Abstract
Aims:
This study evaluated effect of infection control barriers on light intensity (LI) of light-curing unit (LCU) and microhardness of composite.
Materials and Methods:
Four different disposable barriers (n = 30) were tested against the control. LI for each barrier was measured with Lux meter. One hundred and fifty Teflon molds were equally divided into five groups of thirty each. Composite was filled in bulk in these molds and cured without and with barrier. Microhardness was evaluated on top and bottom surface of composite specimen with microhardness testing machine and hardness ratio (HR) was derived.
Statistical Analysis Used:
One-way analysis of variance, Tukey's honestly significant difference test, and paired t-test using SPSS version 18 software.
Results:
All barriers had significantly reduced the baseline LI of LCU (P < 0.0001), but only Cure Elastic Steri-Shield and latex cut glove pieces (LCGP) significantly reduced the microhardness of the composite (P < 0.05). However, HR determined inadequate curing only with LCGP.
Conclusions:
Although entire tested barrier significantly reduced the LI; none, except LCGP markedly affected the degree of cure of the composite.
Keywords: Barriers, hardness ratio, light-curing unit, light intensity, microhardness
INTRODUCTION
“To do no harm” is one of the prime ethical considerations that every dental practitioner should be concerned. Failure to sterilize the instrument can cause cross-infection leading to iatrogenic diseases. The exposure of dentist, auxiliaries, and patients to a variety of infectious agents is a potent danger which was recognized but generally overlooked.[1] Cross-infection with the agents causing diseases such as hepatitis B and acquired immunodeficiency syndrome has diverted clinician's attention to the importance of sterilization and thus led to the development of variety of infection control procedures.[1]
Visible light-curing units (LCUs) are indispensable in the practice of clinical dentistry today.[2] They are commonly used to cure composite and other light-activated resin-based restorative materials.[2] A survey published in 1998 showed that 27% of dentists used resin composites almost exclusively for posterior restorations.[3]
The light guide (LG) of LCU has been put under “semi-critical category” in the Centers for Disease Control and Prevention (CDC) guidelines because they are used within the oral cavity, have the potential for saliva or blood contamination, and can cause transmission of infection among the patients.[1,4] Hence, various attempts to sterilize or disinfect the LGs were considered.
Literature suggests four most common methods of maintaining sterility of the LG: (a) wiping the guide with a suitable disinfectant after use in each patient;[1] (b) using autoclavable guides;[5] (c) using presterilized, single-use plastic guides;[6] and (d) using disposable barriers to cover the guide.[7,8]
The first two methods promised excellent infection control but proved to be time consuming and caused irreversible damage to the structures in the LG.[1,5,9] Single-use plastic LG causes a significant reduction in the light intensity (LI) if the sides of clear LG come into contact with the oral tissues.[6]
Disposable infection control barriers (ICB) such as light tip sleeves, plastic wrap, and finger cots may be a cost-effective alternative to avoid contamination of the LG.[8] It provides a convenient, noninvasive method of preventing contact between the oral tissues and the guide[8] and eliminates the risk of damaging.
However, these types of barriers may have its ill effects on the light output of the LCU, inadequate curing, and thus affecting the properties and quality of the light-cured material. Thus, the present study evaluated the LI of LCU after placement of various disposable ICB on LG, its effect on the Vicker's microhardness (HV) of the composite which indirectly reflects the degree of polymerization of composites. The null hypothesis was made that disposable ICB do not affect the LI of LCU and microhardness of composite.
MATERIALS AND METHODS
Bluephase (Ivoclar Vivadent, Liechtenstein), light-emitting diode (LED) LCU with 10 mm standard LG was used throughout this study. A custom jig was prepared to standardize the position of tip of LCU over photodetector sensor and surface of composite.
Evaluation of light intensity
LCU with fully charged battery was mounted on custom-made jig in such a way that the light-curing tip should descend perpendicular to the photodetector sensor of the Lux meter (TES Digital Light Meter, Taiwan). Based on the type of disposable ICB, the distribution of samples (n = 30) was as follows:
Group A: Control group (CG): No barrier was placed
Group B: Cling Wrap PVC (CWPVC) (Ezee, Mumbai, India)
Group C: Complete LED Curing Light Sleeve (CLCLS) (Pinnacle, Kerr Total Care, Romulus, MI, USA)
Group D: Cure Elastic Steri-Shield (CESS) (Steri-Shield, Santa Barbara, California)
Group E: Latex-cut glove pieces (LCGP) (Nulife, Mumbai, India).
