Abstract
Antibody-mediated rejection (ABMR) is an important risk of allograft dysfunction in kidney transplantation. The complement system is considered to be associated with the generation of alloreative antibodies and donor-specific antibodies. However, the association of complement single nucleotide polymorphisms (SNPs) with ABMR still remained unclear. Blood samples of 199 renal transplant recipients containing 68 with ABMR and 131 with stable graft function were collected, and analyzed by next-generation sequencing with an established gene panel. High quality readout was obtained in 18 C3 SNPs, 9 C4 SNPs and 22 C5 SNPs. Concerning C3 gene polymorphisms, after being adjusted with age, sex and immunosuppressive protocols, rs10411506 and rs2230205 were found to be statistically associated with ABMR in dominant model (rs10411506: OR=2.73, 95% CIs: 1.16, 6.68, P=0.028; rs2230205: OR=2.52, 95% CIs: 1.07, 5.92, P=0.034); rs10411506, rs2230205 and rs2230201 were found different in HET model (rs10411506: OR=3.05, 95% CIs: 1.22, 7.64, P=0.017; rs2230205: OR=2.90, 95% CIs: 1.20, 7.00, P=0.018; rs2230201: OR=2.41, 95% CIs: 1.03, 5.64, P=0.042). The linkage analysis showed relatively high linkage disequilibrium among these SNPs. In addition, no significant correlation was found between C4 SNPs, or C5 SNPs, and the development of ABMR. Our study firstly identified the two SNPs (rs10411506 and rs2230205) in C3 gene were statistically correlated with ABMR in kidney transplantation. These findings may have implications for the diagnosis and prevention of ABMR.
Keywords: kidney transplantation, antibody-mediated rejection, complement, single nucleotide polymorphism, next-generation sequencing
INTRODUCTION
Kidney transplantation is the optimal therapy for patients with end-stage renal disease [1]. Despite the advancement in novel immunosuppressive agents and surgical techniques, challenges still remain in the area of maintaining long-term stable allograft function and minimizing the rejection [2]. Among these, the prevention and treatment of antibody-mediated rejection (ABMR) plays a critical role, which has been emerged as an important cause of both short-term and long-term injury to transplanted kidney [3-5]. ABMR often occurs in the presence of alloreactive antibodies or donor-specific antibodies (DSAs) and leads to the deterioration in graft function [6]. Efficient measures, such as timely monitoring of alloreative antibodies, maintaining of adequate immunosuppressive agents, have been already taken. However, even with strict adherence, the development of ABMR still persists due to the lack of knowledge in its detailed mechanisms and the sufficiently noninvasive monitoring system for renal transplant recipients [7, 8].
ABMR, also known as humoral rejection, is an important cause of short-term and long-term graft injury. The latest Banff criteria for the diagnosis of ABMR include the following three components: detectable DSA, presence of C4d deposition and histological evidence, including vasculitis and glomerulonephritis [9]. In the pathogenesis of ABMR, endothelial tissue is a key target and damage to the graft is primarily attributable to antigen-antibody complex-mediated activation of the classical complement pathway, which triggers multiple downstream processes, such as the promotion of antigen presentation, recruitment of leukocytes and the promotion of inflammatory processes [10]. Moreover, activation of the complement system in solid organ transplantation often occurs in the acute period during the initial ischemia/reperfusion phase and the subsequent adaptive immune responses, contributing to the development of ABMR [11].
The complement dependent mechanism plays a vital role in the pathogenesis of ABMR [12]. The antigen-antibody complex on graft endothelium activates the classical complement pathway, inducing complement dependent cascade [9, 13]. The complement cascade leads to the formation of membrane attack complex (MAC) which disrupts the integrity of phospholipid bilayer of cells, killing the cells [9, 13]. Complement independent mechanisms such as antibody-cell-dependent cytotoxicity (ADCC) can also be mediated by antibodies [13]. Since most of the target antigens present on the endothelium, evidence of acute (glomerulitis, peritubular capillaritis) and chronic (transplant glomerulopathy) microcirculation injury can be found in the biopsy [13]. The damage of endothelium can also lead to the formation of microthrobus, degrading the function of allograft further [9]. In the complement system, all the three pathways, including the classical, alternative and lectin pathways, lead to the activation of C3 component by C3 convertases, release of C3b opsonin, C5 converstion and eventually membrane attack complex C5b-9 formulation, which is the most critical step in the elaboration of the biological effects of the complement system [14-16]. Therefore, modulation of complement-associated reactions may well determine whether initial activation of the complement sequence eventuates in beneficial or detrimental effects for the recipients.
In recent years, some studies have focused on the influence of C3 genetic polymorphisms on outcomes of kidney transplantation, and certain C3 genotypes were identified. Among these, the role of two C3F allotypes, which are called C3F (fast) and C3S (slow), in the short-term and long-term allograft outcomes were the most genotypes reported so far. Mutations from glycine to arginine in a functional region (position 80) of C3F allotype could lead to the variant of C3S [17, 18]. This mutation is possibly associated with the ability of C3 to interact with monocyte complement receptors [19]. As an indispensable part in classical activation pathway of the complement, the fourth complement component (C4) is important in the pathogenesis of ABMR in allograft [20]. C4d is a complement split protein without biological function formed during the C4 activation and its thioester moiety enables C4d to bind endothelial cells and basement membrane with strong covalent bonding [13, 21]. Thus the detection of C4d on biopsy allograft tissues suggests the classical complement activation and the occurrence of ABMR [22]. In addition, complement 5 (C5) is a pivotal complement, which initiates the assembly of the membrane attack complex, and mediates chemotaxis of various immune cells [23]. The progression of complement activation from C3 to C5 results in a soluble cleavage product C5a, a highly potent chemoattractant and activator of neutrophils and monocytes [24]. Associated with ABMR, C5a down-regulates inhibitory FcγR and up-regulates activating FcγR by stimulating macrophages [25]. It is significant to realize that the potentially deleterious effects of the proinflammatory terminal complement component on endothelial cells are controlled by a variety of complement modulators, many of which act on the enzymatic components of C3 and C5 convertases [26]. Recently, a systematic assessment of gene polymorphisms in the complement system, including four C3 allotypes (rs7951, rs11569450, rs11569523 and rs11672613), were performed to investigate the association with graft survival, serum creatinine, delayed graft function and acute rejection of kidney transplantation, and no significant outcome was found [27]. Moreover, previous studies demonstrate that certain genetic variants of C5 are a risk factor for several immune related disorders [28, 29]. As a result, the complement system, containing C3, C4 and C5, may play a crucial role in the development of ABMR episodes; on the other hand, the effects of complement-related single nucleotide polymorphisms (SNPs) still remained largely unknown.
Next-generation sequencing (NGS) technology is a powerful and cost-effective tool for large-scale DNA sequencing, which has already changed the way we think about scientific approaches in genetic and evolutionary research [30]. Compared to conventional method, the primary advantage of NGS technology is the inexpensive production of large volumes of sequence data. Currently, NGS has been applied to an increasing number of human diseases, such as tumors, kidney diseases and obesity [31-33].
