Abstract
Introduction:
Neuroendocrine carcinoma was a rare kind tumor in gallbladders. So far, there is no consensus of treatment of the gallbladder neuroendocrine carcinoma.
Case presentation:
Three patients, 1 male and 2 females, were admitted in our hospital because of right upper quadrant pain. No one complained fever, jaundice, weight loss, or carcinoid syndrome-related symptoms such as diarrhea, flushing, edema, and wheezing. The MRI detected the broad base of gallbladder tumors. However, they refused any radical surgery. We performed a laparoscopic cholecystectomy with gallbladder bed cautery. The pathology results showed that 2 cases were mixed neuroendocrine carcinoma (NECs), and 1 case was a simple NEC. Chromogranin A and synaptophysin were positive in all cases. The pathological TNM stages of all patients were in the T1bN0M0 stage. The range of Ki-67 was from 40% to 80%. During the at least 26 months’ follow-up, there is no case with the recurrence of the carcinoma without any chemotherapy or radiotherapy.
Conclusions:
Cholecystectomy with gallbladder bed cautery might be enough for treatment of T1bN0M0 gallbladder neuroendocrine carcinoma.
Keywords: cholecystectomy, gallbladder, neuroendocrine carcinoma, neuroendocrine tumor, surgery
1. Introduction
Neuroendocrine tumor (NET) is a rare type of carcinoma with the incidence of about 5.25 per 100,000.[1] It had been found in many organs, such as lungs, thyroid, jejunum, ileum. and pancreas, gallbladder NET was seldom reported.[2] According to a survey hosted by National Cancer Institute, the incidence of gallbladder NET was <0.74/100,000.[1] Neuroendocrine carcinoma (NEC) is a kind of poorly differentiated NET or high-grade G3 NET (mitotic count >20 per 10 high power fields and/or >20% Ki-67 index) according to the 2010 WHO classification. Because of a number of reasons, including the rarity of the disease, there is no consensus of treatments of the gallbladder NEC.
Traditionally, the treatment of NEC referred to the treatment of gallbladder cancers in clinical practice. In general, a simple cholecystectomy is sufficient therapy for early tumors, confined to the mucosa (T1a).[3] Whereas the therapeutic modality for gallbladder tumors, which is a higher grade than T1b (muscularis proper), is a radical operation, including cholecystectomy, partial hepatectomy around the gallbladder bed and dissection of regional lymph nodes.[4] However, we had dealt with 3 T1bN0M0 gallbladder NEC cases, they all accept laparoscopic cholecystectomy with gallbladder bed cautery, and have no recurrence of the carcinoma during the at least 26 months’ follow-up.
2. Case presentation
These 3 gallbladder neoplasm cases (1 male and 2 females) were admitted in our hospital because of right upper quadrant pain (Table 1). No one complained fever, jaundice, weight loss, or carcinoid syndrome-related symptoms such as diarrhea, flushing, edema, and wheezing. No positive results of physical examination were found. The MRI detected the broad base of gallbladder tumors (Fig. 1). We planned to perform a radical cholecystectomy if the frozen pathology was positive during the operation. However, these patients refused the radical surgery. After getting their informed consents and the approval of the Ethics Committee of our hospital, we performed a laparoscopic cholecystectomy with gallbladder bed cautery. The whole gallbladder bed was cauterized for at least 30 seconds using active electric L-hook, which was connected with Monopolar radiofrequency energy (Force FX, Covidien, Boulder, CO) on 40 W “Desiccate” coagulation mode. Pathology results showed that 2 cases were mixed NECs (NEC and adenoma), and 1 case was a simple NEC. Chromogranin A (CgA) and synaptophysin were positive in all cases (Fig. 1). The range of Ki-67 was from 40% to 80%. The pathological TNM stages of all patients were in the T1bN0M0 stage, and the tumor resection boundary was negative in all 3 patients.
Table 1.
Clinical features of 3 cases of neuroendocrine carcinoma.
