Abstract
[99mTc]Tc-Sestamibi (MIBI) is an increasingly used tool for evaluation of thyroid nodules. However, there is a lack of evidence about the accuracy of this method in the European population. The aim of this study was to assess the utility of MIBI for the differentiation of thyroid nodules in a large cohort. 161 patients underwent MIBI, followed by a thyroidectomy. We used a dual phase MIBI protocol. Interpretation of the images included a scoring system from 0 (absent) to 3 (increased); this was to provide a scale for the uptake of the thyroid nodule in comparison to the paranodular tissue. Additionally, we evaluated the tracer uptake trend in late images compared to early images. We used the final histopathology as the reference standard. Scores 0-1 in early images, scores 0-2 in late images, and an absence of increasing uptake in the thyroid nodule in late images, showed the best predictive values to exclude malignancy, respectively (negative predictive value (NPV) 89%). Highest sensitivity (91%) for malignant nodules was evident in early images with a score 1-3. Highest specificity (91%) was obtained when the negative was defined as an absence of uptake-increase, in the late images. This study confirms that the most valuable feature of MIBI is the high NPV. Thus, with the appropriate interpretation method, high sensitivity and specificity, and moderate PPV can be obtained.
Keywords: sestamibi, MIBI, thyroid nodules, thyroid cancer, cold nodule
INTRODUCTION
In Germany, more than 15 million people have thyroid nodules and about 90,000-100,000 patients undergo thyroid surgery each year; yet only approximately 6000 of these patients are diagnosed with thyroid cancer. This means that not even 1 in 1000 thyroid nodules is a malignant one [1-4]. To avoid such overtreatment, it is very important to improve the diagnostic approach to thyroid nodules.
Nodules with a diameter of ≥ 1 cm require a thyroid scintigraphy to evaluate the functional activity [5]. There is an increased suspicion of malignancy (2-5%) in hypo- and isofunctional nodules, and in these cases, further evaluation is needed [6].
[99mTc]Tc-Sestamibi(MIBI) is increasingly used in practice for the investigation of thyroid nodules. The tracer accumulates in mitochondria-rich cells, common in hyperplasia, malignant tumors, or parathyroid adenomas [6]. This may help distinguish between benign and malignant nodules, which is important for the selection those patients who would benefit from surgery [7].
Fine needle aspiration biopsy (FNAB) is a safe and minimally invasive method for the evaluation of thyroid nodules [8]. However, FNAB can be problematic, especially in patients with multinodular goiter or in those with difficult to access lesions. Furthermore, this technique is highly examiner-dependent and the rate of non-diagnostic results varies between 2-32%, requiring a re-biopsy [9-15].
Previous retrospective studies showed that MIBI-imaging has a very high negative predictive value (NPV; mean > 97%, range 84-100%) [16-31]. However, most of the studies have a limited number of patients (range 25-83) [9, 16-19, 21, 23-31]. The largest study, with 130 patients, is from the Mexican study group of Hurtado-Lopez et al., which found that the NPV of MIBI-scintigraphy is 100% [20].
Another issue is that there is no standardized MIBI-imaging protocol; there can be either a single-phase protocol with late images (1-2 h post injection) or a dual-phase protocol with early (15-30 min post injection) and late images. The imaging can include planar images and/or single-photon emission computed tomography (SPECT) images [6].
The aim of this study was to examine the accuracy of MIBI-scintigraphy for the differentiation of thyroid nodules in the German population. The secondary objective was to determine the best acquisition time for the images. To our knowledge, this is the largest study, to date, evaluating the utility of MIBI in thyroid nodules.
RESULTS
Patients and thyroid nodules
The mean age of the 122 female (76%) and 39 male (24%) participants was 51 + 14 years (range 18-82 years). The mean volume of the nodules was 5.2 + 6.4 ml (range 0.1–37.6 ml). 33 patients had a single thyroid nodule and 128 patients had a multinodular goiter. In the technetium-99m-pertechnetate (TPT)-scintigraphy, 145 (90%) of the nodules were hypofunctional and 16 (10%) were indifferent. Characteristics of the thyroid nodules are summarized in Table 1.
Table 1. Characteristics of the thyroid nodules.
| Characteristic | Data (%) |
|---|---|
| Goiter | |
| Uninodular | 33 (20.5%) |
| Multinodular | 128 (79.5%) |
| Prior radioiodine treatment (RAI) | |
| Yes | 11 (6.8%) |
| No | 150 (93.2%) |
| Toxic nodular goiter | |
| Yes | 25 (15.5%) |
| No | 136 (84.5%) |
| Nodule functionality in [99mTc]Tc-pertechnetate (TPT) scintigraphy | |
| Hypofunctional | 145 (90.1%) |
| Indifferent | 16 (9.9%) |
| Histopathological diagnosis | |
| Benign nodule | 139 (86.3%) |
| Malignant nodule | 22 (13.7%) |
Histopathological results
The histopathological examination revealed 139 (86%) benign and 22 (14%) malignant nodules. From the malignant tumors, 15 (68%) were papillary, four (18%) were follicular, and three (14%) were papillary cancer with follicular differentiation. There were no cases of anaplastic cancer. Medullary carcinomas were not observed, because all cases of elevated tumor marker calcitonin underwent a calcium stimulation test for further evaluation and did not receive a MIBI-scintigraphy.
