Abstract
The aim of the study is to identify associations between dental anxiety and postoperative pain in patients undergoing extraction of horizontally impacted wisdom teeth.
A total of 119 volunteers provided demographic data, and completed questionnaires, the State-Trait Anxiety Inventory (STAI), Chinese Index of Dental Anxiety and Fear (C-IDAF)-4C, and the Numeric Rating Scale (NRS) for pain.
Mean SAI, TAI, and C-IDAF-4C scores were 42.5 ± 8.7, 46.4 ± 10.9, and 16.9 ± 7.2, respectively. Mean postoperative pain level score was 3.0 ± 1.8 (range: 0.3–8.4). SAI scores increased as preoperative pain levels increased (β = 1.30, 95% confidence interval [CI]: 0.62–1.98, P < .001); females had higher SAI scores than males (5.34; 95% CI: 1.74–8.95, P = .004). Multivariable analysis revealed that females, bad exodontic experience, and higher predicted pain levels were associated with higher IDAF-4C scores. SAI scores (γ = 0.611, P < .001) and TAI scores (γ = 0.305, P < .001) increased as C-IDAF-4C scores increased. Higher C-IDAF-4C scores and longer operative time were significantly associated with higher levels of postoperative pain.
Specific factors are associated with anxiety and stress, and postoperative pain in patients undergoing wisdom teeth extraction. Addressing these factors preoperatively may reduce stress and anxiety, and lead to more favorable treatment outcomes.
Keywords: dental anxiety, extraction, postoperative pain, surgical difficulty, third molar
1. Introduction
Among all dental procedures, wisdom tooth extraction produces the highest levels of dental anxiety and feelings of dread.[1,2] The mandibular third molars, commonly called wisdom teeth, erupt at an average age of 18 to 20 years. Horizontal impaction of the wisdom teeth refers to an angle of 0° to 30° formed by the occlusion line of the second molar and the vertical axis of the third molar.[3,4] The narrow gap between the second and third molars of horizontally impacted wisdom teeth makes oral hygiene difficult, and long-term poor dental hygiene may lead to harmful complications, including inflammation, pain, tooth decay, periodontal disease, and infection.[5–7] To prevent these complications, dental surgeons perform complex surgeries to extract third molars, sometimes involving bone removal and tooth sectioning.[6] Patient fear and anxiety may greatly increase the difficulty of extraction, prolong operative time, and increase postoperative pain.[5,8]
Anxiety can be classified as either state anxiety or trait anxiety.[9,10] State anxiety describes the experience of short-term or temporary psychological discomfort in certain specific situations such as during an academic examination or while waiting to see a doctor. The occurrence and intensity of state anxiety are associated with the individual's subjective perception of situation-specific stimulus. However, when the circumstances that induced the anxiety are removed, state anxiety will resolve. In contrast, trait anxiety describes a long-term psychological state, or personality trait that develops usually through unfavorable living environments experienced during childhood, and it produces persistent stress or worry in many different situations.[10] Dental anxiety and fear of pain are typically classified as trait anxiety. Accordingly, scholars commonly use the State-Trait Anxiety Inventory (STAI) as a survey instrument in the study of dental anxiety.[9–12]
Anxiety and fear may involve changes in a patient's emotions and behavior, as well as their physical and cognitive status.[13] The measurement of dental anxiety and fear must evaluate these 4 aspects of anxiety to understand levels of fear and anxiety before undergoing dental procedures. We hypothesized that the extraction of wisdom teeth may be facilitated when dental personnel fully understand the source of patients’ anxiety and discomfort, and addressing these issues may ultimately reduce patients’ anxiety and postoperative pain.
Thus, the aims of the present study were to develop a Chinese version of the Index of Dental Anxiety and Fear-4C (C-IDAF-4C), validate it against the Chinese STAI, and to evaluate levels of dental anxiety and fear in patients undergoing extraction of horizontally impacted wisdom teeth, and to identify associations between dental anxiety and postoperative pain.
2. Methods
2.1. Patients
This prospective observational study recruited dental outpatients at a medical center in New Taipei, Taiwan, by asking them to participate voluntarily during regular outpatient visits. Purposeful sampling was used to determine the willingness of subjects to participate. Those who volunteered were asked to complete a questionnaire survey. Inclusion criteria were diagnosis of horizontally impacted mandibular third molars requiring extraction; age 20 years or older; and agreed to participate in the questionnaire survey. Exclusion criteria were as follows: could not communicate in Mandarin or Minnan Chinese dialects; prison inmates, indigenous ethnicity, pregnant, persons with disabilities, persons with mental illness or cancer; oral infection and inflammation; and presence of systemic disease based on the American Society of Anesthesiologists (ASA) classification of physiological status. This study only included ASA I or II patients, where ASA I consisted of normal healthy subjects, and ASA II consisted of subjects with mild, well-controlled systemic diseases, including mild hypertension, diabetes, and obesity.[14] All enrolled subjects provided demographic information and answered questions concerning anxiety, dental experiences, degree of pain before tooth extraction, and expected postoperative pain (highest expected level of postoperative pain). All patients underwent third molar extraction using the envelope flap (Koener incision) procedure.[15] All procedures were performed by the same surgeon, and this surgeon evaluated the difficulty of the procedure based on the Pell & Gregory (P&G) classification.[16] The surgeon was blinded to the results of the questionnaires. A researcher recorded the length of surgery (after receiving anesthesia, the time of the procedure was defined as the time the dentist used a scalpel to separate the tissue from the teeth and began third molar extraction procedures to the completion of extraction, excluding suture time). Postoperatively, patients were prescribed amoxicillin 500 mg, tid, and acetaminophen 500 mg, as needed.
