Abstract
Background:
Experts have recommended the adoption of health literacy universal precautions, whereby health care providers make all health information easier to understand, confirm everyone's comprehension, and reduce the difficulty of health-related tasks. The U.S. Department of Health and Human Services selected three health literate practices to track progress in the adoption of health literacy universal precautions.
Objectives:
This study sought to examine whether there has been an increase in the delivery of health literate care and whether recommendations for health literacy universal precautions are being followed.
Methods:
This study used trend and multiple regression analyses of data from 2011 to 2014 from the Medical Expenditure Panel Survey, a national household survey.
Key Results:
The proportion of adults in the U.S. who reported receiving health literate care increased from 2011 to 2014, but fell far short of health literacy universal precautions recommendations of delivering health literate care to everyone. In 2014, 70% of the population reported their providers always gave them instructions that were easy to understand, but only 29% were asked to Teach-Back the instructions and only 17% were offered help with forms. Older, less educated, and racial and ethnic minority group members were more likely to report receiving health literate care than more advantaged groups. People who perceived their health and mental health as fair or poor were less likely to report receiving health literate care.
Conclusions:
Failure to adopt health literacy universal precautions in the face of the high prevalence of limited health literacy in the general population may perpetuate adverse health outcomes that are costly to society. Greater efforts should be made to increase providers' health literacy skills, particularly those who serve populations that are more likely to have limited health literacy, including those with poor health. [Health Literacy Research and Practice. 2017;1(4):e216–e230.]
Plain Language Summary:
This study shows that some health care providers did not always check that their instructions were clear enough for patients to understand. Even fewer providers always offered help in filling out forms. People who were older, less educated, or members of racial or ethnic minority groups were more likely to be asked to confirm their understanding or be offered help with forms. More patients said that their provider was easy to understand, checked their understanding, or offered help with forms in 2014 than in 2011.
A large proportion of the United States population has difficulty obtaining, processing, and understanding basic health information and services to make appropriate health decisions. According to the only national survey of health literacy, which was conducted in 2003, only 12% of American adults did not have difficulty (or, in other words, had proficient health literacy), 53% had intermediate health literacy, and more than 33% had limited health literacy (U.S. Department of Health and Human Services, 2008). Members of disadvantaged groups are more likely to have limited health literacy. These include people with less education, public or no insurance, and poor health; people who did not speak English before the age of 5 years; the elderly; and members of racial and ethnic minority groups (Kutner, Greenberg, Jin, & Paulsen, 2006). People with limited health literacy are less likely to use preventive services or adhere to treatment, and are more likely to be hospitalized (Berkman et al., 2011).
Health literacy can be improved by reducing the difficulty of health information and the complexity of health care tasks (Baker, 2006). With few people possessing the health literacy skills needed to manage the demands of the complex U.S. health care system, the difficulty in identifying which people have limited health literacy, and the fact that a person's health literacy can vary depending on the circumstances, led experts to recommend the adoption of health literacy universal precautions (Paasche-Orlow, Schillinger, Greene, & Wagner, 2006). Health care providers taking universal precautions assume that all patients may have difficulty comprehending health information and accessing health services.
The U.S. Department of Health and Human Services included the goal of improving health literacy in its national health promotion and disease prevention initiative Healthy People (U.S. Department of Health and Human Services, 2000). To track progress in the adoption of health literacy universal precautions, Healthy People 2020 selected measures of three health literacy strategies: (1) giving instructions about what to do about a specific illness or health condition that are easy to understand; (2) asking patients to describe how they were going to follow these instructions (the first step of the Teach-Back method); and (3) offering help in filling out forms (U.S. Department of Health and Human Services, 2017).
The first two are measures of individual providers' actions in the clinical encounter. Using clear language (i.e., common, everyday language free from jargon) and initiating the Teach-Back method of confirming understanding are highly promoted health literacy strategies (DeWalt et al., 2010). The full Teach-Back process is iterative. If the patient fails to teach the information back correctly, the provider has to re-teach the information and again test understanding until the patient can correctly teach-back the information. Our measure captures only the first step of the process. For the sake of simplicity, we refer to this measure as the Teach-Back measure, although it could more precisely be called the initiation of Teach-Back measure. The third measure captures whether health care settings are creating welcoming, stigma-free environments that characterize a health-literate health care organization (Brach et al., 2012).
In this article, we use the Healthy People 2020 measures to examine whether there has been an increase in health literate care and whether recommendations for health literacy universal precautions are being followed. We explore how health literate practices by health care professionals vary across patient characteristics and particularly whether people with characteristics associated with lower health literacy (i.e., people who are older, less educated, members of racial or ethnic minority groups, publicly insured, not proficient in English, and in poorer health) are equally likely to receive health literate care as other people.
Data and Methods
Starting in 2011, the Agency for Healthcare Research and Quality's Medical Expenditure Panel Survey (MEPS)–Household Component has annually tracked the three Healthy People 2020 health literacy measures using questions that were created through the Consumer Assessment of Healthcare Providers and Systems development process (Weidmer, Brach, & Hays, 2012). MEPS data are nationally representative of the civilian non-institutionalized population and contain detailed information on demographic characteristics, health status, and health care use. Health literacy data are collected as part of the MEPS Adult Self-Administered Questionnaire (Adult SAQ), which had a response rate between 88.7% and 94.2% from 2011 to 2014, the most recent data available at the time of this analysis. We restricted our sample to those older than age 25 years with at least one visit in the previous 12 months. To be able to control for provider characteristics, we also limited our sample to those who reported having a person as the usual source of care that is not an emergency room. (Including those people who did not report a usual source of care did not change our results in any significant way.) This gave us a sample size of 21,888. Only respondents who were given instructions (17,309 [79%] of those who had a usual source of care across the 4 years) were asked if instructions were easy to understand and how often they were asked to describe how they planned to follow the instructions. Only respondents who were asked to sign or fill out a form (13,092 across the 4 years) were asked if they were offered help with the form. We derived three outcome variables (Instruction Easy, Teach-Back, and Help with Forms) from the answers to these survey questions. Like the Healthy People measures, we defined an answer of “always” as 1, and anything less than “always” as 0.