In our study, by the application of NGS technologies and comprehensive literature review of C3/C4/C5 genetic polymorphism-related studies, we designed to examine the association between reported C3 SNPs, as well as C4 and C5 SNPs, and the occurrence of ABMR in kidney transplantation in a Chinese population.
RESULTS
Baseline characteristics of renal transplant recipients
The clinical characteristics of these 199 recipients are shown in Table 1. The total incidence of ABMR was 34.17% (68 out of 199 recipients). Between two renal transplant groups, there was no significant association of PRA and HLA mismatch. In addition, no statistical difference was observed in mean age, gender or immunosuppressive protocols. Among patients in ABMR groups, we further collected ABMR-related clinical information, such as C4d scoring, histological classifications and the level of serum DSAs, and reported them in Table 1. We did not observe any significant differences (P>0.05) in age, sex, donor type and immunosuppressive protocol between the stable and ABMR group.
Table 1. Comparison of baseline characteristics between ABMR and stable subjects.
| Characteristics | Stable group | ABMR group | P value |
|---|---|---|---|
| Case number | 131 | 68 | NS |
| Age (years, mean ± SD) | 37.55±1.24 | 38.92±2.01 | NS |
| Male (%) | 62.60 | 55.88 | NS |
| Number of HLA mismatches | 3.52±0.83 | 3.41±0.76 | NS |
| PRA (%) | 0.00 | 0.00 | - |
| Immunosuppressive protocol | NS | ||
| Pred + MMF + CsA | 63 | 26 | |
| Pred + MMF + TAC | 59 | 34 | |
| Pred + MMF + CsA + SIR | 5 | 6 | |
| Pred + MMF + TAC + SIR | 4 | 2 | |
| Type of ABMR* | |||
| Acute ABMR | - | 23 | |
| Chronic active ABMR | - | 45 | |
| Grade of morphologic tissue injury* | |||
| Grade I | - | 25 | |
| Grade II | - | 33 | |
| Grade III | - | 10 | |
| C4d Scroing by IF* | |||
| C4d1 | - | 5 | |
| C4d2 | - | 17 | |
| C4d3 | - | 46 | |
| Criculating DSAs (MFI, mean ± SD) | |||
| Class I | - | 1322.15 ± 545.82 | |
| Class II | - | 1185.22 ± 650.08 |
ABMR, antibody-mediated rejection; NS, not significant; SD, standard deviation; HLA, human lymphocyte antigen; PRA, panel reactive antibody; Pred, prednisone; MMF, Mycophenolate Mofetil; CsA, Cyclosporin A; TAC, tacrolimus; SIR, sirolimus.
*The classification of ABMR are in accordance with Banff 2007 criteria.
The association of C3 genotypes and ABMR
A total of 18 reported C3 SNPs were identified using the NGS technology. No deviation from HWE was observed for any C3 polymorphism. The genotypic distributions of the determined C3 polymorphisms in both groups are shown in (Supplementary Table 1).
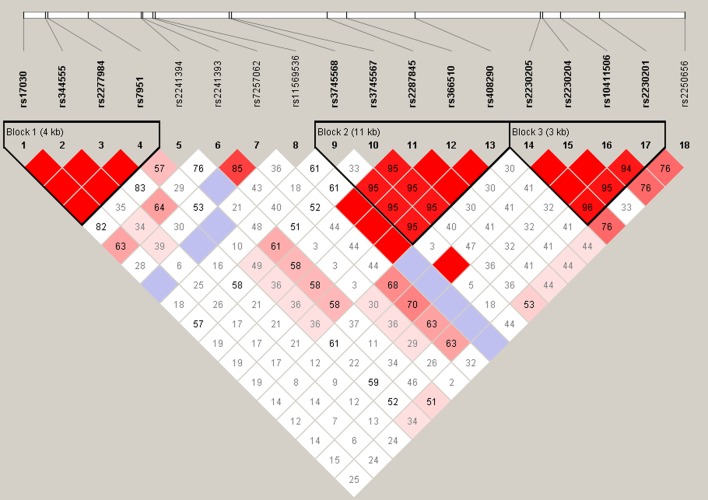
A logistic regression analysis was performed after controlling for age, sex and immunosuppressive protocols as co-variables in all five analytical models (dominant, recessive, additive, HET and HOM) to explore the alternative effects of the variants. For dominant model, rs10411506 and rs2230205 were found to be significantly associated with the occurrence of ABMR [rs10411506 (GG vs. GA+AA): OR=2.73, 95% CIs: 1.16, 6.68, P=0.028; rs2230205 (CC vs. CT+TT): OR=2.52, 95% CIs: 1.07, 5.92, P=0.034; Table 2 ]. Moreover, for HET model, statistically significant difference was observed in rs10411506, rs2230205 and rs2230201 between two groups [rs10411506 (GG vs. GA): OR=3.05, 95% CIs: 1.22, 7.64, P=0.017; rs2230205: OR=2.90, 95% CIs: 1.20, 7.00, P=0.018; rs2230201 (CC vs. CT): OR=2.41, 95% CIs: 1.03, 5.64, P=0.042; Table 2 ]. In addition, there was no statistical difference between other SNPs in C3 gene and the pathogenesis of ABMR (Table 2). Then, the SNPs of rs11569428, rs2230205, rs116528507, rs10411506, rs4807895, rs2230201 were tested for LD analysis, and the results indicate that these significant SNPs were in high LD status (Figure 1).
Table 2. Regression analysis for age-, sex- and immunosuppressive protocol-adjusted C3 genetic polymorphisms among recipients with ABMR.
