Survivorship care at MSTI meets new standards, allows for patient engagement and satisfaction, and improves care coordination; costs are covered by reimbursement.
Abstract
Purpose:
The 2015 Commission on Cancer standards require that cancer survivors receive an individualized survivorship care plan (SCP). To meet this new standard, St Luke's Mountain States Tumor Institute (MSTI), with support from the National Community Cancer Centers Program, implemented a successful survivorship model.
Patients and Methods:
At MSTI, the patient's SCP is prepared in the electronic health record by a registered health information technician. This document is reviewed during an appointment with a nurse practitioner and social worker. The provider's dictation is mailed to the primary care physician with the SCP. From August 2011 to Oct 2012, 118 patients with breast cancer were seen for survivorship appointments. Medical record audit and follow-up telephone call were completed to evaluate patient survivorship needs and satisfaction with the appointment. Patient accounts were reviewed for reimbursement.
Results:
From medical record review, the most common patient concerns were weight management (35%), fatigue (30%), sexuality (27%), anxiety (23%), caregiver stress (17%), and depression (16%). Telephone calls showed high patient satisfaction and understanding. Patients rated the following statements on a Likert scale from 1 (strongly disagree) to 5 (strongly agree): I understand my treatment summary and care plan (88% strongly agree or agree), and I feel the survivorship visit met my survivorship needs (86% strongly agree or agree). At 1 month, 80% of participants were still working on wellness goals. Patient accounts analysis showed revenue covered costs.
Conclusion:
Survivorship care at MSTI meets new standards, allows for patient engagement and satisfaction, and improves care coordination. Costs are covered by reimbursement.
Introduction
The number of cancer survivors in the United States is expected to grow to more than 18 million by the year 2022.1 In 2011, the American College of Surgeons Commission on Cancer (CoC) released a new standard that will require accredited cancer centers to provide all patients who complete cancer treatment with an individualized survivorship care plan (SCP).2 This new standard will go into effect in 2015. The minimum requirements for the care plan are outlined in the Institute of Medicine (IOM) Cancer Survivorship Care Planning Fact Sheet.3 The standards outlined in the IOM fact sheet give particular attention to the provision of information and support as they relate to treatment provided as well as physical and psychosocial late effects. It has been suggested that to meet this standard, oncology practices will be required to dramatically shift their focus and make a major investment in resources.4
Over the last several years, a variety of models for survivorship care delivery have developed across the county. These models include nurse-led programs, which keep costs relatively low; nurse practitioner–run clinics, which provide personalized care but can be expensive to run; and multidisciplinary specialty survivorship clinics, which is the most resource-intense model. These clinics historically have been the most difficult to sustain because of financial cost.4–9
To meet this new standard, St Luke's Mountain States Tumor Institute (MSTI), with support from the National Cancer Institute National Community Cancer Centers Program, implemented a pilot process to deliver SCPs to patients with breast cancer that is multidisciplinary, efficient, and financially sustainable. After reviewing various models of survivorship care around the country, physicians and administration at MSTI opted for an integrated and innovative approach that provides the opportunity for each oncology professional to practice at the top of his or her license, while ensuring the services provided are appropriately reimbursed to cover the cost.
Patients and Methods
The cornerstone of the MSTI survivorship program is the survivorship treatment summary and care plan (Data Supplement). MSTI has developed disease-specific survivorship treatment summaries based on models from the American Society of Clinical Oncology and IOM.10–13 These summaries are electronic templates that exist within the electronic medical record (EMR) and are prepared by a registered health information technician (RHIT). Professionals holding the RHIT credential are educated to ensure the quality of medical records by verifying their completeness and accuracy. They are trained to assemble and analyze patient data for the purpose of improving patient care or controlling costs.14 Use of the EMR allows the RHIT to complete these documents in < 1 hour per patient.
