INTRODUCTION
In community-academic research partnerships, a diverse group of stakeholders, commonly including community members, healthcare providers, and academic researchers, collaborate for the purpose of sharing authority and responsibility in planning and implementing research studies with a mutually beneficial research objective.1,2,3 Research approaches that involve the community as an active partner in addressing health and social concerns are ample and, since the latter part of the 20th century, have become increasingly recognized as an important model for health research.4,5 These approaches are especially needed to engage racial and ethnic minorities who have been historically underrepresented in research studies and who have many reasons to mistrust health research, including cases of unethical research in the past.6–10
The continuum of community participation in research ranges from outreach (some involvement, one-way communication), to consultation (more involvement, two-way communication, connections), to collaboration (community involvement, partnership/trust building), to shared leadership (strong bi-directional relation-ship, joint decision-making, trust).11,12 On this continuum, community-based participatory research (CBPR) is defined by shared decision-making and involvement of all partners in all aspects of the research project and has emerged as a particularly viable approach to improve trust and involvement of underrepresented groups in health research.13 These community-academic research partnerships give everyone a voice in the research enterprise, which is also a tenet of social justice.14–16
Prominent national and international health agencies such as the National Institutes of Health (NIH), Institute of Medicine (IOM), Agency for Healthcare Research and Quality (AHRQ), Patient-Centered Outcomes Research Institute (PCORI) and others, recommend conducting research driven by community-academic partnerships because of their potential to: a) improve the quality and relevance of research; b) increase community capacity to affect change; and, c) alleviate persistent health disparities in historically underserved communities.17–20 It is recognized that the success of community-academic research partnerships is largely dependent on the partnership’s ability to create and maintain trust between a diverse group of stakeholders with varied interests, goals, and values.21 This is a particularly important factor for the success of research efforts in underserved communities.22 Yet, trust continues to remain a poorly understood aspect of community-academic research partnerships.23
Trust is a concept that has been empirically defined in various ways. A common definition of trust is “the willingness of a party to be vulnerable to the actions of another party based on the expectation that the other will perform a particular action important to the trustor, irrespective of the ability to monitor or control the other party.”24 Many researchers note that the concept of trust must be understood from the perspective of all parties and within its context.25,26 In the context of community-academic research partnerships, researchers expound the importance of trust by sharing descriptions of the practices and principles they followed to achieve trusting relationships or by measuring trust as an important outcome of the participatory research process.27–29 However, to date, few studies have identified empirically sound or practical measures of trust for community-academic research partnerships to build from.
To address this gap, we, a community-academic research partnership, conducted a multi-site, multi-institutional study with the purpose of developing a conceptual framework of trust in community-academic research partnerships. Our primary aim was to include the perspectives of major types of stakeholders in order to identify factors that contribute to trust within community-academic research partnerships from the perspectives of community members’, academic researchers’ and healthcare providers’. Our secondary aim was to evaluate the relative importance of the identified factors for creating and maintaining trust within partnerships as well as for improving public trust in research more generally.
METHOD
We used concept mapping, a mixed methods approach that uses structured participatory processes and rigorous data analyses to elicit, integrate, and organize the perspectives of multiple individuals into a conceptual framework. Additional information on the methods used in this study are described by Frerichs et al.30 Originally developed by Trochim, this method produces a conceptual framework for how a group views a topic. In 2005, Burke et al introduced concept mapping as a participatory public health research method and since then it has been used to address a wide range of health topics in several community engaged research projects.31 The visual representation of the group’s collective thoughts relative to a topic of interest (i.e. concept map) is a helpful tool in determining elements of complex or abstract concepts such as trust.28 All research protocols were approved by the institutional review board at each collaborating site.
Setting
This study involved five NIH-funded Clinical and Translational Science Award (CTSA) grantees: University of North Carolina at Chapel Hill (UNC), University of Arkansas for Medical Sciences (UAMS), University of Florida (UF), University of California, Los Angeles (UCLA) and University of Pittsburgh (PITT). PITT served as the data coordinating site and facilitated trainings, data collection sessions, and analyses and reporting of the study findings. UNC, UAMS, UF, and UCLA, each recruited participants and collected data at their respective sites. A steering committee that included representatives from each CTSA, including both academic and community partners, met monthly via conference, to plan the study, review progress, and guide dissemination of study findings.
Participants and Sampling
Respondent-driven sampling, a non-probabilistic sampling method, was used to identify key informants in three major stakeholder groups: (1) community members, (2) healthcare providers, and (3) academic researchers. Each CTSA recruited initial participants using existing research network and community research partner lists, and invited recruited participants to identify potential participants for invitation to the study. Each site also purposively sampled from populations most affected by health disparities within their respective regions. We recruited community members with and without previous experience in community-engaged research in order to obtain a more representative community perspective and mitigate potential selection bias of participants who are more inclined to participate and trust in health research. Healthcare providers had to self-identify as representing a healthcare agency (e.g., hospitals, public health department, primary care clinic), and have a primary role that was not academic research but have at least some experience in community-engaged research projects (e.g., co-investigator, data collection, research design, etc.). Similarly, academic researchers had to self-identify as having at least some experience in community-engaged research projects.32 All participants received incentives for their time and travel reimbursement for participation in the study.
Concept Mapping Procedures
All participants were asked to complete a brief, self-administered on-line questionnaire that included demographic variables (e.g. age, race, education) and years of community-engaged research experience. Each site followed the standard concept mapping research process, and the same cohort of participants from each CTSA site were involved in three major group activities: (1) brainstorming, (2) sorting and rating, and (3) analysis and interpretation.33 At least one academic partner and one community member partnered as co-facilitators for all group sessions. Each facilitator completed a training webinar, led by the PITT data coordinating team on the concept mapping research process and session procedures.