2.2. Data collection and instruments
Patients were asked to complete a 2-stage survey. In the waiting room, before undergoing wisdom tooth extraction, they completed a questionnaire concerning demographic information, state and trait anxiety, dental anxiety and fear, dental experience, and preoperative pain. In the second stage, during each day of the 8 day period from the day of surgery to the time of follow-up and suture removal, the patients recorded their level of pain for that day, the number of analgesic pills taken, and the number of antibiotic pills taken. The patients returned the questionnaire on the day of their follow-up. If patients did not return to the hospital for follow-up, they were contacted by telephone and interviewed regarding their postoperative pain and other information.
Three questionnaires were completed by all enrolled patients.
2.3. State-trait anxiety inventory
The STAI scale was translated into Chinese in 1984 by Chung and Lung (1984), which resulted in the Chinese version of the STAI (C-STAI).[17] The C-STAI scale contains 40 questions, and scores are calculated using a 4-point scale where 1 point indicates not at all, 2 points indicates a bit, 3 points indicate somewhat, and 4 points indicates extremely. The state anxiety and trait anxiety scales both have possible total scores of 80 points, and the higher the score, the greater the degree of anxiety. The Chinese state anxiety inventory (C-SAI) has test-retest reliability of 0.737, and the Cronbach alpha for internal consistency is 0.859. The Chinese trait anxiety inventory (C-TAI) has test-retest reliability of 0.755, and the Cronbach alpha for internal consistency is 0.898.[17] Authors of this study received authorization from Professor Chung for use of the Chinese version of the STAI.
2.4. Developing a Chinese version of the index of dental anxiety and fear
To determine the validity of the expert content of the Chinese version of the IDAF-4C (C-IDAF-4C, 3 clinical dental specialists, including 2 general attending doctors of dentistry and 1 general dental resident, were asked to assess the appropriateness, importance, and clarity of the C-IDAF-4C scale based on the research goals and the English version, and grade each question. Expert validity was calculated on the basis of the content validity index (CVI), and each question was graded using a 5-point scale, with 1 point indicating “extremely poor,” which expressed that the question content was meaningless and should not be included, 2 points indicating “poor,” which expressed that the content should be extensively revised; 3 points indicating “fair,” which expressed that the question should be partially revised; 4 points indicating “very good,” which expressed that the content was important, but the question must be partially revised; and 5 points indicating “extremely good,” which expressed that the content was extremely important and applicable. The questionnaire as a whole had a CVI of 0.875, which was >0.8 and indicated that the questionnaire had excellent expert validity.
Fifty dental patients took the pilot test, and SPSS 20.0 was used to calculate the internal consistency (Cronbach alpha) of the C-IDAF-4C. The questionnaire had a Cronbach alpha of 0.932, which was >0.7 indicating the questionnaire was stable, reliable, and possessed consistency.
2.5. Numeric rating scale
Pain can be assessed using a Numeric Rating Scale (NRS).[18] The NRS pain scale includes 11 levels of pain (NRS-11), which are assigned grades of 0 to 10. This scale is used to assess subjective impressions of pain. On this scale, 0 indicates no pain whatsoever, and 10 indicates extreme pain. Each number represents a certain level of pain among a total of 11 levels.
2.6. Ethical considerations
The study protocol was approved by the research ethics review committee at the Far Eastern Memorial hospital and complied with guidelines of the Declaration of Helsinki. All patients provided signed informed consent to participate.
2.7. Statistical analysis
Sample size calculation was done before the study. A total of 116 participants were required to detect an effect size of 0.2 with a multiple linear regression including 18 variables (all variables listed in Table 5), and a significant level of 0.05 and a power of 0.8.
