This study demonstrates improvements in perceived knowledge and quality of survivorship care after receipt of a comprehensive survivorship care plan.
Abstract
Purpose:
Survivorship care plans (SCPs) have been suggested to reduce fragmentation of care experienced by cancer survivors. Acceptance of SCPs is high, but trials in the United States are few. This pilot study used a quasiexperimental design to examine the outcomes achieved by breast cancer survivors receiving a standardized SCP visit at one of seven comprehensive cancer centers.
Materials and Methods:
Outcomes were assessed before and again 3 months after delivery of an SCP and included survivors' use of and satisfaction with SCPs, perceived knowledge about survivorship, and assessment of the quality and coordination of survivorship care.
Results:
One hundred thirty-nine survivors of breast cancer completed baseline and follow-up measures and received a standardized SCP visit. Participants most commonly used SCP materials to make decisions about exercise (64%), which tests to receive and when (62%), and dietary changes (62%). Only 21% shared the SCP with their primary care provider during that time. Satisfaction with the SCP was high, with 90% of participants reporting being at least satisfied with the SCP. Perceived knowledge about survivorship improved after SCP delivery, as did perceived care coordination and the provider's knowledge of the effects of cancer on survivors (all P < .001). Individuals closer to the time of diagnosis reported greater satisfaction with and use of SCPs.
Conclusion:
This study demonstrates improvements in perceived knowledge and quality of survivorship care after receipt of a comprehensive SCP. Survivors were satisfied with their SCP, and those closer to diagnosis reported greater satisfaction with and use of the materials.
Introduction
Survivorship care plans (SCPs) have been suggested as a possible means to reduce fragmentation of care and suboptimal outcomes experienced by the more than 14 million US cancer survivors.1 Provider and patient acceptance of SCPs is high, but trials have primarily examined outcomes such as cancer-related distress rather than constructs related to the purpose of SCPs, such as improving care coordination and patient knowledge. Moreover, the largest trial2 took place in Canada, where care is generally less fragmented, limiting generalizability.3
An Institute of Medicine (IOM) report4 identified four components of survivorship care as essential: prevention and detection of cancer, cancer surveillance, intervention for long-term/late effects, and coordination of care between providers. One attempt to meet these recommendations is to present patients with a summary of their disease and treatment history (TS) to guide future care outlined in a follow-up plan, together known as the SCP. Although general in nature, the IOM recommends that these plans provide information regarding potential toxicities and late effects, cancer and noncancer surveillance, signs and symptoms of cancer, psychosocial effects, needed referrals, prevention and health promotion, recommendations for genetic testing, and familial cancer risk.5
At the time of the IOM report, the assumption was that SCPs would improve follow-up care and patient outcomes. However, almost 9 years later, cancer centers continue to struggle with implementation barriers including reimbursement issues, institutional resources, and the time required to personalize an SCP.6–8 Despite acknowledgment by professional groups that survivorship should be part of the continuum of cancer care, there remains a lack of evidence-based surveillance guidelines for adult survivors.9 Moreover, there are few data concerning the benefits of SCPs,10–13 inadequate resources to support integrating SCPs into routine care, and lack of processes for examining outcomes. Perry et al14 proposed a framework that includes outcomes such as care coordination; however, it remains unclear whether SCPs improve survivors' knowledge regarding the effects of treatment,15 and there remain no data to indicate whether timing of SCP delivery impacts symptom management, satisfaction, coordination of care, or knowledge.
Some studies have examined attitudes and preferences for delivery of follow-up care among patients and providers. There seems to be a general consensus that survivors and providers are open to written SCPs to support shared care, that content needs to include general information as well as information about specific disease and treatment exposures, and that these SCPs should be personalized to the needs and preferences of patients.16–25 Models for delivering care have been examined including disease-specific and general survivorship clinics, group clinic visits, telephone outreach, consultative clinic visits, shared care, and survivorship care integrated into oncology practices.8,26–30 A variety of care plan templates have been developed31–33; however, providers and investigators continue to debate which specifics should be included.14,34–36 Studies that examine SCP development have focused on identification and management of symptoms, and resource use6–8 with few studies focused on patient experiences.17,23,37,38
Despite inadequate data, SCPs are becoming the standard of care with mandates to comply coming.39 The purpose of this study was to explore the outcomes associated with delivery of a comprehensive, standardized SCP to breast cancer survivors. This pilot study used a quasiexperimental, pretest/post-test design to examine the outcomes achieved by the survivors at seven cancer centers and associated community clinics affiliated with the LIVESTRONG Survivorship Centers of Excellence Network (SCOEN) after a care plan visit. Constructs such as coordination of care, knowledge about survivorship issues, and perceived usefulness of SCPs by patients were examined.
