Abstract
Background
Studies have shown that poor shelter or dwelling conditions may lead to deteriorations in health. Those with asthma may be more susceptible to compromised living conditions and stress leading to a higher risk of asthma exacerbations. To describe the asthma control and quality of life of individuals with diagnosed asthma living in a shelter in Damascus, Syria and estimate the prevalence of respiratory symptoms in shelter dwellers without diagnosed asthma.
Methods
In this cross-sectional study, all individuals 5 years and older living in Al-Herjalleh shelter with diagnosed asthma were recruited to complete a questionnaire, which included items related to their respiratory symptoms, asthma exacerbations, exposure to asthma triggers, medication use, and health-related quality of life before and since entering the shelter. A representative sample of shelter dwellers without diagnosed asthma also completed a questionnaire to establish their demographics, respiratory symptoms, environment and chronic disease co-morbidities, in order to identify factors associated with under-diagnosed asthma. All participants underwent spirometry to measure their lung function. Descriptive statistics were calculated, and chi-square tests and Student’s t-tests were used to compare individuals with asthma before and since entering the shelter, as well as to compare those with under-diagnosed asthma and individuals without asthma.
Results
The prevalence of asthma at the Al-Herjalleh shelter in those aged 5 years and older was approximately 8.5%. Nearly 70% of the asthma group felt their asthma had worsened since entering the shelter, and there was a significant drop in the proportion of individuals using inhaled corticosteroids (ICS), with only 4.3% using daily ICS in the shelter (P<0.0001). The proportion of individuals experiencing a severe asthma attack did not change after entering the shelter (P=0.97), but almost all individuals with asthma (94.4%) reported worsening in their health-related quality of life. In the non-asthma group, 44.2% of participants reported episodes of wheezing, coughing and breathlessness at night, consistent with under-diagnosed asthma. A higher proportion of those with under-diagnosed asthma had allergic rhinitis (57.1%), symptoms of post-traumatic stress disorder (PTSD) (35.1%), and abnormal spirometry (60.0%), compared to those without asthma.
Conclusions
The findings of our study highlight the need for asthma programs in Syrian shelters as significant gaps exist in both the screening and management of chronic respiratory diseases to minimize asthma deterioration in Syrian shelter dwellers.
Keywords: Underdiagnosed asthma, asthma in shelters, PTSD in asthma, war-time asthma
Introduction
According to the United Nations (UN), 6.5 million people have been internally displaced within Syria since the start of the civil war (1). As of 2016, 1.7 million internally displaced persons were living in camps and collective centres, including shelters (2). Studies have shown that poor shelter or dwelling conditions (such as overcrowding, lack of basic resources, and poor sanitation) may lead to deteriorations in health (3-6). For example, in the aftermath of the Great East Japan Earthquake and tsunami in 2011, the prevalence of asthma, exacerbations of chronic obstructive pulmonary disease (COPD), and community-acquired pneumonia were two to three times greater compared to the previous year, with half of the community-acquired pneumonia cases originating in evacuation shelters (6). Individuals with asthma may be more susceptible to compromised living conditions and stress leading to a higher risk of asthma exacerbations and other complications (3-6). It is important to identify uncontrolled asthmatics and those who are underdiagnosed or at-risk of developing asthma in order to target preventive strategies and asthma management to minimize the deterioration of asthma control.
The primary study objective was to describe the asthma control and quality of life of individuals with diagnosed asthma (7,8) living in a shelter in Damascus, Syria. We described the living conditions in shelters and asthma-related health outcomes. Specifically, we investigated frequency of respiratory symptoms, asthma exacerbations, exposure to new triggers associated with the ongoing war, exposure to second-hand smoke (SHS), crowding, access to medication and access to specialty care for those with severe asthma.
In addition, we had three secondary objectives: (I) to measure asthma-related symptoms among shelter dwellers who have not previously been diagnosed with asthma; (II) to estimate the prevalence of symptoms of post-traumatic stress disorder (PTSD) in the shelter dwellers; and (III) to screen for other chronic disease co-morbidities, including allergic rhinitis, hypertension, and diabetes.
Methods
Study populations
A total of 850 internally displaced persons settled in the Al-Herjalleh shelter in Damascus, Syria. Two distinct groups were recruited to participate in this cross-sectional study: (I) prevalent and incident asthma group (those with existing asthma, and those newly diagnosed after coming to the shelter, respectively); and (II) non-asthma group (those without diagnosed asthma).
