Sir,
India accounts for over one-half of the global burden of leprosy cases.[1] According to a recent report by the National Leprosy Elimination Program (NLEP), there were a total of approximately 1.27 lakh new cases of leprosy in India, of which 8.94% were among children.[2] A high proportion of leprosy in children among new cases reflects a high level of transmission of the disease in a given population. If the transmission of leprosy reduces in an area, it is expected that the proportion of children affected will also decrease.[3] Childhood leprosy also determines the efficiency of ongoing disease control programs, therefore, World Health Organization, Regional Office for South- East Asia (WHO SEARO) has declared leprosy as a Flagship Programme that intends to achieve zero child cases and grade 2 disability by 2020.
This study was conducted to assess the current scenario and clinical profile of childhood leprosy at a tertiary care teaching hospital in Southern Rajasthan. All the confirmed cases of childhood (≤14 years) leprosy (by clinical history, cutaneous examination, slit skin smear, and skin biopsy) over a period of 10 years, from January 2006 to December 2015, were included and analyzed. Classification was based upon Ridley–Jopling classification and as per the criteria laid down under NLEP. All the patients received Multidrug therapy (MDT) as per the WHO recommendations ranging from 6 months to 1 year.
A total of 1396 new cases of leprosy were registered during the study period. Of these, 32 (2.3%) were children in the age group of 0–14 years. Trend of childhood leprosy cases over a 10-year period showed that there was a decline in cases in the year 2009 [Figure 1]. Maximum number of patients were in the year 2013 and 2014. Male patients outnumbered females with an M:F ratio of 2.2:1. The age of the children ranged from 7 to 14 years, and majority of cases belonged to the 10–14-year age group (80%). Most of the children were from a rural background [(23; 71.9%) urban (9; 28.1%)]. Duration of the disease ranged from 15 days to 3 years. Family history of contact was present in 9 (28.1%) patients.
Figure 1.
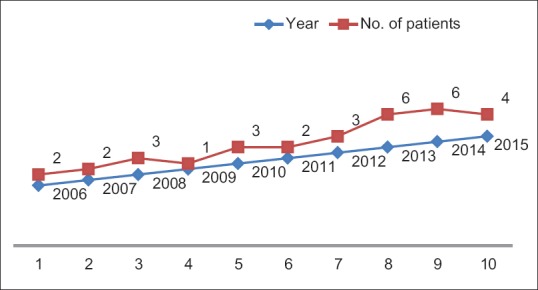
Trend of childhood leprosy
Borderline tuberculoid leprosy was the most common clinical type seen in 15 patients (46.9%) followed by borderline lepromatous (7; 21.9%), lepromatous (6; 18.8%), and pure neural (2; 6.2%) leprosy. One patient each presented with mid-borderline and tuberculoid leprosy. Three patients (9.4%) of MB leprosy (LL) presented with type II lepra reaction. Palpable nerve thickening was seen in 22 (68.7%) children. Multiple nerves were thickened in 18 (56.2%) children and single nerve in 4 (12.5%). Visible deformities (ulnar claw hand) and trophic changes were seen in 4 (12.5%) patients each. Slit skin smear was positive in 11 children.
The scenario of childhood leprosy in India spanning two decades (1990–2009) has been reviewed by Palit et al.[4] The incidence of childhood leprosy recorded in tertiary care hospitals ranged from 5.1% to 11.43%, which is higher than ours. This is probably due to low endemicity of leprosy in Rajasthan in general. The majority of cases in their analysis were paucibacillary (43.28–98%). Borderline tuberculoid was the most common clinical type incidence ranging 35.82–70.8%. Single peripheral nerve trunk was involved in 13.63–40.62% cases, and multiple nerve involvement was recorded in 4.54–59.38% cases. Lepra reactions and deformity was recorded in 0–29.7% and 0–24% cases, respectively. The history of familial contact ranged 0.66–47%. Almost similar observations were made in studies[5,6] conducted at a tertiary care center in north India over a period of 20 years, except for the number of borderline tuberculoid (BT) leprosy patients, which was higher than our study.
Analysis of trends of childhood leprosy offers an insight into the current status of the disease in an area where leprosy has been statistically “eliminated.”[7] The frequency of leprosy in children is an indicator of the level of transmission in a community. According to the NLEP report of March 2015–2016, percentage of new childhood leprosy cases in Rajasthan was 2.35,[2] which is similar to our data. Borderline tuberculoid leprosy was the most common clinical type observed in our study, as reported in other studies as well.[3,5,6]
Early detection of cases due to better awareness about the disease in the community through effective health education campaign, regular and complete treatment with MDT and contact tracing may be important in reducing the burden of leprosy in the community. There is a need to continue leprosy control activities with full force even in areas with low prevalence to sustain the elimination.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.World Health Organization. Global burden of leprosy at the end of 2013. Wkly Epidemiol Rec. 2013;35:365–80. [Google Scholar]
- 2.NLEP-Progress Report for the year 2015-16 ending on 31st March 2016. Central Leprosy Division. New Delhi: Directorate General of Health Services Nirman Bhawan; 2012. Available from: http://www.nlep.nic.in/Revised%20Progress%20report%2031st%20March%202015-16.pdf . [Google Scholar]
- 3.Palit A, Inamadar AC, Desai SS, Sharma P. Childhood leprosy in the post-elimination phase: Data from a tertiary health care Hospital in the Karnataka state of south India. Lepr Rev. 2014;85:85–92. [PubMed] [Google Scholar]
- 4.Palit A, Inamadar AC. Childhood leprosy in India over the past two decades. Lepr Rev. 2014;85:93–9. [PubMed] [Google Scholar]
- 5.Kumar B, Rani R, Kaur I. Childhood leprosy in Chandigarh; clinico-histopathological correlation. Int J Lepr Other Mycobact Dis. 2000;68:330–1. [PubMed] [Google Scholar]
- 6.Dogra S, Narang T, Khullar G, Kumar R, Saikia UN. Childhood leprosy through the post-leprosy-elimination era: A retrospective analysis of epidemiological and clinical characteristics of disease over eleven years from a tertiary care hospital in North India. Lepr Rev. 2014;85:296–310. [PubMed] [Google Scholar]
- 7.Singal A, Sonthalia S, Pandhi D. Childhood leprosy in a tertiary-care hospital in Delhi, India: A reappraisal in the post-elimination era. Lepr Rev. 2011;82:259–69. [PubMed] [Google Scholar]


