Abstract
Purpose
To evaluate the safety and tolerability of intravitreal ISTH0036, an antisense oligonucleotide selectively targeting transforming growth factor beta 2 (TGF-β2), in patients with primary open angle glaucoma (POAG) undergoing trabeculectomy (TE; glaucoma filtration surgery).
Methods
In this prospective phase I trial glaucoma patients scheduled for TE with mitomycin C (MMC) received a single intravitreal injection of ISTH0036 at the end of surgery in escalating total doses of 6.75 μg, 22.5 μg, 67.5 μg or 225 μg, resulting in calculated intraocular ISTH0036 concentrations in the vitreous humor of approximately 0.3 μM, 1 μM, 3 μM or 10 μM after injection, respectively. Outcomes assessed included: type and frequency of adverse events (AEs), intraocular pressure (IOP), numbers of interventions post trabeculectomy, bleb survival, visual acuity, visual field, electroretinogram (ERG), slit lamp biomicroscopy and optic disc assessment.
Results
In total, 12 patients were treated in the 4 dose groups. Main ocular AEs observed were corneal erosion, corneal epithelium defect, or too high or too low IOP, among others. No AE was reported to be related to ISTH0036. All other safety-related analyses did not reveal any toxicities of concern, either. The mean medicated preoperative IOP at decision time-point for surgery was 27.3 mmHg +/- 12.6 mmHg (SD). Mean IOP (±SD) for dose levels 1, 2, 3, and 4 were at Day 43 9.8 mmHg ± 1.0 mmHg, 11.3 mmHg ± 6.7 mmHg, 5.5 mmHg ± 3.0 mmHg and 7.5 mmHg ± 2.3 mmHg SD; and at Day 85 9.7 mmHg ± 3.3 mmHg, 14.2 mmHg ± 6.5 mmHg, 5.8 mmHg ± 1.8 mmHg and 7.8 mmHg ± 0.6 mmHg, respectively. In contrast to IOP values for dose levels 1 and 2, IOP values for dose levels 3 and 4 persistently remained below 10 mmHg throughout the observation period.
Conclusion
This first-in-human trial demonstrates that intravitreal injection of ISTH0036 at the end of TE is safe. Regarding IOP control, single-dose ISTH0036 administration of 67.5 μg or 225 μg at the time of TE resulted in IOP values persistently < 10 mmHg over the three month postoperative observation period.
Introduction
Glaucoma currently affects more than 70 million people worldwide [1] and is the second leading cause for irreversible blindness in the Western world [2]. The disease is characterized by optic nerve head damage, retinal ganglion cell death and progressive visual field loss. In the majority of cases increased IOP is present and appears to be a main contributing pathophysiologic factor. At present existing pharmacologic treatments are directed mainly towards the lowering of IOP.
The majority of patients is treated with IOP lowering therapy. However, if disease progresses in spite of maximally tolerated therapy surgery may be indicated. Trabeculectomy (TE; glaucoma filtration surgery) is one of the most frequent surgical interventions and allows for drainage of aqueous from the anterior chamber of the eye to the subconjunctival space. Despite alternative techniques and devices emerging, TE remains the most frequent procedure for IOP lowering worldwide [3, 4]. However, success of TE is endangered by postoperative scarring, resulting in fibrotic closure of the drainage and rising IOP [5, 6]. To prevent this scarring of conjunctival tissue and the Tenon’s capsule, currently antimetabolites such as MMC and 5-FU are used but are accompanied by unwanted side-effects [7, 8]. Delayed wound healing may even lead to blebitis, choroidal detachments, conjunctival dehiscence, bleb leakage, long-term hypotony [9] and dysesthesia [7, 8].
Transforming growth factor beta 2 (TGF-β2) has been linked to the main pathophysiologic events in glaucoma: (1) trabecular meshwork alteration by epithelial-to-mesenchymal transition resulting in rise of IOP is seen as driven by it [10], and (2) optic nerve head damage by tissue remodeling [11, 12]. Glaucoma patients not only have substantially elevated levels of TGF-β2 [13–16] but the optic nerve head as area of main glaucoma damage contains 70–100 fold elevated levels of TGF-β2 [11]. In addition, TGF-β2 also has been identified as a core driver of intraocular fibrosis [17–20], and specifically has been linked to fibrotic overgrowth following TE. Consequently, it is for several reasons of high interest to investigate the safety and efficacy of TGF-β2 targeting agents in glaucoma and specifically the TE setting. Ultimately, this may not only increase the success rate of glaucoma filtration surgery but may improve outcomes in glaucoma by providing optic nerve protection and preventing further alteration of the trabecular meshwork.
This study is the first-in-human trial of the locked nucleic acid technology modified 14-mer fully phosphorothioate antisense oligodeoxynucleotide ISTH0036 that selectively targets the TGF-β2 isoform. Preclinical data indicated favorable pharmacokinetic and pharmacodynamic properties with potent and selective long-term suppression of the target in in-vitro and in-vivo assays. In addition, ISTH0036 showed potent anti-fibrotic and antiangiogenic effects in a choroidal neovascularization in-vivo model and preserved bleb size and survival in a glaucoma filtration mouse model when administered intravitreally [21–23].
Materials and methods
Trial design and conduct
This prospective phase I, first-in-human, open-label, dose-escalation trial (EudraCT# 2014-004985-74, https://eudract.ema.europa.eu, and NCT02406833 on https://www.clinicaltrials.gov) was conducted between April 2015 and August 2016 at three trial sites (Department of Ophthalmology of Mainz University Medical Center, University Hospital Tuebingen and Otto-von-Guericke University Magdeburg, Germany). Objective of the study was to evaluate the safety and tolerability as well as to observe preliminary clinical efficacy of single intravitreal injections of ISTH0036 at the time of TE. The study was approved by the Ethics Committee of the State Chamber of Medicine Rhineland Palatinate, Mainz and the German Federal Institute for Drugs and Medical Devices, BfArM and was conducted in accordance with the Declaration of Helsinki.
Main inclusion criteria were age 18–80 years, a diagnosis of primary open-angle glaucoma (high tension or normal tension) with patients scheduled for TE due to not tolerating medical therapy or progressing in spite of maximally tolerated medical therapy. Exclusion criteria were history of any other form of glaucoma in either eye, history of relevant ocular trauma in either eye < 6 months, history of ocular infection or ocular inflammation in either eye < 3 months. Patients underwent a washout-period according to their treating surgeons’ standards (usually 4 weeks for topical beta-blockers and prostaglandins, 7 days for topical alpha-2-agonists and carbonic anhydrase inhibitors, and at least 14 days for any ophthalmic medication or substance which had not been taken at a stable dose).
Subjects received TE with topical MMC (100 μl of 0.2 mg/ml solution) and a single intravitreal injection of ISTH0036 at the end of the surgical procedure. Three subjects per dose level (DL) were enrolled, receiving escalating total intravitreal doses of 6.75 μg, 22.5 μg, 67.5 μg or 225 μg (injection volume 50 μl), respectively, resulting in calculated intraocular ISTH0036 concentrations in the vitreous humor of approximately 0.3 μM, 1 μM, 3 μM or 10 μM. The starting dose of 6.75 μg reflects 1/10th of the preclinical No Observed Adverse Effect Level (NOAEL) from a 4-week intravitreal rabbit toxicology study. In preclinical cell-based experiments, ISTH0036 potently and specifically suppressed TGF-β2 mRNA and protein with IC50 values of 0.4 and 0.7 μM, respectively, demonstrating that sub-micromolar concentrations were pharmacodynamically effective [24]. The upper limit of dose escalation was set based upon observed toxicological findings at higher doses. There was a minimum interval of 1 week between the ISTH0036 dosing of the first and all subsequent subjects in each cohort as an additional safety measure. Dose escalation was carried out when data from 3 subjects who had completed the dose limiting toxicity (DLT) monitoring period of 42 days were available and had been reviewed by the Cohort Review Committee and no DLT had been observed.