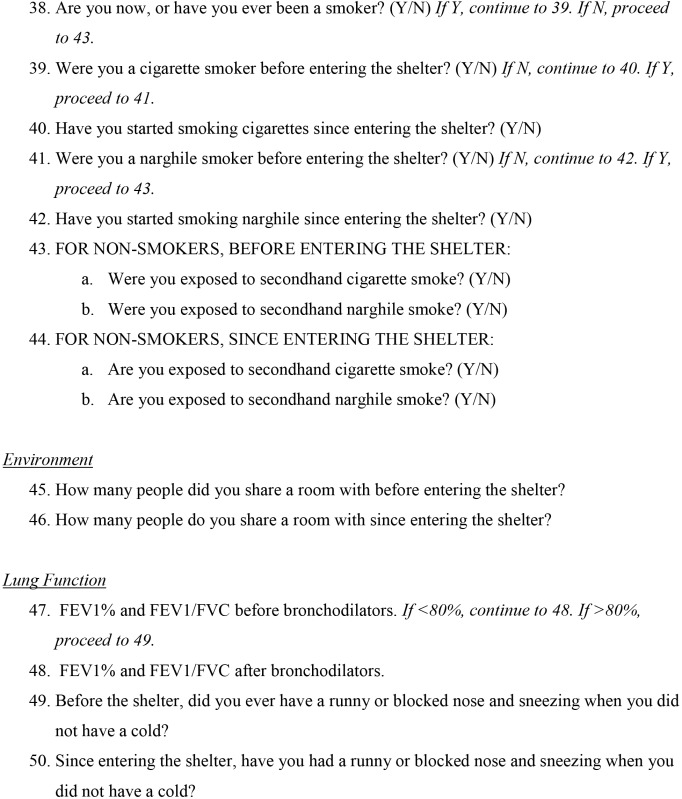
For the prevalent and incident asthma group, all individuals aged 5 years and older with self-reported diagnosed asthma were recruited to participate. The primary outcomes were asthma control and quality of life. Both outcomes were assessed by administering a questionnaire, which included asthma indicators that were recommended by the Canadian Primary Care guidelines (7,8). Participants were asked to recall their symptoms and quality of life prior to entering the shelter, and report their current status as shelter dwellers. Additionally, data on asthma medication use and exposure to new asthma triggers were collected. With respect to environmental factors associated with respiratory health, information was collected on exposure to indoor air pollutants and crowding in the Al-Herjalleh shelter. Participants’ lung function was measured by a trained researcher using a Spirobank portable spirometer, using American Thoracic Society (ATS)/European Respiratory Society (ERS) guidelines. To address our secondary objectives, participants were screened for symptoms of PTSD (including physical symptoms, traumatic flashbacks, and cognitive symptoms) as well as chronic disease co-morbidities (hypertension, allergic rhinitis, and diabetes).
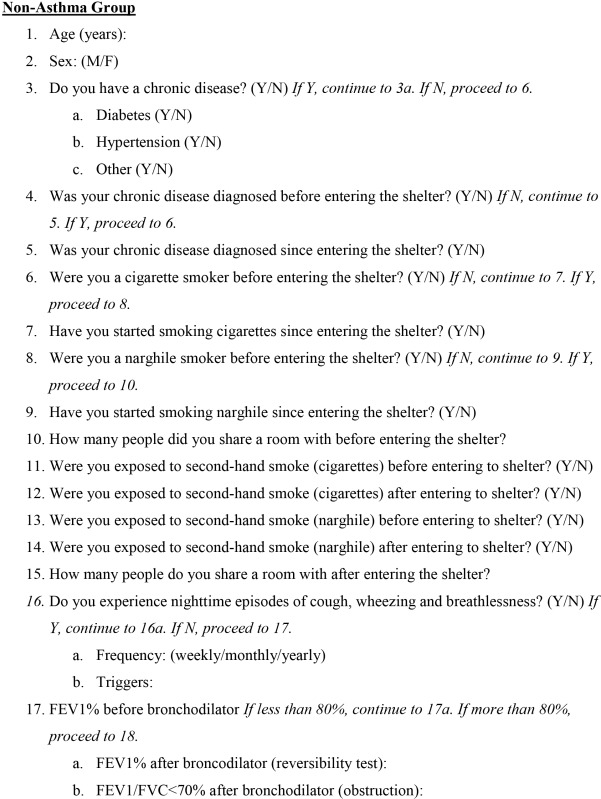
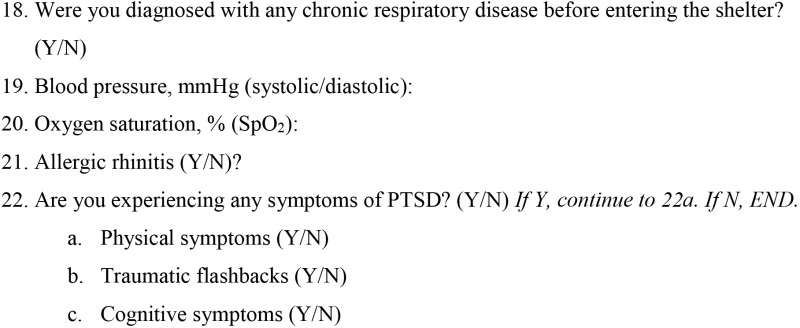
For the non-asthma group, a representative sample of shelter dwellers aged 5 years and older were recruited to participate. A questionnaire was administered to all participants, which included items related to respiratory symptoms, smoking status, chronic disease co-morbidities, crowding, exposure to triggers of respiratory exacerbations, and symptoms of PTSD. A trained researcher measured the participants’ lung function using a Spirobank spirometer. Individuals in the non-asthma group were further subdivided into those with under-diagnosed asthma and those who did not have asthma, based on whether they reported episodes of coughing, wheezing and breathlessness at night. Questionnaires used in this study can be found on the online supplement (Supplement I).