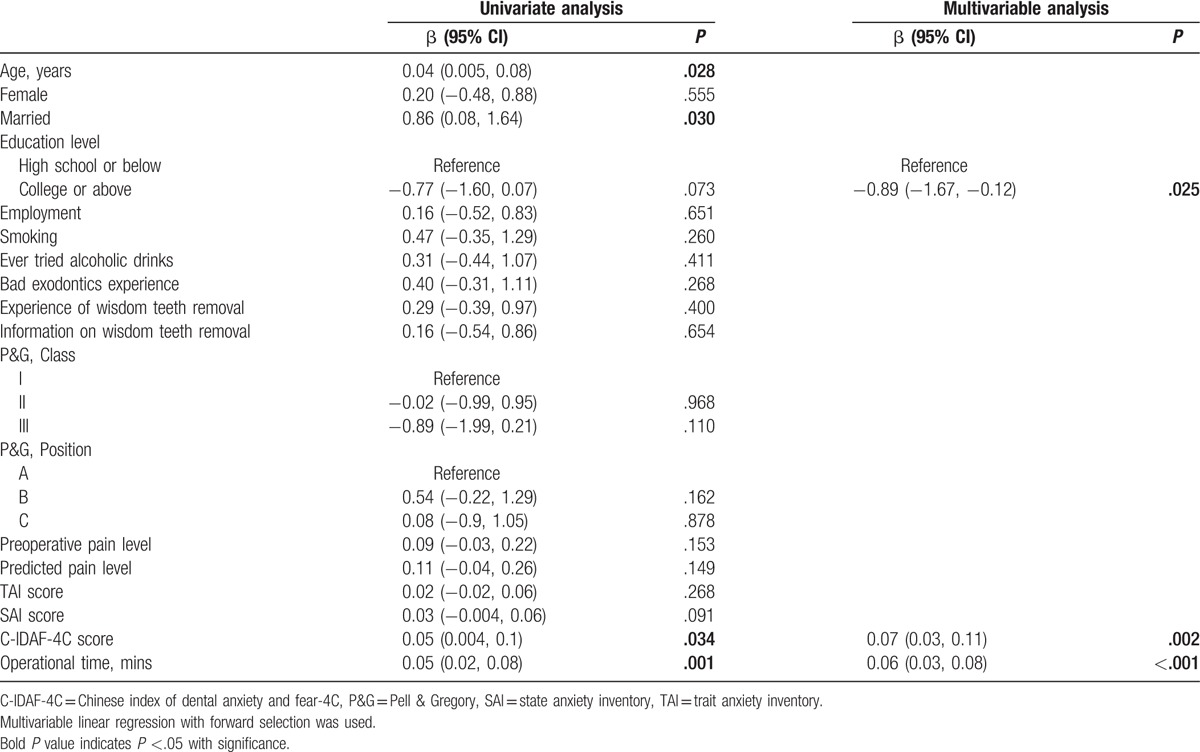
Table 5.
Effectors of postoperative pain.
Patient characteristics were reported as mean and standard deviation, or number and percentage. Pearson coefficients were calculated to quantify the associations between SAI and TAI scores with that of the C-IDAF-4C. Five levels of correlation were defined according to the Pearson correlation coefficient (γ), including very weak (γ < 0.2), weak (0.2 ≤ γ < 0.4), moderate (0.4 ≤ γ < 0.6), strong (0.6 ≤ γ < 0.8), and very strong (γ ≥ 0.8). The linear regression model was used to analyze associations between dependent variables and SAI, TAI, C-IDAF-4C or postoperative pain levels. Parameters with P ≤.1 revealed by univariate analysis were then put into a multivariable regression model, and results of the final model were determined after a backward or forward selection procedure. The level of significance for all tests was set to 5%. All statistical analyses were 2-sided, and performed using PASW software (version 21.0, IBM Corp., Armonk, NY).
