Abstract
Recent observation identifies subendothelial (mural) cells expressing MCAM, a specific system of clonogenic, self-renewing, osteoprogenitors (a.k.a, “mesenchymal stem cells”) in the microvascular compartment of post-natal human bone marrow (BM). In this study, we used MCAM/CD146, as a marker to localize, isolate and assay subendothelial clonogenic cells from the microvasculature of postnatal human skeletal muscle. We show here that these cells share with their BM counterpart, anatomic position (subendothelial/adventitial) and ex vivo clonogenicity (CFU-Fs). When assayed under the stringent conditions, these cells display a high spontaneous myogenic potential (independent of co-culture with myoblasts or of in vivo fusion with local myoblasts), which is otherwise only attained in cultures of satellite cells. These muscle-derived mural cells activated a myogenic program in culture. Cultured CD146+ cells expressed the myogenic factors (Pax7, Pax3 and Myf5), NCAM/CD56, desmin as well as proteins characteristic of more advanced myogenic differentiation, such as myosin heavy chain. In vivo, these cells spontaneously generate myotubes and myofibrils. These data identify the anatomy and phenotype of a novel class of committed myogenic progenitor in human post-natal skeletal muscle of subendothelial cells associated with the abluminal surface of microvascular compartment distinct from satellite cells.
Introduction
Normally a stable tissue that does not undergo significant steady state turnover, skeletal muscle has a limited capacity for repair and regeneration [1, 2]. Like its physiological postnatal growth, and its hypertrophy in response to exercise, muscle repair and regeneration are thought to reflect the biological activity of local progenitor cells [3]. Satellite cells, located beneath the basal lamina of myofibers, are the best characterized myogenic progenitors in postnatal muscle [4]. Once activated in response to injury or stimulated to growth, they resume mitotic activity and generate a pool of myoblasts able to fuse into newly formed myofibers [4, 5].
In spite of their unrivalled myogenic potential, however, satellite cells are unable to cross vascular wall, thus limiting their efficacy in in vivo transplantation [6–8]. In addition, satellite cells are not easy to isolate and expand in culture: only recently they have been isolated from the mouse [9, 10], but not from humans.
Recently, additional postnatal myogenic progenitors have been described to be able to either regenerate myofibers in vivo or myotubes in vitro (when co-cultured with myoblasts) [11–15]. In particular, within the postnatal muscle, a myogenic potential has been associated to a subset of Wnt-inducible CD45+ cells [16], to a class of interstitial multipotent cells (i.e., MDSCs, muscle derived stem cells [17, 18]) and to cells defined by their ability to exclude Hoechst 33342 (i.e., muscle side population, mSP [19, 20]). However, none of the non-canonical myogenic progenitors described to date in the mouse have been shown to display the inherent, spontaneous myogenic activity characteristic of satellite cells in vitro [10].
Outside of skeletal muscle, either bone marrow (BM) or hematopoietic stem cells have been shown to contribute to muscle regeneration following transplantation [21]. “Mesenchymal stem cells” found in the BM ─ also known as bone marrow stromal stem cells (BMSCs), or skeletal stem cells ─ are the best known, assayable progenitors of mesoderm derivatives in human postnatal tissues [22]. Capable of generating multiple skeletal tissues (bone, cartilage, fat, fibroblasts and the hematopoiesis supporting stroma) at the clonal level, BMSCs exhibit limited myogenic activity only when exposed to the chromatin remodeling effects of the demethylating agent, 5’-azacytidine [23], or when genetically modified [24]. We have recently shown that the self-renewing multipotent skeletal stem cells in the postnatal bone marrow are anatomically and phenotypically identified as a class of subendothelial cells associated with the abluminal surface of bone marrow sinusoids [25]. These cells can be prospectively isolated based on the expression of MCAM (the melanoma associated cell adhesion molecule), also known as CD146.
Here, we show that CD146-expressing subendothelial cells associated with the microvasculature of human post-natal muscle include clonogenic, myogenic progenitors (Muscle Colony Forming Unit Fibroblastic, M-CFU-Fs). Like BMSCs (but with a distinct differentiation potential), these cells are phenotypically and anatomically distinct from satellite cells, but share their inherent myogenic activity in vitro.
Materials and methods
Tissue samples
Normal muscle samples (surgical waste, 1–30x102 mg) from various muscle groups, including vastus lateralis, quadriceps femoris, triceps brachii, deltoids, gluteus maximus were obtained from 15 human adult patients (aged from 25 to 65 years) undergoing orthopedic surgery. A consent was orally requested to the human subjects, providing them an assurance to analyze the data anonymously. The human subjects provided us with an oral assurance of their willingness to participate in the research. The study on human tissues was approved by the Research Ethics Committee of Istituto Superiore di Sanità of Rome (approval date September 20, 2016; Prot. PRE-686/16). Tissues were washed in pH 7.3 Hank’s salt solution without Ca2+/Mg2+ (HBSS, Invitrogen Life Technologies Corp., Carlsbad, California) containing 30mM Hepes (Sigma, St. Louis, MO), 100U/ml penicillin, 100μg/ml streptomycin (Invitrogen) for 10 minutes at room temperature with gentle agitation. For explant cultures, tissues were manually minced into 1x1mm fragments, and the fragments were placed into 100mm culture dishes containing complete medium (α-MEM (Invitrogen) supplemented with 20% FBS (Invitrogen), 2mM L-glutamine, 100U/ml penicillin, 100μg/ml streptomycin). Explants were monitored once a day for outgrowth of adherent cells and fresh medium was added every third day. At sub-confluence, adherent cells were detached by trypsin and re-plated for further study. Tissue fragments were discarded.
Preparation of single cell suspensions and establishment of cell cultures
Tissues were washed as described above and then manually minced into 1x1mm fragments. To obtain single cell suspensions, tissue fragments were digested twice with 100U/ml Chlostridium histolyticum type II collagenase (Invitrogen) supplemented with 3mM CaCl2 in Ca2+/Mg2+-free PBS (Invitrogen) for 40 min at 37°C with gentle agitation. The samples were centrifuged at 1000 rpm for 5 min at 4°C, washed with Ca2+/Mg2+-free PBS, resuspended in PBS, passed through 18 gauge needles to break up cell aggregates, and filtered through a 70 μm pore-size cell strainer (Becton Dickinson, Bedford, MA) to obtain a single cell suspension. The total number of nucleated cells was counted using a haemocytometer. The resulting single-cell suspensions were used either for sorting of CD146+ cells or for establishing non-clonal or multi-clonal cultures directly. For non-clonal cultures, cells were seeded at a density of 1.6x103-1.6x106 cells/cm2 in complete medium (described above). For multi-clonal cultures (multi-Colony Forming Unit-Fibroblastic, multi-CFU-F cultures), single cell suspensions were seeded into 100mm dishes at a density of 1.6 cells/cm2, and formation of discrete colonies was scored after 14 days. Cells were cultured in 75 cm2 flasks or in 100mm dishes (Becton Dickinson) containing complete medium αMEM (Invitrogen) with 20% FBS (Invitrogen), 2mM L-glutamine, 100U/ml penicillin, 100μg/ml streptomycin) at 37° in a humidified atmosphere of 95% air, 5% CO2, and were fed twice weekly thereafter. Multi-clonal cultures were passaged on day 14.
Reagents
Antibodies for cell sorting and flow cytometry are listed in S1 Table. Antibodies for immunohistochemistry and immunocytochemistry are listed in S2 Table.