Before the use of the RHIT staff person, the registered nurses who work with each oncologist were responsible for completing the treatment summaries. After significant review and staff feedback, it became apparent this was not the most effective use of the nurses' time. The summaries were often incomplete or filled out with errors. The nursing staff attributed these errors to lack of time in their clinic schedule and frustrations with the EMR. Today, the RHIT completes the summaries with increased efficiency and accuracy. To ensure the SCP is accurate, the RHIT consults with an oncology clinical nurse specialist when questions arise, and all final documents are reviewed by a nurse practitioner before they are delivered to the patient.
When patients at MSTI complete chemotherapy and/or radiation therapy, they are referred for a survivorship follow-up visit. This interdisciplinary visit is approximately 1 hour in length and consists of a joint visit with an oncology nurse practitioner and oncology social worker from the MSTI clinic. During the visit, the nurse practitioner conducts a physical examination and reviews the treatment summary with the patient. He or she addresses the physical late and long-term effects of treatment, reviews the recommendations for surveillance and follow-up care, and discusses health promotion to reduce risk of recurrence and other comorbid conditions. He or she also discusses the importance of care coordination and explains how this document will be shared with the patient's primary care (PCP) and referring physicians. The social worker participates in this visit by reviewing the psychosocial components of the late and long-term effects of treatment. During the visit, the social worker completes a psychosocial assessment and provides intervention as clinically indicated. The social worker assists the nurse practitioner with the discussion of health promotion and healthy survivorship. Information and resources are given to the patient about MSTI survivorship activities and survivorship support available in the community. This discussion concludes when the social worker assists the patient in setting two SMART (specific, measurable, actionable, realistic, time oriented) goals for survivorship wellness. The social worker documents these goals in the patient's copy of the survivorship care plan and in the EMR. After the comprehensive survivorship visit, the RHIT sends a copy of the patient's treatment summary and care plan with the provider's dictation to the patient's PCP and referring physician.
The survivorship pilot for patients with breast cancer began in August 2011. MSTI implemented program evaluation and patient satisfaction processes from the beginning to assess the program pilot success and weaknesses. The St Luke's Health System and MSTI research department do not require institutional review board approval for program evaluation projects.
To evaluate how well the multidisciplinary visit met the comprehensive patient-centered standard, the survivorship coordinator conducted a medical record audit for every survivorship follow-up appointment and classified patients' concerns into the following categories: weight/physical activity, fatigue, sexuality/body image, anxiety/fear of recurrence, caregiver/family stress, depression, nutrition, hot flashes, sleep disturbance, neuropathy, smoking, lymphedema, and pain. The coordinator only reviewed the documentation from the survivorship follow-up appointment.
To evaluate patient satisfaction, the survivorship program coordinator conducted follow-up telephone calls with participants approximately 1 month after the visits to assess patients' understanding of the information provided and overall satisfaction with the visits. An attempt was made to contact every survivorship follow-up patient; a message asking for a return call was left with patients who did not answer. Only one attempt was made to reach the patients. The survivorship coordinator used a script to identify herself and the purpose of the telephone call. She asked patients to rate their impression of the SCP and visit on a Likert scale from 1 (strongly disagree) to 5 (strongly agree). In addition to the patient satisfaction survey, the coordinator asked survivors to share comments about what was most helpful or suggest ways the clinic visits could be improved.
Cost and reimbursement for the survivorship visits were also evaluated. The oncology nurse practitioners, social workers, and RHIT were asked to estimate their time spent on one patient. Salary cost was calculated based on the average salary plus indirect costs for 90 minutes of social work time, 75 minutes of nurse practitioner time, and 60 minutes of RHIT time. This cost was calculated based on the median salary for each of the positions multiplied by the average time spent preparing for the visit, with the patient, on care coordination, and on documentation after each visit. An additional 20% was included to account for indirect costs associated with employment of these staff. The time of others involved including the nurses and oncologists who placed the order for the appointment and the schedulers who scheduled the visits could not be estimated, because this role has been incorporated into their regular day. These data were then compared with the amount billed and reimbursed for each survivorship visit. Average return on investment was calculated using the standard formula: (reimbursement − cost)/cost.