Our multiple regression analyses used pooled 2011 to 2014 MEPS household data to examine the associations between patient characteristics and the probability of a person always receiving health literate care. We controlled for characteristics predictive of health literacy (Kutner et al., 2006; Martin et al., 2009), such as age, race and ethnicity, insurance status, household poverty status, education level, comfort speaking English, and health status.
Before 2013, Medical Expenditure Panel Survey (MEPS) asked whether each member in a household was comfortable speaking English when MEPS respondents reported not everyone in the household was comfortable or not comfortable speaking English. Since 2013, MEPS asks those who speak another language at home how well they speak English. The potential answers are: very well, well, not well, and not at all. For the purpose of this analysis, we categorized very well and well into “comfortable speaking English,” and not well and not at all into “not comfortable speaking English.” A previous analysis has shown that the proportion of respondents who say they are not comfortable speaking English and the proportion who say they speak English not well or not at all are comparable (Brach & Chevarley, 2008).
We also controlled for basic demographics (gender and marital status) and other health-related variables that might influence how providers interact with patients (e.g., weight, taking five or more drugs, and smoking). Census region and an indicator for metropolitan statistical area were included to capture potential geographic variations in provider practice. Provider characteristics (gender, race/ethnicity, specialty, and the location of the usual source of care) were also controlled for. (See Table A for the full specification of these variables and the number of complete cases used in the regression analysis.) We used Stata (version 14.0/SE) to estimate survey-weighted (Adult SAQ weights, which corrects for questionnaire nonresponse) linear probability models, controlling for MEPS complex survey design. For each key demographic and health status variable of interest, we calculated adjusted means.
Table A.
Descriptive Statistics of Adults Age 25 Years and Older Who Had a Usual Source of Care
| Patient Characteristics | Had USC and at Least One Visit (N = 19,172) | Given Instruction (N = 15,140) | Given Forms to Fill Out (N = 11,562) | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| Mean | Standard Error | Mean | Standard Error | Mean | Standard Error | |
|
| ||||||
| Year | ||||||
| 2011 | 0.253 | 0.006 | 0.251 | 0.006 | 0.251 | 0.007 |
| 2012 | 0.238 | 0.004 | 0.241 | 0.004 | 0.241 | 0.005 |
| 2013 | 0.261 | 0.004 | 0.261 | 0.005 | 0.257 | 0.006 |
| 2014 | 0.248 | 0.006 | 0.247 | 0.007 | 0.251 | 0.007 |
|
| ||||||
| Gender | ||||||
| Female | 0.427 | 0.004 | 0.424 | 0.004 | 0.414 | 0.005 |
| Male | 0.573 | 0.004 | 0.576 | 0.004 | 0.586 | 0.005 |
|
| ||||||
| Age | ||||||
| 25–44 | 0.252 | 0.006 | 0.241 | 0.007 | 0.262 | 0.007 |
| 45–64 | 0.443 | 0.007 | 0.447 | 0.008 | 0.447 | 0.009 |
| 65–74 | 0.192 | 0.005 | 0.196 | 0.005 | 0.188 | 0.006 |
| 75+ | 0.113 | 0.005 | 0.116 | 0.005 | 0.102 | 0.005 |
|
| ||||||
| Marital status | ||||||
| Married | 0.645 | 0.008 | 0.647 | 0.008 | 0.662 | 0.009 |
| Widowed | 0.083 | 0.003 | 0.082 | 0.003 | 0.073 | 0.003 |
| Divorced | 0.134 | 0.004 | 0.136 | 0.005 | 0.130 | 0.005 |
| Separated | 0.018 | 0.001 | 0.017 | 0.001 | 0.016 | 0.002 |
| Never married | 0.120 | 0.004 | 0.117 | 0.005 | 0.119 | 0.005 |
|
| ||||||
| Education | ||||||
| No high school | 0.086 | 0.004 | 0.082 | 0.004 | 0.067 | 0.004 |
| High school | 0.255 | 0.006 | 0.248 | 0.007 | 0.229 | 0.007 |
| Some college | 0.288 | 0.005 | 0.292 | 0.006 | 0.285 | 0.006 |
| College degree | 0.221 | 0.006 | 0.224 | 0.006 | 0.242 | 0.007 |
| Postgraduate | 0.150 | 0.005 | 0.155 | 0.006 | 0.178 | 0.006 |
|
| ||||||
| Race | ||||||
| NH Black | 0.089 | 0.005 | 0.086 | 0.005 | 0.078 | 0.004 |
| NH White | 0.767 | 0.010 | 0.777 | 0.010 | 0.800 | 0.009 |
