Abstract
Aldose reductase (AR: human, AKR1B1; mouse, AKR1B3), the first enzyme in the polyol pathway, plays a key role in mediating myocardial ischemia/reperfusion (I/R) injury. In earlier studies, using transgenic mice broadly expressing human AKR1B1 to human-relevant levels, mice devoid of Akr1b3, and pharmacological inhibitors of AR, we demonstrated that AR is an important component of myocardial I/R injury and that inhibition of this enzyme protects the heart from I/R injury. In this study, our objective was to investigate if AR modulates the β-catenin pathway and consequent activation of mesenchymal markers during I/R in the heart. To test this premise, we used two different experimental models: in vivo, Akr1b3 null mice and wild type C57BL/6 mice (WT) were exposed to acute occlusion of the left anterior descending coronary artery (LAD) followed by recovery for 48 hours or 28 days, and ex-vivo, WT and Akr1b3 null murine hearts were perfused using the Langendorff technique (LT) and subjected to 30 min of global (zero-flow) ischemia followed by 60 min of reperfusion. Our in vivo results reveal reduced infarct size and improved functional recovery at 48 hours in mice devoid of Akr1b3 compared to WT mice. We demonstrate that the cardioprotection observed in Akr1b3 null mice was linked to acute activation of the β-catenin pathway and consequent activation of mesenchymal markers and genes linked to fibrotic remodeling. The increased activity of the β-catenin pathway at 48 hours of recovery post-LAD was not observed at 28 days post-infarction, thus indicating that the observed increase in β-catenin activity was transient in the mice hearts devoid of Akr1b3. In ex vivo studies, inhibition of β-catenin blocked the cardioprotection observed in Akr1b3 null mice hearts. Taken together, these data indicate that AR suppresses acute activation of β-catenin and, thereby, blocks consequent induction of mesenchymal markers during early reperfusion after myocardial ischemia. Inhibition of AR might provide a therapeutic opportunity to optimize cardiac remodeling after I/R injury.
Introduction
Acute myocardial infarction (AMI) remains the leading cause of morbidity and mortality worldwide [1]. The extent of myocardial tissue loss (infarct size) is a key determinant of the prognosis of patients with AMI. Timely reperfusion is the most effective way to limit infarct size in patients with AMI [2]. However, efficacy of reperfusion therapy is impaired by factors such as the severity of ischemia, inadequate reflow, presence of residual stenosis, coronary reocclusion, and reperfusion injury [3–5]. In the quest for novel therapeutic strategies for acute myocardial ischemia/reperfusion (I/R) injury, we have focused on interventions that modulate substrate metabolism [6, 7]. In this context, we and others demonstrated that the aldose reductase (AR) pathway contributes to myocardial I/R injury and that the inhibition of AR protects hearts from I/R damage [8–13]. Earlier studies showed that increased flux via AR during I/R leads to ATP depletion and increased mitochondrial oxidative stress, thereby significantly impeding the recovery process in the heart [9, 14, 15]. We and others demonstrated that pharmacological inhibition of AR improves functional recovery and reduces myocardial I/R injury [11, 13, 16, 17].
The Wnt/β-catenin pathway plays an important role in various biological processes including development, differentiation, proliferation and tissue homeostasis [18, 19]. Activation of the Wnt pathway culminates in the transcription of Wnt target genes via β-catenin. Wnt proteins form a family of highly conserved secreted signaling molecules. Upon binding of Wnt to the seven-transmembrane domain spanning frizzled (Fzd) receptor and the co-receptor lipoprotein receptor-related 5/6 (Lrp5/6) proteins, GSK3β is inactivated, thereby preventing the breakdown of β-catenin. After stabilization and accumulation, β-catenin enters the nucleus, where it binds to LEF/TCF transcription factors to activate the transcription of Wnt target genes [20, 21]. Several studies have shown involvement of the canonical Wnt/β-catenin signaling pathway in the pathogenesis of I/R injury [22–24] and that phosphorylation of GSK3β is a key determinant of β-catenin activation [25–27]. Since we previously demonstrated that AR alters the phosphorylation state of GSK3β during I/R [14], here we investigated if AR modulates β-catenin activity and consequent activation of mesenchymal markers during IR in the heart. We used two distinct models to study whether AR affects myocardial β-catenin and consequent activation of mesenchymal markers during I/R: a transient occlusion and reperfusion of the left anterior descending coronary artery (LAD) in vivo model of I/R, and an ex vivo intact heart preparation subjected to I/R. We employed mice devoid of AR (Akr1b3 null mice) to determine whether altered flux via AR influences myocardial β-catenin during I/R. Our results indicate that genetic deletion of Akr1b3 drives acute induction of mesenchymal markers, at least in part via induction of the β-catenin pathway during I/R in the heart.
Results
Akr1b3 deletion reduces infarct size and improves functional recovery after I/R
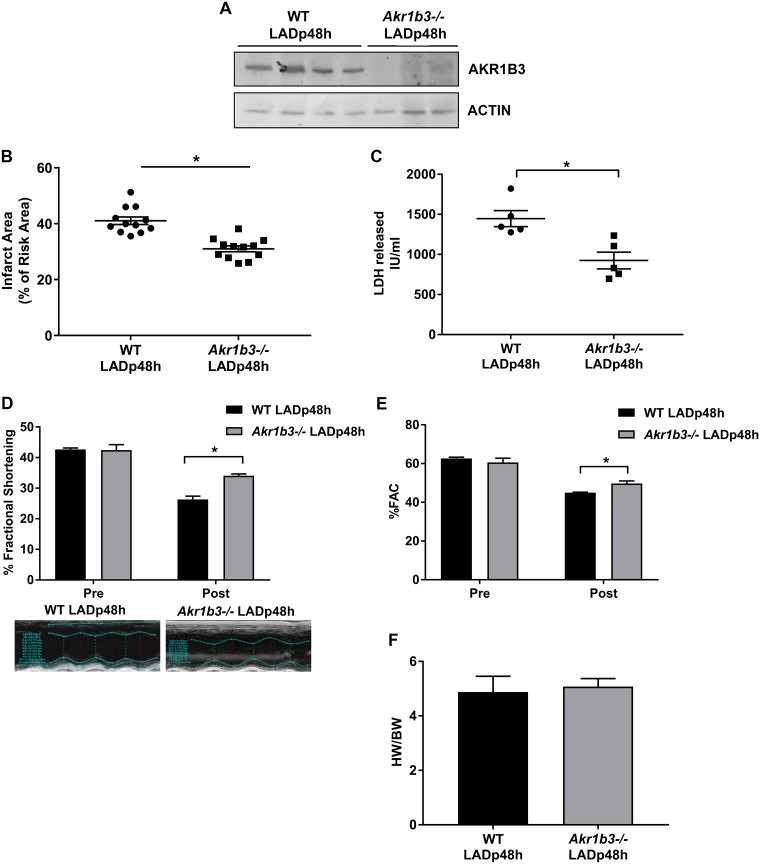
We subjected male WT and Akr1b3 null mice to left anterior descending coronary artery (LAD) occlusion for 30 min, followed by 48 hours of reperfusion (LADp48h). The expression or absence of AKR1B3 in WT and Akr1b3 null mice, respectively, was verified by Western blot (Fig 1A). Infarct size, as a percent of area at risk, measured at 48 h post I/R, was significantly lower in Akr1b3 null mice vs. WT mice (Fig 1B), but there were no differences in area at risk between the two genotypes (data not shown). Plasma LDH levels, a marker of myocardial injury, were significantly lower in mice devoid of Akr1b3 vs. WT mice at 48 h post I/R (Fig 1C). Echocardiographic measurements revealed significant differences in fractional shortening and fractional area change in Akr1b3 null mice compared to WT mice (Fig 1D and 1E). Cardiac hypertrophy, assessed by measuring the heart weight to body weight ratio, revealed no significant differences in Akr1b3 null vs WT mice hearts at 48 h post I/R (Fig 1F). Taken together, these results demonstrate improved functional recovery and reduced markers of injury in Akr1b3 null mice hearts compared to WT mice after I/R.
