Abstract
Food insecurity (FI) has been associated with HIV disease progression among people on antiretroviral therapy (ART), presumably a consequence of poor medication adherence. We assessed whether there is a longitudinal association between FI and two primary outcomes reflecting on HIV disease progression (i.e., CD4 count and time to ART initiation) among people not on ART. Analyses used linear mixed effects and Cox models controlling for confounders. In this cohort (n= 310) FI was common (53%). Most (71.3%) reported past month heavy alcohol use and 37.1% reported past month injection drug use. Only 50 participants initiated ART during the study and mean time to ART was 128 days (SD 120). There were no significant differences in CD4 cell count between the groups with mild/moderate FI or severe FI vs. those with no FI (adjusted mean difference, mild/moderate insecurity vs. no FI −32.5 [95%CI: −94.3, 29.3]; severe vs. no FI −45.5 [95%CI: −124.1, 33.0]; global p=0.42). We found no significant association between FI and longer time to ART initiation (p=0.36). Food security is a desirable goal for overall health and shown beneficial for those on ART, however it does not appear to be associated with HIV disease progression among those with high prevalence of substance use and not yet on ART.
Keywords: HIV progression, Russia, food insecurity, access to care
1. INTRODUCTION
Food insecurity (FI), defined as having limited availability of food; inadequate access to a nutritious diet; and the inability to procure food, is a significant contributor to the morbidity and mortality associated with the HIV epidemic in both developing and developed countries (1, 2). Food security and HIV elimination are two major, hard-to-reach health targets of the global Sustainable Development Goals requiring additional resources to effectively address these challenges by 2030 (3, 4).
Existing studies among HIV-infected people have highlighted three possible important associations between FI and HIV-related outcomes: increased HIV transmission; accelerated HIV progression; and impaired access to HIV care (5–7). Among HIV-infected people, FI is associated with incomplete viral suppression and an increased risk of HIV transmission to uninfected peers via behavioral pathways (e.g., risky sexual behavior and needle sharing practices among people who use drugs) (7–9). Additionally, FI among HIV-infected people has been shown to impede access to HIV care, even when healthcare is provided free of charge, compromising immune status (9–14). Reduced nutrient intake or poor adherence to antiretroviral therapy (ART) medications by food insecure individuals could reduce viral load suppression, potentially even more so among people with substance use (9, 14–16). Nutritional studies among HIV-infected people on ART demonstrate that a reduction in serum micronutrients is associated with an increased risk of HIV progression. Furthermore, micronutrient supplements can delay disease progression and reduce mortality (17, 18). Interrelated mechanisms of FI and HIV infection have been targets for tailored programs to mitigate the global burden of HIV in resource-limited settings (19, 20).
Most of the literature assessing FI and HIV disease progression has been carried out among people on ART. In contrast, little is known about HIV disease progression or access to HIV care among those not yet on ART. Alternative mechanisms previously hypothesized such as mental health, missed clinic visits and nutritional deficiencies could be at work in the setting of FI among those not on ART (21). Studying these key ART-naive populations can shed light on the mechanisms by which FI impacts people with HIV. While evidence suggests that rates of FI are alarmingly high among HIV-infected people who use drugs (PWUD) and other vulnerable populations, FI in Eastern Europe, including Russia, has only been described to a limited extent (22–24). Recently, due to the economic crisis in Russia and sanctions banning certain food imports into the country, concerns about FI have received greater public attention (25–27).
In contrast to decreasing global trends, the number of new HIV infections in Russia grew 5.3% on average between 2005 and 2015, making it the highest increase in Europe (28). Additionally, there are areas of concentrated epidemic where prevalence could exceed 40% such as among PWUD in St. Petersburg (29). The official Russian Ministry of Health 2015 report documents just over a million patients infected with HIV throughout Russia (30) while estimated ART coverage is 14% (28). This rapid HIV growth has become a major public health challenge for Russia, creating a need to better understand the role of FI in this region.
The aim of this study was to gain an understanding of the associations between FI, HIV progression, and access to HIV care, in a setting of a concentrated HIV epidemic. For that purpose, we analyzed data from an observational longitudinal cohort of HIV-infected Russians not on ART at enrollment, many with a history of substance use. We hypothesized that FI would be associated with: (1) measures of HIV disease progression (i.e., CD4 cell count [primary outcome] and HIV viral load) and (2) decreased access to HIV treatment (i.e., longer time until initiation of ART).
2. METHODS
2.1 Design, Participants, and Setting
We conducted a secondary analysis of baseline, 6, and 12-month follow-up data from the Russia ARCH cohort, an observational cohort study (baseline n=351) of HIV-infected Russians not on ART at enrollment. Within the Russia ARCH cohort is a nested double-blinded, randomized placebo controlled trial of zinc supplementation (ZINC) (n=254) (31).
Russia ARCH recruited 351 participants between November 2012 and June 2015 from clinical HIV and addiction sites, non-clinical sites, and via snowball recruitment in St. Petersburg, Russia. Inclusion criteria were the following: 1) documented HIV infection; 2) ART-naïve at baseline; 3) age 18 to 70 years; 4) stable address within 100 kilometers of St. Petersburg; 5) having a phone; and 6) having two contacts to assist with follow-up. Participants were excluded from the study if they 1) were not fluent in Russian; or 2) had a cognitive impairment precluding informed consent. After eligibility was verified and informed consent obtained, participants provided a blood sample and were administered an interview assessment.
For the current analysis of HIV disease progression and access to care, 41 participants were excluded as they had an undetectable viral load at baseline. The Institutional Review Boards of Boston University Medical Campus and First Saint Petersburg Pavlov State Medical University (PSMU) approved the study.
2.2 Variable Selection
2.2.1 Outcomes
To assess HIV disease progression, the primary outcome of interest was CD4 cell count assessed at baseline and 12 months. In addition, we conducted a confirmatory analysis including CD4 cell count dichotomized at CD4 <350 cells/mm3; and plasma HIV RNA load (log10-transformed). Analyses of HIV disease progression were restricted to observations where participants were not on ART.