In CG, LI was measured on thirty separate occasions to achieve mean baseline LI of the LCU. Before proceeding to the every next group, each time battery was fully charged. In study (barrier) groups (i.e., Group B to E), ICB was placed on LG according to manufacturer's instructions, and the LI was measured on ten separate occasions for each barrier and its mean was taken as a LI for that barrier. Before placing every next barrier, the tip of the guide was cleaned with absorbent gauze. The values were recorded in terms of Lux. These values were converted into mW/cm2 by the equation mentioned by McCabe and Carrick[10] and Harrington and Wilson.[11]
1 Lux = 0.005 mW/cm2 Eq. (1)
Evaluation of Vicker's microhardness of composite
One hundred and fifty circular molds (5 mm diameter × 2 mm thickness) were prepared from 150 Teflon disks (Maxwell, India) of 2 mm thickness. The resultant molds were randomly and equally divided into above-mentioned five groups (n = 30). Teflon mold was placed on a Mylar strip (Samit products, New Delhi, India) and glass slab. Bulk of composite resin (Filtek Z 350 × T, 3M ESPE, St. Paul, MN USA.) was inserted into the Teflon mold. Firm pressure for 30 s was applied with the glass slide (Blue Star, Mumbai, India) to extrude the excess of material.
These composite samples were irradiated through the disposable ICB of respective groups; with same Bluephase LED LCU which was mounted on the jig, for 40 s with the tip kept in close contact and perpendicular to the surface of the composite specimen. In CG, the samples were cured without placing any barrier on the LG. The top surface of each Teflon mold was marked with an indelible marker.
Specimens in each group were stored in a light proof container at 37°C and 100% relative humidity for 24 h. Both surfaces of composite restorations were polished with composite finishing and polishing kit (Sof-Lex, 3M ESPE, St. Paul, MN, USA).
HV was measured on top and bottom surface of each composite sample using a Mitutoyo microhardness testing machine (Instrument No. 810-117E, Mitutoyo, New Delhi, India). The indenter was applied at three predetermined points on the central part of each specimen surface with the load of 50 g for 15 s. The indentations in the sample surface were measured under 100 times magnification. The mean of three was taken as a microhardness of each surface of specimen.
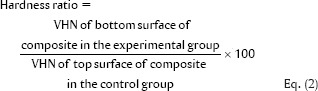
A hardness ratio (HR) was also obtained as suggested by Hwang et al.[12]
The thickness of each barrier in the study group was measured with the digital micrometer (Mitutoyo, Japan).
Data were analyzed with one-way analysis of variance (ANOVA), Tukey's honestly significant difference test, and paired t-test using SPSS version 18 software (SPSS Inc. Released 2009. PASW Statistics for Windows, Version 18.0. Chicago, Ill., USA: SPSS Inc.).
RESULTS
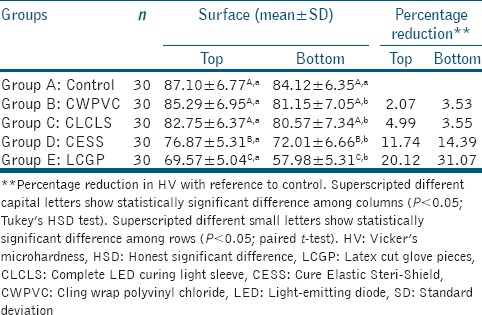
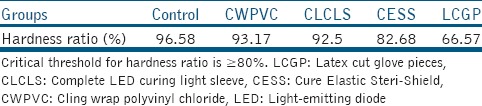
Entire tested barrier had significantly reduced the baseline LI of LCU (P < 0.0001). CWPVC (6.57%) caused the least whereas LCGP (47.19%) caused the greatest percentage reduction [Table 1 and Graph 1]. Except for the CG, all the groups showed the significant difference between mean microhardness of top and bottom surface of composite (P < 0.05). Among the top and bottom surfaces of different groups, HV was significantly reduced in case of CESS and LCGP (P < 0.05) [Table 2 and Graphs 2, 3]. Whereas HR had shown that composite resin in all groups except LCGP was adequately polymerized [Table 3].
