Abstract
This study examined antibiotic susceptibility, genetic diversity, and characteristics of virulence genes in Campylobacter isolates from poultry. Chicken (n = 152) and duck (n = 154) samples were collected from 18 wet markets in Korea. Campylobacter spp. isolated from the carcasses were identified by PCR. The isolated colonies were analyzed for antibiotic susceptibility to chloramphenicol, amikacin, erythromycin, tetracycline, ciprofloxacin, nalidixic acid, and enrofloxacin. The isolates were also used to analyze genetic diversity using the DiversiLabTM system and were tested for the presence of cytolethal distending toxin (cdt) genes. Campylobacter spp. were isolated from 45 poultry samples out of 306 poultry samples (14.7%) and the average levels of Campylobacter contamination were 22.0 CFU/g and 366.1 CFU/g in chicken and duck samples, respectively. Moreover, more than 90% of the isolates showed resistance to nalidixic acid and ciprofloxacin. Genetic correlation analysis showed greater than 95% similarity between 84.4% of the isolates, and three cdt genes (cdtA, cdtB, and cdtC) were present in 71.1% of Campylobacter isolates. These results indicate that Campylobacter contamination should be decreased to prevent and treat Campylobacter foodborne illness.
Keywords: Campylobacter, poultry, antibiotic susceptibility, Rep-PCR, cdt toxin
1. Introduction
Campylobacter spp. are Gram-negative, microaerophilic bacteria, and the most common cause of bacterial foodborne illness in the world [1,2,3,4]. Among 17 Campylobacter species, Campylobacter jejuni and Campylobacter coli are the major causative agents of foodborne illness in human [5,6,7]. Animal species such as chicken, cattle and wild birds are reservoirs for Campylobacter [8,9]. Campylobacter infection causes watery diarrhea, fever, bloody stools, abdominal pain, and some complications such as Guillain-Barré syndrome (GBS) and Reiter’s syndrome in severe case [10]. Facciolà et al. [10] suggested that it is difficult to find the contamination sources because Campylobacter outbreaks were sporadic and caused by cross-contamination.
Recently, campylobacteriosis have increased dramatically in South Korea. Until 2002, there were no Campylobacter outbreaks, but 831 people were infected by Campylobacter in 2016 [11]. In Switzerland, campylobacteriosis have also been increased, and healthcare cost for the patients was $7.5 million per year, expected to increase steadily [12]. Campylobacter have several virulence factors such as flagellin, capsular polysaccharides, and cytotoxins [13]. Regarding cytotoxin production, Campylobacter can produce cytolethal distending toxin (CDT), which is encoded by cdtA, cdtB, and cdtC genes [14,15,16]. This toxin can induce the host cell distension, then lead to cell death [17]. In severe cases, antibiotic (erythromycin, ciprofloxacin, tetracycline, etc.) treatment is necessary to treat Campylobacter infection, but Campylobacter spp. have recently begun to show resistance to several antibiotics [18,19,20]. In a previous study, 159 Campylobacter isolates from poultry samples in China were examined for antibiotic resistance and 94% (149 isolates) of Campylobacter isolates were resistant to tetracycline, doxycycline, and erythromycin [18]. Thus, Campylobacter isolates need to be investigated for antibiotic susceptibility.
To analyze the genetic correlation among bacterial isolates, restriction-based, amplification-based, and sequencing-based methods have been used [21]. Restriction-based methods include plasmid analysis, restriction fragment length polymorphism (RFLP) analysis, and pulsed-field gel electrophoresis (PFGE). Amplification-based methods are amplified fragment length polymorphisms (AFLP), random amplified polymorphic DNA PCR (RAPD-PCR), and repetitive element PCR (Rep-PCR). Sequencing-based methods include multilocus sequence typing (MLST) and single-nucleotide polymorphism (SNP) analysis. Rep-PCR can assign molecular fingerprints according to the repetitive sequences in bacterial genomes [22,23]. Compared to other PCR typing methods, Rep-PCR has advantages: processing is rapid and it has the ability to analyze small amounts of DNA [21,24]. Abay et al. [25] also suggested that Rep-PCR was more powerful for typeability of Campylobacter than PFGE.
The objective of this study was to investigate the prevalence of Campylobacter in poultry carcasses in wet markets, determine antibiotic susceptibility patterns, the presence of cdt genes, and analyzed the genetic diversity between the Campylobacter isolates.
