondary prevention trans-friendly and viral suppression outcomes were not adjusted for young of color versus white (non-Hispanic) in order to avoid overfitting the models
Bold values indicate statistical significance at the alpha 0.05 level
Discussion
This study is among the first to characterize the HIV prevention and care continua among a U.S. national sample of diverse TG youth. Despite reports of sexual risk and substance use behaviors, low rates of PrEP uptake among HIV-uninfected TG youth in the sample were found. While initial engagement in care was high for TG youth living with HIV (83.9%), medication adherence (55.0%), retention in care (66.1%), and viral suppression (65.6%) rates were suboptimal, yet comparable to other studies of people living with HIV, including youth [67], cisgender adults [68–71], and TG adults [1, 42]. Determinants of engagement in the HIV prevention continuum were older age, being a youth of color, having a history of homelessness, and gender affirmation and stigma in primary HIV prevention settings. Medical gender affirmation and stigma in HIV care emerged as factors associated with reduced retention in care and viral suppression (gender affirmation only). Findings highlight the importance of identifying the multiple factors that may shape care involvement for TG youth, including social determinants of health unique to TG youth such as gender affirmation and stigma.
TG youth reported variable levels of engagement in HIV prevention services. The majority of TG youth sampled (92.3%) had been tested for HIV in their lifetime, much higher than national estimates U.S. high school students [72]. This is likely due to the sampling method which recruited youth from the catchment areas of AMTU. Further, only 54.6% of HIV-uninfected or -unknown status TG youth had received primary HIV prevention services in their lifetime, suggesting a high level of lifetime testing, but lower levels of retesting and ongoing engagement in primary prevention services. TG youth also reported low uptake of biomedical HIV prevention services (e.g., 8.2% PrEP and 4.1% PEP). The low to moderate use of HIV prevention services among TG youth is problematic in light of the fact that 18.8–24.1% reported having unintended condomless vaginal or anal sex under the influence substances in the last 6 months. Given the success of biomedical interventions such as PrEP and PEP to prevent HIV in high-risk individuals [39], efforts are needed to educate TG youth and ensure access to HIV prevention interventions as indicated.
In examining factors associated with engagement in primary prevention several key patterns were observed. First, TG youth of color and homeless youth were most likely to be reached by recent primary HIV prevention services; this is encouraging given these are disparately affected populations of the HIV epidemic among youth in general [1]. Second, older age was associated with receipt of trans-friendly prevention services, highlighting the need for intervention efforts to reach individuals of younger ages. Third, both gender affirmative (i.e., felt supported in gender identity) and stigmatizing (i.e., treated negatively because of gender identity) experiences in primary HIV prevention and testing settings increased the odds of ever accessing HIV prevention services, and higher frequency of stigma in HIV prevention and testing contexts was inversely associated with endorsing receipt of trans-friendly HIV prevention services in the last 6 months. These findings underscore the complexity of factors involved in healthcare settings and service utilization for TG individuals [47], including mixed experiences of affirmation and stigma in healthcare. Concomitant affirmation-stigma experiences may occur from visit-to-visit, for example one visit may be more gender-affirming than another for TG youth. Such experiences may also occur within the same visit when interfacing with different prevention care staff and providers, or with administrative and reception staff. It may also be that some aspects of prevention services are gender-affirming (e.g., using the correct name and pronoun) while others are highly stigmatizing (e.g., assuming TM do not have sex with cisgender men, or using inappropriate terminology when discussing sexual risk behaviors). Gender affirmation and stigma are not opposites. Future research is needed to better understand how these multidimensional constructs can be most effectively levied and integrated into interventional research to optimize biobehavioral prevention services to TG youth.
Nearly a third of the sample was living with HIV infection (30.9%) and this occurred exclusively among TF youth. The 40.3% prevalence of HIV infection among of TF youth in the sample is much higher than the 21.7% laboratory-confirmed HIV prevalence (meta-analysis) among TF adults [12], yet comparable to the HIV prevalence observed among Black/African American TF adults across several studies [11.] Study recruitment involved targeted efforts to engage diverse TG youth in and out of services, including those living with HIV. This HIV prevalence estimate should therefore not be taken as a “true” TG youth population parameter. A significantly lower proportion TG youth living with HIV had affirmed their gender compared to HIV-uninfected/unknown status youth (35.7 vs. 56.6%); however, among those who had accessed some form of medical gender affirmation, a significantly higher proportion of HIV-infected TF youth had accessed hormones without a prescription compared to their HIV-uninfected/unknown status counterparts (60.0 vs. 28.9%). Taking hormones outside a physician’s care can pose health risks if taken in excess of recommended doses or if hormone syringes are contaminated with HIV [49]; thus, non-prescription hormone use may be a risk for HIV in TF. Consistent with prior research linking lower educational attainment and sex work history to HIV infection [23, 73], a lower of proportion of the TG youth living with HIV in our sample were current students and a higher proportion reported sex work in their lifetime relative to HIV-uninfected/unknown TG youth. These findings extend prior research with TF youth and adults and point to the need to target multilevel factors in HIV prevention activities for this vulnerable youth group [74].