Diagnostic utility of fine needle aspiration biopsy (FNAB)
109 patients underwent a FNAB, 52 cytology cases (48%) were benign, 23 (21%) suspect, three (3%) were malignant neoplasm, and 31 (28%) were non-diagnostic (Table 2).
Table 2. Utility of fine needle aspiration biopsy (FNAB) for the differentiation between benign and malignant thyroid nodules.
| Cytology results of the FNAB | Histopathology results Data (%) | Total (%) | |
|---|---|---|---|
| Benign | Malignant | ||
| Not done | 45 (32.4%) | 7 (31.8%) | 52 (32.3%) |
| Normal | 48 (34.5%) | 4 (18.2%) | 52 (32.3%) |
| Pathologic | 1 (0.7%) | 2 (9.1%) | 3 (1.9%) |
| Intermediate/suspected | 19 (13.7%) | 4 (18.2%) | 23 (14.3%) |
| Insufficient | 26 (18.7%) | 5 (22.7%) | 31 (19.2%) |
| Total (%) | 139 (100%) | 22 (100%) | 161 (100%) |
Differentiation between benign and malignant tumors was not statistically significant, p = 0.058.
From the histopathologically benign nodules, 48 had normal cytology results and one case had pathologic cytology. There were 19 patients with intermediate cytology, meaning that the results were suspicious but unconducive, for example cellular atypia or follicular neoplasia. In 26 cases there was inadequate aspiration material.
From the malignant nodules, four had normal results, four had intermediate/suspect results, and two had pathological results in the cytology. Five aspirates were non-diagnostic.
The obtained p-value of the utility of FNAB to differentiate between benign and malignant nodules was 0.058 (not significant). Statistical analyses showed a good NPV of 92%, the PPV was 23%. Sensitivity and specificity were 60% and 71%, respectively (Table 3).
Table 3. Diagnostic values of fine needle aspiration biopsy (FNAB).
| Patients with thyroid nodules | ||||
|---|---|---|---|---|
| Malignant nodules | Benign nodules | |||
| FNAB findings | Positive (malignant) | True positive | False positive | PPV |
| 6 (7.7%) | 20 (25.7%) | 23% | ||
| Negative (benign) | False negative | True negative | NPV | |
| 4 (5.1%) | 48 (61.5%) | 92% | ||
| SEN | SPE | |||
| 60% | 71% | |||
SEN = sensitivity, SPE = specifity, PPV = positive predictive value, NPV = negative predictive value.
Imaging findings
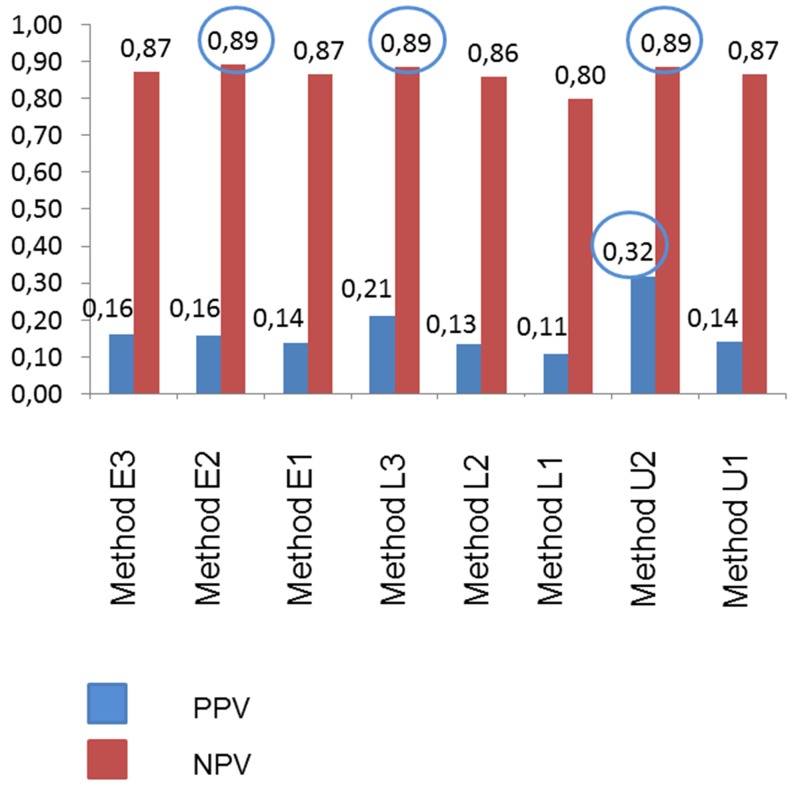
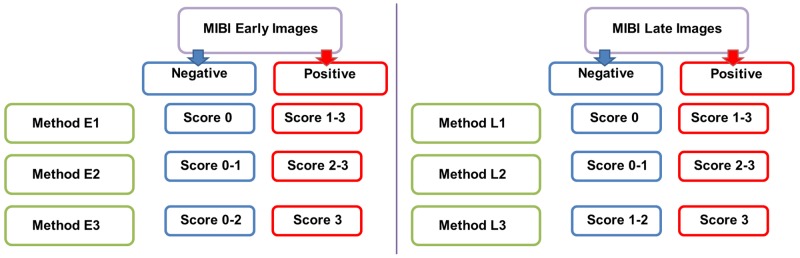
Table 4 presents the utility of MIBI-scintigraphy to differentiate between benign and malignant nodules. Flow charts of different imaging interpretation methods are depicted in Figures 1-3. Tables 5-7 show the diagnostic values (predictivity, sensitivity, specificity, and accuracy) of the different imaging interpretation methods. PPV and NPV of early and late images are also shown in Figure 4. Highest sensitivity (91%) for the detection of benign nodules was observed in the early images, when only score 0 findings were defined as negative. The highest specificity (91%) was obtained in the interpretation of the trend of the tracer uptake in late images; normal finding = decreased or constant uptake, abnormal finding = increased uptake.
