ABSTRACT
Introduction: To prepare for global elimination of trachoma by 2020, the World Health Organization (WHO) recommends mapping of trachoma at district-level to enable planning of elimination activities in affected populations. The aim of our study was to provide data on trachoma for each local government area (LGA) of Kaduna State, Nigeria, as such data were previously unavailable.
Method: As part of the Global Trachoma Mapping Project (GTMP), a population-based cross-sectional trachoma survey was conducted in each of the 23 LGAs of Kaduna State, between May and June 2013. The protocols of the GTMP were used.
Results: The prevalence of trachomatous inflammation – follicular (TF) in children aged 1–9 years was between 0.03% and 8% across the LGAs, with only one LGA (Igabi) having a TF prevalence ≥5%. The LGA-level prevalences of trichiasis in persons aged 15 years and older were between 0.00% and 0.78%. Eleven LGAs had trichiasis prevalences of 0.2% and over in adults; a threshold equivalent to 1 case per 1000 total population. The LGA-level proportion of households with access to improved water sources ranged from 9% to 96%, while household access to latrines ranged from 5% to 99%.
Conclusion: Kaduna State has generally hypoendemic trachoma, but a few trichiasis surgeries are still required to attain the WHO elimination targets. Better access to improved water and sanitation is needed.
KEYWORDS: Global Trachoma Mapping Project, Kaduna, neglected tropical diseases, Nigeria, trachoma, trichiasis, water and sanitation
Introduction
Trachoma, a neglected tropical disease, is caused by Chlamydia trachomatis, and is the leading infectious cause of blindness, accounting for 1.4% of the global burden of blindness.1 It is characterized by chronic conjunctivitis that results in scarring of the conjunctivae, and, in some people, trichiasis (in-turned eyelashes) with consequent corneal scarring. The World Health Organization (WHO) recommends mapping of trachoma at district level2 in areas where disease is suspected, for planning based on disease burden and/or documentation of elimination. Mapping data should help to focus efforts to achieve global elimination of trachoma as a public health problem by the year 2020.3
The Global Trachoma Mapping Project (GTMP) commenced in 2012.4 The GTMP’s goal was to complete the global baseline trachoma map, in order to plan public health interventions and to mobilize resources for trachoma control.5
Kaduna State, located in north-western Nigeria, has a population of 7,474,369 (2013 projection)6 residing in an estimated 1,115,974 regular households located in 23 local government areas (LGAs).7,8 Regular households consist of a group of persons living under the same roof with a recognized head, sharing a common catering arrangement and functioning as a social unit.8 A previous population-based survey reported trachomatous corneal opacity as the 7th most common cause of low vision in the state (0.3% of low vision).9 Kaduna has an eye care program that has provided eye care services, including lid surgery for trichiasis, over the last 20 years, largely in health facilities or during cataract outreach campaigns.
The aim of this study was to provide prevalence data on trachoma in all 23 LGAs of Kaduna State, as no previous trachoma-specific surveys had been conducted here. This should provide data to assist in decision-making with respect to local trachoma elimination. The objectives were to estimate the prevalence of trachomatous inflammation – follicular (TF)10 in children aged 1–9 years in each Kaduna LGA, to estimate the prevalence of trichiasis in persons aged 15 years and older in each Kaduna LGA, and to assess the water and sanitation coverage in each Kaduna LGA.
Materials and methods
Between May and June 2013, in each LGA, we conducted a population-based cross-sectional prevalence survey using GTMP protocols.11
Sample size
Each LGA was considered as a separate evaluation unit. LGA populations ranged from 127,581 to 500,464, with an estimated 50% of the population aged 15 years and older.7 As described elsewhere, for each LGA, the sample size for estimating TF prevalence required framing of sufficient households to reach an expected 1222 children aged 1–9 years.11 To estimate trichiasis prevalence in persons 15 years and older, all eligible persons living in selected households were examined.
Ethical considerations
The Ethics Committee of the London School of Hygiene & Tropical Medicine (reference 6319) and the National Health Research Ethics Committee of Nigeria (reference NHREC/01/01/2007) each granted approval for the study. The Kaduna State Ministry of Health granted administrative permission for the work to go ahead. Consent of participants was obtained verbally, with that for minors granted by parents or guardians; consent was documented in the LINKS Android smartphone application (app).11 Participants found to have trichiasis during the surveys were appropriately referred, while those with active trachoma (TF and/or trachomatous inflammation – intense, TI, in either eye) were offered two tubes of 1% tetracycline eye ointment each.
Survey teams
The survey teams comprised graders and recorders who were trained and certified according to GTMP protocols (version 1).11 Training was conducted over 4 days, with the first 2 days focused on training and selecting graders. Graders who achieved a minimum kappa rating for TF of 0.7 against a GTMP-certified grader trainer were selected for the survey. Ophthalmologists provided supervision to the teams, giving feedback and crosschecking in-service diagnostic accuracy.