| Hispanic | 0.080 | 0.006 | 0.077 | 0.006 | 0.068 | 0.005 |
| Asian | 0.044 | 0.006 | 0.041 | 0.006 | 0.037 | 0.005 |
| Others | 0.020 | 0.002 | 0.019 | 0.002 | 0.017 | 0.002 |
|
| ||||||
| Uncomfortable speaking English | ||||||
| No | 0.972 | 0.002 | 0.974 | 0.002 | 0.981 | 0.002 |
| Yes | 0.028 | 0.002 | 0.026 | 0.002 | 0.019 | 0.002 |
|
| ||||||
| Perceived health status | ||||||
| Excellent | 0.188 | 0.005 | 0.169 | 0.005 | 0.183 | 0.006 |
| Very good | 0.346 | 0.005 | 0.338 | 0.006 | 0.344 | 0.006 |
| Good | 0.298 | 0.004 | 0.309 | 0.005 | 0.299 | 0.006 |
| Fair | 0.127 | 0.004 | 0.137 | 0.005 | 0.130 | 0.005 |
| Poor | 0.042 | 0.002 | 0.046 | 0.002 | 0.044 | 0.003 |
|
| ||||||
| Perceived mental health status | ||||||
| Excellent | 0.335 | 0.006 | 0.326 | 0.006 | 0.337 | 0.007 |
| Very good | 0.316 | 0.005 | 0.312 | 0.006 | 0.315 | 0.006 |
| Good | 0.257 | 0.005 | 0.266 | 0.005 | 0.254 | 0.006 |
| Fair | 0.075 | 0.003 | 0.079 | 0.003 | 0.077 | 0.003 |
| Poor | 0.017 | 0.001 | 0.018 | 0.002 | 0.017 | 0.002 |
|
| ||||||
| Take ≥5 drugs | ||||||
| No | 0.568 | 0.006 | 0.529 | 0.007 | 0.543 | 0.008 |
| Yes | 0.432 | 0.006 | 0.471 | 0.007 | 0.457 | 0.008 |
|
| ||||||
| Census region | ||||||
| South | 0.366 | 0.013 | 0.363 | 0.013 | 0.367 | 0.014 |
| Midwest | 0.227 | 0.013 | 0.232 | 0.014 | 0.233 | 0.014 |
| Northeast | 0.213 | 0.012 | 0.209 | 0.012 | 0.207 | 0.012 |
| West | 0.194 | 0.011 | 0.196 | 0.010 | 0.193 | 0.011 |
|
| ||||||
| Weight categories | ||||||
| Underweight | 0.012 | 0.001 | 0.012 | 0.001 | 0.013 | 0.002 |
| Normal | 0.289 | 0.005 | 0.280 | 0.006 | 0.297 | 0.006 |
| Overweight | 0.347 | 0.005 | 0.344 | 0.006 | 0.343 | 0.006 |
| Obese | 0.352 | 0.006 | 0.364 | 0.007 | 0.347 | 0.008 |
|
| ||||||
| Insurance | ||||||
| Any private | 0.754 | 0.006 | 0.758 | 0.007 | 0.779 | 0.007 |
| Public only | 0.211 | 0.006 | 0.208 | 0.006 | 0.191 | 0.006 |
| Uninsured | 0.035 | 0.002 | 0.034 | 0.002 | 0.030 | 0.002 |
|
| ||||||
| Income | ||||||
| Poor | 0.084 | 0.003 | 0.083 | 0.003 | 0.077 | 0.003 |
| Near poor | 0.036 | 0.002 | 0.036 | 0.002 | 0.031 | 0.002 |
| Low income | 0.108 | 0.003 | 0.103 | 0.003 | 0.096 | 0.004 |
| Middle income | 0.279 | 0.006 | 0.277 | 0.006 | 0.273 | 0.007 |
| High income | 0.493 | 0.008 | 0.501 | 0.009 | 0.523 | 0.009 |
|
| ||||||
| Smoker | ||||||
| No | 0.861 | 0.004 | 0.861 | 0.005 | 0.868 | 0.005 |
| Yes | 0.139 | 0.004 | 0.139 | 0.005 | 0.132 | 0.005 |
|
| ||||||
| Metropolitan statistical area | ||||||
| Yes | 0.850 | 0.016 | 0.851 | 0.016 | 0.852 | 0.017 |
| No | 0.150 | 0.016 | 0.149 | 0.016 | 0.148 | 0.017 |
|
| ||||||
| Provider gender | ||||||
| Male | 0.691 | 0.007 | 0.685 | 0.007 | 0.679 | 0.008 |
| Female | 0.309 | 0.007 | 0.315 | 0.007 | 0.321 | 0.008 |
|
| ||||||
| Provider race | ||||||
| NH White | 0.745 | 0.011 | 0.749 | 0.010 | 0.767 | 0.010 |
| Asian | 0.114 | 0.008 | 0.113 | 0.008 | 0.105 | 0.008 |
| Hispanic | 0.058 | 0.004 | 0.056 | 0.004 | 0.051 | 0.004 |
| NH Black | 0.036 | 0.002 | 0.034 | 0.002 | 0.033 | 0.003 |
| Others | 0.047 | 0.003 | 0.048 | 0.003 | 0.044 | 0.003 |
|
| ||||||
| Practice location | ||||||
| Office | 0.885 | 0.006 | 0.883 | 0.006 | 0.887 | 0.007 |
| Hospital (non-ED) | 0.115 | 0.006 | 0.117 | 0.006 | 0.113 | 0.007 |
|
| ||||||
| Provider specialty | ||||||
| General practitioner | 0.693 | 0.009 | 0.686 | 0.009 | 0.679 | 0.009 |
| Internal medicine | 0.200 | 0.008 | 0.208 | 0.008 | 0.210 | 0.009 |
| NP/PA | 0.039 | 0.004 | 0.039 | 0.004 | 0.040 | 0.004 |
| Other | 0.068 | 0.003 | 0.067 | 0.003 | 0.071 | 0.004 |
Note. Weighted mean and standard errors were estimated using the Stata's svy:proportion command. Only complete cases used in the multivariate regression analysis are used. The “Given Instruction” column reflect the estimation sample of those who answered the question of whether the instructions were easy to understand. ED = emergency department; NH = non-Hispanic; NP = nurse practitioner; PA = physician's assistant; USC = usual source of care.
