ABSTRACT
Purpose: In Ethiopia, trachoma is a major public health problem, accounting for 11.5% of all cases of blindness. In Gambella, one of the country’s most remote regions, the 2005–2006 National Survey of Blindness, Low Vision and Trachoma estimated a region-level prevalence of active trachoma of 19.1% in those aged 1–9 years. Detailed district or sub-regional level estimates are required to implement interventions.
Methods: Population-based prevalence surveys were carried out following a 2-stage cluster random sampling methodology and Global Trachoma Mapping Project protocols. As the 13 districts (woredas) in Gambella had relatively small populations, they were grouped together to form three evaluation units (EUs) of about 100,000 persons each, and all subsequent survey planning and sampling was carried out at EU-level.
Results: Altogether, 558 cases of TF (17.2%) were identified in 3238 children aged 1–9 years across the three EUs. The adjusted TF prevalences in 1–9-year-olds for the three EUs were 11.5%, 12.5% and 19.3%; 14.4% for Gambella overall. A total of 142 cases of trichiasis (3.8%) were identified among 3781 adults aged 15 years or older, with age- and sex-adjusted EU-level trichiasis prevalences in adults being 0.8%, 1.3% and 2.4%; 1.5% overall.
Conclusion: The high prevalences of TF and trichiasis throughout Gambella indicate a need for rapid scaling up of the World Health Organization SAFE strategy (surgery, antibiotics, facial cleanliness, and environmental improvement) to help meet the 2020 target of global elimination of trachoma as a public health problem.
KEYWORDS: Ethiopia, Gambella, mapping, prevalence, trachoma
Introduction
Trachoma is caused by ocular infection with the obligate intracellular bacterium Chlamydia trachomatis. It is the leading infectious cause of blindness, responsible for 1.4% of all blindness worldwide.1 According to estimates for 2011, 7.3 million people worldwide have trichiasis, the potentially blinding stage of the disease.2 In addition to causing blindness, trachoma limits access to education and prevents individuals from being able to work or care for themselves or their families. Trachoma can have a detrimental effect on the economic well-being of communities, with conservative estimates suggesting a total loss of productivity due to trachoma for the visually impaired or blind and their caregivers of between $3 billion and $8 billion annually.3
In Ethiopia, trachoma is a major public health problem, accounting for 11.5% of all cases of blindness.4 It is endemic in all regions, with an estimated 65 million people at risk.4 There is an urgent need to complete the map of trachoma globally to appropriately target resources towards the goal of elimination as a public health problem by the year 2020. The World Health Organization (WHO) simplified trachoma grading system5,6 was designed to be an effective tool for use in large-scale public health surveys. In this scheme, trachomatous inflammation – follicular (TF) is said to be present if five or more follicles each >0.5 mm in diameter are present in the central upper tarsal conjunctiva. If greater than half the normal deep tarsal vessels are obscured by pronounced inflammatory thickening, then the sign trachomatous inflammation – intense (TI) is present. If at least one eyelash touches the eyeball, then trichiasis is present.
The Global Trachoma Mapping Project (GTMP)7 aimed to complete the map of trachoma in all suspected-endemic districts worldwide. District-level TF prevalence in children aged 1–9 years is the key indicator for determining the requirement for three of four components of the SAFE strategy (surgery, antibiotics, facial cleanliness, and environmental improvement); A, F, and E.8,9 A district, in the context of the statement above, represents the normal administrative unit for health care management, which for purposes of clarification consists of a population unit between 100,000 and 250,000 people.10 The prevalence of trichiasis in adults aged 15 years and older is helpful for planning surgical interventions, the S component of the SAFE strategy.8,9
Gambella is one of the most remote and underdeveloped regions in Ethiopia. The region is located on the western tip of the country and borders South Sudan to the west, south and north, Oromia Region to the north-east, and the Southern Nations, Nationalities and People’s Region (SNNPR) to the east. It covers an area of 25,802km2 and has an estimated population of 383,000, of whom 70% live in rural areas.11 The administrative structure in Gambella consists of two zones, subdivided into 13 districts (woredas). According to the national health indicator report (2012/13), household-level access to any kind of sanitation facility is 34% in Gambella.12 There is only one hospital in the region, supported by 28 health centers and 105 rural health posts. The health force includes 14 physicians, 49 health officers, and 500 nurses.12
Trachoma surveys in Gambella have been difficult to plan and conduct due to the remote terrain, and transmission of trachoma in Gambella may be influenced by influxes of refugees from neighboring South Sudan, where trachoma is hyper-endemic.13,14 A study in 2012 found 99 cases of trachomatous trichiasis (19.2%) from only 515 people examined in a refugee camp in Fugnido, Gambella,15 and the 2005–2006 National Survey of Blindness, Low Vision and Trachoma estimated a regional prevalence of active trachoma (TF and/or TI) in Gambella of 19.1% in those aged 1–9 years.16
Eye care services in Gambella are severely limited, with only one ophthalmic nurse for the region and no integrated eye care workers or ophthalmologists. Data on eye care from health facilities are scarce. Although one Gambella zone (Nuer) was listed as a priority for the first phase of the Ethiopian national program for trachoma mapping in 2010–2011, there was no woreda-level mapping of trachoma in the region prior to 2013.