Brainstorming
Brainstorming sessions were conducted at each CTSA site either online or in a face-to-face format for each stakeholder group. This varied by site and stakeholder group, however all stakeholders were asked the same question. During this session, the participants were asked to think about their impressions or experiences with research, and respond to the following prompt: “Based on your experience(s), list all the things that you think can contribute to trust between community and academic partners in research?” After all sites completed brainstorming sessions, the data coordinating site consolidated all items into a final master list by combining similar items and removing duplicates.34
Sorting and Rating
Participants completed sorting and rating activities either in-person or online. Individuals who participated online, directly sorted and rated items using the Concept Systems Global Max© online platform (Concept Systems Inc. Ithaca, NY). Sorting and rating data from in-person sessions were entered into the online platform by research staff. For the sorting component, participants were asked to individually sort items from the master list into distinct piles based on how they perceived the items to be related to each other. There was no right or wrong way to sort the items. Then, participants were asked to rate each item based on the following questions using a Likert-type scale of 1 (not at all) to 5 (extremely):
How important is this item for creating trust between community and academic partners in research?
How important is this item for maintaining trust between community and academic partners in research?
How important is this item for supporting public trust in research more generally?
Analysis and interpretation
All analyses were completed in the Concept Systems Global Max©. Multidimensional scaling was used to create a visual illustration of the sorting data across all participants in a spatially oriented map of the statements, called a point map. The point map was created by summing all participant’s individual similarity matrices of sort data (i.e., N × N binary matrix of sorted items where similarities, Xij, are 1 if items i and j were sorted together, or 0 otherwise) into a total similarity matrix, Tij, which was analyzed using non-metric multidimensional scaling to yield a two-dimensional (x,y) map of each statement.35 The map visually places each statement in the two-dimensional space that locates statements together based on how frequently they were sorted together (i.e., statements closest together were sorted together more frequently and furthest apart, less frequently). Next, hierarchical cluster analysis was used to partition the two-dimensional point map into non-overlapping clusters.36 A range in the number of clusters for partitioning were evaluated systematically, and a five-cluster solution was selected by stakeholders as most appropriate for the final concept map. We calculated the bridging values for each cluster, which are calculated by averaging the bridging values for each statement. Statement bridging values range from 0 to 1, with a lower value indicating it was sorted by many people with statements adjacent to it and a higher value indicating it was sorted with statements somewhat distant in multiple directions. Thus, clusters with lower bridging values are usually more cohesive and reflect the content well in that part of the map.
We also created pattern-matching graphs and conducted go-zone analyses to aid in further interpretation. The pattern-matching graphs allow for visual examination of rating variables across groups or clusters. We used the tool to assess the average rating of creating trust, maintaining trust, and public trust in research for each cluster. Go-zone analyses create a bivariate plot of item ratings to examine the relationship between two rating variables. We plotted the importance for creating trust on the x-axis and the importance for maintaining trust on the y-axis. The plot identifies items in four quadrants (high on both ratings, low on both ratings, high on one and low on the other rating and vice versa).
Finally, all sites held at least one interpretation session either as a webinar or in-person format. During the interpretation session, visual maps and results were presented to the participants. Participants were asked to discuss and review the five clusters and items within each to identify the themes and provide a suggested name for each cluster. All sites provided their suggested names to the steering committee, who condensed and synthesized suggestions into final labels for each cluster. After naming the clusters, pathways and linkages between the items were discussed.
RESULTS
Demographic Characteristics
A total of 186 participants attended one or more concept mapping sessions from each of the four data collecting sites (see table 1). A majority of the participants were females (74.8%) and non-Hispanic. Approximately half the respondents were Caucasians (47.9%) or African American (42.2%). Each site recruited 37–65 participants with a mean sample of 44 individuals per site. Academic researchers were most highly represented in the sample (n=74, 39.7%) followed by community members (n=65, 25.4%) and healthcare providers (n=47, 25.4%). Most of our sample (n=151, 88.3%) had some experience with community-academic research partnerships.
Table 1.
Demographic Characteristics of Respondents* in the Trust Concept Mapping Project, 2014–2015
| Personal Characteristics | Total N (186) |
% |
|---|---|---|
| Gender | ||
| Female | 128 | 74.8 |
| Male | 43 | 25.2 |
| Race | ||
| Caucasian | 82 | 47.9 |
| African American | 72 | 42.2 |
| Asian/Pacific Islander | 15 | 8.7 |
| American Indian | 2 | 1.2 |
| Ethnicity | ||
| Hispanic/Latino | 17 | 10.1 |
| Non-Hispanic/Latino | 152 | 89.9 |
| Location | ||
| UNC | 65 | 34.0 |
| UAMS | 43 | 23.2 |
| UCLA | 41 | 22.0 |
| UFL | 37 | 20.8 |
| Role | ||
| Community Members | 65 | 35.0 |
| Academicians | 74 | 39.7 |
| Healthcare Providers | 47 | 25.4 |
| Years of Experience with Community-Academic Research Partnerships | ||
| None | 20 | 11.7 |
| < 1 year | 5 | 2.9 |
| 1–5 years | 44 | 25.7 |
| > 5 years | 102 | 59.7 |
Totals do not sum to the sample size due to missing data.
Items and Clusters of Factors that Contribute to Trust
Participants generated a total of 2,172 individual responses to the prompt requesting items that contribute to trust in community-academic research partnerships. A final master list of 125 condensed items (after removing duplicates and merging similar items) is provided in table 2. A point-series map (see figure 1) visualizes each of the 125 items with a point (represented by a number) and places the points in relationship to each other based on how frequently the items were sorted together based on similarity i.e. points that are closest to each other are items that were sorted together more frequently and points that are further away from each other were sorted together less frequently. For example, ‘Reputation and track-record of academic institutions’ (item 26) was perceived to be closely related to ‘Skills and credentials of academic researchers’ (item 67). Conversely, “Availability of funding” (item 52) and “Perceptions that partner’s motives are pure” (item 112) were not perceived to be closely related. The final cluster map for all participants included 5 clusters (Figure 2), with the smallest cluster containing 13 items and the largest containing 37 items. The stress value of the five cluster solution was .31. Stress values can range from 0 to 1.0, with lower values indicating better fit. Maps with stress values below 0.39 have less than 1% probability of having either no structure or a random configuration.37
Table 2.