Cell sorting and flow cytometry
For fluorescence-activated cell sorting (FACS), the entire cell suspension obtained from collagenase digestion of tissue fragments (~5x106 cells/10x102 mg), was pelleted, resuspended and preincubated in PBS/1% BSA for 30 min on ice with regular mixing. After washing in PBS, cells were incubated for 30 minutes on ice with a phycoerythrin (PE)-conjugated anti-human CD146 monoclonal antibody for separation of cell subsets [25]. CD146+ cells were sorted using a FACSvantageSE flow cytometer (Becton Dickinson). ~5x104 (~1% of total nucleated cells) freshly vital CD146+ cells were harvested from the digestion of tissue fragments. For flow cytometry, the entire human freshly collagenase-released muscle cell suspensions before culture, were pre-incubated in PBS/1% BSA for 30 min, then for 30 min on ice with antibodies for analysis of cell subsets co-expressing CD146 along with N-CAM/CD56, a marker of satellite cells, Alkaline Phosphatase (ALP) and CD34 as a marker of endothelial cells (listed in S1 Table). Expression of markers was assessed by using a FACSCalibur flow cytometer and CellQuest software (Becton Dickinson Biosciences, San Diego, CA).
Colony forming efficiency assay
Colony Forming Efficiency (CFE) assays were performed with CD146+ and CD146- fractions obtained by cell sorting, and unfractionated total cells. CD146+ cells were seeded at 1.6–3.3 cells/cm2. Cells from the CD146- fraction and unsorted total cells were seeded at an equivalent or higher density (1.6–1.6x105 cells/cm2) and grown under identical conditions. After 14 days, CFE was determined as the mean number ± SD of Giemsa-stained colonies (>50 cells)/102−105 cells initially plated. Assays were done at least in triplicate.
Analysis of cell proliferation
Muscle clonal cell cultures were plated at a density of 1.6x10 cells per cm2 in complete medium containing αMEM (Invitrogen) with 20% FBS (Invitrogen), 2mM L-glutamine, 100U/ml penicillin, 100μg/ml streptomycin. At each passage, the number of cells was counted in triplicate in a haemocytometer.
In vitro myogenic differentiation assays
Spontaneous myogenic differentiation was assessed by plating cells onto MatrigelTM coated dishes, with DMEM/2% Horse Serum (HS), or on plastic with MEM/20% FBS at clonal density. After 7 days, cultures were fixed and labeled for immunofluorescence with a monoclonal antibody against striated myosin heavy chain (MyHC). Efficiency of myogenic differentiation was estimated as the % of DAPI+ nuclei found within myosin positive myotubes. Fluorescence images were obtained using Nikon Eclipse TE2000 Inverted Microscope (Nikon Inc., Melville, U.S.A.). For the statistical analysis see below.
In vivo transplantation assays
Heterotopic in vivo myogenesis: to assess myogenic potential 1x106 cells from multiclonal cultures of human M-CFU-F CD146+ sorted cell cultures and dermal fibroblast cultures, were suspended in 1 ml of MatrigelTM Growth factor-reduced (BD Biosciences Labware, San Diego, CA). Aliquots of ~0.7 ml were injected in the subcutaneous tissue of the back of SCID/beige mice (CB17.Cg-PrkdcscidLystbg-J/Crl, Charles River, Wilmington, Massachusetts).
For in vivo transplantation assays, all animal procedures were approved by the relevant institutional committees (DM n. 98/2011-A, Italian Minister of Health). Briefly, operations were performed under sterile conditions under anesthesia achieved by intramuscular injection of a mixture of Zoletil 20 (Virbac; 5 mL/g of body weight) together with Rompun (Bayer; 1 mL/Zoletil 20 bottles). The mouse back was disinfected with betadine and midlongitudinal skin incisions of about 1 cm in length were made on the dorsal surface of each mouse. Subcutaneous pockets were formed by blunt dissection. A single transplant was placed into each pocket with up to four transplants per animal. The incisions were closed with surgical staples. Mice were euthanized by cervical dislocation after 21 days and transplants were harvested and immediately fixed for histology. Human dermal fibroblasts were used as a negative control. Normal human dermal fibroblasts were purchased from PromoCell GmbH, Heidelberg, Germany. After isolation in primary culture, were cultured in Dulbecco’s modified Eagle’s medium (DMEM)-high glucose (Invitrogen), supplemented with 2 mM glutamine.
Orthotopic in vivo myogenesis, cardiotoxin (CTX) model: to assess myogenic potential, human muscle-derived CD146+ cell populations were injected intramuscular into the left tibialis anterior of 2-month-old female SCID/beige mice (CB17.Cg-PrkdcscidLystbg-J/Crl, Charles River, Wilmington, Massachusetts) injured 1 day earlier by an intramuscular injection of CTX (Latoxan, Valence, France; [26]). Human dermal fibroblasts were used as a negative control.
Immunohistochemistry and immunolocalization studies
Samples of human skeletal muscle, and heterotopic transplants were snap-frozen in OCT embedding medium in liquid nitrogen and cryostat sectioned serially, or alternatively fixed in 4% formaldehyde in phosphate buffer, and processed for routine paraffin embedding. Five-μm thick paraffin sections were used for histology staining (H&E), immunofluorescence and immunoperoxidase studies. All primary antibodies used for immunolocalization studies are listed in S2 Table and were used as per standard immunoperoxidase (DAB reaction) or immunofluorescence protocols. Secondary antibodies labeled with Alexa Fluor 594 and 488 were from Molecular Probes (Invitrogen, Carlsbad, CA). Nuclei were stained by DAPI or propidium iodide (Sigma). Fluorescence images-stacks were obtained using confocal microscopy laser scanning (Leica TCS SP5, Leica microsystems, Mannheim, Germany). Brightfield light microscopy images were obtained using Zeiss Axiophot microscope (Carl Zeiss, Germany).
Karyotype analysis
Muscle-derived CFU-Fs CD146+ cells were karyotyped at a late passage. Cells were processed with the Karyomax kit (Invitrogen, Paisley, UK) according to the manufacturer’s instructions.
Statistical analysis
Statistical analysis was performed by one-way ANOVA and subsequently by Bonferroni post-tests. Differences are considered statistically significant at p≤0.05.