3. Results
3.1. Patient characteristics
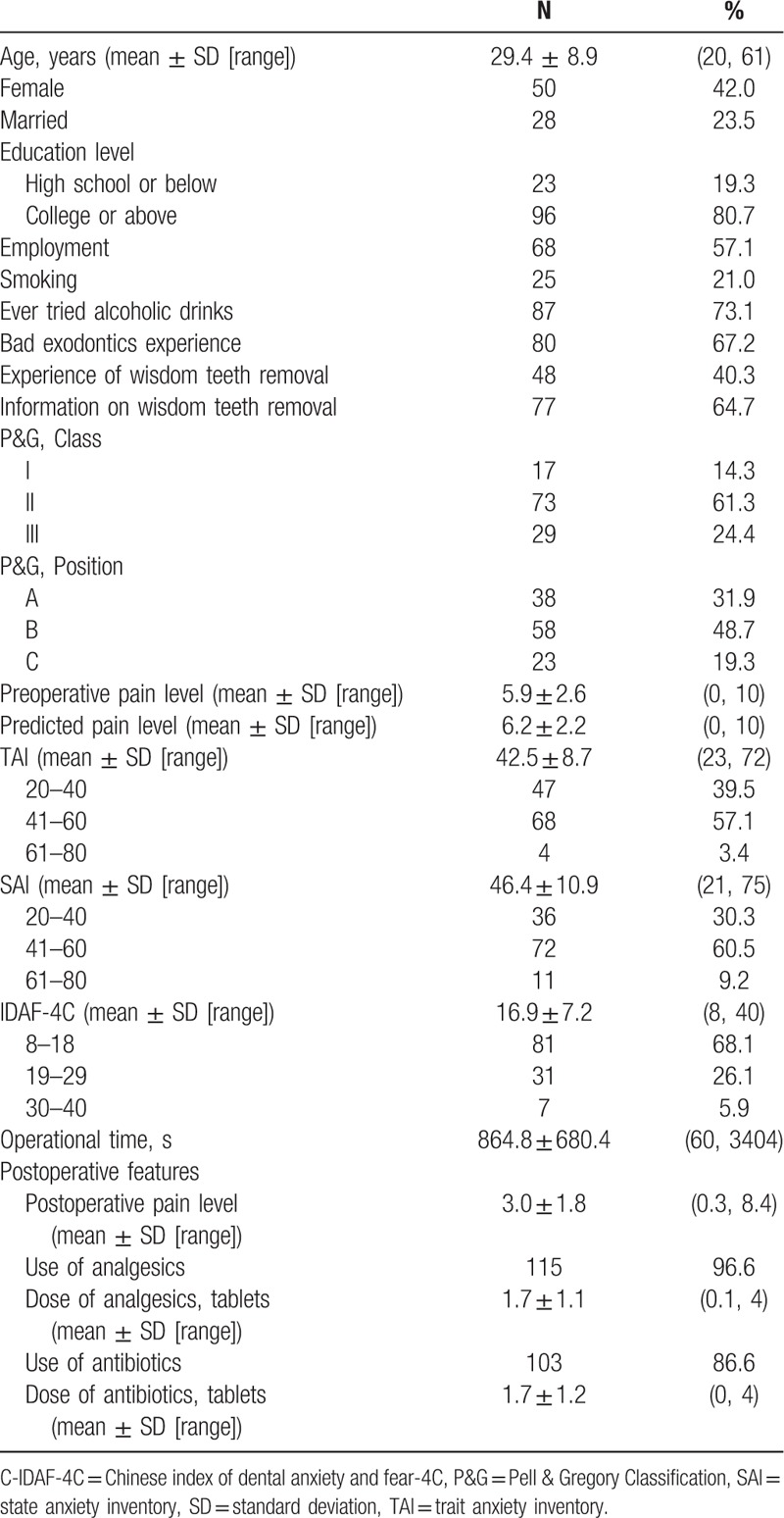
A total of 119 patients with a mean age of 29.4 ± 8.9 (range: 20–61) years were enrolled, and 42% were female (Table 1). More than half of patients (67/2%) reported bad experiences with exodontics. The most common P&G class was class II (61.3%). The mean preoperative pain level score was 5.9 ± 2.6, predicted pain level was 6.2 ± 2.2, SAI score was 42.5 ± 8.7, TAI score was 46.4 ± 10.9, and C-IDAF-4C score was 16.9 ± 7.2. Operative time ranged from 60 to 3404 seconds, and most patients took analgesics (96.6%) or antibiotics (86.6%) after the surgery. The mean postoperative pain level score was 3.0 ± 1.8 (range: 0.3–8.4) (Table 1).
Table 1.
Patient characteristics.
3.2. Measurements
Table 2 shows the effectors of TAI, and only 1 factor, collecting information about wisdom teeth removal, was related to a lower TAI score. Univariate analysis indicated that higher SAI scores were associated with female sex, higher levels of preoperative pain, and higher predicted pain (Table 2). In multivariable analysis, the SAI predicted pain level was eliminated from the final model, but marriage and information of wisdom teeth removal were included. The SAI scores in females were 5.34 points (95% confidence interval [CI]: 1.74–8.95, P = .004) higher than in males, and the SAI scores increased as preoperative pain level increased (β = 1.30, 95% CI: 0.62–1.98, P < .001). However, in patients who were married and those who obtained information before receiving wisdom teeth extraction, SAI scores were 5.65 points (95% CI: −9.82 to −1.49, P = .008) lower than in those not married and 3.96-points (95% CI: −7.66 to −0.27, P = .036) in those who did not seek information before tooth extraction (Table 3).
Table 2.
Univariate analyses for trait anxiety inventory (TAI), state anxiety inventory (SAI), and Chinese index of dental anxiety and fear-4C (C-IDAF-4C).
