Abstract
Introduction:
Hyperglycemia is a common occurrence in critically ill patients, and its prevalence in patients receiving nutritional support is much higher than in other patients. The non-diabetic form is associated with more undesirable outcomes. This study was performed to determine the prevalence of non-diabetic hyperglycemia and its correlates in patients receiving enteral nutrition.
Material and Methods:
This cross-sectional study was performed between March and December 2015. Seven hundred forty eight (748) patients were reviewed to see if they met the inclusion criteria. After random sequence numbering, 414 patients who were eligible for further assessment and data gathering were selected. Hyperglycemia was defined as the blood glucose levels higher than either 126 mg/dL, in the fasting state, or 180 mg/dL, in a random state. Blood glucose was measured by an ACCU-CHECK glucometer (Roche diagnostics, Mannheim, Germany) three times, after ICU admission, in both fasting and random state. A pre-prepared form was used to extract data from hospital records. Data analysis was performed by SPSS 21 software.
Results:
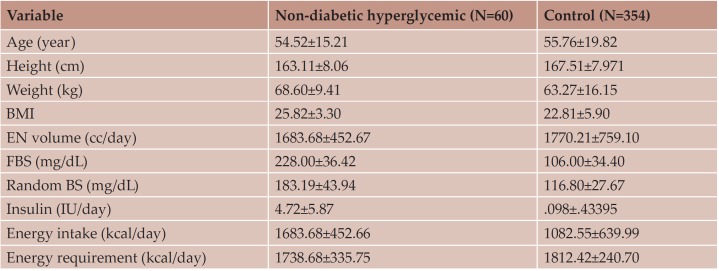
In this group of hospitalized patients, the prevalence of non-diabetic hyperglycemia was 14/49 (60/414). In the hyperglycemic subgroup, mean FBS was 228.00±36.42, mean random BS was 183.19±43.94 and mean blood sugar on the first day of hospitalization was 203.60 ± 60.79. The mean age of patients was 56.64±19.79 years and the mean duration of hospitalization was 19.24±15.33 days. There was no significant relationship between enteral nutrition feeding volume and hyperglycemia. Majorly, patients aged above 60 years were hyperglycemic. The prevalence was higher in men than in women. Most patients were internal cases, but with the highest prevalence of hyperglycemia in surgical patients.
Conclusions:
Since among different studied variables just diagnosed disease and the level of provided calorie showed significant differences between subgroup categories, so it can be suggested that designing on-time appropriate management programs based them can be effective on the administration of non-diabetic hyperglycemia and its undesirable consequences in such patients.
Keywords:Non-diabetic hyperglycemia, correlates, enteral nutrition, ICU patients
INTRODUCTION
Hyperglycemia is a common occurrence in critically ill patients, even in those without any history of diabetes mellitus. During stress, injury or trauma, glucose metabolism will be altered because of changes in endocrine secretions and peripheral insulin resistance, resulting in hyperglycemia (1-3). The prevalence of hyperglycemia in patients receiving nutritional support is much higher than in other patients (4, 5). Elevation of blood glucose can occur by increased hepatic glucose production and its decreased consumption in peripheral tissues. Such changes will appear during hospital stresses, including acute illness states, surgery, and trauma (6). This can provide a state for a change in the metabolism of carbohydrates. This hyperglycemia can be considered a regular and normal physiologic response during stress or trauma, but in non-diabetic patients admitted to Intensive Care Unit (ICU) it has been recognized to be associated with worsening outcomes such as increasing mortality and morbidity (7). Studies have suggested that a range of 70-200 mg/dL was safe for increasing in life survival (1, 8). In general agreement, acute hyperglycemia in ICU has been defined as a fasting blood sugar (BS) higher than 126 mg/dL or a random blood sugar higher than 200 mg/dL (9).