2. Materials and Methods
2.1. Sample Collection
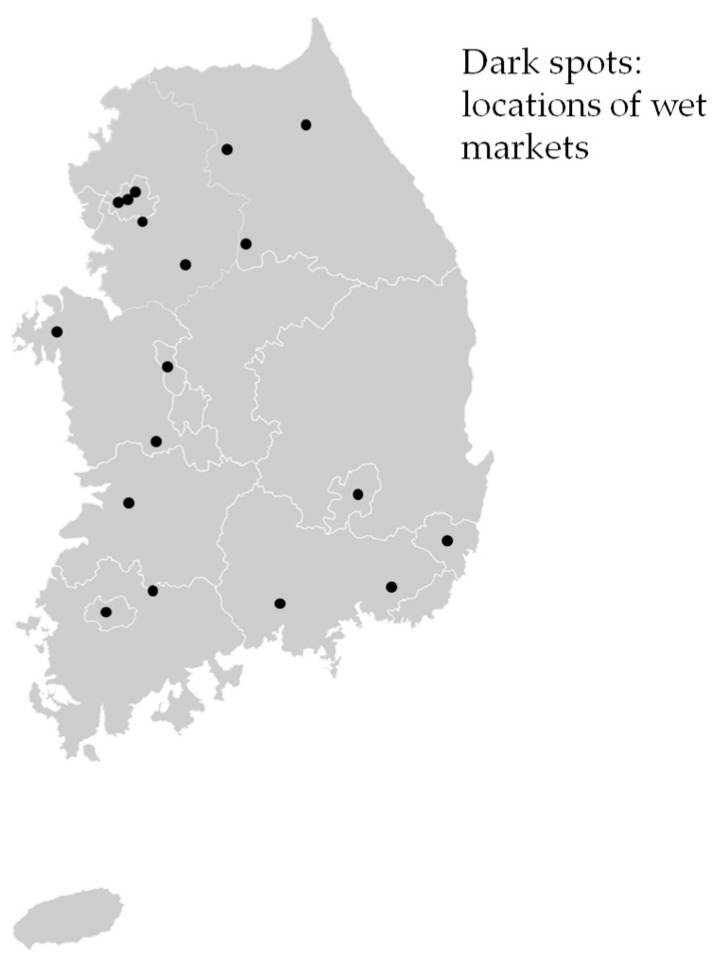
Chicken (n = 152) and duck (n = 154) carcasses were purchased from 18 wet markets throughout Korea during the summer (June–August, in 2014) and winter seasons (December in 2014 to February in 2015) (Figure 1). Three to ten samples for both chicken and duck carcasses were collected per market and per visit, and each market was visited twice for summer and winter. The samples were placed in a cooler on ice and transported to a laboratory. They were analyzed within 24 h.
Figure 1.
The locations of wet markets for poultry samples collected in Korea.
2.2. Campylobacter Isolation, Enumeration, and Identification
Each poultry sample was placed into a sample bag containing 400 mL 0.1% buffered peptone water (BPW, Becton, Dickinson and Company, Sparks, MD, USA) and gently shaken for 60 s. For Campylobacter isolation, the rinsate (27 mL) was mixed with 27 mL 2 × blood-free Bolton broth (Oxoid Ltd., Basingstoke, Hampshire, UK) and the mixture was enriched at 42 °C for 48 h. Loopful portions (10 μL) of the enrichments were streaked on modified charcoal-cefoperazone-deoxycholate agar (mCCDA; Oxoid Ltd., Basingstoke, UK) and incubated at 42 °C for 48 h in a microaerobic environment (5% O2, 10% CO2, and 85% N2) created by CampyGenTM gas packs (Oxoid Ltd., Basingstoke, UK). The two presumptive Campylobacter colonies (gray, mucoid, and flat) on a plate were selected and each colony of them was streaked on two Colombia agar plates (bioMérieux, Marcy-l’Étoile, France) for aerobic and microaerobic conditions at 42 °C for 48 h under both aerobic and microaerobic conditions. The colonies grown under microaerobic conditions were further analyzed to identify Campylobacter by PCR using the primers listed in Table 1. To extract Campylobacter DNA, the presumptive colonies at plate were suspended in 0.2 mL of sterilized distilled water, and heated at 99 °C for 10 min. The suspensions were centrifuged at 14,000 rpm for 3 min, and supernatants were then used for PCR amplification. The program was as follows: pre-denaturation at 95 °C for 15 min, 25 cycles of denaturation at 95 °C for 0.5 min, annealing at 58 °C for 1.5 min, and extension at 72 °C for 1 min. A final extension step at 72 °C for 7 min was performed [26]. The PCR products were visualized by electrophoresis and UV-transillumination. The isolates were used in further experiments for analysis of antibiotic resistance, genetic diversity and cdt genes. To enumerate Campylobacter cells, 1 mL of the rinsate was serially diluted using 0.1% BPW, and 0.1 mL of aliquots were plated on mCCDA (Oxoid Ltd., Basingstoke, UK). The plates were then incubated at 42 °C for 48 h under microaerobic conditions. Five presumptive colonies on each plate were then analyzed by PCR using the conditions described above. The contamination levels of Campylobacter were determined by multiplying the number of positive colonies per five presumptive colonies to the total number of colonies. Additionally, each carcass was weighted to calculate the colony forming units per g (CFU/g).
Table 1.
Primer sequences used to identify the Campylobacter genus and species.
| Species | Target Gene | Primer | Sequence (5’→3’) | Size (bp) | Reference |
|---|---|---|---|---|---|
| Genus Campylobacter | 16S rRNA | C412F | GGATGACACTTTTCGGAGC | 816 | [27] |
| C1228R | CATTGTAGCACGTGTGTC | ||||
| Campylobacter jejuni | cj0414 | C-1 | CAAATAAAGTTAGAGGTAGAATGT | 161 | [28] |
| C-3 | CCATAAGCACTAGCTAGCTGAT | ||||
| Campylobacter coli | ask | CC18F | GGTATGATTTCTACAAAGCGAG | 502 | [27] |
| CC519R | ATAAAAGACTATCGTCGCGTG |
2.3. Antibiotic Susceptibility Testing
The isolated colonies were further analyzed for antibiotic susceptibility to chloramphenicol, amikacin, erythromycin, tetracycline, ciprofloxacin, nalidixic acid, and enrofloxacin (Sigma-Aldrich, St Louis, MO, USA), according to the guidelines of the Clinical & Laboratory Standards Institute [29]. To determine antibiotic resistance, the breakpoints suggested by CLSI [29], CDC [30], Hong et al. [31], and Kang et al. [32] were used as follows: chloramphenicol at 32 μg/mL, amikacin at 64 μg/mL, erythromycin at 32 μg/mL, tetracycline at 16 μg/mL, ciprofloxacin at 4 μg/mL, nalidixic acid at 64 μg/mL, and enrofloxacin at 4 μg/mL. The Campylobacter isolates on Colombia agar (bioMérieux, Marcy-l’Étoile, France) were suspended in Mueller-Hinton broth (MHB; Becton, Dickinson and Company, Sparks, MD, USA) to obtain a McFarland 0.5 standard, and further diluted 10-fold. Using needles, Campylobacter isolates were spotted on Mueller-Hinton agar (MHA; Becton, Dickinson and Company, Sparks, MD, USA) with 5% lysed horse blood plates (Oxoid Ltd., Basingstoke, UK), formulated at 0.5–128 μg/mL with seven antibiotics. The plates were incubated under microaerobic conditions at 37 °C for 48 h. MIC was determined by colony formation on the plates and the reference strain used was Campylobacter jejuni ATCC33560.
