Abstract
Background:
The failure rate for the closed/non-surgical treatment of thoracic and lumbar vertebral body fractures (TLVBF) in trauma patients has not been adequately evaluated utilizing computed tomography (CT) studies.
Methods:
From 2007 to 2008, consecutive trauma patients, who met inclusion criteria, with a CT diagnosis of acute TLVBF undergoing closed treatment were assessed. The failure rates for closed therapy, at 3 months post-trauma, were defined by progressive deformity, vertebral body collapse, or symptomatic/asymptomatic pseudarthrosis. The Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification was utilized to classify the fractures (groups A1 and non-A1 fractures) and were successively followed with CT studies.
Results:
There were 54 patients with 91 fractures included in the study; 66 were A1 fractures, and 25 were non-A1 fractures. All had rigid bracing applied with flat and upright X-ray films performed to rule out instability. None had sustained spinal cord injuries. Thirteen patients (24%) failed closed therapy [e.g. 13 failed fractures (14%) out of 91 total fractures]. Five failed radiographically only (asymptomatic), and eight failed radiographically and clinically (symptomatic). A1 fractures had a 4.5% failure rate, while non-A1 fractures failed at a rate of 40%.
Conclusion:
Failure of closed therapy for TLVBF in the trauma population is not insignificant. Non-A1 fractures had a much higher failure rate when compared to A1 fractures. We recommend close follow-up particularly of non-A1 fractures treated in closed fashion using successive CT studies.
Keywords: Computed tomography, fracture, failure, lumbar, vertebral body fracture, thoracic
INTRODUCTION
Spinal injuries in the trauma population are detected in 23.2% of cases.[16] Fractures involving the thoracic or lumbar spine are typically noted in 4.4% of trauma patients.[5] The majority of these injuries however do not involve neurological deficits, and therefore, the decision to treat them operatively or conservatively will depend on the degree of suspected instability. Initial experience with conservative therapy with or without the application of postural reduction seemed favorable.[3,14] Here, a variety of external orthoses or immobilization have been applied with overall good outcomes.[2,4,6,8,9,11,17,19,20] There are reports of closed treatment of traumatic thoracic and lumbar vertebral body fractures (TLVBF) without bracing documenting good outcomes.[2,8,10,13,15,17] Overall, there are few prospectively evaluated patient series documenting outcome of traumatic TLVBF treated in closed fashion.[1,2,4,9,11,12,17,18,19,23]
MATERIALS AND METHODS
Clinical data
Between 2007 and 2008, trauma patients with a computed tomography (CT) diagnosis of acute TLVBF undergoing closed treatment by senior author with minimum follow-up of 3 months, or failure of treatment, were consecutively evaluated. The bracing was adjusted to the level of fracture and included thoracolumbosacral orthosis (TLSO). For high thoracic injuries halo immobilization was applied.
Injury classification
The Arbeitsgemeinschaft für Osteosynthesefragen (AO) classification was applied to classify the body fractures into A1 and non-A1 fractures. The fractures were followed using CT imaging up to 3 months after initial treatment. The failure with closed therapy was defined as progressive deformity greater than 50% of the initial sagittal or coronal angulation [Figure 1], body collapse greater than 50% of the index height of the involved vertebra [Figure 2], or pseudoarthrosis (e.g., a fracture gap of greater than 1 mm and worsening gap) [Figure 3]. Clinical failure was defined as radiographic failure with symptoms (pain, neurological deficits, or both combined). The radiographic and clinical outcomes were evaluated 3 months later after follow-up CT imaging plus examinations.
Figure 1.