Results
Adult skeletal muscle contains subendothelial CD146+ cells and Colony Forming Units-Fibroblastic (CFU-Fs)
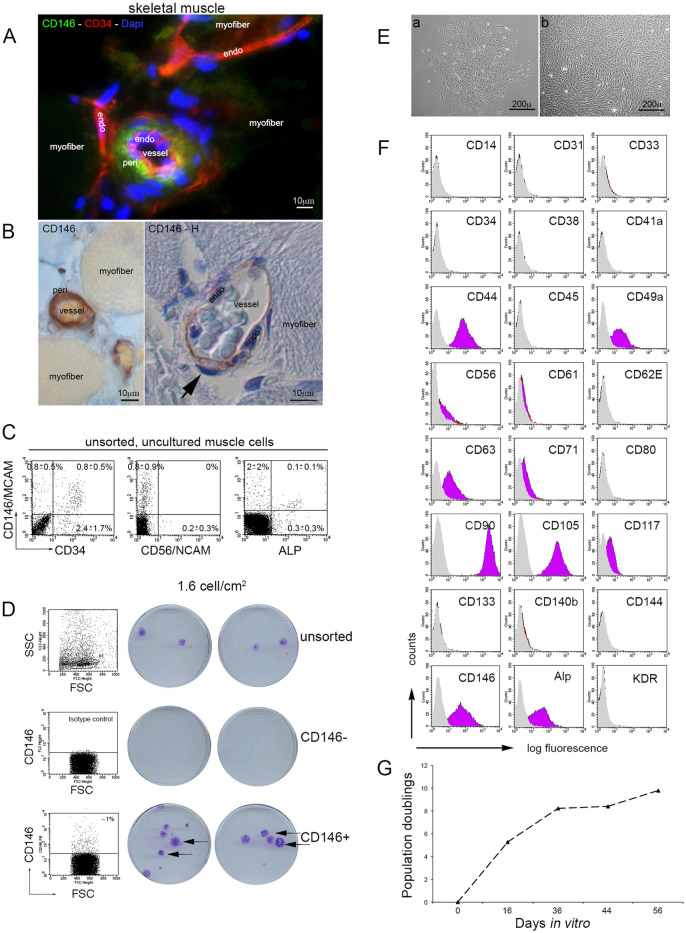
Immunohistochemical survey of human skeletal muscle revealed that CD146+ cells reside specifically in microvascular walls in a subendothelial position (Fig 1A and 1B), reminiscent of the subendothelial position of CFU-Fs in BM sinusoids [25]. Using FACS analysis of cellular suspension, as obtained by the digestion of muscle tissue, we analyzed the expression of CD34 as a marker of endothelial cells, NCAM (also known as CD56), a marker of satellite cells, and Alkaline Phosphatase (ALP), a pericyte and muscle “mesenchymal stem cells” marker [26], along with CD146. The Fig 1C shows that CD146 and CD56 were not co-expressed in the unsorted collagenase released muscle cells. In contrast, a proportion of CD146+ cells co-expressed Alkaline Phosphatase and CD34. Dual label FACS analysis of collagenase-released cell suspensions demonstrated that ~50% of the total CD146-expressing population co-expressed CD34 and ~25% of the total CD34-expressing population co-expressed CD146. These results identified three distinct subsets of cells expressing at least one of the two markers (CD146+/CD34-; CD146+/CD34+; CD146-/CD34+). When CD146+/CD34-, CD146+/CD34+, and CD146-/CD34+ were separately sorted and plated in culture at clonal density, CD146+/CD34- cells efficiently formed fibroblastic colonies, whereas CD146+/CD34+ cells formed rare, small colonies comprised of sparse cells. Cell morphology was clearly distinct in colonies of CD146+/CD34- cells vs CD146+/CD34+ cells. The latter could not be further passaged and expanded, consistent with the use of culture conditions (αMEM/20%FBS) that are not conducive for endothelial cell growth CD146-/CD34+ cells (data not shown). In muscle cells, FACS analysis revealed an overall frequency of ~1% CD146+ cells (Fig 1C and 1D). To determine if skeletal muscle would include clonogenic adherent cells (Muscle-CFU-Fs, M-CFU-Fs), similar to those found in the postnatal BM, we conducted CFE assays with single cell suspensions generated by digesting muscle fragments with collagenase. When unsorted collagenase released cells were plated directly onto plastic at clonal density, discrete colonies formed (Fig 1D), with an average frequency of 2±1.7 colonies/102 plated cells (n = 4).
Fig 1. Cells expressing CD146 in the vascular walls of human adult skeletal muscle.
Identification of M-CFU-Fs as subendothelial CD146+ cells. A) Immunolocalization of CD146 in human adult skeletal muscle. Immunoreactivity is restricted to microvascular walls. endo, endothelial cell nucleus. arrow, subendoethelial cell nucleus. Scale bar = 10 μm. B) Localization of CD146 and CD34 in muscle sections. Detail of a capillary, adjacent to a myofiber. Overview demonstrating that endothelial cells [(endo) in B] express CD34 but not CD146. Subendothelial pericytes [(peri) in B] express CD146. Scale bar = 10 μm. C) In muscle cells, expression of CD146, CD56, ALP and CD34 by FACS fluorescent. Expression of CD146 and CD56 is mutually exclusive in distinct cell subsets, with no co-expression. Co-expression of CD34 and ALP along with CD146, in human muscle cell suspensions before culture. CD146 is expressed in certain subsets of endothelial cells and ALP+ cells. D) Isotype control and FACS analysis of collagenase-generated cell suspensions of muscle, demonstrating an ~1% fraction of CD146-expressing cells. Freshly isolated muscle CD146+ cells were plated at clonal density (1.6 cells/cm2). At clonal density, muscle CD146+ but not muscle CD146- cells formed discrete fibroblastic colonies (arrows point to colonies, Giemsa stain). CFE assay of unsorted total cells, FACS-sorted CD146+ cells and CD146- cell subsets. All muscle CFU-Fs are found in the CD146-expressing subset of muscle cells. Representative cultures are shown. Discrete fibroblastic colonies formed by plating collagenase-released muscle cells at clonal density (1.6 cells/cm2). E) Cell morphology in single colonies generated by CD146+ muscle-derived clonogenic cells at 14 days (scale bars, 200 μm) in culture, in 20% serum, and on plastic. Developing colony photographed 9 days after plating (a). Fully developed colony photographed at day 14 after plating (b). Both demonstrating the characteristic whorled pattern and fibroblast-like cell morphology. F) FACS analysis of a multi-clonal strain obtained by combining multiple primary colonies. Note high expression of multiple markers of BM-derived CFU-Fs (and “mesenchymal stem cells”), CD44, CD90, CD105, CD49a, ALP, and high/bright expression of CD146. Endothelial (CD34, CD133) and hematopoietic markers (CD45) are negative. G) Proliferation curve of muscle-derived CD146+ multi-clonal cell strain. Fig 1A is excluded from this article’s CC BY license. See the accompanying retraction notice for more information.
Prospective isolation of muscle CFU-Fs by immunoselection for CD146
To determine if muscle-derived CFU-Fs would be comprised in a CD146-expressing subset of cells, sorted, collagenase-released cells were plated in culture at clonal density of 1.6 cells/cm2, harvested at 14 days (Fig 1D). Approximately 45% (44.4±3.6; mean±SD; n = 3) of sorted CD146+ cells were clonogenic when plated at clonal density directly on uncoated plastic. In contrast, no colonies formed when CD146- cells were plated on uncoated plastic at the same or higher (up to 4-log) density (n = 3), indicating that all CFU-Fs in muscle are comprised within the CD146+ subset (Fig 1D). Cells displayed a characteristic CFU-F whorled pattern (Fig 1E). The primary cultures, generated by seeding cells at clonal density (1.6 cells/cm2) were harvested at 14 days, and the cell strain analyzed by FACS. FACS analysis (Fig 1F) demonstrated that endothelial and hematopoietic markers (CD31, CD34, CD133, CD45) were not expressed in the multi-clonal cell strains obtained by combining multiple colonies. In contrast, multiple markers of “mesenchymal stem cells”, such as CD44 (hyaluronan receptor), CD90 (Thy-1), CD49a (α1 integrin subunit) and Alkaline Phosphatase (ALP) were expressed along with CD146. Note that a similar profile was observed in cell strains derived from explant cultures (Fig 2A), which only differed from CFU-F-derived multi-clonal strains by a comparatively low expression of CD146 (10–45% vs >90%). When grown in standard media, muscle CFU-Fs (CD146+) generated by seeding cells at clonal density, rapidly proliferate. Most cells maintained a triangular, refractile morphology and a high proliferation rate for approximately 10 population doublings (Fig 1G).