Fig 1. Cardioprotection in Akr1b3 null I/R mice.
Male WT and Akr1b3 null mice were subjected to LAD occlusion followed by reperfusion at age 4 months. (A) Western blot analysis of AKR1B3 in heart tissue lysate at 48 h post-LAD was performed and normalized to levels of B-ACTIN, N = 4 mice/genotype. (B) Akr1b3 null mice exhibit decreased infarct area (expressed as in % of infarct area/area at risk) after LAD/reperfusion vs. WT mice (n = 10/group; * p<0.05 vs. WT LAD) with no genotype differences in area at risk (data not shown). (C) Total plasma LDH levels were measured at 48 h post-LAD, N = 6 mice/group. (D) Changes in % fractional shortening (FS) with representative echocardiographic image. (E) % of fractional area change (FAC), N = 10/group. (F) The ratio of heart weight to body weight was measured, N = 10/group. Error bars represent mean ± SEM. * p<0.05, unless otherwise noted.
Upregulation of TGFB2 in Akr1b3 null mice hearts after I/R
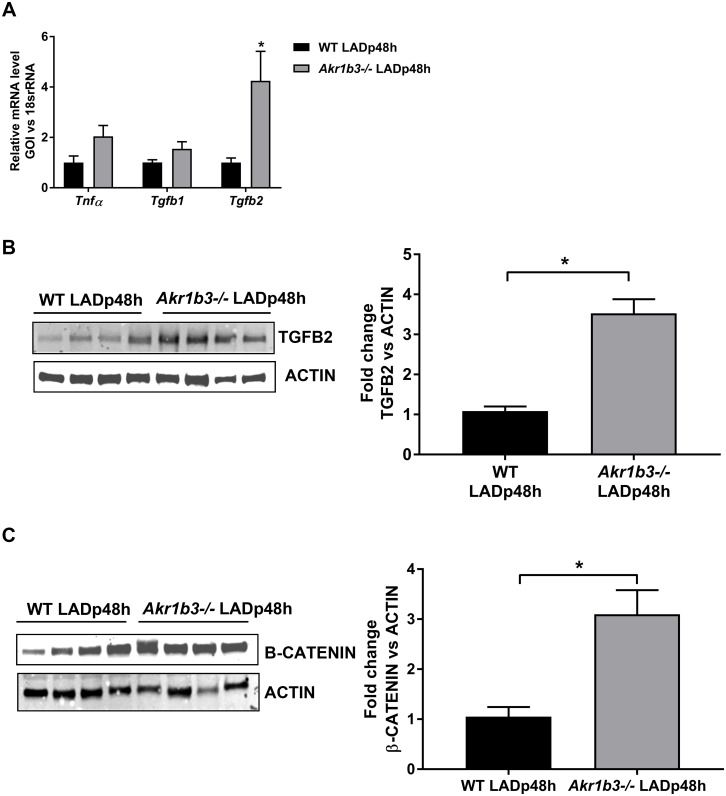
The early phase of recovery post-LAD ligation involves an inflammatory response with the release of cytokines. Hence, we quantified the expression of prominent cytokines involved in wound healing responses, including Tnfα, Tgfb1 and Tgfb2 via qRT-PCR [28, 29]. There were no differences in expression of Tnfa or Tgfb1 between the two mouse groups but we observed ≈4-fold higher Tgfb2 mRNA levels in Akr1b3 null vs. WT mice LADp48h mice (Fig 2A). Consistent with changes in mRNA levels, TGFB2 protein levels were upregulated by ≈3-fold in mice hearts devoid of Akr1b3 compared to WT mice (Fig 2B). Since studies have implicated TGFB2 in modulating β-catenin expression, we examined protein expression of β-catenin in WT and Akr1b3 null mice hearts [21, 30]. Western blot analysis of these heart tissues showed an ≈3-fold increase in β-catenin protein expression in Akr1b3 null mice vs. WT mice post-I/R (Fig 2C). These results indicate that deletion of Akr1b3 enhances TGFB2 and β-catenin expression after I/R in mice hearts.
Fig 2. Upregulation of TGFβ2/β-catenin in Akr1b3 null mice 48 h post-I/R.
(A) qRT-PCR on Tnfα, Tgfb1 and Tgfb2 transcripts from RNA isolated in the heart tissues, N = 5 mice/group. (B) Western blot of TGFB2 protein expression normalized to Beta-actin, N = 4 mice/group (C) Western blot of β-catenin protein expression normalized to Beta-actin, N = 4 mice/group. Error bars represent mean ± SEM. * p<0.05, unless otherwise noted.
Mesenchymal activation in mice hearts devoid of Akr1b3
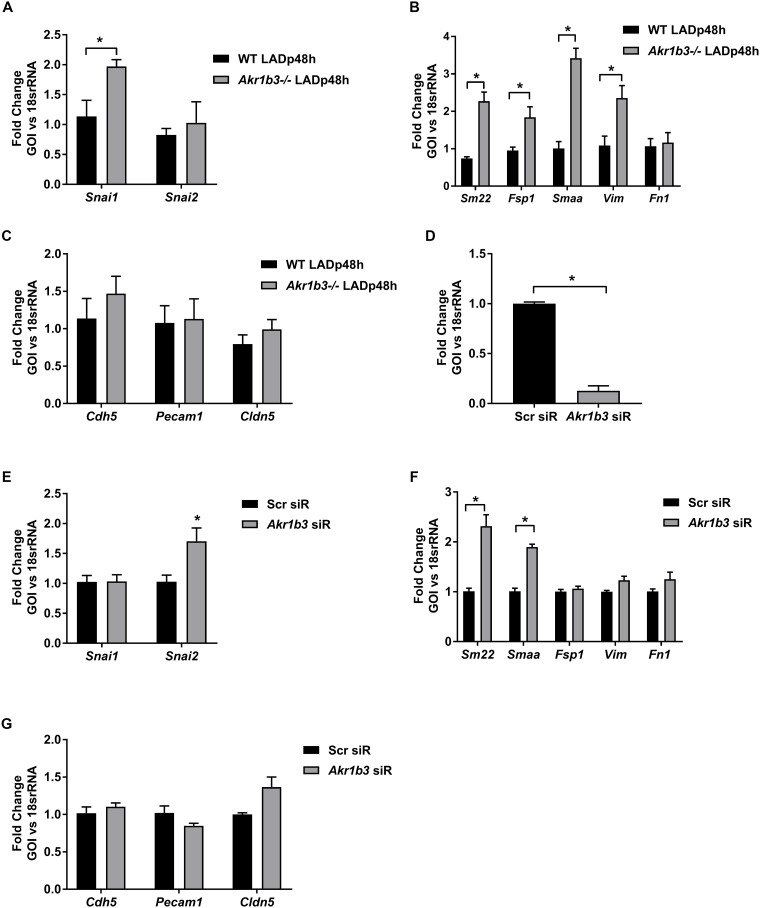
Loss of cardiomyocytes during ischemia is compensated for by the activation of existing fibroblasts or through the trans-differentiation of endothelial cells to mesenchymal cells via endothelial mesenchymal transition (EndMT) [31–33]. Several studies have implicated TGFB2 in the EndMT pathway [31–33]. Canonical Wnt signaling is involved in EndMT-mediated cardiac fibrosis and stabilized β-catenin serves as a marker for activated Wnt signaling [22, 31, 34]. Hence, we investigated whether the increase in TGFB2 and β-catenin observed in Ak1br3 null mice hearts (Fig 2A–2C) leads to EndMT transition.