Sampling design
Study subjects were selected using a 3-stage sampling approach. In the first stage, we systematically selected 25 clusters, using probability proportional to size sampling, from the list of towns and villages in each LGA. Each cluster was then sub-divided into the lowest administrative unit (ward) and one unit was selected using simple random sampling. In each unit, we selected 25 households. Despite its epidemiological drawbacks, the random walk method was used to select households within wards, as the security situation was tenuous, and we felt that locally familiar field methods would place survey teams at less risk of generating unmerited suspicion than ones that would be novel to included communities.12–14 All residents of selected households who were aged 1 year and older and had lived in the area for at least the previous 6 months were enumerated, and invited to participate.
Data collection
Consent to proceed was obtained by the survey team from the head of household or his/her representative, who also provided information on water and sanitation access for the household. Global positioning system (GPS) coordinates for the household’s location were then recorded. Trachoma grading was undertaken according to the WHO simplified grading scheme,10 using ×2.5 magnifying loupes under sunlight illumination. Hands were cleaned with an alcohol-based hand gel between the examination of successive subjects.
Data management
All collected data were directly entered into the LINKS app on Android smartphones and uploaded to a cloud-based server. The GTMP Data Manager cleaned and analyzed the data, as described elsewhere.11 The proportion of 1–9-year-old children seen to have TF in each cluster was adjusted for age in 1-year age bands, and the proportion of ≥15-year-olds seen to have trichiasis in each cluster was adjusted for age and sex in 5-year age bands, with the Kaduna population pyramid from the 2006 census used as the reference. The adjusted prevalences of TF, TI and trichiasis for each LGA were the arithmetic means of the adjusted cluster level proportions of each sign.
Results
Study sample
A total of 33,884 children aged 1–9 years were enumerated, of whom 32,882 (97.0%) were examined, and 43,127 adults aged 15+ years were enumerated, of whom 38,824 (90.0%) were examined, in the 23 LGAs combined. The number of children examined per LGA ranged from 1044 to 1991, while the number of adults examined ranged from 1076 to 2524 per LGA. Sabon Gari LGA had the highest absentee rate (19.8%) among children, while the refusal rate among children was highest in Kaduna North (6.4%; Table 1).
Table 1.
Local government area-level prevalences of trachomatous inflammation – follicular (TF) and trichiasis in Kaduna State, Nigeria, Global Trachoma Mapping Project, 2013.
| Local Government Area | Sample examined n |
Refused n |
Absent n |
Trachoma prevalence % (95% CI) |
||||
