Abstract
Background
Although psoriasis is universal in its occurrence worldwide, its prevalence varies by geographic location and race. A few hospital-based surveys have reported on the demographic characteristics in Korean patients with psoriasis. However, a nation-wide study on the prevalence of psoriasis in Korea remains uncompleted.
Objective
The purpose of this study was to determine the prevalence of psoriasis in Korea and to describe the demographic and social characteristics of afflicted individuals.
Methods
We identified patients with psoriasis using a relevant diagnostic code from the sixth revision of the Korean Standard Classification of Disease in the 2011~2015 claims database of the Health Insurance Review and Assessment Service of Korea. We estimated the annual prevalence of psoriasis and described the age and sex distribution of the patients, type and severity of psoriasis, comorbidities, type of health insurance, type of health-care institution and residence area. Patients with moderate-to-severe psoriasis were defined as those who had been treated with phototherapy, classical systemic agents, and/or biologic agents.
Results
The standardized prevalence of psoriasis was 453 per 100,000 individuals of the database population in 2015. We found male preponderance with a 1.3:1 male-to-female ratio, and that the largest number of patients belonged to the age group of 50s. Of the patients diagnosed with psoriasis in 2015, 83.8% had plaque psoriasis and 22.6% had moderate-to-severe psoriasis.
Conclusion
The annual standardized prevalence of psoriasis in Korea was 453 per 100,000 of the population in 2015.
Keywords: Demography, National health programs, Prevalence, Psoriasis
INTRODUCTION
Psoriasis is a skin disease with a chronic relapsing course that is clinically characterized by erythematous scaly plaque. Although it is globally universal in occurrence, its prevalence varies by geographic location and race1. Generally, psoriasis is more common in Caucasians than in those of African or Asian descent. In northern Europe, about 2%~3% of the population is known to be psoriasis patients. In the United States, the prevalence was reported to be 2.5% in Caucasian Americans and only 1.3% in African-Americans2. The prevalence in Asians is also estimated to be low, it ranges from 0.29% to 1.18% in Japan and from 0.2% to 1.5% in Chinese population1. However, to date, large-scale epidemiological studies of psoriatic patients have predominantly been conducted in Western countries, with few large-scale epidemiological studies on Asians in existence.
In Korea, most of the available previous studies on the clinical characteristics of psoriasis have been performed by tertiary referral hospitals at a single or multiple sites, and contain the possibility of selection bias and therefore cannot provide a clear idea on the prevalence of the disease. The lack of nation-wide research is an obstacle to estimating the exact prevalence and other epidemiological characteristics of psoriasis, including the male-to-female ratio and the age distribution of the patients. However, obtaining precise and detailed epidemiological data is essential to understand the nature of disease and develop appropriate health policies.
The purpose of this study was to investigate the prevalence of psoriasis and describe demographic and social characteristics of psoriasis patients in Korea using Health Insurance Review and Assessment Service (HIRA) data from 2011 to 2015. Since all people in Korea are obligated to join the National Health Insurance (NHI) Program and information on their visits to health institutions and insurance claims are stored in this system, HIRA data is appropriate as means to obtain a national level of epidemiological information on psoriasis.
MATERIALS AND METHODS
Data source
We used insurance claims data from 2011 to 2015 provided by the HIRA in Korea. The HIRA is Korea's NHI system's data repository, in which all residents of the country must be enrolled. Thus, the HIRA database contains the details of patient demographics, diagnoses, medications and medical services as noted in insurance claims made following patients' reception of medical services in all types of medical institutions.
Study population
In this study, the study population included all individuals who had an outpatient visit or admission history with a primary diagnostic code of psoriasis in accordance with the 6th revision of the Korean Standard Classification of Disease (KCD-6), which is modified from the 10th revision of the International Classification of Diseases (ICD-10). The primary diagnostic code is made for the disease for which the resources are consumed majorly. The study population was further classified into those with plaque psoriasis (L40.0, L40.8, and L40.9), guttate psoriasis (L40.4), palmoplantar pustulosis (L40.2 and L40.3), generalized pustular psoriasis (L40.1), and psoriatic arthritis (L40.5, M07.0~M07.3, and M09.0) according to the KCD-6. In addition, patients with mild-to-moderate psoriasis were defined as those who had been treated with phototherapy, acitretin, cyclosporine, methotrexate and/or biologic agents such as tumor necrosis factor-alpha inhibitors and interleukin-12/23 inhibitors, while the others were defined as those with mild psoriasis. In addition, we collected on patients who had at least one claim with a diagnosis of diabetes mellitus (E11 and E11.0~E11.9), dyslipidemia (E78 and E78.0~E78.9), hypertension (I10), cardiovascular (CV) diseases (I20~I25), cerebral infarction (I63), non-alcoholic fatty liver (K76.0), Crohn's disease (K50, K50.0 and K50.9), and/or malignancy including in situ neoplasm (C00~C97 and D00~D09).