Standard concomitant medications during the post-operative phase were topical antibiotics, topical glucocorticoids, and topical atropine or equivalent. Depending on bleb status and if deemed necessary by the Investigator subconjunctival administration of 5-Fluorouracil (5-FU at 5 mg/0.5 ml) and topical anti-glaucoma medications (e.g. beta-blockers, alpha-2-agonists etc.) were permitted, as well as non-pharmacological interventions (e.g. needling, suture lysis or needling procedure) and were documented as post-trabeculectomy interventions.
Primary endpoint was type and frequency of AEs (AE reporting according to National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) v4.03) for the reporting period. Slit-lamp and fundus examination, vital signs and safety laboratory were performed at various timepoints throughout the study. An ERG was conducted at screening and at the end of the DLT period (week 6) to monitor retinal function. DLTs were defined as all toxicities observed during the 42 days DLT period following the intravitreal injection that are at least possibly related to ISTH0036 and are NCI CTCAE v4.03 AE ≥ Grade 3 or eye disorder AE ≥ Grade 2 or cataract, retinal detachment, retinopathy ≥ Grade 1. Slit lamp deterioration of two grades or more had to be reported as AE. Secondary endpoints were IOP at the end of the study, number of interventions post trabeculectomy, bleb filtering and bleb morphology, best corrected visual acuity, visual field, slit lamp biomicroscopy, and optic disc status as determined by biomorphometry of the optic disc Heidelberg Retinograph II (HRTII) and by photography of the optic disc. IOP was measured at baseline, week 6 and week 12 in both eyes by Goldmann applanation tonometry (in sitting position with same fluorescein and anesthetic agents at each measurement). For each eye, the mean of two readings or the median of three readings in case of differences > 2 mmHg were recorded for the analysis using the same calibrated Goldmann applanation tonometer throughout the study in a patient. Bleb morphology and bleb filtering was assessed by using slit lamp images on Day 3, week 6 and week 12. The bleb was classified using the Wuerzburg Bleb Classification Score [25]. Best corrected visual acuity (BCVA) was measured for both eyes under dim room light using Early Treatment Diabetic Retinopathy Study (ETDRS) charts and the logMAR scoring system (baseline, Day 3, week 6 and week 12). Visual field measurement took place at baseline, week 6 and week 12 using Humphrey or Octopus Standard 24–2 or 30–2 white on white perimetry. The eyelids, conjunctiva, cornea, iris/anterior chamber and lens were examined at baseline, week 6 and week 12 by slit lamp biomicroscopy. The stereometric parameters of the optic disc were measured on week 6 and week 12 by confocal scanning laser ophthalmoscopy with Heidelberg Retina Tomograph II (HRTII). The Moorefield’s Regression Analysis and the Topographic Change Analysis were used to detect progression. Optic disc photographs were taken to evaluate changes in the optic disc.
Investigational agent
ISTH0036 is a synthetic 14-mer fully phosphorothioate antisense oligodeoxynucleotide modified with locked nucleic acids [26] (3+3 LNA-modified gapmer) selectively targeting the messenger ribonucleic acid (mRNA) of the TGF-β2 isoform. Potent, selective, sequence- and dose-dependent downregulation of TGF-β2 mRNA and protein was detected in human A172, Panc1 and trabecular meshwork cells as well as in murine astrocytes treated with different concentrations of ISTH0036 [21–24]. In addition, decreased TGF-β2 mRNA and protein levels in ocular tissues were observed after a single intravitreal administration of ISTH0036 to New Zealand White rabbit eyes for up to 8 weeks duration [24]. The drug product contains 6.75 mg anhydrous ISTH0036 sodium salt/vial expressed as total oligonucleotide content. Immediately prior to administration, the lyophilized powder is reconstituted aseptically in isotonic (0.9%) saline solution to 50 μl injection volume in total.
Data review and protocol deviations
After closure of the database a review of data according to the ICH-guideline E9 was conducted in order to classify the whole patient population into two analysis sets by applying the corresponding criteria (full analysis set [FAS] reflective of all subjects included who completed at least the follow-up visit 6 weeks post injection and safety analysis set [SAS] reflective of all subjects that received at least one dose of study medication) and to also decide whether a protocol deviation is major or minor. 36 minor and one major protocol deviation were identified/reported for patients treated in this study. The minor protocol deviations were deviations from the scheduled timing of assessments or missed assessments. The one major protocol deviation occurred when a safety-relevant follow-up visit assessment was performed in error on Day 42 instead of Day 43 (one day before formal completion of the DLT period). None of the patients were excluded from the full analysis set (FAS) due to protocol deviations. FAS and SAS were identical populations.
Statistical analysis
For this phase I study no inferential statistical hypothesis was created, and descriptive analyses were conducted, only, using SAS® Statistical Analysis System, Version 9.3 or higher.
Results
Patient population
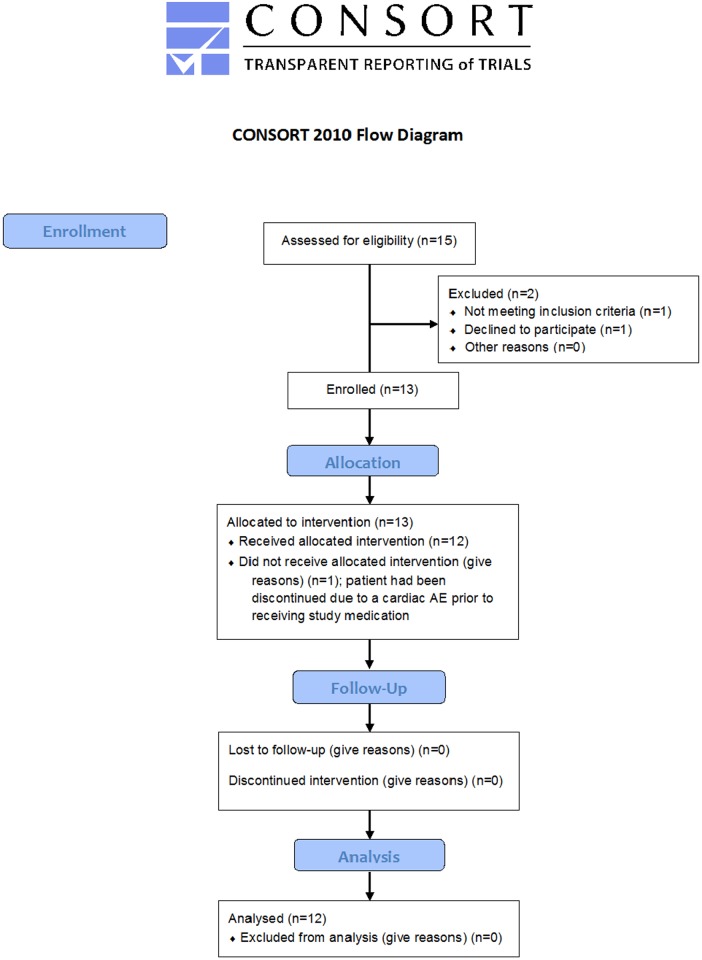
A total of 15 patients were enrolled in this study between April 2015 and August 2016. Twelve patients were included in the efficacy and safety analysis (one subject had failed screening, one had withdrawn consent, and one had been discontinued due to a cardiac AE, all prior to receiving study treatment) (Fig 1). Three of the twelve POAG patients included had been diagnosed with normal tension glaucoma, one each for DL 2, 3 and 4. Mean time since diagnosis of POAG was 12.3 ± 11.2 years (Table 1). At the time-point of inclusion all patients had been scheduled to undergo trabeculectomy as per decision of their treating ophthalmologist. The mean preoperative IOP at this time-point was 27.3 mmHg +/- 12.6 mmHg (SD). Detailed demographics are depicted in Table 1. The average number of anti-glaucoma medications at the time of decision for surgery was 3.3 ± 0.78 (substances), with use of prostaglandins in 10, beta-blockers in 10, carbonic anhydrase inhibitors in 10, and adrenergic agonists in 10 patients, respectively (Table 2).