|---|---|---|---|---|---|---|---|---|
| Children (1-9 yrs) | Adults (15+ yrs) | Children (1-9 yrs) | Adults (15+ yrs) | Children (1-9 yrs) | Adults (15+ yrs) | TF (1-9 yrs) | Trichiasis (15+ yrs) | |
| Birnin Gwari | 1222 | 1225 | 0 | 0 | 1 | 2 | 0.1 (0.0-0.2) | 0.40 (0.14-0.65) |
| Chikun | 840 | 1007 | 4 | 19 | 1 | 321 | 2.7 (1.0-4.8) | 0.03 (03.0-0.10) |
| Giwa | 1500 | 1308 | 1 | 19 | 52 | 213 | 1.7 (1.0-2.6) | 0.35 (0.15-0.61) |
| Igabi | 1444 | 1379 | 4 | 23 | 21 | 76 | 8.1 (5.7-10.9) | 0.34 (0.16-0.59) |
| Ikara | 1169 | 803 | 7 | 92 | 3 | 286 | 1.7 (1.1-2.3) | 0.20 (0.04-0.43) |
| Jaba | 982 | 1302 | 1 | 3 | 4 | 39 | 0.5 (0.3-0.9) | 0.08 (0.00-0.23) |
| Jema’a | 1219 | 1882 | 11 | 8 | 10 | 16 | 1.0 (0.5-1.8) | 0.00 |
| Kachia | 1059 | 1166 | 14 | 1 | 22 | 30 | 1.4 (0.9-1.9) | 0.16 (0.04-0.33) |
| Kaduna North | 827 | 1619 | 60 | 87 | 17 | 117 | 0.6 (0.2-1.1) | 0.07 (0.02-0.14) |
| Kaduna South | 1126 | 918 | 2 | 0 | 36 | 37 | 0.0 (0.0-0.1) | 0.08 (0.0-0.18) |
| Kagarko | 1353 | 1148 | 1 | 5 | 2 | 8 | 2.0 (1.2-2.9) | 0.38 (0.11-0.75) |
| Kajuru | 916 | 1184 | 9 | 12 | 5 | 120 | 2.1 (0.9-3.8) | 0.11 (0.02-0.26) |
| Kaura | 1108 | 1460 | 4 | 2 | 6 | 140 | 2.0 (1.2-3.1) | 0.09 (0.00-0.20) |
| Kauru | 870 | 1378 | 37 | 31 | 60 | 334 | 4.9 (3.1-7.3) | 0.50 (0.23-0.79) |
| Kubau | 1014 | 1168 | 5 | 32 | 52 | 143 | 1.0 (0.3-2.0) | 0.41 (0.22-0.60) |
| Kudan | 1531 | 1282 | 21 | 49 | 50 | 93 | 2.4 (1.7-3.2) | 0.32 (0.06-0.56) |
| Lere | 799 | 1118 | 1 | 0 | 4 | 28 | 1.4 (0.5-2.1) | 0.78 (0.40-1.24) |
| Makarfi | 1070 | 1362 | 2 | 32 | 0 | 104 | 1.1 (0.3-2.3) | 0.33 (0.14-0.55) |
| Sabon Gari | 794 | 1177 | 2 | 36 | 203 | 196 | 0.5 (0.0-1.3) | 0.09 (0.03-0.17) |
| Sanga | 978 | 1279 | 4 | 4 | 5 | 68 | 2.2 (1.3-3.1) | 0.09 (0.01-0.20) |
| Soba | 1219 | 1062 | 3 | 84 | 5 | 97 | 0.2 (0.0-0.4) | 0.23 (0.02-0.41) |
| Zangon Kataf | 1070 | 1280 | 3 | 0 | 7 | 132 | 2.9 (2.0-3.9) | 0.03 (0.00-0.08) |
| Zaria | 898 | 1940 | 4 | 4 | 6 | 126 | 0.0 (0.0-0.4) | 0.08 (0.01-0.14) |
Prevalences of trichiasis are displayed to two decimal places in order to provide clarity on whether or not the best estimate of prevalence was above or below the elimination threshold of 0.2% in adults ≥ 15 years.
CI, confidence interval.
Prevalence of trachoma
The prevalence of TF in children aged 1–9 years ranged from 0.0% (95% confidence interval, CI, 0.0–0.1%) in Kaduna South LGA to 8.1% (95% CI 5.7–10.9%) in Igabi LGA; in this age group, the prevalence of TI ranged from 0.0% in nine LGAs to 1.1% (95% CI 0.4–1.9%) in Makarfi LGA. The prevalence of trichiasis in those aged 15+ years ranged from 0.0% in Jema’a LGA to 0.8% (95% CI 0.4–1.2%) in Lere LGA (Table 1). Figure 1 shows the LGAs surveyed, and Figure 2 shows TF prevalences and Figure 3 shows trichiasis prevalences for each LGA.
Figure 1.
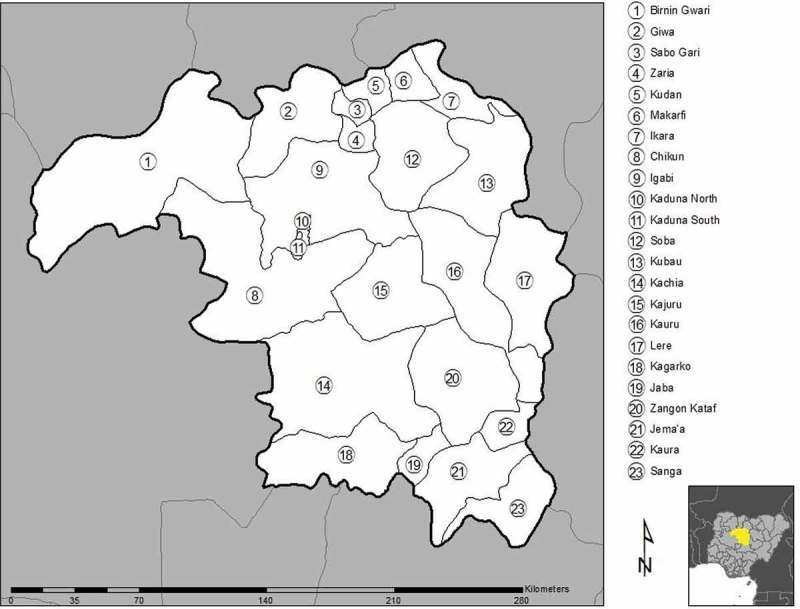
Local government areas surveyed in Kaduna State, Nigeria, Global Trachoma Mapping Project, 2013.
Figure 2.