Prevalence of psoriasis
Adopting the concept of period prevalence, we calculated the annual prevalence because it is not only more easily applicable to the HIRA database, but also more suitable for the interpretation of changes in time series, as compared with point prevalence or lifetime prevalence. The standardized prevalence was obtained by adjusting to the standard population data from the Korean Statistical Information Service in Korea National Statistical Office. For the comparison with world population, it was also standardized to the standard population data of Organization for Economic Co-operation and Development (OECD) and World Health Organization (WHO) countries. Prevalence rates were presented as the annual number per 100,000 members of the population.
Demographic and social characteristics of the patients with psoriasis
Frequency analyses were performed to describe patient sex and age group, type and severity of psoriasis, comorbidities, type of health insurance (NHI or Medical Aid), type of health-care institution (office-based physician practice, hospital, general hospital or tertiary teaching hospital) and residence area (metropolitan city, city and county, or rural place). In addition, we compared the patients with moderate-to-severe psoriasis with those with mild psoriasis.
Statistical analysis
To compare clinical and socioeconomic factors between patients with moderate-to-severe and with mild psoriasis, we conducted multiple logistic regression with moderate-to-severe psoriasis as the dependent variable. The relative risks of moderate-to-severe psoriasis as compared with mild psoriasis were presented as an adjusted odds ratio (aOR) with 95% confidence interval. All analyses were performed with SAS Enterprise Guide (SAS Institute, Inc., Cary, NC, USA). All statistical tests were two-sided, and a p-value<0.05 was considered statistically significant.
RESULTS
Prevalence of psoriasis
The crude and standardized prevalence of psoriasis, respectively, in Korea are summarized in Table 1. Notably, over the past five years, the crude prevalence for psoriasis stabilized, but with a slight increase. As of 2015, there were 233,909 Korean patients with psoriasis, which included, for crude prevalence, 459 per 100,000. After adjusting for age and sex, the standardized prevalence of psoriasis was 453 per 100,000 of the population. For the comparison with worldwide population, the standardized prevalence to OECD and WHO populations were calculated to be 443 and 391 per 100,000 in 2015, respectively.
Table 1. Prevalence of psoriasis in Korea between 2011 and 2015 (per 100,000 persons).
| Year | Crude prevalence | Standardized prevalence (Korea) | Standardized prevalence (OECD) | Standardized prevalence (WHO) |
|---|---|---|---|---|
| 2011 | 438 | 444 | 437 | 389 |
| 2012 | 440 | 444 | 435 | 386 |
| 2013 | 453 | 453 | 445 | 394 |
| 2014 | 457 | 454 | 445 | 394 |
| 2015 | 459 | 453 | 443 | 391 |
OECD: Organization for Economic Co-operation and Development, WHO: World Health Organization.
Demographic and social characteristics of the patients with psoriasis
The annual population of psoriasis patients presented similar patterns of demographic and social characteristics over the past five years (Table 2). As of 2015, the male-to-female ratio was approximately 1.3:1 among patients with psoriasis. The largest subgroup by age was patients in their 50s, followed by those in the 40s and 30s. Of the patients with psoriasis, 77.4% were classified into the mild group, while 22.6% were placed in the moderate-to-severe group. Regarding the type of psoriasis, plaque psoriasis and palmoplantar pustulosis were seen in 83.8% and 11.2% of the patients, respectively. In addition, 27.2% of psoriasis patients had one or more comorbid diseases including diabetes mellitus, dyslipidemia, hypertension, cerebral vascular disorders, ischemic heart disease, Crohn's disease, fatty liver, and malignancies. It was also found that 24.4% of patients were treated in tertiary teaching hospital, 27.4% in general hospital, 13.7% in hospital, and 34.5% in private clinics, respectively.