For the secondary aim examining the impact of FI on ART initiation, we examined self-reported time from study enrollment until initiation of ART. The date of ART initiation was assessed at 6- and 12-month study visits among all study participants (32). Additionally, restricted analyses were conducted among only those eligible for ART based on guidelines of the Russian Federation for the initiation of HIV pharmacotherapy at the time of the study (CD4 <350 cells/mm3) (33).
2.2.2 Main Independent Variable
Past month food insecurity (FI), the main independent variable in this study, was assessed using the Household Food Insecurity Access Scale (HFIAS) at baseline and 12-month follow-up visits (34). In an attempt to increase the applicability of the instrument in a Russian setting, we modified the HFIAS. The modified nine questions ask only about a study participant’s own experience with FI, in comparison to the original nine question version, which also asked participants about their household members’ FI. The scale used in this study is presented in Figure 1; the original version is published (34). We categorized FI as: none (food secure); mild/moderate (combined); or severe. In exploratory analyses, we dichotomized FI as any (mild, moderate and severe combined) versus none (food secure).
Figure 1.
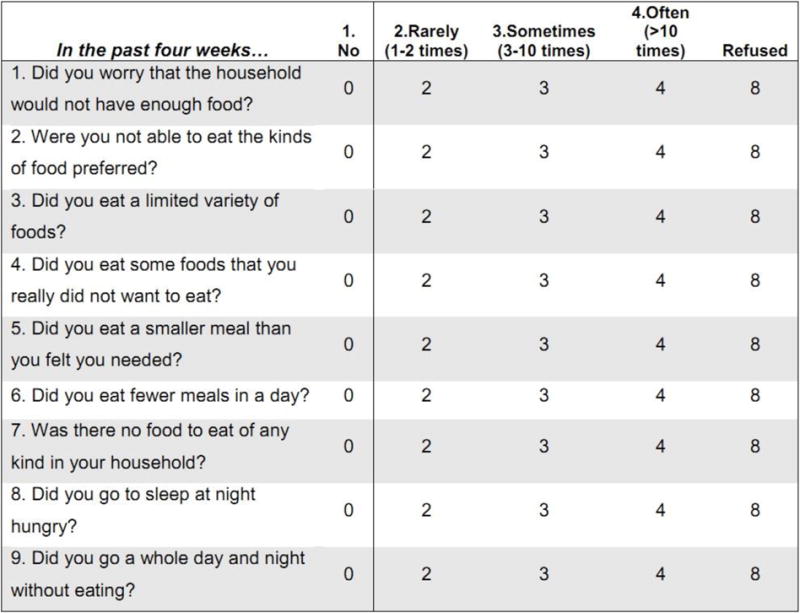
Modified Household Food Insecurity Access Scale, used in our study
According to the HFIAS, mildly food insecure households are those that worry about not having enough food sometimes or often, and/or are unable to eat preferred foods, and/or eat a more monotonous diet than desired and/or consume some food considered undesirable, but only rarely (34). Once the household rarely or sometimes starts to cut back on quantity by reducing the size of meals or number of meals, it is considered moderately FI. A severely food insecure household is one that has to reduce meal size or number of meals often, and/or experiences any of these severe conditions in the past month regardless of frequency: running out of food, going to bed hungry, or going a whole day and night without eating (34).
2.2.3 Covariates
The following covariates were selected a priori based on literature review: assessed at baseline – age; gender; underweight (BMI < 18.5); monthly income (based on median split approach (35), participants with incomes of lower than 20,000 rubles were included in the “low” group); social support (36); and past year arrest; which was only included for analyses related to access to care. Variables assessed at baseline and 12 months included social support score; BMI; income; past week depressive symptoms (Center for Epidemiologic Studies Depression Scale [CESD ≥16] (37, 38); past month injection drug use (39, 40); and past month heavy alcohol use (NIAAA risky drinking criteria) (41). We initially included employment status as a covariate, but as it was highly correlated with income, we omitted this variable from regression models. Confirmatory analyses were also conducted controlling for randomization to zinc supplementation. For the main outcome (CD4 cell count), we performed sensitivity analyses excluding depressive symptoms and past month injection drug use variables given the potential that these factors could have been in the causal pathway with FI.
2.3 Statistical Analyses
We used descriptive statistics to characterize the study cohort overall and stratified by FI at baseline. For descriptive purposes, we compared baseline characteristics across groups using chi-square tests for categorical variables and ANOVA or Kruskal-Wallis as appropriate for continuous variables. We used linear mixed effects models to evaluate associations between FI and the continuous outcomes, CD4 cell count and log HIV RNA, biomarkers of HIV disease progression assessed at the same study visit. HIV RNA was log10-transformed due to skewedness in its distribution. Group differences and corresponding confidence intervals were back-transformed from the log scale to calculate the ratio of results for severe/mild or moderate FI relative to no FI. We used subject-specific random intercepts to account for the correlation due to having repeated observations from the same participant. Generalized estimating equations (GEE) logistic regression models were used to evaluate the association between FI and the binary outcome CD4 <350 vs. ≥350 cells/mm3. The GEE models were fit using an independence working correlation structure and robust standard errors are reported from the models. We implemented Cox proportional hazards models to evaluate the association between FI and time to initiation of ART. Preliminary unadjusted models were fit for each outcome. We then fit adjusted models controlling for age, gender, BMI, income, social support, depressive symptoms, heavy alcohol use and current injection drug use (in addition, we also controlled for incarceration in analyses of ART initiation). Heavy alcohol use, current injection drug use and depressive symptoms were modeled as time-varying covariates in the regression models. Confirmatory analyses were also conducted, adjusting for randomization to the zinc intervention, to assess potential confounding by zinc. We reported adjusted mean differences (mixed effects models), adjusted odds ratios (logistic regression models), and adjusted hazard ratios (Cox models), along with corresponding 95% confidence intervals. Spearman correlations were calculated to assess correlations between independent variables and covariates and no pair of variables included in the same regression model was highly correlated (r<0.40 in all cases). We conducted the analyses using two-sided tests and an alpha level of 0.05. All statistical analyses were conducted using SAS version 9.3 (SAS Institute, Inc., NC, USA).