Names of the five clusters, definitions, and items
| Name | Definition | Example Items |
|---|---|---|
| Communication, credibility and methodology to anticipate and resolve problems | This dimension considers the infrastructure in place to manage on-the-ground and day-to-day realities of research that occurs within community-academic partnerships. | 1. Ease of access to services 22. Dissemination of information/data/results/outcomes to community in methods other than publications 73. Realistic and clearly defined expectations about the research project for all parties 78. Memorandums of Understanding outlining roles, responsibilities, data sharing/ownership, handling disagreements, manuscript authorship, ownership of products 105. Academic researcher experience and track-record with community and engaged research |
| Committed partnerships | This dimension is related to the level of engagement of the partners involved in community-academic research partnerships and their investment in ensuring the its maintenance. | 19. Organized/productive community advisory board that is representative of the community 41. Inclusion of community representation on research team in addition to community advisory board; being inclusive 43. Academic researcher present in the community including showing up at community events not directly related to research 77. Long term commitment to partnership - even when the research ends, the relationship is not over 125. Having community partners participate in all phases of research - hypothesis development, study design, analysis, presentation of results, and as coauthors on publications |
| Sustainability | This dimension consists of statements that relate to the capacity and resources of community-academic research partnerships to continue for long periods of time. | 18. Staffing - Ensuring that research duties are not “added on” to full-time community members’ jobs but that there is sufficient funding to buy out a portion of their time 92. Training programs for researchers, which includes how to use community-engaged approaches and the many aspects to consider when working with communities 101. Equitable funding arrangements and compensation 108. Training opportunities for community partners 117. Capacity building and empowerment of community partners |
| Authentic, effective, and transparent communication | This dimension considers the broad and varied importance of on-going and effective communication between community and academic research partnerships. | 4. Maintaining a feedback loop between participants and researchers/bi-directional communication throughout all phases of research 23. Spending that extra, less formal time together before and after meetings/be human together 36. Honesty & full disclosure/no hidden agenda 84. Personality of community member(s) - such as kind, selfless, sincere, fair, curious, humble and modest 94. Personality of researcher(s) - such as kind, selfless, sincere, fair, curious, humble and modest |
| Mutually respectful and reciprocal relationships | This dimension includes statements that represent the on-going exchange of information and resources that take place between the individuals involved in community-academic research partnerships. | 50. Assuring a mutual “win” for all at the table 54. Equal participation in and prioritization of projects by academic and community partners 66. Shared power and decision making - acknowledge, minimize or address perceived power differentials and imbalances 99. Dependability on each other - community to academic and academic to community 113. Community partners welcoming and taking time with academic researchers to show them their community |
Figure 1.
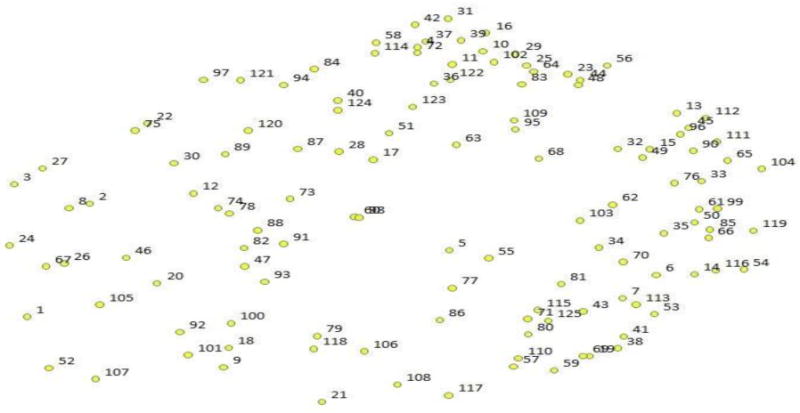
125 items point series map
Figure 2.
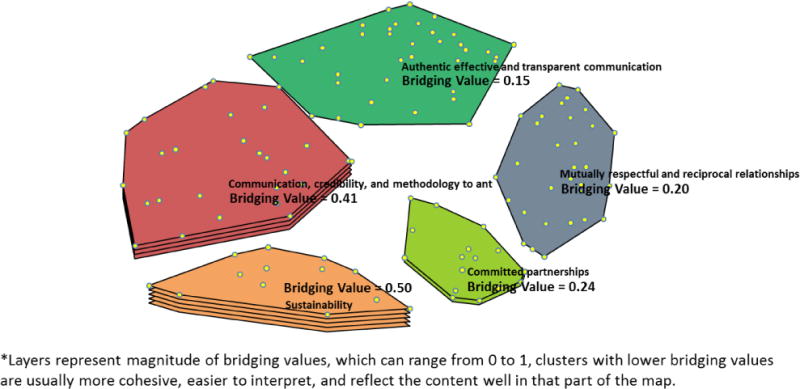
Final Five Cluster Bridging Map with Bridging Values*
The final five clusters representing factors that contribute to trust in community-academic research partnerships, were named as follows: 1) authentic, effective and transparent communication, 2) mutually respectful and reciprocal relationships, 3) sustainability, 4) committed partnerships and, 5) communication, credibility and methodology to anticipate and resolve problems. Figure 2 depicts the 125 statements related spatially to the five clusters, and the number of cluster layers represents bridging values (fewer layers indicate lower bridging values). Authentic, effective and transparent communication had the lowest bridging value (0.15), sustainability had the highest (0.50).
Importance Ratings of Items and Clusters
Figure 3 provides a pattern-matching graph for each of the three importance ratings: (1) creating trust, (2) maintaining trust, and (3) supporting public trust in research. As indicated by the graph, “authentic, effective and transparent communication” and “mutually respectful and reciprocal relationships” were rated with the highest levels of importance for all three importance ratings. Relatively speaking, “committed partnerships” had higher ratings of importance for supporting public trust in research than for creating or maintaining trust. Because of the relatively high importance ratings of the “authentic, effective and transparent communication” and “mutually respectful and reciprocal relationships” clusters, the individual statements were examined with go-zone analysis. The go-zone analysis identified the statements with the highest importance for creating and maintaining trust ratings in these clusters (see table 3).