| SNPs | Model | OR | 95% CIs | P value |
|---|---|---|---|---|
| rs17030 | ||||
| Additive | 1.14 | 0.74, 1.75 | 0.57 | |
| Dominant | 1.39 | 0.67, 2.89 | 0.38 | |
| Recessive | 1.02 | 0.51, 2.06 | 0.95 | |
| HET | 1.43 | 0.66, 3.10 | 0.36 | |
| HOM | 1.31 | 0.54, 3.16 | 0.55 | |
| rs344555 | ||||
| Additive | 1.01 | 0.63, 1.63 | 0.96 | |
| Dominant | 1.26 | 0.68, 2.33 | 0.46 | |
| Recessive | 0.50 | 0.15, 1.65 | 0.25 | |
| HET | 1.44 | 0.76, 2.72 | 0.27 | |
| HOM | 0.60 | 0.17, 2.06 | 0.42 | |
| rs2277984 | ||||
| Additive | 1.15 | 0.75, 1.78 | 0.52 | |
| Dominant | 1.39 | 0.67, 2.89 | 0.38 | |
| Recessive | 1.06 | 052, 2.14 | 0.87 | |
| HET | 1.41 | 0.65, 3.05 | 0.38 | |
| HOM | 1.34 | 0.55, 3.26 | 0.52 | |
| rs7951 | ||||
| Additive | 0.97 | 0.47, 2.02 | 0.94 | |
| Dominant | 0.93 | 0.42, 2.08 | 0.86 | |
| Recessive | 1.61 | 0.095, 27.33 | 0.74 | |
| HET | 0.90 | 0.39, 2.06 | 0.80 | |
| HOM | 1.58 | 0.092, 26.84 | 0.75 | |
| rs2241394 | ||||
| Additive | 1.40 | 0.53, 3.68 | 0.49 | |
| Dominant | 1.40 | 0.53, 3.68 | 0.49 | |
| rs2241393 | ||||
| Additive | 0.96 | 0.34, 2.72 | 0.94 | |
| Dominant | 1.89 | 0.40, 8.94 | 0.42 | |
| rs7257062 | ||||
| Additive | 1.03 | 0.42, 2.53 | 0.95 | |
| Dominant | 1.27 | 0.35, 4.63 | 0.72 | |
| Recessive | 0.61 | 0.061, 6.13 | 0.68 | |
| HET | 1.87 | 0.39, 9.05 | 0.44 | |
| HOM | 0.63 | 0.063, 6.27 | 0.69 | |
| rs11569536 | ||||
| Additive | 1.34 | 0.11, 16.35 | 0.82 | |
| Dominant | 1.34 | 0.11, 16.35 | 0.82 | |
| rs3745568 | ||||
| Additive | 1.48 | 0.64, 3.43 | 0.36 | |
| Dominant | 1.48 | 0.64, 3.43 | 0.36 | |
| rs3745567 | ||||
| Additive | 1.45 | 0.57, 3.67 | 0.44 | |
| Dominant | 1.45 | 0.57, 3.67 | 0.44 | |
| rs2287845 | ||||
| Additive | 1.68 | 0.88, 3.19 | 0.12 | |
| Dominant | 1.71 | 0.86, 3.39 | 0.13 | |
| Recessive | 2.68 | 0.15, 48.48 | 0.50 | |
| HET | 1.67 | 0.83, 3.35 | 0.15 | |
| HOM | 3.01 | 0.17, 54.73 | 0.46 | |
| rs366510 | ||||
| Additive | 1.68 | 0.88, 3.19 | 0.12 | |
| Dominant | 1.71 | 0.86, 3.39 | 0.13 | |
| Recessive | 2.68 | 0.15, 48.48 | 0.50 | |
| HET | 1.67 | 0.83, 3.35 | 0.15 | |
| HOM | 3.01 | 0.17, 54.73 | 0.46 | |
| rs408290 | ||||
| Additive | 1.18 | 0.80, 3.23 | 0.40 | |
| Dominant | 1.68 | 0.88, 3.23 | 0.12 | |
| Recessive | 0.93 | 0.42, 2.07 | 0.86 | |
| HET | 2.91 | 1.19, 7.16 | 0.020 | |
| HOM | 1.12 | 0.49, 2.54 | 0.79 | |
| rs2230205 | ||||
| Additive | 1.26 | 0.79, 2.01 | 0.34 | |
| Dominant | 2.52 | 1.07, 5.92 | 0.034 | |
| Recessive | 0.078 | 0.36, 1.69 | 0.53 | |
| HET | 2.90 | 1.20, 7.00 | 0.018 | |
| HOM | 1.73 | 0.61, 4.88 | 0.30 | |
| rs2230204 | ||||
| Additive | 1.08 | 0.68, 1.69 | 0.75 | |
| Dominant | 1.35 | 0.70, 2.61 | 0.37 | |
| Recessive | 0.76 | 0.31, 1.86 | 0.55 | |
| HET | 1.49 | 0.75, 2.97 | 0.26 | |
| HOM | 0.97 | 0.36, 2.59 | 0.94 | |
| rs10411506 | ||||
| Additive | 1.32 | 0.82, 2.12 | 0.26 | |
| Dominant | 2.73 | 1.12, 6.68 | 0.028 | |
| Recessive | 0.85 | 0.40, 1.82 | 0.68 | |
| HET | 3.05 | 1.22, 7.64 | 0.017 | |
| HOM | 2.02 | 0.70, 5.86 | 0.20 | |
| rs2230201 | ||||
| Additive | 1.23 | 0.77, 1.97 | 0.39 | |
| Dominant | 2.15 | 0.95, 4.90 | 0.068 | |
| Recessive | 0.82 | 0.38, 1.78 | 0.62 | |
| HET | 2.41 | 1.03, 5.64 | 0.042 | |
| HOM | 1.58 | 0.57, 4.36 | 0.38 | |
| rs2250656 | ||||
| Additive | 1.31 | 0.75, 2.30 | 0.34 | |
| Dominant | 1.25 | 0.66, 2.34 | 0.49 | |
| Recessive | 2.75 | 0.43, 17.65 | 0.29 | |
| HET | 1.17 | 0.61, 2.23 | 0.64 | |
| HOM | 2.92 | 0.45, 19.02 | 0.26 |
SNPs, single nuclear polymorphisms; OR, odds ratio; CIs: confidential intervals.
Figure 1. Linkage disequilibrium analysis of rs11569428, rs2230205, rs116528507, rs10411506, rs4807895 and rs2230201 in C3 gene.
The association of C4/C5 genotypes and ABMR
A total of 9 C4 SNPs and 22 C5 SNPs were identified. All genotype frequencies of stable group followed HWE. The genetic distributions of C4/C5 SNPs screened in ABMR and stable subjects are shown in Supplementary Tables 2 and 3.
After adjusting the age, sex and immunosuppressive protocol, results of correlations between C4 or C5 SNPs and the development of ABMR were presented in Tables 3 and 4. Unfortunately, no significant association was found between the occurrence of ABMR and polymorphisms in C4 or C5 by applying various models.
Table 3. Regression analysis of C4 genetic polymorphisms adjusted for age, sex and immunosuppressive protocols in ABMR and stable group.
| Position | Model | OR | 95% CIs | P value |
|---|---|---|---|---|
| chr6:31963786 | ||||
| Additive | 0.73 | 0.24, 2.27 | 0.59 | |
| Dominant | 0.77 | 0.23, 2.56 | 0.67 | |
| chr6:31964228 | ||||
| Additive | 1.01 | 0.44, 2.36 | 0.97 | |
| Dominant | 1.17 | 0.46, 2.97 | 0.75 | |
| chr6:31964391 | ||||
| Additive | 2.08 | 0.12, 36.64 | 0.62 | |
| Dominant | 2.08 | 0.12, 36.64 | 0.62 | |
| chr6:31964584 | ||||
| Additive | 1.49 | 0.62, 3.59 | 0.38 | |
| Dominant | 1.49 | 0.62, 3.59 | 0.38 | |
| chr6:31994974 | ||||
| Additive | 1.7 | 0.67, 4.31 | 0.26 | |
| Dominant | 1.7 | 0.67, 4.31 | 0.26 | |
| chr6:31996524 | ||||
| Additive | 1.03 | 0.57, 1.86 | 0.94 | |
| Dominant | 1.30 | 0.65, 2.59 | 0.46 | |
| chr6:31996966 | ||||
| Additive | 1.07 | 0.58, 1.99 | 0.83 | |
| Dominant | 1.03 | 0.51, 2.09 | 0.93 | |
| Recessive | 1.59 | 0.21, 12.02 | 0.65 | |
| HOM | 1.59 | 0.21, 12.15 | 0.65 | |
| HET | 1.00 | 0.48, 2.05 | 0.99 | |
| chr6:31997321 | ||||
| Additive | 0.78 | 0.14, 4.29 | 0.78 | |
| Dominant | 0.78 | 0.14, 4.29 | 0.78 | |
| chr6:31997401 | ||||
| Additive | 0.98 | 0.52, 1.82 | 0.94 | |
| Dominant | 1.01 | 0.53, 1.90 | 0.99 |
ABMR, antibody-mediated rejection; OR, odds ratio; CIs: confidential intervals.