3. RESULTS
3.1 Participant Characteristics
Of the 351 Russia ARCH participants, 310 met this study’s criteria and were included in analyses. In the survival analysis (i.e., time to ART) we were only able to include participants with 6 or 12-month follow-up visits, the timepoints at which ART initiation was assessed. In this report, all were HIV-infected and ART-naïve at baseline, with detectable HIV viral load. At baseline, measures of HIV status were the following: CD4 cell count below 350 cells/mm3 was observed in 69 (31.1%) participants and mean log HIV viral load was 4.52 (SD 0.91). Only 50 participants initiated ART during the study and mean time to ART was 128 days (SD 120). Among those who started ART before their 12-month visit, the median number of days to ART was 83.
Of the 310 participants, 221 (71.3%) reported past month heavy alcohol use and 115 (37.1%) reported past month injection drug use. FI was common (52.9%, n=164): 92 (29.7%) were categorized as mildly/moderately food insecure and 72 (23.2%) were categorized as severely food insecure (Table I). There were 17 (5.5%) underweight individuals (BMI < 18.5) in the analysis, of which 15 (88.2%) were food insecure. The mean age of study participants was 33.6 years (SD 5.5), 220 (71.0%) were male. Half of the study participants were unemployed, with food insecure individuals more likely to be unemployed. Similarly, most participants in the low-income category were classified as food insecure. In this cohort, 139 (45.1%) participants reported depressive symptoms, and severely food insecure individuals were more likely to have depressive symptoms. Food insecure individuals reported lower levels of social support than those who were food secure.
Table I.
Baseline characteristics of 310 untreated HIV-infected Russians, overall and by food insecurity status
| Characteristic | Total N=310* |
Food Secure N=146* |
Mild/Moderate Food Insecurity N=92* |
Severe Food Insecurity N=72* |
P value |
|---|---|---|---|---|---|
| Age: mean (SD) | 33.6 (5.5) | 33.7 (5.2) | 33.5 (5.3) | 33.7 (5.1) | 0.96 |
| Male | 220 (71%) | 107 (73.3%) | 66 (71.7%) | 47 (65.3%) | 0.46 |
| Underweight | 17 (5.5%) | 2 (1.4%) | 5 (5.4%) | 10 (13.9%) | <0.001 |
| Unemployed | 155 (50%) | 53 (36.3%) | 50 (54.3%) | 52 (72.2%) | <0.001 |
| Low income |
N=307 148 (48%) |
N=144 54 (37.5%) |
N=91 48 (52.7%) |
N=72 46 (63.9%) |
<0.001 |
| Depressive symptoms | 139 (45.1%) | 52 (35.9%) | 42 (45.7%) | 45 (63.4%) | <0.001 |
| Heavy drinking, past month | 221 (71.3%) | 108 (74.0%) | 63 (68.5%) | 50 (69.4%) | 0.61 |
| Social support: mean (SD) | 20.1 (5.3) | 21.6 (4.8) | 18.6 (5.2) | 18.7 (5.7) | <0.001 |
| Injection drug use, past month | 115 (37.1%) | 47 (32.2%) | 31 (33.7%) | 37 (51.4%) | 0.02 |
| Illicit drug use, past month | 125 (40.3%) | 53 (36.3%) | 34 (37.0%) | 38 (52.8%) | 0.048 |
| Heroin use, ever | 267 (86.1%) | 127 (87.0%) | 77 (83.7%) | 63 (87.5%) | 0.72 |
| Arrested, past year | 43 (13.9%) | 18 (12.3%) | 16 (17.4%) | 9 (12.5%) | 0.50 |
| Days to ART Mean (SD) |
N=50 128 (120) |
N=24 113 (96) |
N=17 126 (139) |
N=9 171 (141) |
0.48 |
| HIV load, log mean (SD) |
N=307 4.52 (0.91) |
N=146 4.48 (0.89) |
N=90 4.56 (0.91) |
N=71 4.53 (0.95) |
0.82 |
| CD4 count mean, (SD) |
N=222 510 (276) |
N=113 509 (270) |
N=64 523 (289) |
N=45 494 (278) |
0.86 |
unless stated otherwise
3.2 Food Insecurity and Biomarkers of HIV Disease Progression
We found no significant association between FI and HIV disease progression, assessed at the same study visit. For the primary outcome of CD4 cell count, there were no significant differences between mild/moderate FI or severe FI and those who were food secure, adjusted mean difference (95% CI), mild/moderate insecurity vs. secure −32.5 (95%CI: −94.3, 29.3); severe vs. secure −45.5 (95% CI: −124.1, 33.0); global p=0.42, in analyses controlling for age, gender, social support, BMI, income, depressive symptoms, heavy drinking and injection drug use. Similarly, in adjusted analyses we did not detect significant differences in HIV viral load between the groups: ratio of means (95% CI), mild and moderate insecurity vs. secure 1.19; (95% CI: 0.79, 1.79); severe vs. secure 0.85 (95% CI: 0.51, 1.40); global p=0.39. Further details are presented in Table II; please note that depressive symptoms −22.7 (95% CI: −85.0, 39.7), injection drug use −26.9 (95% CI: −88.0, 34.2) and income 5.2 (95% CI: −54.3, 64.7) were not significantly associated with viral suppression in the model.
Table II.