It has been proposed by AACE/ADA that blood glucose in patients with acute critical situation should be maintained in a 140-180 mg/dL range (10). According to a systematic review published by ASPEN, controlling blood glucose levels in the range of 180–200 mg/dL has been reported as the more safe range for critically ill patients (11). Previous studies have reported that hyperglycemia could be observed in 32-38% of patients (with or without diabetes mellitus) (12), with an occurrence of about 30% in patients with enteral nutrition (EN) (13), while its non-diabetic form was found in about 12% of patients (7). Other previous studies (2, 14, 15) have indicated an ICU prevalence of hyperglycemia in 15-17% of patients with enteral feeding. Reporting the different figures among studies may be in relation to the timing of initiating nutrition, route of nutrition administration, caloric provision, glycemic target, and methods of blood glucose testing (11). In previous studies, various factors such as type of enteral nutrition, formula content, time of starting enteral nutrition (16), enteral nutrition prescription rate and volume (2), type of diagnosis, duration of hospitalization have been reported as factors that could affect the blood glucose level (3, 11, 17). This study was conducted to evaluate the prevalence of hyperglycemia and some previously addressed or anticipated correlates in patients receiving enteral nutrition in ICU.
MATERIALS AND METHODS
This cross-sectional study was performed between March and December 2015 in patients who received enteral feeding. Subjects were recruited from six different ICUs including GICU‘.NICU ‘.SICU ‘.MICU ‘.Stroke and post surge ry ICU. From 748 patients who were reviewed to see if they met the inclusion criteria, 414 were eligible for further assessment and data gathering, and after random sequence numbering, 60 of these were found to have hyperglycemia based on consequently mentioned criteria. Patients whose levels of either fasting blood sugar were higher than 126 mg/dL or random blood sugar were higher than 180 mg/dL were considered to be hyperglycemic. Patients aged 18 years and older were selected. Inclusion criteria were as follows: stay in ICU for at least 72-96 hours, having any type of enteral feeding (NGT, OGT, PEG/PEJ or their combinations), lack of receiving hyperglycemic agents, GCS = 3, absence of liver and pancreatic disorders, or kidney failure, or nephritic syndrome.
A pre-prepared form was used for extracting data from hospital records. Data related to demographic characteristics, baseline blood glucose level (admission time), fasting blood glucose, random blood glucose, length of ICU stay, type of enteral formulas, volume and route of feeding was gathered. Blood glucose was measured by an ACCU-CHECK glucometer (Roche diagnostics, Mannheim, Germany) and recorded in specific forms in the patient¡¦s medical records. The first blood sugar sample that was taken after ICU entrance was considered as admission time BS. Measured blood sugar at the NPO status or eight hours after the latest dietary intake was considered as fasting blood sugar. For each patient, blood glucose data was recorded at 17 to 18 p.m. daily and it was considered as random blood sugar. Mean blood sugar were calculated from different figures recorded for different days during hospitalization. Data analysis was performed by SPSS 21 software. Before data analysis, each dataset was assessed for normality with Kolmogorov-Smirnov test. Independent sample t-test was used for comparing means between two groups based on normal and quantitative variables. Mann-Whitney test was used for comparing two independent groups based on qualitative variables. The χ² test was used for analysis of differences based on sets of categorical variables. ANOVA and Kruskal-Wallis tests were used for comparing data between three different subgroups based on the type of variables (for quantitative and qualitative variables, respectively).
RESULTS
Two hundred and twenty-six (54.6%) patients were men and 188 (45.4%) women. Mean patients age was 56.64±19.79 and the mean duration of hospitalization 19.24±15.33 days. Of all patients, 14.49% (60/414) presented non-dia betic hyperglycemia; in these hyperglycemic patients, mean FBS was 228.00±36.42, mean random BS 183.19±43.94 and mean blood sugar on the first day of hospitalization was 203.60±60.79.