Table 4. Regression analysis for age-, sex- and immunosuppressive protocol-adjusted C5 genetic polymorphisms among recipients with ABMR.
| SNPs | Model | OR | 95% CIs | P value |
|---|---|---|---|---|
| rs76339932 | ||||
| Additive | 0.93 | 0.26, 3.27 | 0.90 | |
| Dominant | 0.93 | 0.26, 3.27 | 0.90 | |
| rs12237774 | ||||
| Additive | 0.92 | 0.52, 1.63 | 0.78 | |
| Dominant | 0.92 | 0.47, 1.79 | 0.81 | |
| Recessive | 0.83 | 0.14, 4.89 | 0.83 | |
| HET | 0.94 | 0.47, 1.87 | 0.85 | |
| HOM | 0.81 | 0.13, 4.85 | 0.82 | |
| rs2300931 | ||||
| Additive | 1.62 | 0.82, 3.15 | 0.16 | |
| Dominant | 1.59 | 0.74, 3.37 | 0.23 | |
| Recessive | 4.42 | 0.36, 53.99 | 0.24 | |
| HET | 1.44 | 0.65, 3.16 | 0.36 | |
| HOM | 4.69 | 0.38, 57.88 | 0.23 | |
| rs10985112 | ||||
| Additive | 1.03 | 0.29, 3.64 | 0.96 | |
| Dominant | 1.03 | 0.29, 3.64 | 0.96 | |
| rs2269066 | ||||
| Additive | 1.05 | 0.60, 1.81 | 0.88 | |
| Dominant | 1.12 | 0.59, 2.13 | 0.73 | |
| Recessive | 0.71 | 0.13, 3.94 | 0.69 | |
| HET | 1.17 | 0.60, 2.29 | 0.64 | |
| HOM | 0.74 | 0.13, 4.19 | 0.74 | |
| rs41260544 | ||||
| Additive | 1.44 | 0.38, 5.44 | 0.59 | |
| Dominant | 1.44 | 0.38, 5.44 | 0.59 | |
| rs117287858 | ||||
| Additive | 2.13 | 0.29, 15.88 | 0.46 | |
| Dominant | 2.13 | 0.29, 15.88 | 0.46 | |
| rs2230212 | ||||
| Additive | 0.75 | 0.31, 1.78 | 0.51 | |
| Dominant | 0.75 | 0.31, 1.78 | 0.51 | |
| rs41311867 | ||||
| Additive | 1.44 | 0.38, 5.44 | 0.59 | |
| Dominant | 1.44 | 0.38, 5.44 | 0.59 | |
| rs187517049 | ||||
| Additive | 2.73 | 0.23, 31.84 | 0.42 | |
| Dominant | 2.73 | 0.23, 31.84 | 0.42 | |
| rs12683026 | ||||
| Additive | 1.44 | 0.38, 5.44 | 0.59 | |
| Dominant | 1.44 | 0.38, 5.44 | 0.59 | |
| rs10985122 | ||||
| Additive | 1.75 | 0.41, 7.47 | 0.45 | |
| Dominant | 1.75 | 0.41, 7.47 | 0.45 | |
| rs41309856 | ||||
| Additive | 1.23 | 0.34, 4.44 | 0.75 | |
| Dominant | 1.23 | 0.34, 4.44 | 0.75 | |
| rs144465545 | ||||
| Additive | 3.27 | 0.52, 20.59 | 0.21 | |
| Dominant | 3.27 | 0.52, 20.59 | 0.21 | |
| rs41309850 | ||||
| Additive | 1.23 | 0.34, 4.44 | 0.75 | |
| Dominant | 1.23 | 0.34, 4.44 | 0.75 | |
| rs181763824 | ||||
| Additive | 0.64 | 0.06, 6.55 | 0.71 | |
| Dominant | 0.64 | 0.06, 6.55 | 0.71 | |
| rs2230214 | ||||
| Additive | 1.23 | 0.34, 4.44 | 0.75 | |
| Dominant | 1.23 | 0.34, 4.44 | 0.75 | |
| rs10985126 | ||||
| Additive | 1.08 | 0.65, 1.77 | 0.77 | |
| Dominant | 1.15 | 0.62, 2.15 | 0.66 | |
| Recessive | 0.90 | 0.25, 3.20 | 0.87 | |
| HET | 1.19 | 0.62, 2.30 | 0.60 | |
| HOM | 0.96 | 0.26, 3.48 | 0.95 | |
| rs10985127 | ||||
| Additive | 1.08 | 0.65, 1.77 | 0.77 | |
| Dominant | 1.15 | 0.62, 2.15 | 0.66 | |
| Recessive | 0.90 | 0.25, 3.20 | 0.87 | |
| HET | 1.19 | 0.62, 2.30 | 0.60 | |
| HOM | 0.96 | 0.26, 3.48 | 0.95 | |
| rs28426093 | ||||
| Additive | 1.85 | 0.82, 4.15 | 0.14 | |
| Dominant | 1.57 | 0.59, 4.18 | 0.37 | |
| rs10818499 | ||||
| Additive | 1.14 | 0.77, 1.70 | 0.51 | |
| Dominant | 1.54 | 0.81, 2.92 | 0.19 | |
| Recessive | 0.89 | 0.42, 1.85 | 0.75 | |
| HET | 1.81 | 0.89, 3.67 | 0.10 | |
| HOM | 1.19 | 0.52, 2.70 | 0.69 | |
| rs17216529 | ||||
| Additive | 0.89 | 0.51, 1.54 | 0.67 | |
| Dominant | 0.94 | 0.49, 1.81 | 0.86 | |
| Recessive | 0.52 | 0.10, 2.78 | 0.45 | |
| HET | 1.02 | 0.52, 2.03 | 0.95 | |
| HOM | 0.53 | 0.10, 2.83 | 0.46 |
SNPs, single nuclear polymorphisms; OR, odds ratio; CIs: confidential intervals.
DISCUSSION
In this study, we investigated the relationships between reported C3 SNPs, as well as C4 and C5 SNPs, and the development of ABMR in renal transplant recipients. Our results showed that rs10411506, rs2230205 and rs2230201 located in C3 gene, especially rs10411506 and rs2230205, were statistically associated with an increased risk of post-transplant ABMR following kidney transplantation. This is the first study to explore the presence and role of complement polymorphisms in ABMR after kidney transplantation.