Materials and Methods
Setting
This project took place within a group of seven National Cancer Institute–designated comprehensive cancer centers and their community practices. Participating sites were required to institute a standardized care visit that included a specified TS and SCP. Practitioners (physician extenders, n = 12; physicians, n = 2) were trained in the use of the SCP materials and visit content via telephone and web-based conference training calls. Materials were to be presented to participants in a standard order, with practitioners first presenting the TS and discussing the need for coordination of care with primary and other providers and then presenting the SCP, focusing on future health and behavioral needs, and finishing with a presentation of any additional educational materials that might be of specific assistance to a given survivor. Sites determined their own procedure for ensuring identification of potential participants and completion of materials but were provided with financial and logistic support for these activities.
Participants
Eligibility included age of 18 years or older, diagnosis and treatment of nonmetastatic breast cancer or ductal carcinoma in situ, completion of acute cancer therapy, and a scheduled survivorship visit at the SCOEN site where acute therapy was administered. Time since diagnosis or end of treatment was not controlled. Receipt of targeted or hormonal therapy was allowed. Participants unable to complete informed consent because of language or intellectual difficulties and those who had previously received an SCP were excluded.
Standardized Care Plan Visit
The visit contained three primary components: the Journey Forward TS,31 a LIVESTRONG SCP powered by Penn's Oncolink,32 and educational materials. The TS contains a summary outlining disease and treatment details, American Society of Clinical Oncology guidelines for cancer follow-up and surveillance, a list of potential late effects, and a list of resources.4,33 In presenting the TS, providers worked with survivors to identify specific providers (eg, primary care) responsible for aspects of survivors' future health care and encouraged survivors to share materials with providers. The LIVESTRONG SCP provides individualized recommendations for surveillance and health care guidelines. Recommendations reflect evidence or consensus-based guidelines whenever possible, were developed with provider input, and were described in plain language. To ensure that minimum IOM recommendations for content were met, additional educational materials covered other surveillance recommendations, legal advice, psychosocial issues, counseling, exercise, weight loss and healthy weight, diet and nutrition, immunizations, fatigue, lymphedema, bone loss and osteoporosis, menopausal symptoms, cognitive effects, and genetic testing recommendations. Providers could add to but not remove materials in the educational packet.
Procedure
After approval by all participating institutions' institutional review boards, clinic schedules were screened for eligible potential participants, and participants were approached while checking in. Participants provided informed consent and completed baseline instruments in the clinic. In a second recruitment method, charts were screened before scheduled survivorship visits, and eligible patients were contacted by phone to invite participation. Those who agreed received a letter explaining the study, an informed consent/Health Insurance Portability and Accountability Act form, baseline questionnaire packet, and an envelope in which to store materials. Each Participant was asked to bring the completed packet to her upcoming visit and received a reminder call.
Approximately 3 months after the survivorship visit and baseline measures, participants with internet access were sent an e-mail asking them to log in to a secure Web site to complete follow-up measures. Individuals who did not complete online measures within 1 week received up to three reminder emails and/or telephone calls before being considered lost to follow-up. Participants without access to the internet or who preferred pen-and-paper questionnaires were sent a follow-up questionnaire packet at 3 months. If materials were not returned within 2 weeks, participants received up to three telephone reminder calls before being considered lost to follow-up.
Measures
Unless otherwise noted, the following measures were designed by members of the investigator team (S.C.P./C.T.S./L.A.J.) through literature review, clinical experience, and consensus (materials available on request).
Demographics.
Demographics included age, race, ethnicity, marital status, education, current employment, and household income.
Quality of life.
Quality of life was assessed using the Medical Outcomes Study Short Form (SF) –12.40 The SF-12 is an extensively validated instrument that has been widely used as an alternative to the SF-36 and shown to account for more than 90% of the variance in SF-36 summary measures.
Use of SCP materials.
A 16-item investigator-developed survey assessed patient use of SCPs.41 The survey covered use of the SCPs for seeking information (eg, online searching, questioning of providers), behavior change (eg, making changes in diet), and communication (eg, sharing with a primary care provider).
Satisfaction with SCP.