Statistical analysis
Descriptive statistics were calculated for both the prevalent and incident asthma group and non-asthma group. Continuous variables were described using medians, means and standard deviations. Categorical variables were described using frequency distributions and percentages. Student’s t-tests and chi-square tests were used to assess the statistical significance of differences between those with under-diagnosed asthma and those who did not have asthma and to identify factors associated with under-diagnosed asthma. All analyses were completed using the Statistical Package for the Social Sciences (SPSS) version 18 (IBM Corporation, Armonk, NY, USA).
Results
Prevalent and incident asthma group
Among the 850 individuals living in the Al-Herjalleh shelter, 72 were previously diagnosed with asthma, either before or since entering the shelter. The prevalence of asthma at the Al-Herjalleh shelter in those aged 5 years and older was approximately 8.5%. Descriptive statistics for the prevalent and incident asthma group are presented in Table 1. The age of participants ranged from 5 to 76 years, with a mean of 26.1 years (SD: 18.8). There was a slightly higher proportion of males (52.8%) and the majority of adults with asthma (91.7%) were married and living with their family. Only one third (34.7%) of those with asthma were employed. The average monthly income in the prevalent and incident asthma group was $16.63 (SD: 10.5), with 91.7% of the group earning less than $2 per day.
Table 1. Descriptive characteristics of participants with diagnosed asthma (n=72).
| Characteristics | Number | % |
|---|---|---|
| Age in years | ||
| 5–12 | 27 | 37.50 |
| 13–18 | 9 | 12.50 |
| 19–45 | 23 | 31.94 |
| >45 | 13 | 18.06 |
| Mean ± SD | 26.1±18.8 | – |
| Gender | ||
| Female | 34 | 47.22 |
| Male | 38 | 52.78 |
| Employment | ||
| Employed | 25 | 34.72 |
| Unemployed | 23 | 31.94 |
| Student | 24 | 33.33 |
| Marital status (>18 years old) | ||
| Married, living with family | 33 | 91.67 |
| Other | 3 | 8.33 |
| Family size | ||
| ≤6 | 19 | 55.88 |
| >6 | 15 | 44.12 |
| Missing | 2 | – |
| Monthly income ($), mean ± SD | 16.63±10.45 | – |
| Daily income ($) | ||
| <2 | 66 | 91.67 |
| ≥2 | 6 | 8.33 |
| Rurality | ||
| Yes | 49 | 73.13 |
| No | 18 | 26.87 |
| Missing | 5 | – |
| Asthma diagnosis | ||
| By pulmonary specialist, private | 37 | 52.86 |
| By general physician | 24 | 34.29 |
| By primary care health center | 9 | 12.86 |
| Missing | 2 | – |
| Self-reported asthma worsening | ||
| Yes | 48 | 68.57 |
| No | 22 | 31.43 |
| Missing | 2 | – |
| SABA inhaler use | ||
| Yes | 40 | 57.14 |
| No | 30 | 42.86 |
| Missing | 2 | – |
| Self-reported increase in SABA inhaler use (in users) | ||
| Yes | 33 | 82.50 |
| No | 7 | 17.50 |
| Uses SABA inhaler correctly (in users) | ||
| Yes | 20 | 50.00 |
| No | 20 | 50.00 |
| Frequency of waking up at night due to asthma at shelter | ||
| 0 (no more) | 3 | 4.23 |
| 1 | 7 | 9.86 |
| 2 | 19 | 26.76 |
| 3 (some more) | 18 | 25.35 |
| 4 | 16 | 22.54 |
| 5 (a lot more) | 8 | 11.27 |
| Missing | 1 | – |
| Exposed to new asthma triggers in shelter | ||
| Stress and psychiatric triggers | 10 | 13.89 |
| Odors (cooking, heating, perfume) | 26 | 36.11 |
| Second-hand smoke | 11 | 15.28 |
| Vapors | 4 | 5.56 |
| Cold and dampness | 9 | 12.50 |
| Dust | 17 | 23.61 |
| Detergents | 10 | 14 |
| Self-reported worsening of quality of life | ||
| 0 | 4 | 5.63 |
| 1 | 5 | 7.04 |
| 2 | 25 | 35.21 |
| 3 | 17 | 23.94 |
| 4 | 16 | 22.54 |
| 5 | 4 | 5.63 |
| Missing | 1 | – |