Table 1.
Light intensity (mW/cm2) among different types of barriers
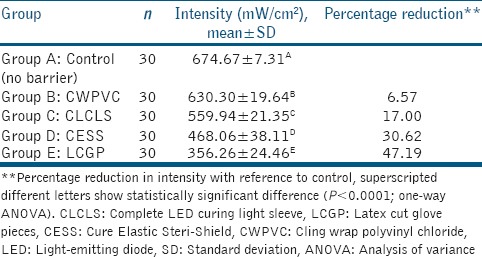
Graph 1.
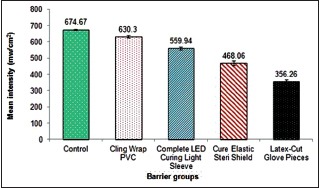
Mean intensity (mw/cm2) for control and different types of barriers. Dissimilar color shows statistically significant difference among different groups (P < 0.0001; one-way analysis of variance)
Table 2.
Vicker's microhardness of composite specimens in different groups
Graph 2.
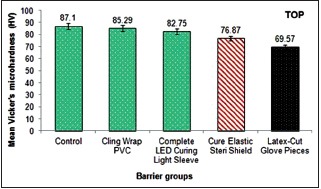
Mean microhardness of top surface of composite specimens in different groups. Dissimilar color shows statistically significant difference among different groups (P < 0.05; Tukey's honestly significant difference test)
Graph 3.
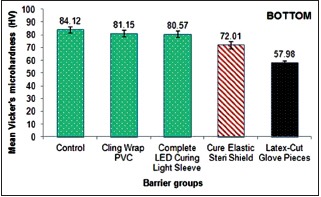
Mean microhardness of bottom surface of composite specimens in different groups. Dissimilar color shows statistically significant difference among different groups (P < 0.05; Tukey's honestly significant difference test)
Table 3.
Hardness ratio for composite resin belonging to different groups
DISCUSSION
Visible light-activated materials have been used in dentistry since 40 years and have revolutionized the field of clinical dentistry. According to the CDC Guidelines for infection control, LGs of LCU should be sterile before using it in every next patient.[4,12]
Use of disposable ICB that covers the LG found to be most acceptable, more practical, and convenient method. However, it apparently causes the reduction in the LI of the LCU.[7,8] The present study evaluated the effect of four commercially available disposable ICB on LI of LCU and its subsequent effect on the microhardness of composite.
Currently, Dental Clinicians are preferring LED LCU over other types because of it's many advantages like: it has longer bulb life with fewer maintenance related problems, it emits radiation only in blue segment of visible spectrum of light, it consumes lesser energy, it can be powered by rechargeable battery source and thus can be cordless and convenient for operator to handle, since it does not generate any heat; cooling fan is not required and hence these are silent, it produces higher power intensity; thus reduces polymerization time.[13]
Precision of commercially available dental radiometers which measures the power output of LCU is proven to be questionable as compared to laboratory grade power meter.[2,14] TES Digital Light Meter is one such laboratory grade light meter which measures LI in terms of Lux.[15] It is analogous to the radiant intensity unit, i.e., watts per square meter.[16]
In the present study, since all the tested barriers have significantly reduced the baseline LI of LCU [Table 1 and Graph 1], the null hypothesis was rejected. These results are in agreement with those of Chong et al.,[7] Scott et al.,[8] Chang et al.,[17] and McAndrew et al.[18]
In the present study, CWPVC was found most efficient in transmitting the light whereas LCGP was least [Table 1 and Graph 1]. However, none of the tested barriers reduced the LI below the critical value 300 mw/cm2. This may be due to high-intensity LCU (675 mW/cm2) was used in this study. However, according to clinical survey by Hegde et al., majority of tested LED LCU were having inherent LI in between 200 and 400 mw/cm2.[19] Therefore, we discourage the use of LCGP as a disposable ICB for LCU with lower inherent power output.
Differences in the mean intensities among different ICB can be attributed to its transparency,[20] thickness of the tested barriers,[17] presence of folds,[21,22] and formation of air pouch between light tip and barrier.[8,23]
Two of the tested barriers, i.e., CWPVC and CLCLS found to be more transparent than CESS and LCGP which were translucent. Thus, CWPVC and CLCLS allowed to pass significantly more light than two other barriers.