Fig 1. CONSORT flow diagram.
Overview indicates the patient allocation.
Table 1. Demographics.
| Dose Level 1 | Dose Level 2 | Dose Level 3 | Dose Level 4 | Total | |
|---|---|---|---|---|---|
| 6.75 μg | 22.5 μg | 67.5 μg | 225 μg | ||
| (0.3 μM) | (1 μM) | (3 μM) | (10 μM) | ||
| N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | N = 12 (100%) | |
| Age (years) | |||||
| Mean | 65.0 | 63.0 | 66.7 | 70.0 | 66.2 |
| Median | 68.0 | 64.0 | 64.0 | 68.0 | 67.0 |
| SD | ± 13.75 | ± 16.52 | ± 4.62 | ± 5.29 | ± 10.01 |
| Range | 50–77 | 46–79 | 64–72 | 66–76 | 46–79 |
| Gender | |||||
| male, number (%) | 1 (33.3) | 2 (66.7) | 2 (66.7) | 2 (66.7) | 7 (58.3) |
| female, number (%) | 2 (66.7) | 1 (33.3) | 1 (33.3) | 1 (33.3) | 5 (41.7) |
| Type of POAG | |||||
| high tension POAG | 3 (100.0) | 2 (66.6) | 2 (66.6) | 2 (66.6) | 9 (75.0) |
| normal tension POAG | 0 (0.0) | 1 (33.3) | 1 (33.3) | 1 (33.3) | 3 (25.0) |
| Involved eye | |||||
| OD | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) |
| OS | 2 (66.7) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (16.7) |
| OU | 1 (33.3) | 3 (100.0) | 3 (100.0) | 3 (100.0) | 10 (83.3) |
| Time since diagnosis of POAG (years) | |||||
| Mean | 20.0 | 9.3 | 16.3 | 3.3 | 12.3 |
| Median | 23.0 | 10.0 | 10.0 | 3.0 | 8.5 |
| SD | ±15.72 | ± 15.72 | ± 13.65 | ± 1.53 | ± 11.18 |
| Range | 3–34 | 7–11 | 7–32 | 2–5 | 2–34 |
| IOP (mmHG) prior to trabeculectomy | |||||
| Mean | 36.3 | 23.3 | 20.5 | 28.83 | 27.25 |
| Median | 27.0 | 23.0 | 23.0 | 26.0 | 23.8 |
| SD | ± 18.82 | ± 9.5 | ± 4.77 | ± 13.48 | ± 12.56 |
Table 2. Preoperative anti-glaucoma medication.
| Dose Level 1 | Dose Level 2 | Dose Level 3 | Dose Level 4 | Total | |
|---|---|---|---|---|---|
| 6.75 μg | 22.5 μg | 67.5 μg | 225 μg | ||
| (0.3 μM) | (1 μM) | (3 μM) | (10 μM) | ||
| N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | N = 12 (100%) | |
| Number of preoperative anti-glaucoma medication componentsa | 3 (100) 10 | 3 (100) 12 | 3 (100) 10 | 3 (100) 8 | 12 (100) 40 |
| Meanb | 3.3 | 4.0 | 3.3 | 2.7 | 3.3 |
| SD | 1.15 | 0.00 | 0.58 | 0.58 | 0.78 |
| Rangec | 2–4 | 4–4 | 3–4 | 2–3 | 2–4 |
| Drug classa | |||||
| β-blocking agents | 2 (66.7) 2 | 3 (100) 3 | 3 (100) 3 | 2 (66.7) 2 | 10 (83.3) 10 |
| Carbonic anhydrase inhibitors | 3 (100) 3 | 3 (100) 3 | 1 (33.3) 1 | 3 (100) 3 | 10 (83.3) 10 |
| Prostaglandin analogues | 2 (66.7) 2 | 3 (100) 3 | 3 (100) 3 | 2 (66.7) 2 | 10 (83.3) 10 |
| Adrenergic agonists | 3 (100) 3 | 3 (100) 3 | 3 (100) 3 | 1 (33.3) 1 | 10 (83.3) 10 |
anumbers indicate patients per dose level receiving medication (percentage of patients) total number of anti-glaucoma medication components/substances
bMean: total number of preoperative anti-glaucoma medication components/number of patients receiving preoperative anti-glaucoma medication
cRange: lowest and highest number of preoperative anti-glaucoma medication components for patients in this dose group
Safety results
All twelve patients treated with ISTH0036 completed the dose limiting toxicity monitoring period at Day 43 and the end of study assessments at 12 weeks follow-up. No DLT occurred. A total of 36 AEs was recorded during this observation period. None was declared to be related to ISTH0036 or the intravitreal injection procedure. 16 were declared to be related to the primary surgery and 20 as not related to investigational drug, to the intravitreal injection procedure itself or surgery. Two serious adverse events occurred during the clinical study in one patient (choroidal effusion, ocular hypertension) in dose cohort 1 (0.3 μM) with both events assessed as not related to ISTH0036 or the intravitreal injection procedure but certain and probably/likely related to primary surgery. Of the 16 clinical AEs declared to be related to primary surgery nine were Grade 1 or 2 eye disorders, three Grade 3 eye disorders, four Grade 1 or 2 events were classified as investigations. No Grade 4 AE occurred in the study. Two Grade 3 events occurred in DL 1 and one Grade 3 events in DL 2, none were observed with DL 3 and 4. See Table 3 for a detailed AE listing. As additional safety monitoring element, ERG evaluations were performed at screening and at 6 weeks follow-up. In total, 24 ERGs in 12 patients were recorded. Due to the small size of the study, only a descriptive patient-by-patient analysis was conducted and no quantitative evaluations were performed. No relevant safety findings were identified by local readers. This was confirmed by a post-hoc external central review.
Table 3. Adverse events by relationship, type and grade.