Table 2. Characteristics of Korean patients with psoriasis between 2011 and 2015.
| Variable | Year | ||||
|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | |
| No. of psoriasis patients | 219,429 (100.0) | 221,704 (100.0) | 228,842 (100.0) | 231,888 (100.0) | 233,909 (100.0) |
| Sex | |||||
| Male | 123,213 (56.2) | 124,960 (56.4) | 129,278 (56.5) | 131,696 (56.8) | 133,954 (57.3) |
| Female | 96,216 (43.8) | 96,744 (43.6) | 99,564 (43.5) | 100,192 (43.2) | 99,955 (42.7) |
| Age (yr) | |||||
| 0~9 | 6,783 (3.1) | 6,324 (2.9) | 6,636 (2.9) | 6,293 (2.7) | 5,312 (2.3) |
| 10~19 | 14,578 (6.6) | 13,671 (6.2) | 13,137 (5.7) | 12,770 (5.5) | 12,078 (5.2) |
| 20~29 | 26,405 (12.0) | 25,660 (11.6) | 25,534 (11.2) | 25,059 (10.8) | 25,217 (10.8) |
| 30~39 | 39,162 (17.8) | 38,654 (17.4) | 39,020 (17.1) | 38,951 (16.8) | 37,605 (16.1) |
| 40~49 | 43,185 (19.7) | 43,388 (19.6) | 43,931 (19.2) | 44,759 (19.3) | 45,173 (19.3) |
| 50~59 | 41,101 (18.7) | 44,065 (19.9) | 46,483 (20.3) | 47,805 (20.6) | 48,775 (20.9) |
| 60~69 | 26,873 (12.2) | 27,337 (12.3) | 29,158 (12.7) | 30,212 (13.0) | 31,925 (13.6) |
| 70~79 | 16,747 (7.6) | 17,782 (8.0) | 19,547 (8.5) | 20,240 (8.7) | 21,363 (9.1) |
| ≥80 | 4,595 (2.1) | 4,823 (2.2) | 5,396 (2.4) | 5,799 (2.5) | 6,461 (2.8) |
| Severity of psoriasis | |||||
| Mild | 175,400 (79.9) | 174,692 (78.8) | 180,350 (78.8) | 180,886 (78.0) | 181,079 (77.4) |
| Moderate-to-severe | 44,029 (20.1) | 47,012 (21.2) | 48,492 (21.2) | 51,002 (22.0) | 52,830 (22.6) |
| Type of psoriasis | |||||
| Plaque psoriasis | 186,199 (84.9) | 188,700 (85.1) | 193,796 (84.7) | 192,529 (83.0) | 196,060 (83.8) |
| Guttate psoriasis | 4,084 (1.9) | 3,764 (1.7) | 3,772 (1.6) | 3,877 (1.7) | 3,587 (1.5) |
| Palmoplantar pustulosis | 22,923 (10.4) | 23,395 (10.6) | 24,610 (10.8) | 26,647 (11.5) | 26,243 (11.2) |
| Generalized pustular psoriasis | 5,158 (2.4) | 4,435 (2.0) | 4,760 (2.1) | 6,350 (2.7) | 6,252 (2.7) |
| Psoriatic arthritis | 1,065 (0.5) | 1,410 (0.6) | 1,904 (0.8) | 2,485 (1.1) | 1,767 (0.8) |
| Type of health insurance | |||||
| National Health Insurance | 207,326 (94.5) | 209,617 (94.5) | 216,531 (94.6) | 219,405 (94.6) | 220,423 (94.2) |
| Medical Aid | 12,112 (5.5) | 12,087 (5.5) | 12,311 (5.4) | 12,483 (5.4) | 13,486 (5.8) |
| No. of comorbidity | |||||
| 0 | 169,381 (77.2) | 168,056 (75.8) | 170,999 (74.7) | 171,293 (73.9) | 170,192 (72.8) |
| 1 | 35,415 (16.1) | 37,947 (17.1) | 40,483 (17.7) | 42,373 (18.3) | 43,973 (18.8) |
| 2 | 12,036 (5.5) | 12,820 (5.8) | 14,173 (6.2) | 15,027 (6.5) | 16,188 (6.9) |
| 3 | 2,268 (1.0) | 2,533 (1.1) | 2,769 (1.2) | 2,791 (1.2) | 3,085 (1.3) |
| ≥4 | 329 (0.1) | 348 (0.2) | 418 (0.2) | 404 (0.2) | 471 (0.2) |
| Comorbid disease | |||||