Table 4. Utility of [99mTc]Tc-Sestamibi (MIBI) for the differentiation between benign and malignant thyroid nodules.
| Method | Histopathology results Data (%) | Total (%) | |
|---|---|---|---|
| Benign | Malignant | ||
| Early images | |||
| Score 0 | 13 (9.4%) | 2 (9.1%) | 15 (9.3%) |
| Score 1 | 46 (33.1%) | 5 (22.7%) | 51 (31.7%) |
| Score 2 | 43 (30.9%) | 8 (36.4%) | 51 (31.7%) |
| Score 3 | 37 (26.6%) | 7 (31.8%) | 44 (27.3%) |
| Total (%) | 139 (100%) | 22 (100%) | 161 (100%) |
| Late images | |||
| Score 0 | 39 (28.1%) | 10 (45.5%) | 49 (30.4%) |
| Score 1 | 41 (29.5%) | 3 (13.6%) | 30 (18.6%) |
| Score 2 | 29 (20.9%) | 1 (4.5%) | 30 (18.6%) |
| Score 3 | 30 (21.6%) | 8 (36.4%) | 38 (23.6%) |
| Total (%) | 139 (100%) | 22 (100%) | 161 (100%) |
| Tracer uptake trend | |||
| Decrease (washout) | 13 (9.4%) | 6 (27.3%) | 19 (11.8%) |
| Increase (retention) | 78 (56.1%) | 12 (54.5%) | 90 (55.9%) |
| Constant (persistence) | 52 (32.3%) | 4 (18.2%) | 48 (34.5%) |
| Total (%) | 139 (100%) | 22 (100%) | 161 (100.0%) |
The p-value from the early images was not significant, the late images achieved p = 0.044, and the washout/tracer retention method was p = 0.034.
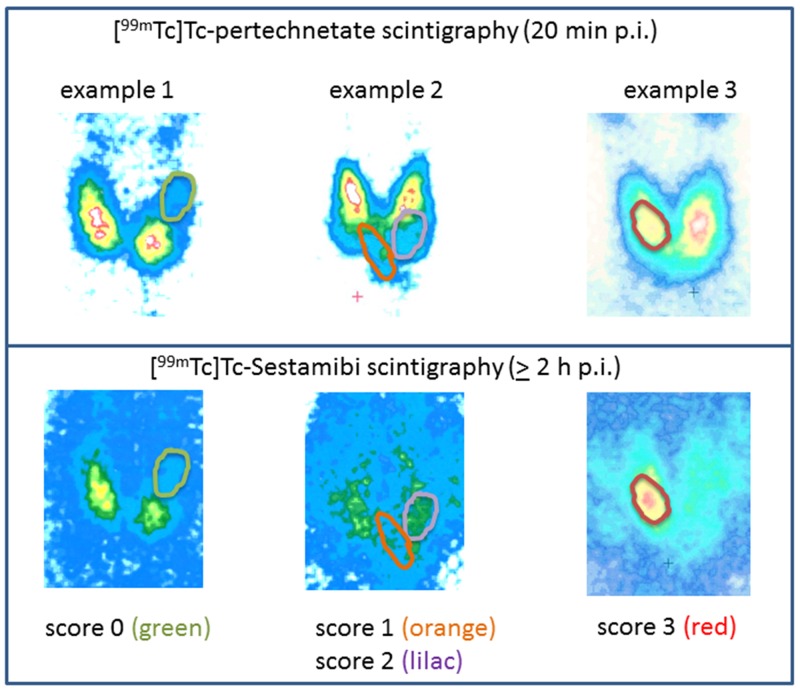
Figure 1. Examples of the scoring system of [99mTc]Tc-Sestamibi (MIBI)- images.
The accumulation of the tracer in the thyroid nodule was classified as absent (score 0), low (score 1), isointense (score 2), or increased (score 3).
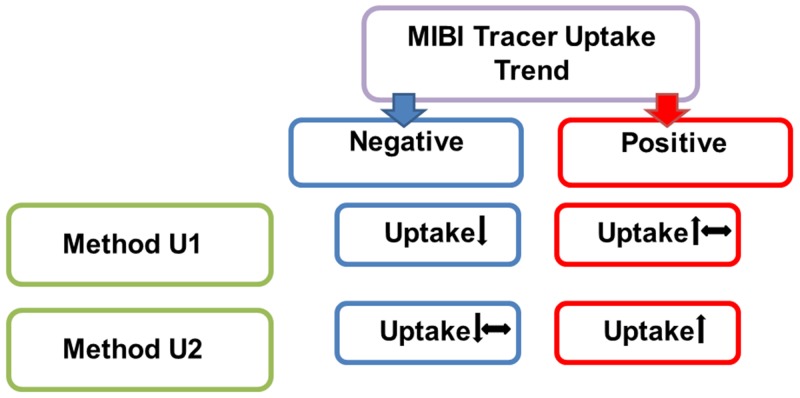
Figure 3. The different methods for the interpretation of tracer uptake trend of [99mTc]Tc-Sestamibi (MIBI) scintigraphy in late images, compared to early images.