EndMT is characterized by reduction of endothelial markers platelet/endothelial adhesion molecule (Pecam1, cadherin 5 (Cdh5) and claudin 5 (Cldn5), with concomitant activation of mesenchymal markers (α-smooth muscle actin (Smaa), Transgelin (Sm22), Vimentin (Vim), S100a4 (Fsp1) and fibronectin 1 (Fn1) and the related EndMT transcription factors (Snai1 and Snai2). Analysis of the transcription factors involved in EndMT, Snai1 and Snai2 revealed upregulation of Snai1, but not Snai2 in hearts devoid of Akr1b3 (Fig 3A). We observed increased expression of all mesenchymal markers, Smaa, Sm22, Vim and Fsp1, except Fn1 (Fig 3B) in Akr1b3 null hearts. Analysis of endothelial markers showed no differences in gene expression of Pecam1, Cdh5 and Cldn5 (Fig 3C). To confirm these results in vitro, we employed mouse primary aortic endothelial cells (MAEC), which were transfected with siRNA against Akr1b3 (Abr1b3 siR). Scrambled siRNA was used as a negative control (scr siR). 90% knockdown efficiency was achieved in these cells (Fig 3D). These cells were then subjected to 30 min of hypoxia followed by 1 h reperfusion (H/R). qRT-PCR analysis showed a significant increase in EndMT transcription factor Snai2 (Fig 3E), a significant increase in Smaa, but not in the other mesenchymal markers (Fig 3F) and no reduction in the endothelial markers (Fig 3G). Taken together, these results ruled out the possibility of classical EndMT processes, both in vitro and in vivo, yet distinct mesenchymal activation was observed in cells depleted of Akr1b3. Furthermore, increased expression of mesenchymal markers (Smaa, Sm22, Vim, Fsp1) suggested an activated fibroblast phenotype in endothelial cells derived from mice devoid of Akr1b3.
Fig 3. Mesenchymal activation in Akr1b3 null mice hearts 48 h post-I/R.
RNA isolated from heart tissues from mice subjected to I/R. (A) qRT-PCR on EndoMT transcription factors- Snai1 and Snai2. (B) qRT-PCR on mesenchymal markers as indicated. (C) qRT-PCR on endothelial markers as indicated. MAECs transfected with scrambled and siR against Akr1b3 and probed for (D) Akr1b3. € qRT-PCR on EndoMT transcription factors as indicated. (F) qRT-PCR on mesenchymal markers as indicated. (G) qRT-PCR on endothelial markers as indicated. N = 3 mice/group. Error bars represent mean ± SEM. * p<0.05, unless otherwise noted.
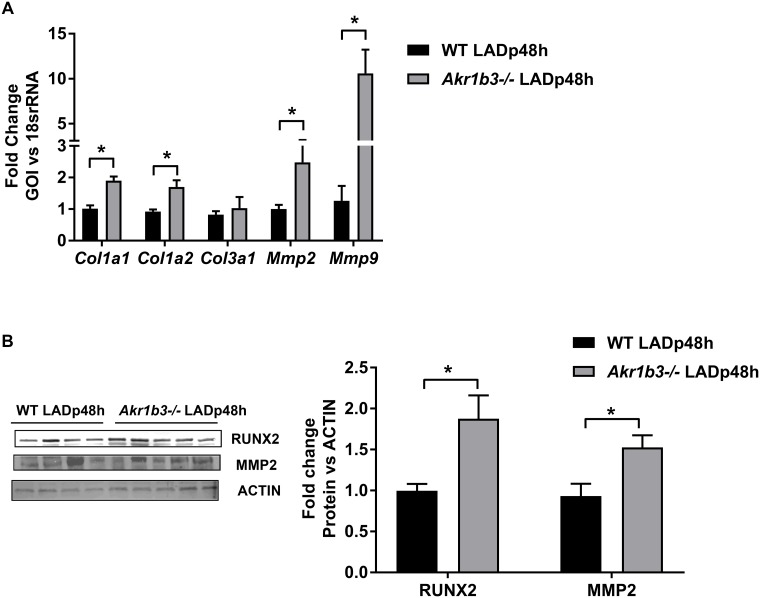
Induction of genes linked to fibrosis in hearts devoid of Akr1b3
Activated fibroblasts are the primary source of increased extracellular matrix, which contributes to tissue fibrosis [35, 36]. The extracellular matrix of myocardium is largely composed of structural proteins, type I and III collagens, which not only provide mechanical support but also force for contraction. The homeostasis of collagens is maintained by the delicate balance between their synthesis and degradation via matrix metalloproteinases (MMPs). The β- catenin pathway has been linked to induction of genes encoding collagens and MMPs [37–39]. We next examined if collagens and MMPs were altered in mice hearts devoid of Akr1b3 post- I/R. qRT-PCR analysis on Type I and III collagens (Col1a1, Col1a2, Col3a1) and MMPs (Mmp2 and Mmp9) revealed an increase in both types of collagens as well as MMPs in mice hearts devoid of Akr1b3 after I/R (Fig 4A). Further, we observed increases in RUNX2 and MMP2 protein expression in Akr1b3 null mice hearts (Fig 4B). These results suggest that in mice hearts devoid of Akr1b3, increased expression of collagens and MMPs may contribute to remodeling responses after I/R.
Fig 4. Increased expression of fibrotic factors in Akr1b3 null I/R mice hearts.
RNA isolated from heart tissues from mice subjected to I/R. (A) qRT-PCR on collagens (Col1a1, Col1a2, Col3a1) and MMPs (Mmp2 and Mmp9), N = 5 mice/group. (B) Western blot analysis on RUNX2 and MMP2 expression in heart tissues subjected to I/R. N = 4/group. Error bars represent mean ± SEM. * p<0.05, unless otherwise noted.