2.4. Analysis of Genetic Diversity
To analyze the genetic diversity, 45 Campylobacter isolates from poultry were streaked on Colombia agar (bioMérieux, Marcy-l’Étoile, France), followed by microaerobic incubation at 42 °C for 48 h. DNA was extracted from Campylobacter isolates using a commercial kit (UltraCleanTM Microbial DNA Isolation Kit, MoBio Laboratories, Solana Beach, CA, USA). The extracted DNA was amplified using DiversiLab Campylobacter Kit (bioMérieux, Marcy-l’Étoile, France). The amplified products were separated by electrophoresis on microfluidics chips (Agilent Technologies, Palo Alto, CA, USA) and analyzed with the Agilent 2100 Bioanalyzer (Agilent Technologies, Palo Alto, CA, USA). The peak and band data were analyzed by DiversiLabTM software version 2.1.66 (bioMérieux, Marcy-l’Étoile, France) using Pearson’s correlation coefficient and unweighted pair group method with the arithmetic mean, followed by dendrogram generation. The cutoff value was 95% for determining genetic similarity [33,34].
2.5. Analysis of Cytolethal Distending Toxin Genes
To observe the presence of cdt genes (cdtA, cdtB, and cdtC) from isolates, the extracted DNA was amplified using the primers listed in Table 2 [14]. The PCR products were visualized by gel electrophoresis and UV-transillumination.
Table 2.
PCR primers and amplification conditions used to analysis of cdt genes for Campylobacter isolates.
| Genus | Gene | Sequence (5’→3’) | Amplification (1) Condition | Size (bp) |
|---|---|---|---|---|
| Campylobacter jejuni | cdtA | F: AGGACTTGAACCTACTTTTC | 94 °C, 30 s −55 °C, 30 s −72 °C, 30 s |
631 |
| R: AGGTGGAGTAGTTAAAAACC | ||||
| cdtB | F: ATCTTTTAACCTTGCTTTTGC | 94 °C, 30 s −56 °C, 30 s −72 °C, 30 s |
714 | |
| R: GCAAGCATTAAAATCGCAGC | ||||
| cdtC | F: TTTAGCCTTTGCAACTCCTA | 94 °C, 30 s −55 °C, 30 s −72 °C, 30 s |
524 | |
| R: AAGGGGTAGCAGCTGTTAA | ||||
| Campylobacter coli | cdtA | F: ATTGCCAAGGCTAAAATCTC | 94 °C, 30 s −55 °C, 30 s −72 °C, 30 s |
329 |
| R: GATAAAGTCTCCAAAACTGC | ||||
| cdtB | F: TTTAATGTATTATTTGCCGC | 94 °C, 30 s −56 °C, 30 s −72 °C, 30 s |
413 | |
| R: TCATTGCCTATGCGTATG | ||||
| cdtC | F: TAGGGATATGCACGCAAAAG | 94 °C, 30 s −55 °C, 30 s −72 °C, 30 s |
313 | |
| R: GCTTAATACAGTTACGATAG |
(1) Amplification: denaturation-annealing-extension.
2.6. Statistical Analysis
The data for the prevalence and contamination levels of Campylobacter between chicken and duck were statistically analyzed by SAS version 9.3 (SAS Institute Inc., Cary, NC, USA), and Chi-square test and t-test were used for prevalence and contamination levels, respectively, to determine significance at α = 0.05.
3. Results and Discussion
3.1. Prevalence and Contamination Levels of Campylobacter
Of 306 poultry samples, Campylobacter spp. were identified from 45 samples (14.7%, 15 chicken samples and 30 duck samples) after enrichment (qualitative), but the number of positive samples was higher in quantitative results than in qualitative samples (Table 3). Since other bacteria may also be enriched with Campylobacter, resulting in disturbing the identification, the prevalence rate was lower in qualitative results than in quantitative results. The mean contamination levels of the isolated Campylobacter spp. in chicken and duck samples were 22.0 ± 36.3 CFU/g and 366.1 ± 733.6 CFU/g, respectively (Table 3).
Table 3.
Prevalence and contamination levels of Campylobacter in chicken and duck carcasses at wet markets in Korea during summer and winter.
| Seasons | Sample | Prevalence (No. of Positive Samples/No. of Samples (%)) | Contamination Level | |
|---|---|---|---|---|
| No. of Positive Samples/No. of Samples (%) | Mean ± SD (CFU/g) | |||
| Summer | Chicken | 7/80 (8.8) | 3/80 (3.8) | 32.1 ± 21.0 |
| Duck | 15/80 (18.8) | 7/80 (8.8) | 15.7 ± 14.2 | |
| Subtotal | 22/160 (13.8) | 10/160 (6.3) | 20.6 ± 17.2 | |
| Winter | Chicken | 8/72 (11.1) | 19/72 (26.4) | 20.4 ± 38.8 |
| Duck | 15/74 (20.3) | 38/74 (51.4) | 427.4 ± 780.2 | |
| Subtotal | 23/146 (15.8) | 57/146 (39.0) | 301.1 ± 673.1 | |
| Total | Chicken | 15/152 (9.9) A | 22/152 (14.5) | 22.0 ± 36.6 b |
| Duck | 30/154 (19.5) A | 45/154 (29.2) | 366.1 ± 733.6 a | |
| Total | 45/306 (14.7) | 67/306 (21.9) | 259.8 ± 628.9 | |
Different upper letters (A, a, and b) in the same column indicate a difference (p < 0.05).