| Medical emergency point accessible 24 h prior to shelter | ||
| Yes | 42 | 59.15 |
| No | 29 | 40.85 |
| Missing | 1 | – |
| Know someone who died from asthma attack at shelter | ||
| Yes | 6 | 9.38 |
| No | 58 | 90.63 |
| Missing | 8 | – |
| Exposed to cigarette smoke in the shelter, non-smokers | ||
| Yes | 18 | 51.43 |
| No | 17 | 48.57 |
| Asthma triggered by cigarette smoke, non-smokers | ||
| Yes | 15 | 83.33 |
| No | 3 | 16.67 |
| FEV1 (%) before bronchodilators (n=70), mean ± SD | 87±19 | – |
| FEV1 (%) before bronchodilators (n=70) | ||
| <80 | 21 | 30.00 |
| ≥80 | 49 | 70.00 |
| FEV1 (%) after bronchodilators (n=21), mean ± SD | 87±19 | – |
| FEV1 (%) after bronchodilators (n=21) | ||
| <80 | 7 | 33.33 |
| ≥80 | 14 | 66.67 |
| FEV1/FVC (%) after bronchodilators (n=21) | ||
| <70 | 7 | 33.33 |
| ≥70 | 14 | 66.67 |
| Oxygen saturation (SpO2) (%) | ||
| <92 | 5 | 7.14 |
| ≥92 | 65 | 92.86 |
| Missing | 2 | – |
| Systolic blood pressure (mmHg) (n=29), mean ± SD | 131±20 | – |
| Diastolic blood pressure (mmHg) (n=29), mean ± SD | 83±14 | – |
| Hypertension (>30 years old) | ||
| Yes | 8 | 26.67 |
| No | 22 | 73.33 |
| Any symptom of PTSD | ||
| Yes | 12 | 16.67 |
| No | 60 | 83.33 |
| PTSD symptoms (n=12) | ||
| Physical symptoms | 8 | 66.67 |
| Flashbacks | 6 | 50.00 |
| Cognitive symptoms | 5 | 41.67 |
SABA, short-acting beta2-agonist; PTSD, post-traumatic stress disorder.
More than half (52.9%) of the individuals with asthma were diagnosed by a private pulmonologist, one third (34.3%) by a general doctor, and 12.9% were diagnosed in a primary care centre. Nearly 70% of the asthma group felt their asthma had worsened since entering the shelter, with 57.1% of those on a short-acting beta2-agonist (SABA) inhaler reporting increased use. There was a significant drop in the proportion of individuals using inhaled corticosteroids (ICS) since entering the shelter, with only 4.3% using daily ICS in the shelter (P<0.0001). When asked how frequently they were awoken by their asthma, 59.2% said they woke up more since coming to the shelter. Even though the shelter dwellers had uncontrolled asthma, the proportion of individuals experiencing a severe asthma attack did not change after entering the shelter (P=0.97). Almost all individuals with asthma (94.4%) reported worsening in their health-related quality of life since coming to the shelter. The mean percent predicted FEV1 (FEV1%) before bronchodilators for the asthma group was 87% (SD: 19%), and the FEV1% for 30.0% of participants indicated an obstructive defect (<80%). After administering a bronchodilator, 66.7% of those with an obstructive defect demonstrated total reversibility, while the spirometry of 33.3% was indicative of a fixed airway disease, with an abnormal FEV1% and an abnormal FEV1/FVC ratio (<70%) after bronchodilators.
Table 2 shows changes in conditions before and after coming to the shelters. In terms of crowding, the number of persons living in the same room at the shelter was not significantly different from before entering the shelter (P=0.83). The most common new asthma trigger was odor from other shelter dwellers (36.1%), including smells associated with cooking and/or heating. Other common asthma triggers were dust, SHS, detergents, and stress. A significantly higher proportion of individuals in the asthma group reported smoking cigarettes since entering the shelter (51.4%, P<0.05).
Table 2. Changes in asthma control before and after coming to the shelter in participants with diagnosed asthma (n=72).