We carried out population-based prevalence surveys covering all woredas in Gambella. Because woreda populations were low, the 13 woredas were grouped into three evaluation units (EUs), each comprising populations of approximately 100,000 inhabitants, and all subsequent survey planning and sampling was carried out at EU-level (Figure 1). Figure 1 first mention. The objectives of this study were to estimate the EU-level TF prevalence in children aged 1–9 years, and the EU-level trichiasis prevalence in those aged 15 years and older.
Figure 1.
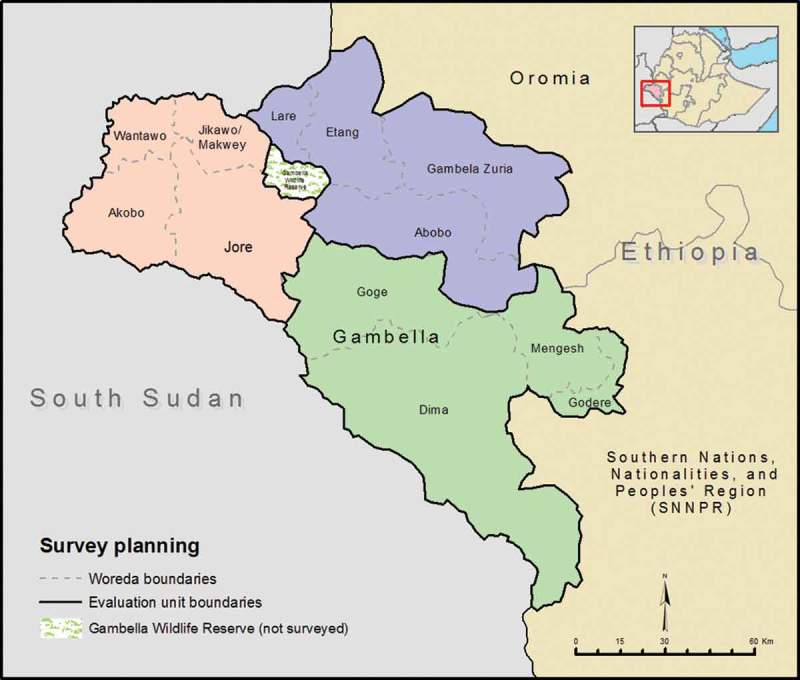
Evaluation unit boundaries, Global Trachoma Mapping Project, Gambella, Ethiopia, 2013–2014.
Materials and methods
Ethics
Ethics clearance was obtained from the ethics committees of the Gambella Health Bureau (To/9666/06), the London School of Hygiene & Tropical Medicine (6319), and the Johns Hopkins Bloomberg School of Public Health. Zonal and woreda health officers approved plans for community sensitization before survey teams arrived at each village (kebele). Informed verbal consent was obtained from household heads and from each individual aged ≥15 years. For those aged between 7 and 15 years, informed verbal assent along with parental or guardian consent was obtained. For those younger than 7 years, parental or guardian verbal consent was considered acceptable.
All individuals found to have active trachoma were provided with 1% tetracycline eye ointment to apply twice daily for 6 weeks, and those with trichiasis were referred to the nearest health institution for appropriate management. Residents of selected villages were informed that they had the right not to participate in the survey, not to respond to uncomfortable questions and to stop responding to questions or terminate the examination at any time, without impacting on their normal health care.