Results
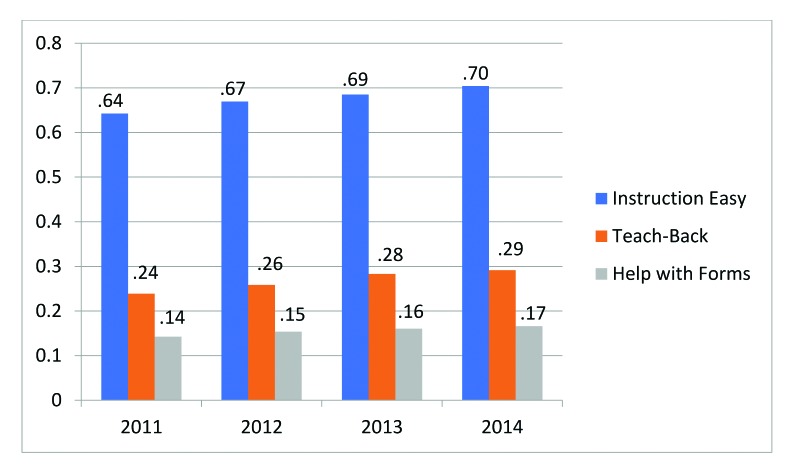
All three measures of health literate care improved between 2011 and 2014 (Figure 1). The percentage of people who reported their providers always gave them instructions that were easy to understand increased from 64% in 2011 to 70% in 2014, a roughly 10% increase (p < .001). During the same time period, the percentage of people who reported their provider always asked them to explain how they will follow instructions increased from 24% to 29%, an increase of 22% (p < .001). In 2014, 17% of people who were given forms were offered help in filling them out, up from 14% in 2011 (a 16% increase, p < .1).
Figure 1.
Proportion of adults age 25 years and older who reported receiving health literate care.
Table 1 shows the regression-adjusted means of the three outcome variables by key patient characteristics that have been shown to predict health literacy. A little more than two-thirds of people in each age group reported that they were always given easy-to-understand instructions. Similarly, the proportion of respondents reporting they were always asked to explain how they planned to follow the instructions, roughly one-quarter from each group, did not vary with age. The oldest group (age ≥75 years), however, was much more likely to always be offered help filling out forms (45.6% more than in people between ages 25 and 44 years, p < .001).
Table 1.
Proportion of Adults Age 25 Years and Older Who Reported Receiving Health Literate Care: Key Demographics
| Demographic | Instruction Easy | Teach-Back | Help with Forms | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Proportion | Relative Differencea | Proportion | Relative Differencea | Proportion | Relative Differencea | |
|
| ||||||
| Total | 0.675 | 0.268 | 0.156 | |||
|
| ||||||
| Age (years) | ||||||
| 25–44b | 0.679 | 0.261 | 0.134 | |||
| 45–64 | 0.686 | 0.276 | 0.153* | 14.5% | ||
| 65–74 | 0.681 | 0.252 | 0.161* | 20.7% | ||
| 75+ | 0.661 | 0.271 | 0.195** | 45.6% | ||
|
| ||||||
| Education | ||||||
| No high school | 0.688 | 0.380** | 93.8% | 0.201** | 47.2% | |
| High school | 0.668 | 0.297** | 51.4% | 0.163* | 19.8% | |
| Some college | 0.685 | 0.287** | 46.3% | 0.160* | 17.4% | |
| College degree | 0.683 | 0.216 | 0.137 | |||
| Postgraduateb | 0.686 | 0.196 | 0.137 | |||
|
| ||||||
| Race | ||||||
| Non-Hispanic Black | 0.689 | 0.356** | 43.7% | 0.170 | ||
| Non-Hispanic Whiteb | 0.686 | 0.248 | 0.149 | |||
| Hispanic | 0.651* | −5.1% | 0.323** | 30.35% | 0.161 | |
| Asian | 0.607** | −11.6% | 0.328** | 32.5% | 0.177 | |
| Others | 0.700 | 0.291 | 0.211 | |||
|
| ||||||
| Language | ||||||
| Comfortable speaking Englishb | 0.681 | 0.266 | 0.152 | |||
| Uncomfortable speaking English | 0.660 | 0.306 | 0.246** | 61.7% | ||
|
| ||||||
| Insurance | ||||||
| Any privateb | 0.685 | 0.265 | 0.152 | |||
| Public only | 0.670 | 0.275 | 0.160 | |||
| Uninsured | 0.647 | 0.267 | 0.152 | |||
|
| ||||||
| Income level | ||||||
| Poorb | 0.684 | 0.260 | 0.156 | |||
| Near poor | 0.686 | 0.311* | 19.4% | 0.162 | ||
| Low income | 0.689 | 0.288 | 0.153 | |||
| Middle income | 0.676 | 0.267 | 0.150 | |||
| High income | 0.681 | 0.260 | 0.155 | |||
Note: Regression-adjusted proportions are presented. Each regression controlled for year fixed effects, gender, age group, marital status, education, race/ethnicity, comfort speaking English, perceived health status and perceived mental health status, taking five or more prescription drugs, body mass index categories, smoking status, U.S. Census region, and metropolitan statistical area. It also controls for the gender, race, specialty, and practice location of the usual source of care. Race/ethnicity categories other than Hispanic include only non-Hispanic people.
Significance refers to differences from the reference group in each category. For significant differences, we calculated how much larger or smaller the value was than the reference group.
Reference group.
p < .1.
p < .001.
The proportion of people reporting being given easy-to-understand instructions did not vary with education. The three groups with lowest education achievements were, however, much more likely to always be asked to describe how they planned to follow the instructions (the first step of the Teach-Back method): 38% of those with no high school degree, 29.7% of those with only a high school degree, and 28.7% of those with some college education reported that they were always asked to Teach-Back instructions, compared to the 19.6% of those with a postgraduate degree who were asked to Teach-Back. The relative differences are large: those with no high school degree were 93.8% more likely than those with a postgraduate degree to report always being asked to Teach-Back instructions, those with only a high school degree were 51.4% more likely, and those with some college education were 46.3% more likely (p < .001 in each case). Whereas the three lowest education groups also received more offers of help with filling out forms (20.1%, 16.3%, and 16%, respectively) than those with a postgraduate degree (13.7%); only the difference between the group with no high school degree and the group with a postgraduate degree was statistically significant at better than the p < .1 level.