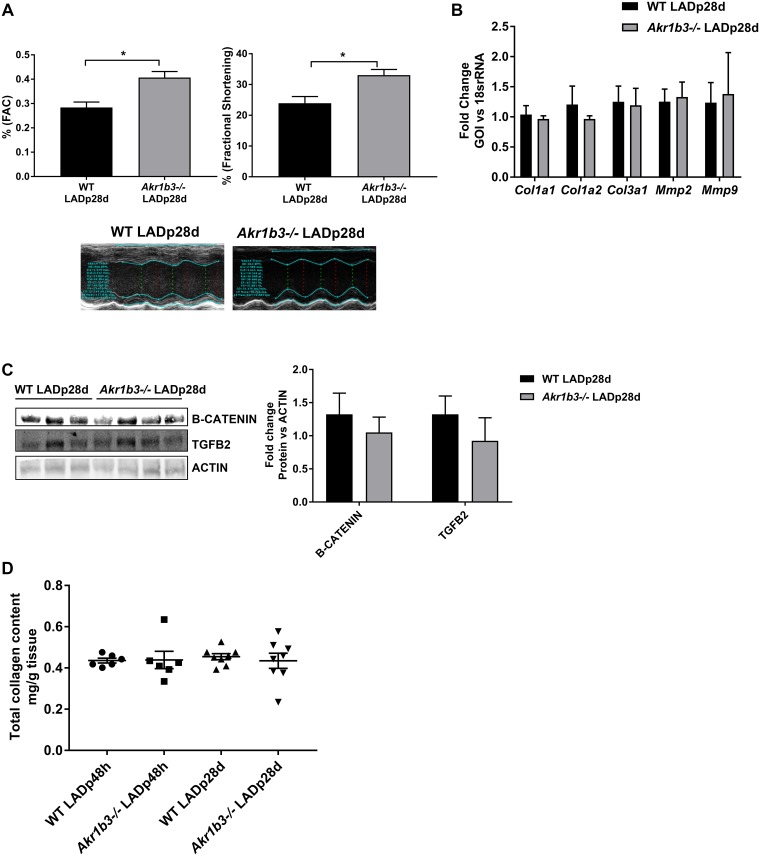
Lack of changes in fibrotic genes at 28 days post infarction
Post-infarction remodeling is a complex process in which cardiomyocyte loss is accompanied by cellular hypertrophy and fibrosis. Initially an adaptive response, extended cardiac fibrosis can lead to maladaptive remodeling and heart failure. Our results indicate that there was no evidence of hypertrophy in either WT or Akr1b3 null mice hearts, but that there was induction of genes linked to fibrotic remodeling in mice hearts devoid of Akr1b3. If ablation of Akr1b3 results in fibroblast activation and induction of genes linked to fibrotic remodeling, we sought to test whether this activation and induction persisted even after a month of infarction, without culminating in fibrosis. Hence we assessed echocardiographic measurements on WT and Akr1b3 null mice 28 days post-LAD occlusion/recovery. We found a significant increase in fractional shortening and fractional area change measurements in Akr1b3 null LAD mice compared to WT, which is consistent with overall superior cardiac function in the hearts devoid of Akr1b3 (Fig 5A). Further, RNA analysis on fibrotic marker expression failed to show any differences between WT and the Akr1b3 null mice on day 28 post-LAD (Fig 5B). Further, β-catenin and TGFB2 protein levels were comparable between both groups of mice at day 28 post-LAD (Fig 5C). We measured the total collagen levels in heart tissues 48 hrs and 28 days post LAD in both WT and mice devoid of Akr1b3 and found no significant differences in collagen levels (Fig 5D). Taken together, these results indicate that changes in β-catenin, TGFB2 and fibrotic markers were unique to early phase of recovery (48 hours) in Akr1b3 mice, and not sustained at the later phase of recovery (28 days).
Fig 5. Absence of changes in expression of fibrotic factors in Akr1b3 null I/R mice hearts after 28 days of recovery.
Mice were subjected to LAD and studies were done 28 days post infarction recovery. (A) Echocardiographic measurements made in WT and Akr1b3 null mice. Functional measurements, fractional shortening (FS) and fractional area change (FAC) are expressed as %, with representative image, N = 10 mice/group. (B) qRT-PCR on collagens (Col1a1, Col1a2, Col3a1) and MMPs (Mmp2 and Mmp9) from heart tissue, N = 5 mice/group. (C) Western blot from heart lysates for detection of β-catenin and TGFB2 normalized to Beta-Actin, N = 4 mice/group. (D) Total collagen levels in hearts from mice subjected to LAD post 48 h and 28 days of recovery, N = 4 mice/group. Error bars represent mean ± SEM. * p<0.05, unless otherwise noted.
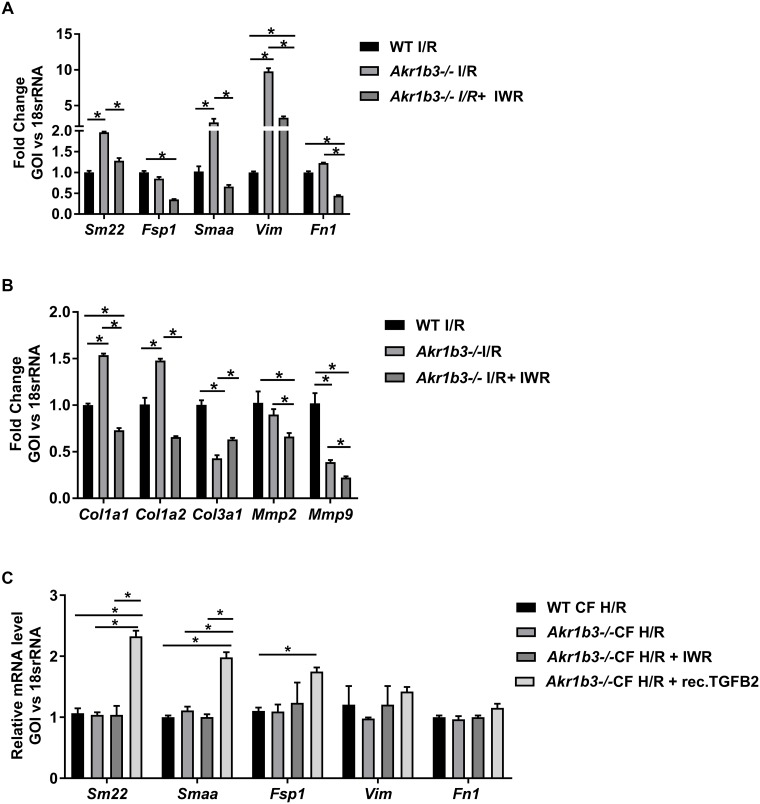
β-catenin inhibition ablates the beneficial effects of deletion of Akr1b3 on expression of mesenchymal markers in the heart in I/R
To confirm the mesenchymal activation observed in mice devoid of Akr1b3 was due to enhanced β-catenin levels, we employed IWR-endo, an inhibitor of Wnt-β catenin pathway [40]. Using an ex-vivo isolated perfused heart for model of I/R, Akr1b3 null mice hearts were treated with either vehicle or IWR-endo during the 30 min of ischemia and 60 min of reperfusion. qRT-PCR analysis from the RNA extracted from heart tissues revealed that IWR-endo treatment reduced the expression of mesenchymal and fibrotic markers after I/R in these mice hearts when compared to the vehicle treatment (Fig 6A and 6B). Further, to determine if cardiac fibroblasts (CF) at key site for the observed mesenchymal markers changes, primary CF were isolated from WT and Akr1b3 null mice and subjected to H/R in the presence of recombinant TGFB2 protein. Treatment of IWR in CFs was used to establish the link to β-catenin. Data presented in Fig 6C shows no significant changes in mesenchymal markers in WT and Akr1b3-/- CF, while treatment with TGFB2 protein upregulated the mesenchymal markers. IWR treatment did not lead to activation of mesenchymal markers in WT and Akr1b3-/- CFs (Fig 6C). These results reveal that mesenchymal activation in Akr1b3-/-, is in part, via TGFB2 in CFs.
Fig 6. β-Catenin pathway inhibitor reverses the Akr1b3 null mediated protection and mesenchymal marker expression.