Participants rated global satisfaction with SCPs on a five-point scale ranging from “extremely unsatisfied” to “extremely satisfied.” Satisfaction was also rated using a newly developed scale indicating degree of agreement with 10 items assessing whether the SCP was useful, informative, and reassuring on a scale of 0 (“strongly disagree”) to 3 (“strongly agree”; Cronbach's alpha = .82).41
Primary outcomes.
Perceived coordination of survivorship care was assessed using a five-item investigator-developed questionnaire. This questionnaire assessed the degree to which patients agreed with statements that health care providers worked together to provide quality care in a coordinated fashion (eg, “My health care providers communicate with one another about my needs”) on a scale of 0 (“strongly disagree”) to 3 (“strongly agree”; Cronbach's alpha = .84).41
Perceived knowledge about survivorship care was assessed using a newly developed 13-item scale assessing degree of agreement with statements concerning patients' knowledge of potential long-term effects of disease and treatment and how to access follow-up care (eg, “I know which provider is responsible for ordering screening tests to look for cancers other than breast cancer”) on a scale of 0 (“strongly disagree”) to 3 (“strongly agree”; Cronbach's alpha = .87).41
Perceived provider knowledge was assessed using three items assessing patient perception of how well follow-up providers understand their medical history and its impact on their quality of life on a scale of 0 (“poor”) to 4 (“excellent”; Cronbach's alpha = .84).41
Provider behavior was assessed using six items assessing the frequency with which providers attended to the informational and supportive needs of participants (eg, “How often did your provider make sure that you understood all the information he or she gave you”) on a scale of 0 (“never”) to 3 (“always”; Cronbach's alpha = .93).41
Results
Participants
Of 193 women recruited, 139 provided both baseline and 3-month follow-up data (72%). As seen in Table 1, these women were primarily middle-age, white, married, college graduates, employed, with incomes of greater than $80,000 per year. Most had been diagnosed with stage I or II breast cancer at an average of 3.4 years previous to enrollment. Using the SF-12, participants at baseline reported mental health that was significantly higher than normative values (M = 54.38; standard deviation [SD] = 11.19; P < .001) whereas physical health was significantly lower than normative values (M = 47.97; SD = 8.85; P < .01). Quality of life was significantly related to time since diagnosis for mental health (r = .286; P = .001) but not for physical health (r = .121; P was not significant).
Table 1.
Participant Demographic and Clinical Characteristics
| Characteristic | No. | % |
|---|---|---|
| Age, years | ||
| Mean | 53.93 | |
| SD | 10.68 | |
| Range | 25-80 | |
| Time since diagnosis, months | ||
| Mean | 3.43 | |
| SD | 3.83 | |
| Range | 3-240 | |
| SF-12 mental health | ||
| Mean | 54.38 | |
| SD | 11.19 | |
| SF-12 physical health | ||
| Mean | 47.97 | |
| SD | 8.85 | |
| Stage at diagnosis | ||
| 0 | 10 | 7.2 |
| I | 52 | 37.4 |
| II | 51 | 36.7 |
| III | 21 | 15.1 |
| Chemotherapy | 93 | 69.4 |
| Endocrine therapy | 96 | 72.7 |
| Race | ||
| White | 126 | 90.6 |
| Black | 10 | 7.2 |
| Marital status | ||
| Married | 112 | 80.6 |
| Unmarried | 27 | 19.4 |
| Employment status | ||
| Working full time | 65 | 46.8 |
| Working part time | 22 | 15.8 |
| Retired | 28 | 20.1 |
| Other | 24 | 17.3 |
| Education | ||
| ≤ High school | 17 | 13.2 |
| Completed college/trade school | 61 | 43.9 |
| Graduate degree | 40 | 28.8 |
| Income, $ | ||
| < 60,000 | 33 | 23.7 |
| 60,000-100,000 | 31 | 22.3 |
| > 100,000 | 62 | 44.6 |
| Comorbidities | ||
| 0 | 50 | 36.2 |
| 1-2 | 55 | 39.9 |
| > 2 | 34 | 23.7 |
Abbreviations: SD, standard deviation; SF, Short Form.
Those who completed both assessments did not differ significantly from those who did not in age, race, marital status, education, employment status, income, stage at diagnosis, or SF-12 mental or physical health (all P > .19). There was a nonsignificant trend among those who did not complete the assessments to be farther from their initial cancer diagnosis (M = 4.78) than those who completed assessments (M = 3.44; F[1, 191] = 3.75; P = .054).