Results
From August 2011 to October 2012, 118 patients with breast cancer were seen in 1-hour joint nurse practitioner/social work survivorship visits. All patients who participated in the visits were female breast cancer survivors who received adjuvant chemotherapy and/or radiation therapy. The patients were seen in one of the five outpatient MSTI clinics in southern Idaho. All but two participants self-identified as white non-Hispanic; two participants self-identified as Hispanic. The average age of the participants was 60 years (range, 30 to 89 years).
Survivors' Documented Concerns
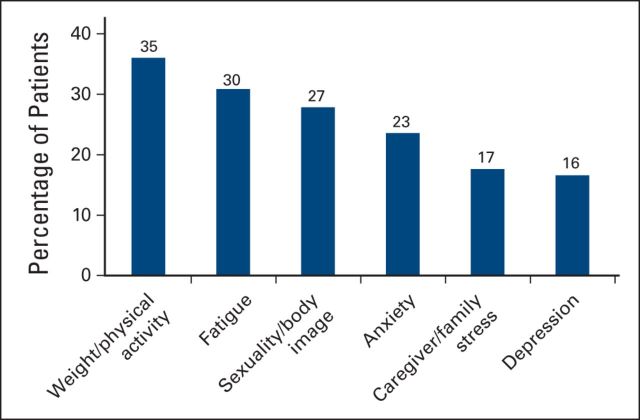
Medical record review illustrated many common concerns. Weight management and/or physical activity were concerns for 35% of the participants. Fatigue was the second most commonly occurring concern, affecting 30% of patients. Twenty-seven percent of patients described sexual functioning and/or body image as an issue for them. Anxiety and/or fear of recurrence were documented concerns for 23% of survivors who participated in the visits. Caregiver stress (17%) and depression (16%) also ranked in the top six documented concerns for the survivors (Fig 1). The remaining concerns were as follows: nutrition (15%), sleep and hot flashes (11%), neuropathy (8%), smoking cessation (7%), lymphedema (4%), and pain (3%). Cognitive changes, comorbid conditions, finances, work, bone loss, home safety, and nausea were all documented in < 3% of medical records.
Figure 1.
Documented survivor concerns.
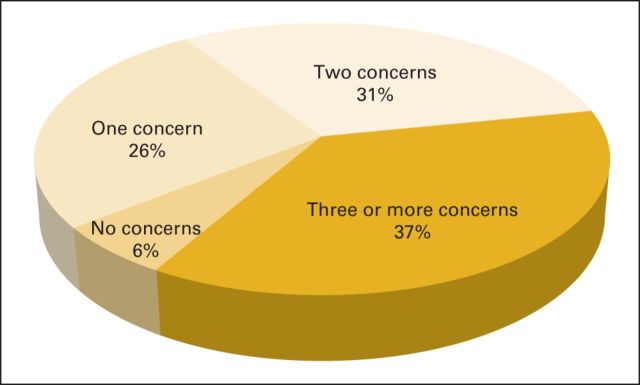
A review of these data indicates that the majority of patients experienced more than one survivorship concern. Only seven patients (5.9%) of the 118 whose medical records were reviewed indicated they had no concerns. Approximately one fourth of patients (26%) had only one concern identified during their survivorship visit; 31% of patients expressed two survivorship concerns. The remaining 36% of patients verbalized difficulty with three or more concerns during the survivorship visit (Fig 2).
Figure 2.
Number of survivorship concerns.
Participant Satisfaction
Fifty of the 118 patients were reached by telephone. Follow-up calls showed high patient satisfaction and understanding of the SCPs. Eighty-eight percent said they agreed or strongly agreed that they understood their treatment summary and care plan, 86% said they strongly agreed or agreed that they felt the survivorship visit met their survivorship needs, and 80% of participants who set survivorship wellness goals were still working on them at the time of the follow-up call.