Mice hearts were subjected to ex vivo I/R using Langendorff technique. (A) qRT-PCR on heart tissues for mesenchymal markers as indicated, N = 3. (B) qRT-PCR on heart tissues for collagen and matrix metalloproteinases as indicated, N = 3 mice/group. (C) qRT-PCR on primary CF for mesenchymal markers treated either with recombinant TGFB2 or IWR as indicated, N = 5/group. Error bars represent mean ± SEM. * p<0.05, unless otherwise noted.
Discussion
Post infarct remodeling in the heart is a complex process, where I/R-associated necrosis and apoptosis of cardiomyocytes is compensated by processes such as cardiomyocyte hypertrophy, transdifferentiation of endothelial to mesenchymal cells (EndMT) and fibroblast activation. Akr1b3 null mice failed to show any hypertrophy. Our studies revealed that enhanced β-catenin signaling at an early time point of reperfusion in mice devoid of Akr1b3 was beneficial to hearts that had been subjected to I/R. The increased TGFB2 and β-catenin protein suggested the EndMT pathway as a potential mechanism. However, this possibility was ruled out as endothelial markers were not downregulated.
Akr1b3 null mice hearts displayed enhanced expression of mesenchymal markers, suggestive of fibroblast activation. Several studies had suggested the role of β-catenin in fibrosis and mesenchymal activation as a key driver of wound healing [41–44]. Published studies have shown that I/R can induce formation of epicardium-derived cells, which then differentiate into mesenchymal cells expressing fibroblast and smooth muscle cell markers [45, 46]. Consistent with these findings, our data show that the mesenchymal markers are upregulated during I/R in the Akr1b3 null hearts and that these increases require β-catenin.
Activation of β-catenin in the mice hearts devoid of Akr1b3 during I/R in our study could be attributed to either TGFB2 or GSK3B phosphorylation or both. Studies have shown that activation of β-catenin could be due, in part, to phosphorylation of GSK3β. The phosphorylation of GSK3β by p-Akt destabilizes GSK3β complex, resulting in the dissociation of β-catenin from the GSK3β complex. This process leads to nuclear translocation of β-catenin [26, 47]. Earlier studies in rats have shown that the cardioprotection afforded by phyllanthus emblica was linked to increasing levels of p-Akt and β-catenin, as well as increased GSK3β phosphorylation [25, 27, 48]. Since our earlier studies demonstrated reduced Tyr216 GSK3β phosphorylation during I/R in Akr1b3-/- hearts compared to WT hearts (14), here we focused on the role of TGFB2. Since TGFB2 has been implicated in β-catenin activation and cellular plasticity [21, 30], it is conceivable that activation of β-catenin in hearts devoid of Akr1b3 could also be due to increases in TGFB2. Our studies in cardiac fibroblasts from WT and Akr1b3 null mice subjected to H/R revealed only modest activation of mesenchymal markers in the presence of TGFB2, indicating other mechanisms are also contributing to mesenchymal activation. Specifically, in addition to TGFB2, secreted factors from other cells in heart may play an important role in activation of mesenchymal markers in our study.
The impact of mesenchymal activation on cardiac remodeling post infarction may, in part, explain reduced I/R injury in Akr1b3-/- hearts. Repair mechanisms to manage tissue scaring are essential for viable recovery after I/R. We believe β-catenin related changes may be of help in reducing the tissue scar through mesenchymal activation. In our studies we show that CF activation results in upregulation of both matrix metalloproteinases and collagens in Akr1b3-/- hearts, key players that facilitate removal and replacement of necrotic tissue. Hence we posit, in Akr1b3-/- mice, TGFB2 mediated mesenchymal activation may aid in the clearance of necrotic tissue thereby reducing injury.
MMPs are involved in physiological as well as pathological processes, such as inflammation, tumor metastasis and tissue remodeling [49]. Several studies have shown that activated MMPs mediate injury to contractile apparatus as well as that they affect the structural proteins within the intra- and extracellular matrix lattices [50–52]. Hence, inhibition of MMPs is considered as a therapeutic strategy to improve functional recovery in the heart after I/R [53]. Though isoform-specific Mmp knockout (global) mice showed cardioprotection, inhibitor studies as well as macrophage-specific MMP9 overexpression studies contradicted the earlier observations [54, 55]. Such studies underscore the complexity and cell type-specificity of MMP actions, both in development and in I/R in the adult heart. In this context, our studies demonstrated acute increases in Mmp2, Mmp9, as well as collagenases, without increases in the total collagen content in the mice hearts devoid of Akr1b3 in I/R. Hence our findings on MMP changes are those in line with macrophage specific MMP9 overexpression mice and MMP9 inhibitor studies [54, 55].
Several studies point out the importance of prolonged structural alteration resulting in fibrosis and heart failure. TGFB2 and β-catenin mediated changes in our studies are likely related to acute structural alterations. Studies in the literature are mixed in regard to the role of TGFB in I/R hearts, with some studies showing the detrimental effects of TGFB and others showing cardioprotective effects of TGFB during I/R. [56–60] Likewise, studies in β-catenin were also contradictory, regarding its role in I/R hearts. Nevertheless, several studies have underscored the importance of β-catenin activation in reducing I/R injury either by reducing oxidative stress or apoptosis [41–44]. We observed that the cardioprotective effects in Akr1b3 null mice in acute (48 hours) as well as extended periods of recovery (28 days) was linked to β-catenin changes. Our study identifies that β-catenin-mediated mesenchymal activation is linked to reduced myocardial I/R injury and that this pathway is downstream of the AKR1B3 pathway. In myocardial I/R, deletion of Akr1b3 modulates the myocardial β-catenin pathway and consequent induction of mesenchymal markers as well as genes linked to fibrotic remodeling, thereby highlighting inhibition of the AKR1B3 pathway as a key strategy in protection against myocardial injury after infarction.
Materials and methods
Animals used
All animal experimentations were performed with the approval of the Institutional Animal Care and Use Committee at New York University School of Medicine. Male Akr1b3 null mice- and wild type littermate mice were used as described earlier [8, 61]. Surgical procedures related to coronary artery ligation (LAD) were performed as previously described [8]. Briefly male mice aged approximately 4 months of age were anesthetized and subjected to LAD/reperfusion. LAD was ligated for 30 min and then blood flow was restored. Mice were allowed to recover and measurements were made after 48 h or 28 days of recovery. For functional measurements, mice were anesthetized with isoflurane via a nose cone and 2-dimensional echocardiography was performed on a Vevo 2100 System (Visual Sonics, Ontario, Canada). The left ventricular end-diastolic and end-systolic dimensions were measured and percent fractional shortening was calculated. Echocardiographic measurements were made before the surgery and after 48 h or 28 days of recovery. Age and sex matched controls were used. Cohort of hearts were used to assess area at risk and infarct area by 2,3,5-triphenyl-2H-tetrazolium chloride and Evan’s blue staining as published earlier [62, 63].
Ex-vivo I/R
Experiments were carried out as described earlier [8, 15]. Briefly, mice were anesthetized using ketamine/xylazine. The hearts were rapidly excised and perfused through the aorta in a non-recirculating mode, using an isovolumic perfusion system through Langerndorff technique (LT) with Krebs-Henseleit buffer. Perfusion pO2>600 mm Hg was maintained in the oxygenation buffer. IWR-endo was added at 10μM final concentration to the buffer, whereas DMSO was added for vehicle control. Hearts were perfused with IWR or vehicle starting at 10 min prior to initiation of ischemia for 30 min and continued throughout 60 min of reperfusion.