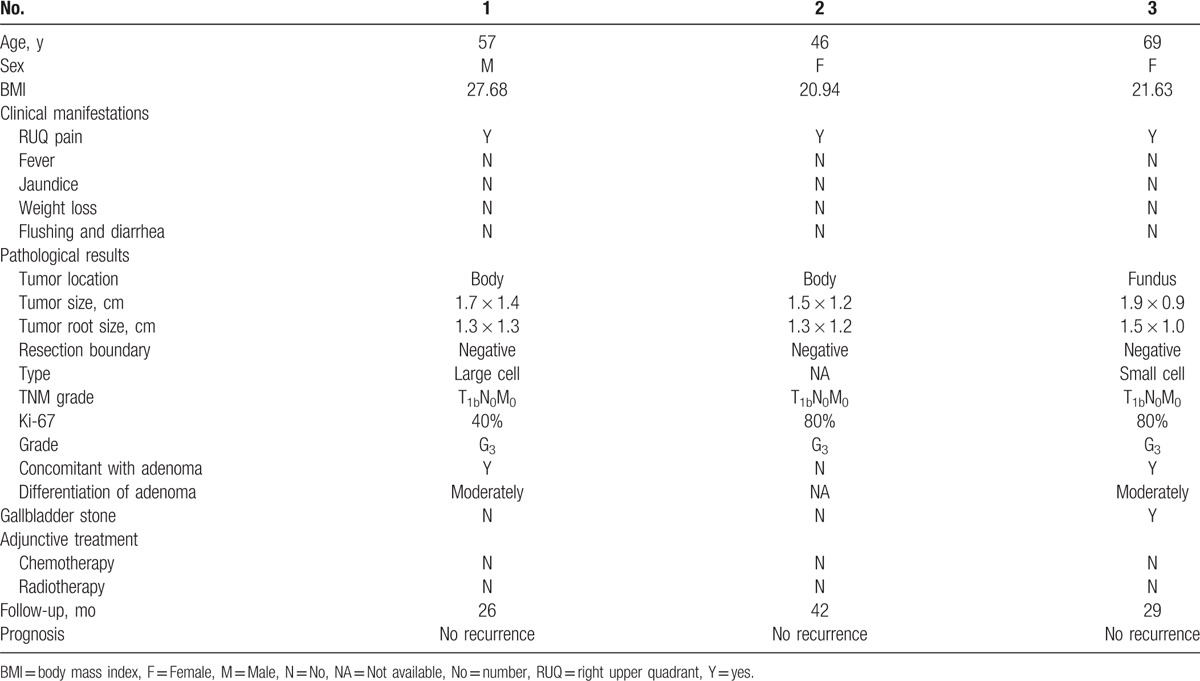
Figure 1.
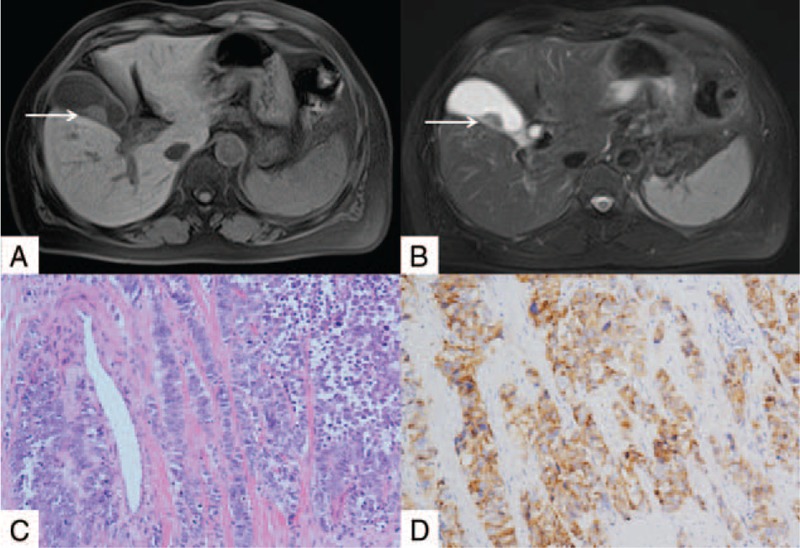
Magnetic resonance imaging (MRI) and pathological results of gallbladder neuroendocrine carcinoma. (A and B) The MRI images of gallbladder. The arrow showed the broad base of gallbladder tumors and the intact of the gallbladder wall. (C) Hematoxylin and eosin staining of carcinoma tissues form gallbladder (200×). (D) CgA staining shows CgA-positive cancer cells (200×). The confirmative diagnosis of neuroendocrine carcinoma of gallbladder relies on the pathological results.
Considering the negative found of metastasis, these 3 patients also insisted on no chemotherapy or radiotherapy. Therefore, they were closely followed-up. The longest follow-up period is 42 months in a 46-year-old female patient. Even the shortest follow-up period is >26 months in a 57-years-old male patient. Up to now, they all have no recurrence of NEC.