As an important molecular in innate immune system, C3 is the most abundant component of the complement pathways, which has a great impact on the downstream signals and activities [34]. C3 component and its regulators are well recognized as the crucial factors in the susceptibility to immune-related diseases. Furthermore, multiple studies have shown that C3 SNPs is associated with the pathogenesis of various diseases, such as age-related macular degeneration (AMD), ocular Behcet’s disease (BD), Vogt-Koyanagi-Harada syndrome (VKH) and chronic hepatitis C infection [28, 35, 36]. Among these various studies, the potential role of rs10411506 and rs2230205 were only studied in the pathogenesis of AMD in Chinese population, and the results showed no significant association of rs10411506 and rs2230205 with AMD [35]. However, our study showed that these two SNPs appeared to be an important risk of the ABMR in kidney transplantation. Moreover, recipients carrying with rs10411506 GG genotype were less susceptible to the occurrence of ABMR post-transplantation when compared with those with A allele. Similarly, the rs2230205 CC genotype was found to protect the recipients from experiencing ABMR. Besides, we also found that C3 rs2230201 SNP was statistically associated with the development of ABMR in HET model, which was consistent with previous studies conducted in ocular BD and VKH syndrome, chronic hepatitis C infection and systemic lupus erythematosus [28, 36, 37]. Nevertheless, considering to the negative results of additive model, dominant model and recessive model, the relative relationship of rs2230201 SNP and ABMR in kidney transplantation by HET model was less convincing when compared with rs10411506 and rs2230205. The linkage analysis further identified the high LD among rs10411506, rs2230205 and rs2230201, which failed to perform the reconstruction of allotype analysis. Given that introns are usually several short sequences that regulate the expression of C3, the rs10411506 GG genotype and rs2230205 CC genotype may have essential impact on the regulation of C3 protein, thus contributing to the relatively lower risk of ABMR in kidney transplantation [38].
In our study, we failed to observe the significant correlation between C4/C5 SNPs and post-transplant ABMR. SNPs in C4 were considered to be responsible for the differences between C4A and C4B isotypes, Rodgers and Chido antigenic determinants and to be associated with several autoimmune diseases [39]. A genome-wide association study conducted in healthy Chinese found eight SNPs resided in a 2-Mb MHC region on chromosome 6p21.3 region where RCCX module situates related to copy numbers of C4 gene and one SNP (rs2857009) independently affected the concentration of C4 level in serum [40]. Pertaining to correlations between C4 variations and kidney transplantation, recent studies concentrated on gene copy number variations (CNVs) of C4 and long term graft survival and suggested a possibly better prognosis in patients with low dose of C4 gene [41]. The available studies indicate the possibility that C4 SNPs have influence on CNVs of C4 or directly affect the expression of C4, thus contributing to the potential regulation in classical complement pathway and changing the chance of ABMR occurrence.
Recently, JC Jeong et al. [23] carried out the systematic assessment of the complement gene polymorphisms, including seven SNPs in C5 gene (rs12237774, rs2159776, rs17611, rs25681, rs2241004, rs10985126 and rs10818500) and one SNP (rs10404456) in the C5aR gene, on the kidney transplant outcomes, showing that the GGCG allotype of C5 in both recipients and donors was associated with lower renal allograft, whereas C5aR genotypes of recipients were not associated with acute rejection, and there was also no statistically significant association between donor C5/C5aR genotypes and acute rejection function [42]. Importantly, this study focused on the long-term outcomes of renal transplant and acute rejection, instead of the subgroup analysis of ABMR from the acute rejection, which is more correlated with the activation and progress of the complement system. However, being restricted with the collected samples, we could not perform quantitative evaluation of serum C5 in two groups to validate our outcomes in genetic polymorphisms, which requires further prospective research.
Recent study conducted by Ermini [27] focused on the influence of SNPs in complement system in the short-term and long-term outcomes of renal transplant, including delayed graft function, acute rejection, graft survival and serum creatinine, instead of the subgroup analysis of ABMR from the acute rejection, which is more correlated with the activation and progress of the complement system. Nevertheless, the case number of eligible recipients in ABMR and stable groups of our transplant center is limited, leading to the potential bias of our outcomes. Therefore, a large-scale, multi-center and well-designed study of the association of C3 SNPs and ABMR in renal transplant recipients should be conducted in the future.
In summary, we show here for the first time that the rs10411506 and rs2230205 in C3 gene are statistically correlated with the development of ABMR in renal transplant recipients, and no significant relationship of C4 or C5 SNPs were observed during the episodes of post-transplant ABMR. These findings may have implications for the diagnosis and prevention of ABMR, contributing to the promotion of the graft survival and patients’ life quality in kidney transplantation.
MATERIALS AND METHODS
Ethics statement
The study protocol was in accordance with the ethical standards of the Declarations of Helsinki and Istanbul. Being limited to the living-related transplantation of kidney tissues to their lineal or collateral relative not beyond the third degree of kinship or the cadaveric allograft donors of cardiac death (DCD), the protocol of this study was approved by the local Ethics Committee of the First Affiliated Hospital with Nanjing Medical University, and written informed consent was obtained from all transplant recipients. None of the transplant donors were from a vulnerable population, and all donors or next of kin freely provided written informed consent.
Study design and subjects
Study design
This was a 12-month, retrospective, case-control trial containing 199 renal transplant recipients who underwent kidney transplantation between February 1st, 2008 and December 1st, 2015 in renal transplant center of the First Affiliated Hospital with Nanjing Medical University. This study was designed to investigate the distributions of C3/C4/C5 SNPs between patients with period of ABMR and stable allograft function. The inclusion criteria to select the patients from stable group were as follows: [1]. The follow-up duration was longer than at least six months, and had never experienced the period of acute rejection, delayed graft dysfunction (DGF) or opportunistic infection; [2]. The concentration of serum creatinine (Scr) was lower than 120 μmol/L (1.36 mg/dl) for at least three months at the time of enrollment; [3]. Patients aged from 18 years old to 60 years old. Patients with following exclusive criteria were excluded in stable group: [1]. Patients aged less than 18 years old or older than 60 years old; [2]. History of acute rejection, DGF or opportunistic infection; [3]. Fluctuation of Scr over than 120 μmol/L (1.36 mg/dl) during the last three months of enrollment; [4]. Pregnant women and active HIV infection; [5]. Chronic lung disease requiring supplemental oxygen therapy. To enroll patients into the ABMR group, patients with significant clinical characteristics, such as an increase in serum creatinine level by 20% from baseline (not attributable to other cases) and overloaded urine protein, were required to perform the indication allograft biopsy immediately before the administration of high-dose steroids therapy. The diagnostic criteria of ABMR were mainly based on the comprehensive histological examination according to Banff 07 classification [43].
Data collection
Medical records were critically reviewed and related data, including age, gender, transplant date, duration of transplantation, transplant times, immunosuppressive protocol, were extracted by at least two clinicians for patient selection. Data on panel reactive antibody (PRA) and human leukocyte antigen (HLA) mismatch during pre-transplant period were also collected.