The survivorship navigator identified consistency within the additional comments provided by patients during the follow-up telephone calls. These comments included appreciation for time spent, the opportunity to address concerns not previously addressed, and expression of new and/or improved understanding of future plans of care based on information provided in the SCP. Patient comments included:
“You always know you aren't the only one who goes through this—you see patients all the time and know people have gone through it. To be able to sit and talk with people who understand the fears and anxieties you want to shield your family from—and to be able to give voice to those feelings—is very empowering—helps you feel you are not alone. They were very helpful—listened, came up with some good ideas.” —67-year-old survivor
“I appreciated the time people took—and that it was available. You can start to feel like you have fallen off a cliff.” —62-year-old survivor
“I was extremely impressed that it was a two-on-one thing—that I had two people there to talk to. That was very positive. I did have some questions and didn't want to bother a doctor with them. The asking of questions was great—they asked me questions about things I would not have thought of. Helped me realize how important some of these things are. You know, you read a lot but having someone tell you that it is important was great.” —67-year-old survivor
“I so appreciated the survivorship treatment summary and care plan. Having all my information all in one place is so helpful!” 54-year-old survivor
When patients were asked if there was anything that would improve the visit, most patients did not have suggestions for improvement, although many patients did say that they thought they were coming to a group class and were pleasantly surprised to see that this was an individual follow-up appointment. Of all the patients interviewed, only three did not understand the purpose of the visit or were unhappy about participation in the visit. Two of the three cited financial stress as the primary reason for dissatisfaction with the appointment. These patients expressed concern about incurring a bill for the appointment and indicated they could not afford additional medical expenses.
Cost and Reimbursement
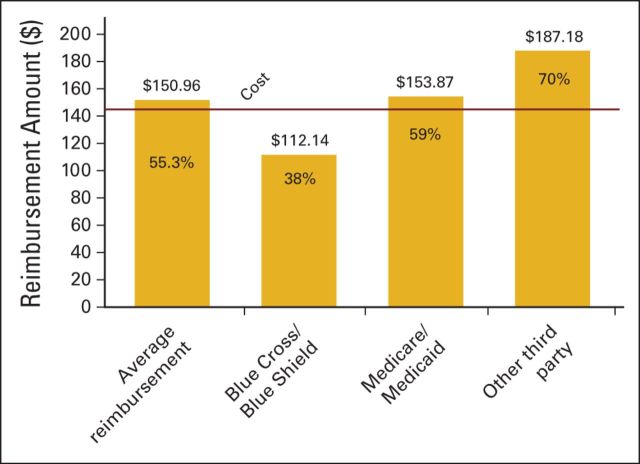
The estimated staff expense per patient visit totaled $141.73. Of the 118 patients seen in a survivorship follow-up appointment, 91 patient accounts were reviewed. Review of these accounts showed considerable charge and reimbursement variation based on the complexity of the visit and the insurer, respectively. The average associated charge for the visit was $272.67. The highest charge was $497, and the lowest charge was $138. This charge usually included a level-three or -four facility fee and level-three or -four professional fee (Current Procedural Terminology codes 99213 and 99214, respectively), with an additional charge for an extended visit with face-to-face education time. Variation in charges can be attributed to varying patient needs addressed with one-on-one education. Some visits were reported to last > 90 minutes, with others completed in just 30 minutes; the majority of survivorship visits were 1 hour in length.
The average associated reimbursement for each visit was $150.69, or 55.3% of the billed amount. The average reimbursement from Blue Cross and Blue Shield was $112.14, or 38% of the billed amount. The average reimbursement from Medicaid/Medicare and Medicare Advantage plans was $153.87, or 59% of the billed amount. The combined average reimbursement for all other third-party payers was $187.18, or 70% of the billed amount (Fig 3). When looking at the average cost per visit of $141.73 compared with the average amount of $150.96 reimbursed, the return on investment is approximately 6%.
Figure 3.
Reimbursement by payers.