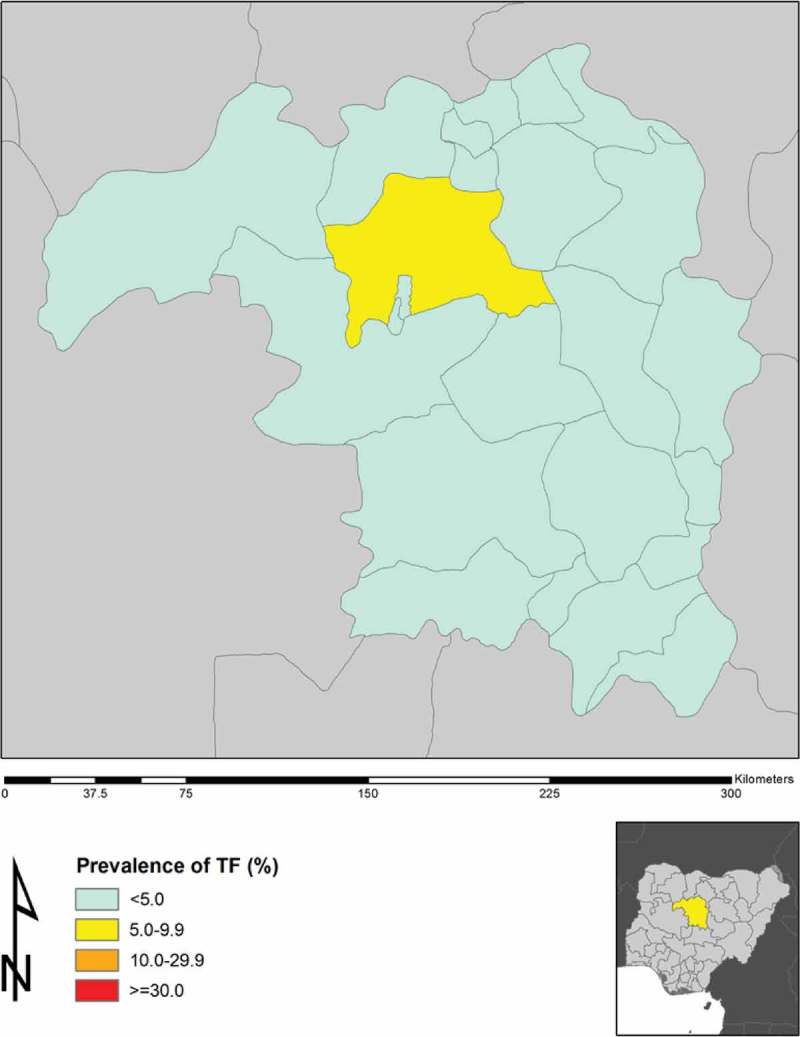
Prevalence of trachomatous inflammation – follicular (TF) in 1–9-year-old children by local government area in Kaduna State, Nigeria, Global Trachoma Mapping Project, 2013.
Figure 3.
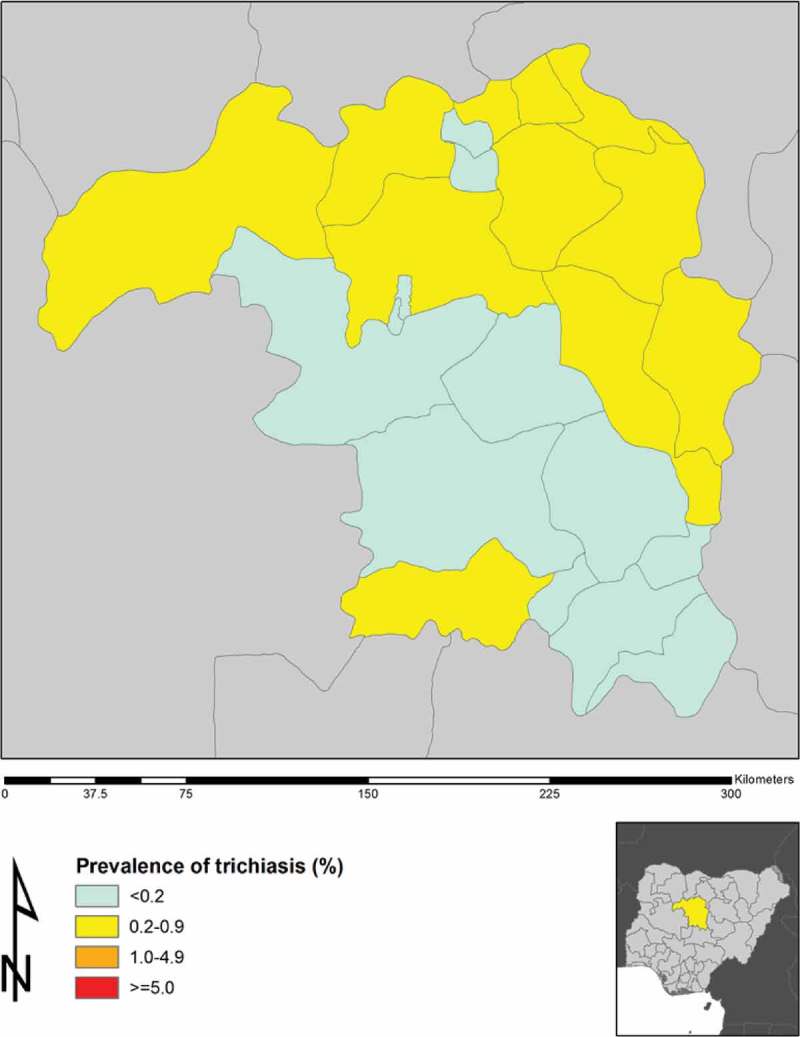
Prevalence of trichiasis in adults aged 15+ years by local government area in Kaduna State, Nigeria, Global Trachoma Mapping Project, 2013.