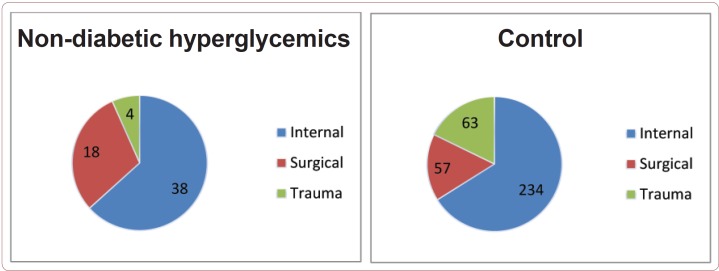
Based on diagnosed disease among the hyperglycemic subgroup, patients distribution was as below: 38 (63.3%) were the internal cases, 18 (30%) surgical cases, and 4 (6.7%) trauma patients. Results for reporting hyperglycemia prevalence based on age showed a higher prevalence (57.14 %) in patients aged above 60 years. Prevalence was higher in males than in females.
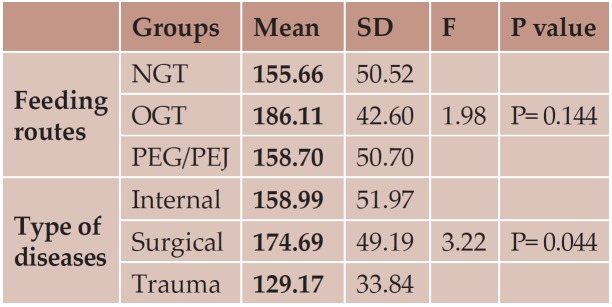
For detecting the association between the prevalence of hyperglycemia and some factors, a comparison between hyperglycemic and nonhyper glycemic groups was done. There were no significant differences between groups with respect to the average volume of received enteral feeding (p=0.20). Results from the correlation analysis with Pearson correlation test showed no significant association between mean random blood sugar and volume of received enteral feeding (p=0.99). Forty nine (81.6%) patients received nasogastric tube (NGT) feeding, 6 (10%) OGT and 5 (8.3%) PEG/PEG. Although the distribution among the three groups based on the route of feeding was unbalanced, one-way ANOVA analysis showed that there was no significant difference in the mean blood glucose level between three groups based on the feeding route. There was just a significant difference between the groups of patients with three different types of diagnosed diseases, with higher prevalence among surgical patients.
Among hyperglycemic patients included in different feeding route categories, the Kruskal-Wallis test showed a significant difference between groups (P<0.001). Results based on hyperglycemia distribution between the two genders showed that 57.15% of the hyperglycemic patients were men and 42.85% women, but the ƒÓ2 test showed no significant difference between sex groups. In 72.7% of hyperglycemic patients, more than 75% of their personal energy requirements was satisfied. Data analysis based on Mann-Whitney test showed a significant hyperglycemia prevalence between two groups (energy requirement satisfaction <74.99% and .75%, respectively) (P<0.001).
DISCUSSION
Hyperglycemia is a common occurrence in critically ill patients even without any history of diabetes mellitus. It has been proposed that its prevalence in patients receiving nutritional support is much higher than in other patients. In this study that was performed on a sample of patients with an average age of 56.64±19.79 years who received enteral nutrition, the prevalence of non-diabetic hyperglycemia was about 14.5%. Results from a current study with respect to the percent of patients with a new prevalence of hyperglycemia are comparable to those reported by Umpierrez et al. (7), who showed that 62% of their study population was normoglycemic, 26% had previously diagnosed diabetes and 12% newly identified hyperglycemia; the authors reported that their patients with new hyperglycemia have a higher in-hospital mortality (16%) compared to others with a known history of diabetes and normoglycemia (3%). In contrast, in our study, the prevalence was higher in men than in women. In the study of Whitcomb et al. (13), the occurrence of hyperglycemia was higher in females than males, and the percent of hyperglycemic females was 29.9% in comparison with males (25.4% of the total studied population). In our study, the percent of hyperglycemic women was 8.27% of the total studied population and that of hyperglycemic men 6.2%. The main difference between our study and Whitcomb et al.’s study was that the latter included all types of hyperglycemic patients (diabetic and non-diabetics), while we included only non-diabetic hyperglycemia patients. In Whitcomb et al.’s stu dy, hyperglycemia has been defined as casual (not-fasting) blood glucose of 200 mg/dL on the admission date to ICU. Just one study performed on non-diabetic hyperglycemia in SAH patients (14) reported that the percent of affected men was 29%, with no reported percent of distribution between the two genders, and the authors considered that patients were hyperglycemic when their blood glucose level was 5.8 mmol/L (105 mg/dL), while in our study we considered hyperglycemia for blood glucose levels higher than 180 mg/dL. As previously mentioned in the introduction section, it has been commonly a - gre ed that it was safer to control blood glucose levels in the range of 180–200 mg/dL.