These results suggest that a quantitative method may be appropriate to investigate Campylobacter prevalence rather than a qualitative method, and duck samples have a higher contamination frequency and have higher levels of contamination significantly (p = 0.0210) than those in chicken samples in the Korean markets. Campylobacter was isolated regardless of the season; however, the contamination levels of Campylobacter were higher in the winter than in the summer. Of the 45 Campylobacter spp. isolates, 29 isolates were C. jejuni and 16 isolates were C. coli. In France, 372 of 425 chicken samples (87.5%) were Campylobacter positive, and their mean contamination level was 2.4 log CFU/g [35]. Also, Garin et al. [36] showed that Campylobacter spp. were detected from 491 of 750 chicken carcasses (65.5%) in five countries (Senegal, Cameroon, Madagascar, New Caledonia and Vietnam), and the mean value of contamination level was 3.2 log CFU/g. Additionally, Zhu et al. [37] analyzed 1587 chicken carcasses collected from seven provinces in China, and 716 carcasses (45.1%) were contaminated to Campylobacter, and the contamination level was 2.1 log CFU/g (median value). These studies indicate that Campylobacter contamination levels were similar among countries, however, the prevalence of Campylobacter can be considered low in wet markets in Korea. Campylobacter are microaerophilic bacteria. Thus, the bacterial cell counts can be gradually decreased under aerobic condition during distribution. Hence, long exposure time to aerobic condition during distribution to wet markets may induce low prevalence of Campylobacter in poultry in Korea.
3.2. Antimicrobial Resistance Patterns
Because antimicrobial resistance patterns were not different between C. jejuni and C. coli, the data were combined in Table 4. The Campylobacter isolates were resistant to nalidixic acid (93.3%), ciprofloxacin (91.1%), and tetracycline (71.1%) (Table 4). The isolates showed especially strong resistance to antibiotics such as nalidixic acid ciprofloxacin, tetracycline. However, Campylobacter isolates were sensitive to chloramphenicol (others), enrofloxacin (fluoroquinolones), erythromycin (macrolides), and amikacin (aminoglycosides) (Table 4). In Italy, Campylobacter isolates also showed high resistance rates to ciprofloxacin, tetracycline, and nalidixic acid [38]. Similarly, in the USA, the rate of antimicrobial resistance to tetracycline was very high, at 99.1% in Campylobacter isolates from broiler carcasses, followed by resistance to nalidixic acid and ciprofloxacin [39].
Table 4.
Percentage of susceptibility and resistance of seven antibiotics for Campylobacter isolates from poultry.
| Class | Antibiotics | Susceptibility | Resistance | ||
|---|---|---|---|---|---|
| No. of Isolates | Ratio (%) | No. of Isolates | Ratio (%) | ||
| A (1) | Amikacin | 25 | 55.6 | 20 | 44.4 |
| M | Erythromycin | 43 | 95.6 | 2 | 4.4 |
| T | Tetracycline | 13 | 28.9 | 32 | 71.1 |
| F | Ciprofloxacin | 4 | 8.9 | 41 | 91.1 |
| F | Enrofloxacin | 38 | 84.4 | 7 | 15.6 |
| Q | Nalidixic acid | 3 | 6.7 | 42 | 93.3 |
| Others | Chloramphenicol | 45 | 100.0 | 0 | 0.0 |
(1) A: Aminoglycosides, M: Macrolides; T: Tetracyclines; F: Fluoroquinolones; Q: Quinolones.
Raeisi et al. [40] showed that Campylobacter isolates from poultry were resistant to ciprofloxacin, tetracycline and nalidixic acid. Also, 100% of C. jejuni isolates (n = 31) from chicken in China had resistance to ciprofloxacin and nalidixic acid [41]. In Poland, Campylobacter isolates were susceptible to erythromycin and resistant to tetracycline and ciprofloxacin [42]. Taken together, we can conclude that both poultry and human isolates of Campylobacter spp. are generally resistant to quinolone and fluoroquinolone antibiotics, such as nalidixic acid and ciprofloxacin. This may be caused by the use of these antibiotics in veterinary and human medicine. Therefore, this result suggests that antibiotics used for humans should not be used in poultry.