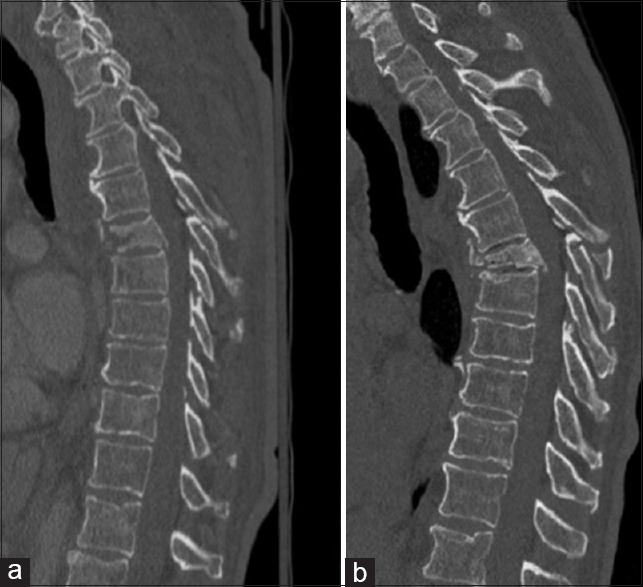
A 69 year old male was involved in a motor cycle accident and suffered from a 2 column thoracic 6 fracture AO type B (a). He was braced but at 6 weeks time imaging revealed significant progression of post traumatic kyphotic deformity (b). Surgery was offered, but he refused since he was asymptomatic. He was followed up elsewhere and kept in brace for a total of 9 months. At 2 years after injury he remained asymptomatic
Figure 2.
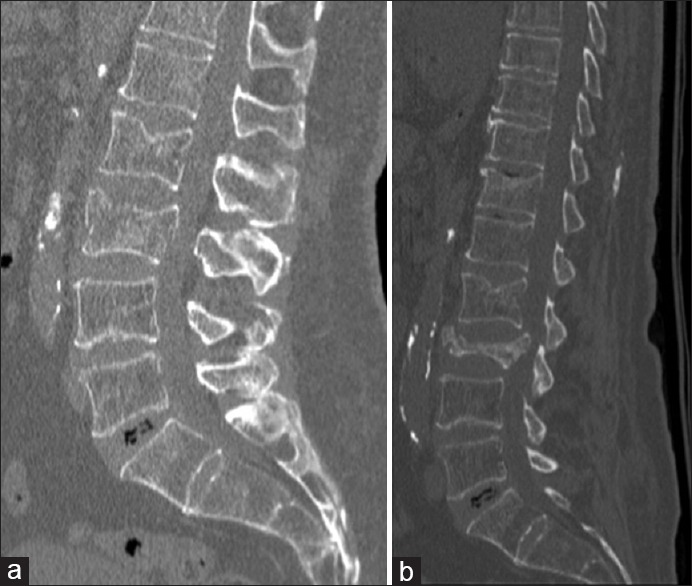
A 71 year old male involved in a motor vehicle accident suffered from an lumbar 3 burst fracture AO type A3 (a). He was placed in a TLSO. At 3 months follow up, patient was asymptomatic. Imaging revealed significant collapse of the fracture (b). He was removed out of brace and had no further clinical complaints at 6 months follow up
Figure 3.
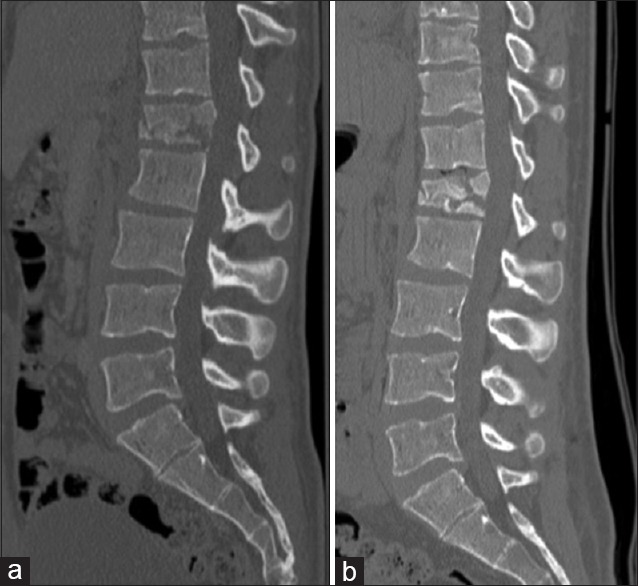
A 22 year old male was involved in a motor cycle accident and suffered from a lumbar 1 fracture AO type A2 (a). He was treated in a TLSO brace for 4.5 months but disclosed pseudo-arthrosis of the fractured vertebral body on imaging (b). Due to ongoing mechanical back pain he was fused operatively at an outside facility closer to his home and did well on follow up at 11 months
Statistical methods of analysis
The Chi-square test was applied for statistical analysis. A P value of 0.05 or lesser was considered statistically significant, and a P value of 0.001 or lesser was considered statistically highly significant. Institutional review board approval was obtained for this study.