Longitudinal association between food insecurity and measures of HIV disease progression and access to HIV care
| CD4 cell counta | HIV viral loadb | Time to ARTc | ||||
|---|---|---|---|---|---|---|
| Outcome
|
Adjusted mean difference (95% CI) |
p-value | Ratio of Means (95% CI) |
p-value | Hazard Ratio (95% CI) |
p-value |
| Variable | ||||||
| Mild and moderate food insecurity (vs. secure) | −32.5 (−94.3, 29.3) |
0.41 | 1.19 (0.79, 1.79) |
0.38 | 1.64 (0.84, 3.24) |
0.36 |
| Severe food insecurity (vs. secure) | −45.5 (−124.1, 33.0) |
0.85 (0.51, 1.40) |
1.22 (0.50, 2.97) |
|||
|
| ||||||
| 12 month (vs. baseline) | −98.9 (−148.5, −49.3) |
<0.001 | 1.27 (0.95, 1.70) |
0.11 | – | – |
|
| ||||||
| Social support | −1.6 (−6.9, 3.6) |
0.53 | 1.00 (0.96, 1.03) |
0.91 | 1.05 (0.99, 1.12) |
0.11 |
|
| ||||||
| Age | 1.9 (−4.0, 7.7) |
0.52 | 1.00 (0.96, 1.04) |
0.89 | 1.07 (1.03, 1.12) |
0.001 |
|
| ||||||
| Gender (female vs. male) | 16.2 (−60.0, 92.5) |
0.67 | 1.02 (0.60, 1.75) |
0.94 | 1.51 (0.82, 2.79) |
0.18 |
|
| ||||||
| Underweight | 82.2 (−41.1,205.5) |
0.18 | 0.73 (0.33, 1.61) |
0.43 | 1.11 (0.35, 3.59) |
0.85 |
|
| ||||||
| Income (high vs. low) | 5.2 (−54.3, 64.7) |
0.86 | 1.38 (0.95, 2.02) |
0.09 | 1.12 (0.61, 2.06) |
0.72 |
|
| ||||||
| Depressive symptoms (past week symptoms) | −22.7 (−85.0, 39.7) |
0.47 | 1.36 (0.92, 2.01) |
0.12 | 1.35 (0.73, 2.48) |
0.33 |
|
| ||||||
| Heavy drinking past month (yes vs. no) | −46.2 (−112.2, 19.7) |
0.16 | 1.04 (0.71, 1.53) |
0.85 | 1.36 (0.73, 2.53) |
0.33 |
|
| ||||||
| Injection drug use past month (yes vs. no) | −26.9 (−88.0, 34.2) |
0.38 | 1.32 (0.87, 2.00) |
0.19 | 0.29 (0.13,0.64) |
0.002 |
|
| ||||||
| Incarcerated Past year(yes vs. no) | – | – | – | – | 1.02 (0.39, 2.67) |
0.96 |
n=253; observations 344
n=307; observations 442
n = 237
3.3 Food Insecurity and ART initiation
For the second aim of assessing the association between FI and ART initiation, we measured time from enrollment to self-reported initiation of ART. The study sample was comprised of 242 participants; and the adjusted analysis included 237 participants due to 5 having missing values for covariates. Only 50 of 242 participants reported initiating ART while in the study. Among the full sample, 24 (48.0%) secure, 17 (34.0%) mild/moderate, and 9 (18.0%) severely food insecure participants reported starting ART within one year from baseline. Participants who were on ART at their 12-month visit were less likely to report past month injection drug use at baseline than those who were not on ART at their 12-month visit (8/50 vs. 75/192; p=0.002).
We found no significant differences in ART initiation between those with and without FI using unadjusted analyses or adjusted regression models (adjusted hazard ratio [95% CI]: mild/moderate vs. secure 1.64 [95% CI: 0.84, 3.24], severe vs. secure 1.22 [95% CI: 0.50, 2.97]; global p=0.36). Notably, most of the variables included in the adjusted regression model (Table II) were not significantly associated with ART initiation, with the exception of age (hazard ratio [95% CI]: 1.07 [1.03, 1.12], p=0.001) and injection drug use (0.29 [0.13, 0.64], p=0.002).
3.4 Confirmatory Analyses
The results from all confirmatory analyses were consistent with the main findings. We performed additional confirmatory regression analyses dichotomizing the main outcome, CD4 cell count as <350 vs. >= 350 cells/mm3 and found no significant differences between groups (Table III). In addition, for the second aim of assessing access to ART, we limited the analysis to participants who were eligible for ART according to the Russian guidelines when participants were enrolled (CD4 count <350 vs. > 350 cells/mm3). A total of 57 participants had a CD4 cell count < 350 at baseline. In unadjusted analyses and adjusted regression models, we found no significant differences in ART initiation between those with and without FI (adjusted hazard ratio [95% CI]: mild/moderate vs. secure 2.88 [95% CI: 0.42, 19.77], severe vs. secure 0.50 [95% CI: 0.11, 2.20]; global p=0.19). Furthermore, for exploratory analyses of the main outcome only (continuous CD4 cell count) we categorized the previously three-category variable of FI into two categories: any vs. none, no significant differences were identified. Subsequently, we ran a regression for the primary outcome (continuous CD4 cell count) as in main analyses controlling for age, gender, social support, BMI, income and heavy drinking but excluded depressive symptoms with injection drug use (data is not shown) and the results were consistent. Finally, results were consistent after adjustment for randomization to the zinc intervention.
Table III.