Lactate dehydrogenase (LDH) levels in plasma (in vivo) and effluents (ex vivo) were measured using a commercially available kit (Pointe Scientific, Canton, MI).
Cell culture
For transfection in mouse aortic endothelial cells, siRNA specific against Akr1b3 was obtained from Life Technologies and were transfected using electroporation kit obtained from Lonza. 48 h post transfection experiments were conducted. For H/R experiment, cells were placed in a hypoxia chamber (Biospherix, Lacona, NY) for 30 min of hypoxia (0.5% O2, 5% CO2) at 37°C followed by 60 min of reoxygenation in 5% CO2 incubator (hypoxia/reoxygenation, H/R). Cells were collected at the end of reoxygenation in ice cold PBS for further analysis.
Primary cardiac fibroblast isolation
Murine primary cardiac fibroblasts were isolated using the protocol mentioned [64]. Briefly, mince the hearts in ice-cold PBS into a size of 1mm using scalpel. The minced tissue was digested using digestion buffer (100U/ml collagenase II, 0.1% trypsin in HBSS buffer). Cells isolated were then plated in fibroblast medium (DMEM/F12, 10%FBS, 100U/ml Pen-Strep, 1X Glutamine, 100uM Ascorbic acid). Recombinant TGFB2 was purchased from R &D systems and used at a concentration of 10ng/ml.
Collagen measurements
Total collagen levels from heart tissues subjected to LAD post 48hrs and 28 days were measured using total collagen assay kit (Biovison). Briefly, tissues were homogenized in concentrated HCl and hydrolyzed at 120°C for 3 h. Hydrolyzed sample were vacuum evaporated and subjected to quantification as per manufacturer‘s protocol.
Western blot analysis
Total lysates from heart tissues or cells were prepared using lysis buffer (Cell Signaling). Tissues/cells were crushed using beads for homogenization and were quantified. For the detection of the protein following antibodies were used β-catenin, RUNX2 (cell signaling), TGFB2 (Santacruz), MMP2 (abcam), β-ACTIN (sigma) and ARKR1B3 (GeneTex). Antibodies were used at a final concentration of 1μg/ml.
Realtime PCR
cDNA was prepared from whole heart tissues or cells using RNAeasy isolation kit (Qiagen). cDNA was prepared using iScript cDNA synthesis kit (BioRad). Fast sybrgreen mastermix and Taqman probes were used for quantification and data were normalized using 18s rRNA. Details of the primers used are in S1 Table.
Statistics
All values are presented as the mean ± standard error of the mean. Data were analyzed by unpaired two-tailed t-tests to assess the difference between groups as specified. A probability value of ≤ 0.05 was considered significant.
Supporting information
(PDF)
Acknowledgments
This work was supported in part by grants from NIH—HL60901 (RR & AMS), and AG026467 (RR & AMS), and the Harry B & Aileen B. Gordon Foundation (KHG), and the Agar Corporation (KHG). We acknowledge Ms. Latoya Woods for her assistance in the preparation of the manuscript.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This work was supported in part by grants from NIH - HL60901 (RR & AMS), and AG026467 (RR & AMS), and the Harry B & Aileen B. Gordon Foundation (KHG), and the Agar Corporation (KHG). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015;131(4):e29–322. doi: 10.1161/CIR.0000000000000152 [DOI] [PubMed] [Google Scholar]
- 2.Gerczuk PZ, Kloner RA. An update on cardioprotection: a review of the latest adjunctive therapies to limit myocardial infarction size in clinical trials. J Am Coll Cardiol. 2012;59(11):969–78. doi: 10.1016/j.jacc.2011.07.054 [DOI] [PubMed] [Google Scholar]
- 3.Buja LM. Myocardial ischemia and reperfusion injury. Cardiovasc Pathol. 2005;14(4):170–5. doi: 10.1016/j.carpath.2005.03.006 [DOI] [PubMed] [Google Scholar]
- 4.Inoue T. Ischemia-reperfusion injury is still a big hurdle to overcome for treatment of acute myocardial infarction. J Cardiol. 2016;67(4):305–6. doi: 10.1016/j.jjcc.2015.09.002 [DOI] [PubMed] [Google Scholar]
- 5.Murphy E, Steenbergen C. Mechanisms underlying acute protection from cardiac ischemia-reperfusion injury. Physiol Rev. 2008;88(2):581–609. doi: 10.1152/physrev.00024.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Camici P, Ferrannini E, Opie LH. Myocardial metabolism in ischemic heart disease: basic principles and application to imaging by positron emission tomography. Prog Cardiovasc Dis. 1989;32(3):217–38. [DOI] [PubMed] [Google Scholar]
- 7.Lopaschuk GD, Wall SR, Olley PM, Davies NJ. Etomoxir, a carnitine palmitoyltransferase I inhibitor, protects hearts from fatty acid-induced ischemic injury independent of changes in long chain acylcarnitine. Circ Res. 1988;63(6):1036–43. [DOI] [PubMed] [Google Scholar]
- 8.Hwang YC, Kaneko M, Bakr S, Liao H, Lu Y, Lewis ER, et al. Central role for aldose reductase pathway in myocardial ischemic injury. FASEB J. 2004;18(11):1192–9. doi: 10.1096/fj.03-1400com [DOI] [PubMed] [Google Scholar]
- 9.Hwang YC, Shaw S, Kaneko M, Redd H, Marrero MB, Ramasamy R. Aldose reductase pathway mediates JAK-STAT signaling: a novel axis in myocardial ischemic injury. FASEB J. 2005;19(7):795–7. doi: 10.1096/fj.04-2780fje [DOI] [PubMed] [Google Scholar]
- 10.Nishimura C, Hamada Y, Tachikawa T, Ishikawa T, Gui T, Tsubouchi J, et al. Enzyme immunoassay for erythrocyte aldose reductase. Clin Chem. 1994;40(6):889–94. [PubMed] [Google Scholar]
- 11.Ramasamy R, Liu H, Oates PJ, Schaefer S. Attenuation of ischemia induced increases in sodium and calcium by the aldose reductase inhibitor zopolrestat. Cardiovasc Res. 1999;42(1):130–9. [DOI] [PubMed] [Google Scholar]
- 12.Ramasamy R, Oates PJ, Schaefer S. Aldose reductase inhibition protects diabetic and nondiabetic rat hearts from ischemic injury. Diabetes. 1997;46(2):292–300. [DOI] [PubMed] [Google Scholar]
- 13.Tracey WR, Magee WP, Ellery CA, MacAndrew JT, Smith AH, Knight DR, et al. Aldose reductase inhibition alone or combined with an adenosine A(3) agonist reduces ischemic myocardial injury. Am J Physiol Heart Circ Physiol. 2000;279(4):H1447–52. [DOI] [PubMed] [Google Scholar]
- 14.Abdillahi M, Ananthakrishnan R, Vedantham S, Shang L, Zhu Z, Rosario R, et al. Aldose reductase modulates cardiac glycogen synthase kinase-3beta phosphorylation during ischemia-reperfusion. Am J Physiol Heart Circ Physiol. 2012;303(3):H297–308. doi: 10.1152/ajpheart.00999.2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Son NH, Ananthakrishnan R, Yu S, Khan RS, Jiang H, Ji R, et al. Cardiomyocyte aldose reductase causes heart failure and impairs recovery from ischemia. PLoS One. 2012;7(9):e46549 doi: 10.1371/journal.pone.0046549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Calderone V, Testai L, Martelli A, La Motta C, Sartini S, Da Settimo F, et al. Anti-ischaemic activity of an antioxidant aldose reductase inhibitor on diabetic and non-diabetic rat hearts. J Pharm Pharmacol. 2010;62(1):107–13. doi: 10.1211/jpp.62.01.0012 [DOI] [PubMed] [Google Scholar]