| Factors | Before shelter | In shelter | P value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Daily ICS use | |||||||
| Yes | 22 | 30.56 | 3 | 4.29 | <0.0001 | ||
| No | 50 | 69.44 | 67 | 95.71 | |||
| Missing | 0 | – | 2 | – | |||
| Exposed to triggers | |||||||
| Stress and psychiatric triggers | 41 | 56.94 | 40 | 55.56 | 0.867 | ||
| Vapors | 44 | 61.11 | 36 | 50.00 | 0.180 | ||
| Odors (cooking, heating)* | 19 | 26.39 | 12 | 16.67 | 0.156 | ||
| Chemicals, from weapons | 16 | 22.22 | 6 | 8.33 | <0.05 | ||
| Others** | 9 | 12.50 | 36 | 50.00 | <0.0001 | ||
| Severe asthma attack at home, without access to hospital | |||||||
| Yes | 25 | 35.21 | 23 | 34.85 | 0.965 | ||
| No | 46 | 64.79 | 43 | 65.15 | |||
| Missing | 1 | – | 6 | – | |||
| Oral or injection corticosteroids available for severe asthma attack at home | |||||||
| Yes | 18 | 26.09 | 14 | 22.22 | 0.605 | ||
| No | 51 | 73.91 | 49 | 77.78 | |||
| Missing | 3 | – | 9 | – | |||
| Used oral or injection corticosteroids for severe asthma attack at home | |||||||
| Yes | 13 | 52.00 | 13 | 56.52 | 0.753 | ||
| No | 12 | 48.00 | 10 | 2.46 | |||
| Cigarette smoking | |||||||
| Yes | 25 | 34.72 | 37 | 51.39 | <0.05 | ||
| No | 47 | 65.28 | 35 | 48.61 | |||
| Narghile smoking | |||||||
| Yes | 11 | 15.28 | 13 | 18.06 | 0.655 | ||
| No | 61 | 84.72 | 59 | 81.94 | |||
| Exposed to narghile smoke, in non-smokers of narghile | |||||||
| Yes | 29 | 47.54 | 20 | 33.90 | 0.129 | ||
| No | 32 | 52.46 | 39 | 66.10 | |||
| Asthma triggered by narghile smoke | |||||||
| Yes | 24 | 82.76 | 9 | 45.00 | |||
| No | 5 | 17.24 | 11 | 55.00 | |||
| Number of persons living in the same room | |||||||
| 1–3 | 10 | 13.89 | 9 | 12.50 | 0.828 | ||
| 4–6 | 42 | 58.33 | 39 | 54.17 | |||
| 7–9 | 15 | 20.83 | 16 | 22.22 | |||
| >9 | 5 | 6.94 | 8 | 11.11 | |||
*, heating or cooking using fuels such as plastic, trashes, cartoon, and wheels; **, odors of unburied victims in conflict zones before coming to shelter; P values in italic form indicate statistical significance if <0.05. ICS, inhaled corticosteroids.
With regard to our secondary objectives, 26.7% of participants aged 30 years and older had hypertension. Of all those in the asthma group, 16.7% reported symptoms of PTSD. Two-thirds of the individuals with symptoms of PTSD had physical manifestations, half had traumatic flashbacks, and 41.7% had cognitive symptoms.
Non-asthma group
Table 3 shows the characteristics of 204 participants with either under-diagnosed asthma or without asthma. Of these shelter dwellers, 113 did not have asthma symptoms and 91 were not previously diagnosed with asthma, but reported episodes of wheezing, coughing and breathlessness at night, which indicate under-diagnosed asthma. Those with under-diagnosed asthma did not differ significantly from those with no asthma in terms of age, gender, diabetes, hypertension, smoking status or exposure to SHS. A significantly higher proportion of those with under-diagnosed asthma had allergic rhinitis compared to those with no asthma (57.1% vs. 25.7%, P<0.0001). Similarly, a higher proportion of those with under-diagnosed asthma reported symptoms of PTSD (35.1% vs. 15.7%, P<0.05), though their PTSD symptom profile was not significantly different from those with no asthma (P=0.70).
Table 3. Characteristics of participants with under-diagnosed asthma (n=91) and those without asthma (n=113).
| Characteristics | Under-diagnosed asthma (n=91) | No asthma (n=113) | P value | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | ||||
| Age in years | |||||||
| 5-12 | 15 | 16.48 | 16 | 14.29 | 0.094 | ||
| 13-18 | 12 | 13.19 | 12 | 10.71 | |||
| 19-45 | 33 | 36.26 | 43 | 38.39 | |||
| 45-65 | 21 | 23.08 | 38 | 33.93 | |||
| >65 | 10 | 10.99 | 3 | 2.68 | |||
| Missing | 0 | – | 1 | – | |||
| Gender | |||||||