Subjects
Intravenous infusion of 500 mg/d of methylprednisolone was used during the surgery and up until 2 days after the operation. Then the dosage was reduced to 400 mg, 300 mg, 200 mg and 80 mg each subsequent day, followed by prednisone 30 mg/d as a maintenance therapy. In addition, Basiliximab (20 mg) was intravenously used at 30 minutes before the operation and the fourth day after the operation, respectively. All recipients received a three-drug or four-drug immunosuppressive regimen: Cyclosporin A (CsA) (n=100) or tacrolimus (n=99) in combination with mycophenolate mofetil (MMF) and prednisone, with or without sirolimus (n=17). The dosage of CsA and tacrolimus was started at 8 mg/kg/d and 0.2mg/kg/d, respectively, and then adjusted according to results of therapeutic drug monitoring the serum creatinine levels. A dosage of 200 mg/d of intravenous methylprednisolone was adopted for ABMR episodes with three to five days.
Sample collection, preparation and NGS
Peripheral blood samples (2ml) from each recipient included in our study were collected with BD Vacutainer tubes containing sodium heparin when they were admitted to our center before the renal biopsy. Then, each collected blood sample was immediately transferred to the laboratory and stored at -80°C. The DNA of subjects was extracted from collected peripheral blood samples using QIAmp DNA Mini Kit (Qiagen, Hilden, Germany). Quantitative detection of concentration and purity of genomic DNA (gDNA) was performed by NanoDrop ND2000 (Thermo, MA, USA), while the gene integrity was tested by agarose gel electrophoresis. Requirements for acceptable gDNA were as follows: total mass ≥1μg, absorbance ratio A260/A280 at ≥ 1.80 and ≤ 2.0. Then a pool containing upstream and downstream oligonucleotides specific to the targeted regions of interest was hybrids to the gDNA samples. Then gDNA was fragmented using a Bioruptor Interrupt instrument (Diagenode, Belgium) and quantitative detection was performed to ensure average fragment size of 150bp to 250bp. Fragmentation was followed by end repair, dA tailing, and sequencing adaptor ligation by ABI 9700 PCR instrument (ABI, USA). The adapter-ligated DNA was amplified by selective, limited-cycle PCR for 5 cycles and then quantitatively analyzed using Qubit dsDNA HS Assay Kit (Invitrogen, USA). Prepared library (750ng) was hybridized with 11μl hybridization block (Allwegene, China), 20μl hybridization buffer (Allwegene, China) and a mix of 5μl RNase block (Invitrogen, USA) and 2μl Probe (Allwegene, China) for overnight (at least 8-16h) at 65°C. The hybridized products were mixed with 200μl nabeads MyOne Streptavidin T1 magnetic beads (Invitrogen, USA) for 30 min at room temperature. After two times of washing by wash buffer (Allwegene, China), the mixture was amplified for 16 PCR cycles and quantitatively assessed using Qubit dsDNA HS Assay Kit (Invitrogen, USA). Captured libraries were denatured and loaded onto an Illumina cBot instrument at 12 to 16pmol/L for cluster generation according to the manufacturer’s instructions. Up to 20 WUCaMP libraries were sequenced per HiSeq lane. A PhiX control (Illumina) was added to lane 8 of each flowcell.
Analysis of NGS data
Sequencing data, such as the number of altered chromosomes, genomic alternation information and the determination of the depth of sequencing coverage, were analyzed. All analyzed were based on the human reference sequence UCSC build hg19 (NCBI build 37.2) using the Burrows-Wheeler Aligner (BWA) [44]. Local alignment and duplication removal were completed by the application of the Genome Analysis Tool Kit (GATK) and Picard software. Detection of SNPs was performed using dbSNP 132. Damaging or deleterious SNPs were predicted using the Gemini software, and prediction tools, including sorting intolerant from tolerant (SIFT) and polymorphism phenotyping (PolyPhen) were used for the analysis of all human non-synonymous SNPs. In addition, putative somatic variant calls were detected with two separate programs, MuTect 1.1.5 and VarScan 2.3.6 softwares, pairing each sample with its matched blood.
Statistical analysis
Hardy-Weinberg equilibrium (HWE) was analyzed using gene frequencies obtained by a single gene counting. Chi-square test was used to compare observed and expected values. Genotype association analysis was performed using dominant model (minor allele homozygotes plus heterozygotes vs. major allele homozygotes), recessive (minor allele homozygotes vs. heterozygotes plus major homozygotes), additive model (major homozygotes vs. heterozygotes vs. minor homozygotes), HET model (major homozygotes vs. heterozygotes) and HOM model (major homozygotes vs. minor homozygotes). Genotypic frequencies comparisons between control and ABMR groups were assessed by the chi-square test. In addition, we explored linkage disequilibrium (LD) blocks using Haploview version 4.2 software. Odds ratios (OR) and 95% confidence intervals (95% CIs) were calculated by SPSS 13.0 software (SPSS Inc., Chicago, IL, USA). P<0.05 was considered significant. The OR provides an effect estimate, the value of which less than 1 is considered as a protective effect, whereas the value more than 1 is associated with an increased risk. In addition, the genotypic distributions of the C3 SNPs in ABMR recipients and in stable subjects were analyzed with logistic regression models adjusted for age, sex and immunosuppressive protocol.
SUPPLEMENTARY MATERIALS TABLES
Abbreviations
- ABMR
antibody-mediated rejection
- HLA
human leukocyte antigens
- MHC
major histocompatibility complex
- DSA
donor-specific antibodies
- PRA
panel reactive antibody
- SNP
single nucleotide polymorphisms
- HWE
Hardy-Weinberg equilibrium
- NGS
next-generation sequencing
- AMD
age-related macular degeneration
- BD
Behcet’s disease
- VKH
Vogt-Koyanagi-Harada syndrome
- CNV
copy number variations
- DCD
donors of cardiac death
- DGF
delayed graft dysfunction
- Scr
serum creatinine
- CsA
Cyclosporin A
- MMF
mycophenolate mofetil
- SIFT
sorting intolerant from tolerant
- GATK
Genome Analysis Tool Kit
- LD
linkage disequilibrium
- OR
odds ratios
- 95%CIs
95% confidence intervals
Footnotes
Author contributions
Zijie Wang: genetic analysis and manuscript preparation;
Haiwei Yang: genetic analysis and study design;
Miao Guo: genetic analysis and data interpretation;
Zhijian Han: sample collection;
Jun Tao: sample collection;
Hao Chen: sample collection and data analysis;
Yuqiu Ge: data analysis;
Chunchun Zhao: data interpretation;
Chuanjian Suo: sample collection;
Ke Wang: data analysis;
Shuhui Si: genetic analysis;
Ruoyun Tan: manuscript preparation and foundation collection;
Jifu Wei: study design and foundation collection;
Min Gu: study design, manuscript preparation and foundation collection;
All authors reviewed this manuscript.
CONFLICTS OF INTEREST
The authors have declared that no competing interests exist.