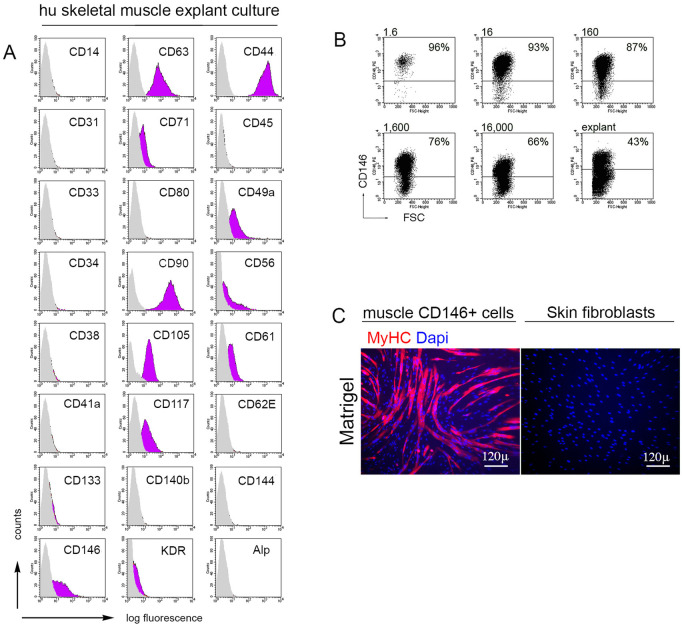
Fig 2. Human muscle cell strains generated by explants cultures.
A) In vitro FACS characterization of human muscle cell strains generated by explants cultures. B) The % of CD146+ cells in the cultures declined as a function of increasing plating density, reaching ~65% in in vitro characterization of human muscle a primary culture generated by seeding cells at a definitively non-clonal density (1.6x104 cells/cm2). The lowest % (~43%) was observed in cell strains generated by explants. A substantial proportion (34–57%) of cells in non-clonal cultures (plated at 1.6x104 cells/cm2 or explant cultures) fail to express CD146+. C) Conventional in vitro myogenic differentiation assays were assessed by plating muscle-derived CFU-Fs CD146+ cells onto MatrigelTM coated dishes, with DMEM/2% Horse Serum. After 7 days, extensive formation of myotubes expressing specific myogenic markers were observed. No myogenic differentiation was observed with non-muscle fibroblasts derived cell strain. MyHC, Myosin Heavy chain, Scale bar = 120 μm.
Muscle-derived mural cells activate spontaneously a myogenic program in culture
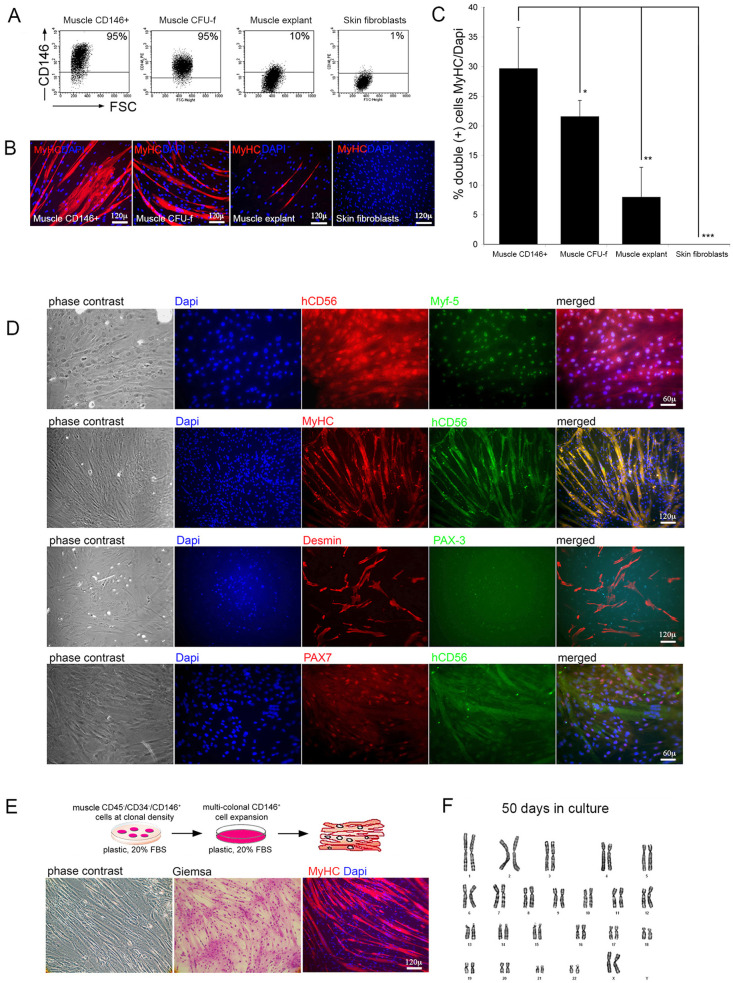
Unsorted, collagenase-released cells were plated in culture at clonal density of 1.6 cells/cm2, harvested at 14 days, and analyzed for CD146 expression by FACS. For comparison, the % of CD146+ cells was determined in cells obtained from CD146+ cells sorted and primary explant culture. This revealed that greater than 95% of the cells generated by M-CFU-Fs (i.e., from cells generating colonies when plated at a clonal density of 1.6 cells/cm2) expressed CD146 (Fig 3A). The % of CD146+ cells in the cultures declined as a function of increasing plating density, reaching ~65% in a primary culture generated by seeding cells at a definitively non-clonal density (1.6x104 cells/cm2). The lowest % (~10–43%) was observed in cell strains generated by explants (Fig 2B). Taken together, these data indicated that not only were all M-CFU-Fs comprised in the sorted CD146+ fraction, but that establishing a primary M-CFU-F culture at clonal density from unfractionated collagenase-released cells in fact selected for CD146-expressing cells, resulting in a cell strain in which >95% of the cells expressed CD146. In contrast, a substantial proportion (34–57%) of cells in non-clonal cultures (plated at 1.6x104 cells/cm2 or explant cultures) fail to express CD146 (Fig 2B). The in vitro myogenic capacity of (i) M-CFU-Fs, (ii) CD146+ cells sorted from muscle, and (iii) cultures derived from muscle explants was tested under stringent conditions (i.e., in the absence of exogenous myoblasts, independent of cell fusion with myoblasts in co-culture [10]). In M-CFU-F cultures and CD146+ sorted cells highly efficient myogenesis was observed spontaneously; i.e., by plating cells on plastic with MEM/20% FBS at clonal density with no recourse to canonical differentiation conditions (2% horse serum on MatrigelTM [26]). M-CFU-Fs and CD146+ cells sorted from muscle readily and efficiently generated myotubes in culture (20–40% nuclei incorporated into myofibers) (Fig 3B and 3C). This suggested that simple culturing in αMEM/20% serum was sufficient to induce myogenic differentiation in muscle-derived CD146+ cells. No myogenic activity was observed in cultures of human dermal fibroblasts-derived cultures (Fig 3B and 3C) or with CD146+ BM-derived cells (data not shown). Immunofluorescence analysis of myogenic differentiation revealed sparse myofibers in muscle explant cultures (<10% conversion; Fig 3B). In parallel experiments, the in vitro myogenic capacity of CD146+ cells sorted from muscle was tested using canonical differentiation conditions (Fig 2C). Cultures established from purified CD146+ cells progressively turned on the expression of CD56, PAX7, PAX3, Myf-5, Desmin (Fig 3D). Terminal differentiation into myotubes could be achieved by replating sub-confluent cultures at very high density with high serum (Fig 3E). Human skeletal muscle cells, generated by pooling colonies of M-CFU-Fs, after 10 population doublings, maintained an euploid number of chromosomes (Fig 3F). To examine tumorigenicity, 2x106 cells were transplanted subcutaneously into SCID/bg mice. Injected mice were maintained up to 2 months after the transplantation and none of them developed any visible tumor that could be detected macroscopically at autopsy (data not shown).
Fig 3. Muscle CFU-F-derived cells are spontaneously myogenic in culture.