Use of SCP Materials
Table 2 shows self-reported use of SCP materials in the 3-month postintervention period. More than 96% of participants reported that they retained their SCP, and 88% said that they read it carefully. Overall, participants reported using the SCP in 6.9 (SD = 3.95) different ways. Although most women shared their SCP with their partner, used it to assist discussion of their cancer experience with family members, or to help inform family members about their own cancer risk, less than 25% shared the SCP with their primary care providers. The most common uses of the SCP were in the realm of health behaviors such as making decisions about exercise, diet, and the type/frequency of medical testing. SCPs were less commonly used to assist in searches for information or resources. There was a small but significant relationship between total use of SCPs and time since diagnosis (r [138] = −.18; P = .03) with individuals closer to diagnosis reporting greater use.
Table 2.
Self-Reported Use of SCP Materials
| Reported Use | No. | % |
|---|---|---|
| Read it carefully | 121 | 87.7 |
| Used it to help you decide what kind of exercise to engage in | 89 | 64.0 |
| Used it to help make changes in what you eat | 86 | 61.9 |
| Used it to help you decide which F/U tests you need and when | 86 | 61.9 |
| Used it to help communicate concerns to provider | 78 | 56.1 |
| Used it to help you talk about your cancer experience with family | 76 | 54.7 |
| Used it to inform yourself about symptoms | 74 | 53.2 |
| Shared it with spouse | 70 | 50.4 |
| Used it to help you talk with family members about their risk for cancer | 68 | 48.9 |
| Used it to help you take action about seeing PCP | 64 | 46.0 |
| Used it to help you make decisions about losing weight | 61 | 43.9 |
| Used it to search for online information | 54 | 38.8 |
| Used it to help you find resources for support | 47 | 33.8 |
| Used it to help find referrals for F/U | 34 | 24.5 |
| Shared it with family members who might be at risk for cancer | 33 | 23.7 |
| Shared it with PCP | 29 | 20.9 |
Abbreviations: F/U, follow-up; PCP, primary care provider; SCP, survivorship care plan.
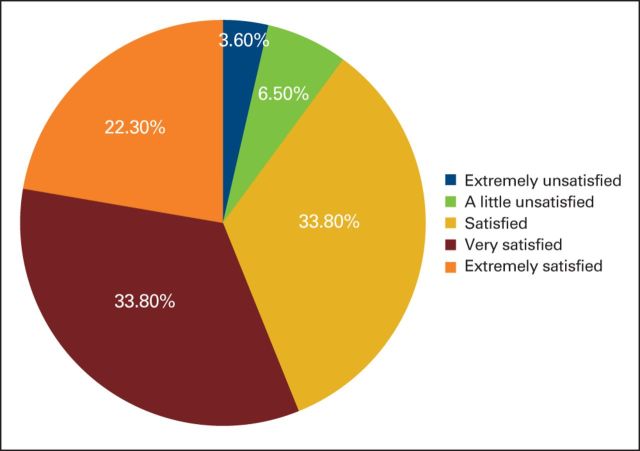
Satisfaction With SCP Materials
Overall satisfaction with the SCP is shown in Appendix Figure A1 (online only). Approximately 56% reported being “very” or “extremely satisfied,” whereas only 10% of participants reported being “unsatisfied.” Satisfaction with SCPs was significantly related to time since diagnosis (r [138] = −.26; P = .002). Examination of means showed that those who reported being “unsatisfied” were on average 5.6 years (SD, 5.08 years) from diagnosis whereas those in the “extremely satisfied” group were an average of 2.6 years (SD, 2.73 years) from diagnosis. Overall satisfaction was moderately related to total use of SCP materials; those who used the materials were more satisfied (r = .37; P < .001).
Participants generally agreed that SCPs were useful, informative, and reassuring (M = 2.14 [0.39]). This was unrelated to time since diagnosis (r = −.06; P was not significant), although moderately related to total use of SCPs (r = .47; P < .001).
Outcomes of the SCP Visit
Table 3 presents means for the pre/post outcome variables. Overall, participants reported significant increases in perceived coordination among providers (t = −4.15; P < .001). Correlation of change scores with time since diagnosis suggested that increased coordination was independent of time since diagnosis (r = −.044; P was not significant). Perceived knowledge concerning cancer care increased significantly after the SCP visit (t = −5.09; P < .001). Change in perceived knowledge was also independent of time since diagnosis (r = .05; P was not significant). Perceived provider knowledge increased after the SCP visit (t = −2.04; P < .05), independent of time since diagnosis (r = −.12; P was not significant). Finally, perceived provider behavior produced a nonsignificant trend toward improvement (t = −1.61; P = .11) independent of time since diagnosis (r = .07; P was not significant). There were no significant differences between SCOEN sites in pre/post change in any primary outcomes (all F < 0.96; all P > .45).