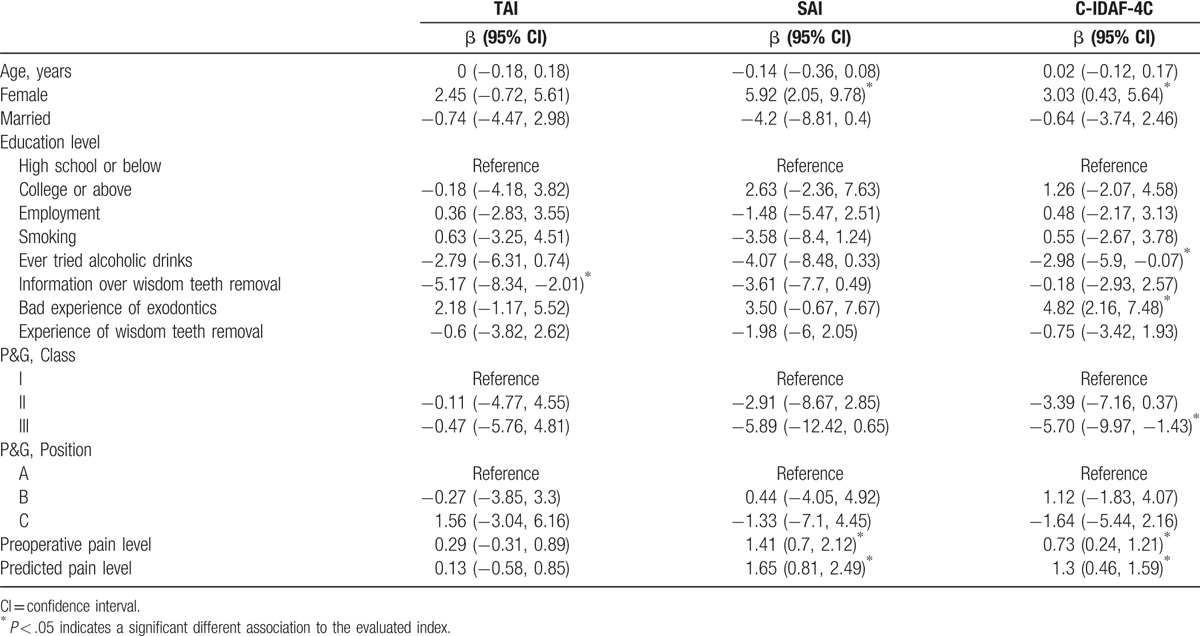
Table 3.
Multivariable analysis for state anxiety inventory (SAI) and Chinese index of dental anxiety and fear-4C (C-IDAF-4C).
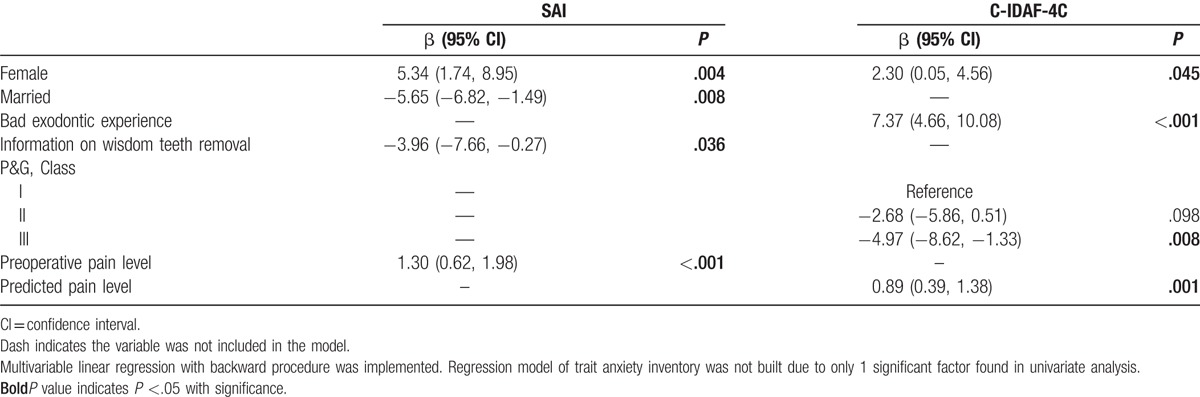
Four parameters were found to affect C-IDAF-4C score (Table 3). Multivariable analysis revealed that females sex (β = 2.30, 95% CI: 0.05–4.56, P = .045), prior bad experience of exodontics (β = 7.37, 95% CI: 4.66–10.08, P < .001), and higher predicted pain level (β = 0.89, 95% CI: 0.39–1.38, P = .001) were associated with increased C-IDAF-4C score. However, P&G class III patients had lower C-IDAF-4C scores than class I patients (β = −4.97, 95% CI: −8.62 to −1.33, P = .008) (Table 3).