| SOC | Adverse event (CTCAE Gradeb) | Dose Level 1 | Dose Level 2 | Dose Level 3 | Dose Level 4 | Total |
|---|---|---|---|---|---|---|
| 6.75 μg | 22.5 μg | 67.5 μg | 225 μg | |||
| (0.3 μM) | (1 μM) | (3 μM) | (10 μM) | |||
| N = 3 | N = 3 | N = 3 | N = 3 | N = 12 | ||
| Overall adverse events, n (%) | 7 (19.4) | 12 (33.3) | 11 (30.6) | 6 (16.7) | 36 (100) | |
| Relateda to ISH0036 | None | None | None | None | None | |
| Relateda to intravitreal injection | None | None | None | None | None | |
| Relateda to primary surgery | 3 | 7 | 4 | 2 | 16 | |
| Eye disorders: | 3 | 6 | 1 | 2 | 12 | |
| Corneal erosion | 0 | 1 | 0 | 0 | 1 | |
| Corneal epithelium defect | 0 | 1 | 0 | 0 | 1 | |
| Astigmatism | 0 | 0 | 0 | 1 (Gr.2) | 1 (Gr.2) | |
| Choroidal effusionc | 1 (Gr.3) | 0 | 0 | 0 | 1 (Gr.3) | |
| Conjunctival hemorrhage | 0 | 0 | 0 | 1 (Gr.2) | 1 (Gr.2) | |
| Conjunctival hyperaemia | 0 | 1 (Gr.2) | 0 | 0 | 1 (Gr.2) | |
| Corneal neovascularisation | 0 | 0 | 1 | 0 | 1 | |
| Corneal oedema | 0 | 1 | 0 | 0 | 1 | |
| Dry eye | 0 | 1 (Gr.2) | 0 | 0 | 1 (Gr.2) | |
| Eczema eyelids | 1 | 0 | 0 | 0 | 1 | |
| Ocular hypertensionc | 1 (Gr.3) | 0 | 0 | 0 | 1 (Gr.3) | |
| Visual acuity reduced | 0 | 1 (Gr.3) | 0 | 0 | 1 (Gr.3) | |
| Investigations: | 0 | 1 | 3 | 0 | 4 | |
| Intraocular pressure decreased | 0 | 1 | 1 (Gr.2) | 0 | 2 (1x Gr.2) | |
| Intraocular pressure increased | 0 | 0 | 2 (Gr.2) | 0 | 2 (Gr.2) | |
| Unrelateda | 4 | 5 | 7 | 4 | 20 | |
| Eye disorders: | 1 | 2 | 3 | 2 | 8 | |
| Corneal erosion | 1 | 0 | 1 (Gr.2) | 0 | 2 (1x Gr. 2) | |
| Conjunctival oedema | 0 | 0 | 1 (Gr.2) | 0 | 1 (Gr.2) | |
| Corneal epithelium defect | 0 | 1 (Gr.2) | 0 | 0 | 1 (Gr.2) | |
| Erythema of eyelid | 0 | 0 | 0 | 1 (Gr.2) | 1 (Gr.2) | |
| Lacrimation increased | 0 | 0 | 1 | 0 | 1 | |
| Ocular hyperaemia | 0 | 1 (Gr.2) | 0 | 0 | 1 (Gr.2) | |
| Vision blurred | 0 | 0 | 0 | 1 | 1 | |
| Infections and infestations: | 1 | 2 | 2 | 1 | 6 | |
| Nasopharyngitis | 1 | 2 | 0 | 1 (Gr.2) | 4 (1x Gr.2) | |
| Gingivitis | 0 | 0 | 1 | 0 | 1 | |
| Urinary tract infection | 0 | 0 | 1 | 0 | 1 | |
| Investigations: | 0 | 1 | 0 | 1 | 2 | |
| Intraocular pressure increasedd | 0 | 1 (Gr.2) | 0 | 0 | 1 (Gr.2) | |
| Vital dye staining cornea present | 0 | 0 | 0 | 1 (Gr.2) | 1 (Gr.2) | |
| Immune system disorders: | Drug hypersensitivity | 1 | 0 | 0 | 0 | 1 |
| Metabolism and nutrition disorders: | Gout | 0 | 0 | 1 (Gr.2) | 0 | 1 (Gr.2) |
| Musculoskeletal and connective tissue disorders: | Muscle spasms | 1 | 0 | 0 | 0 | 1 |
| Vascular disorders: | Hypertension | 0 | 0 | 1 | 0 | 1 |
aReasonable possibility (certain, probable/likely, possible); no reasonable possiblity (unlikely related or unrelated to ISTH0036, intravitreal injection and primary surgery)
bAEs with intencity CTCAE Grade ≥ 2 are indicated in brackets; all other AEs are CTCAE Grade 1
cSerious adverse event
dNon-study eye
Efficacy data
To determine potential preliminary clinical efficacy of ISTH0036 postoperative intraocular pressure course, number of interventions post TE, bleb morphology, best corrected visual acuity, visual field, slit lamp biomicroscopy, and optic disc status (Heidelberg Retinograph II (HRTII) and photograph of the optic disc) were recorded as secondary endpoints at defined time-points.
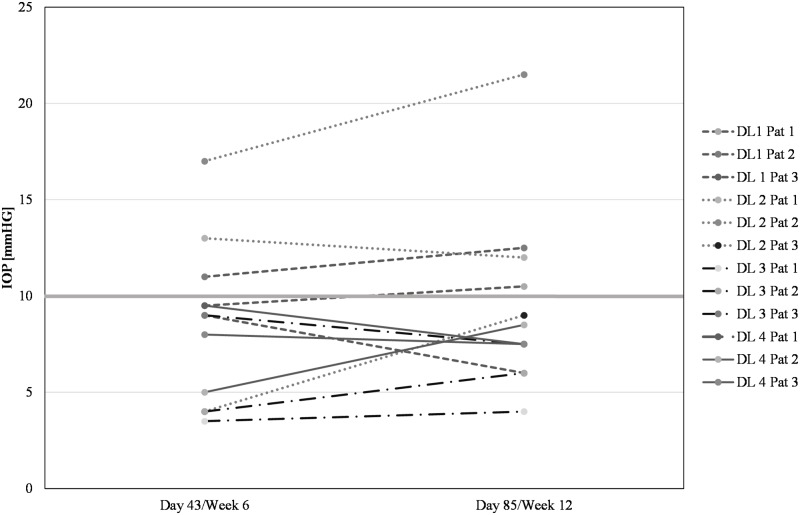
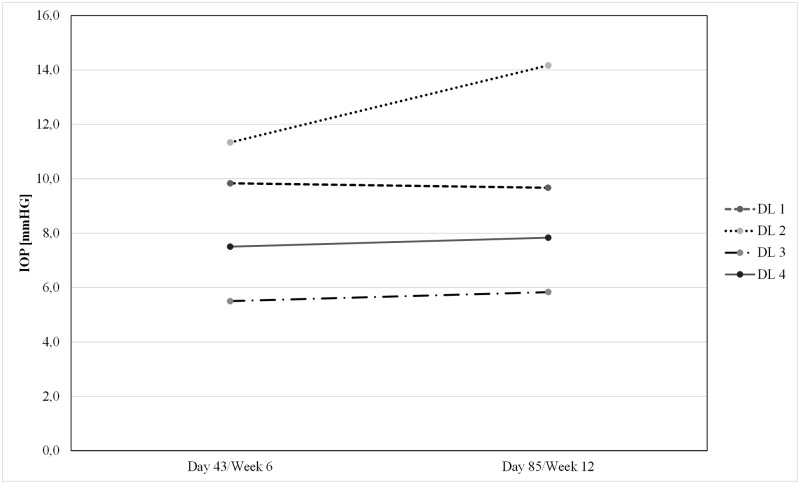
The mean preoperative IOP of all subjects at the time of decision for surgery was 27.3 mmHg ± 12.6 mmHg (SD). After trabeculectomy with standard administration of MMC and single intravitreal injection of ISTH0036, mean postoperative IOP values (± SD) for dose level 1, 2, 3 and 4 were at 6 weeks (Day 43) 9.8 mmHg (± 1.0 mmHg), 11.3 mmHg (± 6.7 mmHg), 5.5 mmHg (± 3.0 mmHg), and 7.5 mmHg (± 2.3 mmHg); and at 12 weeks (Day 85) 9.7 mmHg (± 3.3 mmHg), 14.2 mmHg (± 6.5 mmHg), 5.8 mmHg (± 1.8 mmHg) and 7.8 mmHg (± 0.6 mmHg), respectively (see Fig 2 for individual postoperative IOP course and Fig 3 for mean IOP course per dose level). In contrast to DL 1 and 2, IOP values for DL 3 and 4 consistently remained below 10 mmHg throughout the postoperative observation period (up to Day 85). These results are potentially indicative of a dose-response trend.
Fig 2. Postoperative intraocular pressure on Day 43 and Day 85 per patient.
Bar indicates 10 mmHg IOP level threshold not exceeded by DL 3 and DL 4 patients.
Fig 3. Mean intraocular pressure on Day 43 and Day 85 per dose level.
For most other efficacy parameters no clear trends or significant alterations were observed: number of interventions post trabeculectomy (overview see Table 4), visual field, slit lamp biomicroscopy, and optic disc status did not show any trends in any direction, in line with the duration of the observation period and the small patient number typical for a phase I study. For bleb filtering and bleb morphology there was overall a trend for increase in bleb score over time (except for DL 2; see Table 5 for details). In line with prior observations for trabeculectomy best corrected visual acuity (BCVA) worsened moderately in all patients at all dose levels for the observation period (Table 6), as described in other trabeculectomy outcome analyses, too [27].