Figure 3.
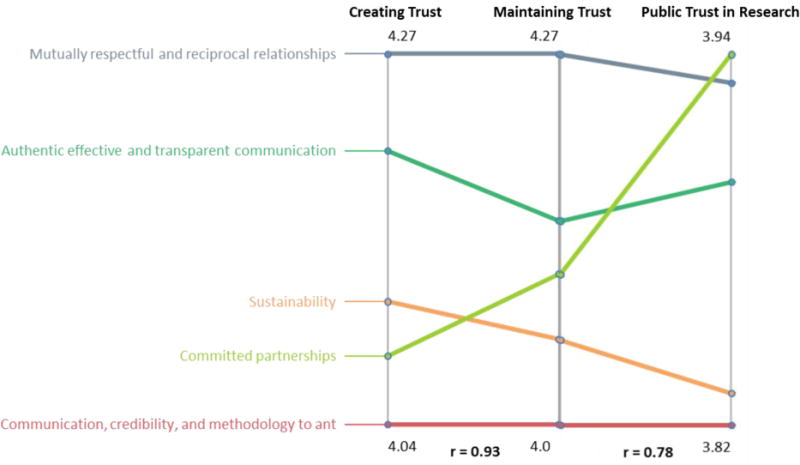
Pattern-Matching results indicating importance rating variables by cluster
Table 3.
Statements in the “mutually respectful and reciprocal relationships” and “authentic, effective, and transparent communication” clusters with highest importance ratings for both creating and maintaining trust
| Mutually respectful and reciprocal relationships | Authentic, effective, and transparent communication |
|---|---|
| 13. Reliability ‐ ability to depend on each other* | 4. Maintaining a feedback loop between participants and researchers/bi-directional communication throughout all phases of research* |
| 45. Treating people as you want to be treated ‐ including treating community as participants rather than as “subjects”* | 10. Encouraging feedback and engaging in active, non-judgmental listening during the collaborative research process |
| 53. Asking for, valuing and incorporating community input at all phases of research project | 16. Communication - avoid talking over someone else and give all partners time to express opinions |
| 61. Shared goals, missions, and objectives | 17. Transparency by all parties of all project goals and expectations for involvement/time; including objectives, data, personnel, budget, compensation* |
| 62. Accountability of all partners throughout the research process* | 28. Maintaining confidentiality at all times - private information should stay private* |
| 65. Mutual recognition of strengths and unique capabilities of all partners | 36. Honesty & full disclosure/no hidden agenda* |
| 66. Shared power and decision making ‐ acknowledge, minimize or address perceived power differentials and imbalances | 37. Clear communication for everyone (benefits, purpose, expectations, constrictions, requirements)* |
| 76. Valuing each other’s strength and expertise ‐ what each person brings to the research (community and academic)* | 40. Leadership style - open, respectful, warm, modest, having concern, knowledge |
| 90. Rapport between community and academic partners | 42. Communication about changes, challenges and project updates, and why things may not be done |
| 96. Mutual respect and acceptance of differences, including differences in expertise* | 44. Sensitivity/sensitive issues - address as they arise |
| 99. Dependability on each other ‐ community to academic and academic to community | 48. Taking responsibility for and forgiving mistakes and issues as they arise (such as offending someone inadvertently) |
| 104. All partners keep commitments/promises and obligations to each other; dependability on each other ‐ community to academic and academic to community* | 51. Cultural awareness and humility and appropriateness |
| 111. Loyalty and “having a partner’s back” | 58. Communicate findings and learned knowledge to the community |
| 119. Mutual motivation and passion about a research project/public health issue | 63. Follow through/backing words with actions* |
| 64. Conflict resolution/conflict negotiation/compromise (agree to disagree; challenges/problems can be addressed without confrontation or intimidation) | |
| 72. Using language that is understood by both parties but is not speaking down to anyone; avoid using acronyms* | |
| 87. Follow “first do no harm” (physical, mental, financial) | |
| 102. Frequent/regular and direct communication both ways between academic research and community partners | |
| 109. Checking in with the community to make sure what you understand is what the community understands as well | |
| 114. Establishing a policy of encouraging questions, contact, and communication |
Statements represent those in the top 6 highest ratings on both creating and maintaining trust
In regard to mutually respectful and reciprocal relationships, three of the six statements with highest ratings related to qualities that suggest being able to count or rely upon someone (e.g., reliability, dependability, accountability), and the other three statements related to showing regard for other individuals in respectful ways (e.g., “treating people as you want to be treated”, valuing other’s strengths). Of the six highest rated statements in “communication”, two related to clarity of communication (i.e., “clear communication for everyone” and “using language that is understood by both parties…”), two related to transparency of communication (i.e., “transparency by all parties…” and “honesty and full disclosure..”), one specifically identified “bi-directional communication throughout all phases of research” and one identified “…backing words with action.”
DISCUSSION
Our study led to the development of a novel, empirically-derived framework of trust in community-academic research partnerships. The framework consisted of five main clusters of trust-related factors: 1) authentic, effective and transparent communication, 2) mutually respectful and reciprocal relationships, 3) sustainability, 4) committed partnerships and, 5) communication, credibility and methodology to anticipate and resolve problems. Two clusters, i.e., authentic, effective and transparent communication and mutually respectful and reciprocal relationships, had lower bridging values, reflecting more cohesive concepts. Overall these two clusters were rated with the highest importance ratings for creating and maintaining trust in partnerships and supporting public trust in research. This suggests a relative coherence and importance of these factors. Committed partnerships cluster was rated with higher importance for supporting public trust in research more generally, as compared to its rating for creating and maintaining trust. Interpreting our findings as they relate to trust in community partnered relationships provide a new roadmap to help guide community-engaged and participatory research toward key factors that build trust, and improve our assessment of trust in community-academic research partnerships. Our work provides a more tangible definition of what “trust”, (a very abstract concept) is. This will also aid in the development of measures to assess the various components of trust, a multi-dimensional construct, based on our findings.