Most patients received their enteral formula through NGT, similarly to other studies that stated that the NGT route was more frequently used. In our study, most cases were internal cases with highest hyperglycemia prevalence in surgical patients. There are several studies whose authors – Krinsley (15), Umpierrez, et al. (7), Campbell and McDowell (2) – also report a similar diagnosis distribution.
In this study, we found an average blood glucose level on admission of 203.60 ± 60.79 mg/dL, which was higher than in previous studies (18, 19), while the values reported by other authors were 170 mg/dL [Rajabian et al. (10)], 137± 53 mg/dL [Mousavi et al. (12)], and 139±43.7 mg/dL [Frier et al. (16)]. The mean random blood sugar in our sample population was 183.19±43.94 mg/dL, but only 142±57.4 mg/dL in the study of Mousavi et al. (12), and 176.2±11.3 mg/dL in Frier’s study (16).
One of the major differences between this study and others is that ours was designed specifically for the detection hyperglycemia prevalence, while others have reported hyperglycemia in the context of other results. Frier (16) and Krinsley (15) reported a hyperglycemia prevalence of 12%. In this study, we considered a usually mixed sample of patients, in contrast with others that reported hyperglycemia values in specifical subgroups of patients (10, 12). For e xample, other previous studies (14, 20, 21) indicated an ICU prevalence hyperglycemia of 15-17% in patients with enteral feeding. This figure has been reported for traumatic patients. In our study, we have calculated the mean random BS from different BS measured at different times during the study. In the current study, the prevalence of hyperglycemia was higher in men than in women, but none of other previous studies have reported such results. In this study, the mean age of the sample population was approximately similar with that of other study populations. The duration of our study (10 months) was longer than that of other studies, that reported a shorter period of time (10, 12).
Our results with respect to the feeding route were in agreement with others (2), that reported higher hyperglycemia in patients with nasogastric tube feeding. In the current study, most of the patients received their provided formula via a nasogastric tube. Since our findings are in line with those of similar previous studies and, typically, in ICU there are more patients with NGT feeding during hospitalization, further good quality and well-controlled randomized trials will be needed to detect the real causal relationship between non-diabetic hyperglycemia and type of EN feeding routes.
Regarding the level of provided calorie and its relation with hyperglycemia, some previous studies indicated that calorie-restricted diets can improve the hyperglycemic status (19, 22). As we see in the current study, the higher level of hyperglycemia was observed in the group with the higher level of energy intake. On another hand, we can see that, in some studies, also in patients with minimum or even no intake, hyperglycemia can be arisen as a result of induced gluconeogenesis and increased level of liver glucose production. It seems that providing a diet with a moderate level of calorie and appropriate with patient’s requirements based on currently provided guidelines may have a remedial effect.