Survey sampling
GTMP standard protocols have been described elsewhere.7 We used a 2-stage cluster random sampling methodology. All 13 woredas in Gambella were included, with each woreda contributing clusters to its EU in proportion to its population size. Urban areas, defined as localities with 2000 or more inhabitants, and all region, zone, and woreda administrative capitals, were excluded from the sampling frame.11
At the first stage of sampling, clusters (kebeles) were randomly selected with a probability proportional to their population size. Kebeles are organized in gares (clusters of 25–35 households). On the day of fieldwork, a gare was selected from the list of gares in the kebele obtained from local leaders or healthcare workers. Starting from the household first reached in a gare, all households in a gare until 30 households were reached were included. In cases where a gare had <30 households, the survey team continued with the next household in the neighboring gare and proceeded until 30 households were reached. This procedure was varied for Akobo woreda because at the time of the survey, people normally resident in Akobo were displaced from their homes due to unrest in neighboring South Sudan, and had been housed in temporary settlement camps. For Akobo, we selected the required number of households using systematic sampling, with a list of heads of households in camps supplied by the Regional Health Bureau as the sampling frame.
Teams went from house to house. All residents of selected households aged 1 year or older were eligible for inclusion in the surveys. Graders examined each consenting person using the WHO simplified trachoma grading system5,6 (Table 1).
Table 1.
Number of clusters (kebeles) selected from each evaluation unit, Global Trachoma Mapping Project, Gambella, Ethiopia, 2013-2014.
| Woredas per evaluation unit | Rural populationa, n | Total rural kebeles, n | Selected kebelesb, n |
|---|---|---|---|
| Makwey | 18,086 | 18 | 5 |
| Wantawo | 24,329 | 20 | 6 |
| Akobo | 24,044 | 20 | 6 |
| Jore | 9,686 | 13 | 2 |
| Jikawo | 25,736 | 24 | 7 |
| Total | 101,881 | 95 | 26 |
| Godere | 42,286 | 12 | 8 |
| Mengesh | 24,883 | 17 | 4 |
| Dima | 10,073 | 17 | 2 |
| Goge | 63,543 | 19 | 12 |
| Total | 140,785 | 65 | 26 |
| Abobo | 20,078 | 17 | 4 |
| Gambella Zuria | 10,212 | 11 | 2 |
| Etang | 48,430 | 23 | 11 |
| Lare | 39,841 | 26 | 9 |
| Total | 118,561 | 77 | 26 |
aRegional health bureau projected estimates from the 2007 Ethiopian Census.
bNumber of kebeles selected in each woreda was proportional to the woreda population in a given evaluation unit.
Sample size
To estimate the prevalence of TF in children aged 1–9 years with 95% confidence at the 10% level with precision of ±3%, a sample size of 1.019 children was needed.7 Inflating this by 1.2 for non-response means that we needed to select sufficient households to reach 1222 children. With the expectation that a team would be able to complete 30 households per day, the cluster size was fixed at 30 households. From the 2007 Gambella census,17 we expected 48 1–9-year-olds for every 30-household cluster. We therefore estimated we would need 26 clusters per EU.
Training
Each survey team consisted of a trachoma grader and a recorder. Graders and recorders were trained using the standardized GTMP training system (version 2) and had to pass in-field examinations to be eligible to be survey team members.7 A standardized field guide in research ethics was included as part of the training.18 Training of graders and recorders was carried out in Wolkite, in the Southern Nations and Nationalities Region of Ethiopia, from November 28 to December 6, 2013. A total of 13 survey teams were subsequently formed.
Quality control
Two supervisors (ophthalmologists who were GTMP-certified grader trainers) were deployed with the teams. Each supervisor was responsible for six or seven teams and spent at least 1 day with each team during the mapping period. They ensured proper diagnostic procedures and data recording. They also reviewed all teams’ activities at the end of each day and gave feedback to team members.
Data management, analysis and reporting
Data were collected using the LINKS app (Task Force for Global Health, Decatur, GA, USA) on Android smartphones. The app automatically encrypted data and transmitted them to a secure server as soon as a mobile network was available. Anonymized data were subsequently used for analysis.