| Female | 55 | 60.44 | 73 | 64.60 | 0.541 | ||
| Male | 36 | 39.56 | 40 | 35.40 | |||
| Any chronic disease | |||||||
| Yes | 40 | 43.96 | 52 | 46.02 | 0.769 | ||
| No | 51 | 56.04 | 61 | 53.98 | |||
| Diabetes | |||||||
| Yes | 6 | 6.59 | 14 | 12.39 | 0.166 | ||
| No | 85 | 93.41 | 99 | 87.61 | |||
| Hypertension | |||||||
| Yes | 14 | 15.38 | 17 | 15.04 | 0.946 | ||
| No | 77 | 84.62 | 96 | 84.96 | |||
| Chronic disease since entering shelter | |||||||
| Yes | 16 | 42.11 | 17 | 37.78 | 0.688 | ||
| No | 22 | 57.89 | 28 | 62.22 | |||
| Missing | 2 | – | 7 | – | |||
| Cigarette smoker, before entering shelter | |||||||
| Yes | 19 | 20.88 | 34 | 30.09 | 0.136 | ||
| No | 72 | 79.12 | 79 | 69.91 | |||
| Cigarette smoker, since entering shelter | |||||||
| Yes | 4 | 5.56 | 5 | 4.42 | 0.841 | ||
| No | 68 | 94.44 | 74 | 93.67 | |||
| Non-smokers exposed to second-hand cigarette smoke, before entering shelter | |||||||
| Yes | 43 | 59.72 | 57 | 72.15 | 0.107 | ||
| No | 29 | 40.28 | 22 | 27.85 | |||
| Non-smokers exposed to second-hand cigarette smoke, since entering shelter | |||||||
| No | 23 | 33.82 | 19 | 25.68 | 0.288 | ||
| Yes | 45 | 66.18 | 55 | 74.32 | |||
| Narghile smoker, before entering shelter | |||||||
| Yes | 7 | 7.69 | 10 | 8.85 | 0.766 | ||
| No | 84 | 92.31 | 103 | 91.15 | |||
| Narghile smoker, since entering shelter | |||||||
| Yes | 4 | 4.76 | 2 | 1.94 | 0.276 | ||
| No | 80 | 95.24 | 101 | 98.06 | |||
| Exposed to second-hand narghile smoke, before entering shelter | |||||||
| Yes | 28 | 33.33 | 29 | 28.16 | 0.444 | ||
| No | 56 | 66.67 | 74 | 71.84 | |||
| Exposed to second-hand narghile smoke, since entering shelter | |||||||
| Yes | 26 | 32.50 | 31 | 30.1 | 0.728 | ||
| No | 54 | 67.50 | 72 | 69.9 | |||
| Allergic rhinitis | |||||||
| Yes | 52 | 57.14 | 29 | 25.66 | <0.0001 | ||
| No | 39 | 42.86 | 84 | 74.34 | |||
| FEV1 (%) before bronchodilators | |||||||
| Mean ± SD | 83±23 | – | 89±17 | – | 0.013 | ||
| FEV1 (%) before bronchodilators (n=195) | |||||||
| <80 | 40 | 45.45 | 29 | 27.10 | 0.008 | ||
| FEV1 (%) after bronchodilators (n1=27, n2=10) | |||||||
| Mean ± SD | 76±25 | – | 84±21 | – | 0.403 | ||
| FEV1 (%) after bronchodilators | |||||||
| <80 | 15/27 | 55.56 | 4/10 | 40.00 | 0.401 | ||
| FEV1/FVC (%) after bronchodilators | |||||||
| <70 | 17/85 | 20.00 | 5/104 | 4.81 | 0.001 | ||
| Oxygen saturation (SpO2) (%) | |||||||
| Mean ± SD | 97±2 | – | 97±2 | – | |||
| Systolic blood pressure (mmHg) (in>30 years) | |||||||
| Mean ± SD | 130±32 | – | 130±31 | – | |||
| Systolic blood pressure (mmHg) (in>30 years) | |||||||
| >140 | 16/57 | 28.07 | 19/71 | 26.76 | |||
| Diastolic blood pressure (mmHg) | |||||||
| Mean ± SD | 85±20 | – | 82±18 | – | |||
| Any symptom of PTSD | |||||||
| Yes | 20 | 35.09 | 11 | 15.71 | <0.05 | ||
| No | 37 | 64.91 | 59 | 84.29 | |||
| Missing | 34 | – | 43 | – | |||
| Symptoms of PTSD | |||||||
| Physical symptoms | 11 | 55.00 | 4 | 36.36 | 0.696 | ||
| Flashbacks | 3 | 15.00 | 3 | 27.27 | |||
| Cognitive symptoms | 4 | 20.00 | 2 | 18.18 | |||
| Multiple symptoms | 2 | 10.00 | 2 | 18.18 | |||
P values in italic form indicate statistical significance if P<0.05.
The mean FEV1% for the under-diagnosed asthma group (83%, SD: 23%) was lower than that of the no asthma group (89%, SD: 17%). More than 45.5% (40 persons) of those in the under-diagnosed asthma group had an FEV1% of less than 80%, indicating an obstructive defect, compared to only 27% in the no asthma group. Four persons of 10 in the no asthma group who underwent reversibility test continued to have FEV1 <80%, and FEV1/FVC <70% in 5 persons (5/104=4.81%). One in 5 persons (17/85=20%) in the under-diagnosed asthma group continued to have FEV1/FVC <70% after bronchodilators which is indicative of fixed airway disease (i.e., COPD, or asthma and COPD overlap).