Table 3.
Outcome Variables
| Variable | Before the Visit |
After the Visit |
t | P | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Coordination of care | 2.11 | 0.49 | 2.27 | 0.44 | −4.15 | < .001 |
| Knowledge about care | 1.76 | 0.54 | 1.99 | 0.42 | −5.09 | < .001 |
| Provider knowledge of cancer's effects | 2.59 | 1.12 | 2.77 | 0.91 | −2.04 | < .05 |
| Satisfaction with provider behavior | 2.56 | 0.61 | 2.64 | 0.52 | −1.61 | .11 |
Abbreviation: SD, standard deviation.
Discussion
SCP delivery will be mandated for the more than 70% of patients with cancer treated in American College of Surgeons–accredited centers,39 and this is likely an underestimate given IOM recommendations.4 Few studies have examined outcomes of providing SCPs in the United States. Our results suggest that breast cancer survivors tend to use and be highly satisfied with SCPs. In the 3 months after SCP receipt, most survivors used the materials to assist them in making health behavior choices and to aid in communication with family and providers. Only approximately one of five participants shared the SCP with their primary care provider, suggesting that follow-up may have been too brief for survivors to have had a primary care provider visit. We examined the rate of sharing SCP materials among participants who had seen a primary care provider and found a somewhat higher rate (approximately 38%). In addition, those closer in time to diagnosis reported greater use and satisfaction than those for whom more time had elapsed, and greater use was associated with greater satisfaction. With respect to changes after receipt of SCPs, patients reported greater belief that their medical care was coordinated, that their provider was knowledgeable, and that they were knowledgeable about managing their own survivorship care.
These findings are similar to those of others who found high satisfaction with SCPs42 and support findings of Kaiser-Hill et al43 that used a prior version of the SCP in a self-selected sample of diverse patients and a post-test–only design. These survivors also reported high satisfaction with the information received, that it assisted them in making health behavior decisions, and that they planned to use the materials to communicate with their health care team. Among those who had already used the materials with their providers, 80% reported that the SCP was helpful in facilitating communication. This study furthers these results by demonstrating pre/post changes in behaviors, perceptions of care, and actual use of materials over a longer period of time in a less self-selected sample. Moreover, our results suggest that earlier access to SCPs results in greater changes than later exposure.
These results differ somewhat from those reported by Grunfeld et al2—satisfaction and perceived coordination of care were either unaffected or slightly decreased at 3 months after an SCP visit, and time from diagnosis did not influence outcomes. Our data suggested both an increase in satisfaction/coordination and that those closer to the time of diagnosis experienced a greater change across several constructs. This may partly reflect the usual care condition described by Grunfeld et al, in which participants received a discharge visit and transfer to primary care, to which the experimental arm added delivery of a written SCP. Care of this quality is seldom routine in US hospital systems, and similarity between control and experimental arms makes interpretation of null results difficult to interpret, let alone generalize.3 Regardless, given the differences between the United States and Canadian health care systems, our results suggest that SCPs may be more impactful in more fragmented health care systems.
This work is limited by its quasiexperimental design and should be seen as suggestive rather than definitive. More sophisticated trials are needed to confirm results and extend these across time and populations. Our sample was primarily white and well-educated and received care at specialized survivorship clinics/visits; these results may not generalize to other populations or settings. Moreover, many of the measures were developed specifically for this study or were relatively new. Although internal consistency was adequate for those measures for which this is an appropriate metric, these measures will require further refinement and validation. Similarly, given that survivors could be seen for later follow-up care by affiliated or nonaffiliated health care providers, we relied on self-report rather than chart abstraction to ascertain follow-up behaviors. Strengths included a well-characterized sample obtained across a wide variety of cancer care settings, pre/post assessments, high retention, and visits and materials that were standardized across settings. Moreover, similar results across participating centers suggest that it is possible to standardize visits and materials across diverse settings and providers, and success at all sites in recruitment and completion suggests that, with institutional commitment and financial and logistical support, SCPs can be delivered to patients.