Further, there was a significant difference in LI in between transparent and in between translucent barriers which can be explained on account of their thicknesses. The mean thickness was as follows:
LCGP - 0.219 mm
CESS - 0.126 mm
CLCLS - 0.055 mm
CWPVC - 0.028 mm.
One-way ANOVA showed a statistically significant difference in mean thickness across the barriers (P < 0.0001). Thus, LCGP due to its greatest thickness caused maximum reduction in the LI.
de Moraes Porto et al.[21] and Coutinho et al.[22] revealed that folds and wrinkles in the barriers at the tip of LG can cause light deviation and energy loss and thus decrease in LI. In this study, the unavoidable fold at the tip in CLCLS might have caused more intensity reduction than CWPVC which was without folds.
Pollington et al.[24] have mentioned that entrapped air between barriers and LG may increase the distance between LG and restoration and decrease the curing effectiveness. Formation of air pouches was avoided in this study by careful placement of barriers.
To confirm whether there is any effect of reduced LI due to various disposable ICB, on the polymerization of composite resin, a HV test was performed on top and bottom surface of composite specimen. LCGP caused the maximum percentage reduction in HV on both the surfaces paralleling its deleterious effect on LI [Table 2].
When compared to CG, CWPVC, and CLCLSs (i.e., transparent barriers) have not significantly affected the mean HV of top and bottom surfaces of composite specimens, whereas CESS and LCGP (i.e., translucent barriers) have significantly decreased it. Thus; in case of microhardness, null hypothesis was accepted for CWPVC and CLCLS whereas it was rejected for CESS and LCGP [Table 2 and Graphs 2, 3]. These results are in partial agreement with those of Chong et al.[7] Al-Marzouk reported the use of nonopaque transparent barriers did not cause any significant difference in the microhardness values of composite resin.[20] In Contrast, Coutinho et al.[22] have concluded that the use of translucent protective barriers on the LGs can impair the percentage degree of conversion (DC) of composite.
According to Hwang et al., the DC of the composite resin specimen is usually assessed by the HR (Eq. 2).[12] The HR should be more than 80% for composite resins that are adequately cured.[12] In the present study, all the barriers except LCGP showed HR more than 80% [Table 3]. These results are in agreement with Sword et al., who revealed only latex-based barriers significantly reduced curing of composite.[25]
CONCLUSIONS
Although different disposable ICB have significantly reduced the LI of the tested LCU, it did not affect the DC of the composite resin to be clinically significant, except for LCGP. Thus, the present study recommends the use of disposable ICB over the LG of the LCU except LCGP.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
Our sincere thanks to Dr. Amruta Mahajan and Mr. Vikrant Dudhkawale, for their kind cooperation while conducting this study.
REFERENCES
- 1.Caughman GB, Caughman WF, Napier N, Schuster GS. Disinfection of visible-light-curing devices. Oper Dent. 1989;14:2–7. [PubMed] [Google Scholar]
- 2.Leonard DL, Charlton DG, Hilton TJ. Effect of curing-tip diameter on the accuracy of dental radiometers. Oper Dent. 1999;24:31–7. [PubMed] [Google Scholar]
- 3.Christensen GJ. Current use of tooth-colored inlays, onlays, and direct-placement resins. J Esthet Dent. 1998;10:290–5. doi: 10.1111/j.1708-8240.1998.tb00506.x. [DOI] [PubMed] [Google Scholar]
- 4.Kohn WG, Collins AS, Cleveland JL, Harte JA, Eklund KJ, Malvitz DM, et al. Guidelines for infection control in dental health-care settings-2003. MMWR Recomm Rep. 2003;52:1–61. [PubMed] [Google Scholar]
- 5.Rueggeberg FA, Caughman WF, Comer RW. The effect of autoclaving on energy transmission through light-curing tips. J Am Dent Assoc. 1996;127:1183–7. doi: 10.14219/jada.archive.1996.0409. [DOI] [PubMed] [Google Scholar]