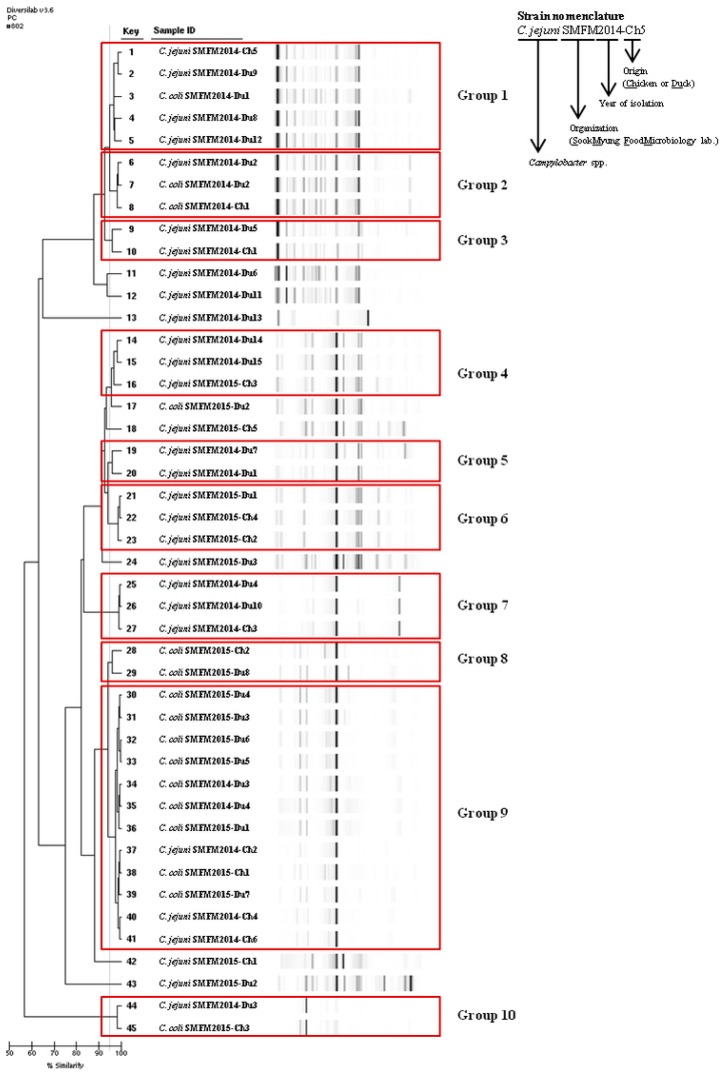
3.3. Genetic Diversity between Isolates
Campylobacter isolates were group according to the Rep-PCR dendrogram patterns (Figure 2). In genetic diversity, more than 95% similarity was shown in 38 isolates (84.4%) and these isolates were grouped into 10 groups (Figure 2). When comparing the 10 groups, obvious geographic correlations were not observed (Figure 2). For instance, key numbers 21–23 in group 6 were isolated from same location (Ulsan). Although 26–27 in group 7, and 39–41 in group 9 were isolated from same location (Cheongju), they were placed in different genetic group. However, Hiett et al. [43] subtyped for 50 Campylobacter isolates, and the most isolates from same location were genetically very similar. Like this result, very close genetic similarity can be expected for the isolates from same locations, but it was not observed in Korea as discussed above. This result indicates that chicken and duck in different wet markets in Korea may be distributed from only few slaughterhouses.
Figure 2.
Dendrogram and gel-like image of the DiversiLab systems for Campylobacter isolates from poultry samples.
3.4. Distribution of cdtA, cdtB, and cdtC
Campylobacter can produce CDT, composed of A, B, and C subunits, which are encoded by cdtA, cdtB, and cdtC genes [44]. The 71.1% of the Campylobacter isolates had these three genes (Table 5). Nine of 15 chicken Campylobacter isolates and 23 of 30 duck Campylobacter isolates had the three cdt genes. Four isolates were found to be without any cdt genes and nine isolates had two cdt genes (cdtA+/cdtB+, cdtA+/cdtC+, or cdtB+/cdtC+). There was no relationship between the distribution of cdt genes and the regions the isolates had been obtained from. Oh et al. [45] showed that 37 C. jejuni isolates out of 38 chicken samples had all cdt genes. Findik et al. [5] found that 75.6% of C. jejuni isolates (127 isolates out of 168) from various sources, including human, poultry, cattle, sheep, and dog, had all cdt genes and five isolates were without cdt genes. In Brazil, all cdt genes were detected in 66.7% of Campylobacter isolates [46]. These results indicate that most Campylobacter isolates from our study have the potential to produce CDT.
Table 5.
Cytolethal Distending Toxin (CDT) gene profiles of Campylobacter isolated from chicken and duck carcasses at wet markets.
| Toxin Profile | Number of Isolates | ||||
|---|---|---|---|---|---|
| Chicken | Duck | Total (%) | |||
| Summer | Winter | Summer | Winter | ||
| Negative | 1 | - | 2 | 1 | 4 (4.3) |
| cdtA+ | - | - | - | - | - |
| cdtB+ | - | - | - | - | - |
| cdtC+ | - | - | - | - | - |
| cdtA+/cdtB+ | - | 1 | - | 1 (2.2) | |
| cdtA+/cdtC+ | - | - | 1 | - | 1 (2.2) |
| cdtB+/cdtC+ | 1 | 4 | 1 | 1 | 7 (15.6) |
| cdtA+/cdtB+/cdtC+ | 5 | 4 | 10 | 13 | 32 (71.1) |
| Total | 7 | 8 | 15 | 15 | 45 (100.0) |
4. Conclusions
In this study, the prevalence of the pathogen, antibiotic resistance, genetic diversity, and the presence of cdt genes in Campylobacter isolates were identified from poultry in Korean wet markets. Although the prevalence of Campylobacter in poultry was relatively low compared to that in other countries, antibiotic resistance patterns of the isolates were similar to those in other countries. In addition, geographic genetic diversity was not observed and a high proportion of cdt genes were present in Campylobacter isolates. Therefore, Campylobacter contamination should be decreased in order to prevent and treat the Campylobacter foodborne illness.
Acknowledgments
This research was supported by a grant (14162MFDS077) from the Ministry of Food and Drug Safety in 2015.