In summary, our data suggest that SCPs are valued and used by breast cancer survivors, particularly among those closer to diagnosis and treatment, and that there may be a teachable moment earlier in the survivorship trajectory when survivors are more open to behavioral change for health promotion.44 SCPs may also influence perceptions of the coordination of care received and knowledge of the transition to survivorship. As mandates for the provision of SCPs are made, research focusing on whether SCPs result in improved health behaviors and outcomes, reduced burden in care transitions from the oncology setting, and research on cost-effectiveness will be needed if efforts are to be sustainable.
Acknowledgment
Supported by the LIVESTRONG Foundation.
Presented the 36th Annual San Antonio Breast Cancer Symposium, San Antonio, TX, December 9-13, 2013.
Appendix
Figure A1.
Overall satisfaction with survivorship care plans.
Authors' Disclosures of Potential Conflicts of Interest
Disclosures provided by the authors are available with this article at jop.ascopubs.org.
Author Contributions
Conception and design: Steven C. Palmer, Carrie Tompkins Stricker, SarahLena L. Panzer, Sarah A. Arvey, Jackie Casillas, Patricia A. Ganz, Mary S. McCabe, Larissa Nekhlyudov, Betsy Risendal, Donald L. Rosenstein, Karen L. Syrjala, Linda A. Jacobs
Administrative support: Sarah A. Arvey
Provision of study materials or patients: Ann H. Partridge, Donald L. Rosenstein, Karen L. Syrjala
Collection and assembly of data: Steven C. Palmer, Carrie Tompkins Stricker, SarahLena L. Panzer, Sarah A. Arvey, Mary S. McCabe, Larissa Nekhlyudov, Linda Overholser, Ann H. Partridge, Betsy Risendal, Karen L. Syrjala
Data analysis and interpretation: Steven C. Palmer, Carrie Tompkins Stricker, SarahLena L. Panzer, K. Scott Baker, Larissa Nekhlyudov, Ann H. Partridge, Betsy Risendal, Karen L. Syrjala, Linda A. Jacobs
Manuscript writing: All authors
Final approval of manuscript: All authors
AUTHORS' DISCLOSURES OF POTENTIAL CONFLICTS OF INTEREST
Outcomes and Satisfaction After Delivery of a Breast Cancer Survivorship Care Plan: Results of a Multicenter Trial
The following represents disclosure information provided by authors of this manuscript. All relationships are considered compensated. Relationships are self-held unless noted. I = Immediate Family Member, Inst = My Institution. Relationships may not relate to the subject matter of this manuscript. For more information about ASCO's conflict of interest policy, please refer to www.asco.org/rwc or jop.ascopubs.org/site/misc/ifc.xhtml.
Steven C. Palmer
No relationship to disclose
Carrie Tompkins Stricker
Employment: On Q Health
Leadership: On Q Health
Stock or Other Ownership: On Q Health
Consulting or Advisory Role: On Q Health
Travel, Accommodations, Expenses: On Q Health
SarahLena L. Panzer
Consulting or Advisory Role: On Q Health
Travel, Accommodations, Expenses: On Q Health
Sarah A. Arvey
No relationship to disclose
K. Scott Baker
Travel, Accommodations, Expenses: Medac
Jackie Casillas
No relationship to disclose
Patricia A. Ganz
Leadership: Intrinsic LifeSciences (I)
Stock or Other Ownership: xenon (I), Intrinsic LifeSciences (I), Silarus Therapeutics (I), Merganser Biotech (I)
Consulting or Advisory Role: Keryx (I), Merganser Biotech (I), Silarus Therapeutics (I)
Research Funding: Keryx (I)
Patents, Royalties, Other Intellectual Property: Related to iron metabolism and the anemia of chronic disease (I)
Travel, Accommodations, Expenses: Intrinsic LifeSciences (I), Keryx (I)
Mary S. McCabe
No relationship to disclose
Larissa Nekhlyudov
No relationship to disclose
Linda Overholser
Stock or Other Ownership: Athena Health (I)
Ann H. Partridge
No relationship to disclose
Betsy Risendal
No relationship to disclose
Donald L. Rosenstein
No relationship to disclose
Karen L. Syrjala
No relationship to disclose
Linda A. Jacobs
No relationship to disclose
References
- 1.American Cancer Society. Cancer treatment and survivorship facts & figures (2012-2013) http://www.cancer.org/Research/CancerFactsStatistics/cancer-treatment-survivorship-facts-figures.pdf.