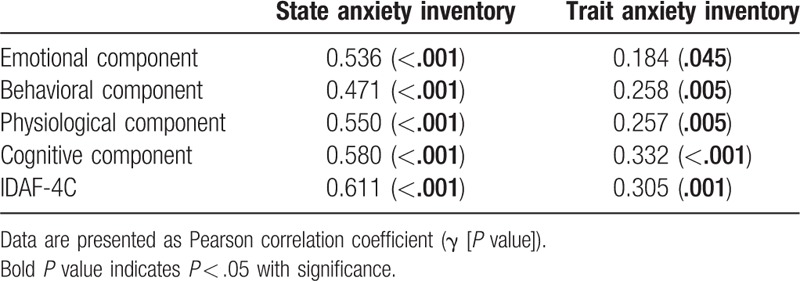
Correlations among SAI, TAI, and C-IDAF-4C scores are shown in Table 4. SAI scores (γ = 0.611, P < .001) and TAI scores (γ = 0.305, P < .001) increased as C-IDAF score increased, and decreased as C-IDAF-4C score decreased. SAI and TAI items were found to be correlated with C-IDAF-4C score (Table 4). The effectors of postoperative pain are summarized in Table 5. Higher C-IDAF-4C scores (β = 0.07, 95% CI: 0.03–0.11, P = .002) and longer surgical time (β = 0.06, 95% CI: 0.03–0.08, P < .001) were significantly associated with higher levels of postoperative pain. Higher education level was associated with lower postoperative pain (β = −0.89, 95% CI: −1.67 to −0.12, P = .025) (Table 5).
Table 4.
Correlations between state-trait anxiety inventory (STAI) and Chinese index of dental anxiety and fear-4C (C-IDAF-4C).
4. Discussion
This was the first study to develop a Chinese version of the IDAF-4C (C-IDAF-4C), and showed that it exhibited good consistency with the Chinese STAI. The present study also showed a correlation between increases in mean scores of fear and anxiety scales and increased postoperative pain levels in patients undergoing wisdom teeth extraction. These results are in agreement with those of other authors who reported significant correlations between dental anxiety and fear and postoperative pain.[19,20] A high degree of patient anxiety inevitably increases the complexity of dental procedures, and may also decrease patient compliance with and understanding of instructions.[21] Dental anxiety may even reduce the willingness to seek dental care.[7] However, the multifaceted aspects of anxiety and fear were not considered in some of the earlier methods of measuring dental anxiety, and these 2 emotions are typically expressed via various overlapping responses.[22] For these reasons, the IDAF-4C[23] takes a comprehensive approach and includes a scale of dental anxiety and fear (IDAF-4C), scale of dental phobia (IDAF-P), and scale of feared dental stimuli (IDAF-S). We found that the 8 questions from the IDAF-4C could effectively assess levels of dental anxiety and fear. This may allow dental personnel to gauge a patient's dental anxiety and fear preoperatively, and address the concerns with them. Patients with high trait anxiety, in particular, are relatively motivated to seek relevant treatment and prognostic information. Some Western studies have effectively used the Amsterdam Preoperative Anxiety and Information Scale (APAIS) as a preoperative anxiety and information assessment instrument.[24,25] The APAIS is highly consistent with the STAI used in the present study.
Other investigators have used the STAI to gauge anxiety prior to explaining an oral surgical procedure, and relationship to postoperative pain and daily analgesic use.[25] The study showed that patients with trait anxiety had approximately twice the dental state anxiety of patients with no trait anxiety, and no significant positive correlation between postoperative pain and state anxiety. As in our study, patients with relatively high levels of trait anxiety tended to take more analgesics, and a significant correlation was found between high state anxiety and swallowing water during the first 3 days after surgery. As in our study, these results suggest that persons with high levels of dental anxiety tend to perceive high levels of pain, which can influence physiological recovery after surgery.[26]
In the present study, multivariable analysis revealed that females with previous bad exodontic experience and higher predicted pain levels were most likely to have higher C-IDAF-4C scores. Previous studies have also indicated that poor dental care experiences correlate with high levels of dental anxiety.[2,27,28] Unpleasant dental experiences during childhood are particularly memorable, and are difficult to accept and overcome, carrying greater negative influences than unpleasant dental care experiences during adulthood.[27] The frequency of previous unpleasant dental experiences also correlates significantly with levels of dental anxiety during a 4-week postoperative period,[16] suggesting that unpleasant previous dental experiences may have a long-term influence on perceptions of dental treatment.