A cleaned dataset was reviewed and approved by the Gambella Health Bureau and Federal Ministry of Health of Ethiopia. Cluster-level TF prevalences were adjusted in 1-year age-bands in children aged 1–9 years, with the overall EU-level TF prevalence being the mean of all adjusted cluster-level prevalences. Trichiasis cluster-level prevalences in those aged 15 years and older were adjusted for sex and age in 5-year age-bands using the latest available census data,11 with the overall EU-level trichiasis prevalence estimated as the mean of all adjusted cluster-level trichiasis prevalences. Full details of the analysis are outlined elsewhere.7
Results
The surveys were carried out from December 18, 2013, to January 30, 2014. A total of three EUs were surveyed, with 8599 individuals from 2143 households enumerated for inclusion in the surveys. Of those enumerated, 8018 (93.2%) were examined, and 56 (0.7%) refused. A total of 525 individuals (6.1%) were absent at the time of survey. Of those examined, 4684 were female (58.4%). Overall, 3324 children aged 1–9 years, and 4185 individuals aged ≥15 years were examined. The mean age of those examined was 19.8 years. The baseline characteristics of those examined in each EU are presented in Table 2.
Table 2.
Characteristics of enumerated individuals, Global Trachoma Mapping Project, Gambella, Ethiopia, 2013-2014.
| Examined, n |
Absent, n |
Refused, n |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Evaluation unit | All | Male | Female | All | Male | Female | All | Male | Female | Total |
| Makwey, Wantawo, Akobo, Jore, Jikawo | 2,790 | 1,123 | 1,667 | 166 | 124 | 42 | 18 | 7 | 11 | 2,974 |
| Godere, Mengesh, Dima, Gog | 2,568 | 1,088 | 1,480 | 192 | 125 | 67 | 15 | 6 | 9 | 2,775 |
| Abobo, Gambela Zuria, Etang, Lare | 2,660 | 1,123 | 1,537 | 167 | 95 | 72 | 23 | 7 | 16 | 2,850 |
| Total | 8,018 | 3,334 | 4,684 | 525 | 344 | 181 | 56 | 20 | 36 | 8,599 |
Across the three EUs, 558 cases of TF (17.2%) were identified out of 3238 children aged 1–9 years examined. The distribution of these cases by EU is shown in Table 3 and Figure 2. Each EU had a TF prevalence in those aged 1–9 years above the WHO 10% threshold for full implementation of the A, F and E components of SAFE, including mass drug administration (MDA) of azithromycin.
Table 3.
Prevalences of trachomatous inflammation — follicular (TF) and trichiasis by evaluation unit, Global Trachoma Mapping Project, Gambella, Ethiopia, 2013-2014.
| Age 1-9 years |
Age ≥15 years |
|||||||
|---|---|---|---|---|---|---|---|---|
| Evaluation unit | Examined, n | TF cases, n | Unadjusted TF, % | Adjusteda TF, % (95% CIb) | Examined, n | Trichiasis cases, n | Unadjusted trichiasis, % | Adjustedc trichiasis, % (95% CIb) |
| Makwey, Wantawo, Akobo, Jore, Jikawo | 904 | 143 | 15.8 | 11.5 (7.3-15.3) | 1,411 | 23 | 1.6 | 0.8 (0.5-1.2) |
| Godere, Mengesh, Dima, Gog | 1,301 | 252 | 19.4 | 19.3 (15.2-24.2) | 1,165 | 84 | 7.2 | 2.4 (1.7-3.3) |
| Abobo, Gambela Zuria, Etang, Lare | 1,119 | 163 | 14.6 | 12.5 (9.1-16.1) | 1,205 | 35 | 2.9 | 1.3 (0.7-1.9) |
| Total | 3,324 | 558 | 16.6 | 14.4 | 3,781 | 142 | 3.8 | 1.5 |
aAdjusted for age by year using Gambella Region data from the Ethiopian Census 2007.
b95% CI estimated by bootstrapping adjusted cluster-level estimates over 10,000 iterations.
cAdjusted for sex and age in 5-year bands using Gambella Region data from the Ethiopian Census 2007.
CI, confidence interval.
Figure 2.

Distribution of trachomatous inflammation – follicular (TF) prevalence in 1–9-year-olds at evaluation unit level, Global Trachoma Mapping Project, Gambella, Ethiopia, 2013–2014.
A total of 142 cases of trichiasis (3.8%) were identified across the three EUs, among 3781 participants examined who were aged 15 years or older. The estimated sex- and age-adjusted trichiasis prevalence in those aged 15 years or older is shown for each EU in Table 3 and Figure 3.