Studies have consistently found that youth and young adults living with HIV are less likely to be retained in care, to be prescribed ART even though it is medically indicated, and to achieve viral suppression than adults [1, 68–71]. Among TF youth living with HIV sampled, 83.1% had been linked to care, 71.4% were retained in care and on ART, and 65.6% were known to be virally suppressed. Our finding that 42.9% of TF youth living with HIV in this sample did not know their current viral load suggests the need for improved patient education and interventional research to increase health literacy for TF youth living with HIV. The levels of engagement in care and viral suppression reported in this sample of TF youth is similar to that of TF adults sampled in San Francisco [29], yet suboptimal relative UNAIDS 90-90-90 targets [75]. Consistent with research conducted in TG adults [28, 42, 76], medication adherence and retention in care were also suboptimal as only 55.0% of those currently taking medications had been adherent in the past 7 days and 33.9% had missed one or more HIV care appointment in the past 6 months. Additionally, in multivariable models, medical gender affirmation was associated with reduced odds of virological suppression and with increased odds of missing appointments. These findings support qualitative research wherein TF adults expressed concern that their HIV medications may limit the benefits of hormones, leading some TF adults to prioritize gender affirmation treatment over HIV care [26]. It is also possible that some of the TF youth sampled were unable to obtain gender affirmation services at the same clinic where they receive HIV care. Accessing care in multiple locations may prove too burdensome for youth who already face a number of psychosocial and structural obstacles to healthcare engagement [77], leading some youth to further prioritize medical gender affirmation care over HIV treatment. Additional research is needed to replicate this finding and to understand gender affirmation alongside HIV care, including implementation and evaluation of models of co-located service delivery [31].
Experiencing stigma in HIV care was associated with poorer rates of retention in care, consistent with prior research supporting the detrimental effects of stigma on both general and HIV-related healthcare avoidance in TG adults [26, 43–46]. This is the first study to our knowledge to show that experiencing transgender stigma while receiving HIV care is associated with reduced retention rates for TG youth living with HIV, specifically. While receiving gender affirmative care has been shown to facilitate primary and HIV care engagement for TG adults living with HIV [26], across multivariable models, having received gender affirmative HIV care was not associated with use of secondary prevention services, medication adherence, viral suppression, or retention in care. While it is possible that medical gender affirmation may facilitate care engagement and associated health outcomes in TG youth living with HIV, this study’s findings suggest that experiencing stigma in HIV care may be a stronger predictor of HIV care retention and viral suppression than receiving gender affirming HIV care. Future longitudinal, mixed methods research is needed to identify and understand facilitators and barriers to HIV care retention and support the development of intervention strategies to improve future care engagement and, ultimately, HIV outcomes.
Several limitations should be noted. First, this study relied on convenience sampling to recruit TG youth from 14 geographically diverse U.S. cities. Thus, potential biases inherent in non-probability sampling methods apply to this study [78]. While we were able to recruit a diverse sample with respect to age, race, ethnicity, SES, gender identity, and HIV status, this is a relatively small sample size for a national study. Furthermore, findings may not be generalizable to all TG youth, including those in other urban areas, as well as in small towns and rural areas. Although AMTU clinics and hospitals often serve a large catchment area, recruitment efforts and study visits held at AMTU may have resulted in a sample with higher HIV prevalence than a general population sample of TG youth. However, the distribution of HIV in the sample is also evidence of the success of the community-engaged approach and participatory collaboration that was implemented by the study team and TG community members to recruit and enroll a sample of diverse TG youth. Second, laboratory biomarker data were not available for this study. Third, the survey relied on self-report, which likely under-estimated the prevalence of healthcare utilization and related-outcomes; however, the use of computer-assisted self-interview may have minimized social desirability bias and led to more accurate reporting of sensitive data. Fourth, limitations pertain to sexual risk data presented. The reporting of transgender as a catch-all gender category for sexual partners without distinguishing subgroups (e.g., TM and TF) and not disaggregating sexual risk by HIV serostatus of sexual partners may obfuscate important differences relevant for understanding HIV transmission risk dynamics. Similarly, data on condomless anal sex for sexual risk assessment without rates of condomless vaginal sex is a limitation, especially for TF youth who may have had genital affirmation surgery (e.g., vaginoplasty) and may acquire or transmit HIV infection via vaginal intercourse. Lastly, given the sample size, and the constraints of survey research to collect data on every possible confounder, it was not possible to adjust for all potential confounders in multivariable models. Future research involving larger samples of at-risk TG youth and TG youth living with HIV is needed to continue to characterize the health and healthcare of this vulnerable youth population. Limitations notwithstanding, this is one of the first studies to our knowledge to characterize the HIV prevention and care continua among a diverse sample of U.S. TF and TM youth with varied gender identities, including those identified as binary and nonbinary.