FUNDING
This work was supported by the National Natural Science Foundation of China [grant numbers 81570676, 81100532, 81470981], the Science and Education Health Project of Jiangsu Province for Important Talent [grant number RC2011055], the “333 High Level Talents Project” in Jiangsu Province, China [grant numbers BRA2015469, BRA2016514 (2011 and 2013)], the Standardized Diagnosis and Treatment Research Program of Key Diseases in Jiangsu Province, China [grant number BE2016791], the Open Project Program of Health Department of Jiangsu Province, China [grant number JSY-2-2016-099], the Jiangsu Province Six Talents Peak from Department of Human Resources, Social Security Office of Jiangsu Province, China [grant numbers 2010WSN-56, 2011-WS-033], the General Program of Health Department of Jiangsu Province, China [grant number H2009907], and the Priority Academic Program Development of Jiangsu Higher Education Institutions [grant number JX10231801]. National Key R&D Plan for Precision Medicine [grant number 2017YFC0910001].
REFERENCES
- 1.Wang Z, Han Z, Tao J, Lu P, Liu X, Wang J, Wu B, Huang Z, Yin C, Tan R, Gu M. Clinical efficacy and safety of pamidronate therapy on bone mass density in early post-renal transplant period: a meta-analysis of randomized controlled trials. PLoS One. 2014;9:e108106. doi: 10.1371/journal.pone.0108106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liu X, Liu K, Wang Z, Liu C, Han Z, Tao J, Lu P, Wang J, Wu B, Huang Z, Yin C, Gu M, Tan R. Advanced glycation end products accelerate arteriosclerosis after renal transplantation through the AGE/RAGE/ILK pathway. Exp Mol Pathol. 2015;99:312–9. doi: 10.1016/j.yexmp.2015.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Terasaki PI, Cai J. Human leukocyte antigen antibodies and chronic rejection: from association to causation. Transplantation. 2008;86:377–83. doi: 10.1097/TP.0b013e31817c4cb8. [DOI] [PubMed] [Google Scholar]
- 4.Colvin RB. Antibody-mediated renal allograft rejection: diagnosis and pathogenesis. J Am Soc Nephrol. 2007;18:1046–56. doi: 10.1681/ASN.2007010073. [DOI] [PubMed] [Google Scholar]
- 5.Magil AB, Tinckam K. Monocytes and peritubular capillary C4d deposition in acute renal allograft rejection. Kidney Int. 2003;63:1888–93. doi: 10.1046/j.1523-1755.2003.00921.x. [DOI] [PubMed] [Google Scholar]
- 6.Halloran PF, Famulski KS, Chang J. A probabilistic approach to histologic diagnosis of antibody-mediated rejection in kidney transplant biopsies. Am J Transplant. 2017;17:129–39. doi: 10.1111/ajt.13934. [DOI] [PubMed] [Google Scholar]
- 7.Ng YW, Singh M, Sarwal MM. Antibody-mediated rejection in pediatric kidney transplantation: pathophysiology, diagnosis, and management. Drugs. 2015;75:455–72. doi: 10.1007/s40265-015-0369-y. [DOI] [PubMed] [Google Scholar]
- 8.Naesens M, Khatri P, Li L, Sigdel TK, Vitalone MJ, Chen R, Butte AJ, Salvatierra O, Sarwal MM. Progressive histological damage in renal allografts is associated with expression of innate and adaptive immunity genes. Kidney Int. 2011;80:1364–76. doi: 10.1038/ki.2011.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kim M, Martin ST, Townsend KR, Gabardi S. Antibody-mediated rejection in kidney transplantation: a review of pathophysiology, diagnosis, and treatment options. Pharmacotherapy. 2014;34:733–44. doi: 10.1002/phar.1426. [DOI] [PubMed] [Google Scholar]
- 10.Muduma G, Odeyemi I, Smith-Palmer J, Pollock RF. Review of the clinical and economic burden of antibody-mediated rejection in renal transplant recipients. Adv Ther. 2016;33:345–56. doi: 10.1007/s12325-016-0292-y. [DOI] [PubMed] [Google Scholar]
- 11.Sacks SH, Zhou W. The role of complement in the early immune response to transplantation. Nat Rev Immunol. 2012;12:431–42. doi: 10.1038/nri3225. [DOI] [PubMed] [Google Scholar]
- 12.Colvin RB, Smith RN. Antibody-mediated organ-allograft rejection. Nat Rev Immunol. 2005;5:807–17. doi: 10.1038/nri1702. [DOI] [PubMed] [Google Scholar]
- 13.Puttarajappa C, Shapiro R, Tan HP. Antibody-mediated rejection in kidney transplantation: a review. J Transplant. 2012;2012:193724. doi: 10.1155/2012/193724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koscielska-Kasprzak K, Bartoszek D, Myszka M, Zabinska M, Klinger M. The complement cascade and renal disease. Arch Immunol Ther Exp (Warsz) 2014;62:47–57. doi: 10.1007/s00005-013-0254-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Walport MJ. Complement. First of two parts. N Engl J Med. 2001;344:1058–66. doi: 10.1056/NEJM200104053441406. [DOI] [PubMed] [Google Scholar]
- 16.Fearon DT, Daha MR, Strom TB, Weiler JM, Carpenter CB, Austen KF. Pathways of complement activation in membranoproliferative glomerulonephritis and allograft rejection. Transplant Proc. 1977;9:729–39. [PubMed] [Google Scholar]
- 17.Teisberg P. High voltage agarose gel electrophoresis in the study of C 3 polymorphism. Vox Sang. 1970;19:47–56. doi: 10.1111/j.1423-0410.1970.tb01494.x. [DOI] [PubMed] [Google Scholar]
- 18.Alper CA, Johnson AM, Birtch AG, Moore FD. Human C'3: evidence for the liver as the primary site of synthesis. Science. 1969;163:286–8. doi: 10.1126/science.163.3864.286. [DOI] [PubMed] [Google Scholar]
- 19.Arvilommi H. Capacity of complement c3 phenotypes to bind on to mononuclear cells in man. Nature. 1974;251:740–1. doi: 10.1038/251740a0. [DOI] [PubMed] [Google Scholar]
- 20.Murata K, Baldwin WM., 3rd Mechanisms of complement activation, C4d deposition, and their contribution to the pathogenesis of antibody-mediated rejection. Transplant Rev (Orlando) 2009;23:139–50. doi: 10.1016/j.trre.2009.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nickeleit V, Mihatsch MJ. Kidney transplants, antibodies and rejection: is C4d a magic marker? Nephrol Dial Transplant. 2003;18:2232–9. doi: 10.1093/ndt/gfg304. [DOI] [PubMed] [Google Scholar]
- 22.Collins AB, Schneeberger EE, Pascual MA, Saidman SL, Williams WW, Tolkoff-Rubin N, Cosimi AB, Colvin RB. Complement activation in acute humoral renal allograft rejection: diagnostic significance of C4d deposits in peritubular capillaries. J Am Soc Nephrol. 1999;10:2208–14. doi: 10.1681/ASN.V10102208. [DOI] [PubMed] [Google Scholar]