Method U1: negative = decreased uptake, positive = increased or constant uptake. Method U2: negative = decreased or constant uptake, positive = increased uptake.
Table 5. Diagnostic values of the early [99mTc]Tc-Sestamibi (MIBI) imaging.
| Early images | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | TP | TN | FP | FN | TOT | SEN | SPE | PPV | NPV | ACC |
| Imaging Interpretation | (%) | (%) | (%) | (%) | (%) | |||||
| Method E1 | 20 | 12 | 126 | 2 | 161 | 0.91 | 0.09 | 0.14 | 0.87 | 0.20 |
| (12.4) | (8.1) | (78.3) | (1.2) | (100) | ||||||
| Method E2 | 15 | 59 | 80 | 7 | 161 | 0.68 | 0.42 | 0.16 | 0.89 | 0.46 |
| (9.3) | (36.6) | (49.7) | (4.3) | (100) | ||||||
| Method E3 | 7 | 102 | 37 | 15 | 161 | 0.32 | 0.73 | 0.16 | 0.87 | 0.68 |
| (4.3) | (63.4) | (23) | (9.3) | (100) | ||||||
Method E1: negative = score 0, positive = score 1-3.
Method E2: negative = score 0-1, positive = score 2-3.
Method E3: negative = score 0-2, positive = score 3.
TP = true positive, TN = true negative, FP = false positive, FN = false negative, TOT = total of valid cases, SEN = sensitivity, SPE = specificity, PPV = positive predictive value, NPV = negative predictive value, ACC = accuracy.
Bold values highlight the most important results.
Table 7. Diagnostic values of the interpretation of the tracer uptake trend in late images from [99mTc]Tc-Sestamibi (MIBI) scintigraphy.
| Tracer uptake trend | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | TP | TN | FP | FN | TOT | SEN | SPE | PPV | NPV | ACC |
| Imaging Interpretation | (%) | (%) | (%) | (%) | (%) | |||||
| Method U1 | 10 | 78 | 61 | 12 | 161 | 0.45 | 0.56 | 0.14 | 0.87 | 0.55 |
| (6.2) | (48.4) | (37.9) | (7.5) | (100) | ||||||
| Method U2 | 6 | 126 | 13 | 16 | 161 | 0.27 | 0.91 | 0.32 | 0.89 | 0.82 |
| (3.7) | (78.3) | (8.1) | (9.9) | (100) | ||||||
Method U1: negative = decreased uptake, positive = increased or constant uptake.
Method U2: negative = decreased or constant uptake, positive = increased uptake.
TP = true positive, TN = true negative, FP = false positive, FN = false negative, TOT = total of valid cases, SEN = sensitivity, SPE = specificity, PPV = positive predictive value, NPV = negative predictive value, ACC = accuracy.
Bold values highlight the most important results.
Figure 4. Positive predictive value (PPV) and negative predictive value (NPV) of different [99mTc]Tc-Sestamibi (MIBI) imaging interpretation methods.
Early Images: Method E1: negative = score 0, positive = score 1-3. Method E2: negative = score 0-1, positive = score 2-3. Method E3: negative = score 0-2, positive = score 3. Late Images: Method L1: negative = score 0, positive = score 1-3. Method L2: negative = score 0-1, positive = score 2-3. Method L3: negative = score 0-2, positive = score 3. Interpretation of the tracer uptake trend in late images: Method U1: negative = decreased uptake, positive = increased or constant uptake. Method U2: negative = decreased or constant uptake, positive = increased uptake.
Figure 2. The different methods for the interpretation of early and late images of [99mTc]Tc-Sestamibi (MIBI) scintigraphy.
Method E1: negative = score 0, positive = score 1-3. Method E2: negative = score 0-1, positive = score 2-3. Method E3: negative = score 0-2, positive = score 3. Method L1: negative = score 0, positive = score 1-3. Method L2: negative = score 0-1, positive = score 2-3. Method L3: negative = score 0-2, positive = score 3.
Table 6. Diagnostic values of the late imaging interpretation of [99mTc]Tc-Sestamibi (MIBI) scintigraphy.
| Late images | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | TP | TN | FP | FN | TOT | SEN | SPE | PPV | NPV | ACC |
| Imaging Interpretation | (%) | (%) | (%) | (%) | (%) | |||||
| Method L1 | 12 | 40 | 99 | 10 | 161 | 0.55 | 0.29 | 0.11 | 0.80 | 0.32 |
| (7.5) | (24.8) | (61.5) | (6.2) | (100) | ||||||
| Method L2 | 9 | 80 | 59 | 13 | 161 | 0.41 | 0.58 | 0.13 | 0.86 | 0.55 |
| (5.6) | (49.7) | (36.6) | (8.1) | (100) | ||||||
| Method L3 | 8 | 109 | 30 | 14 | 161 | 0.36 | 0.78 | 0.21 | 0.89 | 0.73 |
| (5.6) | (49.7) | (36.6) | (8.1) | (100) | ||||||
Method L1: negative = score 0, positive = score 1-3.
Method L2: negative = score 0-1, positive = score 2-3.
Method L3: negative = score 0-2, positive = score 3.