There were also significant disparities among people by race and ethnicity for all three outcome measures. With respect to easy-to-understand instructions, only Asians were significantly less likely to report that instructions were always easy to understand than non-Hispanic Whites (60.7% vs. 68.6%, p < .001). In contrast, non-Hispanic Blacks, Hispanics, and Asians all reported always being asked to Teach-Back how they were going to follow instructions at a higher rate than non-Hispanic Whites (35.6%, 32.3%, and 32.8%, respectively, vs. 24.8%, p < .001 in each case.) Finally, there were no racial/ethnic differences in being offered help filling out forms, but people who were not comfortable speaking English were more likely to report always being offered help with forms than people who were comfortable with speaking English (24.6% vs. 15.2%, p < .001). We did not find any significant variance in health literate practices by insurance status or poverty status.
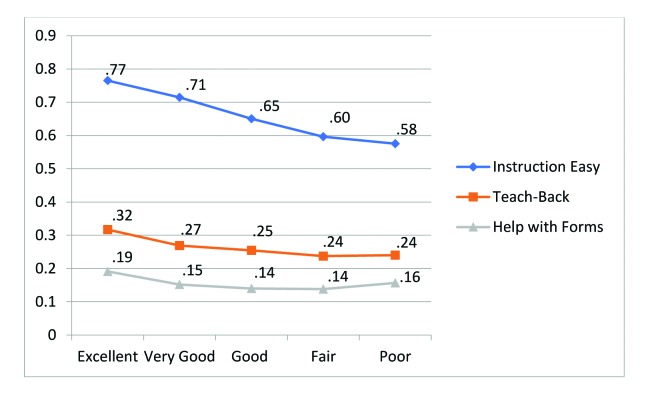
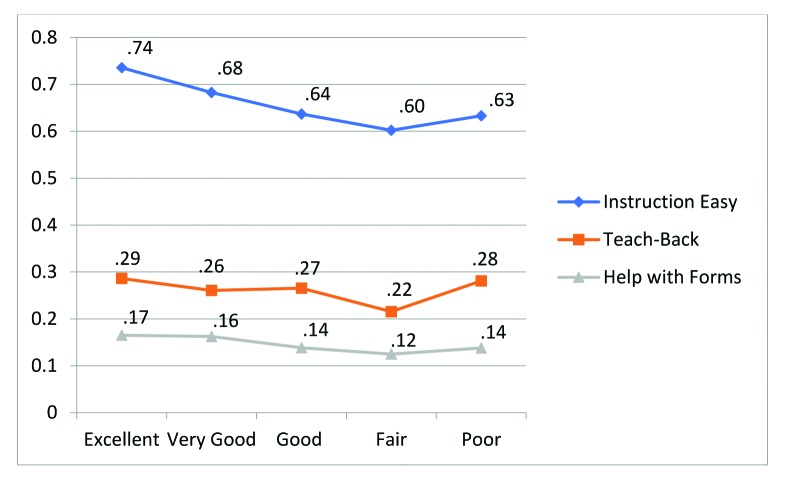
Perceived health status was positively correlated with health literate care. As shown by the regression-adjusted proportions in Figure 2, the better a person's health status was, the more likely it was that they would report always receiving health literate care. Whereas 77% of those who perceived their health as excellent reported that the instructions they received were always easy to understand, only 58% of those who perceived their health as poor responded the same (p < .001). Those who were in the very good, good, and fair groups also were less likely to report always understanding instructions than the excellent group (p < .001 in each case). The patterns of the other two outcomes—being asked to Teach-Back and being offered help filling out forms—are largely the same; as perceived physical health status goes from excellent to poor, the proportion of people within each group reporting health literate care decreased. The results from the perceived mental health status (Figure 3) showed similar patterns to those of the perceived physical health status, although the trend is less consistent and differences are not always statistically significant. Full regression results are presented in Table B.
Figure 2.
Proportion of adults age 25 years and older who reported receiving health literate care by perceived health status. Regression-adjusted proportions are presented. Each regression controlled for year fixed effects, gender, age group, marital status, education, race/ethnicity, comfort speaking English, perceived health status and perceived mental health status, taking five or more drugs, body mass index categories and smoking status, U.S. Census region, and metropolitan statistical area. It also controls for the gender, race, specialty, and practice location of the usual source of care.
Figure 3.
Proportion of adults age 25 years and older who received health literate care by perceived mental health status. Regression-adjusted proportions are presented. Each regression controlled for year fixed effects, gender, age group, marital status, education, race/ethnicity, comfort speaking English, perceived health status and perceived mental health status, taking five or more drugs, body mass index categories and smoking status, U.S. Census region, and metropolitan statistical area. It also controls for the gender, race, specialty, and practice location of the usual source of care.
Table B.