| Diabetes mellitus | 19,637 (8.9) | 20,990 (9.5) | 22,529 (9.8) | 23,189 (10.0) | 24,437 (10.4) |
| Dyslipidemia | 26,366 (12.0) | 28,872 (13.0) | 31,937 (14.0) | 34,536 (14.9) | 37,224 (15.9) |
| Hypertension | 43,198 (19.7) | 45,350 (20.5) | 47,992 (21.0) | 49,019 (21.1) | 50,717 (21.7) |
| Cerebral vascular disorders | 4,378 (2.0) | 4,465 (2.0) | 4,759 (2.1) | 4,527 (2.0) | 4,612 (2.0) |
| Ischemic heart disease | 6,052 (2.8) | 6,608 (3.0) | 6,987 (3.1) | 6,983 (3.0) | 7,184 (3.1) |
| Myocardial infarction | 725 (0.3) | 746 (0.3) | 808 (0.4) | 834 (0.4) | 970 (0.4) |
| Crohn’s disease | 105 0.0 | 129 (0.1) | 116 (0.1) | 140 (0.1) | 168 (0.1) |
| Fat liver | 3,169 (1.4) | 3,283 (1.5) | 3,449 (1.5) | 3,284 (1.4) | 3,511 (1.5) |
| Malignancy | 6,796 (3.1) | 7,047 (3.2) | 7,747 (3.4) | 8,393 (3.6) | 8,822 (3.8) |
| Type of medical center | |||||
| Private clinic | 82,793 (37.7) | 79,751 (36.0) | 80,819 (35.3) | 80,005 (34.5) | 80,621 (34.5) |
| Hospital | 30,014 (13.7) | 31,841 (14.4) | 31,902 (13.9) | 32,182 (13.9) | 32,110 (13.7) |
| General hospital | 56,116 (25.6) | 57,333 (25.9) | 62,059 (27.1) | 65,378 (28.2) | 64,165 (27.4) |
| Tertiary teaching hospital | 50,506 (23.0) | 52,779 (23.8) | 54,062 (23.6) | 54,323 (23.4) | 57,013 (24.4) |
| Residence area | |||||
| Metro city | 83,256 (37.9) | 83,882 (37.8) | 84,247 (36.8) | 85,309 (36.8) | 85,779 (36.7) |
| City and county | 109,468 (49.9) | 110,878 (50.0) | 117,544 (51.4) | 119,136 (51.4) | 120,089 (51.3) |
| Rural place | 26,704 (12.2) | 26,944 (12.2) | 27,051 (11.8) | 27,443 (11.8) | 28,041 (12.0) |
Values are presented as number (%).
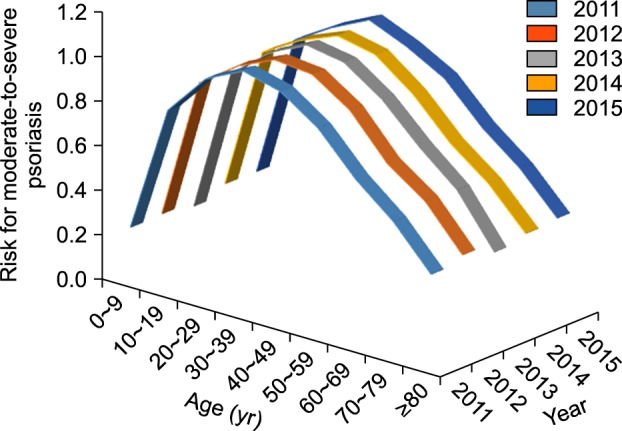
Factors associated with moderate-to-severe psoriasis
To find out the clinical and social factors associated with the severity of psoriasis, we calculated the aOR for moderate-to-severe psoriasis as compared with mild psoriasis (Table 3). The aOR of male sex for moderate-to-severe psoriasis was about 1.11~1.16 with significance. Children younger than 10 (aOR, 0.22~0.26) and elders older than 60 (aOR, 0.40~0.77) years of age had significantly lower aORs than young and mid-aged adult patients (aOR, 0.91~1.08) (Fig. 1). In comparison with plaque psoriasis, generalized pustular psoriasis (aOR, 1.87~2.75), guttate psoriasis (aOR, 1.90~2.25), and psoriatic arthritis (aOR, 1.97~4.31) was significantly associated with moderate-to-severe psoriasis. In addition, our data showed that the level of health institution visited was associated with the severity of psoriasis. However, the type of insurance used did not have a significant association with the severity of psoriasis. We also did not observe consistent differences in the risks of comorbid diseases between patients with mild and those with moderate-to-severe psoriasis, either.