Our work provides important research evidence that is aligned with and can enhance our understanding of theoretical and logic-based models and frameworks of community-academic research partnerships.38 For example, the CTSA’s logic model for community engagement notes that community-university bi-directional trust and reduced barriers to communication and collaboration are key parts of a “critical foundation for community-engaged research success.”22 The CTSA logic models places trust and reduced barriers to communication and collaboration each as short-term outcomes. Our findings indicate that factors aligned with the notion of reduced barriers to communication and collaboration, i.e., “authentic, effective and transparent communication” and “communication, credibility and methodology to anticipate and resolve problems”, are important factors for creating trust. Thus, trust may actually be an intermediate result stemming from work to reduce barriers to communication and collaboration as opposed to a short term result. Our findings align and enhance the understanding of theoretical frameworks of community-academic research partnerships.39
The findings here emphasize the importance of quality, bi-directional communication and relationships in establishing trust, consistent with other scholars in community-academic research.22 More specifically, transparency in communication and by its extension transparency among research partners has been identified as key indicators for community-based research partnership readiness. Similarly, Ahmed and Palermo assert that successful community-engaged is a result of ongoing communication between all involved stakeholders. In our study, “authentic, effective and transparent communication” was one of the highly rated clusters in terms of creating, maintaining and supporting public trust in research.40 Furthermore, our results also indicated the cluster, “mutually respectful and reciprocal relationships”, was rated high for all three levels of importance. Aligned with this finding, the seminal work of Putnam and Carpiano identify mutuality and reciprocity as key elements and essential precursors of developing trust between individuals and their networks in a partnership.41,42
In addition to “authentic, effective and transparent communication” and “communication, credibility and methodology to anticipate and resolve problems”, “committed partnerships” was rated relatively high in importance for supporting trust in research more generally. Past research on trust in health research has emphasized the importance of addressing financial conflicts of interest.43–46 However, statements regarding financial conflicts of interest were not generated by the participants in our study as factors that contribute to trust in community-academic research partnerships. The focus on trust within the specific context of community-academic research partnerships to generate our statements versus trust in research more broadly possibly contributed to this difference.
Our finding about the importance of committed partnerships relative importance does support a key recommendation highlighted in a workshop convened in 2015 by the National Academies of Sciences, Engineering, and Medicine on public trust in science.47 The workshop members indicated that to improve public trust in research a “new trust fabric” needs to be built through “partnership, participation and peer groups.” Similarly, our findings suggest that a “new trust fabric” should be built through active partnership between communities and academic researchers. In addition, the statements within our cluster of “committed partnerships” highlighted the need for dedicated investment to the maintenance of partnerships (e.g., “long term commitment to partnership - even when the research ends, the relationship is not over” and “investing in community/invested, engaged, responsive.”)
Other partnerships may be interested in using a similar concept mapping approach to define trust; however, concept mapping requires a significant level of effort from participants through the process. We used an comprehensive and inclusive sampling strategy that resulted in a robust framework that others may draw from. For example, future research can use item-total correlation analyses to systematically reduce items to a smaller subset and subsequently have additional participants rate the smaller subset and conduct factor analyses to assess construct validity.42 This type of assessment tool may provide more utility to evaluators and planners than concept mapping. Also, future research is needed to further extrapolate and expand the items under the two clusters “sustainability” and “communication, credibility and methodology to anticipate and resolve problems”, which were sorted by more individuals with items further away, in other clusters. Conflict resolution and problem solving are cornerstones of successful partnerships. More research in these domains will allow researchers and practitioners to better understand the ideas generated and sorted by different stakeholders and translate them to actionable strategies to build and maintain trust.
LIMITATIONS
Certain limitations with our study should be noted. First, most of the sites used respondent-driven sampling to recruit our participants. Although, this was desirable to identify academic researchers and healthcare providers with experience in community-academic research partnerships, there could be distinct differences between individuals who do and do not participate in community-academic research partnerships. Researchers and providers who do not have experience in community-academic research partnerships may have a different perspective that is not represented by our research. Conversely, we did recruit community members with and without experience, and researchers and providers with varying levels of experience (from 1 year to over 10).
In particular, our study generated 125 unique statements, and participants were asked to rate each of the 125 items on 3 different Likert-type scales of importance. This did result in fewer participants fully completing the rating portion of the procedures. Finally, the differences in importance ratings were relatively small and while we have demonstrated statistically significant differences among the cluster ratings in other studies, the meaningfulness in these differences is unclear.30
CONCLUSIONS
National health funding agencies often desire or even require community engagement components to their grantees, such as PCORI and the NIH’s Clinical and Translational Science Award (CTSA) institutes. In a recent CTSA review report conducted by Institute of Medicine (IOM), the review panel recommended that the next steps for CTSAs should be to ensure community engagement in all phases of research.48 The mechanics and processes of community engagement (e.g., holding community forums, conducting needs assessments) are well-documented, but the strategies for trust building and maintenance are less clear.39 Our empirically-derived framework represents factors that contribute to trust in community-academic research partnerships from the views of key stakeholders. Although not a trivial task, the factors of our framework have potential to be operationalized into actionable strategies. For example, the domain of “mutually respectful and reciprocal relationships” suggests that partnerships should set aside specific time for an exercise where partners discuss and document what each “gives” and “gets.”
This framework may itself serve as a potential engagement tool within existing or new community-academic research collaborations to improve effective dialogue about needs for building trust. For example, partnerships can be asked to conduct a self-assessment of how well they are performing on based on factors noted as high importance from the five concept mapping clusters. Furthermore, if certain clusters/factors are considered weak, partnership members could further assess specific items within each cluster to aid in strategic planning for making improvements.