- 2.Grunfeld E Julian JA Pond G, etal: Evaluating survivorship care plans: Results of a randomized, clinical trial of patients with breast cancer J Clin Oncol 29:4755–4762,2011 [DOI] [PubMed] [Google Scholar]
- 3.Stricker CT, Jacobs LA, Palmer SC: Survivorship care plans: An argument for evidence over common sense J Clin Oncol 30:1392–1393,2012author reply 1393-1395 [DOI] [PubMed] [Google Scholar]
- 4.Hewitt M, Greenfield S, Stovall E: From Cancer Patient to Cancer Survivor: Lost in Transition 2006Washington, DC: National Academies Press [Google Scholar]
- 5.Palmer SC Jacobs LA DeMichele A, etal: Metrics to evaluate treatment summaries and survivorship care plans: A scorecard Support Care Cancer 22:1475–1483,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dulko D Pace CM Dittus KL, etal: Barriers and facilitators to implementing cancer survivorship care plans Oncol Nurs Forum 40:575–580,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mayer DK: Survivorship care plans: Necessary but not sufficient? Clin J Oncol Nurs 18:7–8,2014suppl [DOI] [PubMed] [Google Scholar]
- 8.Eshelman-Kent D Kinahan KE Hobbie W, etal: Cancer survivorship practices, services, and delivery: A report from the Children's Oncology Group (COG) nursing discipline, adolescent/young adult, and late effects committees J Cancer Surviv 5:345–357,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jacobs LA Palmer SC Schwartz LA, etal: Adult cancer survivorship: Evolution, research, and planning care CA Cancer J Clin 59:391–410,2009 [DOI] [PubMed] [Google Scholar]
- 10.Earle CC: Long term care planning for cancer survivors: A health services research agenda J Cancer Surviv 1:64–74,2007 [DOI] [PubMed] [Google Scholar]
- 11.Faul LA Shibata D Townsend I, etal: Improving survivorship care for patients with colorectal cancer Cancer Control 17:35–43,2010 [DOI] [PubMed] [Google Scholar]
- 12.Oeffinger KC Hudson MM Mertens AC, etal: Increasing rates of breast cancer and cardiac surveillance among high-risk survivors of childhood Hodgkin lymphoma following a mailed, one-page survivorship care plan Pediatr Blood Cancer 56:818–824,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Grunfeld E Julian JA Pond G, etal: Survivorship care plans, quality of care, and barriers to care J Clin Oncol 29:551s,2011suppl 15s abstr 9005 [DOI] [PubMed] [Google Scholar]
- 14.Parry C Kent EE Forsythe LP, etal: Can't see the forest for the care plan: A call to revisit the context of care planning J Clin Oncol 31:2651–2653,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rocque GB Wisinski KB Buhr KA, etal: Development and evaluation of a survey to assess survivor knowledge change after survivorship care plans: WiSDOM-B (Wisconsin Survey of cancer DiagnOsis and Management in Breast cancer) J Cancer Educ 29:270–277,2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Brennan ME Butow P Spillane AJ, etal: Survivorship care after breast cancer: Follow-up practices of Australian health professionals and attitudes to a survivorship care plan Asia Pac J Clin Oncol 6:116–125,2010 [DOI] [PubMed] [Google Scholar]
- 17.Brennan ME Butow P Marven M, etal: Survivorship care after breast cancer treatment: Experiences and preferences of Australian women Breast 20:271–277,2011 [DOI] [PubMed] [Google Scholar]
- 18.Marbach TJ, Griffie J: Patient preferences concerning treatment plans, survivorship care plans, education, and support services Oncol Nurs Forum 38:335–342,2011 [DOI] [PubMed] [Google Scholar]
- 19.Brothers BM Easley A Salani R, etal: Do survivorship care plans impact patients' evaluations of care? A randomized evaluation with gynecologic oncology patients Gynecol Oncol 129:554–558,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salz T Oeffinger KC Lewis PR, etal: Primary care providers' needs and preferences for information about colorectal cancer survivorship care J Am Board Fam Med 25:635–651,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mao JJ Bowman MA Stricker CT, etal: Delivery of survivorship care by primary care physicians: The perspective of breast cancer patients J Clin Oncol 27:933–938,2009 [DOI] [PubMed] [Google Scholar]
- 22.Grunfeld E Fitzpatrick R Mant D, etal: Comparison of breast cancer patient satisfaction with follow-up in primary care versus specialist care: Results from a randomized controlled trial Br J Gen Pract 49:705–710,1999 [PMC free article] [PubMed] [Google Scholar]