Water and sanitation coverage
The proportion of households with access to an improved water source ranged from 9% in Kudan to 96% in Jema’a LGA (Table 2). Access to water inside the compound or within 1 km of the house was lowest in Zangon Kataf (53%) and universal in Giwa (100%). Household-level latrine access ranged from 5% in Giwa to 100% in Kudan and Soba (Table 2).
Table 2.
Household access to water and sanitation facilities in Kaduna State, Nigeria, Global Trachoma Mapping Project, 2013.
| Local Government Area | Households enumerated, n | Proportion of households, % |
||
|---|---|---|---|---|
| With access toimproved water source | With water sourcewithin yard/1 km | With access to improvedsanitation facilities | ||
| Birnin Gwari | 612 | 45 | 78 | 96 |
| Chikun | 632 | 61 | 95 | 43 |
| Giwa | 614 | 50 | 100 | 5 |
| Igabi | 624 | 26 | 99 | 8 |
| Ikara | 613 | 79 | 96 | 19 |
| Jaba | 623 | 67 | 87 | 44 |
| Jema’a | 623 | 96 | 79 | 83 |
| Kachia | 616 | 56 | 86 | 24 |
| Kaduna North | 615 | 84 | 86 | 99 |
| Kaduna South | 613 | 85 | 94 | 95 |
| Kagarko | 622 | 41 | 93 | 20 |
| Kajuru | 607 | 64 | 89 | 41 |
| Kaura | 613 | 80 | 82 | 82 |
| Kauru | 625 | 27 | 92 | 26 |
| Kubau | 623 | 28 | 99 | 54 |
| Kudan | 616 | 9 | 96 | 99 |
| Lere | 600 | 66 | 98 | 47 |
| Makarfi | 624 | 59 | 95 | 31 |
| Sabon Gari | 626 | 64 | 99 | 49 |
| Sanga | 619 | 68 | 80 | 16 |
| Soba | 624 | 17 | 97 | 99 |
| Zangon Kataf | 613 | 48 | 53 | 8 |
| Zaria | 873 | 56 | 99 | 90 |
Trachoma elimination targets
All LGAs except Igabi recorded TF prevalences <5%. The majority of LGAs had prevalences of trichiasis below the elimination threshold, with ten LGAs needing to carry out more trichiasis surgeries to reach the elimination target of <1 case of unmanaged trichiasis per 1000 total population (0.1%), equivalent to a prevalence of 0.2% in adults aged 15+ years.15
Related targets
Our water, sanitation and hygiene (WASH) data show that United Nations sustainable development goal 6 (“Ensure access to water and sanitation for all”)16 will require considerable work in most LGAs of Kaduna (Table 3). Providing universal access to water and sanitation will help to prevent future recrudescence of trachoma in this population and contribute to the control and elimination of other neglected tropical diseases, as noted in a recent WHO Global Strategy document.17
Table 3.
Activities needed for trachoma elimination as a public health problem and achievement of United Nations sustainable development goal 6 in Kaduna State, Nigeria, as of 2013.
| Local Government Area | 2006 population, n | Households, n (2006 census)8 | Households in need of improved water sources, n | Households in need of latrines, n | Trichiasis surgeries to achieve elimination target (<0.2%), n | Need for mass antibiotic treatment to clear ocular Chlamydia trachomatis infection |
|---|---|---|---|---|---|---|
| Birnin Gwari | 258,581 | 44,643 | 24,554 | 1786 | 290 | Individualized |
| Chikun | 372,272 | 76,289 | 29,936 | 43,698 | 0 | Individualized |
| Giwa | 292,384 | 49,552 | 24,533 | 46,891 | 246 | Individualized |
| Igabi | 430,753 | 77,243 | 56,944 | 70,809 | 338 | Mass treatment (single round before re-survey), or re-survey at finer level |
| Ikara | 194,723 | 34,017 | 7269 | 27,414 | 0 | Individualized |
| Jaba | 155,973 | 29,472 | 9602 | 16,557 | 0 | Individualized |
| Jema’a | 278,202 | 51,839 | 1913 | 8569 | 0 | Individualized |
| Kachia | 252,568 | 47,116 | 20,500 | 35,719 | 0 | Individualized |
| Kaduna North | 364,575 | 71,283 | 11,591 | 813 | 0 | Individualized |
| Kaduna South | 402,731 | 81,693 | 12,524 | 3995 | 0 | Individualized |
| Kagarko | 239,058 | 43,306 | 25,620 | 34,671 | 241 | Individualized |
| Kajuru | 109,810 | 19,183 | 6985 | 11,345 | 0 | Individualized |
| Kaura | 174,626 | 33,008 | 6730 | 6083 | 0 | Individualized |
| Kauru | 221,276 | 38,382 | 27,942 | 28,372 | 372 | Individualized |
| Kubau | 280,704 | 50,606 | 36,472 | 23,233 | 330 | Individualized |
| Kudan | 138,956 | 24,406 | 22,107 | 39 | 93 | Individualized |
| Lere | 339,740 | 57,962 | 19,898 | 30,529 | 1103 | Individualized |
| Makarfi | 146,574 | 26,785 | 10,859 | 18,543 | 107 | Individualized |
| Sabon Gari | 291,358 | 52,977 | 18,955 | 27,251 | 0 | Individualized |
| Sanga | 151,485 | 27,302 | 8734 | 22,846 | 0 | Individualized |
| Soba | 291,173 | 50,483 | 41,664 | 81 | 49 | Individualized |
| Zangon Kataf | 318,991 | 59,646 | 30,843 | 54,880 | 0 | Individualized |
| Zaria | 406,990 | 68,781 | 30,016 | 6775 | 0 | Individualized |
Discussion