Our results have important implications for improving measurement of trust. Trust is often considered an important outcome of community-academic research partnerships; yet, there are limited measures of the trust within the context of such partnerships. Measuring a concept such as trust is challenging since it is an individual perception about a complex issue, which does not fit easily operationalized into survey scales. Concept mapping is a method to achieve this as researchers have used concept mapping to aid in the development of scales for other similarly challenging topics such as evaluation measures for a family planning program and capacity for sustainability of public health programs.39 Finally, the resulting five-cluster framework could be used to plan, design and implement training programs for the research workforce at academic institutions (e.g., CTSAs) and community organizations to foster awareness, knowledge and capacities for community-academic research partnerships. For example, trainings could specifically focus on effective communication between research partners and/or conflict resolution or and/or methods on maintaining and sustaining community-academic research partnerships.
This study is an important first step in identifying an initial set of determinants of trust that can be applied and measured across the CTSA consortium with those involved in community engagement efforts or community-academic research partnerships. This is one of the first studies that brought community members, academic researchers and healthcare providers together and discussed each one of their perspectives in creating and maintaining trust. The clusters generated in this study can be used to guide to evaluate the effectiveness of any community engaged research initiative. The findings from this study can be a foundation for effective planning and implementation of community-engaged research.
Highlights.
The aim of this pilot study was to engage stakeholders in defining determinants of trust in community academic research partnerships and to develop a framework for measuring trust.
We used concept mapping to engage three stakeholders: community members, healthcare providers and academicians.
We conducted hierarchical cluster analysis to assess the determinants of trust in community-academic research partnerships.
A five cluster solution was defined: authentic, effective and transparent communication; mutually respectful and reciprocal relationships; sustainability; committed partnerships; and, communication, credibility and methodology to anticipate and resolve problems.
Biographies
Dr. Gaurav Dave attended the University of North Carolina at Greensboro and completed a Masters and a Doctorate in Public Health in 2006 and 2011 respectively, with a concentration in public health, community-based prevention research and evaluation. Dr. Dave is affiliated with The American Evaluation Association, American Public Health Association, and The UNC Center for Health Equity Research.
Dr. Leah Frerichs received her PhD from the University of Nebraska Medical Center in Health Promotion and Disease Prevention Research and completed a postdoctoral fellowship with the Center for Health Equity Research at the University of North Carolina at Chapel Hill. Dr. Leah Frerichs is an Assistant Professor in the Department of Health Policy and Management at the University of North Carolina at Chapel Hill.
Jennifer Jones received her MPH at the University Of Pittsburgh Graduate School Of Public Health. She is currently the community engagement coordinator at the University Of Pittsburgh Graduate School Of Public Health.
Mimi Kim received her MPH at Columbia University in the City of New York and is currently a research fellow at the Center for Biobehavioral Research at Duke University.
Jennifer Schaal is affiliated with The Partnership Project, Inc.
Stefanie Vassar is affiliated with the University of California at Los Angeles Clinical and Translational Science institute.
Dr. Deepthi Varma received her doctoral degree in Psychiatric Social Work at National Institute of Mental Health and Neuro Sciences, Bangalore, India. Her research studies include HIV/AIDS prevention interventions among women, mental health correlates of intimate partner violence, and on the perceived need for HIV prevention interventions among drug abusing female offenders.
Dr. Catherine Striley received the Master of Social Work in 1989 and the Doctorate of Philosophy in Social Work from the Brown School at Washington University of St, Louis is 2002 where she was a National Institute of Mental Health (NIMH) predoctoral fellow. As a psychiatric epidemiologist, Catherine Woodstock Striley, PhD, MSW, ACSW, MPE, conducts community-engaged research that aims to increase the recognition of need for mental health and behavioral health services and decrease barriers to those services.
Corrine Ruktanonchai is affiliated with the University of Florida where she teaches in the department of epidemiology in the College of Medicine.
Adina Black is affiliated with the CARES team at the University of North Carolina at Chapel Hill.
Dr. Jennifer Hankins is affiliated with the University of North Carolina at Chapel Hill and her research interests include preventative care and community engaged research and is
Dr. Nakita Lovelady received her PhD from University of Arkansas for Medical Sciences and is currently a lay community program manager for the University of Arkansas for Medical Sciences Translational Research Institute.
Dr. Wiley Cené is a native North Carolinian. She moved to the “Southern part of heaven” for undergraduate training at the University of North Carolina at Chapel Hill, where she received her B.A. in Psychology in 1995. She graduated from the Brody School of Medicine at East Carolina University. Her research interests focus on understanding how social networks and network-based resources (e.g. social support) influence health behaviors and health outcomes for patients with or at risk for cardiovascular disease.
Melissa Green is the Deputy Director for Communication and Recruitment for the Clinical Scholars Program funded by the Robert Wood Johnson Foundation and is affiliated with CHER. Melissa’s experience includes 15 years managing research intervention studies in community settings using principles of community based participatory research with and for African American and Latino populations.
Dr. Tiffany L. Young completed her doctorate at the University of South Florida (USF), School of Aging Studies. During her tenure at USF, Dr. Young also earned a cognate in Evaluation from the Department of Educational Measurement & Research. While at USF, her research focused on developing and evaluating community programs for older adults.
Shristi Tiwari graduated from UNC Chapel Hill in 2016 with a B.A. in Psychology and History. Her research interests are women, health, and economics, and how those factors intersect/effect each other in relation to public health. She is currently working on the Heart Matters and Greenwall Projects at CHER.
Dr. Ann Cheney is assistant professor in the Center for Healthy Communities at the University of California, Riverside School of Medicine. She is a medical anthropologist with research experience in mental health and substance use health services, with a focus on trauma and co-occurring mental health and substance abuse disorders among women. She has conducted research among underserved populations, including women in rural communities, veterans, and ethnic and racial minorities.
Dr. Linda Cottler is the Associate Dean for Research and Planning at the College of Public Health and Health Professions and Dean’s Professor and Founding Chair of the Department of Epidemiology at the College of Public Health and Health Professions and the College of Medicine at the University of Florida, is involved in studies in several major areas with public health importance.