TP = true positive, TN = true negative, FP = false positive, FN = false negative, TOT = total of valid cases, SEN = sensitivity, SPE = specificity, PPV = positive predictive value, NPV = negative predictive value, ACC = accuracy.
Bold values highlight the most important results.
Early images
Among the benign nodules the score was 0 in 13 nodules, while 46 nodules had a low MIBI-uptake (score 1), in comparison to the paranodular tissue. Another 43 nodules had a score 2, and 37 lesions had score 3.
Among the malignant nodules, the score was 0 in two nodules. Five lesions had a score 1, eight were isointense (score 2), and seven nodules showed increased uptake (score 3) in the scintigraphy.
The ability of the early images to differentiate between benign and malignant nodules was not significant.
Late images
In the late images, among the benign nodules, 39 had no uptake (score 0), 41 had a score 1, and 29 had a score 2. 30 benign lesions had a score 3.
Among the malignant nodules, the score in the late images was 0 in 10 lesions, 1 in three nodules, and 2 in one nodule. Eight nodules showed high uptake (score 3).
In summary, the late images could reliably differentiate between benign and malignant nodules (p = 0.044, according to chi-square-test).
Washout/tracer retention in the late images
Among the benign lesions, tracer uptake in the late images, compared with the early images, remained constant in 48 cases. There was an uptake decline in 78 of the lesions and an uptake increase in 13 lesions.
Among the malignant nodules, there was a sufficient washout in 12 cases, in four nodules the uptake was constant, and six nodules showed an increased retention of the tracer over time.
The washout/tracer retention method showed good reliability (p = 0.034) in terms of differentiation between benign and malignant nodules.
DISCUSSION
There are several publications reporting the diagnostic value of MIBI-scintigraphy for the evaluation of thyroid nodules. Most impressing is MIBI’s high negative predictive value, of up to 100%; mean > 97% [9, 16-31]. Only Kresnik et. al. reported a much lower NPV of 84%; however, the study included only 62 patients [21]. Most of the studies have a small patient cohort (range 25-83 patients) [9, 16-20, 22-31]. The largest MIBI study (130 patients) from Hurtado Lopez et. al. was conducted in Mexico, where there is a high prevalence (38%) of thyroid carcinomas in this patient population [6, 20]. In comparison, the prevalence in Germany is only 11% [6]. It is the opinion of the authors, that image interpretation should be adapted to the prevalence of thyroid carcinomas in the studied population.
In the current study, the best NPV (89%) of thyroid nodules was observed in lesions with a score of 0-1 in the early images, and a score of 0-2 and in the late images (86% NPV). Good NPV (89%) was also obtained in the interpretation of the trend of the uptake over time; negative finding = decreased or constant uptake in the late images. This method also showed the best specificity of 91%. The reliable NPV of MIBI-scintigraphy can justify a “wait-and-see” strategy.
Another consideration is the positive predictive value of MIBI-scintigraphy. The PPV varies in the published literature between < 10% and > 61% [9, 16-31]. The utility of this value can be relevant for the indication for surgery. Our data show that the best PPV was obtained in the interpretation of tracer uptake trend. If a lesion has an increasing uptake in the late images, the PPV is 32%, and this can justify surgery.
False-negative findings are rarely reported in the literature. Examples are two patients with undifferentiated / anaplastic carcinoma from the study of Kresnik et al and Foldes et al [19, 21]. However, there were also small number of patients with differentiated cancer (papillary n=3 / follicular n=1), who had a negative MIBI-scan [26, 28, 29]. In our patient group, there were two cases of score 0 malignant nodules in the early images, and 10 false negative results in the late images. The false negatives may indicate that a continuous follow-up with ultrasound of the neck and if necessary repeated FNAB are needed in these patients.
We used the dual-phase study protocol with planar images for performing MIBI. The late images could reliably differentiate between benign and malignant nodules, p = 0.044. Good reliability for the differentiation (p = 0.034) was also revealed in the interpretation of the tracer uptake trend (washout or tracer retention) in the late images. However, better diagnostic values could have been achieved with SPECT imaging. For example, the study of Schenke et. al. compared SPECT with planar MIBI-imaging, achieving a much better NPV; 100% versus 91.7% [27].
There are some limitations and biases in the current study which need to be mentioned. Firstly, not all patients underwent a FNAB. From the 109 patients who had an ultrasound-guided FNAB, 31 (28%) had non-diagnostic biopsies. A better pre-operative diagnostic procedure would have decreased the benign nodules in this study. Secondly, we informed patients who did not undergo a FNAB, or who had an inadequate biopsy, or who had a FNAB with no evidence of malignancy, that the only way to exclude a malignancy is to undergo surgery. This may have raised the number of cases of operated patients. Thirdly, the majority of the malignant nodules were papillary carcinoma (68%); therefore, it is uncertain if the utility of MIBI-scintigraphy is the same for all thyroid cancer entities. Furthermore, there were no cases of anaplastic cancer in this study. This may be because anaplastic cancer is often clinically classified as suspect (fast growing and irregular in the ultrasound) and directly referred for surgical evaluation. Finally, there were patients who received MIBI-scintigraphy despite suspicious FNAB findings. The reason for this is that these patients received both a FNAB and MIBI on the same day, and we were not aware of the cytopathology results. To avoid such bias in the future, and to confirm the reliability of MIBI, prospective studies are needed.