Finally, results from this study recommended that the prevalence of hyperglycemia in our intensive care units could be situated in the range of 14-15%. It can be different in various patient groups without a previously diagnosed diabetes history. The prevalence of hyperglycemia was not associated with the feeding volume. The frequency of hyperglycemia episodes in these patients was different according to patients’ diagnosed disease groups. Also, in this study group of ICU hospitalized patients, the level of calorie intake and type of enteral feeding was related to non-diabetic hyperglycemia, so it might be suggested that designing on-time appropriate ma - na gement programs could be effective on the administration of non-diabetic hyperglycemia and its undesirable consequences in such patients.
CONCLUSION
Our results demonstrate that the M694V mutation is the most common risk factor for FMF in the studied population.
Acknowledgments: The authors would like to thank all the nurses, staff and residents of Urmia Imam Khomeini Hospital in different ICU settings for their participation in this study.
Conflicts of interest: none declared.
Financial support: none declared.
TABLE 1.
Baseline and demographic characteristics of the study population
FIGURE 1.
Patients distribution based on diagnosed disease categories in two groups
TABLE 2.
Results from one-way ANOVA between three feeding route groups and disease types based on blood sugar levels
Contributor Information
Mohammad Amin VALIZADEH HASANLOEI, Associated professor of Anesthesiology, fellowship of intensive care medicine, Urmia University of Medical Sciences, Urmia, Iran.
Zahra VAHDAT SHARIATPANAHI, Associated professor of Nutrition, Dept of Clinical Nutrition, Faculty of Nutrition and Food Technology, Shahid Beheshti University of Medical Science, Tehran, Iran.
Davoud VAHABZADEH, PhD Student in Nutrition, International Branch of Shahid Beheshti University of Medical Sciences, Tehran, Iran.
Zakaria VAHABZADEH, Liver & Digestive Research Center, Kurdistan University of Medical Sciences, Sanandaj, Iran.
Leila NASIRI, General practitioner in clinic, Emam Khomeini Hospital, Urmia University of Medical Sciences, Iran.
Ali SHARGH, Evaluation and accreditation manager for hospital settings, Urmia University of Medical Sciences, Urmia, Iran.
REFERENCES
- Gosmanov AR, Umpierrez GE. - Management of hyperglycemia during enteral and parenteral nutrition therapy. Current diabetes reports. 2013;1:155–162. doi: 10.1007/s11892-012-0335-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell J, McDowell JR. - Comparative study on the effect of enteral feeding on blood glucose. British Journal of Nursing. 2007;6:344–349. doi: 10.12968/bjon.2007.16.6.23006. [DOI] [PubMed] [Google Scholar]
- Falciglia M, Freyberg RW, Almenoff PL, et al. - Hyperglycemia-related mortality in critically ill patients varies with admission diagnosis. Critical care medicine. 2009;12:301–309. doi: 10.1097/CCM.0b013e3181b083f7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gale SC, Sicoutris C, Reilly PM, et al. - Poor glycemic control is associated with increased mortality in critically ill trauma patients. The American Surgeon. 2007;5:454–460. doi: 10.1177/000313480707300507. [DOI] [PubMed] [Google Scholar]
- Lee Y-M. - Enteral Nutrition Strategies for Achieving Glycemic Control in the Critical Care Sett ing. Journal of Korean Diabetes. 2015;1:33–37. [Google Scholar]
- Kavanagh BP, McCowen KC. - Glycemic control in the ICU. NEJM. 2010;26:2540–2546. doi: 10.1056/NEJMcp1001115. [DOI] [PubMed] [Google Scholar]