RESULTS
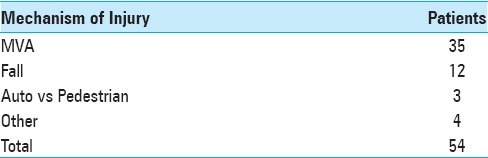
A total of 54 patients, harboring 91 vertebral body fractures, (31 male, 23 female; mean age 44 years), who survived the initial injury and had sufficient follow-up were enrolled consecutively. The mechanism of injury included motorized vehicle accidents (N = 35), falls (N = 12), auto versus pedestrian (N = 3) and other mechanisms (N = 4) [Table 1]. Of the total fractures, 66 were A1 fractures and 25 were non-A1 fractures. All had rigid bracing (turtle shell bracing or halo), and none had spinal cord injury. Thirteen patients (24%) failed closed therapy: in short, 13 failed body fractures (14%) out of 91 total broken vertebrae. Five (5.5%) failed radiographically only (asymptomatic), and eight (8.8%) failed radiographically and clinically (symptomatic). A1 fractures had a 4.5% (N = 3) failure rate; all were clinical failures. Non-A1 fractures failed at 40% (N = 10); half of these were radiographic, and the other half were clinical failures. There was a highly significant association between A1 fractures and healing after bracing, when comparing them to non-A1 fractures (P = 0.0001).
Table 1.
Distribution of patient population by mechanism of injury
Clinical failures; Symptomatic patients
All eight patients (61.5%) with symptomatic clinical failure complained of back pain without neurological deficit. One underwent pedicle screw fixation for pseudoarthrosis of the fracture with pain relief following surgery. The remainder were treated conservatively. One was referred for percutaneous cement injection for progressive body collapse, but was not felt to be a good candidate for the procedure on consultation.
Without failure of closed management
In the cohort of patients without failure of closed management (N = 41) five patients (12%) were complaining of persistent back pain without neurological deficits; all of them were managed conservatively. There was a highly significant association between healed fractures and absence of back pain, when comparing them to non-healed fractures and pain freedom (P = 0.0001).
DISCUSSION
Traumatic vertebral body fractures of the thoracic and lumbar spine can successfully be managed nonoperatively.[1,2,4,8,10,11,13,17,19,20,22] Overall, the risk of neurological injury in these patients is low in association with nonoperative therapies. Earlier concern of significant risk to sustain new or worsened neurological damage with nonoperative therapy could not be substantiated by other published reports that examined a broader range of TLVBF.[1,2,4,6,7,10,11,17,19,20,21,22] Due to the excellent results associated with nonoperative therapies, surgery has been generally reserved in cases of fractures associated with neurological deficits. The fact that only 14% of all patients were managed operatively underscores a general conservative approach in our experience. In other words, treating these patients with a more severe fracture pattern upfront with surgery is expected to result in lower failure rate in the conservatively treated cohort. Yet, even with more severe fractures being included for nonoperative therapy, no significant neurological compromise was encountered. Open surgery was successfully avoided in almost all cases of failures but one. Therefore, one can conclude that closed therapy in this population was safe in all followed subjects and effective in most of them.
The presence of failure of closed therapy for TLVBF may be associated with development of back pain. In the failure group of 13 patients 61.5% complained of back pain, in contrast to only 12% in the nonfailure group. In the present literature there are conflicting data to prove that non-healing or deformity of TLVBF are more frequently associated with pain.[4,6,8,13,20,22]
For future studies, it will be important to evaluate the method of nonoperative therapies. Only then can we implement guidelines for more accurate stratifications of therapies for patients with TLVBF.