3. Discussion and conclusions
There is no consensus of treatment of gallbladder NEC. This might be because of the rarity of the disease, the lack of predictive prognostic factors, and the limited understanding of the biology of the disease. A multicenter study assessed the clinicopathological features, therapeutic approaches, and prognosis of as much as 43 biliary NET patients, but the optimal treatment and prognoses were still not well established.[5] The treatment of the NEC referred to the treatment of gallbladder cancers in clinical practice. However, for the stage of T1bN0M0 gallbladder cancer, there are also many controversies about the surgical strategy.[6] Radical resections were widely performed for T1b tumors because residual cancer in the resected gallbladder bed was identified in many cases.[6] In a study of 115 cases of resection after previous cholecystectomy, 46% of patients had residual disease in the resection specimen on final histologic analysis.[7] However, some series support a simple cholecystectomy as a sufficient management for T1b cancers. After all, the tumor did not invade the gallbladder bed. Lee et al[8] analyzed 29 relevant publications involved 560 patients, found that there is no definite evidence that radical cholecystectomy is advantageous over simple cholecystectomy for T1b gallbladder cancer.
Moreover, most NECs are relatively slow-growing neoplasms and clinically less aggressive than adenocarcinomas.[9] The mixed NECs in our cases are mixture of NEC and adenoma, not the mixed adenoneuroendocrine carcinoma according to the 2010 WHO classification.[10] Although the NEC was poorly differentiated, the tumor resection boundary was negative in all 3 patients. Besides, we performed the gallbladder bed cautery after cholecystectomy, which might kill the possible residual tumor cells. The prognosis of these 3 patients could explain the effectiveness of the strategy. There is no case with no recurrence after at least 26 months’ follow-up without postsurgical chemotherapy. It is much longer than the progression-free survival and the survival time reported previously. Lee et al[5] collected 11 NECs of gallbladder patients, found that the median overall survival time was 7.9 months, and the median progression free survival time was 5.1 months. Duffy et al reported that the median survival of the cohort of 13 gallbladder NEC patients was 9.8 months.[11] Therefore, cholecystectomy with gallbladder bed cautery might be sufficient for treatment of T1bN0M0 gallbladders NEC. Although the size of our report is limited and further larger studies are needed, the result will be very meaningful for surgeons to make a decision that no more surgery would be needed when the T1bN0M0 NEC is incidental found after cholecystectomy.
Footnotes
Abbreviations: CgA = Chromogranin A, MRI = magnetic resonance imaging, NEC = neuroendocrine carcinoma, NET = neuroendocrine tumor, WHO = World Health Organization.
WL and WC contributed equally to this work
The authors report no conflicts of interest.
References
- [1].Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol 2008;26:3063–72. [DOI] [PubMed] [Google Scholar]
- [2].Chen C, Wang L, Liu X, et al. Gallbladder neuroendocrine carcinoma: report of 10 cases and comparision of clinicopathologic features with gallbladder adenocarcinoma. Int J Clin Exp Pathol 2015;8:8218–26. [PMC free article] [PubMed] [Google Scholar]
- [3].Eltawil KM, Gustafsson BI, Kidd M, et al. Neuroendocrine tumors of the gallbladder: an evaluation and reassessment of management strategy. J Clin Gastroenterol 2010;44:687–95. [DOI] [PubMed] [Google Scholar]
- [4].Sikora SS, Singh RK. Surgical strategies in patients with gallbladder cancer: nihilism to optimism. J Surg Oncol 2006;93:670–81. [DOI] [PubMed] [Google Scholar]
- [5].Lee KJ, Cho JH, Lee SH, et al. Clinicopathological characteristics of biliary neuroendocrine neoplasms: a multicenter study. Scand J Gastroenterol 2017;52:437–41. [DOI] [PubMed] [Google Scholar]
- [6].Zhu AX, Hong TS, Hezel AF, et al. Current management of gallbladder carcinoma. Oncologist 2010;15:168–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Pawlik TM, Gleisner AL, Vigano L, et al. Incidence of finding residual disease for incidental gallbladder carcinoma: implications for re-resection. J Gastrointest Surg 2007;11:1478–86. [DOI] [PubMed] [Google Scholar]
- [8].Lee SE, Jang JY, Lim CS, et al. Systematic review on the surgical treatment for T1 gallbladder cancer. World J Gastroenterol 2011;17:174–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Caplin ME, Buscombe JR, Hilson AJ, et al. Carcinoid tumour. Lancet 1998;352:799–805. [DOI] [PubMed] [Google Scholar]
- [10].Hu HJ, Zhou RX, Tan YQ, et al. Coexisting cancers: a mixture of neuroendocrine carcinoma and adenocarcinoma in the gallbladder: a case report. Medicine 2016;95:e5281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Duffy A, Capanu M, Abou-Alfa GK, et al. Gallbladder cancer (GBC): 10-year experience at Memorial Sloan-Kettering Cancer Centre (MSKCC). J Surg Oncol 2008;98:485–9. [DOI] [PubMed] [Google Scholar]