Table 3. Factors Associated with Moderate-to-Severe Psoriasis.
| Variable | Year | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2011 | 2012 | 2013 | 2014 | 2015 | |||||||||||
| aOR | 95% CI | p-value | aOR | 95% CI | p-value | aOR | 95% CI | p-value | aOR | 95% CI | p-value | aOR | 95% CI | p-value | |
| Sex | |||||||||||||||
| Female | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Male | 1.15 | 1.13~1.18 | <0.0001 | 1.14 | 1.12~1.16 | <0.0001 | 1.14 | 1.11~1.16 | <0.0001 | 1.14 | 1.12~1.17 | <0.0001 | 1.11 | 1.09~1.13 | <0.0001 |
| Age (yr) | |||||||||||||||
| 0~29 | 1 | 1 | 1 | 1 | 1 | ||||||||||
| 30~59 | 1.26 | 1.23~1.30 | <0.0001 | 1.24 | 1.2~1.27 | <0.0001 | 1.25 | 1.22~1.29 | <0.0001 | 1.20 | 1.16~1.23 | <0.0001 | 1.18 | 1.15~1.21 | <0.0001 |
| ≥60 | 0.85 | 0.81~0.88 | <0.0001 | 0.84 | 0.81~0.87 | <0.0001 | 0.86 | 0.83~0.89 | <0.0001 | 0.80 | 0.78~0.83 | <0.0001 | 0.80 | 0.78~0.83 | <0.0001 |
| Type | |||||||||||||||
| Plaque psoriasis | 1 | 1 | 1 | 1 | 1 | ||||||||||
| Guttate psoriasis | 2.26 | 2.11~2.41 | <0.0001 | 1.93 | 1.8~2.07 | <0.0001 | 2.02 | 1.97~2.26 | <0.0001 | 2.29 | 2.14~2.45 | <0.0001 | 2.26 | 2.11~2.42 | <0.0001 |
| Palmoplantar pustulosis | 1.05 | 1.01~1.09 | 0.0061 | 1.11 | 1.07~1.14 | <0.0001 | 1.32 | 1.28~1.37 | <0.0001 | 1.28 | 1.24~1.32 | <0.0001 | 1.24 | 1.20~1.28 | <0.0001 |
| Generalized pustular psoriasis | 1.98 | 1.86~2.10 | <0.0001 | 2.63 | 2.47~2.80 | <0.0001 | 2.01 | 1.89~2.14 | <0.0001 | 1.83 | 1.73~1.93 | <0.0001 | 1.79 | 1.69~1.89 | <0.0001 |
| Psoriatic arthritis | 3.98 | 3.52~4.50 | <0.0001 | 2.76 | 2.48~3.07 | <0.0001 | 2.15 | 1.95~2.36 | <0.0001 | 1.99 | 1.83~2.17 | <0.0001 | 4.36 | 3.95~4.80 | <0.0001 |
| Type of medical center | |||||||||||||||
| Clinic | 1 | 1 | 1 | 1 | 1 | ||||||||||
| General hospital | 1.31 | 1.27~1.35 | <0.0001 | 1.35 | 1.31~1.39 | <0.0001 | 1.30 | 1.26~1.33 | <0.0001 | 1.35 | 1.31~1.38 | <0.0001 | 1.37 | 1.34~1.41 | <0.0001 |
| Hospital | 0.95 | 0.92~0.99 | <0.0001 | 0.93 | 0.9~0.97 | <0.0001 | 0.94 | 0.91~0.97 | 0.0003 | 1.03 | 1.00~1.07 | 0.0863 | 1.00 | 0.97~1.04 | 0.8819 |
| Tertiary teaching hospital | 2.04 | 1.99~2.10 | <0.0001 | 2.10 | 2.05~2.16 | <0.0001 | 2.12 | 2.06~2.18 | <0.0001 | 2.23 | 2.17~2.29 | <0.0001 | 2.15 | 2.09~2.21 | <0.0001 |
aOR: adjusted odd ratio, 95% CI: 95% confidence interval.
Fig. 1. Risk for moderate-to-severe psoriasis by age group between 2011 and 2015 in Korea.
DISCUSSION
Psoriasis is a worldwide disease. Population-based studies in many countries have reported a prevalence of psoriasis ranging from 0.2% to 4.8%3. Studies in Europe and the United States have yielded prevalences around 1% to 2%4,5,6,7,8. However, the prevalence of psoriasis in Asians has been reported to be lower, specifically, the prevalence of psoriasis was only 0.19% in Taiwan9, 0.34% in Japan10, and 0.3% in China, respectively11. In our study, the standardized prevalence in the Korean population ranged from 0.44% to 0.45%, confirming the results of previous studies involving Korean populations12,13.