Figure 3.
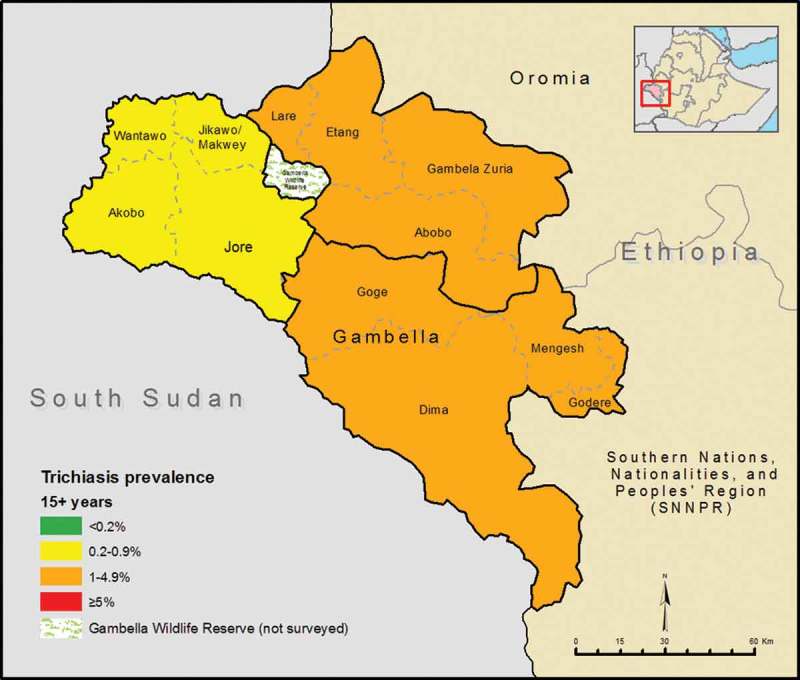
Distribution of trichiasis prevalence in those aged 15 years or older at evaluation unit level, Global Trachoma Mapping Project, Gambella, Ethiopia, 2013–2014.
Discussion
There is a moderately high prevalence of trachoma throughout Gambella, with estimates from these surveys largely in agreement with the 14.6% regional TF prevalence estimate from the national survey of 2005–2006.16 In the global context, the TF prevalences recorded here are high, particularly when compared to the WHO 5% TF elimination threshold, but they are noticeably lower than TF prevalences in adjacent areas of SNNPR19 and Oromia.20 TF prevalences above 10% mandate full implementation of the A, F and E components of the SAFE strategy. These interventions should be continued for 3 years before re-surveying to gauge the impact of the program.
These are the first high-resolution estimates of trachoma prevalence in Gambella, and will allow more accurate estimates to be made of the number of people with trichiasis needing treatment than have previously been available. Further work is still needed to determine the relative impacts of mortality in unoperated individuals with trichiasis, surgical interventions, post-surgical recurrence, and incident trichiasis (in the years before the A, F and E interventions begin to halt progression of trachoma) on surgical backlog numbers; to avoid fixing a false target, we have not provided a total surgical backlog number for the region here. Trichiasis patients are those at imminent risk of developing irreversible blindness, and therefore identifying and treating these patients must be a priority. There is an urgent need for fundraising, planning, and training to increase the local capacity to deal with trichiasis cases over the coming years.
There was some variability in the trichiasis prevalences between EUs. The reason for this is unclear. However, in the latest estimates available from the United Nations High Commissioner for Refugees, Gambella has a refugee population of 269,853 individuals.21 The degree to which refugees contribute to the variation in trichiasis prevalence is unknown, and further study is required. Implementation of the SAFE strategy in the refugee and displaced population is likely to be a challenge, due to occasional uncertain security, population efflux complicating surgical follow-up, and continuing immigration compromising the effectiveness of both antibiotic MDA and facial cleanliness promotion.
Although there are current efforts to improve water supply and sanitation in Gambella, they are not tied to trachoma elimination programs. Two ophthalmic nurses provide trichiasis surgery and occasional community outreach, but these activities will not be sufficient to address the large backlog of trichiasis surgery in the region. No MDA for trachoma has yet been started in Gambella.