Conclusions
Incomplete knowledge about the health of diverse TG youth impedes their inclusion in the U.S. public health agenda [9,] including national public health efforts to address the HIV epidemic. The present study identified multiple individual, interpersonal, and structural factors associated with HIV infection, use of HIV prevention services, engagement in HIV care, and HIV-related health outcomes for a sample TG youth. This research underscores the need to engage and retain TG youth across the HIV prevention and care continua is order to curb rising rates of HIV infection and improve the health outcomes of TG youth living with HIV. Even in the catchment areas of clinical sites and centers specializing in HIV care, TG youth have unmet needs pertaining to HIV services and transgender-specific social determinants which influence engagement in care. Multilevel intervention efforts that aim educate TG youth about their HIV risks and facilitate access to prevention and HIV care services, reduce stigma in healthcare through provider cultural and clinical competency training, and improve TG youth access to integrated gender affirmation and HIV care services may help to improve engagement in HIV prevention and treatment services, and ultimately the health of TG youth. Studies that seek to identify and leverage existing resiliencies among TG youth represent a way forward to inform interventions to improve HIV prevention, testing, and treatment engagement for TG youth. Community-engagement is a critical component of any efforts that seek to improve HIV prevention and care continua among TG youth, including in clinical care settings. For TG youth, it is critical to target individual, interpersonal, and structural-level factors in interventions that not only buffer against poor HIV-related outcomes, but which also capitalize on resiliencies to positively impact HIV-related health of TG individual youth and communities.
Acknowledgments
We would also like to thank the following individuals, groups, and entities for their contributions to this study: Elliot Popoff and Bré Anne Campbell, University of Michigan research staff who made this study possible. The investigators and staff at the following sites that participated in this study: University of South Florida, Tampa (Emmanuel, Straub, Bruce, Kerr), Children’s Hospital of Los Angeles (Belzer, Tucker, Franco), Children’s National Medical Center (D’Angelo, Trexler, Carr, Sinkfield), Children’s Hospital of Philadelphia (Douglas, Tanney, DiBenedetto, Franklin, Smith), John H. Stroger Jr. Hospital of Cook County and the Ruth M. Rothstein CORE Center (Henry-Reid, Bojan, Balthazar), Montefiore Medical Center (Futterman, Campos, Wesp, Nazario, Reopell), Tulane University Health Sciences Center (Abdalian, Kozina, Baker, Wilkes), University of Miami School of Medicine (Friedman, Maturo), St. Jude’s Children’s Research Hospital (Gaur, Flynn, Dillard, Hurd-Sawyer), Baylor College of Medicine (Paul, Head, Sierra), Wayne State University (Secord, Cromer, Walters, Houston), Johns Hopkins University (George-Agwu, Anderson, Worrel-Thorne), Fenway Institute (Mayer, Dormitzer, Massaquoi, Gelman), University of Colorado Denver (Reirden, Hahn, Bernath). Network, scientific and logistical support was provided by the ATN Coordinating Center (C. Wilson, C. Partlow) at The University of Alabama at Birmingham and the ATN 130 protocol team. Network operations and data management support was provided by the ATN Data and Operations Center at Westat, Inc. (G. Price). The authors are grateful to the members of the Affirming Voices for Action (AVA) Youth Advisory Board for their insight and guidance. We would like to thank the trans* youth who raised their voices and shared their experiences with us. We hear you.
Funding This work was supported by The Adolescent Medicine Trials Network for HIV/AIDS Interventions (ATN) from the National Institutes of Health [U01 HD 040533 and U01 HD 040474] through the National Institute of Child Health and Human Development (B. Kapogiannis, S. Lee), with supplemental funding from the National Institutes on Drug Abuse and Mental Health. Dr. Gary Harper was the Protocol Chair (PI) of ATN 130: Assessing the Engagement of Gender Minority Youth Across the HIV Continuum of Care. Protocol Vice-Chairs (Co-Is) were Dr. Sari Reisner, Miguel Martinez, and Liza Salomon. The views and opinions expressed in this report are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the U.S. Government.
Footnotes
Compliance with Ethical Standards
All study activities were approved at the Institutional Review Boards at the 14 Adolescent Medicine Trials Unit (AMTU) sites, as well as investigators’ institutions.
Conflicts of interest The authors have no relevant conflicts of interest to disclose.