- Umpierrez GE, Isaacs SD, Bazargan N, et al. - Hyperglycemia: an independent marker of in-hospital mortality in patients with undiagnosed diabetes. The Journal of Clinical Endocrinology & Metabolism. 2002;3:978–982. doi: 10.1210/jcem.87.3.8341. [DOI] [PubMed] [Google Scholar]
- Fahy BG, Sheehy AM, Coursin DB. - Glucose control in the intensive care unit. Critical Care Medicine. 2009;5:1769–1776. doi: 10.1097/CCM.0b013e3181a19ceb. [DOI] [PubMed] [Google Scholar]
- Amini A, Derakhshanfar H, Kariman H, et al. - Hyperglycemia and Related Factors in Multiple Trauma Patients in Imam Hossein Hospital, 2010. Journal of Mazandaran University of Medical Sciences (JMUMS) 2013;98:328–332. [Google Scholar]
- Rajabian R, Khaje Dalooei M, Fazlinejad A, et al. - The prevalence of hyperglycemia in acute myocardial infarction and its relation to in-hospital complications. Iranian Journal of Diabetes and Lipid Disorders. 2005;4:37–41. [Google Scholar]
- McMahon MM, Nystrom E, Braunschweig C, et al. - ASPEN clinical guidelines: nutrition support of adult patients with hyperglycemia. Journal of Parenteral and Enteral Nutrition. 2012;1:23–36. doi: 10.1177/0148607112452001. [DOI] [PubMed] [Google Scholar]
- Mousavi Z, Hezarkhani SH, Rokni Yazdi H, et al. - Prevalence of stress hyperglycemia and its associated morbidity and mortality in patients in the emergency ward of Imam Reza (AS) in Mashhad. Journal of Diabetes and Metabolism. 2008;1:19–26. [Google Scholar]
- Whitcomb BW, Pradhan EK, Pitt as AG, et al. - Impact of admission hyperglycemia on hospital mortality in various intensive care unit populations*. Critical care medicine. 2005;12:2772–2777. doi: 10.1097/01.ccm.0000189741.44071.25. [DOI] [PubMed] [Google Scholar]
- Frontera JA, Fernandez A, Claassen J, et al. - Hyperglycemia after SAH Predictors, associated complications, and impact on the outcome. Stroke. 2006;1:199–203. doi: 10.1161/01.STR.0000194960.73883.0f. [DOI] [PubMed] [Google Scholar]
- Krinsley JS, editor. - Association between hyperglycemia and increased hospital mortality in a heterogeneous population of critically ill patients. Mayo Clinic Proceedings. 2003;78:1471–1478. doi: 10.4065/78.12.1471. [DOI] [PubMed] [Google Scholar]
- Freire AX, Bridges L, Umpierrez GE, et al. - Admission hyperglycemia and other risk factors as predictors of hospital mortality in a medical ICU population. CHEST Journal. 2005;5:3109–3116. doi: 10.1378/chest.128.5.3109. [DOI] [PubMed] [Google Scholar]
- Krinsley JS, Jones RL. - Cost analysis of intensive glycemic control in critically ill adult patients. CHEST Journal. 2006;3:644–650. doi: 10.1378/chest.129.3.644. [DOI] [PubMed] [Google Scholar]
- De La Rosa GD, Donado JH, Restrepo AH, et al. - Strict glycaemic control in patients hospitalised in a mixed medical and surgical intensive care unit: a randomised clinical trial. Critical Care. 2008;5:R120. doi: 10.1186/cc7017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inzucchi SE, Siegel MD. - Glucose control in the ICU—how tight is too tight. NEJM. 2009;13:1346–1349. doi: 10.1056/NEJMe0901507. [DOI] [PubMed] [Google Scholar]
- Leite SAO, Locatelli SB, Niece SP, et al. - Impact of hyperglycemia on morbidity and mortality, length of hospitalization and rates of re-hospitalization in a general hospital sett ing in Brazil. Diabetology & Metabolic Syndrome. 2010;1:49. doi: 10.1186/1758-5996-2-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farrokhi F, Smiley D, Umpierrez GE. - Glycemic control in non-diabetic critically ill patients. Best practice & research. Clinical endocrinology & metabolism. 2011;5:813–824. doi: 10.1016/j.beem.2011.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inzucchi SE. - Management of hyperglycemia in the hospital sett ing. NEJM. 2006;18:1903–1911. doi: 10.1056/NEJMcp060094. [DOI] [PubMed] [Google Scholar]