Author Contributions
Jeeyeon Lee participated in the design and coordination of the study, performed the experiments, analyzed the data, and wrote the manuscript. Jiyeon Jeong participated in the design of the study, performed the experiments and analyzed the data. Heeyoung Lee participated in the design of the study and helped draft the manuscript. Jimyeong Ha, Sejeong Kim, Yukyung Choi, and Hyemin Oh performed the experiments and helped the draft the manuscript. Kunho Seo participated in the design and coordination of the study. Yohan Yoon participated in the design of the study, oversaw the data collection in the study and contributed to the manuscript revision process. Soomin Lee also participated in the design of the study and contributed to the manuscript revision process. All authors read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- 1.Han K., Jang S.S., Choo E., Heu S., Ryu S. Prevalence, genetic diversity, and antibiotic resistance patterns of Campylobacter jejuni form retail raw chickens in Korea. Int. J. Food Microbiol. 2007;114:50–59. doi: 10.1016/j.ijfoodmicro.2006.10.042. [DOI] [PubMed] [Google Scholar]
- 2.Miflin J.K., Templeton J.M., Blackall P.J. Antibiotic resistance in Campylobacter jejuni and Campylobacter coli isolated from poultry in the South-East Queensland region. J. Antimicrob. Chemother. 2007;59:775–778. doi: 10.1093/jac/dkm024. [DOI] [PubMed] [Google Scholar]
- 3.Qin S.-S., Wu C.-M., Wang Y., Jeon B., Shen Z.-Q., Wang Y., Zhang Q., Shen J.-Z. Antimicrobial resistance in Campylobacter coli isolated from pigs in two provinces of China. Int. J. Food Microbiol. 2011;146:94–98. doi: 10.1016/j.ijfoodmicro.2011.01.035. [DOI] [PubMed] [Google Scholar]
- 4.Suzuki H., Yamamoto S. Campylobacter contamination in retail poultry meats and by-products in the world: A literature survey. J. Vet. Med. Sci. 2009;71:255–261. doi: 10.1292/jvms.71.255. [DOI] [PubMed] [Google Scholar]
- 5.Findik A., Ica T., Onuk E.E., Percin D., Kevenk T.O., Ciftci A. Molecular typing and cdt genes prevalence of Campylobacter jejuni isolates from various sources. Trop. Anim. Health Prod. 2011;43:711–719. doi: 10.1007/s11250-010-9758-0. [DOI] [PubMed] [Google Scholar]
- 6.Moore J.E., Corcoran D., Dooley J.S.F., Fanning S., Lucey B., Matsuda M., McDowell D.A., Mégraud F., Millar B.C., O’Mahony R., et al. Campylobacter. Vet. Res. 2005;36:351–382. doi: 10.1051/vetres:2005012. [DOI] [PubMed] [Google Scholar]
- 7.On S.L. Taxonomy of Campylobacter, Arcobacter, Helicobacter and related bacteria: Current status, future prospects and immediate concerns. J. Appl. Microbiol. 2001;90:1S–15S. doi: 10.1046/j.1365-2672.2001.01349.x. [DOI] [PubMed] [Google Scholar]
- 8.Refregier-Petton J., Rose N., Denis M., Salvat G. Risk factors for Campylobacter spp. contamination in French broiler-chicken flocks at the end of the rearing period. Prev. Vet. Med. 2001;50:89–100. doi: 10.1016/S0167-5877(01)00220-3. [DOI] [PubMed] [Google Scholar]
- 9.Skarp C.P.A., Hänninen M.L., Rautelin H.I.K. Campylobacteriosis: The role of poultry meat. Clin. Microbiol. Inf. 2016;22:103–109. doi: 10.1016/j.cmi.2015.11.019. [DOI] [PubMed] [Google Scholar]
- 10.Facciolà A., Riso R., Avventuroso E., Visalli G., Delia S.A., Laganà P. Campylobacter: From microbiology to prevention. J. Prev. Med. Hyg. 2017;58:E79–E92. [PMC free article] [PubMed] [Google Scholar]
- 11.Ministry of Food and Drug Safety Statistics of Foodborne Illness. [(accessed on 17 October 2017)]; Available online: http://www.foodsafetykorea.go.kr/portal/healthyfoodlife/foodPoisoningStat.do?menu_no=519&menu_grp=MENU_GRP02.