In conclusion, the current study confirms that the most valuable feature of MIBI-scintigraphy is its NPV. Using a dual-phase protocol, 89% NPV could be achieved either in early images of lesions with a score 0-1, or in late images with a score 0-2. Furthermore, with the appropriate image interpretation method, a high sensitivity (91%), high specificity (91%) and moderate PPV (32%) can be obtained. The current study confirms that the most valuable feature of MIBI is the NPV. Thus, with the appropriate image interpretation method, high sensitivity and specificity, and moderate PPV can be obtained.
MATERIALS AND METHODS
Patients
In total, 603 patients underwent a MIBI-scintigraphy at our department between October 2005 and August 2014. All patients had at least one thyroid nodule, which was cold/indifferent in the [99mTc]Tc-pertechnetate (TPT)-scintigraphy. At the time this study was conducted, MIBI was not an established diagnostic tool. For that reason, we informed patients who did not undergo a FNAB, or who had an inadequate biopsy, or who underwent a FNAB with no evidence of malignancy, that the only way to exclude a malignancy is surgery. Patients with elevated tumor marker calcitonin and suspicion of medullary cancer did not receive a MIBI-scintigraphy. In these cases we used the calcium stimulation test for further evaluation. From the 603 studied patients, 161 received a histopathological diagnosis after thyroid surgery, and were included for further analysis. The local ethics committee of our university approved this retrospective study; informed consent was obtained from all participants.
Imaging and interpretation
All patients underwent TPT-scintigraphy followed by MIBI-scintigraphy. After intravenous injection of MIBI (standard dose 370 MBq) we used a dual-phase protocol with planar images approximately 20 min post-injection (p.i.) and 2 h p.i.
The uptake in the examined nodule was compared with the paranodular thyroid tissue. The findings were classified visually; accumulation of the tracer in the thyroid nodule was classified as absent (score 0), low (score 1), isointense (score 2), or increased (score 3). Examples of this scoring system are presented in Figure 1. We also considered the washout or the tracer-retention in the late images, compared to the early images.
A correlation with the TPT-scintigraphy showed either a “match” (i.e., concordant decreased uptake of both tracers) or a “mismatch” (i.e., cold nodule with increased MIBI-uptake).
Fine needle aspiration biopsy (FNAB)
109 patients underwent a FNAB. The biopsy was performed through guided ultrasound using a 20-gauge needle attached to a 20 ml Cameco syringe-pistol. Smears were made and air-dried slides were stained with hematoxylin-eosin. The remaining aspirate material in the syringe was rinsed with 0.9% sodium chloride. The fluid material was centrifuged, the sediment was smeared and slides were prepared. Adequacy of the aspirates was assessed on the basis of the guidelines of the Papanicolaou Society [32].
Histopathology
The gold standard for histologic diagnosis served as a reference. From the 603 patients, 161 patients underwent surgery for further histopathological examination of the thyroid nodules. Routine staining with hematoxylin-eosin, Elastica van-Giesson and immunochemistry, if necessary, was performed.
Statistical analyses
Statistical analyses were performed with IBM SPSS software version 22. Different image interpretation methods were compared for their utility to differentiate between benign and malignant nodules. We used the chi-square test to determine the statistical significance of the results. The significance level was accepted at 5%. Additionally, to obtain the validity of the imaging, we classified the findings into true positive (TP), true negative (TN), false positive (FP), and false negative (FN). Sensitivity (SEN) was calculated as TP/(TP + FN), specificity (SPE) as TN/(TN + FP), and accuracy (ACC) as (TP + TN)/(TP + TN + FP + FN). The positive predictive value (PPV) was defined as TP/(TP + FP), the negative predictive value (NPV) as TN/(TN + FN).
Author contributions
Conception and design: Hojjat Ahmadzadehfar, Hans Jürgen Biersack.
Provision of study materials or patients: Soha Mahjoob, Anna Yordanova, Markus Essler and Glen Kristiansen.
Manuscript writing: Anna Yordanova, Soha Mahjoob, Hojjat Ahmadzadehfar.
Data analysis and interpretation: Anna Yordanova, Hojjar Ahmadzadehfar, Soha Mahjoob, Philipp Lingohr, Jörg Kalff, Jamshid Farahati, Holger Palmedo, Andreas Türler.
Revision: Anna Yordanova, Hojjat Ahmadzadehfar, Soha Mahjoob.
Final approval of manuscript: Hojjat Ahmadzadehfar, Anna Yordanova, Markus Essler, Philipp Lingohr, Jörg Kalff, Andreas Türler, Holger Palmedo, Hans-Jürgen Biersack, Glen Kristiansen, Jamshid Farahati, Soha Mahjoob.
CONFLICTS OF INTEREST
We declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
FUNDING
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
REFERENCES
- 1.Koch-Institut R. Krebs in Deutschland 2011/2012. Gesundheitsberichterstattung des Bundes. 2015 10 Ausg.