A significant up-scaling of efforts is needed to eliminate trachoma from Gambella. It is hoped that the publication of these results can serve to highlight the need for research, collaboration and funding that will advance the goal of elimination of trachoma from the region by 2020.
Appendix
The Global Trachoma Mapping Project Investigators are: Agatha Aboe (1,11), Liknaw Adamu (4), Wondu Alemayehu (4,5), Menbere Alemu (4), Neal D. E. Alexander (9), Berhanu Bero (4), Simon J. Brooker (1,6), Simon Bush (7,8), Brian K. Chu (2,9), Paul Courtright (1,3,4,7,11), Michael Dejene (3), Paul M. Emerson (1,6,7), Rebecca M. Flueckiger (2), Allen Foster (1,7), Solomon Gadisa (4), Katherine Gass (6,9), Teshome Gebre (4), Zelalem Habtamu (4), Danny Haddad (1,6,7,8), Erik Harvey (1,6,10), Dominic Haslam (8), Khumbo Kalua (5), Amir B. Kello (4,5), Jonathan D. King (6,10,11), Richard Le Mesurier (4,7), Susan Lewallen (4,11), Thomas M. Lietman (10), Chad MacArthur (6,11), Colin Macleod (3,9), Silvio P. Mariotti (7,11), Anna Massey (8), Els Mathieu (6,11), Siobhain McCullagh (8), Addis Mekasha (4), Tom Millar (4,8), Caleb Mpyet (3,5), Beatriz Muñoz (6,9), Jeremiah Ngondi (1,3,6,11), Stephanie Ogden (6), Alex Pavluck (2,4,10), Joseph Pearce (10), Serge Resnikoff (1), Virginia Sarah (4), Boubacar Sarr (5), Alemayehu Sisay (4), Jennifer L. Smith (11), Anthony W. Solomon (1,2,3,4,5,6,7,8,9,10,11), Jo Thomson (4); Sheila K. West (1,10,11), Rebecca Willis (2,9).
Key: (1) Advisory Committee, (2) Information Technology, Geographical Information Systems, and Data Processing, (3) Epidemiological Support, (4) Ethiopia Pilot Team, (5) Master Grader Trainers, (6) Methodologies Working Group, (7) Prioritisation Working Group, (8) Proposal Development, Finances and Logistics, (9) Statistics and Data Analysis, (10) Tools Working Group, (11) Training Working Group.
Funding Statement
This study was principally funded by the Global Trachoma Mapping Project (GTMP) grant from the United Kingdom’s Department for International Development (ARIES: 203145) to Sightsavers, which led a consortium of non-governmental organizations and academic institutions to support ministries of health to complete baseline trachoma mapping worldwide. The GTMP was also funded by the United States Agency for International Development (USAID), through the ENVISION project implemented by RTI International under cooperative agreement number AID-OAA-A-11-00048, and the END in Asia project implemented by FHI360 under cooperative agreement number OAA-A-10-00051. A committee established in March 2012 to examine issues surrounding completion of global trachoma mapping was initially funded by a grant from Pfizer to the International Trachoma Initiative. AWS was a Wellcome Trust Intermediate Clinical Fellow (098521) at the London School of Hygiene & Tropical Medicine. None of the funders had any role in project design, in project implementation or analysis or interpretation of data, in the decisions on where, how or when to publish in the peer-reviewed press, or in the preparation of the manuscript.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Funding
This study was principally funded by the Global Trachoma Mapping Project (GTMP) grant from the United Kingdom’s Department for International Development (ARIES: 203145) to Sightsavers, which led a consortium of non-governmental organizations and academic institutions to support ministries of health to complete baseline trachoma mapping worldwide. The GTMP was also funded by the United States Agency for International Development (USAID), through the ENVISION project implemented by RTI International under cooperative agreement number AID-OAA-A-11-00048, and the END in Asia project implemented by FHI360 under cooperative agreement number OAA-A-10-00051. A committee established in March 2012 to examine issues surrounding completion of global trachoma mapping was initially funded by a grant from Pfizer to the International Trachoma Initiative. AWS was a Wellcome Trust Intermediate Clinical Fellow (098521) at the London School of Hygiene & Tropical Medicine. None of the funders had any role in project design, in project implementation or analysis or interpretation of data, in the decisions on where, how or when to publish in the peer-reviewed press, or in the preparation of the manuscript.