- 23.Jeong JC, Hwang YH, Kim H, Ro H, Park HC, Kim YJ, Kim MG, Ha J, Park MH, Chae DW, Ahn C, Yang J. Association of complement 5 genetic polymorphism with renal allograft outcomes in Korea. Nephrol Dial Transplant. 2011;26:3378–85. doi: 10.1093/ndt/gfr025. [DOI] [PubMed] [Google Scholar]
- 24.Coulthard LG, Woodruff TM. Is the complement activation product C3a a proinflammatory molecule? Re-evaluating the evidence and the myth. J Immunol. 2015;194:3542–8. doi: 10.4049/jimmunol.1403068. [DOI] [PubMed] [Google Scholar]
- 25.Konrad S, Engling L, Schmidt RE, Gessner JE. Characterization of the murine IgG Fc receptor III and IIB gene promoters: a single two-nucleotide difference determines their inverse responsiveness to C5a. J Biol Chem. 2007;282:37906–12. doi: 10.1074/jbc.M707937200. [DOI] [PubMed] [Google Scholar]
- 26.Baldwin WM, 3rd, Valujskikh A, Fairchild RL. Mechanisms of antibody-mediated acute and chronic rejection of kidney allografts. Curr Opin Organ Transplant. 2016;21:7–14. doi: 10.1097/MOT.0000000000000262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ermini L, Weale ME, Brown KM, Mesa IR, Howell WM, Vaughan R, Chowdhury P, Sacks SH, Sheerin NS. Systematic assessment of the influence of complement gene polymorphisms on kidney transplant outcome. Immunobiology. 2016;221:528–34. doi: 10.1016/j.imbio.2015.12.006. [DOI] [PubMed] [Google Scholar]
- 28.Xu D, Hou S, Zhang J, Jiang Y, Kijlstra A, Yang P. Copy number variations and gene polymorphisms of complement components in ocular Behcet's disease and Vogt-Koyanagi-Harada syndrome. Sci Rep. 2015;5:12989. doi: 10.1038/srep12989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Giles JL, Choy E, van den Berg C, Morgan BP, Harris CL. Functional analysis of a complement polymorphism (rs17611) associated with rheumatoid arthritis. J Immunol. 2015;194:3029–34. doi: 10.4049/jimmunol.1402956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Metzker ML. Sequencing technologies - the next generation. Nat Rev Genet. 2010;11:31–46. doi: 10.1038/nrg2626. [DOI] [PubMed] [Google Scholar]
- 31.Kumondai M, Hosono H, Orikasa K, Arai Y, Arai T, Sugimura H, Ozono S, Sugiyama T, Takayama T, Sasaki T, Hirasawa N, Hiratsuka M. CYP2A13 genetic polymorphisms in relation to the risk of bladder cancer in Japanese smokers. Biol Pharm Bull. 2016;39:1683–6. doi: 10.1248/bpb.b16-00422. [DOI] [PubMed] [Google Scholar]
- 32.Paolini B, Maltese PE, Del Ciondolo I, Tavian D, Missaglia S, Ciuoli C, Zuntini M, Cecchin S, Bertelli M, Pompucci G. Prevalence of mutations in LEP, LEPR, and MC4R genes in individuals with severe obesity. Genet Mol Res. 2016 doi: 10.4238/gmr.15038718. [DOI] [PubMed] [Google Scholar]
- 33.Edrees BM, Athar M, Al-Allaf FA, Taher MM, Khan W, Bouazzaoui A, Al-Harbi N, Safar R, Al-Edressi H, Alansary K, Anazi A, Altayeb N, Ahmed MA, Abduljaleel Z. Next-generation sequencing for molecular diagnosis of autosomal recessive polycystic kidney disease. Gene. 2016;591:214–26. doi: 10.1016/j.gene.2016.07.021. [DOI] [PubMed] [Google Scholar]
- 34.Mullins RF, Russell SR, Anderson DH, Hageman GS. Drusen associated with aging and age-related macular degeneration contain proteins common to extracellular deposits associated with atherosclerosis, elastosis, amyloidosis, and dense deposit disease. FASEB J. 2000;14:835–46. [PubMed] [Google Scholar]
- 35.Pei XT, Li XX, Bao YZ, Yu WZ, Yan Z, Qi HJ, Qian T, Xiao HX. Association of c3 gene polymorphisms with neovascular age-related macular degeneration in a chinese population. Curr Eye Res. 2009;34:615–22. doi: 10.1080/02713680903003484. [DOI] [PubMed] [Google Scholar]
- 36.Chowdhury SJ, Karra VK, Gumma PK, Bharali R, Kar P. rs2230201 polymorphism may dictate complement C3 levels and response to treatment in chronic hepatitis C patients. J Viral Hepat. 2015;22:184–91. doi: 10.1111/jvh.12280. [DOI] [PubMed] [Google Scholar]
- 37.Miyagawa H, Yamai M, Sakaguchi D, Kiyohara C, Tsukamoto H, Kimoto Y, Nakamura T, Lee JH, Tsai CY, Chiang BL, Shimoda T, Harada M, Tahira T, et al. Association of polymorphisms in complement component C3 gene with susceptibility to systemic lupus erythematosus. Rheumatology (Oxford) 2008;47:158–64. doi: 10.1093/rheumatology/kem321. [DOI] [PubMed] [Google Scholar]
- 38.Rodriguez-Trelles F, Tarrio R, Ayala FJ. Origins and evolution of spliceosomal introns. Annu Rev Genet. 2006;40:47–76. doi: 10.1146/annurev.genet.40.110405.090625. [DOI] [PubMed] [Google Scholar]
- 39.Blanchong CA, Chung EK, Rupert KL, Yang Y, Yang Z, Zhou B, Moulds JM, Yu CY. Genetic, structural and functional diversities of human complement components C4A and C4B and their mouse homologues, Slp and C4. Int Immunopharmacol. 2001;1:365–92. doi: 10.1016/s1567-5769(01)00019-4. [DOI] [PubMed] [Google Scholar]
- 40.Yang X, Sun J, Gao Y, Tan A, Zhang H, Hu Y, Feng J, Qin X, Tao S, Chen Z, Kim ST, Peng T, Liao M, et al. Genome-wide association study for serum complement C3 and C4 levels in healthy Chinese subjects. PLoS Genet. 2012;8:e1002916. doi: 10.1371/journal.pgen.1002916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bay JT, Schejbel L, Madsen HO, Sorensen SS, Hansen JM, Garred P. Low C4 gene copy numbers are associated with superior graft survival in patients transplanted with a deceased donor kidney. Kidney Int. 2013;84:562–9. doi: 10.1038/ki.2013.195. [DOI] [PubMed] [Google Scholar]
- 42.Gunesacar R, Opelz G, Erken E, Dohler B, Ruhenstroth A, Susal C. Complement C5a receptor gene 450 C/T polymorphism in renal transplant recipients: association of the CT genotype with graft outcome. Tissue Antigens. 2015;85:104–7. doi: 10.1111/tan.12495. [DOI] [PubMed] [Google Scholar]
- 43.Solez K, Colvin RB, Racusen LC, Haas M, Sis B, Mengel M, Halloran PF, Baldwin W, Banfi G, Collins AB, Cosio F, David DS, Drachenberg C, et al. Banff 07 classification of renal allograft pathology: updates and future directions. Am J Transplant. 2008;8:753–60. doi: 10.1111/j.1600-6143.2008.02159.x. [DOI] [PubMed] [Google Scholar]
- 44.Li H, Durbin R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics. 2010;26:589–95. doi: 10.1093/bioinformatics/btp698. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.