Secondary exploratory analyses of the association between food insecurity and measures of HIV disease progression and access to HIV care
| CD4 dichotomousa | CD4 continuousb | Time to ARTc | ||||
|---|---|---|---|---|---|---|
| Outcome
|
Odds Ratio (95% CI) |
p-value | Adjusted mean difference (95% CI) |
p-value | Hazard Ratio | p-value |
| Variable | ||||||
| Mild and moderate food insecurity (vs. secure) | 1.14 (0.66, 2.00) |
0.74 | Food secure vs. food insecure | 2.88 (0.42, 19.77) |
0.19 | |
| Severe food insecurity (vs. secure) | 1.28 (0.67, 2.46) |
−36.7 (−92.9, 19.5) |
0.19 | 0.50 (0.11,2.20) |
||
|
| ||||||
| 12 month (vs. baseline) | 1.44 (0.90, 2.29) |
0.13 | −99.7 (−149.0, −50.4) |
0.0001 | – | – |
|
| ||||||
| Social support | 1.01 (0.97, 1.06) |
0.55 | −1.7 (−6.9, 3.6) |
0.52 | 1.24 (1.07, 1.44) |
0.004 |
|
| ||||||
| Age | 1.00 (0.95, 1.04) |
0.88 | 1.9 (−4.0, 7.7) |
0.53 | 0.98 (0.86, 1.11) |
0.75 |
|
| ||||||
| Gender (female vs. male) | 0.74 (0.42, 1.32) |
0.31 | 16.7 (−59.5, 92.9) |
0.66 | 0.55 (0.16, 1.98) |
0.36 |
|
| ||||||
| Underweight | 1.05 (0.35, 3.12) |
0.93 | 79.5 (−42.1,201.1) |
0.19 | 5.60 (0.49, 63.65) |
0.16 |
|
| ||||||
| Income (high vs. low) | 0.75 (0.44, 1.26) |
0.28 | 5.4 (−53.9, 64.8) |
0.85 | 2.31 (0.72, 7.43) |
0.16 |
|
| ||||||
| Depressive symptoms (past week symptoms) | 1.17 (0.69, 1.99) |
0.55 | −24.3 (−85.8, 37.1) |
0.43 | 2.07 (0.62, 6.99) |
0.23 |
|
| ||||||
| Heavy drinking past month (yes vs. no) | 1.70 (0.94, 3.07) |
0.07 | −45.7 (−111.4, 20.0) |
0.17 | 2.67 (0.64, 11.17) |
0.17 |
|
| ||||||
| Injection drug use past month (yes vs. no) | 1.77 (1.05, 3.00) |
0.03 | −27.9 (−88.5, 32.7) |
0.36 | 0.18 (0.04, 0.79) |
0.023 |
|
| ||||||
| Incarcerated Past year(yes vs. no) | – | – | – | – | 2.21 (0.52, 9.44) |
0.28 |
n=253; observations 344. Outcomes dichotomized at CD4 < 350 cells/mm3.
n=253; observations 344. This outcome is continuous, but independent variable in the model is dichotomized as food secure, vs any food insecurity.
n=57. Time to ART exploratory outcome limited to subjects with CD4 < 350 cells/mm3 i.e. only those who should have been eligible for ART via local guidelines.
We conducted an additional analysis limited to those who reported lifetime heroin use (n=214), controlling for the same covariates as in the main model (age, gender, social support, BMI, income, depressive symptoms, heavy drinking and injection drug use). Comparing those with some or severe FI to those who were food secure, there were no significant differences in CD4 cell count (p=0.50) or HIV viral load (p=0.37) in unadjusted and adjusted models. Adjusted mean differences (95% CI) for the primary outcome of CD4 cell count were: mild/moderate insecurity vs. secure −25.7 (95% CI: −95.4, 44.1); severe vs. secure −48.9 (95% CI: −135.1, 37.2); global p=0.50.
In addition, we conducted an exploratory regression analysis assessing FI at baseline (3-category version) and changes from baseline to 12 months in both CD4 cell count and HIV viral load. For the outcome of “change in CD4 cell count”, in analyses controlling for age, gender, social support, BMI, income, depressive symptoms, heavy drinking and injection drug use, adjusted mean differences (95% CI) were as follows: mild/moderate insecurity vs. secure 7.5 (95% CI: −101, 116); severe vs. secure −25.6 (95% CI: −179, 127.9); global p=0.91. For the outcome of change in HIV viral load, adjusted mean differences (95% CI) were as follows: mild/moderate insecurity vs. secure 151 592 (95% CI: −227 759, 561 081); severe vs. secure 166 661 (95% CI: −227 759, 561 089); global p=0.56.
For the main outcome, we also conducted an additional analysis, using log transformed CD4 cell count. The conclusions were consistent with the original analyses. The adjusted ratio of means (95% CI) (back transformed results) were as follows: mild/moderate insecurity vs. secure 0.98 (95% CI: 0.82,1.17); severe vs. secure 0.93 (95% CI: 0.75, 1.15); global p=0.80, in analyses controlling for age, gender, social support, BMI, income, depressive symptoms, heavy drinking and injection drug use.
4. DISCUSSION
In this study of 310 HIV-infected individuals, many with a history of substance use, in St. Petersburg, Russia, the prevalence of food insecurity was high (52.9%). Descriptive analyses suggested that FI may be related to lower BMI, unemployment, lower incomes, lower levels of social support, and depressive symptoms. In longitudinal regression analyses controlling for potential confounders, we did not find a significant association between FI and HIV disease progression among people not on ART or with ART initiation.
Food insecurity and its potential association with HIV disease progression and access to care among HIV-infected people in Eastern Europe has received limited attention. Furthermore, assessing these associations longitudinally among HIV-infected individuals not on ART is novel and can assess consequences beyond poor adherence to ART. Of note, for Russians, health care is provided free of charge, as it is a constitutional right (42), although ART drug supply shortages and other costs still exist (43).
The high prevalence of FI in this study is notable but not inconsistent with studies conducted in Canada and the US assessing similar populations (16, 44–47). However, our findings showed no associations between FI and HIV disease progression or initiation of ART among a population not on ART at enrollment, in contrast to findings from the existing literature from other geographic regions among people on ART. The majority of previous studies demonstrated an association between FI and HIV disease progression and access to HIV care (11, 15, 45, 48–51). To our knowledge, only one study did not demonstrate a statistically significant association in adjusted analyses between FI and virologic suppression among participant receiving ART (16); authors of this study attributed the lack of association to methodological factors, such as confounding and misclassification. We were unable to find any studies with negative findings among participants who were not on ART.