We found that patients with high levels of state anxiety anticipated high levels of surgical pain. Similarly, other studies have found that persons with high levels of state anxiety and dental anxiety tended to anticipate high levels of surgical pain and postoperative pain.[28,29] The anticipated pain, however, does not correlate with measures of actual postoperative pain, and may actually be greater than the actual pain.[28] It is evident that a high anxiety level transforms the surgical treatment process into a high-stress situation, which may even affect medical care-seeking behavior, and may cause avoidance of treatment.[30]
The present study found that longer duration of surgery was associated with greater postoperative pain, a result consistent with that of a prior Western study.[31] Longer surgical time also correlates significantly with other postoperative complications, such as swelling and clenching of the teeth due to prolonged injuries to tissues, while shorter surgical time is associated with reduced analgesic consumption.[32]
4.1. Limitations
This study has certain relatively minor limitations. The majority of patients undergoing extraction of horizontally impacted third molars were between 20 and 30 years of age (60.5%). As a result, the patients had similar demographic characteristics, which may make it difficult to extend the results of this study to other age groups, and patients receiving other types of dental treatment. In addition, while the patients in this study had relatively high levels of dental anxiety, this does not necessarily reflect the psychological states of the general public. We focused on horizontally impacted wisdom teeth extraction because it is one of the most difficult procedures, and in general there is anxiety regarding the wisdom teeth extraction. There are many types of extractions, and the results may or may not be generalizable to other procedures. Postoperative medication use was self-reported, and there may be inaccuracies in the recorded information.
5. Conclusions
The C-IDAF-4C was developed and validated against the STAI. When patients are undergoing wisdom teeth extraction, a stressful and complex dental surgery, trait dental anxiety, especially individual variation in the cognitive and behavioral domains, is a clinically important indicator of postoperative pain. Female sex, previous bad experience with dental procedures, and preoperative discomfort were all associated with anxiety. Understanding of these factors may assist dental personnel in reducing patient dental stress and anxiety, and improve treatment outcomes.
Footnotes
Abbreviations: APAIS = Amsterdam Preoperative Anxiety and Information Scale, ASA = American Society of Anesthesiologists, CI = confidence interval, CVI = content validity index, IDAF = Index of Dental Anxiety and Fear, NRS = Numeric Rating Scale, P&G = Pell & Gregory, SAI = state anxiety inventory, STAI = State-Trait Anxiety Inventory, TAI = trait anxiety inventory.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
The authors declare that there are no conflicts of interest related to this study.
References
- [1].Kazancioglu HO, Tek M, Ezirganli S, et al. Does watching a video on third molar surgery increase patients’ anxiety level? Oral Surg Oral Med Oral Pathol Oral Radiol 2015;119:272–7. [DOI] [PubMed] [Google Scholar]
- [2].Sirin Y, Humphris G, Sencan S, et al. What is the most fearful intervention in ambulatory oral surgery? Analysis of an outpatient clinic. Int J Oral Maxillofac Surg 2012;41:1284–90. [DOI] [PubMed] [Google Scholar]
- [3].Santosh P. Impacted mandibular third molars: review of literature and a proposal of a combined clinical and radiological classification. Ann Med Health Sci Res 2015;5:229–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Singh V, Alex K, Pradhan R, et al. Techniques in the removal of impacted mandibular third molar: a comparative study. Eur J Gen Dent 2013;2:25–30. http://www.ejgd.org/temp/EurJGenDent2125-1302959_033709.pdf [Google Scholar]
- [5].Aznar-Arasa L, Figueiredo R, Valmaseda-Castellon E, et al. Patient anxiety and surgical difficulty in impacted lower third molar extractions: a prospective cohort study. Int J Oral Maxillofac Surg 2014;43:1131–6. [DOI] [PubMed] [Google Scholar]
- [6].Susarla SM, Dodson TB. Risk factors for third molar extraction difficulty. J Oral Maxillofac Surg 2004;62:1363–71. [DOI] [PubMed] [Google Scholar]
- [7].Zuniga JR. Guidelines for anxiety control and pain management in oral and maxillofacial surgery. J Oral Maxillofac Surg 2000;58(suppl 2):4–7. [DOI] [PubMed] [Google Scholar]
- [8].Lago-Mendez L, Diniz-Freitas M, Senra-Rivera C, et al. Relationships between surgical difficulty and postoperative pain in lower third molar extractions. J Oral Maxillofac Surg 2007;65:979–83. [DOI] [PubMed] [Google Scholar]