- 2.Musholt TJ, Clerici T, Dralle H, Frilling A, Goretzki PE, Hermann MM, Kussmann J, Lorenz K, Nies C, Schabram J, Schabram P, Scheuba C, Simon D, et al. German Association of Endocrine Surgeons practice guidelines for the surgical treatment of benign thyroid disease. Langenbeck’s archives of surgery. 2011;396:639–649. doi: 10.1007/s00423-011-0774-y. [DOI] [PubMed] [Google Scholar]
- 3.Reiners C, Wegscheider K, Schicha H, Theissen P, Vaupel R, Wrbitzky R, Schumm-Draeger PM. Prevalence of thyroid disorders in the working population of Germany: ultrasonography screening in 96,278 unselected employees. Thyroid. 2004;14:926–932. doi: 10.1089/thy.2004.14.926. [DOI] [PubMed] [Google Scholar]
- 4.Verburg FA. Is thyroid surgery performed too often in Germany? Nuklearmedizin. 2015;54:101–105. [PubMed] [Google Scholar]
- 5.Dietlein M, Dressler J, Eschner W, Leisner B, Reiners C, Schicha H. [Procedure guideline for thyroid scintigraphy (version 3)]. [Article in German] Nuklearmedizin. 2007;46:203–205. [PubMed] [Google Scholar]
- 6.Bucerius J, Ahmadzadehfar H, Biersack H. 99mTc-Sestamibi. Berlin Heidelberg: Springer; 2012. [Google Scholar]
- 7.Schmidt M. MIBI-Szintigrafie bei hypofunktionellen Schilddrüsenknoten. Nuklearmediziner. 2016;39:178–190. [Google Scholar]
- 8.Schicha H, Hellmich M, Lehmacher W, Eschner W, Schmidt M, Kobe C, Schober O, Dietlein M. [Should all patients with thyroid nodules > or = 1 cm undergo fine-needle aspiration biopsy?]. [Article in German] Nuklearmedizin. 2009;48:79–83. doi: 10.3413/nukmed-0313. [DOI] [PubMed] [Google Scholar]
- 9.Izquierdo R, Shankar R, Kort K, Khurana K. Ultrasound-guided fine-needle aspiration in the management of thyroid nodules in children and adolescents. Thyroid. 2009;19:703–705. doi: 10.1089/thy.2009.0058. [DOI] [PubMed] [Google Scholar]
- 10.Nam-Goong IS, Kim HY, Gong G, Lee HK, Hong SJ, Kim WB, Shong YK. Ultrasonography-guided fine-needle aspiration of thyroid incidentaloma: correlation with pathological findings. Clinical endocrinology. 2004;60:21–28. doi: 10.1046/j.1365-2265.2003.01912.x. [DOI] [PubMed] [Google Scholar]
- 11.Oertel YC, Miyahara-Felipe L, Mendoza MG, Yu K. Value of repeated fine needle aspirations of the thyroid: an analysis of over ten thousand FNAs. Thyroid. 2007;17:1061–1066. doi: 10.1089/thy.2007.0159. [DOI] [PubMed] [Google Scholar]
- 12.Orija IB, Pineyro M, Biscotti C, Reddy SS, Hamrahian AH. Value of repeating a nondiagnostic thyroid fine-needle aspiration biopsy. Endocrine practice. 2007;13:735–742. doi: 10.4158/EP.13.7.735. [DOI] [PubMed] [Google Scholar]
- 13.Redman R, Zalaznick H, Mazzaferri EL, Massoll NA. The impact of assessing specimen adequacy and number of needle passes for fine-needle aspiration biopsy of thyroid nodules. Thyroid. 2006;16:55–60. doi: 10.1089/thy.2006.16.55. [DOI] [PubMed] [Google Scholar]
- 14.van Roosmalen J, van Hemel B, Suurmeijer A, Groen H, Ruitenbeek T, Links TP, Plukker JT. Diagnostic value and cost considerations of routine fine-needle aspirations in the follow-up of thyroid nodules with benign readings. Thyroid. 2010;20:1359–1365. doi: 10.1089/thy.2008.0268. [DOI] [PubMed] [Google Scholar]
- 15.Woo SH, Kim KH, Kim RB. Thyroid nodules with repeat nondiagnostic cytologic results: the role of clinical and ultrasonographic findings. World journal of surgery. 2015;39:1721–1727. doi: 10.1007/s00268-015-3013-9. [DOI] [PubMed] [Google Scholar]
- 16.Alonso O, Mut F, Lago G, Aznarez A, Nunez M, Canepa J, Touya E. 99Tc(m)-MIBI scanning of the thyroid gland in patients with markedly decreased pertechnetate uptake. Nuclear medicine communications. 1998;19:257–261. doi: 10.1097/00006231-199803000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Demirel K, Kapucu O, Yucel C, Ozdemir H, Ayvaz G, Taneri F. A comparison of radionuclide thyroid angiography, (99m)Tc-MIBI scintigraphy and power Doppler ultrasonography in the differential diagnosis of solitary cold thyroid nodules. European journal of nuclear medicine and molecular imaging. 2003;30:642–650. doi: 10.1007/s00259-003-1124-2. [DOI] [PubMed] [Google Scholar]
- 18.Erdil TY, Ozker K, Kabasakal L, Kanmaz B, Sonmezoglu K, Atasoy KC, Turoglu HT, Uslu I, Isitman AT, Onsel C. Correlation of technetium-99m MIBI and thallium-201 retention in solitary cold thyroid nodules with postoperative histopathology. European journal of nuclear medicine. 2000;27:713–720. doi: 10.1007/s002590050567. [DOI] [PubMed] [Google Scholar]