The racial differences in the prevalence of psoriasis can be explained by the difference in genetic backgrounds between races. An association of psoriasis with several human leukocyte antigen (HLA) loci such as A1, B13, B17, and Cw6 have been reported1. In particular, HLA-Cw6 is strongly associated with psoriasis. It is believed that the lower prevalence of psoriasis in Asian populations might result from the lower frequency of HLA-Cw6 in this population1. In the Korean population, HLA-Cw0602 was found in 69.6% of the patients with psoriasis, but only in 9.0% of the healthy controls14.
It is known that psoriasis is equally common in men and women3,15. However, several studies on Asian populations have reported a male preponderance11,12,13,16,17,18. In Japan, the incidence in men was twice that in women18. Mild male preponderance in the Korean population was also found in this study, as well as in previous studies12,13. However, it is unclear whether Korean men are indeed more vulnerable to psoriasis, or if this finding comes from the difference in health-related behaviors between the sexes. To confirm this, further community-based study is necessary. The distribution of psoriasis patients by age group was reported differ in accordance with the study population. The highest prevalence was observed among 20 to 50-year-old subjects in Spain19, while it was noted in those patients in their 50s and 60s in the United Kingdom4. In Taiwan, the prevalence inclines with age, and peaks in people aged 70 years and older9. In our study, the highest prevalence was observed among people in their 40s and 50s, which was younger than in the Taiwan population.
Consistent with previous studies13,18,20,21, the plaque type was the most common, found in 85% of psoriasis patients in this study. The second most common type of psoriasis in this study was palmoplantar pustulosis, which was seen in more than 10% of the patients studied. However, Na et al. previously reported that palmoplantar pustulosis was found in only 3.5% of psoriasis patients who visited a tertiary teaching hospital. This difference may come from the differences in the study population between these two studies, or the potential misclassification of patients due to incorrect diagnostic codes in the HIRA database.
We found that 20% of psoriasis patients were treated with phototherapy, conventional systemic agents, and/or biologic agents. In this study, we regarded those individuals as patients with moderate-to-severe psoriasis because it is widely accepted as basic therapeutic strategy for psoriasis22. Consistent with the previous study13, male sex was significantly associated with more severe psoriasis than female sex. Interestingly, the risk of moderate-to-severe psoriasis was found to decline in patients 40 years of age and older. Considering this, together with the previous study reporting that the elderly-onset psoriasis was generally milder than early-onset psoriasis21,23,24,25, this finding supports the association between age and the severity of psoriasis. However, the correlation might be due to selection bias, because the elders more frequently have medical conditions that prohibit the use of systemic and biologic agents.
It has been reported that CV morbidity increases in psoriasis patients26,27. In particular, patients with severe psoriasis have an increased risk of CV mortality, as compared to people without psoriasis28. A case-control study conducted in Korea showed a higher prevalence of metabolic syndrome, CV disease, hypertension, and hyperlipidemia in psoriasis patients than in controls29. A study using a Korean nation-wide database reported that only the risk of dyslipidemia was significantly higher in Korean patients with psoriatic arthritis than in those with psoriasis vulgaris12. In this study, we did not observe the difference in the risks of comorbid diseases according to the severity of psoriasis. Further analyses by age, sex, and type of psoriasis are necessary to elucidate the association between psoriasis and CV morbidity in the Korean population.
This study has several limitations. First, the presence of psoriasis and comorbid diseases was defined by diagnostic codes from an insurance claims database and thus, bias might occur owing to the misclassification and omission of patients. Second, data of disease severity were not available in the HIRA. Instead, we used an assumption that patients treated with phototherapy or systemic agents would most like have moderate-to-severe psoriasis, as opposed to mild psoriasis. Third, the prevalence of psoriasis may be underestimated because we used the NHI claim database; if psoriasis patients did not visit clinics or hospitals, their cases were not included in calculating prevalence. Nevertheless, to yield more accurate prevalence, we used the entire Korean population database rather than sampled database and performed analyses based on period prevalence. Therefore, the current results of this study might provide the best representation for the prevalence of psoriasis in Korea.
In conclusion, we found that the standardized prevalence of psoriasis was around 450 per 100,000 of the Korean population. The prevalence peaked in the age of 50s and there was a male preponderance. This nation-wide study provides highly reliable epidemiologic information on Korean patients with psoriasis.