The results of this study suggests that active trachoma is not of public health significance in most LGAs of Kaduna State, except Igabi, which could benefit from implementation of the SAFE strategy (surgery, antibiotics, facial cleanliness and environmental improvement), including a single round of mass azithromycin treatment, and implementation of the F and E components before re-survey.18 Alternatively, given Igabi’s relatively large population, consideration could be given to undertaking further surveys at a more granular level, to determine whether there is really a need for interventions throughout the entire LGA. This LGA has a densely populated urban slum that may explain the higher TF prevalence than seen in other LGAs of Kaduna State.
The prevalence of TI was low in all LGAs. The generally low level of trachoma endemicity in Kaduna State may be partly due to ongoing provision of a comprehensive eye care program for more than two decades and the social development efforts that have happened over the same period. Our findings contrast with reports from neighboring Katsina,12,19 Kano,13 Kebbi and Sokoto20 States, and also from the Republic of Niger further to the north,21 where many surveyed evaluation units have recorded TF prevalences higher than 10% and trachomatous trichiasis prevalences higher than 1%.
Trichiasis, the blinding stage of trachoma, was below the elimination threshold (0.2% prevalence in adults) in most LGAs. However, ten of the 23 LGAs may need to undertake more trichiasis surgeries to reach the elimination threshold. The low precision of the trichiasis estimates generated needs to be taken into account when interpreting these data, as previously acknowledged.11 Stakeholders should prioritize these ten LGAs by engaging already-available human resources to offer active trichiasis case finding and community-based surgeries. Eyelid surgery services will need to be continuously available even after elimination end points have been reached, as new cases are likely to continue to develop.
The United Nations Millennium Development Goal target 7C was to halve, by 2015, the proportion of people without sustainable access to safe drinking water and basic sanitation.22 The results of this study provide a snapshot of the 2013 situation in Kaduna. A total of 12 of the 23 LGAs in Kaduna State had <60% of households with access to improved water sources and 15 of 23 LGAs lacked 60% household-level access to improved sanitation. This situation calls for all stakeholders to redouble current efforts at improving access to water and sanitation, if the targets enshrined in the Sustainable Development Goals are to be achieved by 2030.23 We note that in this set of surveys, Igabi, which had the highest TF prevalence, had the second-lowest household-level access to improved sanitation. Even if not necessarily causal, both active trachoma and lack of access to sanitation are markers of deprivation, and prioritizing WASH sector actions to populations with higher trachoma prevalences would go some way towards putting the most vulnerable people first.17
Our data have some limitations. First, a number of LGAs (Table 2) had total populations that exceeded the 250,000 recommended as the upper limit for “districts” in trachoma surveys; it is possible that small foci of disease were missed by chance. Second, the response rate in some LGAs such as Ikara, where only 803 of 1181 resident adults aged 15+ years (68%) were examined, may have introduced bias in the prevalence estimates. In general, however, the response was excellent; examination rates for resident 1–9-year-olds, for example, ranged from 79–100%, with the majority exceeding 90% (Table 1). Third, the random-walk method has been justifiably criticized for potentially permitting biased household selection;24–26 unfortunately, we felt that security considerations here outweighed epidemiological ones. Fourth, because trichiasis is a rare condition, the CIs for estimates of its prevalence are relatively wide.11 Finally, we did not record the presence or absence of trachomatous conjunctival scarring in eyes that had trichiasis; the recognition that this might be critical for distinguishing trachomatous from non-trachomatous trichiasis did not emerge until 2015,27 after these surveys were completed.
These surveys show that Kaduna State has relatively hypoendemic trachoma. To reach the trachoma elimination threshold (trichiasis prevalences <0.2% in adults aged 15+ years and TF prevalences <5% in 1–9-year-olds), provision of community-based trichiasis surgery for 11 LGAs, and implementation of the A, F and E components of the SAFE strategy in one LGA will be needed. Our data also demonstrate a particular need for attention towards improving access to appropriate water and sanitation facilities for the local population.