A) Expression by FACS of CD146 and B-C) by fluorescent immunocytochemistry generation of myofibers in cultures of CD146-sorted muscle CFU-Fs, unsorted muscle CFU-Fs, muscle explant cultures and skin fibroblasts. Only rare myotubes are observed in cultures of muscle explant cultures. Data are expressed as percentage double positive cells MyHC/Dapi (***P < 0.001). Data are shown as mean ± standard deviation (SD). Scale bar = 120 μm. D) Sorted and cultured CD146+ human muscle-derived cells progressively turn on expression of myogenic markers PAX7, PAX3, Myf5, CD56, Desmin and MyHC, as verified by fluorescent immunocytochemistry. Scale bar = 120 μm, 60 μm. E) Terminal differentiation into myotubes could be achieved by replating CD146+ muscle-derived clonogenic cells at very high density with high serum. Multinucleated myotubes are obvious after Giemsa staining and expressing MyHC. F) Karyotype of human skeletal muscle cells generated by pooling colonies of M-CFU-Fs, after 10 population doublings, showed an euploid number of chromosomes. The Fig 3B skin fibroblasts panel is excluded from this article’s CC BY license. See the accompanying retraction notice for more information.
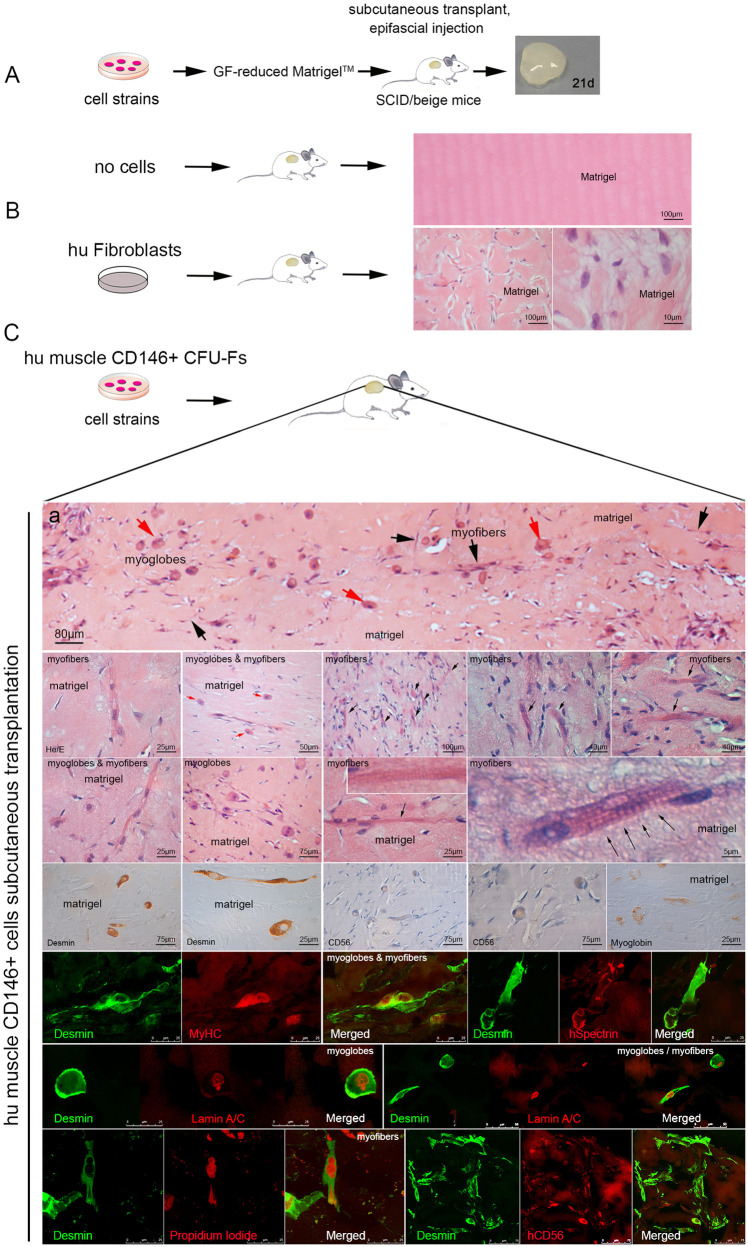
Muscle CFU-Fs are spontaneously myogenic in vivo
To assess myogenic potential of human muscle-derived CD146+ cell populations we used a stringent in vivo myogenesis assay (Fig 4A) which excludes fusion between donor cells and host myoblasts. To this end, we suspended equal numbers of cultured muscle-derived CD146+ cells in growth factor reduced MatrigelTM, and injected the resulting suspension into the epifascial space of the back of SCID/beige immunocompromised mice. The injected cells were harvested 3 weeks later for immunohistochemical studies (Fig 4A). No myogenic differentiation was observed with CD146+ BM-derived cells (data not shown) or human dermal-derived fibroblasts used as negative controls (Fig 4B). In contrast, in parallel experiments, plugs demonstrated that muscle CD146+ cells had efficiently generated clusters of myotubes, myofibers (Fig 4C) and a unique form of spheroidal syncytia expressing a differentiated muscle phenotype [desmin, MyHC, CD56, spectrin, dystrophin, myoglobin; (Fig 4C)] and syncytia myotubes [propidium iodide, human lamin A/C; (Fig 4C)] indicating that the in vivo myogenic capacity of human muscle CD146+ cells is independent of fusion with local myoblasts under these experimental conditions. The myosac phenotype may result from spontaneous contraction of the myotube poorly adhering to the substrate and obviously not constrained by tendons.
Fig 4. CD146+ mural cells are spontaneously myogenic in vivo.
To assess myogenic potential of human muscle-derived CD146+ cell populations we used a stringent in vivo myogenesis assay. A) In a heterotopic transplantation assay, CD146+ muscle cells were suspended in growth factor-reduced MatrigelTM and injected into the epifascial space of the back of SCID/beige mice, and harvested 3 weeks later. Plugs harvested demonstrated that: B) No myogenic differentiation was observed with human dermal-derived fibroblasts, while remaining viable in the plug; C) In vivo activation of a myogenic program in CD146+ muscle cells. Human CD146+ muscle cells revealed an extensive formation not only of myotubes expressing human-specific myogenic markers, desmin, MyHC, CD56 (counterstained with hematoxylin), spectrin, dystrophin, myoglobin, but even of striated myofibers (black arrows) and non-conventional muscle structures (syncytia myoglobes, red arrows), as demonstrated by H&E staning. Scale bar = 80 μm, 75 μm, 50 μm, 40 μm, 25 μm, 10 μm, 5 μm. The Fig 4B lower right-hand Matrigel panel and Fig 4C myoglobes & myofibers panels are excluded from this article’s CC BY license. See the accompanying retraction notice for more information.