Ethical Approval All procedures performed in this study involving human participants were in accordance with the ethical standards of the Institutional Review Boards at the 14 participating sites, as well as with the investigators’ institutions, including with the 1964 Helsinki Declaration and its later amendments and ethical standards.
Informed Consent Informed consent was obtained from all individuals participants included in the study.
References
- 1.Centers for Disease Control and Prevention. [Accessed 25 Jan 2017];HIV Among Youth. 2016 https://www.cdc.gov/hiv/group/age/youth/
- 2.McNairy ML, El-Sadr WM. A paradigm shift: focus on the HIV prevention continuum. Clin Infect Dis. 2014;59:S12–5. doi: 10.1093/cid/ciu251. https://doi.org/10.1093/cid/ciu251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bradley H, Hall HI, Wolitski RJ, et al. Vital signs: HIV diagnosis, care, and treatment among persons living with HIV–United States, 2011. MMWR. 2014;63(47):1113–17. [PMC free article] [PubMed] [Google Scholar]
- 4.Horn T, Sherwood J, Remien RH, Nash D, Auerbach J. Towards an integrated primary and secondary HIV prevention continuum for the United States: a cyclical process model. J Int AIDS Soc. 2016;19(1):21263. doi: 10.7448/IAS.19.1.21263. https://doi.org/10.7448/ias.19.1.21263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Health Resources and Services Administration. National HIV/AIDS Strategy for the United States: Updated to 2020. Washington: 2015. [Google Scholar]
- 6.Zanoni BC, Mayer KH. The adolescent and young adult HIV cascade of care in the United States: exaggerated health disparities. AIDS Pat Care STDS. 2014;28(3):128–35. doi: 10.1089/apc.2013.0345. https://doi.org/10.1089/apc.2013.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.The Health of Lesbian, Gay, Bisexual, and Transgender People: Building a Foundation for Better Understanding. Washington, DC: 2011. https://iom.nationalacademies.org/Reports/2011/The-Health-of-Lesbian-Gay-Bisexual-and-Transgender-People.aspx. [PubMed] [Google Scholar]
- 8.Shields JP, Cohen R, Glassman JR, Whitaker K, Franks H, Bertolini I. Estimating population size and demographic characteristics of lesbian, gay, bisexual, and transgender youth in middle school. J Adolesc Health. 2013;52(2):248–50. doi: 10.1016/j.jadohealth.2012.06.016. https://doi.org/10.1016/j.jadohealth.2012.06.016. [DOI] [PubMed] [Google Scholar]
- 9.Conron KJ, Landers SJ, Reisner SL, Sell RL. Sex and gender in the US health surveillance system: a call to action. Am J Public Health. 2014;104(6):970–6. doi: 10.2105/AJPH.2013.301831. https://doi.org/10.2105/AJPH.2013.301831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Flores A, Brown TM, Herman J. How Many adults identify as transgender in the United States. Los Angeles: Williams Institute UCLA School of Law; 2016. [Google Scholar]
- 11.Herbst JH, Jacobs ED, Finlayson TJ, et al. Estimating HIV prevalence and risk behaviors of transgender persons in the United States: a systematic review. AIDS Behav. 2008;12(1):1–17. doi: 10.1007/s10461-007-9299-3. https://doi.org/10.1007/s10461-007-9299-3. [DOI] [PubMed] [Google Scholar]
- 12.Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214–22. doi: 10.1016/S1473-3099(12)70315-8. https://doi.org/10.1016/S1473-3099(12)70315-8. [DOI] [PubMed] [Google Scholar]
- 13.Schulden JD, Song B, Barros A, et al. Rapid HIV testing in transgender communities by community-based organizations in three cities. Public Health Rep. 2008;3:101–14. doi: 10.1177/00333549081230S313. https://doi.org/10.1177/00333549081230S313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Reisner SL, Murchison GR. A global research synthesis of HIV and STI biobehavioural risks in female-to-male transgender adults. Glob Public Health. 2016;11(7–8):866–87. doi: 10.1080/17441692.2015.1134613. https://doi.org/10.1080/17441692.2015.1134613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stephens SC, Bernstein KT, Philip SS. Male to female and female to male transgender persons have different sexual risk behaviors yet similar rates of STDs and HIV. AIDS Behav. 2011;15(3):683–96. doi: 10.1007/s10461-010-9773-1. https://doi.org/10.1007/s10461-010-9773-1. [DOI] [PubMed] [Google Scholar]
- 16.Scheim AI, Bauer GR, Travers R. HIV-related sexual risk among transgender men who are gay, bisexual, or have sex with men. JAIDS J Acquir Immune Defic Syndr. 2017;74(4):e89–e96. doi: 10.1097/QAI.0000000000001222. https://doi.org/10.1097/QAI.0000000000001222. [DOI] [PubMed] [Google Scholar]