Discussion
This programmatic review of survivorship care at MSTI illustrates comprehensive screening for physical and psychosocial late effects, high patient satisfaction, and strong evidence that reimbursement will cover costs as the program grows. Additionally, this survivorship model may allow for increased coordination of care with the patients' PCPs and patient engagement and adherence to general healthy behaviors and preventative strategies. These metrics have been identified as important considerations when assessing models for survivorship care.15 One challenge for cancer centers across the country has been to identify how to deliver comprehensive survivorship care that meets standards, including the IOM minimum requirements. The social worker/nurse practitioner combination visit allows for a comprehensive discussion to take place and for all of the minimum requirements to be addressed. This is evident by the wide range of survivorship concerns documented. These concerns mirror those of survivors across the country.16 Unfortunately, in many centers, providing comprehensive survivorship care has been expensive. CoC-accredited community cancer centers across the country have been looking for sustainable models of comprehensive survivorship care. Although many models of care have been evaluated for patient satisfaction, few models have reviewed costs compared with reimbursement.
Currently, reimbursement does not exist for the development of the care plan, but if the care plan is delivered in an appointment with strong clinical components and good patient education, then clinics can maximize the reimbursement of the visit through appropriate professional and facility fees. Ensuring providers and staff are coding the survivorship visits correctly will assist with maximizing revenue.
Although this model of integrated and comprehensive survivorship care seems to be successful, it is important to recognize that the patients were all female breast cancer survivors who were predominately white, English speaking, and insured and who were seen in the context of a hospital-based cancer center. Similar review is warranted for other cancer diagnoses and demographic groups in other health care systems before the findings can be generalized to all patients.
Additionally, at this point, no long-term data exist for these patients. It would be helpful to know if patients continue to make progress on their wellness goals 6 and 12 months down the road. This model also cannot suggest that a one-time survivorship follow-up appointment can meet the ongoing needs of a cancer survivor. Significant opportunities remain to study long-term outcomes for patients who receive comprehensive survivorship care. Will they follow through with recommendations for surveillance and healthy lifestyle? Will they generate increased downstream revenues for the health system if they maintain regular follow-up for cancer screening and health maintenance? Does comprehensive survivorship care result in better health outcomes long term?
Reimbursement may also change in the coming years. If insurers begin paying for value rather than paying for services, long-term survivorship research will become increasingly important. It is also possible that insurers may begin to reimburse for the development of the SCP in addition to the delivery. The Comprehensive Cancer Care Improvement Act, which was reintroduced to Congress in December 2011, aims to address this issue. The act will create a reimbursement structure that will support the development of cancer care planning.17 This will generate additional revenue if the development of the care plan can be accomplished by an RHIT instead of nursing staff.
In conclusion, after reviewing the results from the evaluation of the breast cancer pilot, MSTI has expanded this model of survivorship care to patients with colorectal and anal cancers, diffuse large B-cell lymphoma, and non–small-cell lung cancer. Plans are in place to make these survivorship follow-up appointments available to all patients who complete treatment in 2014.
Evaluation of this model of survivorship care has shown that an integrated and interdisciplinary approach will meet the new CoC standards, result in patient satisfaction and engagement in healthy behaviors, and provide important revenue for cancer centers. It is critical that cancer centers use staff resources and EMRs efficiently as they develop and implement SCPs for all patients. Meeting the new survivorship standards could require cancer centers to make significant investments in resources, but if careful consideration is given to using each professional at the top of his or her licensure, then the program can function with a neutral budget. Opportunities remain to measure long-term health outcomes and downstream revenues associated with this survivorship model.
Acknowledgment
Supported in whole or in part with federal funds from the National Cancer Institute, under Contract No. HHSN261200800001E. The content of this publication does not necessarily reflect the views of policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government. Presented in part at the American Society of Clinical Oncology Quality Symposium, San Diego, CA, November 30-December 1, 2012, and 10th Annual Conference of the American Psychosocial Oncology Society, Huntington Beach, CA, February 14-16, 2013.