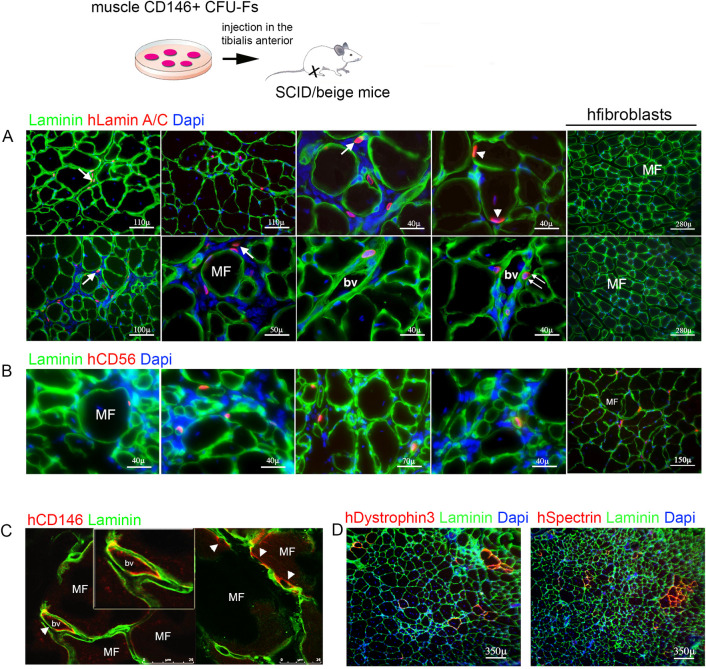
Muscle-derived CD146+ cells contribute to myofibers and satellite cells in vivo
Cultured muscle-derived CD146+ cells were injected intramuscular into CTX-injured tibialis anterior muscle of SCID/bg immunocompromised mice. The injected tibialis anterior muscle and the un-injected contralateral tibialis anterior muscle as control, were harvested 1 month later for immunofluorescence studies. Cells expressing human lamin A/C were easily identified in the transplanted muscle, where they resided mostly in the interstitium, or in walls of blood vessels, or in a position consistent with satellite cells (Fig 5A), revealing an efficient incorporation of donor nuclei. Cells in a satellite position also expressed the human satellite cell marker, hCD56 (Fig 5B). Clusters of myofibers expressing human-specific dystrophin and spectrin were generated (Fig 5C). Fibers expressing human specific dystrophin and spectrin (Fig 5D) demonstrated contribution of transplanted cells to regenerating fibers into injured muscle. In contrast, human dermal fibroblasts, used as negative control, failed to contribute to regenerating muscle (Fig 5).
Fig 5. In vivo generation of satellite cells, microvascular cells and contribution to regenerating myofibers in a model of muscle damage by transplanted CD146+ cells.
Muscle-derived CD146+ cells were injected intramuscular into cardiotoxin-injured muscle tibialis anterior of SCID/beige mice, injured 1 day earlier by an intramuscular injection of CTX. A) After 4 weeks transplanted human muscle-derived cells, identified by expression of human Lamin A/C (red), were distributed to the interstitium (arrow), but also to the surface of myofibers (MF; green) in a satellite cell-like position (arrowhead), and to walls of small blood vessels (bv, double arrows). Scale bar = 110 μm, 100 μm, 50 μm, 40 μm. B) Cells in a satellite cell-like position express human CD56 (red). Scale bar = 150 μm, 70 μm, 40 μm. C) Cells blood vessel walls (bv) express human CD146 (red, arrowhead). The inset shows immunoreactivity of CD146 was restricted to microvascular walls of the interstitial tissue. D) Clusters of myofibers expressing human dystrophin 3 and spectrin (red) were generated by muscle CD146+ cells by in vivo transplantation into SCID/beige/CTX-treated mice (DAPI: nuclear stain). Scale bar = 350 μm. Human dermal fibroblasts were used as negative control. Scale bar = 280 μm. The Fig 5D hSpectrin Laminin Dapi panel is excluded from this article’s CC-BY license. See the accompanying retraction notice for more information.
Discussion
Identification of myogenic progenitors in post-natal tissues is of paramount importance for the prospective potential of tackling severe muscle disorders such as muscular dystrophy through cell therapy [8]. To date, satellite cells [4] represent the only unequivocally characterized post-natal myogenic progenitor that may be endowed with sizable spontaneous myogenic activity [10, 14, 27]. Satellite cells are primarily defined by their location over the surface of myofibers, underneath their basal lamina [4] and expression of different non-unique markers such as Pax7, NCAM, M-cadherin, syndecans, which have been mostly characterized in mice. However, their use in future cell therapy protocols is limited because satellite cells (i.e., NCAM/CD56+ cells) are not easy to isolate, must be expanded on collagen-coated dishes, and lose their myogenic potency in vivo following expansion in culture. In addition, they are unable to cross the vessel wall [7].
Thus, the search for non-canonical myogenic progenitors finds an applicative horizon in the feeble regenerative potential of satellite cells once transplanted in vivo. Some of these non-canonical progenitors are derived from muscle itself, such as the mSP [19] or the MDSCs [17, 18, 28]. Others may represent the myogenic activity of non-muscle cells, including hematopoietic cells and their progenitors [21, 29, 30]. Of note, all these non-canonical myogenic progenitors were shown to induce the expression of donor markers in regenerating myofibers following in vivo transplantation, or to be incorporated into newly formed myofibers when co-cultured with myoblasts. Unfortunately, none of them was shown to be endowed with the spontaneous myogenic activity characteristically displayed by satellite cells [10, 14, 27] in in vitro differentiation assays that do not involve co-culture with myoblasts [31]. Results of in vivo transplantation, therefore, correlate with results of in vitro co-culture assays better than with the inherent myogenic property of test cells, as probed by in vitro myogenesis assays of purified populations in the absence of exogenous myoblasts. Muscle fibers are natural syncytia, arising from cell fusion. In vivo transplantation assays for muscle differentiation, particularly if conducted in the context of muscle damage in a recipient animal, may reflect the propensity of the test cell strain for cell fusion, rather than an inherent myogenic ability thereof. A number of different cell types can actually fuse with myoblasts [10], either in culture or in vivo, without implying an inherent myogenic capacity other than the one directly induced by cell fusion. We have observed that fully tumorigenic cell lines can efficiently incorporate into damaged and regenerating muscle of recipient mice, and contribute donor markers to newly formed myofibers, while not exhibiting any myogenic potential in vitro (data not shown). Paradoxically, and at variance with other systems in which in vivo assays are crucial for investigating properties of stem/progenitor cells, in vitro assays of myogenic differentiation may be more stringent than in vivo studies.
Here, we have shown that a population of cells that is anatomically and phenotypically distinct from satellite cells, but endowed with a comparable spontaneous myogenic activity in culture, can be isolated from the interstitium of adult human skeletal muscle by virtue of their expression of CD146. Satellite marker (NCAM/CD56) was not expressed in the unsorted collagenase released muscle cells, along with CD146. Expression of CD146 and CD56 is mutually exclusive in distinct cell subsets, with no co-expression. In contrast, a proportion of CD146+ cells co-expressed Alkaline Phosphatase, a pericyte/muscle “mesenchymal stem cells” marker [26] and CD34, a marker of endothelial cells. CD146 subset accounts for ~1% of collagenase-released mononuclear cells in human muscle, and includes a significantly high proportion (>40%) of cells able to establish discrete clonal colonies of fibroblast-like cells (CFU-Fs) on plastic. The progeny of muscle CFU-Fs undergoes myogenic conversion at a high rate (>30%) by plating cells on plastic with MEM/20% FBS with no recourse to canonical differentiation conditions (2% horse serum on MatrigelTM) and with no requirement for co-culture with myoblasts. Moreover, sorted and cultured CD146+ human muscle-derived cells, in the absence of any other cell type, were dramatically myogenic [13].
Their ability to form fibroblastic colonies, their phenotype noted for high expression of CD146, and their subendothelial position in vivo establish a remarkable kinship between muscle CFU-Fs cells and bone marrow CFU-Fs. The latter, however, are not spontaneously myogenic both in vitro and in vivo [32].