- 17.Iwata K, Matsuno K, Nishinaka T, Persson C, Yabe-Nishimura C. Aldose reductase inhibitors improve myocardial reperfusion injury in mice by a dual mechanism. J Pharmacol Sci. 2006;102(1):37–46. [DOI] [PubMed] [Google Scholar]
- 18.MacDonald BT, Tamai K, He X. Wnt/beta-catenin signaling: components, mechanisms, and diseases. Dev Cell. 2009;17(1):9–26. doi: 10.1016/j.devcel.2009.06.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moon RT, Bowerman B, Boutros M, Perrimon N. The promise and perils of Wnt signaling through beta-catenin. Science. 2002;296(5573):1644–6. doi: 10.1126/science.1071549 [DOI] [PubMed] [Google Scholar]
- 20.Cadigan KM, Liu YI. Wnt signaling: complexity at the surface. J Cell Sci. 2006;119(Pt 3):395–402. doi: 10.1242/jcs.02826 [DOI] [PubMed] [Google Scholar]
- 21.Willert K, Nusse R. Beta-catenin: a key mediator of Wnt signaling. Curr Opin Genet Dev. 1998;8(1):95–102. [DOI] [PubMed] [Google Scholar]
- 22.Duan J, Gherghe C, Liu D, Hamlett E, Srikantha L, Rodgers L, et al. Wnt1/βcatenin injury response activates the epicardium and cardiac fibroblasts to promote cardiac repair. The EMBO journal. 2012;31(2):429–42. doi: 10.1038/emboj.2011.418 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lehwald N, Tao GZ, Jang KY, Sorkin M, Knoefel WT, Sylvester KG. Wnt–β-catenin signaling protects against hepatic ischemia and reperfusion injury in mice. Gastroenterology. 2011;141(2):707–18. e5 doi: 10.1053/j.gastro.2011.04.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou L, Li Y, Zhou D, Tan RJ, Liu Y. Loss of Klotho contributes to kidney injury by derepression of Wnt/β-catenin signaling. Journal of the American Society of Nephrology. 2013;24(5):771–85. doi: 10.1681/ASN.2012080865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Juhaszova M, Zorov DB, Yaniv Y, Nuss HB, Wang S, Sollott SJ. Role of glycogen synthase kinase-3beta in cardioprotection. Circ Res. 2009;104(11):1240–52. doi: 10.1161/CIRCRESAHA.109.197996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thirunavukkarasu M, Han Z, Zhan L, Penumathsa SV, Menon VP, Maulik N. Adeno-sh-beta-catenin abolishes ischemic preconditioning-mediated cardioprotection by downregulation of its target genes VEGF, Bcl-2, and survivin in ischemic rat myocardium. Antioxid Redox Signal. 2008;10(8):1475–84. doi: 10.1089/ars.2008.2042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Thirunavukkarasu M, Selvaraju V, Tapias L, Sanchez JA, Palesty JA, Maulik N. Protective effects of Phyllanthus emblica against myocardial ischemia-reperfusion injury: the role of PI3-kinase/glycogen synthase kinase 3beta/beta-catenin pathway. J Physiol Biochem. 2015;71(4):623–33. doi: 10.1007/s13105-015-0426-8 [DOI] [PubMed] [Google Scholar]
- 28.Sautner T, Fugger R, Gotzinger P, Mittlbock M, Winkler S, Roth E, et al. Tumour necrosis factor-alpha and interleukin-6: early indicators of bacterial infection after human orthotopic liver transplantation. Eur J Surg. 1995;161(2):97–101. [PubMed] [Google Scholar]
- 29.Yoshimoto T. [The expression of ICAM-1 and cytokines in the reperfusional state]. Hokkaido Igaku Zasshi. 1997;72(1):97–112. [PubMed] [Google Scholar]
- 30.Lim S, Becker A, Zimmer A, Lu J, Buettner R, Kirfel J. SNAI1-mediated epithelial-mesenchymal transition confers chemoresistance and cellular plasticity by regulating genes involved in cell death and stem cell maintenance. PLoS One. 2013;8(6):e66558 doi: 10.1371/journal.pone.0066558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chrobak I, Lenna S, Stawski L, Trojanowska M. Interferon-gamma promotes vascular remodeling in human microvascular endothelial cells by upregulating endothelin (ET)-1 and transforming growth factor (TGF) beta2. J Cell Physiol. 2013;228(8):1774–83. doi: 10.1002/jcp.24337 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nie L, Lyros O, Medda R, Jovanovic N, Schmidt JL, Otterson MF, et al. Endothelial-mesenchymal transition in normal human esophageal endothelial cells cocultured with esophageal adenocarcinoma cells: role of IL-1beta and TGF-beta2. Am J Physiol Cell Physiol. 2014;307(9):C859–77. doi: 10.1152/ajpcell.00081.2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Paruchuri S, Yang JH, Aikawa E, Melero-Martin JM, Khan ZA, Loukogeorgakis S, et al. Human pulmonary valve progenitor cells exhibit endothelial/mesenchymal plasticity in response to vascular endothelial growth factor-A and transforming growth factor-beta2. Circ Res. 2006;99(8):861–9. doi: 10.1161/01.RES.0000245188.41002.2c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ye B, Ge Y, Perens G, Hong L, Xu H, Fishbein MC, et al. Canonical Wnt/beta-catenin signaling in epicardial fibrosis of failed pediatric heart allografts with diastolic dysfunction. Cardiovasc Pathol. 2013;22(1):54–7. doi: 10.1016/j.carpath.2012.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kisseleva T, Brenner DA. Hepatic stellate cells and the reversal of fibrosis. J Gastroenterol Hepatol. 2006;21 Suppl 3:S84–7. doi: 10.1111/j.1440-1746.2006.04584.x [DOI] [PubMed] [Google Scholar]
- 36.Scholten D, Reichart D, Paik YH, Lindert J, Bhattacharya J, Glass CK, et al. Migration of fibrocytes in fibrogenic liver injury. Am J Pathol. 2011;179(1):189–98. doi: 10.1016/j.ajpath.2011.03.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Distler A, Deloch L, Huang J, Dees C, Lin NY, Palumbo-Zerr K, et al. Inactivation of tankyrases reduces experimental fibrosis by inhibiting canonical Wnt signalling. Ann Rheum Dis. 2013;72(9):1575–80. doi: 10.1136/annrheumdis-2012-202275 [DOI] [PubMed] [Google Scholar]
- 38.Liu P, Yang J, Pei J, Pei D, Wilson MJ. Regulation of MT1-MMP activity by beta-catenin in MDCK non-cancer and HT1080 cancer cells. J Cell Physiol. 2010;225(3):810–21. doi: 10.1002/jcp.22292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhou S, Mizuno S, Glowacki J. Wnt pathway regulation by demineralized bone is approximated by both BMP-2 and TGF-beta1 signaling. J Orthop Res. 2013;31(4):554–60. doi: 10.1002/jor.22244 [DOI] [PubMed] [Google Scholar]