CONCLUSIONS
We were able to safely and successfully treat the majority of patients with traumatic TLVBF in closed fashion with bracing; none suffered significant or permanent neurological damage, and only a single patient underwent operative therapy.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank Ocean C Feiz-Erfan for her help in the preparation of this manuscript.
Footnotes
Contributor Information
Jarvis W. Walters, Email: Jarvis.Walters3@mihs.org.
Tammy R. Kopelman, Email: Tammy_Kopelman@dmgaz.org.
Arpan A. Patel, Email: arpan425@email.arizona.edu.
Patrick J. O’Neill, Email: Patrick_Oneill@dmgaz.org.
Poya Hedayati, Email: Poya_Hedayati@dmgaz.org.
Paola G. Pieri, Email: Paola_Pieri@dmgaz.org.
Sydney J. Vail, Email: Sydney_Vail@dmgaz.org.
Salvatore C. Lettieri, Email: Salvatore_Lettieri@dmgaz.org.
Iman Feiz-Erfan, Email: Iman_feiz-erfan@dmgaz.org.
REFERENCES
- 1.Alanay A, Yazici M, Acaroglu E, Turhan E, Cila A, Surat A. Course of nonsurgical management of burst fractures with intact posterior ligamentous complex: An MRI study. Spine (Phila Pa 1976) 2004;29:2425–31. doi: 10.1097/01.brs.0000143169.80182.ac. [DOI] [PubMed] [Google Scholar]
- 2.Bailey CS, Dvorak MF, Thomas KC, Boyd MC, Paquett S, Kwon BK, et al. Comparison of thoracolumbosacral orthosis and no orthosis for the treatment of thoracolumbar burst fractures: Interim analysis of a multicenter randomized clinical equivalence trial. J Neurosurgery Spine. 2009;11:295–303. doi: 10.3171/2009.3.SPINE08312. [DOI] [PubMed] [Google Scholar]
- 3.Bohler L. Conservative treatment of fractures of the thoracic and lumbar spine. Z Unfallmed Berufskr. 1972;65:100–4. [PubMed] [Google Scholar]
- 4.Cantor JB, Lebwohl NH, Garvey T, Eismont FJ. Nonoperative management of stable thoracolumbar burst fractures with early ambulation and bracing. Spine. 1993;18:971–6. doi: 10.1097/00007632-199306150-00004. [DOI] [PubMed] [Google Scholar]
- 5.Cooper C, Dunham CM, Rodriguez A. Falls and major injuries are risk factors for thoracolumbar fractures: Cognitive impairment and multiple injuries impede the detection of back pain and tenderness. J Trauma Acute Care Surg. 1995;38:692–6. doi: 10.1097/00005373-199505000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Dai LY, Jiang LS, Jiang SD. Conservative treatment of thoracolumbar burst fractures: A long-term follow-up results with special reference to the load sharing classification. Spine (Phila Pa 1976) 2008;33:2536–44. doi: 10.1097/BRS.0b013e3181851bc2. [DOI] [PubMed] [Google Scholar]
- 7.Denis F, Armstrong G, Searls K, Matta L. Acute thoracolumbar burst fractures in the absence of neurologic deficit A comparison between operative and nonoperative treatment. Clin Orthop. 1984;189:142–9. [PubMed] [Google Scholar]
- 8.Folman Y, Gepstein R. Late outcome of nonoperative management of thoracolumbar vertebral wedge fractures. J Orthop Trauma. 2003;17:190–2. doi: 10.1097/00005131-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Hitchon PW, Torner JC, Haddad SF, Follett KA. Management options in thoracolumbar burst fractures. Surg Neurol. 1998;49:619–27. doi: 10.1016/s0090-3019(97)00527-2. [DOI] [PubMed] [Google Scholar]
- 10.Joaquim AF, Daubs MD, Lawrence BD, Brodke DS, Cendes F, Tedeschi H, et al. Retrospective evaluation of the validity of the thoracolumbar injury classification system in 458 consecutively treated patients. Spine J. 2013;13:1760–5. doi: 10.1016/j.spinee.2013.03.014. [DOI] [PubMed] [Google Scholar]