Table 4. Postoperative interventions.
| Intervention | Dose Level 1 | Dose Level 2 | Dose Level 3 | Dose Level 4 | Total |
|---|---|---|---|---|---|
| 6.75 μg | 22.5 μg | 67.5 μg | 225 μg | ||
| (0.3 μM) | (1 μM) | (3 μM) | (10 μM) | ||
| N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | N = 12 (100%) | |
| Number | 3 (100) 8 | 3 (100) 8 | 3 (100) 14 | 2 (66.7) 10 | 11 (91.7) 40 |
| Mean | 2.7 | 2.7 | 4.7 | 3.3 | 3.3 |
| SD | ± 2.08 | ± 2.08 | ± 2.31 | ± 4.16 | ± 2.53 |
| Range | 1–5 | 1–5 | 2–6 | 0–8 | 0–8 |
| Type | |||||
| 5-FU | 5 (62.5) | 4 (50.0) | 5 (35.7) | 5 (50.0) | 19 (47.5) |
| Suturolysis | 1 (12.5) | 2 (25.0) | 4 (28.6) | 4 (40.0) | 11 (27.5) |
| Bulbus massage | 1 (12.5) | 0 | 2 (14.3) | 1 (10.0) | 4 (10.0) |
| Othera | 1 (12.5) | 2 (25.0) | 3 (21.4) | 0 | 6 (15.0) |
aOther: 1x addition of nylon sutures, 1x therapeutic lens and other therapeutics 3x glucocorticoid or 1x cycloplegic agents.
Table 5. Bleb filtering and morphology evaluation (Wuerzburg bleb classification Score).
| Wuerzburg Bleb Score | Wuerzburg Bleb Score | Wuerzburg Bleb Score | Wuerzburg Bleb Score | |
|---|---|---|---|---|
| Dose Level 1 | Dose Level 2 | Dose Level 3 | Dose Level 4 | |
| 6.75 μg (0.3 μM) | 22.5 μg (1 μM) | 67.5 μg (3 μM) | 225 μg (10 μM) | |
| N = 3 | N = 3 | N = 3 | N = 3 | |
| Day 3 | ||||
| Mean | 7.3 | 8.0 | 4.0 | 7.0 |
| SD | ± 2.52 | ± 2.65 | ± 0.00 | ± 2.00 |
| Range | 5–10 | 5–10 | 4–4 | 5–9 |
| Day 43 | ||||
| Mean | 10.0 | 8.7 | 9.3 | 7.7 |
| SD | ± 0.00 | ± 1.53 | ± 2.08 | ± 3.21 |
| Range | 10–10 | 7–10 | 7–11 | 4–10 |
| Day 85 | ||||
| Mean | 11.3 | 7.0 | 11.0 | 9.7 |
| SD | ± 0.58 | ± 1.00 | ± 0.00 | ± 1.53 |
| Range | 11–12 | 6–8 | 11–11 | 8–11 |
Table 6. Best corrected visual acuity (logMAR Score).
| logMAR Score | logMAR Score | logMAR Score | logMAR Score | |
|---|---|---|---|---|
| Dose Level 1 | Dose Level 2 | Dose Level 3 | Dose Level 4 | |
| 6.75 μg (0.3 μM) | 22.5 μg (1 μM) | 67.5 μg (3 μM) | 225 μg (10 μM) | |
| N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | N = 3 (100%) | |
| Screening | ||||
| Mean | 0.40 | 0.21 | 0.01 | 0.09 |
| SD | ± 0.31 | ± 0.21 | ± 0.12 | ± 0.25 |
| Baseline | ||||
| Mean | 0.41 | 0.17 | -0.03 | 0.14 |
| SD | ± 0.30 | ± 0.15 | ± 0.14 | ± 0.22 |
| Day 3 | ||||
| Mean | 0.72 | 0.26 | 0.25 | 0.55 |
| SD | ± 0.16 | ± 0.00 | ± 0.13 | ± 0.55 |
| Day 43 | ||||
| Mean | 0.58 | 0.41 | 0.23 | 0.28 |
| SD | ± 0.35 | ± 0.40 | ± 0.11 | ± 0.07 |
| Day 85 | ||||
| Mean | 0.51 | 0.27 | 0.12 | 0.27 |
| SD | ± 0.36 | ± 0.28 | ± 0.16 | ± 0.13± |
Discussion
Glaucoma continues to be a threat to visual function for millions of patients worldwide. Despite multiple medical treatment options, in the US alone more than 120.000 patients have turned bilaterally blind from glaucoma, representing 1/10 of all cases [27]. So far, the pathophysiology and underlying molecular mechanisms of glaucoma have not been fully understood [28]. However, IOP elevation plays a critical role in the majority of patients, and lowering of IOP can retard or even arrest progression of glaucoma. Retinal ganglion cell death appears to be initiated and impacted by several pathophysiologic mechanisms.
One important mechanism is tissue and extracellular matrix remodeling which may lead to trabecular meshwork alterations and subsequently IOP rise and tissue structure alterations of the optic nerve head, all resulting in direct and indirect optic nerve head damage. TGF-β2 has been recently identified as a key driver in those mechanisms and is now targeted for drug development [29]. In this context it is suggested that targeting TGF-β2 may (1) provide potent anti-fibrosis/anti-scarring activity in trabeculectomy (2) mediate effective neuroprotection by blocking extracellular matrix remodeling, and (3) prevent trabecular meshwork alteration, (with 2) and (3) both being central to glaucoma disease pathophysiology. Consequently, TGF-ß2 has become a prime target in glaucoma. Noteworthy, TGF-β2 has also been linked to other key ophthalmic diseases such as wet and dry age-related macular degeneration (AMD), diabetic retinopathy, proliferative vitreoretinopathy and corneal diseases, being involved in tissue remodeling and fibrotic processes [30].
For advanced-stage glaucoma it is therefore highly desirable to explore novel treatment options to achieve more optimal IOP control, and protect visual field more efficiently. ISTH0036 could play here an important role, by not only providing improved postoperative IOP control but also by preventing further alteration of the trabecular meshwork and the direct pathologic impact of elevated TGF-β2 levels on the optic nerve head [11].
In this first clinical exploration ISTH0036 demonstrated to be safe when administered in patients undergoing trabeculectomy with MMC. No adverse event observed was linked to ISTH0036 and safety evaluations such as ERG did not indicate any toxicity by the compound. Regarding efficacy, a dose-response trend regarding IOP could be observed for the two highest doses evaluated. Remarkably, none of the six patients treated at these dose levels exceeded an IOP of 10 mmHg in the observation period (12 weeks), maintaining early postoperative IOP in ranges shown to result in more favorable outcomes for patients [31]. No hypotony of clinical concern was observed. Despite the limited size of this phase I study and not being designed to demonstrate efficacy on statistically significant level this finding is suggestive of a potentially beneficial therapeutic effect.
An earlier exploration of anti-TGF-β treatment based upon an antibody (CAT-152) had failed to demonstrate a clinical benefit [32]. This failure appeared to be due to several limitations: The dosing strategy for CAT-152 appeared suboptimal (administration just between Day -1 and Day 8 although the scarring process is expected to last for many months, a comparatively short half-life and pharmacodynamic effect of the compound, with limited PK/PD explorations available. Furthermore, the subconjunctival administration might also have contributed to the lack of efficacy. ISTH0036 may provide a different option here, with long tissue half-life and pharmacodynamic activity persisting for up to 8 weeks in preclinical in vivo models. Therefore, repeat dosing up to one year is planned for phase II studies to maintain an anti-fibrotic effect for clinically relevant time-periods.
Despite various surgical options, trabeculectomy remains a standard surgical intervention by which aqueous humor is drained from the anterior chamber to the subconjunctival space forming a filtration bleb. Alternative methods, such as microinvasive surgical techniques, have been developed but did not surpass the results achieved with trabeculectomy nor replace it [33]. Excessive wound healing in the subconjunctival space is the major threat for long-term success with glaucoma filtration surgery (and the alternative surgical interventions) and is the most frequent cause for failure of TE [5, 34]. While wound healing in general is a physiologic and positive phenomenon, in TE wound healing resulting in excessive scarring and closure of the surgically opened drainage canal and filtering bleb represents a major threat to success. Consequently, to suppress excessive scarring various agents have been explored in past decades in randomized trials, among them anti-metabolites such as 5-FU and MMC.