Several unique features of our study may explain the negative findings. Study participants were not on ART at baseline, while other studies that showed an association between FI and HIV disease progression included patients already on ART. This could be a key factor, as those who are on ART might have poor HIV outcomes due to lower adherence to medications. A large body of research shows that FI may negatively impact adherence to HIV medications, which further compromises virologic and immune status (5, 52). Interestingly, based on the literature, the mediation effect of adherence alone could not explain its role in viral progression. Studies have shown that the magnitude of effect between FI and HIV viral load suppression decreases when adjusting for ART adherence (53), which is in contrast to findings where controlling for adherence does not explain the associations (50). FI and adherence among key populations are not the only factors related to poor HIV outcomes; other social drivers of poor health may have not been captured in this or other studies, such as income security and healthcare barriers (54). Associations of FI and HIV disease progression among ART-naïve patients might also be confounded by the degree and timeframe of direct biological effects of severe FI and hunger – malnutrition (e.g., deficiencies of protein, vitamins, trace minerals, antioxidants) may be directly related to immune function; we did not measure these in this study. In addition, this study was conducted in Russia and includes a greater proportion of people with a history of drug use. Finally, there might be unknown, undocumented confounders in the analyses, which are related to the specific study context and cohort characteristics. The feasibility of this assumption is reinforced by the observation that other well-known predictors of poor HIV clinical outcomes, such as depressive symptoms, income and substance use were not associated with HIV progression in these analyses, suggesting potential unique aspects of the specific context or cohort in which our study was carried out.
A multitude of policy and system level strategies such as ART at first visit, harm reduction, and integration of HIV and substance use facilities clearly play an important role in reaching optimal HIV care outcomes. When designing HIV policies and interventions among populations with a high prevalence of drug use, there is no single pathway, but achieving food security as part of a complex system in combination with other important interventions, such as ART at first visit, might be part of the solution (55).
This observational study has several limitations, which may affect the generalizability of its results. Based on the magnitudes of associations that were observed, the study was likely underpowered to detect the relationships of interest. For example, in post-hoc power calculations for the primary outcome CD4 cell count, assuming moderate correlation among repeated measures (rho=0.5), an average of 2 repeated measures and the standard deviations observed at baseline, the minimum difference that the study can detect with 80% power is 120 cells/mm3 for those with severe FI vs. those who are food secure and 111 cells/mm3 for those with mild/moderate FI vs. those who are food secure. Also, our assessment of FI was self-reported and potentially subject to recall bias.
In summary, in examining the relationship between food insecurity and HIV disease progression among HIV-infected individuals not on ART, we were unable to detect an association between these measures. There are several possible explanations for the discrepancies in our findings compared to previous published work. Our sample included a higher proportion of people who use drugs, who may represent a different patient population than those reported previously. It is also possible that the study was underpowered to detect associations with modest changes of CD4 cell count and HIV viral load. Finally, suboptimal adherence to ART is an important mechanism for how food insecurity contributes to worse HIV clinical outcomes, and this mechanism may only be relevant among people on ART. Food security is a desirable goal for overall health and shown beneficial for those on ART, however it does not appear to be associated with HIV disease progression among those with high prevalence of substance use and not yet on ART.
Acknowledgments
Dr. Idrisov was funded by The National Institute on Drug Abuse (NIDA) International Program INVEST Drug Abuse Research Fellowship. The study was supported by the following NIH grant funding: U01AA020780, U24AA020778, U24AA020779, U01AA021989, R25DA013582, K99DA041245, P30AI042853.
Footnotes
Compliance with Ethical Standards
Conflict of interest: The authors declare that they have no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.FAO, WFP, and IFAD. The State of Food Insecurity in the World: Economic growth is necessary but not sufficient to accelerate reduction of hunger and malnutrition. Rome: FAO; 2012. Available from: http://www.fao.org/docrep/016/i3027e/i3027e.pdf (accessed 5 July 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.FAO, WFP, and IFAD. The State of Food Insecurity in the World 2015 Meeting the 2015 international hunger targets: taking stock of uneven progress. Rome: FAO; 2015. 2015. Available from: http://www.fao.org/3/a-i4646e.pdf (accessed 5 July 2016) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.GBD 2015 SDG Collaborators. Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1813–50. doi: 10.1016/S0140-6736(16)31467-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.United Nations. Sustainable Development Knowledge Platform. Goal 2: End hunger, achieve food security and improved nutrition and promote sustainable agriculture. 2014 Available from: https://sustainabledevelopment.un.org/?page=view&nr=164&type=230&menu=2016 (accessed 5 July 2016)
- 5.Young S, Wheeler AC, McCoy SI, Weiser SD. A review of the role of food insecurity in adherence to care and treatment among adult and pediatric populations living with HIV and AIDS. AIDS Behav. 2014;18(Suppl 5):S505–15. doi: 10.1007/s10461-013-0547-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anema A, Fielden SJ, Castleman T, Grede N, Heap A, Bloem M. Food security in the context of HIV: towards harmonized definitions and indicators. AIDS Behav. 2014;18(Suppl 5):S476–89. doi: 10.1007/s10461-013-0659-x. [DOI] [PubMed] [Google Scholar]