Linear Probability Models of Receiving Health Literate Care
| Patient Characteristics | Instruction Easy Coefficient (Standard Error) (N = 15,140) | Teach-Back Coefficient (Standard Error) (N = 15,152) | Help with Form Coefficient (Standard Error) (N = 11,562) |
|---|---|---|---|
|
| |||
| Year | |||
| 2011a | – | – | – |
| 2012 | 0.023* (0.013) | 0.016 (0.011) | 0.011 (0.011) |
| 2013 | 0.045** (0.013) | 0.050** (0.012) | 0.019 (0.012) |
| 2014 | 0.063*** (0.014) | 0.056** (0.012) | 0.023* (0.013) |
|
| |||
| Gender | |||
| Femalea | – | – | – |
| Male | −0.013 (0.010) | 0.030** (0.010) | 0.017* (0.009) |
|
| |||
| Age (years) | |||
| 25–44a | – | – | – |
| 45–64 | 0.007 (0.013) | 0.015 (0.011) | 0.019* (0.010) |
| 65–74 | 0.002 (0.018) | −0.009 (0.015) | 0.028* (0.016) |
| 75+ | −0.018 (0.023) | 0.010 (0.020) | 0.061** (0.019) |
|
| |||
| Marital status | |||
| Marrieda | – | – | – |
| Widowed | 0.039*** (0.019) | 0.009 (0.019) | 0.023 (0.018) |
| Divorced | −0.006 (0.015) | −0.012 (0.015) | 0.010 (0.013) |
| Separated | 0.062* (0.034) | −0.016 (0.031) | 0.018 (0.030) |
| Never married | 0.005 (0.015) | −0.008 (0.017) | 0.027* (0.014) |
|
| |||
| Education | |||
| No high school | 0.003 (0.022) | 0.184** (0.025) | 0.064** (0.021) |
| High school | −0.018 (0.017) | 0.101** (0.016) | 0.027* (0.014) |
| Some college | −0.000 (0.018) | 0.091** (0.016) | 0.024* (0.013) |
| College degree | −0.003 (0.017) | 0.020 (0.015) | 0.00 (0.013) |
| Postgraduatea | – | – | – |
|
| |||
| Race | |||
| NH Black | 0.003 (0.016) | 0.108b (0.016) | 0.021 (0.015) |
| NH Whitea | – | – | – |
| Hispanic | −0.035a (0.019) | 0.075b (0.016) | 0.012 (0.016) |
| Asian | −0.079b (0.023) | 0.080b (0.021) | 0.027 (0.020) |
| Others | 0.014 (0.034) | 0.043 (0.036) | 0.062 (0.038) |
|
| |||
| Uncomfortable speaking English | |||
| Noa | – | – | – |
| Yes | −0.021 (0.031) | 0.040 (0.031) | 0.094b (0.031) |
|
| |||
| Perceived health status | |||
| Excellenta | – | – | – |
| Very good | −0.050** (0.016) | −0.048** (0.016) | −0.039** (0.013) |
| Good | −0.114** (0.017) | −0.063* (0.018) | −0.051** (0.015) |
| Fair | −0.169** (0.019) | −0.080* (0.021) | −0.053** (0.016) |
| Poor | −0.190** (0.032) | −0.077* (0.028) | −0.035 (0.023) |
|
| |||
| Perceived mental health status | |||
| Excellenta | – | – | – |
| Very good | −0.053** (0.013) | −0.025* (0.014) | −0.003 (0.011) |
| Good | −0.099** (0.014) | −0.021 (0.014) | −0.027*** (0.012) |
| Fair | −0.133** (0.020) | −0.071** (0.019) | −0.040*** (0.017) |
| Poor | −0.102** (0.037) | −0.005 (0.036) | −0.027 (0.028) |
|
| |||
| Take ≥5 drugs | |||
| Noa | – | – | – |
| Yes | −0.004 (0.011) | −0.025** (0.009) | −0.002 (0.009) |
|
| |||
| Census region | |||
| South | −0.010 (0.016) | −0.018 (0.018) | 0.003 (0.013) |
| Midwest | −0.001 (0.014) | −0.029 (0.019) | 0.021 (0.014) |
| Northeast | – | – | – |
| West | −0.036*** (0.016) | −0.016 (0.020) | 0.002 (0.015) |
|
| |||
| Weight categories | |||
| Underweight | 0.064 (0.039) | 0.022 (0.042) | −0.024 (0.030) |
| Normala | – | – | – |
| Overweight | 0.023*** (0.011) | 0.026*** (0.012) | 0.002 (0.010) |
| Obese | 0.045** (0.012) | 0.053** (0.011) | 0.024*** (0.011) |
|
| |||
| Insurance | |||
| Any privatea | – | – | – |
| Public only | −0.015 (0.015) | 0.011 (0.012) | 0.008 (0.013) |
| Uninsured | −0.038 (0.025) | 0.002 (0.025) | −0.001 (0.027) |
|
| |||
| Income levels | |||
| Poora | – | – | – |
| Near poor | 0.001 (0.029) | 0.051* (0.026) | 0.006 (0.026) |
| Low income | 0.005 (0.022) | 0.028 (0.020) | −0.004 (0.019) |
| Middle income | −0.009 (0.020) | 0.007 (0.017) | −0.006 (0.017) |
| High income | −0.003 (0.022) | 0.000 (0.018) | −0.001 (0.018) |
|
| |||
| Smoker | |||
| Noa | – | – | – |
| Yes | 0.011 (0.013) | 0.013 (0.013) | −0.008 (0.013) |
|
| |||
| Metropolitan statistical area | |||
| Yes | −0.027* (0.015) | 0.015 (0.016) | −0.026* (0.014) |
| Noa | – | – | – |
|
| |||
| Provider gender | |||
| Male | 0.017* (0.010) | 0.012 (0.010) | 0.017* (0.009) |
| Femalea | – | – | – |
|
| |||
| Provider race | |||
| NH Black | 0.004 (0.028) | 0.008 (0.026) | 0.011 (0.024) |
| NH Whitea | – | – | – |
| Hispanic | 0.022 (0.020) | −0.001 (0.021) | 0.027 (0.021) |
| Asian | 0.001 (0.017) | −0.010 (0.018) | −0.001 (0.016) |
| Others | −0.011 (0.023) | 0.002 (0.020) | 0.023 (0.019) |
|
| |||
| Practice location | |||
| Office | – | – | – |
| Hospital (non-ED) | 0.020 (0.016) | 0.026* (0.015) | 0.026* (0.014) |
|
| |||
| Provider specialty | |||
| General practitionera | – | – | – |
| Internal medicine | 0.010 (0.013) | 0.004 (0.013) | −0.009 (0.011) |
| NP/PA | −0.014 (0.029) | −0.007 (0.025) | 0.014 (0.020) |
| Other | −0.006 (0.019) | −0.002 (0.018) | 0.026* (0.015) |
|
| |||
| Constant | 0.799** (0.034) | 0.163** (0.037) | 0.125** (0.028) |
Notes: Coefficients and standard errors (in parentheses) were obtained using Stata's svy:regression command. ED = emergency department; NP = nurse practitioner; PA = physician assistant.
Reference group.
p < .10.
p < .01.
p < .05
To mitigate the concern that people in poorer health would be more likely to have more visits and therefore be less likely to respond “always” when asked about health literate care, we ran a similar regression with the outcome variables being defined as “always” or “usually” receiving health literate care. The results showed similar patterns. In yet another specification, we controlled for the number of health care visits. These results were also not qualitatively different.