- [9].Dao J, Zhang J, Song G, et al. Effect of preoperative anxiety level on postoperative pain sensation in patients receiving implant denture for partial edentulism. Nan Fang Yi Ke Da Xue Xue Bao 2014;34:528–31. [in Chinese]. [PubMed] [Google Scholar]
- [10].Spielberger CD, Lushene RE. Manual for the State-Trait Anxiety Inventory. Palo Alto, CA: Consulting Psychologists Press; 1983. [Google Scholar]
- [11].Kazancioglu HO, Dahhan AS, Acar AH. How could multimedia information about dental implant surgery effects patients’ anxiety level? Med Oral Patol Oral Cir Bucal 2017;22:e102–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Yildirim TT, Dundar S, Bozoglan A, et al. Is there a relation between dental anxiety, fear and general psychological status? PeerJ 2017;5:e2978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kneeland ET, Dovidio JF, Joormann J, et al. Emotion malleability beliefs, emotion regulation, and psychopathology: Integrating affective and clinical science. Clin Psychol Rev 2016;45:81–8. [DOI] [PubMed] [Google Scholar]
- [14].American Society of Anesthesiologists (ASA). ASA physical status classification system. 2014. Available at: https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system. Accessed June 30, 2016. [Google Scholar]
- [15].Pell GJ. Impacted mandibular third molars: classification and modified techniques for removal. Dental Dig 1933;39:330–8. [Google Scholar]
- [16].Chung SC. Revision of the State-Trait Anxiety inventory. Testing Yearbook of the Chinese Association of Psychological Testing 1984;31: http://tci.ncl.edu.tw/cgi-bin/gs32/gsweb.cgi?o=dnclresource&s=id=%22A83024003%22.&searchmode=basic&tcihsspage=tcisearch_opt1_searchhttp://tci.ncl.edu.tw/cgi-bin/gs32/gsweb.cgi?o=dnclresource&s=id=%22A83024003%22.&searchmode=basic&tcihsspage=tcisearch_opt1_search (chinese version). Accessed November 14, 2014. [Google Scholar]
- [17].Hartrick CT, Kovan JP, Shapiro S. The numeric rating scale for clinical pain measurement: a ratio measure? Pain Pract 2003;3:310–6. [DOI] [PubMed] [Google Scholar]
- [18].Lin CS, Wu SY, Yi CA. Association between anxiety and pain in dental treatment. J Dent Res 2017;96:153–62. [DOI] [PubMed] [Google Scholar]
- [19].Kyle BN, McNeil DW, Weaver B, et al. Recall of dental pain and anxiety in a cohort of oral surgery patients. J Dent Res 2016;95:629–34. [DOI] [PubMed] [Google Scholar]
- [20].Eli I, Schwartz-Arad D, Bartal Y. Anxiety and ability to recognize clinical information in dentistry. J Dent Res 2008;87:65–8. [DOI] [PubMed] [Google Scholar]
- [21].Stouthard MEA, Hoogstraten GJ. Assessment of dental anxiety: a facet approach. Anxiety Stress Coping 1993;6:89–105. [Google Scholar]
- [22].Armfield JM. Development and psychometric evaluation of the Index of Dental Anxiety and Fear (IDAF-4C+). Psychol Assess 2010;22:279–87. [DOI] [PubMed] [Google Scholar]
- [23].Moerman N, van Dam FS, Muller MJ, et al. The Amsterdam Preoperative Anxiety and Information Scale (APAIS). Anesth Analg 1996;82:445–51. [DOI] [PubMed] [Google Scholar]
- [24].Nishimori M, Moerman N, Fukuhara S, et al. Translation and validation of the Amsterdam preoperative anxiety and information scale (APAIS) for use in Japan. Qual Life Res 2002;11:361–4. [DOI] [PubMed] [Google Scholar]
- [25].Torres-Lagares D, Recio-Lora C, Castillo-Dali G, et al. Influence of state anxiety and trate anxiety in postoperative in oral surgery. Med Oral Patol Oral Cir Bucal 2014;19:e403–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Locker D, Liddell A, Shapiro D. Diagnostic categories of dental anxiety: a population-based study. Behav Res Ther 1999;37:25–37. [DOI] [PubMed] [Google Scholar]
- [27].Muglali M, Komerik N. Factors related to patients’ anxiety before and after oral surgery. J Oral Maxillofac Surg 2008;66:870–7. [DOI] [PubMed] [Google Scholar]
- [28].Brignardello-Petersen R. Previous bad experience, propensity to anxiety, and pain expectations may be associated with fear and anxiety when undergoing tooth extractions. J Am Dent Assoc 2017;148:e4. [DOI] [PubMed] [Google Scholar]
- [29].Heyman RE, Slep AM, White-Ajmani M, et al. Dental fear and avoidance in treatment seekers at a large, urban dental clinic. Oral Health Prev Dent 2016;14:315–20. [DOI] [PubMed] [Google Scholar]
- [30].de Santana-Santos T, de Souza-Santos aA, Martins-Filho PR, et al. Prediction of postoperative facial swelling, pain and trismus following third molar surgery based on preoperative variables. Med Oral Patol Oral Cir Bucal 2013;18:e65–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Gopalraju P, Lalitha RM, Prasad K, et al. Comparative study of intravenous Tramadol vs. Ketorolac for preventing postoperative pain after third molar surgery-a prospective randomized study. J Cranio Maxillofac Surg 2014;42:629–33. [DOI] [PubMed] [Google Scholar]
- [32].Desai A, Patel R, Desai K, et al. Comparison of two incision designs for surgical removal of impacted mandibular third molar: A randomized comparative clinical study. Contemp Clin Dent 2014;5:170–4. [DOI] [PMC free article] [PubMed] [Google Scholar]