Footnotes
CONFLICTS OF INTEREST: The authors have nothing to disclose.
References
- 1.Raychaudhuri SP, Farber EM. The prevalence of psoriasis in the world. J Eur Acad Dermatol Venereol. 2001;15:16–17. doi: 10.1046/j.1468-3083.2001.00192.x. [DOI] [PubMed] [Google Scholar]
- 2.Gelfand JM, Stern RS, Nijsten T, Feldman SR, Thomas J, Kist J, et al. The prevalence of psoriasis in African Americans: results from a population-based study. J Am Acad Dermatol. 2005;52:23–26. doi: 10.1016/j.jaad.2004.07.045. [DOI] [PubMed] [Google Scholar]
- 3.Gudjonsson JE, Elder JT. Psoriasis: epidemiology. Clin Dermatol. 2007;25:535–546. doi: 10.1016/j.clindermatol.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 4.Gelfand JM, Weinstein R, Porter SB, Neimann AL, Berlin JA, Margolis DJ. Prevalence and treatment of psoriasis in the United Kingdom: a population-based study. Arch Dermatol. 2005;141:1537–1541. doi: 10.1001/archderm.141.12.1537. [DOI] [PubMed] [Google Scholar]
- 5.Nevitt GJ, Hutchinson PE. Psoriasis in the community: prevalence, severity and patients' beliefs and attitudes towards the disease. Br J Dermatol. 1996;135:533–537. [PubMed] [Google Scholar]
- 6.Braathen LR, Botten G, Bjerkedal T. Prevalence of psoriasis in Norway. Acta Derm Venereol Suppl (Stockh) 1989;142:5–8. [PubMed] [Google Scholar]
- 7.Egeberg A, Skov L, Gislason GH, Thyssen JP, Mallbris L. Incidence and prevalence of psoriasis in denmark. Acta Derm Venereol. 2017;97:808–812. doi: 10.2340/00015555-2672. [DOI] [PubMed] [Google Scholar]
- 8.Barisić-Drusko V, Paljan D, Kansky A, Vujasinović S. Prevalence of psoriasis in Croatia. Acta Derm Venereol Suppl (Stockh) 1989;146:178–179. [PubMed] [Google Scholar]
- 9.Chang YT, Chen TJ, Liu PC, Chen YC, Chen YJ, Huang YL, et al. Epidemiological study of psoriasis in the national health insurance database in Taiwan. Acta Derm Venereol. 2009;89:262–266. doi: 10.2340/00015555-0642. [DOI] [PubMed] [Google Scholar]
- 10.Kubota K, Kamijima Y, Sato T, Ooba N, Koide D, Iizuka H, et al. Epidemiology of psoriasis and palmoplantar pustulosis: a nationwide study using the Japanese national claims database. BMJ Open. 2015;5:e006450. doi: 10.1136/bmjopen-2014-006450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yip SY. The prevalence of psoriasis in the Mongoloid race. J Am Acad Dermatol. 1984;10:965–958. doi: 10.1016/s0190-9622(84)80314-x. [DOI] [PubMed] [Google Scholar]
- 12.Oh EH, Ro YS, Kim JE. Epidemiology and cardiovascular comorbidities in patients with psoriasis: A Korean nationwide population-based cohort study. J Dermatol. 2017;44:621–629. doi: 10.1111/1346-8138.13761. [DOI] [PubMed] [Google Scholar]
- 13.Na SJ, Jo SJ, Youn JI. Clinical study on psoriasis patients for past 30 years (1982-2012) in Seoul National University Hospital Psoriasis Clinic. J Dermatol. 2013;40:731–735. doi: 10.1111/1346-8138.12224. [DOI] [PubMed] [Google Scholar]
- 14.Nam SH, Kim CW, Kim SS, Kim KH, Lee KW, Kim KJ. Correlations between HLA-Cw*0602 and clinical picture in Korean psoriatic patients. Korean J Dermatol. 2001;39:183–189. [Google Scholar]
- 15.Christophers E. Psoriasis--epidemiology and clinical spectrum. Clin Exp Dermatol. 2001;26:314–320. doi: 10.1046/j.1365-2230.2001.00832.x. [DOI] [PubMed] [Google Scholar]
- 16.Tsai TF, Wang TS, Hung ST, Tsai PI, Schenkel B, Zhang M, et al. Epidemiology and comorbidities of psoriasis patients in a national database in Taiwan. J Dermatol Sci. 2011;63:40–46. doi: 10.1016/j.jdermsci.2011.03.002. [DOI] [PubMed] [Google Scholar]