MCAM/CD146, a cell adhesion molecule of the immunoglobulin superfamily [33], is expressed in the myotome [34] as well as by human fetal muscle myoblasts, but is reported to be downregulated in postnatal human myoblasts [35]. Satellite cells, the only known myoblast-like cells in postnatal muscle, are identified by NCAM/CD56 immunoreactivity and located over the surface of myofibers, underneath their basal lamina [4]. CD146 immunoreactivity is restricted to cells of the microvascular walls. These include a subset of subendothelial pericytes. Myogenic cells derived from muscle CFU-Fs do not express CD34, and the culture conditions employed to grow them are not conducive for endothelial cell growth. Accordingly, the spontaneous myogenic activity of cells isolated as CD146+ revealed by our data can be ascribed solely to non-endothelial, vessel-associated progenitors that are capable of clonal growth on plastic and do not express CD34. Taken together with our localization results, our data identify subendothelial pericytes of human muscle as a specific population of myogenic progenitors, anatomically associated with vascular walls rather than with myofibers, and distinct from satellite cells both spatially and phenotypically. However, whether an inherent myogenic potential is also associated with CD146-expressing endothelial cells cannot be conclusively excluded by our data, as it may be concealed due to the culture conditions employed, which were not conducive for endothelial growth. Some somite derived myogenic progenitors do display a potential for endothelial differentiation. Evidence available for the existence of myogenic progenitors within the wall of the dorsal aorta in the AGM region [36] might also be related to an inherent myogenic potential of a subset of embryonic endothelial cells. Evidence exists that myogenic cells can be related to the endothelial cell lineage in human skeletal muscle [37]. These authors show that myogenic cells are contained in endothelial cell lineage CD56+/CD34+ from muscle [37]. An inherent myogenic potential of any post-natal endothelial cell subset remains, however, to be directly demonstrated.
The developmental origin of myogenic cells in the muscle microvasculature awaits direct demonstration. Conceivably, a subset of myoblasts may be recruited to a pericyte fate during development and growth, possibly via specific interactions with endothelial cells of nascent or growing blood vessels. Recruitment of mesenchymal cells to a pericyte fate during vasculogenesis and angiogenesis is regulated by a close interaction of endothelial cells with the surrounding cells, and is mediated by the concerted action of a narrow range of local factors including FGF-2, PDGF-BB and TGF-β [38, 39]. Whereas FGF-2 promotes the growth of presumptive pericytes, PDGF-BB mediates their recruitment to the vascular wall. TGF-β, activated at sites of contact between the endothelium and the presumptive pericytes, induces their mitotic quiescence and stabilizes the vessel. Through similar mechanisms, pre-natal myoblasts might remain associated with the muscle vasculature during development and growth as mitotically quiescent pericytes, and be prevented from entering or completing their myogenic differentiation. In this view, two anatomically and phenotypically distinct classes of assayable, myoblast-derived, myogenic progenitors—satellite cells and pericytes—would be retained within different ‘niches’ in the post-natal muscle through a spatial selection mechanism. This would imply their interaction with myofibers or vessel walls, respectively, and a distinct repertoire of adhesion molecules mediating the respective interaction. The mutually exclusive expression of NCAM and MCAM in satellite cells and myogenic pericytes, respectively, might reflect or mediate such events. The reported expression of MCAM in myotome cells [34] and embryonic myoblasts [35], would be consistent with an origin of myogenic cells in the vascular wall from embryonic myoblasts, and thus ultimately from somites. However, it should be noted that MCAM marks pericytes or subendothelial cells in a number of other tissues, including the bone marrow, periosteum and dermis. Likewise, MCAM expression per se does not reflect an inherent myogenic potential and does not provide a marker of myogenic cells across different mesodermal tissues [32]. Unlike their muscle cognates, MCAM-expressing CFU-Fs from the bone marrow are not spontaneously myogenic, while capable of forming skeletal tissues in vivo. Conversely, the lack of an in vivo skeletogenic potential of muscle CFU-Fs [32] indicates that MCAM is neither a marker of functionally homogeneous “mesenchymal stem cells” across different tissues. Rather, MCAM is similarly expressed in functionally heterogeneous progenitors found in different tissues, and at least in BM stromal cells appears to be functionally involved in the interaction of subendothelial cells with endothelial cells. The location of such progenitors in the subendothelial microvascular compartment in different tissues, and their phenotypic similarity, however, do provide a unifying thread. Common developmental mechanisms may underlie the origin of assayable clonogenic progenitors (endowed with tissue-specific potential) located in the microvascular district of different adult mesodermal tissues.
Supporting information
(PDF)
(PDF)
Acknowledgments
BS is grateful to Prof. Paolo Bianco † (Sapienza University, Rome) for his expertise and invaluable support. Furthermore, we wish to thank dr. Mauro Valtieri for his contribution.
Abbreviations
- ALP
alkaline phosphatase
- BM
bone marrow
- BMSCs
bone marrow stromal stem cells
- NCAM/CD56
satellite cells marker
- CFE
colony forming efficiency
- MCAM/CD146
subendothelial clonogenic cells marker
- M-CFU-Fs
muscle colony forming unit fibroblastic
- MDSCs
muscle derived stem cells
- mSP
muscle side population
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Charge SBP, Rudnicki MA. Cellular and molecular regulation of muscle regeneration. Physiological Reviews. 2004;84(1):209–238. doi: 10.1152/physrev.00019.2003 [DOI] [PubMed] [Google Scholar]
- 2.Wagers AJ, Conboy IM. Cellular and molecular signatures of muscle regeneration: Current concepts and controversies in adult myogenesis. Cell. 2005;122(5):659–667. doi: 10.1016/j.cell.2005.08.021 [DOI] [PubMed] [Google Scholar]
- 3.Tajbakhsh S. Skeletal muscle stem and progenitor cells: Reconciling genetics and lineage. Experimental Cell Research. 2005;306(2):364–372. doi: 10.1016/j.yexcr.2005.03.033 [DOI] [PubMed] [Google Scholar]
- 4.Morgan JE, Partridge TA. Muscle satellite cells. International Journal of Biochemistry & Cell Biology. 2003;35(8):1151–1156. [DOI] [PubMed] [Google Scholar]
- 5.Dhawan J, Rando TA. Stem cells in postnatal myogenesis: molecular mechanisms of satellite cell quiescence, activation and replenishment. Trends in Cell Biology. 2005;15(12):666–673. doi: 10.1016/j.tcb.2005.10.007 [DOI] [PubMed] [Google Scholar]
- 6.Boldrin L, Morgan JE. Activating muscle stem cells: therapeutic potential in muscle diseases. Current Opinion in Neurology. 2007;20(5):577–582. doi: 10.1097/WCO.0b013e3282ef5919 [DOI] [PubMed] [Google Scholar]
- 7.Cossu G, Sampaolesi M. New therapies for Duchenne muscular dystrophy: challenges, prospects and clinical trials. Trends in Molecular Medicine. 2007;13(12):520–526. doi: 10.1016/j.molmed.2007.10.003 [DOI] [PubMed] [Google Scholar]
- 8.Partridge TA. Stem cell route to neuromuscular therapies. Muscle & Nerve. 2003;27(2):133–141. [DOI] [PubMed] [Google Scholar]
