Sir,
Granuloma annulare (GA) has been described in several morphologic forms, i.e., annular disseminated, subcutaneous, papular, and perforating. GA is primarily a disease of children and young adults, yet it has been reported in virtually all age groups. Females are affected twice as often as males. Disseminated GA has a possible association with diabetes, a later age of onset, and rare spontaneous resolution. GA localized to only over palms and soles is uncommon and is infrequently reported in the literature. In most cases, it is associated with classical lesions of GA elsewhere, when the diagnosis is relatively easy.[1] In case of isolated lesions, a high degree of clinical suspicion of GA is required and histopathology is of vital importance in making the diagnosis.
A 55-year-old woman presented with a 10 days history of pink-red papules, nodules, and plaques on palms and soles with slight scaling which were painful on pressure [Figure 1]. There were no systemic complaints and no history suggestive of diabetes mellitus or any chronic disease. Examination of the skin revealed erythematous to violaceous papules, nodules, and plaques on palms and soles. There was superficial scaling present over the skin lesions. There was mild itching on few of the lesions. Rest of the mucocutaneous examination revealed no abnormality. Systemic examination was within normal limits. Various clinical possibilities considered were erythema multiforme, erythema elevatum diutinum, drug reactions, vasculitis/urticarial vasculitis, secondary syphilis, etc., Her complete blood count, liver function test, renal function test, and chest X-ray were also normal. Human immunodeficiency virus (HIV) serology and venereal disease research laboratory (VDRL) was nonreactive. A 5-mm punch biopsy from a skin lesion on the right palm showed a sparse superficial and deep perivascular lymphocytic infiltrate with numerous histiocytes in the interstitium of reticular dermis. Between the histiocytes was seen abundant mucin. The histopathology was suggestive of GA of interstitial variety [Figure 2].
Figure 1.

Clinical photograph showing the erythematous papules and plaques with scaling presenton palms
Figure 2.
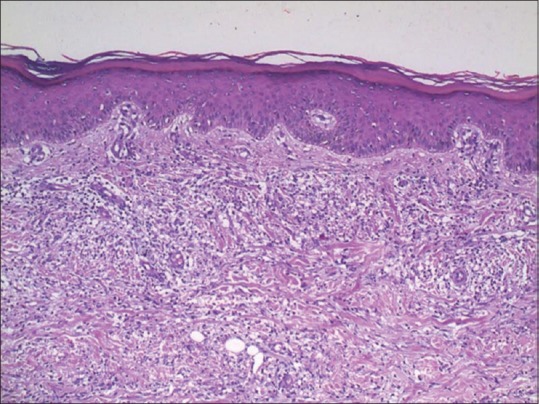
Photomicrograph showing lymphohistiocytic infiltrate extending in between the collagen bundles which appeared to be separated from each other along with mucin deposition (H and E, ×100)
The patient was started on oral prednisone 30 mg/day, topical clobetasol propionate 0.05% twice daily, and oral levocetirizine 5 mg daily. She came for follow-up after 2 weeks and the lesions are improving [Figure 3].
Figure 3.

Clinical photograph showing improvement after 2 weeks of starting treatment
Papular form of GA has been reported to be familial. None of the family members of our patient was similarly affected. Of the cases of GA on the palms that we reviewed, one case involved a woman with dermatomyositis who developed a solitary lesion of GA on the palm.[2] Painful lesions of GA on the palm and soles were also noted in 3 of 13 patients with GA and lymphoma evaluated in a retrospective study by Barksdale et al., leading the authors to conclude that atypical presentations, such as involvement on the palms and soles, may be associated with an underlying hematopoietic malignancy’.[3] Our patient had slightly tender papules and nodules on palms and soles. The localized variety of GA is the most common and presents with skin-colored to violaceous papules in an annular configuration, most commonly over the dorsal side of the feet, ankles, lower limbs, and wrists. In the generalized variety (encountered in only 15% cases), lesions are more widespread, consisting of papules as well as plaques, and involve the trunk, neck, extremities, face, scalp, palms, and soles.[4] Therefore, while palms and soles are frequently involved in the less common generalized variant, they are usually spared in the localized papular variant, which typically affects the dorsa of hands and feet. Although GA is regarded as the prototype of palisading granulomatous dermatoses, the interstitial and mixed patterns predominate.[5] Our patient also had the interstitial pattern of GA. We had ruled out interstitial granulomatous dermatitis with arthritis (IGDA), palisading neutrophilic and granulomatous dermatitis, and interstitial granulomatous drug eruption in the present case. IGDA is an infrequent dermatosis, more common in women with a previous diagnosis of rheumatoid arthritis (RA). Classically, it presents itself as linear subcutaneous cords, known as rope sign. Other clinical forms were reported such as papules, subcutaneous plaques, annular lesions or nodules, predominantly in lateral walls of thorax, abdomen, and medial surface of thighs. Histopathological examination is characterized as dense and diffuse interstitial infiltrate in the reticular dermis, composed of histiocytes in a palisade arrangement, sometimes with necrobiosis of collagen and involved by some neutrophils and eosinophils. Usually there are deposits of mucin and absence of vasculitis. Lesions are usually asymptomatic. Our patient had no systemic complaints. The palisaded neutrophilic granulomatous dermatitis is histopathologically characterized by histiocytes present throughout the dermis, differently from IGDA, which is located in the middle and deep dermis and demonstrates an infiltrate rich in neutrophils, with vascular alterations and leukocytoclasia. Granulomatous drug reactions have been associated with many medications, and presents after few months of onset of drug intake. Our patient was not on any medications. Unique histopathological picture clinched the diagnosis of GA in our patient. GA on palms and soles poses a clinical diagnostic challenge because many other cases share similar clinical features. Localized GA is self-limited and asymptomatic treatment usually is not necessary. Systemic therapy is required for disseminated GA. Many other treatments proposed are topical, intralesional and systemic corticosteroids, chloroquine, hydroxychloroquine sulfate, potassium iodide, niacinamide, chlorpropamide, cyclosporine, chlorambucil, etretinate, etc.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Stewart LR, George S, Hamacher KL, Hsu S. Granuloma annulare on the palms. Dermatol Online J. 2011;17:7. [PubMed] [Google Scholar]
- 2.Imamura S, Ohnishi R, Kawasaki Y, Yoshida MJ. Longstanding solitary granuloma annulare on the palm of a patient with dermatomyositis. J Dermatol. 2008;35:304–5. doi: 10.1111/j.1346-8138.2008.00472.x. [DOI] [PubMed] [Google Scholar]
- 3.Barkesdale SK, Perniciario C, Halling KC, Strickler JG. Granuloma annulare in patient with malignant lymphoma: Cliniclopathological study of thirteen new cases. J Am Acad Dermatol. 1994;31:42–8. doi: 10.1016/s0190-9622(94)70133-4. [DOI] [PubMed] [Google Scholar]
- 4.Julie S. Prendiville: Granuloma Annulare. In: Goldsmith LA, Katz SI, Gilhrest BA, Paller AS, Leffell JD, Wolff K, editors. Fitzpatrick's Dermatology in General Medicine. 8th ed. USA: Mc Graw-Hill; 2012. pp. 467–72. [Google Scholar]
- 5.Chaitra V, Inchara YK, Rajalakshmi T, Antony M. Granuloma annulare-Histology reconsidered. Indian J Dermatol Venereol Leprol. 2010;76:568–9. doi: 10.4103/0378-6323.69050. [DOI] [PubMed] [Google Scholar]