Discussion
To our knowledge, this analysis is the first study of reports of health literate practices in the U.S. using a nationally representative sample. During the 4-year study period, there was significant improvement in people reporting that instructions were easy to understand and of being asked for Teach-Back of instructions, and an increase in reports of offers of help with forms that approached statistical significance. Improvement has been steady, but the small percentage of people reporting they were always given health literate care is disappointing. Although over two-thirds of the population in 2014 always found instructions their providers gave easy to understand, fewer than one-third were always asked to Teach-Back instructions, and even fewer (17%) were always offered help with forms.
Certain disadvantaged groups are more likely to have limited health literacy, so it is encouraging that there were almost no demographic differences in the reports of instructions always being easy to understand. If it is, in fact, the case that these disadvantaged group members are equally likely to understand as groups with higher health literacy (not only equally likely to report understanding), there are three possible explanations. First, members of disadvantaged groups are seeing a distinct set of providers who make themselves easily understood by that population. Second, providers are identifying disadvantaged group members as needing health literate communication and are tailoring their instructions accordingly. Third, a subset of providers is being clear to all their patients (i.e., they are observing health literacy universal precautions), whereas the instructions of other providers are unclear to all of their patients, including those with higher health literacy.
The lack of differences between patients who were comfortable and were not comfortable speaking English was surprising, given data from the National Healthcare Quality and Disparities Report that a large proportion of people reporting having a hard time understanding their doctor stated that speaking a different language was the reason (Agency for Healthcare Research and Quality, 2016). The fact that Asian patients were the one racial group less likely to report always understanding at the level of p < .01, even after controlling for comfort with speaking English, may indicate that cultural differences play a role in communication difficulties.
Those with the least education and members of racial and ethnic groups were more likely to be asked to Teach-Back instructions. These differences can be explained either by members of these groups going to providers more likely to initiate the Teach-Back method, or by providers initiating it more frequently with their patients who are members of those groups (Turner et al., 2009). Although members of these disadvantaged groups tend to see a distinct set of providers (e.g., safety net providers and providers who are themselves members of minority groups) (Marrast, Zallman, Woolhandler, Bor, & McCormick, 2014), we have reduced that effect in our analysis by controlling for provider characteristics. Furthermore, if market segmentation was driving our findings we would expect to see similar differences in Teach-Back rates between publicly and privately insured people as well as between people with higher and lower income. Therefore, it appears that at least some of the reason minority group members are more likely than their nonminority counterparts to be asked to Teach-Back instructions is due to providers targeting minority patients and those with less education. The fact that the elderly were no more likely to be asked to Teach-Back instructions than young adults indicates that providers who specialize in serving the elderly are no more likely to use this health literate practice than others and/or that providers who see patients of all ages do not recognize the greater vulnerability of their elderly patients.
In contrast, help with forms was more likely to be always offered to the elderly (age ≥75 years), as well as to those less educated and those uncomfortable with speaking English. The emergence of disparities associated with comfort in speaking English for this measure may be related to the presence, or absence, of language assistance (i.e., interpreters or bilingual providers). It is possible that interpreters waiting for the clinical encounter to begin offer their assistance with forms. Alternatively, office staff (e.g., receptionists and medical assistants) may offer help with forms precisely because interpreters or providers who speak the patient's language are available only for the clinical encounter. The overall low rates of offers of help with forms, even for the most vulnerable patients, indicate that health literate practices are not widely integrated into health systems' nonclinical workflows.
Some might argue that resources are limited and rather than pursue universal precautions, providers should concentrate on those most needing extra help. This approach, however, would shortchange many people. For example, focusing health literate care on racial and ethnic minority groups would overlook non-Hispanic Whites, who comprise 41% of those with the lowest level of health literacy (U.S. Department of Health and Human Services, 2008). Furthermore, health literacy can fluctuate with fatigue, fear, and illness—meaning that any level of health literate care that falls short of universal precautions is bound to miss many who are at risk of misunderstanding critical information, such as medication instructions.
Our results suggest that until health literacy universal precautions can be achieved, health care providers should focus more on one vulnerable group—people with poor physical and mental health. People with perceived poor health have worse health literacy (Kutner et al., 2006), yet in our study they were less likely to receive health literate care. A possible explanation for why those with worse physical and mental health status were less likely to always find instructions easy to understand is that they were given more complicated instructions. However, it is unclear why they were also less likely to be asked to Teach-Back to check their understanding of the instructions they received or be offered help filling out forms. Understanding their conditions and how to manage them is especially important for this vulnerable group.
This study is subject to several limitations. First, we do not directly observe the use of health literate strategies, but rely on reports of their use. People who reported instructions were always easy to understand may have misunderstood the instructions because providers were not easy to understand, but did not realize they misunderstood. Similarly, people who reported they were asked to Teach-Back instructions may have only been asked, “Do you understand?” or “Do you have any questions?” We would not, however, expect this limitation to bias our temporal analysis because reporting bias would not be expected to change over time. We have no information if misreporting of Teach-Back or offers of help with forms varies by the respondent characteristics included in our model. Second, the health literacy questions are asked at the person level and not at the visit level. It is possible that people who have a large number of visits find it harder to answer they “always” received health literate care. We mitigated this by running two sensitivity analyses: (1) combining “usually” and “always” for all three outcomes, and (2) including total number of visits in the regression analysis as a control variable. Third, the SAQ is available only in English and Spanish. For languages other than English, an interpreter, on site for the verbally administered portion of the MEPS data collection process, may have sight-translated the SAQ and read the questions out loud, but we do not have those data. Fourth, completing the SAQ requires reading and writing skills (although interviewers are permitted to write the answers down if a medical condition prevents the respondent from doing so, and a toll-free number was available to ask questions). Although we found that people with lower levels of education are less likely to complete the SAQ, the completion rates were between 88.7% and 94.2%, and the SAQ weights account for item nonresponse using variables such as education. Although the point-in-time estimates of the proportion of the population receiving health literate care may be higher than our estimates, our trend analysis remains unaffected. Fifth, respondents with less education were less likely to answer that they received instructions and that they were given forms and, therefore, were not asked about Teach-Back or help with forms. Because these respondents were more likely to report that Teach-Back was initiated and that help with forms was offered, this also could result in a downward bias in our point-in-time estimates. Finally, our data are from a household survey and not a survey of providers. Therefore, differences in the receipt of health literate care that are associated with patient characteristics may be the result of (1) providers varying the level of health literate care they deliver based on each patient's characteristics, or (2) people with similar characteristics being more likely to see providers that deliver more (or less) health literate care.