- 12.Schmutz C., Mäusezahl D., Bless P.J., Hatz C., Schwenkglenks M., Urbinello D. Estimating healthcare costs of acute gastroenteritis and human campylobacteriosis in Switzerland. Epidemiol. Infect. 2017;145:627–641. doi: 10.1017/S0950268816001618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zilbauer M., Dorrell N., Wren B.W., Bajaj-Elliott M. Campylobacter jejuni-mediated disease pathogenesis: An update. Trans. R. Soc. Trop. Med. Hyg. 2008;102:123–129. doi: 10.1016/j.trstmh.2007.09.019. [DOI] [PubMed] [Google Scholar]
- 14.Asakura M., Samosornsuk W., Hinenoya A., Misawa N., Nishimura K., Matsuhisa A., Yamasaki S. Development of a cytolethal distending toxin (cdt) gene-based species-specific multiplex PCR assay for the detection and identification of Campylobacter jejuni, Campylobacter coli and Campylobacter fetus. FEMS Immunol. Med. Microbiol. 2008;52:260–266. doi: 10.1111/j.1574-695X.2007.00369.x. [DOI] [PubMed] [Google Scholar]
- 15.Bolton D.J. Campylobacter virulence and survival factors. Food Microbiol. 2015;48:99–108. doi: 10.1016/j.fm.2014.11.017. [DOI] [PubMed] [Google Scholar]
- 16.Yamasaki S., Asakura M., Tsukamoto T., Faruque S.M., Deb R., Ramamurthy T. Cytolethal distending toxin (CDT): Genetic diversity, structure and role in diarrheal disease. Toxin Rev. 2006;25:61–88. doi: 10.1080/15569540500320938. [DOI] [Google Scholar]
- 17.Weis A.M., Miller W.A., Byrne B.A., Chouicha N., Boyce W.M., Townsend A.K. Prevalence and pathogenic potential of Campylobacter isolates from free-living, human-commensal American crows. Appl. Environ. Microbiol. 2014;80:1639–1644. doi: 10.1128/AEM.03393-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ge B., White D.G., McDermott P.F., Girard W., Zhao S., Hubert S., Meng J. Antimicrobial-resistant Campylobacter species from retail raw meats. Appl. Environ. Microbiol. 2003;69:3005–3007. doi: 10.1128/AEM.69.5.3005-3007.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gibreel A., Tracz D.M., Nonaka L., Ngo T.M., Connell S.R., Taylor D.E. Incidence of antibiotic resistance in Campylobacter jejuni isolated in Alberta, Canada, from 1999 to 2002, with special reference to tet(O)-mediated tetracycline resistance. Antimicrob. Agents Chemother. 2004;48:3442–3450. doi: 10.1128/AAC.48.9.3442-3450.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zhong X., Wu Q., Zhang J., Shen S. Prevalence, genetic diversity and antimicrobial susceptibility of Campylobacter jejuni isolated from retail food in China. Food Control. 2016;62:10–15. doi: 10.1016/j.foodcont.2015.09.032. [DOI] [Google Scholar]
- 21.Foley S.L., Lynne A.M., Nayak R. Molecular typing methodologies for microbial source tracking and epidemiological investigations of Gram-negative bacterial foodborne pathogens. Infect. Genet. Evol. 2009;9:430–440. doi: 10.1016/j.meegid.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Behringer M., Miller W.G., Oyarzabal O.A. Typing of Campylobacter jejuni and Campylobacter coli isolated from live broilers and retail broiler meat by flaA-RFLP, MLST, PFGE and REP-PCR. J. Microbiol. Meth. 2011;84:194–201. doi: 10.1016/j.mimet.2010.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Hulton C.S.J., Higgins C.F., Sharp P.M. ERIC sequences, a novel family of repetitive elements in the genome of Escherichia coli, Salmonella typhimurium and other enterobacterial. Mol. Microbiol. 1991;5:825–834. doi: 10.1111/j.1365-2958.1991.tb00755.x. [DOI] [PubMed] [Google Scholar]
- 24.Appuhamy S., Parton R., Coote J.G., Gibbs H.A. Genomic fingerprinting of Haemophilus somnus by a combination of PCR methods. J. Clin. Microbiol. 1997;35:288–291. doi: 10.1128/jcm.35.1.288-291.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Abay S., Kayman T., Otlu B., Hizlisoy H., Aydin F., Ertas N. Genetic diversity and antibiotic resistance profiles of Campylobacter jejuni isolates from poultry and humans in Turkey. Int. J. Food Microbiol. 2014;178:29–38. doi: 10.1016/j.ijfoodmicro.2014.03.003. [DOI] [PubMed] [Google Scholar]
- 26.Yamazaki-Matsune W., Taguchi M., Seto K., Kawahara R., Kawatsu K., Kumeda Y., Kitazato M., Nukina M., Misawa N., Tsukamoto T. Development of a multiplex PCR assay for identification of Campylobacter coli, Campylobacter fetus, Campylobacter hyointestinalis subsp. hyointestinalis, Campylobacter jejuni, Campylobacter lari and Campylobacter upsaliensis. J. Med. Microbiol. 2007;56:1467–1473. doi: 10.1099/jmm.0.47363-0. [DOI] [PubMed] [Google Scholar]
- 27.Linton D., Owen R.J., Stanley J. Rapid identification by PCR of the genus Campylobacter and five Campylobacter species enteropathogenic for man and animals. Res. Microbiol. 1996;147:707–718. doi: 10.1016/S0923-2508(97)85118-2. [DOI] [PubMed] [Google Scholar]
- 28.Wang R.F., Salvic M.F., Cao W.W. A rapid PCR method for direct detection of low numbers of Campylobacter jejuni. J. Rapid Methods Autom. Microbiol. 1992;1:101–108. doi: 10.1111/j.1745-4581.1992.tb00074.x. [DOI] [Google Scholar]
- 29.Clinical and Laboratory Standards Institute . Performance Standards for Antimicrobial Susceptibility Testing; 20th Informational Supplement. CLSI; Pennsylvania, PA, USA: 2010. M100-S20. [Google Scholar]
- 30.Centers for Disease Control and Prevention . National Antimicrobial Resistance Monitoring System for Enteric Bacteria (NARMS): 2005 Human Isolates Final Report. Department of Health and Human Services, CDC; Atlanta, GA, USA: 2008. [Google Scholar]