At present, solely MMC has been approved as an anti-scarring agent in trabeculectomy (US, only), but is frequently used on an off-label basis in other regions of the world. 5-FU appears to be overall significantly less active than MMC [35, 36]. In addition, corticosteroids are routinely used as postoperative anti-inflammatory agent with some, though quite limited anti-fibrotic activity. MMC has been explored in numerous studies in the past decades at different concentrations and exposure durations. Variability in study populations, dose/exposures explored and assessment time-point and endpoint variability do not allow for direct comparisons across most studies and make meta-analyses quite challenging. Yet, various clinical data support that MMC is effective in achieving IOP lowering versus (vs.) placebo when administered during trabeculectomy. In five randomized and prospective studies that were conducted between 1995 and 2015 [6, 37–40], MMC use resulted in mean IOP values of 10.6/11.0 mmHg at 3 months and 9.9/12.2/12.8/13.7/13.7 mmHg at 12 months. Various large retrospective studies [41] report similar IOP ranges achieved with MMC use post TE. In a meta-analysis Fendi et al. [42] analyzed 5 randomized, controlled trials (RCT) that compared MMC with 5-FU in TE. MMC use was associated with a statistically significantly lower mean IOP level following TE than 5-FU, with a mean IOP of 11.25 mmHg vs. 13.58 mmHg with 5-FU (p < 0.001). Three RCTs within this meta-analysis evaluated the qualified surgical success rates defined as IOP < 18 mmHg. The MMC group showed in a pooled analysis a higher qualified success rate (130/156 [83.3%]) than the 5-FU group (111/148 [75.0%]; p = 0.04). In conclusion, prospective as well as retrospective studies and meta-analyses have shown that MMC as adjuvant results in lower IOP as compared to placebo or 5-FU. Achieved IOP improvement vs. placebo or other controls ranged depending on study and conditions/population from roughly 2.0 to over 5.0 mmHg in the first year.
MMC is effective in maintaining a comparatively lower IOP post trabeculectomy by an anti-scarring effect vs. other agents. However, this effect comes at a price. The Center for Drug Evaluation review of MMC (Mitosol™) lists as most frequent adverse reactions to topical MMC use in trabeculectomy hypotony, choroidal detachment, shallow anterior chamber, hyphema, corneal endothelial defects, and cataract progression. Frequencies range from 0–3% but also from 30–50% within different studies. This may depend on study design (retrospective versus prospective) but also on the adverse event reporting regulations applied [http://www.accessdata.fda.gov/drugsatfda_docs/nda/2012/022572Orig1s000MedR.pdf].
MMC does not block glaucoma-specific pathophysiologic processes nor does it prevent glaucoma progression apart from its anti-scarring effect after trabeculectomy. The fact that individuals still progress to blindness despite availability of effective surgical interventions and the frequency of postoperative IOP rises underlines the need for further improvement with effective agents targeting the underlying pathology of glaucoma.
Due to the need for improved IOP control and the suboptimal AE profile of MMC alternatives have been explored. Here in past years a main focus was on anti-vascular endothelial growth factor (VEGF) treatments, such as bevacizumab, ranibizumab, aflibercept. It is debatable whether the scarring process is mainly dependent upon vascularization, but wound healing disturbances observed with systemic use of anti-VEGF agents in cancer patients and molecular evidence for the role of VEGF in this regard [43] support a distinct role in the wound healing process. Yet, although some early trials suggested that anti-VEGF agents may have some effect against scarring and bleb failure, other reports fail to demonstrate this effect. A recent large meta-analysis of 9 studies with 349 patients came to the conclusion that antimetabolites are more effective in IOP lowering than anti-VEGF approaches, and that combining MMC with anti-VEGF compounds does not improve in a statistically significant way the complete or qualified success rate of trabeculectomy [44]. In the trabeculectomy setting some effects on IOP appear to be achievable on top of MMC, but again no improved success rates could be demonstrated so far [45]. Consequently, at present anti-VEGF treatment is not seen as a clinical standard in the trabeculectomy setting for POAG.
Recent scientific analyses have demonstrated that it is highly desirable to stabilize the early postoperative IOP in ranges below 10 mmHg, in some cases even below 8 mmHg [31]. While by the use of MMC alone such IOP ranges are rarely reached, achieving such IOP is highly desirable as this is indicative of long-term success of trabeculectomy. It heralds better clinical outcome for the patient, both in POAG and in closed-angle glaucoma [31, 46],.
A randomized, prospective trial will be needed to clarify if ISTH0036 may be efficacious in combination with MMC or even may be sufficiently efficacious as monotherapy alone. Therapeutic target would be to achieve consistent IOP ranges of 6–10 mmHg for patients post trabeculectomy and to provide significantly improved IOP control over MMC alone. Naturally, hypotony rates need to be monitored carefully in phase II to determine whether the combination with MMC may not be too potent and may result in too low IOPs for some patients. In addition, in monotherapy or combination, additional potentially beneficial effects such as neuroprotection and trabecular meshwork protection by preventing further extracellular matrix remodeling of the optic nerve head area and the trabecular meshwork may contribute further to a potential beneficial effect.
Noteworthy, TGF-β has not only been shown to be involved in glaucoma pathophysiology, but in recent years has also been linked to various other major ophthalmic diseases such as wet [47] and dry [30] AMD, diabetic retinopathy [48], proliferative vitreoretinopathy [49, 50], secondary cataract [51] and corneal disease [52]. With its anti-fibrotic and antiangiogenic effects ISTH0036 currently also undergoes preclinical evaluation in other disease models than glaucoma to consider expansion of development into these disease entities.
In summary, this first-in-human study of ISTH0036 demonstrates that selective suppression of TGF-β2 with single doses of this LNA-based antisense oligonucleotide is safe and potentially clinically efficacious. Signs of a potentially meaningful clinical activity have been observed in terms of a dose-response trend and encouraging IOP control < 10 mmHg for the first 12 weeks for all patients treated at dose levels 3 and 4 (67.5 μg or 225 μg dose). In the light of its potent anti-fibrotic effect, but also the suspected capability to block major glaucoma pathophysiology mechanisms (epithelial-to-mesenchymal transition of the trabecular meshwork, extracellular matrix remodeling affecting the optic nerve head, other mechanisms) ISTH0036 warrants further clinical evaluation in glaucoma filtration surgery. Due to the potent anti-fibrotic effect and the additionally observed potent antiangiogenic effect other ophthalmic diseases that are linked to TGF-β2 (wet AMD, dry AMD, diabetic retinopathy, proliferative vitreoretinopathy) may also be explored for ISTH0036 development.
Supporting information
(PDF)
(PDF)
(PDF)
(TIF)
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was fully sponsored by Isarna Therapeutics GmbH (study design, data collection and analysis, decision to publish, or preparation of the manuscript). The sponsor did not provide any salaries to Investigators. Norbert Pfeiffer is Coordinating Investigator of the study and a paid member of the scientific advisory board to Isarna Therapeutics GmbH. Bogomil Voykov is an Investigator and received a travel grant from Isarna Therapeutics GmbH. Giulia Renieri, Katharina Bell, Paul Richter, Melanie Weigel, Hagen Thieme and Barbara Wilhelm are Investigators and have no further financial relationship to the sponsor. Martin Feindor is an employee of and Katrin Lorenz is a consultant to SynteractHCR. SynteractHCR is a contract research organization paid for by Isarna Therapeutics GmbH. Katja Wosikowski, Daniela Päckert, Regina Römmich, Carola Mala and Petra Fettes are employees of Isarna Therapeutics GmbH. Michel Janicot and Eugen Leo are consultants to Isarna Therapeutics GmbH. Isarna Therapeutics GmbH provided support in the form of salaries for authors KW, DP, RR, CM and PF and consultant payments for authors EL and MJ. Isarna Therapeutics had a role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section. SynteractHCR provided support in the form of salary for author MF and consultant payments for author KL, but did not have any additional role in the study design, data collection and analysis, decision to publish, or preparation of the manuscript. The specific roles of these authors are articulated in the ‘author contributions’ section.