Conclusion
During the period from 2011 to 2014, rates of health literate care increased slowly but steadily. However, almost one-third of the population seeing health care providers had, at one time during 2014, found that instructions given by their health care provider were not easy to understand. At some point during the year, over two-thirds did not have their understanding of instructions they received verified using the Teach-Back method. Some vulnerable populations (members of racial and ethnic minority groups, the elderly, and those with little education) were more likely to receive some forms of health literate care. Failure to adopt health literacy universal precautions in the face of the high prevalence of limited health literacy in the general population may perpetuate adverse health outcomes that are costly to society (Howard, 2004). Greater efforts should be made to increase providers' health literacy skills, particularly those who serve populations that are more likely to have limited health literacy—including those with poor health. Importantly, health systems will need to redesign workflows to integrate health literate practices if health literacy universal precautions are ever to be achieved (Brach, 2017; Brach et al., 2012).
References
- Agency for Healthcare Research and Quality. (2016). National healthcare quality and disparities report chartbook on person- and family-centered care. Retrieved from https://www.ahrq.gov/research/findings/nhqrdr/chartbooks/personcentered/index.html
- Baker D. W. (2006). The meaning and the measure of health literacy. Journal of General Internal Medicine, 21(8), 878–883. 10.1111/j.1525-1497.2006.00540.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman N. D. Sheridan S. L. Donahue K. E. Halpern D. J. Viera A. Crotty K. Viswanathan M. (2011). Health literacy interventions and outcomes: An updated systematic review. Retrieved from Agency for Healthcare Research and Quality website: https://archive.ahrq.gov/research/findings/evidence-based-reports/litupsum.html [PMC free article] [PubMed]
- Brach C. (2017). The journey to become a health literate organization: A snapshot of health system improvement. Studies in Health Technology and Informatics, 240, 203–237. [PMC free article] [PubMed] [Google Scholar]
- Brach C. Keller D. Hernandez L. M. Baur C. Parker R. Dreyer B. Schillinger D. (2012). Ten attributes of health literate health care organizations. Retrieved from National Academy of Medicine website: https://nam.edu/perspectives-2012-ten-attributes-of-health-literate-health-care-organizations/
- Brach C. Chevarley F. M. (2008). Demographics and health care access and utilization of limited-English-proficient and English-proficient Hispanics. Retrieved from Agency for Healthcare Research and Quality website: http://meps.ahrq.gov/mepsweb/data_files/publications//rf28/rf28.pdf
- DeWalt D. A. Callahan L. F. Hawk V. H. Broucksou K. A. Hink A. Rudd R. Brach C. (2010). Health literacy universal precautions toolkit. Retrieved from Agency for Healthcare Research and Quality website: http://www.ahrq.gov/qual/literacy/healthliteracytoolkit.pdf
- Howard D. H. (2004). The relationship between health literacy and medical costs. Retrieved from The National Academies Press website: https://www.nap.edu/read/10883/chapter/11
- Kutner M. Greenberg E. Jin Y. Paulsen C. (2006). The health literacy of America's adults: Results from the 2003 national assessment of adult literacy. Retrieved from National Center for Educational Statistics website: https://nces.ed.gov/pubsearch/pubsinfo.asp?pubid=2006483
- Marrast L. M. Zallman L. Woolhandler S. Bor D. H. McCormick D. (2014). Minority physicians' role in the care of underserved patients: Diversifying the physician workforce may be key in addressing health disparities. JAMA Internal Medicine, 174(2), 289–291. 10.1001/jamainternmed.2013.12756 [DOI] [PubMed] [Google Scholar]
- Martin L. T. Ruder T. Escarce J. J. Ghosh-Dastidar B. Sherman D. Elliott M. Lurie N. (2009). Developing predictive models of health literacy. Journal of General Internal Medicine, 24(11), 1211–1216. 10.1007/s11606-009-1105-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paasche-Orlow M. K. Schillinger D. Greene S. M. Wagner E. H. (2006). How health care systems can begin to address the challenge of limited literacy. Journal of General Internal Medicine, 21(8), 884–887. 10.1111/j.1525-1497.2006.00544.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Turner T. Cull W. L. Bayldon B. Klass P. Sanders L. M. Frintner M. P. Dreyer B. (2009). Pediatricians and health literacy: Descriptive results from a national survey. Pediatrics, 124(Suppl. 3), S299–S305. 10.1542/peds.2009-1162F [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2008). America's health literacy: Why we need accessible health information. Retrieved from http://www.health.gov/communication/literacy/default.htm
- U.S. Department of Health and Human Services. (2000). Healthy people 2010: Understanding and improving health. Retrieved from www.healthypeople.gov/2010/document/pdf/uih/2010uih.pdf
- U.S. Department of Health and Human Services. (2017). Healthy people 2020. Retrieved from https://www.healthypeople.gov/2020/topics-objectives/topic/health-communication-and-health-information-technology/objectives
- Weidmer B. A. Brach C. Hays R. D. (2012). Development and evaluation of CAHPS survey items assessing how well healthcare providers address health literacy. Medical Care, 50(Suppl. 2), S3–S11. 10.1097/MLR.0b013e3182652482 [DOI] [PMC free article] [PubMed] [Google Scholar]