- 19.Foldes I, Levay A, Stotz G. Comparative scanning of thyroid nodules with technetium-99m pertechnetate and technetium-99m methoxyisobutylisonitrile. European journal of nuclear medicine. 1993;20:330–333. doi: 10.1007/BF00169809. [DOI] [PubMed] [Google Scholar]
- 20.Hurtado-Lopez LM, Arellano-Montano S, Torres-Acosta EM, Zaldivar-Ramirez FR, Duarte-Torres RM, Alonso-De-Ruiz P, Martinez-Duncker I, Martinez-Duncker C. Combined use of fine-needle aspiration biopsy, MIBI scans and frozen section biopsy offers the best diagnostic accuracy in the assessment of the hypofunctioning solitary thyroid nodule. European journal of nuclear medicine and molecular imaging. 2004;31:1273–1279. doi: 10.1007/s00259-004-1544-7. [DOI] [PubMed] [Google Scholar]
- 21.Kresnik E, Gallowitsch HJ, Mikosch P, Gomez I, Lind P. Technetium-99m-MIBI scintigraphy of thyroid nodules in an endemic goiter area. Journal of nuclear medicine. 1997;38:62–65. [PubMed] [Google Scholar]
- 22.Leidig-Bruckner G, Cichorowski G, Sattler P, Bruckner T, Sattler B. Evaluation of thyroid nodules--combined use of (99m)Tc-methylisobutylnitrile scintigraphy and aspiration cytology to assess risk of malignancy and stratify patients for surgical or nonsurgical therapy--a retrospective cohort study. Clinical endocrinology. 2012;76:749–758. doi: 10.1111/j.1365-2265.2011.04292.x. [DOI] [PubMed] [Google Scholar]
- 23.Listewnik MH, Birkenfeld B, Piwowarska-Bilska H, Cichon-Bankowska K, Iglinska-Wagner L, Watrak W, Smolira W, Zorga P, Niedzialkowska K, Elbl B, Sawrymowicz M. The application of SPECT/CT scintigraphy with MIBI-Tc(9)(9)(m) in the diagnosis of thyroid nodules - a preliminary report. Endokrynologia Polska. 2010;61:422–426. [PubMed] [Google Scholar]
- 24.Mezosi E, Bajnok L, Gyory F, Varga J, Sztojka I, Szabo J, Galuska L, Leovey A, Kakuk G, Nagy E. The role of technetium-99m methoxyisobutylisonitrile scintigraphy in the differential diagnosis of cold thyroid nodules. European journal of nuclear medicine. 1999;26:798–803. doi: 10.1007/s002590050451. [DOI] [PubMed] [Google Scholar]
- 25.Nakahara H, Noguchi S, Murakami N, Hoshi H, Jinnouchi S, Nagamachi S, Ohnishi T, Futami S, Flores LG, 2nd, Watanabe K. Technetium-99m-sestamibi scintigraphy compared with thallium-201 in evaluation of thyroid tumors. Journal of nuclear medicine. 1996;37:901–904. [PubMed] [Google Scholar]
- 26.Sathekge MM, Mageza RB, Muthuphei MN, Modiba MC, Clauss RC. Evaluation of thyroid nodules with technetium-99m MIBI and technetium-99m pertechnetate. Head & neck. 2001;23:305–310. doi: 10.1002/hed.1035. [DOI] [PubMed] [Google Scholar]
- 27.Schenke S, Zimny M, Rink T, Stahl U, Fritzel M, Klett R. [99mTc-MIBI scintigraphy of hypofunctional thyroid nodules. Comparison of planar and SPECT imaging]. [Article in German] Nuklearmedizin. 2014;53:105–110. doi: 10.3413/Nukmed-0619-13-08. [DOI] [PubMed] [Google Scholar]
- 28.Sundram FX, Mack P. Evaluation of thyroid nodules for malignancy using 99Tcm-sestamibi. Nuclear medicine communications. 1995;16:687–693. doi: 10.1097/00006231-199508000-00011. [DOI] [PubMed] [Google Scholar]
- 29.Theissen P, Schmidt M, Ivanova T, Dietlein M, Schicha H. MIBI scintigraphy in hypofunctioning thyroid nodules--can it predict the dignity of the lesion? Nuklearmedizin. 2009;48:144–152. doi: 10.3413/nukmed-0240. [DOI] [PubMed] [Google Scholar]
- 30.Treglia G, Caldarella C, Saggiorato E, Ceriani L, Orlandi F, Salvatori M, Giovanella L. Diagnostic performance of (99m)Tc-MIBI scan in predicting the malignancy of thyroid nodules: a meta-analysis. Endocrine. 2013;44:70–78. doi: 10.1007/s12020-013-9932-z. [DOI] [PubMed] [Google Scholar]
- 31.Wale A, Miles KA, Young B, Zammit C, Williams A, Quin J, Dizdarevic S. Combined (99m)Tc-methoxyisobutylisonitrile scintigraphy and fine-needle aspiration cytology offers an accurate and potentially cost-effective investigative strategy for the assessment of solitary or dominant thyroid nodules. European journal of nuclear medicine and molecular imaging. 2014;41:105–115. doi: 10.1007/s00259-013-2546-0. [DOI] [PubMed] [Google Scholar]
- 32.Papanicolaou Society of Cytopathology Task Force on Standards of Practice Guidelines of the Papanicolaou Society of Cytopathology for the examination of cytologic specimens obtained from the respiratory tract. Diagnostic cytopathology. 1999;21:61–69. doi: 10.1002/(sici)1097-0339(199907)21:1<61::aid-dc17>3.0.co;2-o. [DOI] [PubMed] [Google Scholar]