- 7.Aibibula W, Cox J, Hamelin AM, Mamiya H, Klein MB, Brassard P. Food insecurity and low CD4 count among HIV-infected people: a systematic review and meta-analysis. AIDS Care. 2016;28(12):1577–85. doi: 10.1080/09540121.2016.1191613. [DOI] [PubMed] [Google Scholar]
- 8.Aberman NL, Rawat R, Drimie S, Claros JM, Kadiyala S. Food security and nutrition interventions in response to the AIDS epidemic: assessing global action and evidence. AIDS Behav. 2014;18(Suppl 5):S554–65. doi: 10.1007/s10461-014-0822-z. [DOI] [PubMed] [Google Scholar]
- 9.Anema A, Vogenthaler N, Frongillo EA, Kadiyala S, Weiser SD. Food insecurity and HIV/AIDS: current knowledge, gaps, and research priorities. Curr HIV/AIDS Rep. 2009;6(4):224–31. doi: 10.1007/s11904-009-0030-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Surratt HL, O’Grady CL, Levi-Minzi MA, Kurtz SP. Medication adherence challenges among HIV positive substance abusers: the role of food and housing insecurity. AIDS Care. 2015;27(3):307–14. doi: 10.1080/09540121.2014.967656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kalichman SC, Washington C, Grebler T, et al. Treatment outcomes among people living with HIV who are food insecure and prescribed antiretrovirals taken with food. J Prim Care Community Health. 2015;6(1):35–40. doi: 10.1177/2150131914549055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hong SY, Fanelli TJ, Jonas A, et al. Household food insecurity associated with antiretroviral therapy adherence among HIV-infected patients in Windhoek, Namibia. J Acquir Immune Defic Syndr. 2014;67(4):e115–22. doi: 10.1097/QAI.0000000000000308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pellowski JA, Kalichman SC, Cherry S, et al. Thedaily relationship between aspects of food insecurity and medication adherence among people living with HIV with recent experiences of hunger. Ann Behav Med. 2016;50(6):844–53. doi: 10.1007/s12160-016-9812-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kalichman SC, Washington C, Grebler T, et al. Medication adherence and health outcomes of people living with HIV who are food insecure and prescribed antiretrovirals that should be taken with food. Infect Dis Ther. 2015 Jan 23; doi: 10.1007/s40121-015-0057-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sicotte M, Langlois EV, Aho J, Ziegler D, Zunzunegui MV. Association between nutritional status and the immune response in HIV + patients under HAART: protocol for a systematic review. Syst Rev. 2014;3:9. doi: 10.1186/2046-4053-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Anema A, Kerr T, Milloy MJ, Feng C, Montaner JS, Wood E. Relationship between hunger, adherence to antiretroviral therapy and plasma HIV RNA suppression among HIV-positive illicit drug users in a Canadian setting. AIDS Care. 2014;26(4):459–65. doi: 10.1080/09540121.2013.832724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Carter GM, Indyk D, Johnson M, et al. Micronutrients in HIV: a Bayesian meta-analysis. PLoS One. 2015;10(4):e0120113. doi: 10.1371/journal.pone.0120113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Drain PK, Kupka R, Mugusi F, Fawzi WW. Micronutrients in HIV-positive persons receiving highly active antiretroviral therapy. Am J Clin Nutr. 2007;85(2):333–45. doi: 10.1093/ajcn/85.2.333. [DOI] [PubMed] [Google Scholar]
- 19.de Pee S, Semba RD. Role of nutrition in HIV infection: review of evidence for more effective programming in resource-limited settings. Food Nutr Bull. 2010;31(4):S313–44. [PubMed] [Google Scholar]
- 20.Frega R, Duffy F, Rawat R, Grede N. Food insecurity in the context of HIV/AIDS: a framework for a new era of programming. Food Nutrition Bull. 2010;31(4):S292–312. [PubMed] [Google Scholar]
- 21.Weiser SD, Young SL, Cohen CR, et al. Conceptual framework for understanding the bidirectional links between food insecurity and HIV/AIDS. Am J Clin Nutr. 2011;94(6):1729s–39s. doi: 10.3945/ajcn.111.012070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lunze K, Yurasova E, Idrisov B, Gnatienko N, Migliorini L. Food security and nutrition in the Russian Federation – a health policy analysis. Glob Health Action. 2015;8:27537. doi: 10.3402/gha.v8.27537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Idrisov B, Lunze K, Cheng DM, et al. Food insecurity and HIV drug and sex risk behaviors among Russians living with HIV. Poster presented at: College on Problems of Drug Dependence 77th Annual Scientific Meeting & NIDA International Forum; 2015 June; Phoenix, AZ. [Google Scholar]
- 24.Patts GJ, Cheng DM, Emenyonu N, et al. Alcohol use and food insecurity among people living with HIV in Mbarara, Uganda and St. Petersburg, Russia. AIDS Behav. 2017;21(3):724–33. doi: 10.1007/s10461-016-1556-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Guriev S. Deglobalizing Russia. Carnegie Moscow Center. 2015 Available from: http://carnegie.ru/2015/12/16/deglobalizing-russia-pub-62294 (accessed 5 July 2016)
- 26.Stanovaya T. Destroy at any cost: the political rationale behind Russia’s food burnings. Carnegie Moscow Center. 2015 Available from: http://carnegie.ru/commentary/?fa=61021 (accessed 5 July 2016)
- 27.Wegren SK, Nikulin AM, Trotsuk I. The Russian variant of food security. Problems of post-communism. 2016:1–16. [Google Scholar]
- 28.GBD 2015 HIV Collaborators. Estimates of global, regional, and national incidence, prevalence, and mortality of HIV, 1980–2015: the Global Burden of Disease Study 2015. Lancet HIV. 2016;3(8):e361–87. doi: 10.1016/S2352-3018(16)30087-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dukhovlinova E, Masharsky A, Toussova O, et al. Two independent HIV epidemics in Saint Petersburg, Russia revealed by molecular epidemiology. AIDS Res Hum Retroviruses. 2015;31(6):608–14. doi: 10.1089/aid.2014.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ministry of Health. HIV infection in Russia Federal Research Center for HIV/AIDS Prevention and Treatment [Russian] 2015 Available from: http://aids-centr.perm.ru//Статистика/ВИЧ/СПИД-в-России (accessed 5 July 2016)