- 17.Kaur I, Handa S, Kumar B. Natural history of psoriasis: a study from the Indian subcontinent. J Dermatol. 1997;24:230–234. doi: 10.1111/j.1346-8138.1997.tb02779.x. [DOI] [PubMed] [Google Scholar]
- 18.Japanese Society For Psoriasis Research. Takahashi H, Nakamura K, Kaneko F, Nakagawa H, Iizuka H. Analysis of psoriasis patients registered with the Japanese Society for Psoriasis Research from 2002-2008. J Dermatol. 2011;38:1125–1129. doi: 10.1111/j.1346-8138.2010.01145.x. [DOI] [PubMed] [Google Scholar]
- 19.Ferrándiz C, Bordas X, García-Patos V, Puig S, Pujol R, Smandía A. Prevalence of psoriasis in Spain (Epiderma Project: phase I) J Eur Acad Dermatol Venereol. 2001;15:20–23. doi: 10.1046/j.1468-3083.2001.00191.x. [DOI] [PubMed] [Google Scholar]
- 20.Fan X, Yang S, Sun LD, Liang YH, Gao M, Zhang KY, et al. Comparison of clinical features of HLA-Cw*0602-positive and -negative psoriasis patients in a Han Chinese population. Acta Derm Venereol. 2007;87:335–340. doi: 10.2340/00015555-0253. [DOI] [PubMed] [Google Scholar]
- 21.Ferrándiz C, Pujol RM, García-Patos V, Bordas X, Smandía JA. Psoriasis of early and late onset: a clinical and epidemiologic study from Spain. J Am Acad Dermatol. 2002;46:867–873. doi: 10.1067/mjd.2002.120470. [DOI] [PubMed] [Google Scholar]
- 22.Ashcroft DM, Li Wan, Griffiths CE. Therapeutic strategies for psoriasis. J Clin Pharm Ther. 2000;25:1–10. doi: 10.1046/j.1365-2710.2000.00254.x. [DOI] [PubMed] [Google Scholar]
- 23.Kwon HH, Kwon IH, Youn JI. Clinical study of psoriasis occurring over the age of 60 years: is elderly-onset psoriasis a distinct subtype? Int J Dermatol. 2012;51:53–58. doi: 10.1111/j.1365-4632.2011.04979.x. [DOI] [PubMed] [Google Scholar]
- 24.Henseler T, Christophers E. Psoriasis of early and late onset: characterization of two types of psoriasis vulgaris. J Am Acad Dermatol. 1985;13:450–456. doi: 10.1016/s0190-9622(85)70188-0. [DOI] [PubMed] [Google Scholar]
- 25.Bernhard JD. Clinical differences in juvenile vs adult-onset psoriasis. Br J Dermatol. 1996;135:501–502. doi: 10.1111/j.1365-2133.1996.tb01537.x. [DOI] [PubMed] [Google Scholar]
- 26.Edson-Heredia E, Zhu B, Lefevre C, Wang M, Barrett A, Bushe CJ, et al. Prevalence and incidence rates of cardiovascular, autoimmune, and other diseases in patients with psoriatic or psoriatic arthritis: a retrospective study using Clinical Practice Research Datalink. J Eur Acad Dermatol Venereol. 2015;29:955–963. doi: 10.1111/jdv.12742. [DOI] [PubMed] [Google Scholar]
- 27.Reich K. The concept of psoriasis as a systemic inflammation: implications for disease management. J Eur Acad Dermatol Venereol. 2012;26(Suppl 2):3–11. doi: 10.1111/j.1468-3083.2011.04410.x. [DOI] [PubMed] [Google Scholar]
- 28.Mehta NN, Azfar RS, Shin DB, Neimann AL, Troxel AB, Gelfand JM. Patients with severe psoriasis are at increased risk of cardiovascular mortality: cohort study using the General Practice Research Database. Eur Heart J. 2010;31:1000–1006. doi: 10.1093/eurheartj/ehp567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choi WJ, Park EJ, Kwon IH, Kim KH, Kim KJ. Association between psoriasis and cardiovascular risk factors in Korean patients. Ann Dermatol. 2010;22:300–306. doi: 10.5021/ad.2010.22.3.300. [DOI] [PMC free article] [PubMed] [Google Scholar]