- 17.Rowniak S, Chesla C, Rose CD, Holzemer WL. Transmen: the HIV risk of gay identity. AIDS Educ Prev. 2011;23(6):508–20. doi: 10.1521/aeap.2011.23.6.508. https://doi.org/10.1521/aeap.2011.23.6.508. [DOI] [PubMed] [Google Scholar]
- 18.Sevelius J. There’s no pamphlet for the kind of sex I have: HIV-related risk factors and protective behaviors among transgender men who have sex with nontransgender men. J Assoc Nurses AIDS Care. 2009;20(5):398–410. doi: 10.1016/j.jana.2009.06.001. https://doi.org/10.1016/j.jana.2009.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Reisner SL, Perkovich B, Mimiaga MJ. A mixed methods study of the sexual health needs of New England transmen who have sex with nontransgender men. AIDS Patient Care STDS. 2010;24(8):501–13. doi: 10.1089/apc.2010.0059. https://doi.org/10.1089/apc.2010.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Clark H, Babu AS, Wiewel EW, Opoku J, Crepaz N. Diagnosed HIV infection in transgender adults and adolescents: results from the National HIV Surveillance System, 2009–2014. AIDS Behav. 2016 doi: 10.1007/s10461-016-1656-7. https://doi.org/10.1007/s10461-016-1656-7. [DOI] [PMC free article] [PubMed]
- 21.Wilson EC, Chen Y-H, Arayasirikul S, et al. Differential HIV risk for racial/ethnic minority transfemale youths and socioeconomic disparities in housing, residential stability, and education. Am J Public Health. 2015;105:e41–7. doi: 10.2105/AJPH.2014.302443. https://doi.org/10.2105/AJPH.2014.302443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reisner SL, Vetters R, White JM, et al. Laboratory-confirmed HIV and sexually transmitted infection seropositivity and risk behavior among sexually active transgender patients at an adolescent and young adult urban community health center. AIDS Care. 2015;27(8):1031–36. doi: 10.1080/09540121.2015.1020750. https://doi.org/10.1080/09540121.2015.1020750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garofalo R, Deleon J, Osmer E, Doll M, Harper GW. Overlooked, misunderstood and at-risk: exploring the lives and HIV risk of ethnic minority male-to-female transgender youth. J Adolesc Health. 2006;38(3):230–6. doi: 10.1016/j.jadohealth.2005.03.023. https://doi.org/10.1016/j.jadohealth.2005.03.023. [DOI] [PubMed] [Google Scholar]
- 24.Brennan J, Kuhns LM, Johnson AK, et al. Syndemic theory and HIV-related risk among young transgender women: the role of multiple, co-occurring health problems and social marginalization. Am J Public Health. 2012;102(9):1751–7. doi: 10.2105/AJPH.2011.300433. https://doi.org/10.2105/AJPH.2011.300433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dowshen N, Matone M, Luan X, et al. Behavioral and health outcomes for HIV+ young transgender women (YTW) linked to and engaged in medical care. LGBT Heal. 2016;3(2):162–7. doi: 10.1089/lgbt.2014.0062. https://doi.org/10.1089/lgbt.2014.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sevelius JM, Patouhas E, Keatley JG, Johnson MO. Barriers and facilitators to engagement and retention in care among transgender women living with Human Immunodeficiency Virus. Ann Behav Med. 2014;47(1):5–16. doi: 10.1007/s12160-013-9565-8. https://doi.org/10.1007/s12160-013-9565-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doshi RK, Milberg J, Isenberg D, et al. High rates of retention and viral suppression in the US HIV safety net system: HIV care continuum in the Ryan White HIV/AIDS Program, 2011. Clin Infect Dis. 2015;60(1):117–25. doi: 10.1093/cid/ciu722. https://doi.org/10.1093/cid/ciu722. [DOI] [PubMed] [Google Scholar]
- 28.Baguso GN, Gay CL, Lee KA. Medication adherence among transgender women living with HIV. AIDS Care. 2016;28(8):976–81. doi: 10.1080/09540121.2016.1146401. https://doi.org/10.1080/09540121.2016.1146401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Santos G-M, Wilson EC, Rapues J, Macias O, Packer T, Raymond HF. HIV treatment cascade among transgender women in a San Francisco respondent driven sampling study. Sex Transm Infect. 2014;90(5):430–3. doi: 10.1136/sextrans-2013-051342. https://doi.org/10.1136/sextrans-2013-051342. [DOI] [PubMed] [Google Scholar]