Appendix
The Global Trachoma Mapping Project Investigators are: Agatha Aboe (1,11), Liknaw Adamu (4), Wondu Alemayehu (4,5), Menbere Alemu (4), Neal D. E. Alexander (9), Berhanu Bero (4), Simon J. Brooker (1,6), Simon Bush (7,8), Brian K. Chu (2,9), Paul Courtright (1,3,4,7,11), Michael Dejene (3), Paul M. Emerson (1,6,7), Rebecca M. Flueckiger (2), Allen Foster (1,7), Solomon Gadisa (4), Katherine Gass (6,9), Teshome Gebre (4), Zelalem Habtamu (4), Danny Haddad (1,6,7,8), Erik Harvey (1,6,10), Dominic Haslam (8), Khumbo Kalua (5), Amir B. Kello (4,5), Jonathan D. King (6,10,11), Richard Le Mesurier (4,7), Susan Lewallen (4,11), Thomas M. Lietman (10), Chad MacArthur (6,11), Colin Macleod (3,9), Silvio P. Mariotti (7,11), Anna Massey (8), Els Mathieu (6,11), Siobhain McCullagh (8), Addis Mekasha (4), Tom Millar (4,8), Caleb Mpyet (3,5), Beatriz Muñoz (6,9), Jeremiah Ngondi (1,3,6,11), Stephanie Ogden (6), Alex Pavluck (2,4,10), Joseph Pearce (10), Serge Resnikoff (1), Virginia Sarah (4), Boubacar Sarr (5), Alemayehu Sisay (4), Jennifer L. Smith (11), Anthony W. Solomon (1,2,3,4,5,6,7,8,9,10,11), Jo Thomson (4); Sheila K. West (1,10,11), Rebecca Willis (2,9).
Key: (1) Advisory Committee, (2) Information Technology, Geographical Information Systems, and Data Processing, (3) Epidemiological Support, (4) Ethiopia Pilot Team, (5) Master Grader Trainers, (6) Methodologies Working Group, (7) Prioritisation Working Group, (8) Proposal Development, Finances and Logistics, (9) Statistics and Data Analysis, (10) Tools Working Group, (11) Training Working Group.
Funding Statement
This study was principally funded by the Global Trachoma Mapping Project (GTMP) grant from the United Kingdom’s Department for International Development (ARIES: 203145) to Sightsavers, which led a consortium of non-governmental organizations and academic institutions to support ministries of health to complete baseline trachoma mapping worldwide. The GTMP was also funded by the United States Agency for International Development (USAID) through the ENVISION project implemented by RTI International under cooperative agreement number AID-OAA-A-11-00048, and the END in Asia project implemented by FHI360 under cooperative agreement number OAA-A-10-00051. A committee established in March 2012 to examine issues surrounding completion of global trachoma mapping was initially funded by a grant from Pfizer to the International Trachoma Initiative. BAG is an employee of the World Health Organization (WHO); the views expressed in this article are the views of the authors alone and do not necessarily reflect the views or policy of WHO. AWS was a Wellcome Trust Intermediate Clinical Fellow (098521) at the London School of Hygiene & Tropical Medicine. None of the funders had any role in project design, in project implementation or analysis or interpretation of data, in the decisions on where, how or when to publish in the peer-reviewed press, or in the preparation of the manuscript.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Funding
This study was principally funded by the Global Trachoma Mapping Project (GTMP) grant from the United Kingdom’s Department for International Development (ARIES: 203145) to Sightsavers, which led a consortium of non-governmental organizations and academic institutions to support ministries of health to complete baseline trachoma mapping worldwide. The GTMP was also funded by the United States Agency for International Development (USAID) through the ENVISION project implemented by RTI International under cooperative agreement number AID-OAA-A-11-00048, and the END in Asia project implemented by FHI360 under cooperative agreement number OAA-A-10-00051. A committee established in March 2012 to examine issues surrounding completion of global trachoma mapping was initially funded by a grant from Pfizer to the International Trachoma Initiative. BAG is an employee of the World Health Organization (WHO); the views expressed in this article are the views of the authors alone and do not necessarily reflect the views or policy of WHO. AWS was a Wellcome Trust Intermediate Clinical Fellow (098521) at the London School of Hygiene & Tropical Medicine. None of the funders had any role in project design, in project implementation or analysis or interpretation of data, in the decisions on where, how or when to publish in the peer-reviewed press, or in the preparation of the manuscript.