Authors' Disclosures of Potential Conflicts of Interest
The author(s) indicated no potential conflicts of interest.
Author Contributions
Conception and design: Alicia R. Rosales, Dia Byrne, Lori Watts, Kathleen N. Clifford, Dan S. Zuckerman, Thomas Beck
Administrative support: Thomas Beck
Collection and assembly of data: Alicia R. Rosales, Christa Burnham, Lori Watts
Data analysis and interpretation: Alicia R. Rosales, Christa Burnham, Thomas Beck
Manuscript writing: All authors
Final approval of manuscript: All authors
References
- 1.American Cancer Society. Cancer Treatment and Survivorship: Facts and Figures 2012-2013. http://www.cancer.org/acs/groups/content/@epidemiologysurveilance/documents/document/acspc-033876.pdf.
- 2.American College of Surgeons Commission on Cancer. Cancer Program Standards 2012, Version 1.1: Ensuring Patient-Centered Care. http://www.facs.org/cancer/coc/programstandards2012.html.
- 3.Institute of Medicine. Cancer Survivorship Care Planning: Institute of Medicine Fact Sheet 2005. http://www.iom.edu/∼/media/Files/Report%20Files/2005/From-Cancer-Patient-to-Cancer-Survivor-Lost-in-Transition/factsheetcareplanning.pdf.
- 4.Advisory Board Company. Oncology Round Table: Delivering Sustainable Survivorship Care: Lessons for Program Design and Implementation. http://www.advisory.com/Research/Oncology-Roundtable/Studies/2011/Delivering-Sustainable-Survivorship-Care.
- 5.Chatigny A, Macdonald JS: Delivering effective and meaningful survivorship care Oncol Issues 39–43,2010May-Jun [Google Scholar]
- 6.Peairs KS Wolff AC Olsen SJ, etal: Coordination of care in breast cancer survivors: An overview J Support Oncol 9:210–215,2011 [DOI] [PubMed] [Google Scholar]
- 7.Patton A: M.D. Anderson breast cancer survivor clinic Oncol Issues 44–47,2010May-Jun [Google Scholar]
- 8.Schlairet M, Heddon MA, Griffis M: Piloting a needs assessment to guide development of a survivorship program for a community cancer center Oncol Nurs Forum 37:501–507,2010 [DOI] [PubMed] [Google Scholar]
- 9.Khatcheressian JL Hurley P Bantug E, etal: Breast cancer follow-up and management after primary treatment: American Society of Clinical Oncology clinical practice guideline update J Clin Oncol 31:961–965,2013 [DOI] [PubMed] [Google Scholar]
- 10.Hewitt M, Ganz PA: Implementing Cancer Survivorship Care Planning: Workshop Summary 2007Washington, DC: National Academies Press [Google Scholar]
- 11.Breast Cancer Adjuvant Treatment Plan and Summary, Version 3 10/09. http://www.cancer.net/survivorship/asco-cancer-treatment-summaries.
- 12.Breast Cancer Survivorship Care Plan, Version 3 10/09. http://www.cancer.net/survivorship/asco-cancer-treatment-summaries.
- 13.Hewitt M, Greenfield S, Stovall E: From Cancer Patient to Cancer Survivor: Lost in Transition 2006Washington, DC: Institute of Medicine and National Research Council [Google Scholar]
- 14.American Health Information Management Association. http://www.ahima.org/certification/rhit.aspx.
- 15.McCabe M Bhatia S Oeffinger K, etal: American Society of Clinical Oncology statement: Achieving high-quality cancer survivorship care J Clin Oncol 31:631–640,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ness S Kokal J Fee-Schroeder K, etal: Concerns across the survivorship trajectory: Results form a survey of cancer survivors Oncol Nurs Forum 40:35–42,2013 [DOI] [PubMed] [Google Scholar]
- 17.Comprehensive Cancer Care Improvement Act. HR 3705, 112th Cong, 2011 [Google Scholar]