References
- 1.Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262–7. doi: 10.1136/bjo.2005.081224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kingman S. Glaucoma is second leading cause of blindness globally. Bulletin of the World Health Organization. 2004;82(11):887–8. [PMC free article] [PubMed] [Google Scholar]
- 3.Burr J, Azuara-Blanco A, Avenell A, Tuulonen A. Medical versus surgical interventions for open angle glaucoma. The Cochrane database of systematic reviews. 2012(9):CD004399 doi: 10.1002/14651858.CD004399.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hitchings R. Initial treatment for open-angle glaucoma- medical, laser, or surgical? Surgery is the treatment of choice for open-angle glaucoma. Arch Ophthalmol. 1998;116(2):241–2. [DOI] [PubMed] [Google Scholar]
- 5.Lama PJ, Fechtner RD. Antifibrotics and wound healing in glaucoma surgery. Surv Ophthalmol. 2003;48(3):314–46. [DOI] [PubMed] [Google Scholar]
- 6.Saeed AM. Comparative study between trabeculectomy with photodynamic therapy (BCECF-AM) and trabeculectomy with antimetabolite (MMC) in the treatment of primary open angle glaucoma. Clinical ophthalmology. 2012;6:1651–64. doi: 10.2147/OPTH.S29909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Al Habash A, Aljasim LA, Owaidhah O, Edward DP. A review of the efficacy of mitomycin C in glaucoma filtration surgery. Clinical ophthalmology. 2015;9:1945–51. doi: 10.2147/OPTH.S80111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fan Gaskin JC, Nguyen DQ, Soon Ang G, O’Connor J, Crowston JG. Modulation in Glaucoma Filtration Surgery-Conventional Practices and New Perspectives: The Role of Antifibrotic Agents (Part I). Journal of current glaucoma practice. 2014;8(2):37–45. doi: 10.5005/jp-journals-10008-1159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mietz H, Krieglstein GK. Three-year follow-up of trabeculectomies performed with different concentrations of mitomycin-C. Ophthalmic surgery and lasers. 1998;29(8):628–34. [PubMed] [Google Scholar]
- 10.Damiano V, Caputo R, Garofalo S, Bianco R, Rosa R, Merola G, et al. TLR9 agonist acts by different mechanisms synergizing with bevacizumab in sensitive and cetuximab-resistant colon cancer xenografts. Proc Natl Acad Sci U S A. 2007;104(30):12468–73. doi: 10.1073/pnas.0705226104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fuchshofer R. The pathogenic role of transforming growth factor-beta2 in glaucomatous damage to the optic nerve head. Exp Eye Res. 2011;347(1):279–90. [DOI] [PubMed] [Google Scholar]
- 12.Schneider M, Fuchshofer R. The role of astrocytes in optic nerve head fibrosis in glaucoma. Exp Eye Res. 2016;142:49–55. doi: 10.1016/j.exer.2015.08.014 [DOI] [PubMed] [Google Scholar]
- 13.Inatani M, Tanihara H, Katsuta H, Honjo M, Kido N, Honda Y. Transforming growth factor-beta 2 levels in aqueous humor of glaucomatous eyes. Graefes Arch Clin Exp Ophthalmol. 2001;239(2):109–13. [DOI] [PubMed] [Google Scholar]
- 14.Min SH, Lee TI, Chung YS, al. E. Transforming growth factor-beta levels in human aqueous humor of glaucomatous, diabetic and uveitic eyes. Korean J Ophthalmol. 2006;20(3):162–5. doi: 10.3341/kjo.2006.20.3.162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ochiai Y, Ochiai H. Higher concentration of transforming growth factor-beta in aqueous humor of glaucomatous eyes and diabetic eyes. Jpn J Ophthalmol. 2002;46(3):249–53. [DOI] [PubMed] [Google Scholar]
- 16.Trivedi RH, Nutaitis M, Vroman D, Crosson CE. Influence of race and age on aqueous humor levels of transforming growth factor-beta 2 in glaucomatous and nonglaucomatous eyes. Journal of ocular pharmacology and therapeutics: the official journal of the Association for Ocular Pharmacology and Therapeutics. 2011;27(5):477–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tektas OY, Lütjen-Drecoll E. Structural changes of the trabecular meshwork in different kinds of glaucoma. Exp Eye Res. 2009;88(4):763–75. [DOI] [PubMed] [Google Scholar]
- 18.Bollinger KE, Crabb JS, Yuan X, Putliwala T, Clark AF, Crabb JW. Quantitative Proteomics: TGF{beta}2 Signaling in Trabecular Meshwork Cells. Invest Ophthalmol Vis Sci. 2011;52(11):8287–94. doi: 10.1167/iovs.11-8218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Fuchshofer R, Yu AH, Welge-Lüssen U, al. E. Bone morphogenetic protein-7 is an antagonist of transforming growth factor-beta2 in human trabecular meshwork cells. Invest Ophthalmol Vis Sci. 2007;48(2):715–26. doi: 10.1167/iovs.06-0226 [DOI] [PubMed] [Google Scholar]
- 20.Wordinger RJ, Sharma T, Clark AF. The role of TGF-beta2 and bone morphogenetic proteins in the trabecular meshwork and glaucoma. Journal of ocular pharmacology and therapeutics: the official journal of the Association for Ocular Pharmacology and Therapeutics. 2014;30(2–3):154–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hasenbach K, Bergen TV, Vandewalle E, Groef LD, Hove IV, Moons L, et al. Potent and selective antisense oligonucleotides targeting the transforming growth factor beta (TGF-β) isoforms in advanced glaucoma: a preclinical evaluation. Journal for Modeling in Ophthalmology. 2016;2(2):20–8. [Google Scholar]
- 22.Hasenbach K, Herrnberger L, Kuespert S, R. F, Korhonen H, Wosikowski K, et al., editors. Targeting Transforming Growth Factor beta 2 (TGF-β2) Isoform with ISTH0036—a Potent and Selective Antisense OligonucLeotide—for the Treatment of Glaucoma. ARVO; 2015; Denver, USA.
- 23.Wosikowski K, Van Hove I, Puranen J, de Groef L, Haapaniemi AM, Sergeys J, et al., editors. Targeting Transforming Growth Factor beta 2 (TGF-β2) mRNA with ISTH0036 as Novel Therapeutic Intervention in Neovascular Ocular Disease. The Annual Meeting of the Association for Research in Vision and Ophthalmology (ARVO) 2017; Baltimore, MD.
- 24.Wosikowski K, Hasenbach K, Allais L, Fant P, Bellebeau F, Truchot N, et al., editors. Preclinical Profile of ISTH0036, a Potent and Selective Antisense Oligonucleotide Targeting Transforming Growth Factor beta 2 (TGF-β2) for the Treatment of Ophthalmic Diseases. The Annual Meeting of the Association for Research in Vision and Ophthalmology (ARVO) 2015; Denver, CO.