Discussion
In our study, which included both children and adults settled in the Al-Herjalleh shelter, we estimated the prevalence of asthma to be 8.5%, which is consistent with the average of estimates from the International Study of Asthma and Allergies in Childhood (ISAAC) and the WHO-Global Alliance against Chronic Respiratory Disease (WHO-GARD). ISAAC estimated that the prevalence of asthma (defined as wheezing in the last 12 months without having a cold in children aged 13–14 years) was 5.2% in Syria (9), and according to a primary care survey implemented in collaboration with the WHO-GARD, the prevalence of asthma in Syrian individuals presenting to a primary care center for any reason was estimated to be 13% (10). The average of these two asthma prevalence estimates, 9.1%, is very close to what we observed in the Al-Herjalleh shelter.
Individuals with previously diagnosed asthma at the Al-Herjalleh shelter had poorly controlled and worsening asthma, which impacted their quality of life. Daily ICS use was low, declining from 30.1% before entering the shelter to 4.3% in the shelter, and only half of those using an inhaler demonstrated the correct technique. The war and subsequent displacement have led those with asthma to be exposed to several new triggers, including odors, stress, SHS, and chemicals. A number of individuals with asthma have also taken up smoking cigarettes or narghile since entering the shelter. Surprisingly, the proportion of individuals experiencing severe asthma attacks did not change significantly after entering the shelter, nor did their access to emergency department. However, nearly half of them took oral corticosteroids as rescue medication. Nighttime symptoms are considered the most sensitive and specific for asthma diagnosis in validated epidemiological studies such as the ECRHS (11). In the non-asthma group, a shocking 44.2% of participants reported episodes of wheezing, coughing and breathlessness at night, consistent with under-diagnosed asthma. A high proportion of those subdivided into the under-diagnosed asthma group (35.1%) reported symptoms of PTSD, which may account for their shortness of breath or coughing at night (paroxysmal nocturnal dyspnea, wheeze and cough). It is plausible because individuals with PTSD exhibit an altered phenotype of regulatory T cells (12) and furthermore, it has been suggested that asthma onset can be linked to family/personal disasters (13) which is the case in these shelter dwellers (loss of home and/or family member).There are also other adverse factors in shelter living. For example, cooking in the same room where the family lives may increase the exposure to particulate matters (PM2.5) which can exacerbate asthma (14). Other triggers include use of detergent such as bleach (sodium hypochlorite), which is widely used in Syria (15) and amongst the shelter dwellers, exposure to SHS (16,17) and poverty (17,18) (the study participants had an average daily income of less than 2 USD/day). Finally, our spirometry data also suggested that both asthma and COPD were severely under-diagnosed, and thus not adequately managed.
The findings of our study highlight the need for asthma programs in Syrian shelters, as significant gaps exist in both the screening and management of chronic respiratory diseases. Although a primary care centre was nearby, and those in the Al-Herjalleh shelter had access to an emergency department during the conflict, however, screening and management campaigns were not integrated into the shelters. Fortunately, since our survey was conducted, collaborators from the Non-Communicable Disease (NCD) Department at the Syrian Ministry of Health (MOH) and the WHO country office agreed to include shelters in the national chronic respiratory disease program. Already, the MOH has distributed ICS to shelter dwellers with asthma, and provided training for primary care doctors and nurses in chronic respiratory disease. The MOH is also collaborating with Tishreen University and WHO Country office to publish national guidelines on evidence-based diagnosis and management of chronic respiratory disease. With continued funding, support and evaluation, we hope these programs will minimize asthma deterioration in Syrian shelter dwellers.
Conclusions
Amongst shelter dweller in Syria, asthma is uncontrolled and poorly managed and underdiagnosed asthma is prevalent. More than 2 of 5 of those indicated without asthma had night attacks of wheeze, cough and breathlessness consistent with asthma with the majority of them confirmed of asthma with lung function measures. Fixed airflow limitation after bronchodilators allude to underdiagnosed COPD, very severe uncontrolled asthma, or asthma-COPD overlap (19,20). As result to our survey and findings, shelters have been included in the national program of Chronic Respiratory Disease (CRD) launched in collaboration amongst the MOH, the Ministry of Higher Education and the WHO country office.
Acknowledgements
We thank the Syrian Private University Council for sponsoring the survey. Special thanks to: Drs. Fatmeh Hassan and Bashar Kaddour of the Department of Rural Health in Damascus for their administrative and implementation assistance in the field work; Drs. Rania Shifa and Ahmad Dmeirieh of the Directorate of NCD in MOH for initiating the National Committee for Chronic Respiratory Disease in collaboration with WHO and the Ministry of Higher Education; and Drs. Elizabeth Hoff, Aicha Al-jaber and Ghada Muhjazi of the WHO country office for reviewing the manuscript prior to submission. Last but not least, we acknowledge the Global Alliance Against Chronic Respiratory Disease (GARD www.who.int/gard) for the opportunity to collaborate with the Ontario Asthma Surveillance Information System (OASIS) in Toronto, Canada. The study was funded by a grant from the Syrian Private University. Damascus Hospital and Tishreen University gave Spirometric equipment.