- 11.Krompinger WJ, Fredrickson BE, Mino DE, Yuan HA. Conservative treatment of fractures of the thoracic and lumbar spine. Orthop Clin North Am. 1986;17:161–70. [PubMed] [Google Scholar]
- 12.Mohanty S, Venkatram N. Does neurological recovery in thoracolumbar and lumbar burst fractures depend on the extent of canal compromise? Spinal Cord. 2002;40:295. doi: 10.1038/sj.sc.3101283. [DOI] [PubMed] [Google Scholar]
- 13.Moller A, Hasserius R, Redlund-Johnell I, Ohlin A, Karlsson MK. Nonoperatively treated burst fractures of the thoracic and lumbar spine in adults: A 23-to 41-year follow-up. Spine J. 2007;7:701–7. doi: 10.1016/j.spinee.2006.09.009. [DOI] [PubMed] [Google Scholar]
- 14.Nicoll EA. Fractures of the dorso-lumbar spine. J Bone Joint Surg Br. 1949;31B:376–94. [PubMed] [Google Scholar]
- 15.Ohana N, Sheinis D, Rath E, Sasson A, Atar D. Is there a need for lumbar orthosis in mild compression fractures of the thoracolumbar spine.: A retrospective study comparing the radiographic results between early ambulation with and without lumbar orthosis? Clin Spine Surg. 2000;13:305–8. doi: 10.1097/00002517-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Pirouzmand F. Epidemiological trends of spine and spinal cord injuries in the largest Canadian adult trauma center from 1986 to 2006. J Neurosurgery Spine. 2010;12:131–40. doi: 10.3171/2009.9.SPINE0943. [DOI] [PubMed] [Google Scholar]
- 17.Shen W, Shen Y. Nonsurgical treatment of Three-Column thoracolumbar junction burst fractures without neurologic deficit. Spine. 1999;24:412–5. doi: 10.1097/00007632-199902150-00024. [DOI] [PubMed] [Google Scholar]
- 18.Siebenga J, Leferink VJ, Segers MJ, Elzinga MJ, Bakker FC, Haarman HJ, et al. Treatment of traumatic thoracolumbar spine fractures: A multicenter prospective randomized study of operative versus nonsurgical treatment. Spine (Phila Pa 1976) 2006;31:2881–90. doi: 10.1097/01.brs.0000247804.91869.1e. [DOI] [PubMed] [Google Scholar]
- 19.Stadhouder A, Buskens E, Vergroesen DA, Fidler MW, de Nies F, Oner FC. Nonoperative treatment of thoracic and lumbar spine fractures: A prospective randomized study of different treatment options. J Orthop Trauma. 2009;23:588–94. doi: 10.1097/BOT.0b013e3181a18728. [DOI] [PubMed] [Google Scholar]
- 20.Tropiano P, Huang RC, Louis CA, Poitout DG, Louis RP. Functional and radiographic outcome of thoracolumbar and lumbar burst fractures managed by closed orthopaedic reduction and casting. Spine (Phila Pa 1976) 2003;28:2459–65. doi: 10.1097/01.BRS.0000090834.36061.DD. [DOI] [PubMed] [Google Scholar]
- 21.Weninger P, Schultz A, Hertz H. Conservative management of thoracolumbar and lumbar spine compression and burst fractures: Functional and radiographic outcomes in 136 cases treated by closed reduction and casting. Arch Orthop Trauma Surg. 2009;129:207–19. doi: 10.1007/s00402-008-0780-x. [DOI] [PubMed] [Google Scholar]
- 22.Weinstein JN, Collalto P, Lehmann TR. Thoracolumbar “burst” fractures treated conservatively: A long-term follow-up. Spine. 1988;13:33–8. doi: 10.1097/00007632-198801000-00008. [DOI] [PubMed] [Google Scholar]
- 23.Wood K, Buttermann G, Mehbod A, Garvey T, Jhanjee R, Sechriest V. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: A prospective, randomized study. JBJS. 2003;85:773–81. doi: 10.2106/00004623-200305000-00001. [DOI] [PubMed] [Google Scholar]