- 40.Lee SC, Kim OH, Lee SK, Kim SJ. IWR-1 inhibits epithelial-mesenchymal transition of colorectal cancer cells through suppressing Wnt/beta-catenin signaling as well as survivin expression. Oncotarget. 2015;6(29):27146–59. doi: 10.18632/oncotarget.4354 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chilosi M, Poletti V, Zamo A, Lestani M, Montagna L, Piccoli P, et al. Aberrant Wnt/beta-catenin pathway activation in idiopathic pulmonary fibrosis. Am J Pathol. 2003;162(5):1495–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Douglas IS, Diaz del Valle F, Winn RA, Voelkel NF. Beta-catenin in the fibroproliferative response to acute lung injury. Am J Respir Cell Mol Biol. 2006;34(3):274–85. doi: 10.1165/rcmb.2005-0277OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hu BL, Shi C, Lei RE, Lu DH, Luo W, Qin SY, et al. Interleukin-22 ameliorates liver fibrosis through miR-200a/beta-catenin. Sci Rep. 2016;6:36436 doi: 10.1038/srep36436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shaikh G, Zhang J, Perez-Aso M, Mediero A, Cronstein B. Adenosine A2A receptor promotes collagen type III synthesis via beta-catenin activation in human dermal fibroblasts. Br J Pharmacol. 2016. doi: 10.1111/bph.13615 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ruiz-Villalba A, Simon AM, Pogontke C, Castillo MI, Abizanda G, Pelacho B, et al. Interacting resident epicardium-derived fibroblasts and recruited bone marrow cells form myocardial infarction scar. J Am Coll Cardiol. 2015;65(19):2057–66. doi: 10.1016/j.jacc.2015.03.520 [DOI] [PubMed] [Google Scholar]
- 46.Zhou B, Honor LB, He H, Ma Q, Oh JH, Butterfield C, et al. Adult mouse epicardium modulates myocardial injury by secreting paracrine factors. J Clin Invest. 2011;121(5):1894–904. doi: 10.1172/JCI45529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Adluri RS, Thirunavukkarasu M, Zhan L, Akita Y, Samuel SM, Otani H, et al. Thioredoxin 1 enhances neovascularization and reduces ventricular remodeling during chronic myocardial infarction: a study using thioredoxin 1 transgenic mice. J Mol Cell Cardiol. 2011;50(1):239–47. doi: 10.1016/j.yjmcc.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Warboys CM, Chen N, Zhang Q, Shaifta Y, Vanderslott G, Passacquale G, et al. Bidirectional cross-regulation between the endothelial nitric oxide synthase and beta-catenin signalling pathways. Cardiovasc Res. 2014;104(1):116–26. doi: 10.1093/cvr/cvu173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Chen Q, Jin M, Yang F, Zhu J, Xiao Q, Zhang L. Matrix metalloproteinases: inflammatory regulators of cell behaviors in vascular formation and remodeling. Mediators Inflamm. 2013;2013:928315 doi: 10.1155/2013/928315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Ducharme A, Frantz S, Aikawa M, Rabkin E, Lindsey M, Rohde LE, et al. Targeted deletion of matrix metalloproteinase-9 attenuates left ventricular enlargement and collagen accumulation after experimental myocardial infarction. J Clin Invest. 2000;106(1):55–62. doi: 10.1172/JCI8768 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jacob-Ferreira AL, Schulz R. Activation of intracellular matrix metalloproteinase-2 by reactive oxygen-nitrogen species: Consequences and therapeutic strategies in the heart. Arch Biochem Biophys. 2013;540(1–2):82–93. doi: 10.1016/j.abb.2013.09.019 [DOI] [PubMed] [Google Scholar]
- 52.Lindsey ML, Escobar GP, Dobrucki LW, Goshorn DK, Bouges S, Mingoia JT, et al. Matrix metalloproteinase-9 gene deletion facilitates angiogenesis after myocardial infarction. Am J Physiol Heart Circ Physiol. 2006;290(1):H232–9. doi: 10.1152/ajpheart.00457.2005 [DOI] [PubMed] [Google Scholar]
- 53.DeCoux A, Lindsey ML, Villarreal F, Garcia RA, Schulz R. Myocardial matrix metalloproteinase-2: inside out and upside down. J Mol Cell Cardiol. 2014;77:64–72. doi: 10.1016/j.yjmcc.2014.09.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Iyer RP, de Castro Bras LE, Patterson NL, Bhowmick M, Flynn ER, Asher M, et al. Early matrix metalloproteinase-9 inhibition post-myocardial infarction worsens cardiac dysfunction by delaying inflammation resolution. J Mol Cell Cardiol. 2016;100:109–17. doi: 10.1016/j.yjmcc.2016.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zamilpa R, Ibarra J, de Castro Bras LE, Ramirez TA, Nguyen N, Halade GV, et al. Transgenic overexpression of matrix metalloproteinase-9 in macrophages attenuates the inflammatory response and improves left ventricular function post-myocardial infarction. J Mol Cell Cardiol. 2012;53(5):599–608. doi: 10.1016/j.yjmcc.2012.07.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Euler G. Good and bad sides of TGFbeta-signaling in myocardial infarction. Front Physiol. 2015;6:66 doi: 10.3389/fphys.2015.00066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Fujiu K, Nagai R. Fibroblast-mediated pathways in cardiac hypertrophy. J Mol Cell Cardiol. 2014;70:64–73. doi: 10.1016/j.yjmcc.2014.01.013 [DOI] [PubMed] [Google Scholar]
- 58.Kehat I, Molkentin JD. Molecular pathways underlying cardiac remodeling during pathophysiological stimulation. Circulation. 2010;122(25):2727–35. doi: 10.1161/CIRCULATIONAHA.110.942268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Leask A. Getting to the heart of the matter: new insights into cardiac fibrosis. Circ Res. 2015;116(7):1269–76. doi: 10.1161/CIRCRESAHA.116.305381 [DOI] [PubMed] [Google Scholar]
- 60.Travers JG, Kamal FA, Robbins J, Yutzey KE, Blaxall BC. Cardiac Fibrosis: The Fibroblast Awakens. Circ Res. 2016;118(6):1021–40. doi: 10.1161/CIRCRESAHA.115.306565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Gabbay KH, Bohren KM, Morello R, Bertin T, Liu J, Vogel P. Ascorbate synthesis pathway: dual role of ascorbate in bone homeostasis. J Biol Chem. 2010;285(25):19510–20. doi: 10.1074/jbc.M110.110247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Aleshin A, Ananthakrishnan R, Li Q, Rosario R, Lu Y, Qu W, et al. RAGE modulates myocardial injury consequent to LAD infarction via impact on JNK and STAT signaling in a murine model. Am J Physiol Heart Circ Physiol. 2008;294(4):H1823–32. doi: 10.1152/ajpheart.01210.2007 [DOI] [PubMed] [Google Scholar]
- 63.Ananthakrishnan R, Li Q, O’Shea KM, Quadri N, Wang L, Abuchowski A, et al. Carbon monoxide form of PEGylated hemoglobin protects myocardium against ischemia/reperfusion injury in diabetic and normal mice. Artif Cells Nanomed Biotechnol. 2013;41(6):428–36. doi: 10.3109/21691401.2012.762370 [DOI] [PubMed] [Google Scholar]
- 64.Xin Y, Liu S, Xu XF, Li WB, Huang YM, Luo Y, et al. [Primary culture and biological characteristics of cardiac fibroblasts of adult mice]. Xi Bao Yu Fen Zi Mian Yi Xue Za Zhi. 2012;28(11):1194–9. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.