Supplement I Online supplement: study questionnaires
Ethical statement: Ethical approval was obtained according to our university rules. Written informed consent was obtained from the patient for publication of this manuscript and any accompanying images.
Footnotes
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- 1.The United Nations Refugee Agency (Syria). Internally Displaced People. Accessed June 28 2017. Available online: http://www.unhcr.org/sy/29-internally-displaced-people.html
- 2.Syria Emergency Shelter Sector. Syria Emergency Shelter Sector Factsheet, 2016 August. Accessed June 28 2017. Available online: http://www.unhcr.org/sy/wp-content/uploads/sites/3/2016/11/Shelter-Sector-August.pdf
- 3.Kolwaite AR, Hlady WG, Simon MC, et al. Assessing functional needs sheltering in Pike County, Kentucky: using a community assessment for public health emergency response. Disaster Med Public Health Prep 2013;7:597-602. 10.1017/dmp.2013.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Szema AM, Peters MC, Weissinger KM, et al. New-onset asthma among soldiers serving in Iraq and Afghanistan. Allergy Asthma Proc 2010;31:67-71. [DOI] [PubMed] [Google Scholar]
- 5.Cutuli JJ, Herbers JE, Rinaldi M, et al. Asthma and behavior in homeless 4- to 7-year-olds. Pediatrics 2010;125:145-51. 10.1542/peds.2009-0103 [DOI] [PubMed] [Google Scholar]
- 6.Ohkouchi S, Shibuya R, Yanai M, et al. Deterioration in regional health status after the acute phase of a great disaster: respiratory physicians' experiences of the Great East Japan Earthquake. Respir Investig 2013;51:50-5. 10.1016/j.resinv.2012.12.003 [DOI] [PubMed] [Google Scholar]
- 7.To T, Guttmann A, Lougheed MD, et al. Evidence-based performance indicators of primary care for asthma: a modified RAND Appropriateness Method. International Journal for Quality in Health Care 2010;22:476-85. 10.1093/intqhc/mzq061 [DOI] [PubMed] [Google Scholar]
- 8.To T, McLimont S, Daly C, et al. Is it feasible to use indicators to collect data on asthma care performance in the primary care setting? A feasibility study. Prim Care Respir J 2011;20:452-3. 10.4104/pcrj.2011.00081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mohammad Y, Tabbah K, Mohammad S, et al. International study of asthma and allergies in childhood: phase 3 in the Syrian Arab Republic. East Mediterr Health J 2010;16:710-6. [PubMed] [Google Scholar]
- 10.Mohammad Y, Shaaban R, Yassine F, et al. Executive summary of the multicenter survey on the prevalence and risk factors of chronic respiratory diseases in patients presenting to primary care centers and emergency rooms in Syria. J Thorac Dis 2012;4:203-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Burney PG, Luczynska C, Chinn S, et al. The European Community Respiratory Health Survey. Eur Respir J 1994;7:954-60. 10.1183/09031936.94.07050954 [DOI] [PubMed] [Google Scholar]
- 12.Jergović M, Bendelja K, Vidovic A, et al. Patients with posttraumatic stress disorder exhibit an altered phenotype of regulatory T cells. Allergy Asthma Clin Immunol 2014;10:43. 10.1186/1710-1492-10-43 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Halimi L, Vachier I, Varrin M, et al. Interference of psychological factors in difficult-to-control asthma. Respir Med 2007;101:154-61. 10.1016/j.rmed.2006.03.036 [DOI] [PubMed] [Google Scholar]
- 14.Phillips MJ, Smith EA, Mosquin PL, et al. Sri Lanka Pilot Study to Examine Respiratory Health Effects and Personal PM2.5 Exposures from Cooking Indoors. Int J Environ Res Public Health 2016;13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Quirce S, Barranco P. Cleaning agents and asthma. J Investig Allergol Clin Immunol 2010;20:542-50; quiz 2p following 550. [PubMed]
- 16.Mohammad Y. Passive smoking interference with wheezing and asthma: short review of current knowledge. Pulmonology and Respiratory Research 2015;3:1 10.7243/2053-6739-3-2 [DOI] [Google Scholar]
- 17.Zar HJ, Ferkol TW. The global burden of respiratory disease-impact on child health. Pediatr Pulmonol 2014;49:430-4. 10.1002/ppul.23030 [DOI] [PubMed] [Google Scholar]
- 18.Fattore GL, Santos CA, Barreto ML. Social determinants of childhood asthma symptoms: an ecological study in urban Latin America. J Community Health 2014;39:355-62. 10.1007/s10900-013-9769-7 [DOI] [PubMed] [Google Scholar]
- 19.Global Initiative for Asthma (GINA). Global strategy for asthma management and prevention. 2017. Accessed June 28 2017. Available online: http://www.ginasthma.org
- 20.(GOLD) TGIfCOLD. Global initiative for chronic obstructive lung diseases 2017. Accessed June 28 2017. Available online: http://www.goldcopd.org