Dr. Greer Sullivan, M.D., joined the UCR School of Medicine in 2014, charged with developing the school’s health services research program and as founding director of the UCR Center for Healthy Communities. Sullivan is a professor of psychiatry in the Division of Clinical Sciences, an adjunct senior scientist for the Rand Corporation. She came to UCR from the Department of Psychiatry at the University of Arkansas for Medical Sciences. She has also served as a visiting professor at the Tulane School of Medicine and the University of Mississippi School of Medicine.
Dr. Arleen F. Brown is a general internist and health services researcher with expertise in quality of care for older adults and minorities with diabetes. She has focused on health care system, social, and individual level determinants of health for persons with diabetes. She had headed a project, funded by the Robert Wood Johnson Foundation, on quality of care for older persons with diabetes in fee-for-service and managed Medicare.
Dr. Jennifer Burke’s work aims to improve the health and wellbeing of women and children by addressing complex community health issues including intimate partner violence, HIV/AIDS and racial disparities in birth outcomes. She uses integrated qualitative and quantitative methods and a stakeholder engaged approach to my community health research.
Dr. Corbie-Smith is Professor of Social Medicine and Medicine at the School of Medicine, and nationally recognized for her scholarly work on the practical and ethical issues regarding involvement of minorities in research. She directs the Program on Health Disparities at the Cecil G. Sheps Center for Health Services Research at UNC-Chapel Hill and has been a member of several national and regional committees including Institute of Medicine committees examining the ethical issues of involving minority communities and underserved groups in housing-related research and on standards for systematic reviews in comparative effective research. University of Arkansas for Medical Sciences, and research health scientist in Health Services Research & Development at the Central Arkansas Veterans Healthcare System.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Berge JM, Mendenhall TJ, Doherty WJ. Using community-based participatory research (CBPR) to target health disparities in families. Family Relations. 2009;58(4):475–488. doi: 10.1111/j.1741-3729.2009.00567.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lasker RD, Weiss ES, Miller R. Partnership synergy: A practical framework for studying and strengthening the collaborative advantage. The Milbank Quarterly. 2001;79(2):179–205. doi: 10.1111/1468-0009.00203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lindquist-Grantz R, Vaughn LM. The journey and destination need to be intentional: Perceptions of success in community-academic research partnerships. Gateways: International Journal of Community Research and Engagement. 2016;9(1):1–21. [Google Scholar]
- 4.Andrews JO, et al. Partnership readiness for community-based participatory research. Health Educ Res. 2012;27(4):555–71. doi: 10.1093/her/cyq050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Israel BA EE, Schultz AJ, Parker EA, editors. Methods in community-based participatory research for health. 2nd. San Francisco: Jossey-Bass Publishers; 2013. [Google Scholar]
- 6.Ferreira MP, Fidji G. Community-based participatory research with traditional and indigenous communities of the Americas: Historical context and future directions. The International Journal of Critical Pedagogy. 2011;3(3):153–68. [Google Scholar]
- 7.Hodge FS. No meaningful apology for American Indian unethical research abuses. Ethics & Behavior. 2012;22(6):431–44. [Google Scholar]
- 8.Scharff DP, et al. More than Tuskegee: understanding mistrust about research participation. J Health Care Poor Underserved. 2010;21(3):879–97. doi: 10.1353/hpu.0.0323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shern DL, Trochim WMK, LaComb CA. The use of concept mapping for assessing fidelity of model transfer: An example from psychiatric rehabilitation. Evaluation and Program Planning. 1995;;18(2):143–153. doi: 10.1016/0149-7189(95_0005-v). [DOI] [Google Scholar]
- 10.Vaughn LM, Jones JR, Booth E, Burke JG. Concept mapping methodology and community-engaged research: A perfect pairing. Evaluation and Program Planning. 2017;60:229–237. doi: 10.1016/j.evalprogplan.2016.08.013. [DOI] [PubMed] [Google Scholar]
- 11.Cottler LB, McCloskey DJ, Aguilar-Gaxiola S, et al. Community needs, concerns, and perceptions about health research: Findings from the clinical and Translational science award sentinel network. American Journal of Public Health. 2013;103(9):1685–1692. doi: 10.2105/ajph.2012.300941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: Assessing partnership approaches to improve public health. Annual review of public Health. 1998;19(1):173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 13.Wallerstein N, Duran B. Community-based participatory research contributions to intervention research: The intersection of science and practice to improve health equity. American Journal of Public Health. 2010;100(S1):S40–S46. doi: 10.2105/AJPH.2009.184036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Barnett M, et al. The process of trust building between university researchers and urban school personnel. Urban Education. 2010;45(5):630–60. [Google Scholar]
- 15.Carlton EL, Whiting JB, Bradford K, Dyk PH, Vail A. Defining factors of successful university‐community collaborations: An exploration of one healthy marriage project. Family Relations. 2009;58(1):28–40. [Google Scholar]
- 16.Wright KN, Williams P, Wright S, Lieber E, Carrasco SR, Gedjeyan H. Ties that bind: Creating and sustaining community-academic partnerships. Gateways: International Journal of Community Research and Engagement. 2011;4:83–99. [Google Scholar]
- 17.Jagosh J, Bush PL, Salsberg J, et al. A realist evaluation of community-based participatory research: Partnership synergy, trust building and related ripple effects. BMC Public Health. 2015;15(1) doi: 10.1186/s12889-015-1949-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Butterfoss FD. Process evaluation for community participation. Annual review of public Health. 2006;27:323–340. doi: 10.1146/annurev.publhealth.27.021405.102207. [DOI] [PubMed] [Google Scholar]