- 6.Rueggeberg FA, Caughman WF. Factors affecting light transmission of single-use, plastic light-curing tips. Oper Dent. 1998;23:179–84. [PubMed] [Google Scholar]
- 7.Chong SL, Lam YK, Lee FK, Ramalingam L, Yeo AC, Lim CC, et al. Effect of various infection-control methods for light-cure units on the cure of composite resins. Oper Dent. 1998;23:150–4. [PubMed] [Google Scholar]
- 8.Scott BA, Felix CA, Price RB. Effect of disposable infection control barriers on light output from dental curing lights. J Can Dent Assoc. 2004;70:105–10. [PubMed] [Google Scholar]
- 9.Dugan WT, Hartleb JH. Influence of a glutaraldehyde disinfecting solution on curing light effectiveness. Gen Dent. 1989;37:40–3. [PubMed] [Google Scholar]
- 10.McCabe JF, Carrick TE. Output from visible-light activation units and depth of cure of light-activated composites. J Dent Res. 1989;68:1534–9. doi: 10.1177/00220345890680111301. [DOI] [PubMed] [Google Scholar]
- 11.Harrington L, Wilson HJ. Determination of radiation energy emitted by light activation units. J Oral Rehabil. 1995;22:377–85. doi: 10.1111/j.1365-2842.1995.tb00788.x. [DOI] [PubMed] [Google Scholar]
- 12.Hwang IN, Hong SO, Lee BN, Hwang YC, Oh WM, Chang HS, et al. Effect of a multi-layer infection control barrier on the micro-hardness of a composite resin. J Appl Oral Sci. 2012;20:576–80. doi: 10.1590/S1678-77572012000500014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antonson SA, Antonson DE, Hardigan PC. Should my new curing light be an LED? Oper Dent. 2008;33:400–7. doi: 10.2341/07-103. [DOI] [PubMed] [Google Scholar]
- 14.Rueggeberg FA. Precision of hand-held dental radiometers. Quintessence Int. 1993;24:391–6. [PubMed] [Google Scholar]
- 15. [Last accessed on 2017 Nov 08]. Available from: http://www.alaron.ca/pdf/TES1335.pdf .
- 16.Ryer AD, editor. Light Measurement Handbook. 2nd Printing. Newburyport, MA, USA: Technical Publication Dept.; 1998. Measurement geometrics; pp. 29–38. [Google Scholar]
- 17.Chang HS, Lee SR, Hong SO, Ryu HW, Song CK, Min KS. Effect of infection control barrier thickness on light curing units. J Korean Acad Cons Dent. 2010;35:368–73. [Google Scholar]
- 18.McAndrew R, Lynch CD, Pavli M, Bannon A, Milward P. The effect of disposable infection control barriers and physical damage on the power output of light curing units and light curing tips. Br Dent J. 2011;210:E12. doi: 10.1038/sj.bdj.2011.312. [DOI] [PubMed] [Google Scholar]
- 19.Hegde V, Jadhav S, Aher GB. A clinical survey of the output intensity of 200 light curing units in dental offices across Maharashtra. J Conserv Dent. 2009;12:105–8. doi: 10.4103/0972-0707.57633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Marzok MI. The effect of wrapping of light-cure tips on the cure of composite resin. Eur J Gen Dent. 2012;1:183–6. [Google Scholar]
- 21.de Moraes Porto IC, Ramos de Brito AC, Parolia A. Effect of cross infection control barriers used on the light-curing device tips on the cure depth of a resin composite. J Conserv Dent. 2013;16:224–8. doi: 10.4103/0972-0707.111319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coutinho M, Trevizam NC, Takayassu RN, Leme AA, Soares GP. Distance and protective barrier effects on the composite resin degree of conversion. Contemp Clin Dent. 2013;4:152–5. doi: 10.4103/0976-237X.114845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chang HS. Infection control of light curing units. J Korean Acad Cons Dent. 2010;35:235–7. [Google Scholar]
- 24.Pollington S, Kahakachchi N, van Noort R. The influence of plastic light cure sheaths on the hardness of resin composite. Oper Dent. 2009;34:741–5. doi: 10.2341/09-024-L. [DOI] [PubMed] [Google Scholar]
- 25.Sword RJ, Do UN, Chang JH, Rueggeberg FA. Effect of curing light barriers and light types on radiant exposure and composite conversion. J Esthet Restor Dent. 2016;28:29–42. doi: 10.1111/jerd.12173. [DOI] [PubMed] [Google Scholar]