- 25.Picht G, Grehn F. Classification of filtering blebs in trabeculectomy: biomicroscopy and functionality. Current opinion in ophthalmology. 1998;9(2):2–8. [DOI] [PubMed] [Google Scholar]
- 26.Saeed AM, AboulNasr TT. Subconjunctival bevacizumab to augment trabeculectomy with mitomycin C in the management of failed glaucoma surgery. Clinical ophthalmology. 2014;8:1745–55. doi: 10.2147/OPTH.S67730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lorenz K, Wasielica-Poslednik J, Bell K, Renieri G, Keicher A, Ruckes C, et al. Efficacy and safety of preoperative IOP reduction using a preservative-free fixed combination of dorzolamide/timolol eye drops versus oral acetazolamide and dexamethasone eye drops and assessment of the clinical outcome of trabeculectomy in glaucoma. PLoS One. 2017;12(2):e0171636 doi: 10.1371/journal.pone.0171636 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Weinreb RN, Aung T, Medeiros FA. The pathophysiology and treatment of glaucoma: a review. JAMA. 2014;311(18):1901–11. doi: 10.1001/jama.2014.3192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Prendes MA, Harris A, Wirostko BM, Gerber AL, Siesky B. The role of transforming growth factor beta in glaucoma and the therapeutic implications. Br J Ophthalmol. 2013;97(6):680–6. doi: 10.1136/bjophthalmol-2011-301132 [DOI] [PubMed] [Google Scholar]
- 30.Radeke MJ, Radeke CM, Shih YH, Hu J, Bok D, Johnson LV, et al. Restoration of mesenchymal retinal pigmented epithelial cells by TGFbeta pathway inhibitors: implications for age-related macular degeneration. Genome medicine. 2015;7(1):58 doi: 10.1186/s13073-015-0183-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Okimoto S, Kiuchi Y, Akita T, Tanaka J. Using the early postoperative intraocular pressure to predict pressure control after a trabeculectomy. J Glaucoma. 2014;23(6):410–4. doi: 10.1097/IJG.0b013e318285fd7d [DOI] [PubMed] [Google Scholar]
- 32.Khaw P, Grehn F, Hollo G, Overton B, Wilson R, Vogel R, et al. A phase III study of subconjunctival human anti-transforming growth factor beta(2) monoclonal antibody (CAT-152) to prevent scarring after first-time trabeculectomy. Ophthalmology. 2007;114(10):1822–30. doi: 10.1016/j.ophtha.2007.03.050 [DOI] [PubMed] [Google Scholar]
- 33.Richter GM, Coleman AL. Minimally invasive glaucoma surgery: current status and future prospects. Clinical ophthalmology. 2016;10:189–206. doi: 10.2147/OPTH.S80490 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Georgoulas S, Dahlmann-Noor A, Brocchini S, Khaw PT. Modulation of wound healing during and after glaucoma surgery. Progress in brain research. 2008;173:237–54. doi: 10.1016/S0079-6123(08)01117-5 [DOI] [PubMed] [Google Scholar]
- 35.Wong TT, Khaw PT, Aung T, Foster PJ, Htoon HM, Oen FT, et al. The singapore 5-Fluorouracil trabeculectomy study: effects on intraocular pressure control and disease progression at 3 years. Ophthalmology. 2009;116(2):175–84. doi: 10.1016/j.ophtha.2008.09.049 [DOI] [PubMed] [Google Scholar]
- 36.Masoumpour MB, Nowroozzadeh MH, Razeghinejad MR. Current and Future Techniques in Wound Healing Modulation after Glaucoma Filtering Surgeries. The open ophthalmology journal. 2016;10:68–85. doi: 10.2174/1874364101610010068 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Robin AL, Ramakrishnan R, Krishnadas R, Smith SD, Katz JD, Selvaraj S, et al. A Long-term Dose-Response Study of Mitomycin in Glaucoma Filtration Surgery. Arch Ophthalmol. 1997;115:969–74. [DOI] [PubMed] [Google Scholar]
- 38.Singh K, Mehta K, Shaikh NM, Tsai JC, Moster MR, Budenz DL, et al. Trabeculectomy with intraoperative mitomycin C versus 5-fluorouracil. Prospective randomized clinical trial. Ophthalmology. 2000;107(12):2305–9. [DOI] [PubMed] [Google Scholar]
- 39.Lamping KA, Belkin JK. 5-Fluorouracil and mitomycin C in pseudophakic patients. Ophthalmology. 1995;102(1):70–5. [DOI] [PubMed] [Google Scholar]
- 40.WuDunn D, Cantor LB, Palanca-Capistrano AM, Hoop J, Alvi NP, Finley C, et al. A prospective randomized trial comparing intraoperative 5-fluorouracil vs mitomycin C in primary trabeculectomy. American journal of ophthalmology. 2002;134(4):521–8. [DOI] [PubMed] [Google Scholar]
- 41.Bindlish R, Condon GP, Schlosser JD, D’Antonio J, Lauer KB, Lehrer R. Efficacy and Safety of Mitomycin-C in Primary Trabeculectomy. Ophthalmology. 2002;109(7):1336–41. [DOI] [PubMed] [Google Scholar]
- 42.De Fendi LI, Arruda GV, Scott IU, Paula JS. Mitomycin C versus5-fluorouracil as an adjunctive treatment for trabeculectomy: a meta-analysis of randomized clinical trials. Clinical & Experimental Ophthalmology. 2013;41(8):798–806. [DOI] [PubMed] [Google Scholar]
- 43.Bao P, Kodra A, Tomic-Canic M, Golinko MS, Ehrlich HP, Brem H. The role of vascular endothelial growth factor in wound healing. J Surg Res. 2009;153(2):347–58. doi: 10.1016/j.jss.2008.04.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Xiong Q, Li Z, Li Z, Zhu Y, Abdulhalim S, Wang P, et al. Anti-VEGF agents with or without antimetabolites in trabeculectomy for glaucoma: a meta-analysis. PLoS One. 2014;9(2):e88403 doi: 10.1371/journal.pone.0088403 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Takihara Y, Inatani M, Kawaji T, Fukushima M, Iwao K, Iwao M, et al. Combined intravitreal bevacizumab and trabeculectomy with mitomycin C versus trabeculectomy with mitomycin C alone for neovascular glaucoma. J Glaucoma. 2011;20(3):196–201. doi: 10.1097/IJG.0b013e3181d9ce12 [DOI] [PubMed] [Google Scholar]
- 46.Rong SS, Feng MY, Wang N, Meng H, Thomas R, Fan S, et al. Can early postoperative intraocular pressure predict success following mitomycin-C augmented trabeculectomy in primary angle-closure glaucoma. Eye. 2013;27(3):403–9. doi: 10.1038/eye.2012.291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nagineni CN, Samuel W, Nagineni S, Pardhasaradhi K, Wiggert B, Detrick B, et al. Transforming growth factor-beta induces expression of vascular endothelial growth factor in human retinal pigment epithelial cells: involvement of mitogen-activated protein kinases. J Cell Physiol. 2003;197(3):453–62. doi: 10.1002/jcp.10378 [DOI] [PubMed] [Google Scholar]
- 48.Gerhardinger C, Dagher Z, Sebastiani P, Park YS, Lorenzi M. The transforming growth factor-beta pathway is a common target of drugs that prevent experimental diabetic retinopathy. Diabetes. 2009;58(7):1659–67. doi: 10.2337/db08-1008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Connor TB Jr., Roberts AB, Sporn MB, Danielpour D, Dart LL, Michels RG, et al. Correlation of fibrosis and transforming growth factor-beta type 2 levels in the eye. J Clin Invest. 1989;83(5):1661–6. doi: 10.1172/JCI114065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Chen Z, Shao Y, Li X. The roles of signaling pathways in epithelial-to-mesenchymal transition of PVR. Mol Vis. 2015;21:706–10. [PMC free article] [PubMed] [Google Scholar]
- 51.Wormstone IM, Wang L, Liu CS. Posterior capsule opacification. Exp Eye Res. 2009;88(2):257–69. doi: 10.1016/j.exer.2008.10.016 [DOI] [PubMed] [Google Scholar]
- 52.Engler C, Chakravarti S, Doyle J, Eberhart CG, Meng H, Stark WJ, et al. Transforming growth factor-beta signaling pathway activation in Keratoconus. American journal of ophthalmology. 2011;151(5):752–9 e2. doi: 10.1016/j.ajo.2010.11.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
(PDF)
(PDF)
(TIF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.