References
- 1. Bourne RRA, Stevens GA, White RA, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Global Health 2013;1:e339–349. [DOI] [PubMed] [Google Scholar]
- 2. Solomon AW, Zondervan M, Kuper H, et al. Trachoma control: a guide for program managers. Geneva: World Health Organization, 2006. [Google Scholar]
- 3. Smith JL, Haddad D, Polack S, et al. Mapping the global distribution of trachoma: why an updated atlas is needed. PLoS Negl Trop Dis 2011;5:e973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Solomon AW, The Global Kurylo E.. Trachoma Mapping Project. Comm Eye Health 2014;27(85):18. [PMC free article] [PubMed] [Google Scholar]
- 5. Emerson P. The SAFE strategy for trachoma control: poised for rapid scale-up. Comm Eye Health 2014;27(86):38. [PMC free article] [PubMed] [Google Scholar]
- 6. Kaduna State Government About Kaduna state. Available at: www.kadunastate.gov.ng Accessed 22 December; 2013. [Google Scholar]
- 7. National Population Commission 2006 National and state population and housing tables – Priority tables I. Abuja, Nigeria: Author, 2010. [Google Scholar]
- 8. National Population Commission 2006. Housing characteristics and amenities tables – Priority tables (LGA) volume II. Abuja, Nigeria: Author, 2010. [Google Scholar]
- 9. Rabiu MM. Prevalence of blindness and low vision in north central, Nigeria. West Afr J Med 2008;27:238–244. [PubMed] [Google Scholar]
- 10. Thylefors B, Dawson CR, Jones BR, et al. A simple system for the assessment of trachoma and its complications. Bull World Health Organ 1987;65:477–483. [PMC free article] [PubMed] [Google Scholar]
- 11. Solomon AW, Pavluck AL, Courtright P, et al. The Global Trachoma Mapping Project: methodology of a 34-country population-based study. Ophthalmic Epidemiol 2015;22:214–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mpyet C, Muhammad N, Adamu MD, et al. Prevalence of trachoma in Katsina state, Nigeria: results of 34 district-level surveys. Ophthalmic Epidemiol 2016;23(S1):55–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Mpyet C, Muhammad N, Adamu MD, et al. Prevalence of trachoma in Kano state, Nigeria: results of 44 local government area-level surveys. Ophthalmic Epidemiol. doi: 10.1080/09286586.2016.1265657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Mpyet C, Muhammad N, Adamu MD, et al. Prevalence of trachoma in Bauchi state, Nigeria: results of 20 local government area-level surveys. Ophthalmic Epidemiol 2016;23(S1):39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. World Health Organization Report of the 2nd global scientific meeting on trachoma, Geneva, 25–27 August, 2003 Geneva: World Health Organization, 2003. [Google Scholar]
- 16. United Nations General Assembly. Resolution adopted by the General Assembly on 25 September 2015 (A/70/L.1) Transforming our world: the 2030 agenda for sustainable development New York: United Nations, 2015. [Google Scholar]
- 17. Boisson S, Engels D, Gordon BA, et al. Water, sanitation and hygiene for accelerating and sustaining progress on neglected tropical diseases: a new Global Strategy 2015–20. Intl Health 2016;8(Suppl. 1):i19–i21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. World Health Organization Technical Consultation on Trachoma Surveillance Meeting Report Decatur, GA, USA, 2014. [Google Scholar]
- 19. Jip NF, King JD, Diallo MO, et al Blinding trachoma in Katsina State, Nigeria: population-based prevalence survey in ten local government areas. Ophthalmic Epidemiol 2008;15:294–302. [DOI] [PubMed] [Google Scholar]
- 20. Muhammad N, Mohammed A, Isiyaku S, et al. Mapping trachoma in 25 local government areas of Sokoto and Kebbi states, northwestern Nigeria. Br J Ophthalmol 2014;98:432–437. [DOI] [PubMed] [Google Scholar]
- 21. Cromwell EA, Amza A, Kadri B, et al. Trachoma prevalence in Niger: results of 31 district-level surveys. Trans R Soc Trop Med Hyg 2014;108:42–48. [DOI] [PubMed] [Google Scholar]
- 22. International Agency for the Prevention of Blindness. Blindness, poverty and development: the impact of VISION 2020 on the U.N. Millennium Development Goals. 2006 12 pp. Available from: http://www.v2020.org Accessed 26 April 2014.
- 23. World Health Organization. Health in 2015 from MDGs to SDGs; 2015:216 pp. [Google Scholar]
- 24. Turner AG, Magnani RJ, Shuaib M.. A not quite as quick but much cleaner alternative to the Expanded Programme on Immunization (EPI) cluster survey design. Int J Epidemiol 1996, 25:198–203. [DOI] [PubMed] [Google Scholar]
- 25. Brogan D, Flagg EW, Deming M, et al. Increasing the accuracy of the Expanded Programme on Immunization’s cluster survey design. Ann Epidemiol 1994;4:302–311. [DOI] [PubMed] [Google Scholar]
- 26. Grais RF, Rose AMC, Guthmann JP.. Don’t spin the pen: two alternative methods for second stage sampling in cluster surveys in urban zones. Emerg Themes Epidemiol 2007;4:8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. World Health Organization Alliance for the Global Elimination of Trachoma by 2020. Second Global Scientific Meeting on Trachomatous Trichiasis, November 4–6, 2015, Cape Town, South Africa. Geneva: World Health Organization, 2016. [Google Scholar]