- 9.Buckingham M. Myogenic progenitor cells and skeletal myogenesis in vertebrates. Current Opinion in Genetics & Development. 2006;16(5):525–532. [DOI] [PubMed] [Google Scholar]
- 10.Sherwood RI, Christensen JL, Conboy IM, Conboy MJ, Rando TA, Weissman IL, et al. Isolation of adult mouse myogenic progenitors: Functional heterogeneity of cells within and engrafting skeletal muscle. Cell. 2004;119(4):543–554. doi: 10.1016/j.cell.2004.10.021 [DOI] [PubMed] [Google Scholar]
- 11.Chen WC, Baily JE, Corselli M, Diaz ME, Sun B, Xiang G, et al. Human myocardial pericytes: multipotent mesodermal precursors exhibiting cardiac specificity. Stem Cells. 2015;33(2):557–573. doi: 10.1002/stem.1868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chen WC, Saparov A, Corselli M, Crisan M, Zheng B, Peault B, et al. Isolation of blood-vessel-derived multipotent precursors from human skeletal muscle. J Vis Exp. 2014;(90):e51195. doi: 10.3791/51195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Crisan M, Yap S, Casteilla L, Chen CW, Corselli M, Park TS, et al. A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell. 2008;3(3):301–313. doi: 10.1016/j.stem.2008.07.003 [DOI] [PubMed] [Google Scholar]
- 14.Montarras D, Morgan J, Collins C, Relaix F, Zaffran S, Cumano A, et al. Direct isolation of satellite cells for skeletal muscle regeneration. Science. 2005;309(5743):2064–2067. doi: 10.1126/science.1114758 [DOI] [PubMed] [Google Scholar]
- 15.Peault B, Rudnicki M, Torrente Y, Cossu G, Tremblay JP, Partridge T, et al. Stem and progenitor cells in skeletal muscle development, maintenance, and therapy. Molecular Therapy. 2007;15(5):867–877. doi: 10.1038/mt.sj.6300145 [DOI] [PubMed] [Google Scholar]
- 16.Polesskaya A, Seale P, Rudnicki MA. Wnt signaling induces the myogenic specification of resident CD45(+) adult stem cells during muscle regeneration. Cell. 2003;113(7):841–852. [DOI] [PubMed] [Google Scholar]
- 17.Lee JY, Qu-Petersen Z, Cao BH, Kimura S, Jankowski R, Cummins J, et al. Clonal isolation of muscle-derived cells capable of enhancing muscle regeneration and bone healing. Journal of Cell Biology. 2000;150(5):1085–1099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Qu-Petersen ZQ, Deasy B, Jankowski R, Ikezawa M, Cummins J, Pruchnic R, et al. Identification of a novel population of muscle stem cells in mice: potential for muscle regeneration. Journal of Cell Biology. 2002;157(5):851–864. doi: 10.1083/jcb.200108150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Asakura A, Seale P, Girgis-Gabardo A, Rudnicki MA. Myogenic specification of side population cells in skeletal muscle. Journal of Cell Biology. 2002;159(1):123–134. doi: 10.1083/jcb.200202092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McKinnell IW, Parise G, Rudnicki MA. Muscle stem cells and regenerative myogenesis. Current Topics in Developmental Biology, Vol 71. 2005;71:113–+. doi: 10.1016/S0070-2153(05)71004-8 [DOI] [PubMed] [Google Scholar]
- 21.Ferrari G, Cusella-De Angelis G, Coletta M, Paolucci E, Stornaiuolo A, Cossu G, et al. Muscle regeneration by bone marrow derived myogenic progenitors. Science. 1998;279(5356):1528–1530. [DOI] [PubMed] [Google Scholar]
- 22.Bianco P, Robey PG, Simmons PJ. Mesenchymal stem cells: Revisiting history, concepts, and assays. Cell Stem Cell. 2008;2(4):313–319. doi: 10.1016/j.stem.2008.03.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wakitani S, Saito T, Caplan AI. Myogenic Cells Derived from Rat Bone-Marrow Mesenchymal Stem-Cells Exposed to 5-Azacytidine. Muscle & Nerve. 1995;18(12):1417–1426. [DOI] [PubMed] [Google Scholar]
- 24.Dezawa M, Ishikawa H, Itokazu Y, Yoshihara T, Hoshino M, Takeda S, et al. Bone marrow stromal cells generate muscle cells and repair muscle degeneration. Science. 2005;309(5732):314–317. doi: 10.1126/science.1110364 [DOI] [PubMed] [Google Scholar]
- 25.Sacchetti B, Funari A, Michienzi S, Di Cesare S, Piersanti S, Saggio I, et al. Self-renewing osteoprogenitors in bone marrow sinusoids can organize a hematopoietic microenvironment. Cell. 2007;131(2):324–336. doi: 10.1016/j.cell.2007.08.025 [DOI] [PubMed] [Google Scholar]
- 26.Dellavalle A, Sampaolesi M, Tonlorenzi R, Tagliafico E, Sacchetti B, Perani L, et al. Pericytes of human skeletal muscle are myogenic precursors distinct from satellite cells. Nature Cell Biology. 2007;9(3):255–U230. doi: 10.1038/ncb1542 [DOI] [PubMed] [Google Scholar]
- 27.Collins CA, Olsen I, Zammit PS, Heslop L, Petrie A, Partridge TA, et al. Stem cell function, self-renewal, and behavioral heterogeneity of cells from the adult muscle satellite cell niche. Cell. 2005;122(2):289–301. doi: 10.1016/j.cell.2005.05.010 [DOI] [PubMed] [Google Scholar]
- 28.Huard J. Identification and characterization of muscle derived stem cells: Potential for skeletal and cardiac muscle repair. Faseb Journal. 2003;17(5):A1374–A1374. [Google Scholar]
- 29.Camargo FD, Green R, Capetenaki Y, Jackson KA, Goodell MA. Single hematopoietic stem cells generate skeletal muscle through myeloid intermediates. Nature Medicine. 2003;9(12):1520–1527. doi: 10.1038/nm963 [DOI] [PubMed] [Google Scholar]
- 30.Gussoni E, Soneoka Y, Strickland CD, Buzney EA, Khan MK, Flint AF, et al. Dystrophin expression in the mdx mouse restored by stem cell transplantation. Nature. 1999;401(6751):390–394. doi: 10.1038/43919 [DOI] [PubMed] [Google Scholar]
- 31.Rando TA, Blau HM. Primary Mouse Myoblast Purification, Characterization, and Transplantation for Cell-Mediated Gene-Therapy. Journal of Cell Biology. 1994;125(6):1275–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sacchetti B, Funari A, Remoli C, Giannicola G, Kogler G, Liedtke S, et al. No Identical “Mesenchymal Stem Cells” at Different Times and Sites: Human Committed Progenitors of Distinct Origin and Differentiation Potential Are Incorporated as Adventitial Cells in Microvessels. Stem Cell Reports. 2016;6(6):897–913. doi: 10.1016/j.stemcr.2016.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shi IM. The role of CD146 (Mel-CAM) in biology and pathology. Journal of Pathology. 1999;189(1):4–11. doi: [DOI] [PubMed] [Google Scholar]
- 34.Pujades C, Guez-Guez B, Dunon D. Melanoma Cell Adhesion Molecule (MCAM) expression in the myogenic lineage during early chick embryonic development. International Journal of Developmental Biology. 2002;46(2):263–266. doi: 10.1387/ijdb.011493 [DOI] [PubMed] [Google Scholar]
- 35.Cerletti M, Molloy MJ, Tomczak KK, Yoon S, Ramoni MF, Kho AT, et al. Melanoma cell adhesion molecule is a novel marker for human fetal myogenic cells and affects myoblast fusion. Journal of Cell Science. 2006;119(15):3117–3127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Minasi MG, Riminucci M, De Angelis L, Borello U, Berarducci B, Innocenzi A, et al. The meso-angioblast: a multipotent, self-renewing cell that originates from the dorsal aorta and differentiates into most mesodermal tissues. Development. 2002;129(11):2773–2784. [DOI] [PubMed] [Google Scholar]
- 37.Zheng B, Cao B, Crisan M, Sun B, Li G, Logar A, et al. Prospective identification of myogenic endothelial cells in human skeletal muscle. Nat Biotechnol. 2007;25(9):1025–1034. doi: 10.1038/nbt1334 [DOI] [PubMed] [Google Scholar]
- 38.Hirschi KK, DAmore PA. Pericytes in the microvasculature. Cardiovascular Research. 1996;32(4):687–698. [PubMed] [Google Scholar]
- 39.Jain RK. Molecular regulation of vessel maturation. Nature Medicine. 2003;9(6):685–693. doi: 10.1038/nm0603-685 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.