- 30.Reisner SL, Poteat T, Keatley J, et al. Global health burden and needs of transgender populations: a review. Lancet. 2016;388(10042):412–36. doi: 10.1016/S0140-6736(16)00684-X. https://doi.org/10.1016/S0140-6736(16)00684-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Reisner SL, Radix A, Deutsch MB. Integrated and gender-affirming transgender clinical care and research. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S235–42. doi: 10.1097/QAI.0000000000001088. https://doi.org/10.1097/QAI.0000000000001088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White Hughto JM, Reisner SL. A systematic review of the effects of hormone therapy on psychological functioning and quality of life in transgender individuals. Transgender Health. 2016;1(1):21–31. doi: 10.1089/trgh.2015.0008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Murad MH, Elamin MB, Garcia MZ, et al. Hormonal therapy and sex reassignment: a systematic review and meta-analysis of quality of life and psychosocial outcomes. Clin Endocrinol. 2010;72(2):214–31. doi: 10.1111/j.1365-2265.2009.03625.x. https://doi.org/10.1111/j.1365-2265.2009.03625.x. [DOI] [PubMed] [Google Scholar]
- 34.Shumer DE, Nokoff NJ, Spack NP. Advances in the care of transgender children and adolescents. Adv Pediatr. 2016;63(1):79–102. doi: 10.1016/j.yapd.2016.04.018. https://doi.org/10.1016/j.yapd.2016.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olson J, Forbes C, Belzer M. Management of the transgender adolescent. Arch Pediatr Adolesc Med. 2011;165(2):111–28. doi: 10.1001/archpediatrics.2010.275. https://doi.org/10.1001/archpediatrics.2010.275. [DOI] [PubMed] [Google Scholar]
- 36.Olson-Kennedy J, Cohen-Kettenis PT, Kreukels BPC, et al. Research priorities for gender nonconforming/transgender youth: gender identity development and biopsychosocial outcomes. Curr Opin Endocrinol Diabetes Obes. 2016;23(2):172–9. doi: 10.1097/MED.0000000000000236. https://doi.org/10.1097/MED.0000000000000236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sevelius JM, Deutsch MB, Grant R. The future of PrEP among transgender women: the critical role of gender affirmation in research and clinical practices. J Int AIDS Soc. 2016;19(7) Suppl 6:21105. doi: 10.7448/IAS.19.7.21105. https://doi.org/10.7448/IAS.19.7.21105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sevelius JM. Gender affirmation: a framework for conceptualizing risk behavior among transgender women of color. Sex Roles. 2013;68(11–12):675–89. doi: 10.1007/s11199-012-0216-5. https://doi.org/10.1007/s11199-012-0216-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Deutsch MB, Glidden DV, Sevelius J, et al. HIV pre-exposure prophylaxis in transgender women: a subgroup analysis of the iPrEx trial. Lancet HIV. 2015;2(12):e512–9. doi: 10.1016/S2352-3018(15)00206-4. https://doi.org/10.1016/S2352-3018(15)00206-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Glynn TR, Gamarel KE, Kahler CW, Iwamoto M, Operario D, Nemoto T. The role of gender affirmation in psychological well-being among transgender women. Psychol Sex Orientat Gend Divers. 2016;3(3):336–44. doi: 10.1037/sgd0000171. https://doi.org/10.1037/sgd0000171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Reisner SL, White Hughto JM, Pardee D, Sevelius J. Syndemics and gender affirmation: HIV sexual risk in female-to-male trans masculine adults reporting sexual contact with cisgender males. Int J STD AIDS. 2015;11:955–66. doi: 10.1177/0956462415602418. https://doi.org/10.1177/0956462415602418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Radix A, Sevelius J, Deutsch MB. Transgender women, hormonal therapy and HIV treatment: a comprehensive review of the literature and recommendations for best practices. J Int AIDS Soc. 2016;19(3 Suppl 2):20810. doi: 10.7448/IAS.19.3.20810. https://doi.org/10.7448/IAS.19.3.20810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Reisner SL, Pardo ST, Gamarel KE, White Hughto JM, Pardee DJ, Keo-Meier CL. Substance use to cope with stigma in healthcare among US female-to-male trans masculine adults. LGBT Heal. 2015;2(4):324–32. doi: 10.1089/lgbt.2015.0001. https://doi.org/10.1089/lgbt.2015.0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Reisner SL, White Hughto JM, Dunham EE, et al. Legal protections in public accommodations settings: a critical public health issue for transgender and gender-nonconforming people. Milbank Q. 2015;93(3):484–515. doi: 10.1111/1468-0009.12127. https://doi.org/10.1111/1468-0009.12127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.White Hughto JM, Murchison GR, Clark K, Pachankis JE, Reisner SL. Geographic and individual differences in healthcare access for U.S. transgender adults: a multilevel analysis. LGBT Heal. 2016;3(6):424–33. doi: 10.1089/lgbt.2016.0044. https://doi.org/10.1089/lgbt.2016.0044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.White Hughto JM, Rose AJ, Pachankis JE, Reisner SL. Barriers to gender transition-related healthcare: identifying under-served transgender adults in Massachusetts. Transgender Health. 