References
- 1. Bourne RRA, Stevens GA, White RA, et al. Causes of vision loss worldwide, 1990–2010: a systematic analysis. Lancet Glob Health 2013;1(6):e339–e349. [DOI] [PubMed] [Google Scholar]
- 2. Global WHO Alliance for the Elimination of Blinding Trachoma by 2020. Wkly Epidemiol Rec 2012;87(17):161–168. [PubMed] [Google Scholar]
- 3. Burton MJ, Mabey DCW.. The global burden of trachoma: a review. PLoS Negl Trop Dis 2009;3(10): e460. doi: 10.1371/journal.pntd.0000460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Berhane Y, Worku A, Bejiga A, et al. Prevalence and causes of blindness and low vision in Ethiopia. Ethiop J Health Dev 2008;21:204–210. [Google Scholar]
- 5. Thylefors B, Dawson CR, Jones BR, et al. A simple system for the assessment of trachoma and its complications. Bull World Health Organ 1987;65:477–483. [PMC free article] [PubMed] [Google Scholar]
- 6. Solomon AW, Peeling RW, Foster A, et al Diagnosis and assessment of trachoma. Clin Microbiol Rev 2004;17:982–1011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Solomon AW, Pavluck A, Courtright P, et al. The Global Trachoma Mapping Project: methodology of a 34-country population-based study. Ophthalmic Epidemiol 2015;22:214–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bailey R, Lietman T.. The SAFE strategy for the elimination of trachoma by 2020: will it work? Bull World Health Organ 2001;79:233–236. [PMC free article] [PubMed] [Google Scholar]
- 9. Emerson PM, Burton M, Solomon AW, et al. The SAFE strategy for trachoma control: using operational research for policy, planning and implementation. Bull World Health Organ 2006;84:613–619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. World Health Organization Report of the 3rd Global Scientific Meeting on Trachoma, Johns Hopkins University, Baltimore, MD, 19–20 July 2010. Geneva: World Health Organization, 2010. [Google Scholar]
- 11. Central Statistical Agency of Ethiopia Population and Housing Census Report 2007 Addis Ababa: Federal Democratic Republic of Ethiopia Population Census Commission, 2008. [Google Scholar]
- 12. Federal Ministry of Health of Ethiopia Health and Health Related Indicators. Addis Ababa: Federal Ministry of Health of Ethiopia, 2005. [Google Scholar]
- 13. Robinson E, Kur LW, Ndyaba A, et al. Trachoma rapid assessments in Unity and Northern Bahr-el-Ghazal States, Southern Sudan. PLoS One 2010;5(10):e13138. doi: 10.1371/journal.pone.0013138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Edwards T, Smith J, Sturrock HJW, et al. Prevalence of trachoma in Unity State, South Sudan: results from a large-scale population-based survey and potential implications for further surveys. PLoS Negl Trop Dis 2012;6(4):e1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Gelaw Y, Abateneh A.. Blinding trachoma among refugees: complicating social disaster. Asian Pac J Trop Biomed 2015;5:124–127. [Google Scholar]
- 16. Berhane Y, Worku A, Bejiga A, et al. National Survey on Blindness, Low Vision and Trachoma in Ethiopia, Vol 21 Addis Ababa, 2006. [Google Scholar]
- 17. Central Statistical Agency Federal Democratic Republic of Ethiopia Population Census. Addis Ababa: Federal Democratic Republic of Ethiopia Population Census Commission, 2007. [Google Scholar]
- 18. Johns Hopkins University Human Subjects Research Ethics Field Training Guide. Baltimore: Johns Hopkins University, 2010. [Google Scholar]
- 19. Adera TH, Macleod C, Endriyas M, et al. Prevalence of and risk factors for trachoma in Southern Nations, Nationalities, and Peoples’ Region, Ethiopia: results of 40 population-based prevalence surveys carried out with the Global Trachoma Mapping Project. Ophthalmic Epidemiol 2016;23(S1):84–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Bero B, Macleod CK, Alemayehu W, et al. Prevalence of and risk factors for trachoma in Oromia Regional State of Ethiopia: results of 79 population-based prevlence surveys conducted with the Global Trachoma Mapping Project. Ophthalmic Epidemiol 2016;23:392–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. United Nations High Commissioner for Refugees Refugee Population in Gambella. London: UNHCR, 2016. [Google Scholar]