- 31.NIH. Research Portfolio Online Reporting Tools (RePORT) Project Information. 2016 Available from: https://projectreporter.nih.gov/project_info_description.cfm?aid=8210505&icde=11361542 (Accessed 19 Oct 2016)
- 32.Chesney MA, Ickovics JR, Chambers DB, et al. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: the AACTG adherence instruments. Patient Care Committee & Adherence Working Group of the Outcomes Committee of the Adult AIDS Clinical Trials Group (AACTG) AIDS Care. 2000;12(3):255–66. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- 33.Mazus A, G K, Zimina V, et al. National Clinical Guidlines for HIV Diagnostics and Treatment among Adults [Russian] Moscow: 2014. Available from: http://www.spid.ru/spid/ru/articles/o_1119 (accessed 5 July 2016) [Google Scholar]
- 34.Coates J, Swindale A, Bilinsky P. Household Food Insecurity Access Scale (HFIAS) for measurement of food access: indicator guide. Washington, DC: Food and Nutrition Technical Assistance Project, Academy for Educational Development; 2007. [Google Scholar]
- 35.Iacobucci D, Posavac SS, Kardes FR, Schneider M, Popovich DL. The median split: robust, refined, and revived. J Consum Psychol. 2015;25(4):690–704. [Google Scholar]
- 36.Fleishman JA, Sherbourne CD, Crystal S, et al. Coping, conflictual social interactions, social support, and mood among HIV-infected persons. HCSUS Consortium. Am J Community Psychol. 2000;28(4):421–53. doi: 10.1023/a:1005132430171. [DOI] [PubMed] [Google Scholar]
- 37.Chishinga N, Kinyanda E, Weiss HA, Patel V, Ayles H, Seedat S. Validation of brief screening tools for depressive and alcohol use disorders among TB and HIV patients in primary care in Zambia. BMC Psychiatry. 2011;11:75. doi: 10.1186/1471-244X-11-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Radloff LS. The CES-D scale a self-report depression scale for research in the general population. Appl Psychol Meas. 1977;1(3):385–401. [Google Scholar]
- 39.Weatherby NL, Needle R, Cesari H, et al. Validity of self-reported drug use among injection drug users and crack cocaine users recruited through street outreach. Eval Program Plann. 1994;17:347–55. [Google Scholar]
- 40.Needle R, Fisher DG, Weatherby N, et al. Reliability of self-reported HIV risk behaviors of drug users. Psychol Addict Behav. 1995;9(4):242. [Google Scholar]
- 41.Sobell LC, Sobell MB. Alcohol Timeline Followback (TLFB) Users’ Manual. Toronto, Canada: Addiction Research Foundation; 1995. [Google Scholar]
- 42.Danishevski K, Balabanova D, McKee M, Atkinson S. The fragmentary federation: experiences with the decentralized health system in Russia. Health Policy Plan. 2006;21(3):183–94. doi: 10.1093/heapol/czl002. [DOI] [PubMed] [Google Scholar]
- 43.Prime minister Dmitry Medvedev warns that Russia is facing shortages of HIV drugs and testing kits. Meduza; 2015. Oct 23, Available from: https://meduza.io/en/news/2015/10/23/prime-minister-dmitry-medvedev-warns-that-russia-is-facing-shortages-of-hiv-drugs-and-testing-kits (accessed 11 Oct 2016) [Google Scholar]
- 44.Anema A, Weiser SD, Fernandes KA, et al. High prevalence of food insecurity among HIV-infected individuals receiving HAART in a resource-rich setting. AIDS Care. 2011;23(2):221–30. doi: 10.1080/09540121.2010.498908. [DOI] [PubMed] [Google Scholar]
- 45.Kalichman SC, Cherry C, Amaral C, et al. Health and treatment implications of food insufficiency among people living with HIV/AIDS, Atlanta, Georgia. J Urban Health. 2010;87(4):631–41. doi: 10.1007/s11524-010-9446-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Vogenthaler NS, Hadley C, Lewis SJ, Rodriguez AE, Metsch LR, del Rio C. Food insufficiency among HIV-infected crack-cocaine users in Atlanta and Miami. Public Health Nutr. 2010;13(09):1478–84. doi: 10.1017/S1368980009993181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Anema A, Weiser SD, Fernandes KA, et al. High prevalence of food insecurity among HIV-infected individuals receiving HAART in a resource-rich setting. AIDS Care. 2011;23(2):221–30. doi: 10.1080/09540121.2010.498908. [DOI] [PubMed] [Google Scholar]
- 48.Kalichman SC, Pellowski J, Kalichman MO, et al. Food insufficiency and medication adherence among people living with HIV/AIDS in urban and peri-urban settings. Prevention Sci. 2011;12(3):324–32. doi: 10.1007/s11121-011-0222-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Wang EA, McGinnis KA, Fiellin DA, et al. Food insecurity is associated with poor virologic response among HIV-infected patients receiving antiretroviral medications. J Gen Intern Med. 2011;26(9):1012–8. doi: 10.1007/s11606-011-1723-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Weiser SD, Frongillo EA, Ragland K, Hogg RS, Riley ED, Bangsberg DR. Food insecurity is associated with incomplete HIV RNA suppression among homeless and marginally housed HIV-infected individuals in San Francisco. J Gen Intern Med. 2009;24(1):14–20. doi: 10.1007/s11606-008-0824-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.McMahon JH, Wanke CA, Elliott JH, Skinner S, Tang AM. Repeated assessments of food security predict CD4 change in the setting of antiretroviral therapy. J Acquir Immune Defic Syndr. 2011;58(1):60–3. doi: 10.1097/QAI.0b013e318227f8dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Singer AW, Weiser SD, McCoy SI. Does food insecurity undermine adherence to antiretroviral therapy? A systematic review. AIDS Behav. 2015;19(8):1510–26. doi: 10.1007/s10461-014-0873-1. [DOI] [PubMed] [Google Scholar]
- 53.Weiser SD, Yuan C, Guzman D, et al. Food insecurity and HIV clinical outcomes in a longitudinal study of urban homeless and marginally housed HIV-infected individuals. AIDS. 2013;27(18):2953–8. doi: 10.1097/01.aids.0000432538.70088.a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.WHO. Social determinants of health: Key concepts. 2016 Available from: http://www.who.int/social_determinants/thecommission/finalreport/key_concepts/en/ (accessed 19 Oct 2016)
- 55.Rutter H, Savona N, Glonti K, et al. The need for a complex systems model of evidence for public health. Lancet. 2017 Jun 13; doi: 10.1016/S0140-6736(17)31267-9. pii: S0140-6736(17)31267-9. [DOI] [PubMed] [Google Scholar]