2017;2(1):107–118. doi: 10.1089/trgh.2017.0014. https://doi.org/10.1089/trgh.2017.0014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Poteat T, German D, Kerrigan D. Managing uncertainty: a grounded theory of stigma in transgender health care encounters. Soc Sci Med. 2013;84:22–9. doi: 10.1016/j.socscimed.2013.02.019. https://doi.org/10.1016/j.socscimed.2013.02.019. [DOI] [PubMed] [Google Scholar]
- 48.Bockting WO, Miner MH, Swinburne Romine RE, Hamilton A, Coleman E. Stigma, mental health, and resilience in an online sample of the US transgender population. Am J Public Health. 2013;103(5):943–51. doi: 10.2105/AJPH.2013.301241. https://doi.org/10.2105/AJPH.2013.301241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.White Hughto JM, Reisner SL, Pachankis JE. Transgender stigma and health: a critical review of stigma determinants, mechanisms, and interventions. Soc Sci Med. 2015;147:222–31. doi: 10.1016/j.socscimed.2015.11.010. https://doi.org/10.1016/j.socscimed.2015.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Rowe C, Santos G-M, McFarland W, Wilson EC. Prevalence and correlates of substance use among trans female youth ages 16–24 years in the San Francisco Bay Area. Drug Alcohol Depend. 2015;147:160–6. doi: 10.1016/j.drugalcdep.2014.11.023. https://doi.org/10.1016/j.drugalcdep.2014.11.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hotton AL, Garofalo R, Kuhns LM, Johnson AK. Substance use as a mediator of the relationship between life stress and sexual risk among young transgender women. AIDS Educ Prev. 2013;25(1):62–71. doi: 10.1521/aeap.2013.25.1.62. https://doi.org/10.1521/aeap.2013.25.1.62. [DOI] [PubMed] [Google Scholar]
- 52.Centers for Disease Control and Prevention. [Accessed 25 Jan 2017];HIV Among Transgender People. 2016 https://www.cdc.gov/hiv/group/gender/transgender/
- 53.Hendricks ML, Testa RJ. A conceptual framework for clinical work with transgender and gender nonconforming clients: an adaptation of the Minority Stress Model. Prof Psychol Res Pract. 2012;43(5):460–7. http://dx.doi.org/10.1037/a0029597. [Google Scholar]
- 54.Baral S, Logie CH, Grosso A, Wirtz AL, Beyrer C. Modified social ecological model: a tool to guide the assessment of the risks and risk contexts of HIV epidemics. BMC Public Health. 2013;13(1):482. doi: 10.1186/1471-2458-13-482. https://doi.org/10.1186/1471-2458-13-482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Israel BA, Krieger J, Vlahov D, et al. Challenges and facilitating factors in sustaining community-based participatory research partnerships: lessons learned from the Detroit, New York City and Seattle Urban Research Centers. J Urban Health. 2016;83(6):1022–40. doi: 10.1007/s11524-006-9110-1. https://doi.org/10.1007/s11524-006-9110-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Wallerstein NB, Duran B. Using community-based participatory research to address health disparities. Health Promot Pract. 2006;7(3):312–23. doi: 10.1177/1524839906289376. https://doi.org/10.1177/1524839906289376. [DOI] [PubMed] [Google Scholar]
- 57.Reisner S, Keatley J, Baral S, et al. Transgender community voices: a participatory population perspective. Lancet. 2016;388(10042):327–30. doi: 10.1016/S0140-6736(16)30709-7. https://doi.org/10.1016/S0140-6736(16)30709-7. [DOI] [PubMed] [Google Scholar]
- 58.Harper GW, Willard N, Ellen JM. Adolescent Medicine Trials Network for HIV/AIDS Interventions. Connect to Protect®: utilizing community mobilization and structural change to prevent HIV infection among youth. J Prev Interv Commun. 2012;40(2):81–6. doi: 10.1080/10852352.2012.660119. https://doi.org/10.1080/10852352.2012.660119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Siskind RL, Andrasik M, Karuna ST, et al. Engaging transgender people in NIH-funded HIV/AIDS clinical trials research. J Acquir Immune Defic Syndr. 2016;72(Suppl 3):S243–7. doi: 10.1097/QAI.0000000000001085. https://doi.org/10.1097/QAI.0000000000001085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Reisner SL, Conron KJ, Tardiff LA, Jarvi S, Gordon AR, Austin SB. Monitoring the health of transgender and other gender minority populations: validity of natal sex and gender identity survey items in a US national cohort of young adults. BMC Public Health. 2017;14:1224. doi: 10.1186/1471-2458-14-1224. https://doi.org/10.1186/1471-2458-14-1224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shaffer HJ. A new brief screen for adolescent substance abuse. Arch Pediatr Adolesc Med. 1999;153(6):591–6. doi: 10.1001/archpedi.153.6.591. [DOI] [PubMed] [Google Scholar]