- 31.Hong J., Kim J.M., Jung W.K., Kim S.H., Bae W., Koo H.C., Gil J., Kim M., Ser J., Park Y.H. Prevalence and antibiotic resistance of Campylobacter spp. isolated from chicken meat, pork, and beef in Korea, from 2001 to 2006. J. Food Prot. 2007;70:860–866. doi: 10.4315/0362-028X-70.4.860. [DOI] [PubMed] [Google Scholar]
- 32.Kang Y.S., Cho Y.S., Yoon S.K., Yu M.A., Kim C.M., Lee J.O., Pyun Y.R. Prevalence and antimicrobial resistance of Campylobacter jejuni and Campylobacter coli isolated from raw chicken meat and human stools in Korea. J. Food Prot. 2006;69:2915–2923. doi: 10.4315/0362-028X-69.12.2915. [DOI] [PubMed] [Google Scholar]
- 33.Herbold N.M., Clotilde L.M., Anderson K.M., Kase J., Hartman G.L., Himathongkham S., Lin A., Lauzon C.R. Clustering of clinical and environmental Escherichia coli O104 isolates using the DiversiLab™ repetitive sequence-based PCR system. Curr. Microbiol. 2015;70:436–440. doi: 10.1007/s00284-014-0728-z. [DOI] [PubMed] [Google Scholar]
- 34.Ross T.L., Merz W.G., Farkosh M., Carroll K.C. Comparison of an automated repetitive sequence-based PCR microbial typing system to pulsed-field gel electrophoresis for analysis of outbreaks of Methicillin-resistant Staphylococcus aureus. J. Clin. Microbiol. 2005;43:5642–5647. doi: 10.1128/JCM.43.11.5642-5647.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hue O., Le Bouquin S., Laisney M.J., Allain V., Lalande F., Petetin I., Rouxel S., Quesne S., Gloaguen P.Y., Picherot M., et al. Prevalence of and risk factors for Campylobacter spp. contamination of broiler chicken carcasses at the slaughterhouse. Food Microbiol. 2010;27:992–999. doi: 10.1016/j.fm.2010.06.004. [DOI] [PubMed] [Google Scholar]
- 36.Garin B., Gouali M., Wouafo M., Perchec A.M., Thu P.M., Ravaonindrina N., Urbès F., Gay M., Diawara A., Leclercp A., et al. Prevalence, quantification and antimicrobial resistance of Campylobacter spp. on chicken neck-skins at points of slaughter in 5 major cities located on 4 continents. Int. J. Food Microbiol. 2012;157:102–107. doi: 10.1016/j.ijfoodmicro.2012.04.020. [DOI] [PubMed] [Google Scholar]
- 37.Zhu J., Yao B., Song X., Wang Y., Cui S., Xu H., Yang B., Huang J., Liu G., Yang X., et al. Prevalence and quantification of Campylobacter contamination on raw chicken carcasses for retail sale in China. Food Control. 2017;75:196–202. doi: 10.1016/j.foodcont.2016.12.007. [DOI] [Google Scholar]
- 38.Di Giannatale E., Di Serafino G., Zilli K., Alessiani A., Sacchini L., Garofolo G., Aprea G., Marotta F. Characterization of antimicrobial resistance patterns and detection of virulence genes in Campylobacter isolates in Italy. Sensors. 2014;14:3308–3322. doi: 10.3390/s140203308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Son I., Englen M.D., Berrang M.E., Fedorka-Cray P.J., Harrison M.A. Antimicrobial resistance of Arcobacter and Campylobacter from broiler carcasses. Int. J. Antimicrob. Agents. 2007;29:451–455. doi: 10.1016/j.ijantimicag.2006.10.016. [DOI] [PubMed] [Google Scholar]
- 40.Raeisi M., Khoshbakht R., Ghaemi E.A., Bayani M., Hashemi M., Seyedghasemi N.S., Shirzad-Aski H. Antimicrobial resistance and virulence-associated genes of Campylobacter spp. isolated from raw milk, fish, poultry, and red meat. Microb. Drug Resist. 2017;23:925–933. doi: 10.1089/mdr.2016.0183. [DOI] [PubMed] [Google Scholar]
- 41.Ma H., Su Y., Ma L., Ma L., Li P., Du X., Gölz G., Wang S., Lu X. Prevalence and characterization of Campylobacter jejuni isolated from retail chicken in Tianjin, China. J. Food Prot. 2017;80:1032–1040. doi: 10.4315/0362-028X.JFP-16-561. [DOI] [PubMed] [Google Scholar]
- 42.Szczepanska B., Andrzejewska M., Spica D., Klawe J.J. Prevalence and antimicrobial resistance of Campylobacter jejuni and Campylobacter coli isolated from children and environmental sources in urban and suburban areas. BMC Microbiol. 2017;17:80. doi: 10.1186/s12866-017-0991-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hiett K.L., Seal B.S., Siragusa G.R. Campylobacter spp. subtype analysis using gel-based repetitive extragenic palindromic-PCR discriminates in parallel fashion to fla A short variable region DNA sequence analysis. J. Appl. Microbiol. 2006;101:1249–1258. doi: 10.1111/j.1365-2672.2006.03026.x. [DOI] [PubMed] [Google Scholar]
- 44.Mortensen N.P., Schiellerup P., Boisen N., Klein B.M., Locht H., Abuoun M., Newell D., Krogfelt K.A. The role of Campylobacter jejuni cytolethal distending toxin in gastroenteritis: Toxin detection, antibody production, and clinical outcome. APMIS. 2011;119:626–634. doi: 10.1111/j.1600-0463.2011.02781.x. [DOI] [PubMed] [Google Scholar]
- 45.Oh J.Y., Kwon Y.K., Wei B., Jang H.K., Lim S.K., Kim C.H., Jung S.C., Kang M.S. Epidemiological relationships of Campylobacter jejuni strains isolated from humans and chickens in South Korea. J. Microbiol. 2017;55:13–20. doi: 10.1007/s12275-017-6308-8. [DOI] [PubMed] [Google Scholar]
- 46.Carvalho A.F.D., Silva D.M.D., Azevedo S.S., Piatti R.M., Genovez M.E., Scarcelli E. Detection of CDT toxin genes in Campylobacter spp. strains isolated from broiler carcasses and vegetables in São Paulo, Brazil. Braz. J. Microbiol. 2013;44:693–699. doi: 10.1590/S1517-83822013000300005. [DOI] [PMC free article] [PubMed] [Google Scholar]