- 23.Smith SL Singh-Carlson S Downie L, etal: Survivors of breast cancer: Patient perspectives on survivorship care planning J Cancer Surviv 5:337–344,2011 [DOI] [PubMed] [Google Scholar]
- 24.Smith SL Wai ES Alexander C, etal: Caring for survivors of breast cancer: Perspective of the primary care physician Curr Oncol 18:e218–e226,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mayer DK Gerstel A Leak AN, etal: Patient and provider preferences for survivorship care plans J Oncol Pract 8:e80–e86,2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jefford M Lotfi-Jam K Baravelli C, etal: Development and pilot testing of a nurse-led posttreatment support package for bowel cancer survivors Cancer Nurs 34:E1–E10,2011 [DOI] [PubMed] [Google Scholar]
- 27.Horning SJ: Follow-up of adult cancer survivors: New paradigms for survivorship care planning Hematol Oncol Clin North Am 22:201–210,2008 [DOI] [PubMed] [Google Scholar]
- 28.Trotter K Frazier A Hendricks CK, etal: Innovation in survivor care: Group visits Clin J Oncol Nurs 15:E24–E33,2011 [DOI] [PubMed] [Google Scholar]
- 29.Kent EE Smith AW Keegan TH, etal: Talking about cancer and meeting peer survivors: Social information needs of adolescents and young adults diagnosed with cancer J Adolesc Young Adult Oncol 2:44–52,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCabe MS, Jacobs LA: Clinical update: survivorship care: Models and programs Semin Oncol Nurs 28:e1–e8,2012 [DOI] [PubMed] [Google Scholar]
- 31.Journey Forward. About survivorship care planning. http://www.journeyforward.org/about-survivorship-care.
- 32.LIVESTRONG. LIVESTRONG care plan. http://www.livestrongcareplan.org/
- 33.American Cancer Society. Survivorship care plans. http://www.cancer.org/Treatment/SurvivorshipDuringandAfterTreatment/SurvivorshipCarePlans/index.
- 34.Ashing-Giwa K Tapp C Brown S, etal: Are survivorship care plans responsive to African-American breast cancer survivors? Voices of survivors and advocates J Cancer Surviv 7:283–291,2013 [DOI] [PubMed] [Google Scholar]
- 35.Smith TJ, Snyder C: Is it time for (survivorship care) plan B? J Clin Oncol 29:4740–4742,2011 [DOI] [PubMed] [Google Scholar]
- 36.Stricker CT Jacobs LA Risendal B, etal: Survivorship care planning after the Institute of Medicine recommendations: How are we faring? J Cancer Surviv 5:358–370,2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Hill-Kayser CE Vachani C Hampshire MK, etal: An internet tool for creation of cancer survivorship care plans for survivors and health care providers: Design, implementation, use and user satisfaction J Med Internet Res 11:e39,2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Hill-Kayser CE Vachani C Hampshire MK, etal: High level use and satisfaction with internet-based breast cancer survivorship care plans Breast J 18:97–99,2012 [DOI] [PubMed] [Google Scholar]
- 39.American College of Surgeons. Cancer Program Standards 2012: Ensuring patient-centered care. https://www.facs.org/quality%20programs/cancer/coc/standards.
- 40.Ware J, Jr, Kosinski M, Keller SD: A 12-item short-form health survey: Construction of scales and preliminary tests of reliability and validity Med Care 34:220–233,1996 [DOI] [PubMed] [Google Scholar]
- 41.Stricker CT Palmer SC Panzer SL, etal: Breast cancer survivors' outcomes and satisfaction following delivery of a survivorship care plan: Results of a multicenter trial Presented at the 36th Annual San Antonio Breast Cancer Symposium December 9-13, 2013 San Antonio, TX (abstr P3-08-02) [Google Scholar]
- 42.Sprague BL Dittus KL Pace CM, etal: Patient satisfaction with breast and colorectal cancer survivorship care plans Clin J Oncol Nurs 17:266–272,2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hill-Kayser CE Vachani CC Hampshire MK, etal: Impact of internet-based cancer survivorship care plans on health care and lifestyle behaviors Cancer 119:3854–3860,2013 [DOI] [PubMed] [Google Scholar]
- 44.Demark-Wahnefried W Aziz NM Rowland JH, etal: Riding the crest of the teachable moment: Promoting long-term health after the diagnosis of cancer J Clin Oncol 23:5814–5830,2005 [DOI] [PMC free article] [PubMed] [Google Scholar]