- 19.Butterfoss FD, Goodman RM, Wandersman A. Community coalitions for prevention and health promotion: Factors predicting satisfaction, participation, and planning. Health education quarterly. 1996;23(1):65–79. doi: 10.1177/109019819602300105. [DOI] [PubMed] [Google Scholar]
- 20.Wallerstein N, Oetzel J, Duran B, Tafoya G, Belone L, Rae R. What predicts outcomes in cbpr Community-based participatory research for health: from processes to outcomes. 2nd. San Francisco: Jossey-Bass; 2008. p. 371388. [Google Scholar]
- 21.Nichols N, Anucha U, Houwer R, Wood M. Building equitable community-academic research collaborations: Learning together through tensions and contradictions. Gateways: International Journal of Community Research and Engagement. 2013;6(1):57–76. [Google Scholar]
- 22.Christopher S, Watts V, McCormick AKHG, Young S. Building and maintaining trust in a community-based participatory research partnership. American Journal of Public Health. 2008;98(8):1398–1406. doi: 10.2105/ajph.2007.125757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mayer RC, et al. An Integrative Model of Organizational Trust. The Academy of Management Review. 1995;20(3):709–34. [Google Scholar]
- 24.Balkrishnan R, et al. Trust and satisfaction with physicians, insurers, and the medical profession. Med Care. 2003;41(9):1058–64. doi: 10.1097/01.MLR.0000083743.15238.9F. [DOI] [PubMed] [Google Scholar]
- 25.Northouse PG. Interpersonal trust and empathy in nurse-nurse relationships. Nurs Res. 1979;28(6):365–68. [PubMed] [Google Scholar]
- 26.Moreno G, et al. Eight years of building community partnerships and trust: The UCLA family medicine community-based participatory research experience. Acad Med. 2009;84(10):1426–33. doi: 10.1097/ACM.0b013e3181b6c16a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Plowfield LA, et al. Time, tact, talent, and trust: Essential ingredients of effective academic-community partnerships. Nurs Educ Perspect. 2005;26(4):217–20. [PubMed] [Google Scholar]
- 28.Kane M, Trochim W. Concept Mapping for Planning and Evaluation (Applied Social Research Methods) Sage Publications, Inc; Beverly Hills, CA: 2007. [Google Scholar]
- 29.Shern DL, Trochim WMK, LaComb CA. The use of concept mapping for assessing fidelity of model transfer: An example from psychiatric rehabilitation. Evaluation and Program Planning. 1995;18(2):143–153. doi: 10.1016/0149-7189(95_0005-v). [DOI] [Google Scholar]
- 30.Frerichs L, et al. Stakeholder Perspectives on Creating and Maintaining Trust in Community-Academic Research Partnerships. Health Educ Behav. 2016;25 doi: 10.1177/1090198116648291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Burke JG, et al. An introduction to concept mapping as a participatory public health research method. Qual Health Res. 2005;15(10):1392–410. doi: 10.1177/1049732305278876. [DOI] [PubMed] [Google Scholar]
- 32.Kruskal JB, Wish M. Multidimensional Scaling. Sage Publications, Inc; Beverly Hills, CA: 1978. [Google Scholar]
- 33.Everitt B. Cluster Analysis. Halsted Press; New York: 1980. [Google Scholar]
- 34.Rosas SR, Camphausen LC. Planning, the use of concept mapping for scale development. Eval Program Plann. 2007;30(2):125–35. doi: 10.1016/j.evalprogplan.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 35.Eder MM, et al. A logic model for community engagement within the Clinical and Translational Science Awards consortium: can we measure what we model? Acad Med. 2013;88(10):1430–6. doi: 10.1097/ACM.0b013e31829b54ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Michener L, et al. Aligning the goals of community-engaged research: why and how academic health centers can successfully engage with communities to improve health. Adad Med. 2012;87(3):285–91. doi: 10.1097/ACM.0b013e3182441680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rosas SR, Kane M. Quality and rigor of the concept mapping methodology: A pooled study analysis. Eval Program Plann. 2012;35:236–45. doi: 10.1016/j.evalprogplan.2011.10.003. [DOI] [PubMed] [Google Scholar]
- 38.Sandoval JA, Lucero J, Oetzel J, Avila M, Belone L, Mau M, et al. Process and outcome constructs for evaluating community-based participatory research projects: A matrix of existing measures. Health Education Research. 2012;27(4):680–690. doi: 10.1093/her/cyr087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Minkler M, Wallerstein N. Community-based participatory research for health: From process to outcomes. John Wiley& Sons; 2011. [Google Scholar]
- 40.Ahmed SM, Palermo AG. Community Engagement in Research: Frameworks for Education and Peer Review. Am J Public Health. 2010;100(8):1380–7. doi: 10.2105/AJPH.2009.178137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Carpiano RM. Toward a neighborhood resource-based theory of social capital for health: Can Bourdieu and sociology help? Soc Sci Med. 2006;62(1):165–175. doi: 10.1016/j.socscimed.2005.05.020. [DOI] [PubMed] [Google Scholar]
- 42.Putnam RD, et al. Making democracy work: Civic traditions in modern Italy. Princeton University Press; Princeton, NJ: 1994. [Google Scholar]
- 43.Association of American Medical Colleges. Protecting Subjects, Preserving Trust, Promoting Progress - Policy and Guidelines for the Oversight of Individual Financial Interests in Human Subjects Research. 2001 Available https://www.aamc.org/download/75302/data/firstreport.pdf. Accessed on October, 2016. [PubMed]
- 44.Cohen JJ. Trust us to make a difference: Ensuring public confidence in the integrity of clinical research. Acad Med. 2001;76(2):209–214. doi: 10.1097/00001888-200102000-00028. [DOI] [PubMed] [Google Scholar]
- 45.Corbie-Smith G, et al. Attitudes and Beliefs of African Americans Toward Participation in Medical Research. 1999;14(9):537–46. doi: 10.1046/j.1525-1497.1999.07048.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gatter R. Walking the talk of trust in human subjects research: the challenge of regulating financial conflicts of interest. Emory Law J. 2003;52:327–401. [PubMed] [Google Scholar]
- 47.MyNAP. Trust and Confidence at the Interfaces of the Life Sciences and Society: Does the Public Trust Science? A Workshop Summary. Available at: http://www.nap.edu/read/21798/chapter/1 Accessed on October, 2016. [PubMed]
- 48.Luke DA, et al. The program sustainability assessment tool a new instrument for public health programs. Prev Chronic Ds. 2014;11 doi: 10.5888/pcd11.130184. [DOI] [PMC free article] [PubMed] [Google Scholar]