- 62.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156(6):607–14. doi: 10.1001/archpedi.156.6.607. [DOI] [PubMed] [Google Scholar]
- 63.Hosek SG, Harper GW, Domanico R. Predictors of medication adherence among HIV-infected youth. Psychol Health Med. 2005;10(2):166–79. doi: 10.1080/1354350042000326584. https://doi.org/10.1080/1354350042000326584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sikkema KJ, Hansen NB, Kochman A, et al. The development and feasibility of a brief risk reduction intervention for newly HIV-diagnosed men who have sex with men. J Commun Psychol. 2011;39(6):717–32. doi: 10.1002/jcop.20463. https://doi.org/10.1002/jcop.20463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Harper GW, Jadwin-Cakmak L, Reisner S, et al. Exploring utilization of HIV-related services and care among transgender and other gender minority youth in the U.S. National Transgender Health Summit. Oakland: 2015. [Google Scholar]
- 66.Hosmer DJ, Lemeshow SSR. Applied logistic regression. Hoboken: Wiley; 2013. [Google Scholar]
- 67.Ferrand RA, Briggs D, Ferguson J, et al. Viral suppression in adolescents on antiretroviral treatment: review of the literature and critical appraisal of methodological challenges. Trop Med Int Health. 2016;21(3):325–33. doi: 10.1111/tmi.12656. https://doi.org/10.1111/tmi.12656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Agwu AL, Fleishman JA, Korthuis PT, et al. Disparities in antiretroviral treatment: a comparison of behaviorally HIV-infected youth and adults in the HIV Research Network. J Acquir Immune Defic Syndr. 2011;58(1):100–7. doi: 10.1097/QAI.0b013e31822327df. https://doi.org/10.1097/QAI.0b013e31822327df. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Althoff KN, Rebeiro P, Brooks JT, et al. Disparities in the quality of HIV care when using US department of health and human services indicators. Clin Infect Dis. 2014;58(8):1185–9. doi: 10.1093/cid/ciu044. https://doi.org/10.1093/cid/ciu044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ulett KB, Willig JH, Lin H-Y, et al. The therapeutic implications of timely linkage and early retention in HIV care. AIDS Patient Care STDS. 2009;23(1):41–9. doi: 10.1089/apc.2008.0132. https://doi.org/10.1089/apc.2008.0132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Whiteside YO, Cohen SM, Bradley H, et al. Progress along the continuum of HIV care among blacks with diagnosed HIV- United States, 2010. MMWR Morb Mortal Wkly Rep. 2014;63(5):85–9. [PMC free article] [PubMed] [Google Scholar]
- 72.Kann L, McManus T, Harris W, et al. Youth Risk Behavior Surveillance-United States, 2013. Morbidity and Mortality Weekly Report. 2014;63:SS-4. [PubMed] [Google Scholar]
- 73.Operario D, Soma T, Underhill K. Sex work and HIV status among transgender women: systematic review and meta-analysis. J Acquir Immune Defic Syndr. 2008;48(1):97–103. doi: 10.1097/QAI.0b013e31816e3971. https://doi.org/10.1097/QAI.0b013e31816e3971. [DOI] [PubMed] [Google Scholar]
- 74.Poteat T, Wirtz AL, Radix A, et al. HIV risk and preventive interventions in transgender women sex workers. Lancet. 2015;385(9964):274–86. doi: 10.1016/S0140-6736(14)60833-3. https://doi.org/10.1016/S0140-6736(14)60833-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.UNAIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. Geneva: 2014. [Google Scholar]
- 76.Stone VE. Optimizing the care of minority patients with HIV/AIDS. Clin Infect Dis. 2004;38(3):400–4. doi: 10.1086/380969. https://doi.org/10.1086/380969. [DOI] [PubMed] [Google Scholar]
- 77.Greifinger R, Batchelor M, Fair C. Improving engagement and retention in adult care settings for lesbian, gay, bisexual, transgender and questioning (LGBTQ) youth living with HIV: recommendations for health care providers. J Gay Lesbian Ment Health. 2013;17(1):80–95. http://dx.doi.org/10.1080/19359705.2013.739533. [Google Scholar]
- 78.Bauer GR, Scheim AI. Sampling bias in transgender studies. Lancet Infect Dis. 2013;13(10):832. doi: 10.1016/S1473-3099(13)70242-1. https://doi.org/10.1016/S1473-3099(13)70242-1. [DOI] [PubMed] [Google Scholar]